Abstract
Objective:
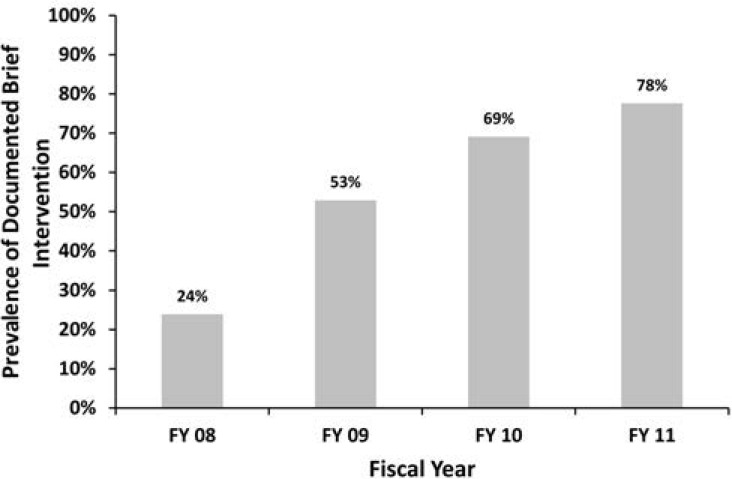
Brief alcohol interventions are recommended for primary care patients who screen positive for alcohol misuse, but implementation is challenging. The U.S. Veterans Health Administration (Veterans Affairs [VA]) implemented brief interventions for patients with alcohol misuse in 2008, and rates of brief interventions documented in the electronic medical record increased from 24% to 78% (2008–2011). This study examined whether an independent measure of brief interventions—patient-reported alcohol-related advice—also increased among VA outpatients who screened positive for alcohol misuse on a mailed survey.
Method:
This retrospective cross-sectional study included VA outpatient respondents to the VA’s Survey of Healthcare Experiences of Patients (SHEP; 2007–2011) who reported past-year alcohol use and answered a question about alcohol-related advice. Alcohol-related advice was defined as a report of past-year advice from a VA clinician to abstain from or reduce drinking. The adjusted prevalence of alcohol-related advice among patients who screened positive for alcohol misuse (SHEP AUDIT-C ≥ 5) was estimated for each year.
Results:
Among patients with alcohol misuse (n = 61,843), the adjusted prevalence of alcohol-related advice increased from 40.4% (95% CI [39.3%, 41.5%]) in 2007 to 55.5% (95% CI [53.3%, 57.8%]) in 2011. Rates of alcohol-related advice increased significantly each year except the last.
Conclusions:
The VA’s efforts to implement brief interventions were associated with increased patient-reported alcohol-related advice over time, with a majority of patients with alcohol misuse reporting its receipt. Other systems considering similar approaches to implementation may benefit from collecting patient-reported measures of brief interventions for an additional perspective on implementation.
Alcohol misuse includes a spectrum ranging from drinking above recommended limits to meeting diagnostic criteria for alcohol use disorders (Jonas et al., 2012) and is a leading preventable cause of morbidity and mortality (Mokdad et al., 2004; Murray et al., 2013; Rehm et al., 2010). Approximately 20% of adult primary care patients drink alcohol at unhealthy levels (Saitz, 2005; Vinson et al., 2010). Based on the effectiveness of brief interventions for reducing drinking in patients with alcohol misuse (Jonas et al., 2012; Kaner et al., 2007), routine screening and brief intervention are widely recommended for primary care patients (Moyer, 2013; National Health Service, 2010). Although the content of brief interventions varies across studies, effective interventions typically include personalized feedback linking drinking to health and advice to drink below recommended limits or abstain from drinking (Jonas et al., 2012; Whitlock et al., 2004). The length of brief interventions can be as short as 5 minutes, but implementation of brief interventions in real-world clinical settings has proven challenging (Nilsen, 2010; Williams et al., 2011).
The U.S. Veterans Health Administration (Veterans Affairs [VA]) implemented brief interventions using national quality improvement strategies, beginning with implementation of outpatient alcohol screening in 2004 (Bradley et al., 2006). An early evaluation showed that alcohol screening alone did not increase rates of brief interventions (Bradley et al., 2006, 2007b), so a performance measure for brief interventions linked to financial incentives for health system leaders was implemented in 2008. The performance measure required clinicians to document two core elements of brief interventions for patients who screen positive for alcohol misuse: advice to drink below recommended limits and feedback linking drinking to health (Lapham et al., 2012; Whitlock et al., 2004). In addition, a brief intervention clinical reminder in the electronic medical record (EMR) was disseminated nationwide that clinicians could use to easily document the required elements of brief interventions. In general, nonphysician clinic triage staff screened outpatients with an alcoholscreening clinical-reminder prompt, and a different VA provider, usually the primary care provider, was prompted to offer brief interventions for patients who screened positive for alcohol misuse. Each VA facility was free to implement brief interventions as they chose and, although core components of the performance measure were required at all sites, electronic clinical reminders could be modified locally. Clinician training for conducting brief interventions was largely left to individual clinics (Williams et al., 2016).
Following these efforts, rates of provider-documented brief interventions that met performance measure requirements increased markedly over the first 4 years of implementation beginning in fiscal year (FY) 2008 (October 1, 2007) (Lapham et al., 2012). Figure 1 shows average monthly national rates of brief interventions for each fiscal year based on performance reporting in the VA of EMR documentation among eligible patients who screened positive (Bradley et al., 2011). Rates of brief interventions among VA patients who screened positive for alcohol misuse far exceed those typically seen elsewhere; more than 70% of VA patients who screened positive had documented brief interventions in FY 2011. Only one other study reported similarly high rates of 73% (Babor et al., 2005). Moreover, many prior studies reported much lower rates, as low as 3% (Williams et al., 2011). However, financial incentives and the ease of documentation in the EMR may have only encouraged VA providers to document counseling that was already occurring or was so brief that patients may not have recalled alcohol-related advice (Coleman, 2010; Flocke & Stange, 2004).
Figure 1.
Veterans Affairs (VA) national performance measure for brief intervention (BI), proportion of patients with documentation of brief interventions among screen positive patients (AUDIT-C ≥ 5). Fiscal year rates of BI are based on the average monthly rates available from the VA’s National Performance Measure Reporting System. AUDIT-C = Alcohol Use Disorders Identification Test–Consumption; FY = fiscal year.
