Abstract
Objective:
This study involves a pilot investigation of associations between marijuana and synthetic cannabis use with PTSD symptoms among a young adult sample of U.S. veterans.
Method:
In a cross-sectional survey of a community sample of 790 young adult U.S. veterans, we assessed demographics, combat severity, marijuana and synthetic cannabis use, expectancies of marijuana use, and PTSD symptoms.
Results:
Overall, 61.8% and 20.4% of our sample reported lifetime and past-month marijuana use, whereas 17.0% and 3.4% reported lifetime and past-month synthetic cannabis use. Veterans screening positive for PTSD were more likely to use marijuana and synthetic cannabis in their lifetime and in the past month. Positive PTSD screens, as well as greater expectancies that marijuana leads to relaxation and tension reduction, were associated with past-month marijuana use in logistic regression analyses. Expectancies moderated the relationship between PTSD and marijuana use, such that those with positive PTSD screens reporting higher levels of relaxation and tension-reduction expectancies were most likely to report past-month marijuana use.
Conclusions:
Our findings suggest an association of PTSD symptoms with marijuana and synthetic cannabis use among young adult U.S. veterans. Future research should further investigate the link between PTSD and marijuana use, as well as the rates and consequences of synthetic cannabis use among veterans.
Substance use among u.s. veterans with post-traumatic stress disorder (PTSD) is of growing concern (Kessler et al., 2005; Substance Abuse and Mental Health Services Administration, 2007), and a substantial number of U.S. veterans with PTSD use psychoactive substances (Carlson et al., 2010; Erbes et al., 2007; Hoge et al., 2006). Recent research suggests that PTSD symptoms and substance use are related (Brady et al., 2004; Jakupcak et al., 2010; Kehle et al., 2012), such that when PTSD symptoms become exacerbated, substance use increases (Back et al., 2014). When PTSD and substance use co-occur, veterans tend to experience poorer treatment outcomes (Norman et al., 2007; Ouimette et al., 1999; Young et al., 2005).
Marijuana use in particular deserves focused attention in this context, given the use of marijuana by veterans with PTSD (Calhoun et al., 2000; Institute of Medicine, 2010) and established associations between trauma exposure and marijuana use in other contexts (Kilpatrick et al., 2000; Vlahov et al., 2002). Although applicable to other substances, a coping model of marijuana use is a prominent explanation for co-occurring PTSD symptoms and marijuana use (Bonn-Miller et al., 2011) (i.e., those with PTSD symptoms who consume marijuana do so to cope with, control, or momentarily alleviate symptoms; Tomlinson et al., 2006). Compared with veterans without PTSD, those with PTSD report greater use of marijuana to cope, and severity of PTSD symptoms is associated with greater coping reasons for using marijuana (Boden et al., 2013). Moreover, exacerbation of PTSD symptoms that triggers cravings for marijuana use could in turn hinder the efficacy of PTSD treatment or lead to relapse (Back et al., 2014; Boden et al., 2013; Bonn-Miller et al., 2007, 2011).
To complicate issues, the growing popularity and availability of a new class of substances—synthetic cannabis or “spice” (synthetic cannabinoid receptor agonists that bind to similar brain cell receptors as the active ingredient of marijuana)—among young people may prompt new challenges (Hu et al., 2011; Johnston et al., 2013; Stogner & Miller, 2014). For instance, if synthetic cannabis has similar psychoactive effects to marijuana, the coping model of PTSD symptoms and marijuana use may apply to synthetic cannabis as well (i.e., those with PTSD symptoms may report greater use of the substance). Moreover, some forms of synthetic cannabis (at article submission) can be obtained legally in the United States, and drug test kits only recently became available for the military and employers to detect synthetic cannabis use. Not much is known about the drug’s effects on the brain, but users report more intense subjective “highs,” such as hallucinations, paranoia, and anxiety, in addition to the relaxation and elevated mood effects reported from marijuana (National Institute on Drug Abuse, 2015). Although synthetic cannabis use among veterans has received little research attention, Walker and colleagues (2014) found that about 1 in 10 active-duty Army soldiers in their sample reported past-90-day use, and those who reported any drug use were twice as likely to prefer synthetic cannabis over marijuana.
