Summary
Parathyroid carcinoma represents an extremely rare neoplasm with diverse clinical manifestations. Herein we aimed at presenting an unique case of a young patient with late manifestations of parathyroid cancer and reviewing the relevant literature. A 45-year-old male patient presented in the Outpatient Clinic with an episode of nephrolithiasis. His personal medical history includes: recurrent episodes of nephrolithiasis, laminectomy in the cervical spine due to ossification of the cervical ligamentum flavum and surgical resection of a giant cell tumor of the brain. Laboratory testing revealed findings of primary hyperparathyroidism (serum calcium 16,0 mmol/l phosphorus 1,46 mg/dl and parathyroid hormone/PTH 8560 pg/ml). Neck ultrasound and technetium-99 m sestamibi scan were performed showing a parathyroid tumor. Due to the persistently high serum calcium and PTH levels, the high alkaline phosphatase levels (440 IU/L) and the late manifestations of HPT, surgical excision of the tumor was performed. The tumor was identified as parathyroid carcinoma. Immediately after surgery serum calcium and phosphorus levels were normalized. The patient is on a regular follow-up program with no signs of recurrence or metastasis one year after the excision. We describe the coexistence of rare late manifestations of HPT, which had not been adequately investigated at their onset in this young patient. Therefore, increased awareness is needed in order to recognize and further investigate signs or symptoms of HPT.
Keywords: parathyroid carcinoma, primary hyperparathyroidism
Introduction
Parathyroid carcinoma represents an extremely rare neoplasmatic entity, accounting for approximately 1% of primary hyperparathyroidism (HPT). Although hormonally functional tumors are observed in the majority of cases, clinical manifestations of parathyroid carcinoma can vary from none (asymptomatic patients) to severe manifestations of hypercalcemia or parathyrotoxicosis. Thus, its diagnosis remains a challenge for the clinicians and is primarily based on laboratory and imaging testing (1).
Herein we aimed at presenting an unique case of a young patient with severe manifestations of parathyroid cancer and reviewing the relevant literature.
Case presentation
A 45-year-old Greek Caucasian male patient presented in the Outpatient Clinic of our Department with abrupt, severe, colicky pain in the flank and ipsilateral lower abdomen and diffuse bone pain. His personal medical history includes: recurrent episodes of nephrolithiasis, laminectomy in the cervical spine due to ossification of the cervical ligamentum flavum in C2-C3 and C4-C5 without signs of myelopathy two years ago and surgical resection of a giant cell tumor of the brain one year ago. No familial history of cancer is recorded. Based on the clinical examination and renal ultrasonography the patient was diagnosed with another episode of nephrolithiasis. Beyond that, however, laboratory testing revealed findings of primary hyperparathyroidism (serum calcium 16,0 mmol/l with normal values 8–10.4 mmol/L, phosphorus 1,46 mg/dl with normal values 2.5–5.9 mg/dl and parathyroid hormone/PTH 8560 pg/ml with normal values 8–76 pg/ml). Thus, the patient was admitted for further diagnostic procedures.
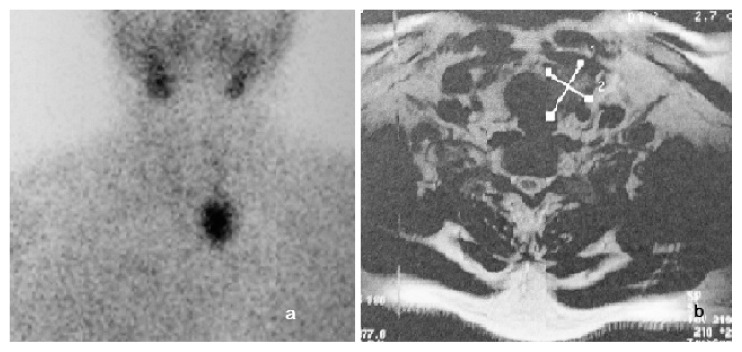
During his admittance the patient’s history and medical records were carefully reviewed. As shown in Figure 1, the patient had been suffering from misdiagnosed manifestations of hypercalcemia for the last two years. Based on his history, neck ultrasound and technetium-99 m sestamibi scan were performed revealing a parathyroid tumor, as shown in Figure 2. No further abnormalities were observed in the thorax and abdomen CT and neck MRI that followed. Due to the persistently high serum calcium and PTH levels, the high alkaline phosphatase levels (440 IU/L with normal values 38–155 IU/L) and the late manifestations of HPT, surgical excision of the tumor was performed. According to the histopathology the tumor was identified as parathyroid carcinoma and total surgical excision was achieved. Immediately after surgery serum calcium and phosphorus levels were normalized. The patient is on a regular follow-up program with no signs of recurrence or metastasis one year after the excision.