Although a positive trend in the VA’s provider-documented brief interventions is encouraging, a similar positive trend in an independent patient-report measure over the same period could provide further evidence that an increasing proportion of VA patients were in fact being offered brief interventions. Patient reporting of preventive services is not a gold standard and has known limitations, including the potential for patients to forget receiving counseling and not report it when surveyed (Flocke & Stange, 2004). However, patient reporting is often used to assess receipt of preventive counseling, such as for smoking-cessation counseling (Agency for Healthcare Research and Quality, 2008). Therefore, patient reporting of brief interventions could be useful to corroborate increases in documented brief interventions because it is independent of provider documentation. Therefore, the purpose of this study was to determine whether the prevalence of patient-reported alcohol-related advice increased among VA outpatients who screened positive for alcohol misuse on a mailed survey over a period when provider-documented brief interventions were increasing.
Method
Study setting and population
This retrospective cross-sectional study included VA outpatient respondents to the mailed Survey of Healthcare Experiences of Patients (SHEP), which is administered by the VA Office of Analytics and Business Intelligence. Respondents are asked about their most recent outpatient visit, as well as about smoking, health status, and alcohol use. SHEP respondents were included in the present study if they had an outpatient visit that occurred during the year before the VA’s brief intervention implementation efforts (FY 2007; October 1, 2006–September 30, 2007) or the subsequent 4 fiscal years (through FY 2011; October 1, 2010–September 30, 2011), reported past-year alcohol use, and responded to a survey item that asked drinkers about receipt of alcohol-related advice from a VA clinician. Although SHEP respondents could have been mailed a survey more than once during the study period, only their first completed survey was used. The VA Puget Sound Health Care System Institutional Review Board reviewed and approved this study and granted waivers of informed consent and Health Insurance Portability and Accountability Act (HIPAA) authorization.
The sampling strategy for the SHEP survey was modified over the years of this study. Before FY 2010, patients were randomly selected from VA medical facilities with equal representation of new primary care patients, established primary care patients, and established specialty care patients (Wright et al., 2006). However, beginning in FY 2010, patients were selected from each VA medical facility by simple random sampling. The alcohol-related questions used in this study were included on all SHEP surveys before FY 2009, and thereafter they were included only on a “long” form of the survey sent to 10% of surveyed patients. National response rates for the overall SHEP survey during the study period were 54% across all years (55% FY 2007, 54% FY 2008, 55% FY 2009, 53% FY 2010, and 51% FY 2011), with lower response rates among younger and female patients (VHA Office of Analytics and Business Intelligence, 2011).
Measures
Alcohol use and misuse.
The Alcohol Use Disorders Identification Test–Consumption (AUDIT-C) screening questionnaire included on the SHEP survey was used to identify past-year drinking and alcohol misuse. The three-item AUDIT-C (0–12 total points) is validated to detect alcohol misuse (Bradley et al., 2003, 2007a; Bush et al., 1998). A score of 0 points indicates no past-year alcohol use, and the severity of alcohol misuse increases as AUDIT-C scores increase (Bradley et al., 2004; Rubinsky et al., 2010). AUDIT-C scores ≥4 points for men and ≥3 points for women are the gender-specific thresholds for identifying alcohol misuse based on VA validation studies (Bradley et al., 2003; Bush et al., 1998). However, as above, the VA assesses brief interventions performance among patients who screen positive at AUDIT-C scores ≥5 points for both men and women (e.g., moderate to severe alcohol misuse) to reduce the burden of false positives on healthcare providers (Lapham et al., 2012). Therefore, this higher threshold was used to define the subsample of patients included in primary analyses of patient-reported alcohol-related advice to allow for comparison of our findings with previous studies of the VA's brief intervention performance measure that assess EMR documentation of brief interventions (Lapham et al., 2012).
Patient-reported alcohol-related advice.
The main outcome measure—patient-reported alcohol-related advice—was based on a “yes” response to the following SHEP survey question, which was asked of all patients who reported past-year drinking: “In the past 12 months, has a VA doctor or other VA health care provider advised you about your drinking (to drink less or not to drink alcohol)?”
Time periods.
To assess differences in patient-reported alcohol-related advice over time, a categorical variable was constructed to indicate the fiscal year of the patient’s outpatient visit that led to the mailing of the SHEP survey (FY 2007–FY 2011). FY 2007 represents a baseline period before introduction of the VA’s national performance measure and clinical reminder prompting EMR documentation of brief interventions.
Covariates.
Patient characteristics available on SHEP surveys were included as covariates to adjust for characteristics known to be associated with receipt of alcohol-related advice (Arndt et al., 2002; Burman et al., 2004; Dobscha et al., 2009; Kaner et al., 2001), including age (<50, 50–59, 60–69, ≥70 years), gender, race (White non-Hispanic, Black non-Hispanic, Hispanic, and other), education (high school or less, some college, completed college or more), and smoking status. A missing category was created for covariates (race, education, and smoking) without complete data (missing <3%).
Statistical analyses
Descriptive statistics were used to characterize the study sample of patients reporting past-year drinking (AUDIT-C > 0). Primary analyses were conducted in the subsample of patients with AUDIT-C scores ≥5 points on SHEP. A logistic regression model was used to evaluate the association between patient-reported alcohol-related advice and time periods, with fiscal years modeled as categorical dummy variables. All analyses used robust error variance and were clustered on VA medical facility (n = 130) to account for potential correlation of outcomes. Results are presented as the average adjusted probability of patient-reported alcohol-related advice among patients who screened positive for moderate to severe alcohol misuse (AUDIT-C ≥ 5) for each of 5 fiscal years, which was estimated using the method of recycled predictions that held all covariates constant and allowed fiscal year to vary (Kleinman & Norton, 2009). The differences in the adjusted probability of advice were also estimated for adjacent fiscal years, as well as for the first year (FY 2007) and last year (FY 2011) of the study period. Post-estimation Wald tests evaluated differences between the adjusted probabilities of patient-reported advice across adjacent fiscal years, and a linear contrast tested for an overall linear trend across all fiscal years.
Secondary analyses were conducted to determine whether an increasing trend in patient-reported alcohol-related advice was present among all past-year drinkers. It was hypothesized that evidence of a greater increase in patient-reported advice among those who screened positive at the threshold for which brief interventions was incentivized (AUDIT-C ≥5) would provide stronger support that differences in trend could be attributable to the VA’s implementation efforts specifically targeting such patients. Moreover, it was also expected that trends could vary depending on whether SHEP respondents screened positive at lower thresholds or screened negative. Therefore, past-year drinkers were assigned to one of three groups based on SHEP responses: negative screens for alcohol misuse (AUDIT-C scores 1–2 for women, 1–3 for men), positive screens for mild alcohol misuse (AUDIT-C scores 3–4 for women, 4 for men), and positive screens for moderate to severe alcohol misuse (AUDIT-C ≥ 5). Primary analyses were repeated in this larger sample, and an AUDIT-C Group × Time interaction was added to the logistic regression model. A post-estimation Wald test was used to evaluate whether there were differences in trends across groups. All analyses were conducted using Stata MP Parallel Edition, software Version 12.0 (StataCorp LP, College Station, TX).