Veterans who do not utilize Veterans Health Administration (VHA) services are a population at risk for mental health concerns; of those with mental health need (e.g., those screening positive for PTSD), approximately 50% have not received services at the VHA (Bagalman, 2013; Schell & Marshall, 2008; VHA, 2013). Unfortunately, little is known about marijuana and synthetic cannabis use among this population. Previous studies examining PTSD symptoms and marijuana use have tended to recruit participants through treatment settings at the VHA or within the military behavioral health system (Back et al., 2014; Boden et al., 2013; Bonn-Miller et al., 2011, 2012a). Furthermore, previous research in this area has been largely limited to interviews with a small sample of veterans about their perceptions of relationships between their substance use and PTSD symptoms (Back et al., 2014). Larger surveys with U.S. veterans recruited outside of treatment settings could further elucidate potential links of PTSD symptoms with marijuana and synthetic cannabis use (Bonn-Miller et al., 2012a).
Using data from a larger research project (Pedersen et al., 2015, 2016), the current pilot study involved exploratory analyses examining PTSD symptoms—as well as marijuana and synthetic cannabis use—in a large sample of young adult U.S. veterans who were recruited via the Internet outside of any treatment setting and who are not known to be attempting to quit cannabis use (Boden et al., 2013). This study has three objectives based on previous research. First, this study provides data on marijuana and synthetic cannabis use among young adult veterans of the recent conflicts in Iraq and Afghanistan to extend previous studies investigating rates of marijuana (Bonn-Miller et al., 2012b) and synthetic cannabis use among military populations (Walker et al., 2014). Second, this study assesses associations of symptoms of PTSD with marijuana and synthetic cannabis use to build on prior research suggesting that those with PTSD symptoms may be more likely to report marijuana and synthetic cannabis use (Cougle et al., 2011; Boden et al., 2013). Last, building on research examining marijuana use as a means to cope with PTSD symptoms, this study explores whether the expectancy that marijuana use leads to relaxation and tension-reduction effects moderates the relationship between marijuana use and PTSD symptoms: namely, whether greater relaxation and tension-reduction expectancies are associated with greater use among those screening positive (vs. not) for PTSD.
Method
Research procedures
The data for this pilot study are derived from a larger online survey examining health and risk behaviors and attitudes of young adult U.S. veterans (Pedersen et al., 2015, 2016). Participants were recruited through Facebook advertisements targeted toward young veterans of the conflicts in Iraq and Afghanistan. We had a series of checks in place to verify that participants were actual veterans (Kramer et al., 2014); more details about these methods (e.g., ensuring consistent responses on items such as branch of service, rank and pay grade at discharge) and representativeness of the sample are described in the project protocol (Pedersen et al., 2015). Participants accessed the survey through clicking on an ad, reading a statement about the study, and indicating consent.
Participants had to meet the following eligibility criteria: (a) be separated veterans from the Air Force, Army, Marines, or Navy; (b) be between ages 18 and 34; (c) have access to a computer or smartphone with Internet; and (d) have a working Facebook account. Participants were excluded if they were still affiliated with the military through the National Guard or reserve units. Participants received a $20 gift card for completing the 20- to 30-minute survey. The RAND Human Subjects Protection Committee approved all procedures in this study.
Measures
Demographics.
We collected self-reported age, gender, and race/ethnicity. We used a combat trauma exposure scale (Schell & Marshall, 2008) to assess the number of 11 specific combat experiences one had while deployed (e.g., having a friend who was seriously wounded or killed, being injured). Participants responded yes/no to each of these experiences. Affirmative responses were summed to form a combat severity score ranging from 0 to 11. Reliability of the 11 items in our sample was adequate (α = .84).
PTSD symptoms.
We used the Primary Care PTSD Scale (PC-PTSD), a four-item screen for potential PTSD in the past month that has been validated with veteran populations (Prins et al., 2003). Scores range from 0 to 4, with 3 or higher indicating participants screened positive for PTSD and 2 or less indicating they screened negative. Reliability in our sample was adequate (α = .87).
Substance use.
