Abstract
Socioeconomic disadvantage has been linked to elevated blood pressure (BP), and the purpose of this study was to assess whether interpersonal social supports buffer these adverse relations in African-American adults. In three communities matched demographically, a subsample of participants (N=204) of the Positive Action for Today’s Health (PATH) trial provided measures of perceived social support, annual household income, and BP. Multiple regression analyses with cross-product interactions were conducted using follow-up data. The sample had a mean age of 52.8 years (SD=15.1), and was predominantly female (66%) with a high body mass index (M=33.5, SD=14.7). Results indicated an inverse relationship between social support and diastolic BP (B=−.178, p=.005), and also an interaction with income (p=.046), such that higher social support related to lower diastolic BP in the lowest-income individuals (B=−1.05). The same direct (B=−.141, p=.025) and interacting (B=−1.42, p=.040) social support effects were present for systolic BP, however the omnibus model for systolic BP was not significant, F(6, 196)=1.80, p=.09. The hypothesized buffering effect of social support on the adverse relation of income to BP was partially supported in at-risk African-American adults. Prevention efforts for reducing the impact of socioeconomic stress on BP may aim to increase perceptions of social support.
Introduction
High blood pressure affects African-American adults more than any other ethnic group in the U.S., and this pervasive health disparity has been linked to socioeconomic disadvantage (Anderson & Armstead, 1995; Go et al., 2014). Currently, 44% of African-American adults suffer from high BP in contrast to 28% of Caucasians (Cutler et al., 2008; Gadegbeku, Lea, & Jamerson, 2005), and chronic exposure to income-related socioeconomic stressors may account in part for this inequality (Johnson et al., 1995). Stress-buffering theory posits that interpersonal social supports may attenuate or buffer the negative impact of socioeconomic stress on health and cardiovascular “wear and tear,” especially in more disadvantaged individuals (Cohen & Wills, 1985; Matthews & Gallo, 2011). The relation of socioeconomic disadvantage (e.g. low-income status) and higher BP and cardiovascular dysfunction is indeed well-established (Adler & Ostrove, 1999), and the link between social support and better cardiovascular health is solid as well (Barth, Schneider, & von Kanel, 2010). However, few studies have examined how social support buffers the negative effects of socioeconomic disadvantage, and none have investigated such interactions relative to a physical health outcome such as blood pressure, in at-risk African-American adults.
The purpose of this study was to test whether perceiving oneself to have greater collective social supports from family, friends, and significant others was protective against the adverse link between low-income status and BP. It was hypothesized that social support and income would be inversely related to BP, and that social support would buffer the impact of income on BP, especially in individuals who had the lowest incomes and were at greatest risk.
Methods
This cross-sectional study used 24-month follow-up data that were collected from a subsample of adults (N=204) participating in the Positive Action for Today’s Health trial (Wilson et al., 2010; Wilson et al., 2014). In 2008 participants were recruited from three matched communities in the southeastern U.S. to participate in the 24-month trial, which aimed to assess the efficacy of an environmental intervention for increasing safety and access for neighborhood physical activity (PA) in at-risk African-American communities. The larger PATH trial resulted increased walking on the neighborhood trail but showed no effects on accelerometry-assessed moderate-to-vigorous PA (MVPA) at the community level (Wilson et al., 2015); these follow-up analyses focused on the secondary outcome of BP, and not the primary outcome of MVPA. Participants were > 18 years old, African American, and had no conditions that would limit moderate activity. Communities experienced high levels of chronic disease, poverty (23–39% of households), and crime relative to state and national averages. Follow-up data assessing perceived social support were collected at the 24-month time point during community health screenings. Health screenings also included collection of blood pressure, annual income, perceived social support, anthropometric, and demographic data were also collected using self-report methods by trained research staff, in collaboration with community project leaders. Participants presented to community centers during scheduled times in the afternoon, to complete data collection visits that took approximately 1.5 hours. Approval from the Institutional Review Board of the University of South Carolina was obtained, and informed consent procedures were completed prior to enrollment. Participants were compensated monetarily for their time.