Results
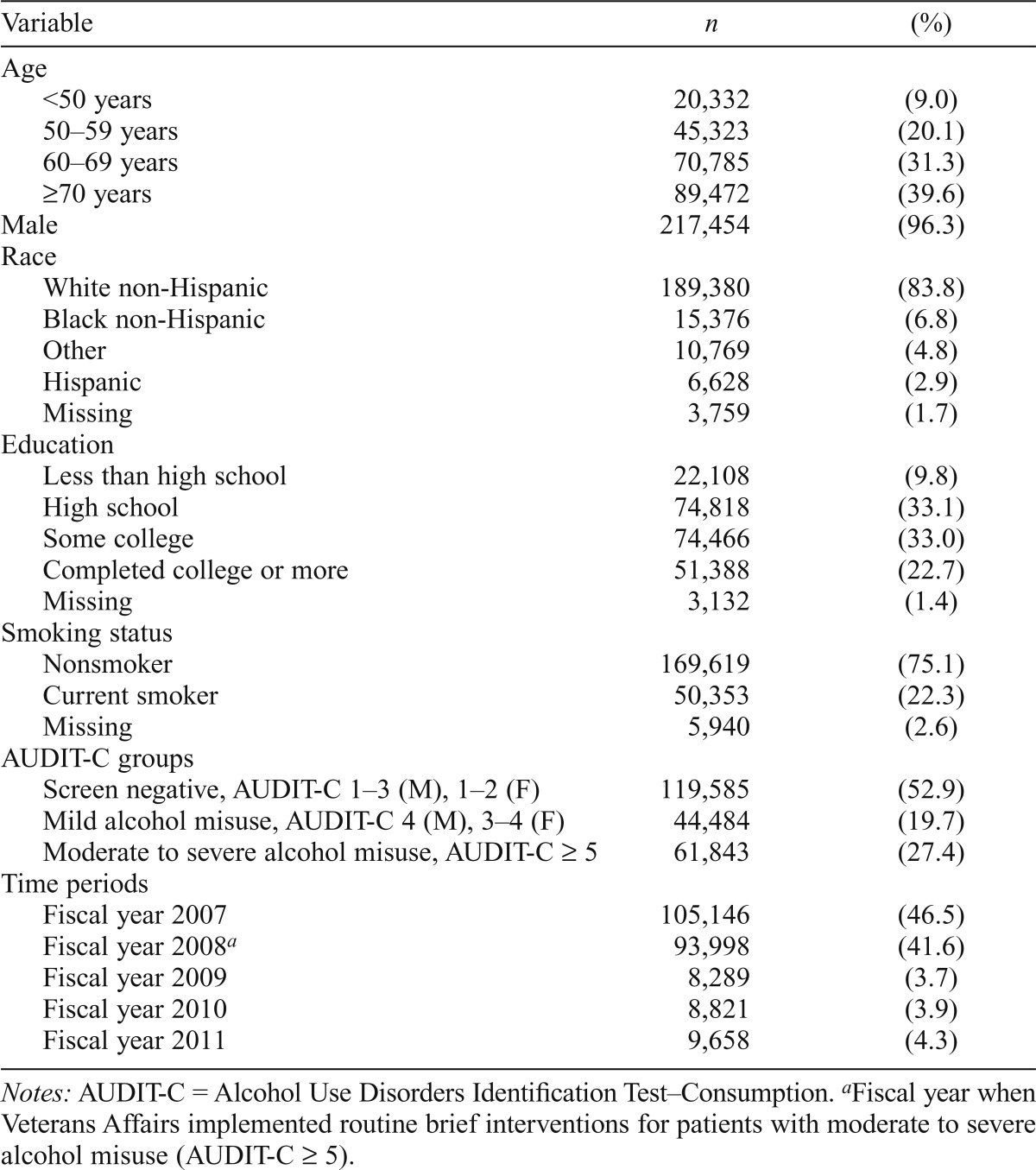
A total of 225,912 SHEP respondents reported past-year drinking and completed the alcohol-related advice question. Among past-year drinkers, 52.9% screened negative for alcohol misuse, 19.7% screened positive for mild alcohol misuse, and 27.4% screened positive for moderate to severe alcohol misuse on the survey (Table 1). Among patients who screened positive for moderate to severe alcohol misuse (AUDIT-C ≥ 5), 98.4% completed the alcohol-related advice question. Nonresponse to the alcohol-related advice question in this sample varied by fiscal year (0.7%–5.6%, p < .001), with the largest proportion of nonresponse occurring in FY 2009. Nonresponse was associated with respondent age (2.2% for age >70 years vs. 1.0% for age <50 years, p < .001) and AUDIT-C score (1.9% for AUDIT-C scores 8–12 vs. 1.5% for scores 5–7, p < .001). Overall, SHEP respondents reporting past-year drinking were predominantly male, older (age ≥ 60 years), White non-Hispanic, nonsmokers, and had not completed college (Table 1).
Table 1.
Characteristics of survey respondents who reported past-year alcohol use (n = 225,912)
| Variable | n | (%) |
| Age | ||
| <50 years | 20,332 | (9.0) |
| 50–59 years | 45,323 | (20.1) |
| 60–69 years | 70,785 | (31.3) |
| ≥70 years | 89,472 | (39.6) |
| Male | 217,454 | (96.3) |
| Race | ||
| White non-Hispanic | 189,380 | (83.8) |
| Black non-Hispanic | 15,376 | (6.8) |
| Other | 10,769 | (4.8) |
| Hispanic | 6,628 | (2.9) |
| Missing | 3,759 | (1.7) |
| Education | ||
| Less than high school | 22,108 | (9.8) |
| High school | 74,818 | (33.1) |
| Some college | 74,466 | (33.0) |
| Completed college or more | 51,388 | (22.7) |
| Missing | 3,132 | (1.4) |
| Smoking status | ||
| Nonsmoker | 169,619 | (75.1) |
| Current smoker | 50,353 | (22.3) |
| Missing | 5,940 | (2.6) |
| AUDIT-C groups | ||
| Screen negative, AUDIT-C 1–3 (M), 1–2 (F) | 119,585 | (52.9) |
| Mild alcohol misuse, AUDIT-C 4 (M), 3–4 (F) | 44,484 | (19.7) |
| Moderate to severe alcohol misuse, AUDIT-C ≥ 5 | 61,843 | (27.4) |
| Time periods | ||
| Fiscal year 2007 | 105,146 | (46.5) |
| Fiscal year 2008a | 93,998 | (41.6) |
| Fiscal year 2009 | 8,289 | (3.7) |
| Fiscal year 2010 | 8,821 | (3.9) |
| Fiscal year 2011 | 9,658 | (4.3) |
Notes: AUDIT-C = Alcohol Use Disorders Identification Test–Consumption.