Participants indicated if they had ever used marijuana (pot, hash, hashish; in smoke, vapor, or edible form) in their lifetime and, if so, how many days they used in the past 30 days. They also indicated if they had ever used synthetic cannabis (“spice” or “K2”) in their lifetime and, if so, how many days they used in the past 30 days.
Relaxation and tension-reduction marijuana use expectancy.
The expectancy that marijuana leads one to feel relaxed and relieves tension was assessed with the relaxation and tension-reduction item (“Marijuana helps a person relax and feel less tense”) from the Marijuana Effect Expectancy Questionnaire-Brief version (Torrealday et al., 2008). This single item represents the subscale of relaxation and tension reduction that was modified from the three-item subscale from the original, longer Marijuana Effect Expectancy Questionnaire (Schafer & Brown, 1991). The subscale in the brief version contains wording to capture the two items in the original scale that most highly loaded onto the factor. Participants rated on a 5-point scale how much they agreed or disagreed with the item (1 = disagree strongly, 3 = uncertain, 5 = agree strongly).
Statistical analyses
We calculated descriptive statistics for demographics, PTSD symptoms, marijuana expectancy, and substance use measures. We then ran independent samples t tests to examine differences in demographics, substance use, and marijuana expectancies between those who screened positive for PTSD and those who did not. Last, we conducted a logistic regression model to examine potential correlates of any past-month marijuana use, comprising PTSD screening status, relaxation and tension-reduction marijuana use expectancies, and the interaction between PTSD status and expectancies. Continuous variables were mean centered to facilitate interpretation. All analyses were conducted in SPSS Statistics for Windows, Version 21 (IBM Corp., Armonk, NY).
Results
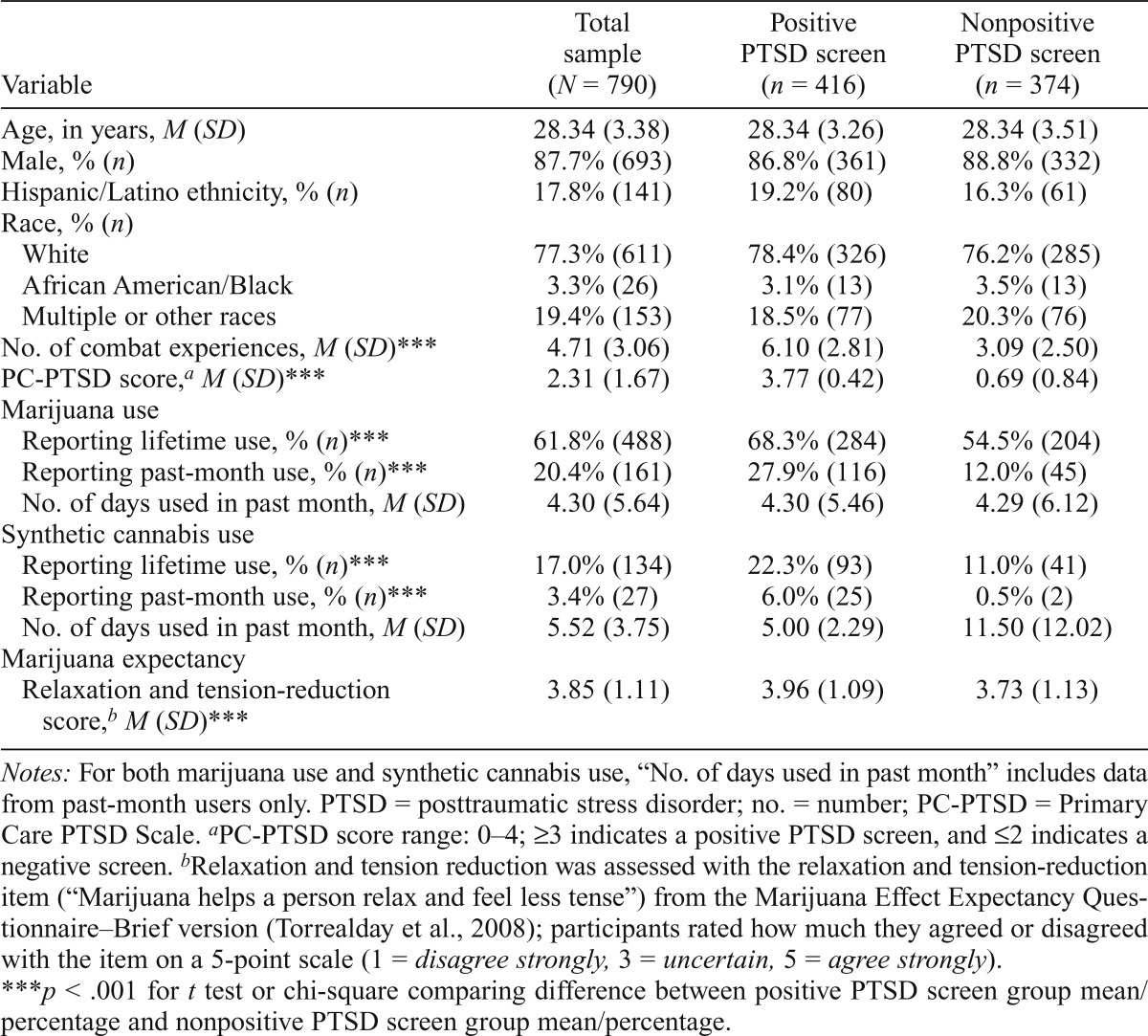