Figure 1.
a) Ossification of the cervical ligamentum flavum in C2-C3 and C4-C5 without signs of myelopathy. b) Nephrolithiasis in both kidneys and c. Left parietal bone tumor (5.5×3.2×4.4 cm) from an MRI scan.
Figure 2.
Technetium-99 m sestamibi scan and MRI scan showing the parathyroid tumor.
Discussion
In our case report we describe the coexistence of rare late manifestations of HPT, such as recurrent nephrolithiasis, ossification of the cervical ligamentum flavum and brown tumor, which had not been adequately investigated at their onset in this young patient.
The clinical presentation of parathyroid carcinoma is diverse and not pathognomonic. Skeletal involvement is rather common in parathyroid carcinoma (22–91%) (2). It primarily concerns diffuse osteopenia, osteoporosis, or pathological fractures and osteitis fibrosa cystica, subperiostial bone resorption or absence of the lamina dura. Our patient presented with two rare skeletal manifestations of HPT that were misdiagnosed and thus, surgically removed during the initial evaluations of the patient. Firstly, brown tumor constitutes a rare osseous lesion observed as a focal manifestation of osteitis fibrosa cystica that had been considered a prominent manifestation of primary HPT in the past (3). Thus, brown tumors are well described radiological findings of primary HPT that have been previously reported in 4.5–24% of patients with primary HPT (4, 5). In our patient histopathology of the brown tumor it was initially misdiagnosed as a giant cell tumor of the bone. Of note, such misdiagnoses are also evident in the recent literature (6).
Secondly, our patient presented with another extremely rare skeletal manifestation, ossification of the cervical ligamentum flavum which is caused by mechanical stress, growth factors and trauma and has been exceptionally reported in limited case reports in Caucasian people (7). To our knowledge, there is no such previous report in a patient with hyperparathyroidism of any cause.
Except for those rare skeletal manifestations, our patient presented also with ligament calcification of the knee joint (5). In addition, our patient’s clinical presentation was characterized by concomitant skeletal and renal manifestations (recurrent episodes of nephrolithiasis) which are rarely seen in benign primary HPT and are rather indicative of parathyroid carcinoma (1). Beyond the high index of clinical suspicion, our patient presented also with extremely increased calcium, PTH levels and alkaline phosphatase. Therefore, the recommended imaging approach for the diagnosis of parathyroid cancer (1) was followed that combines technetium-99 m sestamibi scan and a neck ultrasound. Thorax, neck and abdomen CT or MRI scans are also advisable and were performed in our patient in order to exclude metastatic lesions due to the observed severe clinical manifestations. Complete tumor resection was achieved as confirmed by the histopathology. An immediate normalization of calcium and PTH levels was observed that persists one year after initial surgery. Taking into consideration the high recurrence (more than 50%) and metastatic (approximately 25%) rate of the disease (1), long-term regular follow-up visits should be performed.
In conclusion, parathyroid carcinoma is a rare neoplasm with diverse clinical manifestations. Since the patients are often referred to primary care physicians, general surgeons, orthopedic surgeons or neurosurgeons for their initial symptoms, increased awareness is needed in order to recognize and further investigate signs or symptoms mimicking those observed in HPT.
Footnotes
Conflicts of interest
None declared.
References
- 1.Wei CH, Harari A. Parathyroid carcinoma: update and guidelines for management. Curr Treat Options Oncol. 2012;13:11–23. doi: 10.1007/s11864-011-0171-3. [DOI] [PubMed] [Google Scholar]
- 2.Shane E. Clinical review 122: Parathyroid carcinoma. J Clin Endocrinol Metab. 2001;86(2):485–93. doi: 10.1210/jcem.86.2.7207. [DOI] [PubMed] [Google Scholar]
- 3.Walker MD, Rubin M, Silverberg SJ. Nontraditional manifestations of primary hyperparathyroidism. J Clin Densitom. 2013;16:40–7. doi: 10.1016/j.jocd.2012.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Keyser JS, Postma GN. Brown tumor of the mandible. Am J Otolaryngol. 1996;17:407–10. doi: 10.1016/s0196-0709(96)90075-7. [DOI] [PubMed] [Google Scholar]
- 5.Polat P, Kantarci M, Alper F, et al. The spectrum of radiographic findings in primary hyperparathyroidism. Clin Imaging. 2002;26:197–205. doi: 10.1016/s0899-7071(01)00386-2. [DOI] [PubMed] [Google Scholar]
- 6.Vera L, Dolcino M, Mora M, et al. Primary hyperparathyroidism diagnosed after surgical ablation of a costal mass mistaken for giant-cell bone tumor: a case report. J Med Case Rep. 2011;5:596. doi: 10.1186/1752-1947-5-596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fotakopoulos G, Alexiou GA, Mihos E, et al. Ossification of the ligamentum flavum in cervical and thoracic spine. Report of three cases. Acta Neurol Belg. 2010;110:186–9. [PubMed] [Google Scholar]