Fiscal year when Veterans Affairs implemented routine brief interventions for patients with moderate to severe alcohol misuse (AUDIT-C ≥ 5).
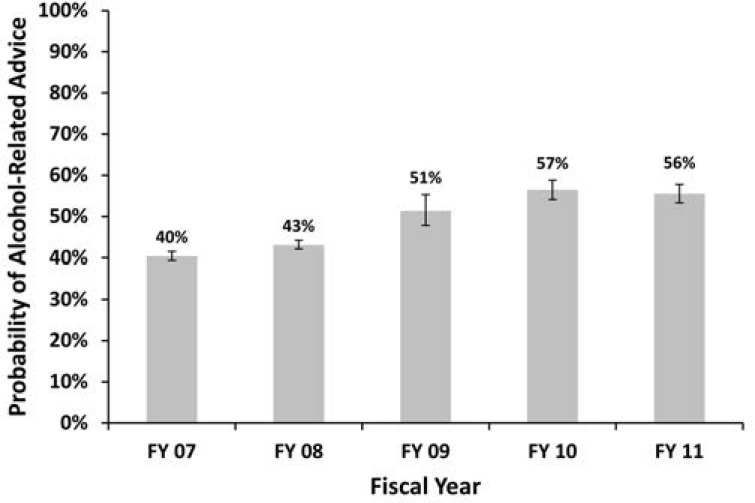
Among respondents who screened positive for moderate to severe alcohol misuse (n = 61,843), the unadjusted prevalence of patient-reported advice ranged from 40.2% in the baseline year to 56.9% in the final fiscal year. After we adjusted for covariates, the average adjusted probability of patient-reported alcohol-related advice increased from 40.4% (95% CI [39.3%, 41.5%]) in the baseline year to 55.5% (95% CI [53.3%, 57.8%]) in the final fiscal year (Figure 2) (test for trend p < .001). Significant differences in the adjusted probability were observed between each adjacent fiscal year (p values all < .05) except between the last two fiscal years (2010–2011). The greatest difference occurred in the period immediately following the VA’s implementation efforts (FY 2009), where the average adjusted probability of patient-reported alcohol-related advice increased by 8.2% (95% CI [6.1%, 10.3%]).
Figure 2.
Adjusted probability of patient-reported alcohol-related advice, among screen positive patients (AUDIT-C≥5). Adjusted for age, gender, race/ethnicity, education, and smoking status. AUDIT-C = Alcohol Use Disorders Identification Test–Consumption; FY = fiscal year.
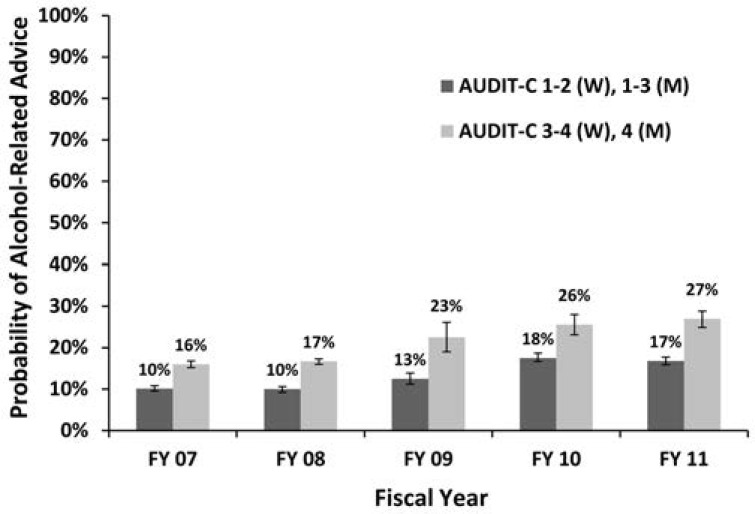
In secondary analyses among all patients reporting past-year drinking (n = 225,912), there was a significant AUDIT-C Group × Time interaction (p = .003). At the baseline year, the unadjusted probabilities of patient-reported alcohol-related advice among those who screened negative or had positive screens for mild alcohol misuse were 9.6% and 13.6%, respectively. After adjustment for covariates, the baseline prevalence of alcohol-related advice was 10.1% (95% CI [9.7%, 10.7%]) and 16.0% (95% CI [15.2%, 16.8%]) (Figure 3). The adjusted differences in the probability of patient-reported alcohol-related advice from FY 2007 to FY 2011 in the three AUDIT-C groups were the following: 6.8% (95% CI [5.9%, 7.8%]) increase for those with negative AUDIT-C screens, 10.6% (95% CI [8.7%, 12.6%]) increase for those who screened positive for mild alcohol misuse, and 14.5% (95% CI [12.2%, 16.8%]) increase for those who screened positive for moderate to severe alcohol misuse. For patients who screened positive for moderate to severe alcohol misuse, the adjusted difference in patient-reported alcohol-related advice was significantly greater than that of patients who screened positive for mild alcohol misuse (p = .005) and who screened negative (p < .001).
Figure 3.
Adjusted probability of patient-reported alcohol-related advice, among screen negative and patients with mild alcohol misuse. Adjusted for age, gender, race/ethnicity, education, and smoking status. Screen negative = AUDIT-C scores 1–2 points for women (W) or 1–3 points for men (M); mild alcohol misuse = AUDIT-C scores 3–4 points for women (W) or 4 points for men (M). AUDIT-C = Alcohol Use Disorders Identification Test–Consumption; FY = fiscal year.
Discussion
This study suggests that the VA's nationwide effort to implement population-based brief interventions for patients with moderate to severe alcohol misuse was associated with an increase in rates over time of patient-reported alcohol-related advice—a key component of evidence-based brief interventions (Bertholet et al., 2014; Kaner et al., 2007; Whitlock et al., 2004). From the year before the VA’s implementation of brief interventions (FY 2007) to the third year after implementation (FY 2010), report of alcohol-related advice among patients who screened positive for alcohol misuse increased from 40.4% to 56.7% and remained stable at 55.5% in FY 2011. The adjusted difference in rates of patient-reported alcohol-related advice was greater for patients with positive screens for moderate to severe alcohol misuse (AUDIT-C scores 5–12) who were targeted by the VA’s performance measure for brief interventions compared with those with lower AUDIT-C scores who were not expected to be offered brief interventions (Bradley et al., 2007b). These findings further suggest that the observed increases in rates of patient-reported alcohol-related advice may be related to the VA’s efforts to implement brief interventions.