Of 2,275 individuals who accessed our consent page through Facebook, 1,023 (45.0%) participated in our survey, and 790 of those (77.2%) provided complete data for the analyses in this pilot study. Veterans were primarily Army (59.9%) and Marine Corps (24.7%) veterans, with a minority having served in the Navy (8.6%) and Air Force (6.8%). About half (55.6%) reported attending an appointment at the VHA for any reason in the past year, with 21.8% using the VHA for any reason in the past month. Participant demographics, PTSD symptoms, substance use, and marijuana expectancies can be found in Table 1. In summary, participants screening positive for PTSD were more likely than participants not screening positive for PTSD to have used marijuana and synthetic cannabis in their lifetimes and in the past month. Participants screening positive for PTSD were more likely than those not screening positive to agree with expectancies that marijuana use leads to relaxation and tension reduction (Table 1).
Table 1.
Participant demographics, PTSD symptoms, substance use, and marijuana expectancies
| Variable | Total sample (N = 790) | Positive PTSD screen (n = 416) | Nonpositive PTSD screen (n = 374) |
| Age, in years, M (SD) | 28.34 (3.38) | 28.34 (3.26) | 28.34 (3.51) |
| Male, % (n) | 87.7% (693) | 86.8% (361) | 88.8% (332) |
| Hispanic/Latino ethnicity, % (n) | 17.8% (141) | 19.2% (80) | 16.3% (61) |
| Race, % (n) | |||
| White | 77.3% (611) | 78.4% (326) | 76.2% (285) |
| African American/Black | 3.3% (26) | 3.1% (13) | 3.5% (13) |
| Multiple or other races | 19.4% (153) | 18.5% (77) | 20.3% (76) |
| No. of combat experiences, M (SD)*** | 4.71 (3.06) | 6.10 (2.81) | 3.09 (2.50) |
| PC-PTSD score,a M (SD)*** | 2.31 (1.67) | 3.77 (0.42) | 0.69 (0.84) |
| Marijuana use | |||
| Reporting lifetime use, % (n)*** | 61.8% (488) | 68.3% (284) | 54.5% (204) |
| Reporting past-month use, % (n)*** | 20.4% (161) | 27.9% (116) | 12.0% (45) |
| No. of days used in past month, M (SD) | 4.30 (5.64) | 4.30 (5.46) | 4.29 (6.12) |
| Synthetic cannabis use | |||
| Reporting lifetime use, % (n)*** | 17.0% (134) | 22.3% (93) | 11.0% (41) |
| Reporting past-month use, % (n)*** | 3.4% (27) | 6.0% (25) | 0.5% (2) |
| No. of days used in past month, M (SD) | 5.52 (3.75) | 5.00 (2.29) | 11.50 (12.02) |
| Marijuana expectancy | |||
| Relaxation and tension-reduction score,b M (SD)*** | 3.85 (1.11) | 3.96 (1.09) | 3.73 (1.13) |
Notes: For both marijuana use and synthetic cannabis use, “No. of days used in past month” includes data from past-month users only. PTSD = posttraumatic stress disorder; no. = number; PC-PTSD = Primary Care PTSD Scale.