Blood Pressure was measured three times with Dinamap equipment using standard procedures. During assessments participants were seated with legs uncrossed, and the appropriate cuff size was selected based on upper-arm diameter. The cuff was placed on the left arm and three readings were taken after a 5-minute resting period. The average of the second and third readings were used for analyses, with the first excluded as initial BP readings are typically elevated due to reactivity.(Pickering et al., 2005) The Multidimensional Scale of Perceived Social Support (MSPSS) assessed collective family, friend, and significant other supports through 7-point Likert responses to 12 items such as “There is a special person who is around when I am in need.” A response of 1 indicated the lowest level perceived social support, and a response of 7 indicated the highest. The MSPSS has strong internal consistency overall (α=0.88) and has been used in African-American samples (Zimet, Dahlem, Zimet, & Farley, 1988). Mean scores across the 12 items were calculated for each participant. Participants indicated the monetary range of their household’s total annual income on a 7-point ordinal scale of income ranges that spanned from $10,000 or less annually, to $80,000 or more annually. Using these 24-month data, two multiple regressions were tested to examine the direct and interacting relations among perceived social support and income on systolic and diastolic BP. Social support and income predictors were mean-centered, and the cross-product interaction term was calculated. Age, sex, body mass index (BMI), and community were included as control variables. The final model for systolic and diastolic BP was estimated as follows:
Results
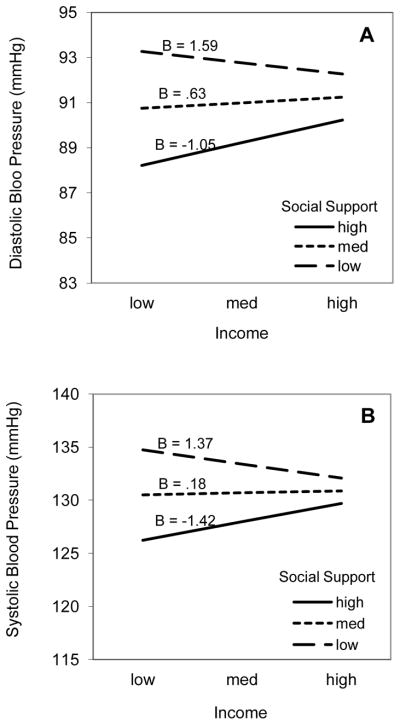
The sample (N = 204) had a mean age of 53.0 years (SD = 15.1) and was predominantly female (65%) and overweight or obese (MBMI = 33.5, SD = 14.7). Mean systolic and diastolic BP were 128.4 mmHg (SD = 20.9) and 77.3 mmHg (SD = 10.9), respectively. Mean perceived social support was 5.5 (SD = 1.0), indicating that on average the sample had relatively positive perceptions of support. Mean income was 2.8 (approximately $15,000; SD = 1.9. The model for diastolic BP was significant (p = .004, F = 3.29; Table 1) and overall accounted for 13% of the total variance in diastolic BP (r2 = .1344). Age and community control variables were associated with diastolic BP; community differences in diastolic BP were present at baseline (Wilson et al., 2010). Perceived social support demonstrated an inverse relation with diastolic BP (B = −1.76, p = .014), with lower support related to higher diastolic BP, and higher support related to lower diastolic BP. The interaction of social support with income was significant (B = .716, p = .046), with the pattern of effects indicating a relation whereby high social support buffered the impact of lowest-income status on diastolic BP (Figure 1a). High (6.5) and low (4.5) values of social support were determined by adding one standard deviation to the mean (M=5.5), which served as the median value. The overall model for systolic BP was not significant (p = .090, F = 1.80, r2=.060), however there was a trend for the association of social support with BP (B = −2.7, p = .060) and for an interaction (B = 1.47, p = .04), with the buffering association identical to that seen for diastolic BP (Figure 1b). Income was not directly related to BP in either model.
Table 1.
Regression of Diastolic BP on Control Variables, Social Support and Income
| Model | B | β | SE | t | p | LCL | UCL |
|---|---|---|---|---|---|---|---|
| Intercept, β 0 | 90.98 | - | 4.61 | 19.75 | .000 | 81.91 | 100.08 |
| Age, β1 | −.12 | −.16 | .05 | −2.37 | .019* | −.21 | −.02 |
| Sex, β2 | .61 | .027 | 1.58 | .39 | .385 | −2.51 | 3.73 |
| BMI, β3 | −.07 | −.10 | .05 | −1.44 | .151 | −.17 | .03 |
| Community, β4 | −2.84 | −.21 | .90 | −3.16 | .002* | −4.62 | −1.07 |
| Income, β5 | .24 | .04 | .40 | .61 | .542 | −.55 | 1.42 |
| SS, β6 | −1.76 | −.17 | .71 | −2.47 | .014* | −3.17 | −.35 |
| SS × Income, β7 | .72 | .14 | .36 | 2.01 | .046* | .012 | 1.42 |
p<.05
Note: BMI, body mass index; SS, social support. Data were collected in three communities in the southeastern U.S. in 2010.