The VA’s national efforts to implement brief interventions using clinical reminders and a performance measure were broad, system-level changes that incentivized brief intervention delivery and achieved high rates of documented brief interventions (Lapham et al., 2012). Rates of documented brief interventions were similar to those seen in a multisite, quasi-experimental research study (73%) (Babor et al., 2005) but were in a real-world clinical setting and sustained over several years. System-level implementation strategies—such as the use of electronic reminders in an EMR, feedback on performance, and financial incentives—have been used in other settings to increase delivery and clinician documentation of brief interventions in medical records (Hamilton et al., 2014; Ornstein et al., 2013; Rose et al., 2008). Such strategies are increasingly important for improving the quality of care and are central to the practice of medicine, but their effectiveness is under-studied. Although some qualitative evidence from a single VA region suggests that the VA’s system-level approaches to brief intervention implementation may have contributed to a culture of checking boxes (Williams et al., 2016), the results of the present national study suggest some positive changes in patient-reported receipt of recommended alcohol-related advice.
The rates of patient-reported alcohol-related advice in this study far exceed rates seen among general U.S. population samples, which have changed little over time. Among population-based samples of U.S. adults, only 23% of adults who reported a past-year clinic visit and heavy episodic drinking in 1997 said that a clinician had discussed alcohol with them (Denny et al., 2003), and this rate was also low in 2011, with 25% of past-year heavy episodic drinkers reporting alcohol-related discussions with a clinician (McKnight-Eily et al., 2014). The relatively high rates of patient-reported advice observed in this VA study may not be attributable to the VA's national brief interventions implementation alone, as other efforts to encourage VA clinicians to address alcohol misuse occurred over this period. For example, the Behavioral Health Lab (BHL) was developed at the Philadelphia VA Medical Center in 2003 to provide integrated mental health follow-up, which often includes brief interventions, for patients who initially screened positive for alcohol misuse, depression, or posttraumatic stress disorder during an outpatient visit (Oslin et al., 2006). The BHL was disseminated nationally in 2007 as one of three options for integrating mental health care into primary care (Hedrick et al., 2003; Pomerantz et al., 2014). The BHL was used in 20% of VA facilities in 2010 (Tew et al., 2010), although patients with alcohol misuse were less likely to be referred to BHL than those with other mental health conditions (Maust et al., 2011). Therefore, it is possible that surveyed outpatients were not reporting specifically on the alcohol-related advice that they received during outpatient visits, but rather on alcohol-related discussions more generally, including mental health follow-up that addressed alcohol.
However, the increase in patient-reported advice appeared to plateau between FY 2010 and FY 2011, and 44% of patients who screened positive on surveys did not report receiving advice from providers in 2011 (Figure 2). There were marked increases in the rates of clinician-documented brief interventions from FY 2008 to FY 2011—a 54% absolute increase (from 24% to 78%) (Figure 1). Yet, patient-reported alcohol-related advice among patients who screened positive for alcohol misuse increased by only 13% over this same period. However, these measures of brief interventions were obtained in different patient samples, and patients who respond to SHEP are known to be older than nonresponders, but older patients are less likely to be counseled about their drinking (Burman et al., 2004). Thus, the lower rates of patient-reported advice than clinician-documented brief interventions could be attributable to differences between patient samples.
The plateau in patient-reported rates of alcohol-related advice observed in this study could also reflect the fact that VA providers may not have been prompted to provide brief interventions for many patients in our sample as a result of patients under-reporting alcohol use or low-quality alcohol screening in the clinical setting. Previous research has identified low sensitivity of clinical screening for identifying alcohol misuse in the VA compared with AUDIT-Cs on SHEP surveys (Bradley et al., 2011a), and local qualitative research suggests that this may occur because of nonstandardized verbal administration of alcohol screening by triage staff (Williams et al., 2015). Therefore, it could be that many of the patients in our study sample who screened positive on SHEP did not screen positive during a past-year VA outpatient visit and that their VA provider was not prompted to offer brief interventions. Under-identification of patients with alcohol misuse who would screen positive on a confidential mailed survey could produce a ceiling effect in rates of patient-reported advice. For example, patient-reported alcohol-related advice can only increase up to the proportion of patients identified as eligible for brief interventions during outpatient screening. To see additional increases in patient-reported brief interventions, efforts may be needed to improve clinical identification of patients with alcohol misuse, such as through alcohol screening using paper surveys, computer tablets, kiosks, or other approaches that standardize patient reporting.
This study has several limitations. First, our outcome measured patient reporting of alcohol-related advice and not what actually occurred during the clinical visit. Patients may forget receipt of advice or may not wish to report receiving such advice because of social desirability and alcohol-related stigma. The study outcome measure may not adequately capture alcohol-related discussions with clinicians, and some patients may have interpreted alcohol screening as brief interventions. However, the proportion of patients with moderate to severe misuse who reported alcohol-related advice did not increase in the first 4 years of screening alone, before brief interventions were implemented. In 2004, when screening was introduced, the rate was 40%—the same as that in 2007 (Bradley et al., 2007b). This suggests that increases in patient-reported alcohol-related advice may be attributable to brief interventions implementation rather than screening itself. Second, advice is only one of the two components of evidence-based brief interventions incentivized by the VA’s performance measure (Kaner et al., 2007; Whitlock et al., 2004). However, we would not expect different trends between this component and health-related feedback, given that both were required to satisfy the VA’s performance measure (Lapham et al., 2012). Third, patients who are satisfied with their providers may overreport receipt of advice if they think providers should have offered preventive alcohol advice (a “halo effect” in satisfied patients). Fourth, the period for the study outcome was categorized based on the fiscal year in which the outpatient visit occurred that triggered the SHEP survey mailing, creating a potential lag in past-year patient-reported alcohol-related advice if patients were reporting on receipt of advice at a visit before their most recent outpatient visit. However, we do not expect that this affected overall changes over time in patient-reported alcohol-related advice. Fifth, there were associations between nonresponse on the alcohol-related advice question and some patient characteristics, but we do not expect that item-level nonresponse would greatly bias changes over time in patient-reported alcohol-related advice. Although there was greater nonresponse in FY 2009 (5%) compared with other years (1%–2%), even if all nonresponders had reported not receiving advice this could not completely negate the 9% increase in patient-reported advice that we observed from 2008 to 2009. Sixth, because this study did not have a control group, it is possible that the changes over time in patient-reported advice across the VA are reflective of secular trends in alcohol-related discussions over time and not the brief intervention implementation efforts. However, given the challenge of implementing brief interventions in a sustainable way in real-world settings, and the lack of increased patient-reported brief interventions from 2004 to 2007, we believe it is unlikely that observed changes represent a historic trend.