PC-PTSD score range: 0-4; ≥3 indicates a positive PTSD screen, and ≤2 indicates a negative screen.
Relaxation and tension reduction was assessed with the relaxation and tension-reduction item (“Marijuana helps a person relax and feel less tense”) from the Marijuana Effect Expectancy Questionnaire–Brief version (Torrealday et al., 2008); participants rated how much they agreed or disagreed with the item on a 5-point scale (1 = disagree strongly, 3 = uncertain, 5 = agree strongly).
p < .001 for t test or chi-square comparing difference between positive PTSD screen group mean/percentage and nonpositive PTSD screen group mean/percentage.
Logistic regression results indicated that marijuana use in the past month was associated with a positive screen for PTSD (exponentiated b = 4.19, 95% CI [2.44, 7.18]) and higher expectancies about relaxation and tension reduction from marijuana use (exponentiated b = 3.81, 95% CI [2.32, 6.26]). The interaction for PTSD status by relaxation and tension reduction was significant (exponentiated b = 0.41, 95% CI [0.24, 0.72]); specifically, those with a positive PTSD screen who reported high expectancies regarding the relaxation and tension-reduction effects of marijuana were the most likely to report past-month marijuana use.
Discussion
This is the first study, to our knowledge, to look at marijuana and synthetic cannabis use among a large sample of veterans outside a clinical or VHA setting and who are not known to be attempting to quit cannabis use (Boden et al., 2013). No participants were still affiliated with the military through the National Guard or reserve units, and only about half reported that they had ever been to a VHA clinic in the past year for any reason. Overall, our findings suggested an association of PTSD symptoms with marijuana and synthetic cannabis use among young adult U.S. veterans. First, we found that lifetime and past-month marijuana and synthetic cannabis use, as well as number of past-month days of use among current use, was moderately high in this sample. For example, one in five participants reported using marijuana in the past month, with a 17% lifetime prevalence rate for synthetic cannabis use. We also found that those who screened positive for PTSD (vs. those who did not) were more likely to use marijuana and synthetic cannabis both in their lifetimes and in the past month. Concretely, the rates of past-month marijuana use and lifetime synthetic cannabis use were approximately twice as high among those who screened positive for PTSD as compared with those who did not.
We found that the association between PTSD symptoms and marijuana use may be moderated by beliefs (among those screening positive for PTSD) that marijuana use generally does lead to effects of relaxation and tension reduction. That is, veterans who screened positive for PTSD in our sample and who reported high expectancies about the relaxation and tension-reduction effects of marijuana were most likely to report past-month marijuana use. These findings complement previous research indicating a relationship between PTSD symptom severity and motives to use cannabis to cope with PTSD symptoms (Boden et al., 2013). The belief that marijuana would lead one to feel calm/relaxed may be related to reducing PTSD symptoms specifically associated with hyperarousal, anger/irritability, or difficulties falling asleep. However, it should be noted that we assessed expectancies (i.e., what one expects to happen if using) and not actual effects of the drug (e.g., does the person subjectively report that marijuana leads them to feel relaxed). Moreover, our study did not assess expectancies of synthetic cannabis use, as no such measure currently exists. Follow-up studies could consider subjective reports of actual relaxation (including reduced symptom expression), the association between marijuana use and symptom expression within the specific clusters of PTSD (e.g., intrusive symptoms, alterations in arousal and reactivity), and the synthetic cannabis use expectancies.