Figure 1.
Buffering patterns of social support-by-income interaction predicting blood pressure. Highest, medium, and lowest values of both income and social support were determined by adding one standard deviation to the mean of each variable. Unstandardized betas are depicted for highest, medium, and lowest social support slopes across income levels. Data were collected in three communities in the southeastern U.S. in 2010.
Discussion
Results of this study provide preliminary support for the hypothesized stress-buffering pattern in a relatively large, cross-sectional sample of at-risk African-American adults. At the lowest levels of income, greater perceived social support was protective against the negative relation of income on diastolic BP. Specifically, there was a difference of about 2.6 mmHg across lower-income adults at one standard deviation below versus above the mean of social support. There were also direct effects of social support on diastolic BP, with a 1-point increase in support equating to about a 2 mmHg decrease in BP. Patterns seen for buffering and direct effects were consistent for trends on systolic blood pressure. The magnitudes of these buffering and direct effects are clinically meaningful, and are important from a public health standpoint, because epidemiologic data indicate that a 2 mmHg population-level decrease in diastolic BP may reduce the prevalence of HTN by 17%, and of stroke events by 15% (Cutler et al., 2008).
Previous research assessing social support buffering effects has produced mixed findings. Consistent with our findings, one study found that social supports buffered the negative effects of neighborhood disorder and poverty on self-rated health, only in individuals with the greatest exposures to stressors (Moskowitz, Vittinghoff, & Schmidt, 2013), and other studies with diverse samples have produced similar results (Gorman & Sivaganesan, 2007; Wight, Aneshensel, & LeBlanc, 2003). However, a number of studies have shown that the moderating role of social support for the relation of stress-related risk factors (e.g. low socioeconomic status, financial stress, worry) and mental or self-assessed health can vary as a function of age, sex, and race (Abolfathi Momtaz, Ibrahim, & Hamid, 2014; Bae, Hashimoto, Karlson, Liang, & Daltroy, 2001; Cadzow & Servoss, 2009; Krause, 2005). This study’s report of a social support-by-income buffering interaction that predicts a physical health outcome that is an indicator of persistent and pervasive cardiovascular health disparities is original and builds on these previous findings.
A strength of this study is that its hypotheses were tested in a sample of at-risk African-American adults that was relatively large and included a meaningful proportion of men; this population has traditionally been underserved and understudied (Davis et al., 2009). The study’s cross-sectional design is a limitation in that it does not allow for causal inferences that would be consistent with stress-buffering theory. Additionally, the use of data collected after the completion of the PATH environmental intervention is a limitation, however the analytical model did control for the community interventions.
This study contributes to a growing literature that demonstrates that social support likely has an important role to play in understanding and promoting health in disadvantaged communities. Enhancement of social support among at-risk, impoverished communities could have cardiovascular health benefits, and controlled trials are needed to test these opportunities.
Acknowledgments
This research was supported by the National Institute on Aging (F31AG039930 to SMC and DKW), the National Institute of Digestive and Kidney Diseases (R01DK067615 to DKW), the National Institute of Child Health and Human Development (R01HD072153 to DKW), and the National Institute of General Medical Sciences (T32GM081740).
Footnotes
The authors have no conflicts of interest to declare.
Compliance with Ethical Standards
The authors have no conflicts of interest to disclose. The research was conducted in accordance with ethical standards outlined by the University of South Carolina’s Institutional Review Board. All procedures performed with human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards, and informed consent procedures were completed prior to participation.