Despite some of the limitations of our study’s outcome measure, patient-reported measures of alcohol-related advice are commonly used to assess the delivery of brief interventions following implementation efforts (Aalto et al., 2003; Babor et al., 2005; Chossis et al., 2007; Nilsen et al., 2011), and similar patient-reported measures of smoking-cessation advice are widely used to evaluate performance on preventive counseling (Agency for Healthcare Research and Quality, 2008; Boyle et al., 2011; Szatkowski et al., 2011). Moreover, a patient-reported measure clearly adds value to the assessment of the VA’s brief interventions implementation: the plateau in patient-reported advice observed in the final periods of this study would have been missed if brief interventions performance was based on clinical documentation alone. Thus, health systems choosing similar system-level approaches to brief interventions implementation may also benefit from collecting information on brief interventions delivery from the patient perspective (Bradley et al., 2011b).
Conclusions
Findings from this study have important implications for implementing widely recommended preventive brief interventions into routine care (Jonas et al., 2012; Moyer, 2013; National Health Service, 2010). First, a program of performance measurement and incentives, in conjunction with EMR clinical reminders, was associated with significant increases in patient reporting of brief alcohol-related advice, from 40.4% to 55.5% overall. However, rates of patient-reported alcohol-related advice largely plateaued, with more than 40% of patients with alcohol misuse not reporting receipt of alcohol-related advice from a VA provider. These findings suggest a need for further quality improvement efforts. Moreover, it highlights the value of patient reports on surveys for identifying deficits in alcohol-related care that may be obscured by performance measures that rely on chart documentation alone, especially if patients with alcohol misuse are under-identified.
Footnotes
This study was supported by the Veteran’s Affairs (VA) Substance Use Disorders Quality Enhancement Research Initiative (SUD QUERI). Dr. Chavez was supported by a National Institutes of Health Agency for Healthcare Research and Quality (AHRQ) Dissertation Grant (NIH 1R36HS022800-01). Dr. Williams is supported by a Career Development Award from VA Health Services Research & Development (CDA 12-276). Dr. Bradley’s support for this project was from Group Health Research Institute and the VA’s Seattle Center of Excellence for Substance Abuse Teaching and Education. Views expressed in this article are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs, the University of Washington, or Group Health Research Institute. Laura J. Chavez, Emily C. Williams, Gwen T. Lapham, Anna D. Rubinsky, Daniel R. Kivlahan, and Katharine A. Bradley do not have any conflicts of interest to disclose.
References
- Aalto M., Pekuri P., Seppä K. Primary health care professionals’ activity in intervening in patients’ alcohol drinking during a 3-year brief intervention implementation project. Drug and Alcohol Dependence. 2003;69:9–14. doi: 10.1016/s0376-8716(02)00228-4. doi:10.1016/S0376-8716(02)00228-4. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality. 2008 doi: 10.1080/15360280802537332. CAHPS Health Plan Survey 4.0 Version: Adult Commercial Questionnaire. Retrieved from https://cahps.ahrq.gov/surveys-guidance/survey4.0-docs/1151a_en-gadultcom_40.pdf. [DOI] [PubMed]
- Arndt S., Schultz S. K., Turvey C., Petersen A. Screening for alcoholism in the primary care setting: Are we talking to the right people? Journal of Family Practice. 2002;51:41–46. [PubMed] [Google Scholar]
- Babor T. E., Higgins-Biddle J., Dauser D., Higgins P., Burleson J. A. Alcohol screening and brief intervention in primary care settings: Implementation models and predictors. Journal of Studies on Alcohol. 2005;66:361–368. doi: 10.15288/jsa.2005.66.361. doi:10.15288/jsa.2005.66.361. [DOI] [PubMed] [Google Scholar]
- Bertholet N., Palfai T., Gaume J., Daeppen J. B., Saitz R. Do brief alcohol motivational interventions work like we think they do? Alcoholism: Clinical and Experimental Research. 2014;38:853–859. doi: 10.1111/acer.12274. doi:10.1111/acer.12274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle R., Solberg L., Fiore M. Use of electronic health records to support smoking cessation. 2011 doi: 10.1002/14651858.CD008743.pub2. Cochrane Database of Systematic Reviews, Issue 12, Article No. CD008743. doi:10.1002/14651858.CD008743.pub2. [DOI] [PubMed] [Google Scholar]
- Bradley K. A., Bush K. R., Epler A. J., Dobie D. J., Davis T. M., Sporleder J. L., Kivlahan D. R. Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): Validation in a female Veterans Affairs patient population. Archives of Internal Medicine. 2003;163:821–829. doi: 10.1001/archinte.163.7.821. doi:10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- Bradley K. A., Kivlahan D. R., Zhou X.-H., Sporleder J. L., Epler A. J., McCormick K. A., Fihn S. D. Using alcohol screening results and treatment history to assess the severity of at-risk drinking in Veterans Affairs primary care patients. Alcoholism: Clinical and Experimental Research. 2004;28:448–455. doi: 10.1097/01.alc.0000117836.38108.38. doi:10.1097/01.ALC.0000117836.38108.38. [DOI] [PubMed] [Google Scholar]
- Bradley K. A., DeBenedetti A. F., Volk R. J., Williams E. C., Frank D., Kivlahan D. R. AUDIT-C as a brief screen for alcohol misuse in primary care. Alcoholism: Clinical and Experimental Research. 2007a;31:1208–1217. doi: 10.1111/j.1530-0277.2007.00403.x. doi:10.1111/j.1530-0277.2007.00403.x. [DOI] [PubMed] [Google Scholar]
- Bradley K. A., Johnson M. L., Williams E. C. Commentary on Nilsen et al. (2011): The importance of asking patients-the potential value of patient report of brief interventions. Addiction. 2011a;106:1757–1759. doi: 10.1111/j.1360-0443.2011.03587.x. doi:10.1111/j.1360-0443.2011.03587.x. [DOI] [PubMed] [Google Scholar]
- Bradley K. A., Lapham G. T., Hawkins E. J., Achtmeyer C. E., Williams E. C., Thomas R. M., Kivlahan D. R. Quality concerns with routine alcohol screening in VA clinical settings. Journal of General Internal Medicine. 2011b;26:299–306. doi: 10.1007/s11606-010-1509-4. doi:10.1007/s11606-010-1509-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bradley K. A., Williams E. C., Achtmeyer C. E., Hawkins E. J., Harris A. H. S., Frey M. S., Kivlahan D. R. Measuring performance of brief alcohol counseling in medical settings: A review of the options and lessons from the Veterans Affairs (VA) health care system. Substance Abuse. 2007b;28:133–149. doi: 10.1300/J465v28n04_05. doi:10.1300/J465v28n04_05. [DOI] [PubMed] [Google Scholar]