Our results highlight the need for future research that prospectively and rigorously investigates the relationship between PTSD and cannabis use—both marijuana and synthetic cannabis—and addresses limitations present in the current study. For instance, a central limitation of this study is the cross-sectional and self-reported nature of the data, which does not provide a basis for strong causal inference. Although findings are consistent with the notion that marijuana is used as a means of reducing PTSD symptoms, other causal pathways are also plausible and cannot be empirically distinguished with our cross-sectional data. Future research would benefit from a longitudinal design that involves other data sources (e.g., participant observation, medical records) and measures of subjective effects actually experienced when using marijuana. In addition, pre-military PTSD symptoms and substance use were not collected in this cross-sectional study; no inferences can be made about how marijuana may or may not have been used in the absence of PTSD for those who may have developed symptoms while in military service. Importantly, this study used screening measures for PTSD and self-reported frequency of substance use. Future research should use measures that more comprehensively address the full range of PTSD symptoms, formal diagnoses for PTSD and substance use disorders, other possibly-related mental health issues (e.g., conduct or antisocial personality disorder), and other or more granular aspects of substance use (e.g., quantity of use, number of times used per day). Last, researchers in this area should consider use of medical marijuana and state legalization of medical or recreational marijuana use in their selection of variables (Bonn-Miller et al., 2012b). This research would have the potential to better help in designing behavioral health screening, assessment, and treatment services for veteran populations.
Acknowledgments
The authors acknowledge the RAND Multimode Interviewing Capability team and Michael Woodward for assistance with survey development and recruitment.
Declarations of Interest
Sean Grant’s fiancée is a salaried employee of Eli Lilly and Company and owns stock. Sean Grant has accompanied his fiancée on company-sponsored travel. All other authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
Footnotes
This research was supported by National Institute on Alcohol Abuse and Alcoholism Grant R34AA022400 awarded to Eric R. Pedersen.
References
- Bagalman E. Mental disorders among OEF/OIF veterans using VA health care: Facts and figures. Washington, DC: Congressional Research Service; 2013. [Google Scholar]
- Back S. E., Killeen T. K., Teer A. P., Hartwell E. E., Federline A., Beylotte F., Cox E. Substance use disorders and PTSD: An exploratory study of treatment preferences among military veterans. Addictive Behaviors. 2014;39:369–373. doi: 10.1016/j.addbeh.2013.09.017. doi:10.1016/j.addbeh.2013.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boden M. T., Babson K. A., Vujanovic A. A., Short N. A., Bonn-Miller M. O. Posttraumatic stress disorder and cannabis use characteristics among military veterans with cannabis dependence. American Journal on Addictions. 2013;22:277–284. doi: 10.1111/j.1521-0391.2012.12018.x. doi:10.1111/j.1521-0391.2012.12018.x. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Bucossi M. M., Trafton J. A. The underdiagnosis of cannabis use disorders and other Axis-I disorders among military veterans within VHA. Military Medicine. 2012a;177:786–788. doi: 10.7205/milmed-d-12-00052. doi:10.7205/MILMED-D-12-00052. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Harris A. H. S., Trafton J. A. Prevalence of cannabis use disorder diagnoses among veterans in 2002, 2008, and 2009. Psychological Services. 2012b;9:404–16. doi: 10.1037/a0027622. doi:10.1037/a0027622. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Vujanovic A. A., Drescher K. D. Cannabis use among military veterans after residential treatment for posttraumatic stress disorder. Psychology of Addictive Behaviors. 2011;25:485–491. doi: 10.1037/a0021945. doi:10.1037/a0021945. [DOI] [PubMed] [Google Scholar]