References
- Abolfathi Momtaz Y, Ibrahim R, Hamid TA. The impact of giving support to others on older adults’ perceived health status. Psychogeriatrics. 2014;14(1):31–37. doi: 10.1111/psyg.12036. [DOI] [PubMed] [Google Scholar]
- Adler NE, Ostrove JM. Socioeconomic status and health: what we know and what we don’t. Ann N Y Acad Sci. 1999;896:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- Anderson NB, Armstead CA. Toward understanding the association of socioeconomic status and health: a new challenge for the biopsychosocial approach. Psychosom Med. 1995;57(3):213–225. doi: 10.1097/00006842-199505000-00003. [DOI] [PubMed] [Google Scholar]
- Bae SC, Hashimoto H, Karlson EW, Liang MH, Daltroy LH. Variable effects of social support by race, economic status, and disease activity in systemic lupus erythematosus. J Rheumatol. 2001;28(6):1245–1251. [PubMed] [Google Scholar]
- Barth J, Schneider S, von Kanel R. Lack of social support in the etiology and the prognosis of coronary heart disease: a systematic review and meta-analysis. Psychosom Med. 2010;72(3):229–238. doi: 10.1097/PSY.0b013e3181d01611. [DOI] [PubMed] [Google Scholar]
- Cadzow RB, Servoss TJ. The association between perceived social support and health among patients at a free urban clinic. J Natl Med Assoc. 2009;101(3):243–250. doi: 10.1016/s0027-9684(15)30852-x. [DOI] [PubMed] [Google Scholar]
- Cohen S, Wills T. Stress, social support, and the buffering hypothesis. Psychological bulletin. 1985;98(2):310–357. [PubMed] [Google Scholar]
- Cutler J, Sorlie P, Wolz M, Thom T, Fields L, Roccella E. Trends in hypertension prevalence, awareness, treatment, and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension. 2008 doi: 10.1161/HYPERTENSIONAHA.108.113357. [DOI] [PubMed] [Google Scholar]
- Davis RM, Hitch AD, Nichols M, Rizvi A, Salaam M, Mayer-Davis EJ. A collaborative approach to the recruitment and retention of minority patients with diabetes in rural community health centers. Contemp Clin Trials. 2009;30(1):63–70. doi: 10.1016/j.cct.2008.09.007. S1551-7144(08)00120-1 [pii] [DOI] [PubMed] [Google Scholar]
- Gadegbeku C, Lea J, Jamerson K. Update on disparities in the pathophysiology and management of hypertension: focus on African Americans. The Medical clinics of North America. 2005;89(5) doi: 10.1016/j.mcna.2005.05.003. [DOI] [PubMed] [Google Scholar]
- Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Blaha MJ Stroke Statistics S. Heart disease and stroke statistics--2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–e292. doi: 10.1161/01.cir.0000441139.02102.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman BK, Sivaganesan A. The role of social support and integration for understanding socioeconomic disparities in self-rated health and hypertension. Soc Sci Med. 2007;65(5):958–975. doi: 10.1016/j.socscimed.2007.04.017. [DOI] [PubMed] [Google Scholar]
- Johnson KW, Anderson NB, Bastida E, Kramer BJ, Williams D, Wong M. Macrosocial and environmental influences on minority health. Health Psychol. 1995;14(7):601–612. doi: 10.1037//0278-6133.14.7.601. [DOI] [PubMed] [Google Scholar]
- Krause N. Exploring age differences in the stress-buffering function of social support. Psychol Aging. 2005;20(4):714–717. doi: 10.1037/0882-7974.20.4.714. [DOI] [PubMed] [Google Scholar]
- Matthews KA, Gallo LC. Psychological perspectives on pathways linking socioeconomic status and physical health. Annu Rev Psychol. 2011;62:501–530. doi: 10.1146/annurev.psych.031809.130711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moskowitz D, Vittinghoff E, Schmidt L. Reconsidering the effects of poverty and social support on health: a 5-year longitudinal test of the stress-buffering hypothesis. J Urban Health. 2013;90(1):175–184. doi: 10.1007/s11524-012-9757-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickering TG, Hall JE, Appel LJ, Falkner BE, Graves JW, Hill MN, Roccella EJ. Recommendations for blood pressure measurement in humans: an AHA scientific statement from the Council on High Blood Pressure Research Professional and Public Education Subcommittee. J Clin Hypertens (Greenwich) 2005;7(2):102–109. doi: 10.1111/j.1524-6175.2005.04377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wight RG, Aneshensel CS, LeBlanc AJ. Stress buffering effects of family support in AIDS caregiving. AIDS Care. 2003;15(5):595–613. doi: 10.1080/09540120310001595096. [DOI] [PubMed] [Google Scholar]
- Wilson DK, Trumpeter NN, St George SM, Coulon SM, Griffin S, Lee Van Horn M, Gadson B. An overview of the “Positive Action for Today’s Health” (PATH) trial for increasing walking in low income, ethnic minority communities. Contemp Clin Trials. 2010;31(6):624–633. doi: 10.1016/j.cct.2010.08.009. S1551-7144(10)00155-2 [pii] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Van Horn ML, Siceloff ER, Alia KA, St George SM, Lawman HG, Gadson B. The Results of the “Positive Action for Today’s Health” (PATH) Trial for Increasing Walking and Physical Activity in Underserved African-American Communities. Annals of Behavioral Medicine. 2015;49(3):398–410. doi: 10.1007/s12160-014-9664-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimet G, Dahlem N, Zimet S, Farley G. The multidimensional scale of perceived social support. Journal of Personality Assessment. 1988;52(1):30–41. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]