- Bradley K. A., Williams E. C., Achtmeyer C. E., Volpp B., Collins B. J., Kivlahan D. R. Implementation of evidence-based alcohol screening in the Veterans Health Administration. American Journal of Managed Care. 2006;12:597–606. Retrieved from http://www.ajmc.com/journals/issue/2006/2006-10-vol12-n10/oct06-2375p597-606. [PubMed] [Google Scholar]
- Burman M. L., Kivlahan D., Buchbinder M., Broglio K., Zhou X. H., Merrill J. O., Bradley K. A. the Ambulatory Care Quality Improvement Project Investigators. Alcohol-related advice for Veterans Affairs primary care patients: Who gets it? Who gives it? Journal of Studies on Alcohol. 2004;65:621–630. doi: 10.15288/jsa.2004.65.621. doi:10.15288/jsa.2004.65.621. [DOI] [PubMed] [Google Scholar]
- Bush K., Kivlahan D. R., McDonell M. B., Fihn S. D., Bradley K. A. The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Archives of Internal Medicine. 1998;158:1789–1795. doi: 10.1001/archinte.158.16.1789. doi:10.1001/archinte.158.16.1789. [DOI] [PubMed] [Google Scholar]
- Chossis I., Lane C., Gache P., Michaud P. A., Pécoud A., Rollnick S., Daeppen J. B. Effect of training on primary care residents’ performance in brief alcohol intervention: A randomized controlled trial. Journal of General Internal Medicine. 2007;22:1144–1149. doi: 10.1007/s11606-007-0240-2. doi:10.1007/s11606-007-0240-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman T. Do financial incentives for delivering health promotion counselling work? Analysis of smoking cessation activities stimulated by the quality and outcomes framework. BMC Public Health. 2010;10:167. doi: 10.1186/1471-2458-10-167. doi:10.1186/1471-2458-10-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denny C. H., Serdula M. K., Holtzman D., Nelson D. E. Physician advice about smoking and drinking: Are U.S. adults being informed? American Journal of Preventive Medicine. 2003;24:71–74. doi: 10.1016/s0749-3797(02)00568-8. doi:10.1016/S0749-3797(02)00568-8. [DOI] [PubMed] [Google Scholar]
- Dobscha S. K., Dickinson K. C., Lasarev M. R., Lee E. S. Associations between race and ethnicity and receipt of advice about alcohol use in the Department of Veterans Affairs. Psychiatric Services. 2009;60:663–670. doi: 10.1176/ps.2009.60.5.663. doi:10.1176/appi.ps.60.5.663. [DOI] [PubMed] [Google Scholar]
- Flocke S. A., Stange K. C. Direct observation and patient recall of health behavior advice. Preventive Medicine. 2004;38:343–349. doi: 10.1016/j.ypmed.2003.11.004. doi:10.1016/j.ypmed.2003.11.004. [DOI] [PubMed] [Google Scholar]
- Hamilton F. L., Laverty A. A., Gluvajic D., Huckvale K., Car J., Majeed A., Millett C. Effect of financial incentives on delivery of alcohol screening and brief intervention (ASBI) in primary care: Longitudinal study. Journal of Public Health. 2014;36:450–459. doi: 10.1093/pubmed/fdt121. doi:10.1093/pubmed/fdt121. [DOI] [PubMed] [Google Scholar]
- Hedrick S. C., Chaney E. F., Felker B., Liu C.-F., Hasenberg N., Heagerty P., Katon W. Effectiveness of collaborative care depression treatment in Veterans’ Affairs primary care. Journal of General Internal Medicine. 2003;18:9–16. doi: 10.1046/j.1525-1497.2003.11109.x. doi:10.1046/j.1525-1497.2003.11109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonas D. E., Garbutt J. C., Amick H. R., Brown J. M., Brownley K. A., Council C. L., Harris R. P. Behavioral counseling after screening for alcohol misuse in primary care: A systematic review and meta-analysis for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2012;157:645–654. doi: 10.7326/0003-4819-157-9-201211060-00544. doi:10.7326/0003-4819-157-9-201211060-00544. [DOI] [PubMed] [Google Scholar]
- Kaner E. F. S., Dickinson H. O., Beyer F. R., Campbell F., Schlesinger C., Heather N., Pienaar E. D. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database of Systematic Reviews. 2007 doi: 10.1002/14651858.CD004148.pub3. Issue 2, Article No. CD004148. doi:10.1002/14651858.CD004148.pub3. [DOI] [PubMed] [Google Scholar]
- Kaner E. F. S., Heather N., Brodie J., Lock C. A., McAvoy B. R. Patient and practitioner characteristics predict brief alcohol intervention in primary care. British Journal of General Practice. 2001;51:822–827. [PMC free article] [PubMed] [Google Scholar]
- Kleinman L. C., Norton E. C. What’s the risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Services Research. 2009;44:288–302. doi: 10.1111/j.1475-6773.2008.00900.x. doi:10.1111/j.1475-6773.2008.00900.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapham G. T., Achtmeyer C. E., Williams E. C., Hawkins E. J., Kivlahan D. R., Bradley K. A. Increased documented brief alcohol interventions with a performance measure and electronic decision support. Medical Care. 2012;50:179–187. doi: 10.1097/MLR.0b013e3181e35743. doi:10.1097/MLR.0b013e3181e35743. [DOI] [PubMed] [Google Scholar]
- Maust D. T., Mavandadi S., Klaus J., Oslin D. W. Missed opportunities: Fewer service referrals after positive alcohol misuse screens in VA primary care. Psychiatric Services. 2011;62:310–312. doi: 10.1176/ps.62.3.pss6203_0310. doi:10.1176/ps.62.3.pss6203_0310. [DOI] [PubMed] [Google Scholar]
- McKnight-Eily L. R., Liu Y., Brewer R. D., Kanny D., Lu H., Denny C. H., Collins J. the Centers for Disease Control and Prevention. Vital signs: Communication between health professionals and their patients about alcohol use—44 states and the District of Columbia, 2011. Morbidity and Mortality Weekly Report. 2014, January 10;63:16–22. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6301a4.htm. [PMC free article] [PubMed] [Google Scholar]
- Mokdad A. H., Marks J. S., Stroup D. F., Gerberding J. L. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. doi:10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Moyer V. A. the Preventive Services Task Force. Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: U.S. preventive services task force recommendation statement. Annals of Internal Medicine. 2013;159:210–218. doi: 10.7326/0003-4819-159-3-201308060-00652. doi:10.7326/0003-4819-159-3-201308060-00652. [DOI] [PubMed] [Google Scholar]
- Murray C. J., Atkinson C., Bhalla K., Birbeck G., Burstein R., Chou D., Wulf S. the U.S. Burden of Disease Collaborators. The state of US health, 1990-2010: Burden of diseases, injuries, and risk factors. JAMA. 2013;310:591–608. doi: 10.1001/jama.2013.13805. doi:10.1001/jama.2013.13805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Health Service. 2010 National Institute for Health and Care Excellence: Alcohol-use disorders: Prevention. NICE Guidance PH24. https://www.nice.org.uk/guidance/ph24.