- Bonn-Miller M. O., Vujanovic A. A., Feldner M. T., Bernstein A., Zvolensky M. J. Posttraumatic stress symptom severity predicts marijuana use coping motives among traumatic event-exposed marijuana users. Journal of Traumatic Stress. 2007;20:577–586. doi: 10.1002/jts.20243. doi:10.1002/jts.20243. [DOI] [PubMed] [Google Scholar]
- Brady K. T., Back S. E., Coffey S. F. Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science. 2004;13:206–209. doi:10.1111/j.0963-7214.2004.00309.x. [Google Scholar]
- Calhoun P. S., Sampson W. S., Bosworth H. B., Feldman M. E., Kirby A. C., Hertzberg M. A., Beckham J. C. Drug use and validity of substance use self-reports in veterans seeking help for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2000;68:923–927. doi:10.1037/0022-006X.68.5.923. [PubMed] [Google Scholar]
- Carlson K. F., Nelson D., Orazem R. J., Nugent S., Cifu D. X., Sayer N. A. Psychiatric diagnoses among Iraq and Afghanistan war veterans screened for deployment-related traumatic brain injury. Journal of Traumatic Stress. 2010;23:17–24. doi: 10.1002/jts.20483. doi:10.1002/jts.20483. [DOI] [PubMed] [Google Scholar]
- Cougle J. R., Bonn-Miller M. O., Vujanovic A. A., Zvolensky M. J., Hawkins K. A. Posttraumatic stress disorder and cannabis use in a nationally representative sample. Psychology of Addictive Behaviors. 2011;25:554–558. doi: 10.1037/a0023076. doi:10.1037/a0023076. [DOI] [PubMed] [Google Scholar]
- Erbes C., Westermeyer J., Engdahl B., Johnsen E. Posttraumatic stress disorder and service utilization in a sample of service members from Iraq and Afghanistan. Military Medicine. 2007;172:359–363. doi: 10.7205/milmed.172.4.359. doi:10.7205/MILMED.172.4.359. [DOI] [PubMed] [Google Scholar]
- Hoge C. W., Auchterlonie J. L., Milliken C. S. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–1032. doi: 10.1001/jama.295.9.1023. doi:10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Hu X., Primack B. A., Barnett T. E., Cook R. L. College students and use of K2: An emerging drug of abuse in young persons. Substance Abuse Treatment, Prevention, and Policy. 2011;6:16. doi: 10.1186/1747-597X-6-16. doi:10.1186/1747-597X-6-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine. Returning home from Iraq and Afghanistan: Preliminary assessment of readjustment needs of veterans, service members, and their families. Washington, DC: National Academies Press; 2010. [PubMed] [Google Scholar]
- Jakupcak M., Tull M. T., McDermott M. J., Kaysen D., Hunt S., Simpson T. PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors. 2010;35:840–843. doi: 10.1016/j.addbeh.2010.03.023. doi:10.1016/j.addbeh.2010.03.023. [DOI] [PubMed] [Google Scholar]
- Johnston L., O’Malley P. M., Bachman J. G., Schulenberg J. E.2013Monitoring the Future National Survey Results on Drug Use, 1975–2011 .Rockville, MI: Institute for Social Research, the University of Michigan [Google Scholar]
- Kehle S. M., Ferrier-Auerbach A. G., Meis L. A., Arbisi P. A., Erbes C. R., Polusny M. A. Predictors of postdeployment alcohol use disorders in National Guard soldiers deployed to Operation Iraqi Freedom. Psychology of Addictive Behaviors. 2012;26:42–50. doi: 10.1037/a0024663. doi:10.1037/a0024663. [DOI] [PubMed] [Google Scholar]
- Kessler R. C., Berglund P., Demler O., Jin R., Merikangas K. R., Walters E. E. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. doi:10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kilpatrick D. G., Acierno R., Saunders B., Resnick H. S., Best C. L., Schnurr P. P. Risk factors for adolescent substance abuse and dependence: Data from a national sample. Journal of Consulting and Clinical Psychology. 2000;68:19–30. doi: 10.1037//0022-006x.68.1.19. doi:10.1037/0022-006X.68.1.19. [DOI] [PubMed] [Google Scholar]
- Kramer J., Rubin A., Coster W., Helmuth E., Hermos J., Rosenbloom D., Lachowicz M. Strategies to address participant misrepresentation for eligibility in Web-based research. International Journal of Methods in Psychiatric Research. 2014;23:120–129. doi: 10.1002/mpr.1415. doi:10.1002/mpr.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Drug Abuse. DrugFacts: Synthetic cannabinoids. 2015. Retrieved from http://www.drugabuse.gov/publications/drugfacts/synthetic-cannabinoids. [Google Scholar]
- Norman S. B., Tate S. R., Anderson K. G., Brown S. A. Do trauma history and PTSD symptoms influence addiction relapse context? Drug and Alcohol Dependence. 2007;90:89–96. doi: 10.1016/j.drugalcdep.2007.03.002. doi:10.1016/j.drugalcdep.2007.03.002. [DOI] [PubMed] [Google Scholar]
- Ouimette P. C., Finney J. W., Moos R. H. Two-year posttreatment functioning and coping of substance abuse patients with posttraumatic stress disorder. Psychology of Addictive Behaviors. 1999;13:105–114. doi:10.1037/0893-164X.13.2.105. [Google Scholar]
- Pedersen E. R., Helmuth E. D., Marshall G. N., Schell T. L., PunKay M., Kurz J. Using Facebook to recruit young adult veterans: Online mental health research. JMIR Research Protocols. 2015;4:e63. doi: 10.2196/resprot.3996. doi:10.2196/resprot.3996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen E. R., Marshall G. N., Schell T. L., Neighbors C. Young adult veteran perceptions of peers’ drinking behavior and attitudes. Psychology of Addictive Behaviors. 2016;30:39–51. doi: 10.1037/adb0000120. doi:10.1037/adb0000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prins A., Ouimette P., Kimerling R., Cameron R. P., Hugelshofer D. S., Shaw-Hegwer J., Sheikh J. I. The Primary Care PTSD Screen (PC-PTSD): Development and operating characteristics. Primary Care Psychiatry. 2003;9:9–14. [Google Scholar]
- Schafer J., Brown S. A. Marijuana and cocaine effect expectancies and drug use patterns. Journal of Consulting and Clinical Psychology. 1991;59:558–565. doi: 10.1037//0022-006x.59.4.558. doi:10.1037/0022-006X.59.4.558. [DOI] [PubMed] [Google Scholar]
- Schell T. L., Marshall G. N. Survey of individuals previously deployed for OEF/OIF. In: Tanielian T., Jaycox L. H., editors. Invisible wounds of war: Psychological and cognitive injuries, their consequences, and services to assist recovery. Santa Monica, CA: RAND MG-720; 2008. [Google Scholar]
- Stogner J. M., Miller B. L. A spicy kind of high: A profile of synthetic cannabinoid users. Journal of Substance Use. 2014;19:199–205. doi:10.3109/14659891.2013.770571. [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Results from the 2006 National Survey on Drug Use and Health: National findings. Rockville, MD: Office of Applied Studies; 2007. [Google Scholar]
- Tomlinson K. L., Tate S. R., Anderson K. G., McCarthy D. M., Brown S. A. An examination of self-medication and rebound effects: Psychiatric symptomatology before and after alcohol or drug relapse. Addictive Behaviors. 2006;31:461–474. doi: 10.1016/j.addbeh.2005.05.028. doi:10.1016/j.addbeh.2005.05.028. [DOI] [PubMed] [Google Scholar]
- Torrealday O., Stein L. A., Barnett N., Golembeske C., Lebeau R., Colby S. M., Monti P. M. Validation of the Marijuana Effect Expectancy Questionnaire-Brief. Journal of Child & Adolescent Substance Abuse. 2008;17:1–17. doi: 10.1080/15470650802231861. doi:10.1080/15470650802231861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Veterans Health Administration, Department of Veterans Affairs. Analysis of VA Health Care Utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) Veterans–Revised. Washington, DC: Epidemiology Program, Post-Deployment Health Group, Office of Public Health; 2013. [Google Scholar]
- Vlahov D., Galea S., Resnick H., Ahern J., Boscarino J. A., Bucuvalas M., Kilpatrick D. Increased use of cigarettes, alcohol, and marijuana among Manhattan, New York, residents after the September 11th terrorist attacks. American Journal of Epidemiology. 2002;155:988–996. doi: 10.1093/aje/155.11.988. doi:10.1093/aje/155.11.988. [DOI] [PubMed] [Google Scholar]
- Walker D., Neighbors C., Walton T., Pierce A., Mbilinyi L., Kaysen D., Roffman R. Spicing up the military: Use and effects of synthetic cannabis in substance abusing army personnel. Addictive Behaviors. 2014;39:1139–1144. doi: 10.1016/j.addbeh.2014.02.018. doi:10.1016/j.addbeh.2014.02.018. [DOI] [PubMed] [Google Scholar]
- Young H. E., Rosen C. S., Finney J. W. A survey of PTSD screening and referral practices in VA addiction treatment programs. Journal of Substance Abuse Treatment. 2005;28:313–319. doi: 10.1016/j.jsat.2005.02.006. doi:10.1016/j.jsat.2005.02.006. [DOI] [PubMed] [Google Scholar]