- Nilsen P. Brief alcohol intervention—where to from here? Challenges remain for research and practice. Addiction. 2010;105:954–959. doi: 10.1111/j.1360-0443.2009.02779.x. doi:10.1111/j.1360-0443.2009.02779.x. [DOI] [PubMed] [Google Scholar]
- Nilsen P., McCambridge J., Karlsson N., Bendtsen P. Brief interventions in routine health care: A population-based study of conversations about alcohol in Sweden. Addiction. 2011;106:1748–1756. doi: 10.1111/j.1360-0443.2011.03476.x. doi:10.1111/j.1360-0443.2011.03476.x. [DOI] [PubMed] [Google Scholar]
- Ornstein S. M., Miller P. M., Wessell A. M., Jenkins R. G., Nemeth L. S., Nietert P. J. Integration and sustainability of alcohol screening, brief intervention, and pharmacotherapy in primary care settings. Journal of Studies on Alcohol and Drugs. 2013;74:598–604. doi: 10.15288/jsad.2013.74.598. doi:10.15288/jsad.2013.74.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oslin D. W., Ross J., Sayers S., Murphy J., Kane V., Katz I. R. the Behavioral Health Laboratory. Screening, assessment, and management of depression in VA primary care clinics. Journal of General Internal Medicine. 2006;21:46–50. doi: 10.1111/j.1525-1497.2005.0267.x. doi:10.1111/j.1525-1497.2005.0267.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pomerantz A. S., Kearney L. K., Wray L. O., Post E. P., McCarthy J. F. Mental health services in the medical home in the Department of Veterans Affairs: Factors for successful integration. Psychological Services. 2014;11:243–253. doi: 10.1037/a0036638. doi:10.1037/a0036638. [DOI] [PubMed] [Google Scholar]
- Rehm J., Baliunas D., Borges G. L., Graham K., Irving H., Kehoe T., Taylor B. The relation between different dimensions of alcohol consumption and burden of disease: An overview. Addiction. 2010;105:817–843. doi: 10.1111/j.1360-0443.2010.02899.x. doi:10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose H. L., Miller P. M., Nemeth L. S., Jenkins R. G., Nietert P. J., Wessell A. M., Ornstein S. Alcohol screening and brief counseling in a primary care hypertensive population: A quality improvement intervention. Addiction. 2008;103:1271–1280. doi: 10.1111/j.1360-0443.2008.02199.x. doi:10.1111/j.1360-0443.2008.02199.x. [DOI] [PubMed] [Google Scholar]
- Rubinsky A. D., Kivlahan D. R., Volk R. J., Maynard C., Bradley K. A. Estimating risk of alcohol dependence using alcohol screening scores. Drug and Alcohol Dependence. 2010;108:29–36. doi: 10.1016/j.drugalcdep.2009.11.009. doi:10.1016/j.drugalcdep.2009.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saitz R. Clinical practice. Unhealthy alcohol use. The New England Journal of Medicine. 2005;352:596–607. doi: 10.1056/NEJMcp042262. doi:10.1056/NEJMcp042262. [DOI] [PubMed] [Google Scholar]
- Szatkowski L., McNeill A., Lewis S., Coleman T. A comparison of patient recall of smoking cessation advice with advice recorded in electronic medical records. BMC Public Health. 2011;11:291. doi: 10.1186/1471-2458-11-291. doi:10.1186/1471-2458-11-291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tew J., Klaus J., Oslin D. W. The Behavioral Health Laboratory: Building a stronger foundation for the patient-centered medical home. Families, Systems, & Health. 2010;28:130–145. doi: 10.1037/a0020249. doi:10.1037/a0020249. [DOI] [PubMed] [Google Scholar]
- VHA Office of Analytics and Business Intelligence. 2011. Patient Experiences Dimensions of Care: Outpatient Reports. Available from the authors upon request.
- Vinson D. C., Manning B. K., Galliher J. M., Dickinson L. M., Pace W. D., Turner B. J. Alcohol and sleep problems in primary care patients: A report from the AAFP National Research Network. Annals of Family Medicine. 2010;8:484–492. doi: 10.1370/afm.1175. doi:10.1370/afm.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock E. P., Polen M. R., Green C. A., Orleans T., Klein J. the U.S. Preventive Services Task Force. ). Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: A summary of the evidence for the U.S. Preventive Services Task Force. Annals of Internal Medicine. 2004;140:557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. doi:10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- Williams E. C., Achtmeyer C. E., Thomas R. M., Grossbard J. R., Lapham G. T., Chavez L. J., Bradley K. A. Factors underlying quality problems with alcohol screening prompted by a clinical reminder in primary care: A multi-site qualitative study. Journal of General Internal Medicine. 2015;30:1125–1132. doi: 10.1007/s11606-015-3248-z. doi:10.1007/s11606-015-3248-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams E. C., Achtmeyer C. E., Young J. P., Rittmueller S. E., Ludman E. J., Lapham G. T., Bradley K. A. Local implementation of alcohol screening and brief intervention at five Veterans Health Administration primary care clinics: Perspectives of clinical and administrative staff. Journal of Substance Abuse Treatment. 2016;60:27–35. doi: 10.1016/j.jsat.2015.07.011. doi:10.1016/j.jsat.2015.07.011. [DOI] [PubMed] [Google Scholar]
- Williams E. C., Johnson M. L., Lapham G. T., Caldeiro R. M., Chew L., Fletcher G. S., Bradley K. A. Strategies to implement alcohol screening and brief intervention in primary care settings: A structured literature review. Psychology of Addictive Behaviors. 2011;25:206–214. doi: 10.1037/a0022102. doi:10.1037/a0022102. [DOI] [PubMed] [Google Scholar]
- Wright S. M., Craig T., Campbell S., Schaefer J., Humble C. Patient satisfaction of female and male users of Veterans Health Administration services. Journal of General Internal Medicine. 2006;21(Supplement 3):S26–S32. doi: 10.1111/j.1525-1497.2006.00371.x. doi:10.1111/j.1525-1497.2006.00371.x. [DOI] [PMC free article] [PubMed] [Google Scholar]