Abstract
Background
Nationally, immunization coverage for the DTaP/3HPV/1MMR/3HepB/3Hib/1VZV antigen series in children ages 19–35 months are near or above the Healthy People 2020 target (80%). However, children in lower socioeconomic families experience lower coverage rates.
Objective
Using a community-based participatory research (CBPR) approach, Community Health Improvement for Milwaukee Children (CHIMC) intervened to reduce disparities in childhood immunizations.
Methods
The CHIMC adopted a self-assessment to examine the effectiveness of adhering to CBPR principles. Using behavior change models, CHIMC implemented education, social marketing campaign, and theory of planned behavior interventions. Community residents and organizational representatives vetted all processes, messages, and data collection tools.
Results
Adherence to the principles of CBPR was consistently positive over the 8-year period. CHIMC enrolled 565 parents/caregivers with 1,533 children into educational and planned behavior change (PBC) interventions, and enrolled another 406 surveyed for the social marketing campaign. Retention rate was high (80%) with participants being predominately Black females (90%) and the unemployed (64%); children’s median age was 6.2 years. Increased knowledge about immunizations was consistently observed among parents/caregivers. Social marketing data revealed high recognition (85%) of the community-developed message (“Take Control: Protect Your Child with Immunizations”). Barriers and facilitators to immunize children revealed protective factors positively correlated with up-to-date (UTD) status (p < 0.007). Ultimately, children between the ages of 19 and 35 months whose parents/caregivers completed education sessions and benefitted from a community-wide social marketing message increased their immunization status from 45% baseline to 82% over 4 years.
Conclusions
Using multilayered interventions, CHIMC contributed to the elimination of immunization disparities in children. A culturally tailored CBPR approach is effective to eliminate immunization disparities.
Keywords: Immunizations, community-based participatory research, community engagement, health disparities, action research, community improvement
In the United States, immunization coverage rates are increasing, yet in many communities these rates do not approach the national goals of Healthy People 2020.1,2 This is partially owing to persisting disparities experienced by racial/ethnic groups.3,4 In particular, children living in lower socioeconomic families have much lower coverage rates.2,5 Religious objections, misconceptions that vaccines increase negative health outcomes, and unfamiliarity with diseases that are suppressed by population-wide vaccinations foment distrust among many.6 With increasingly complex immunization schedules, escalating expectations of performance in primary care, and increasing documentation demands on primary care physicians, it is important to understand and promote population-tailored interventions. For example, previous reviews have identified several promising strategies to improve immunization rates.1,7 This manuscript highlights the components of a CBPR project that aims to eliminate immunization disparities in an urban, underserved population.
Nationally, the immunization antigen series 4:3:1:3:3:1 (4 diphtheria, tetanus, acellular pertussis; 3 polio; 1 measles, mumps rubella; 3 hepatitis b; 3 Haemophilus influenzae b; 1 varicella) for children between the ages of 19 and 35 months are near or above the Healthy People 2020 target of 80%. Wisconsin school laws on immunizations are very effective in achieving higher immunization coverage at school entry regardless of children’s socioeconomic status, race and ethnicity.8 For example, previous studies have demonstrated that immunization coverage levels of kindergarteners (K-4 and K-5) are significantly increased from school entry up to the first 30 days of school.9
To decrease immunization disparities among children and youth less than 14 years of age, the CHIMC “Save Lives-Immunize!” intervention was implemented (Table 1). Targeted geographic areas were occupied predominately by populations of color with the lowest immunization coverage rates for children and youth in the city of Milwaukee. CHIMC began in 2005 as a 3-year planning and pilot phase in two ZIP Codes and segued into an intervention phase from 2008 through 2013 to four ZIP Codes (Table 1). This CHIMC project was designed based on the knowledge exchange between parents/caregivers and academic–community partners. Emphasis was placed on the important role that vaccines play in reducing the incidence of common childhood diseases and an appreciation of what motivates and/or influences parents/caregivers to comply with recommended vaccination schedules.
Table 1.
Demographic of Children by Age Groups in the Community Health Improvement for Milwaukee Children Target Areas Compared to City of Milwaukee, State of Wisconsin and USA (2010)
| Variable | ZIP Code | Milwaukee | WI | US | |||
|---|---|---|---|---|---|---|---|
| 53205 | 53206 | 53208 | 53210 | ||||
| Population | 10,050 | 28,210 | 31,133 | 28,126 | 947,735 | 5,686,986 | 308,745,538 |
| Ages (y) | |||||||
| Overall (0–14) | 2,970 | 7,918 | 7,836 | 7,739 | 196,785 | 1,102,987 | 61,227,213 |
| <5 | 36% | 34% | 37% | 34% | 35% | 32% | 33% |
| 5–9 | 32% | 32% | 32% | 31% | 33% | 34% | 33% |
| 10–14 | 32% | 34% | 31% | 35% | 32% | 34% | 34% |
| African American | 87% | 97% | 54% | 78% | 28% | 7% | 13% |
| Parents/caregivers of children w/high school diploma or less | 76% | 74% | 75% | 52% | 43% | 46% | 46% |
| Parents/caregivers of children unemployed | 23% | 22% | 14% | 11% | 9% | 6% | 7% |
OBJECTIVES
This project was designed to create an infrastructure that allowed the most impacted populations to be fully engaged in all phases of research. This manuscript demonstrates the effectiveness of multidisciplinary, multilayered, and culturally tailored interventions using a CBPR framework10,11 to eliminate disparities in childhood immunization rates.
METHODS
CPBR Approach
The general approach used in this project is commonly referred to as CBPR. Community members, living in or connected to organizations serving the target areas, vetted all messages, data collection tools, and approaches included in this case study. CHIMC is an ongoing partnership of local community organizations, community residents, and academic partners (Figure 1). CHIMC conducted a local community self-assessment adapted from the Coalition Self-Assessment Survey12 using primary and secondary data in the planning phase and agreed to decrease childhood immunization disparities. Memorandums of understanding documented mutually agreed upon roles and responsibilities for primary partners as part of sub-award contracts with the fiscal agent, Medical College of Wisconsin.
Figure 1.
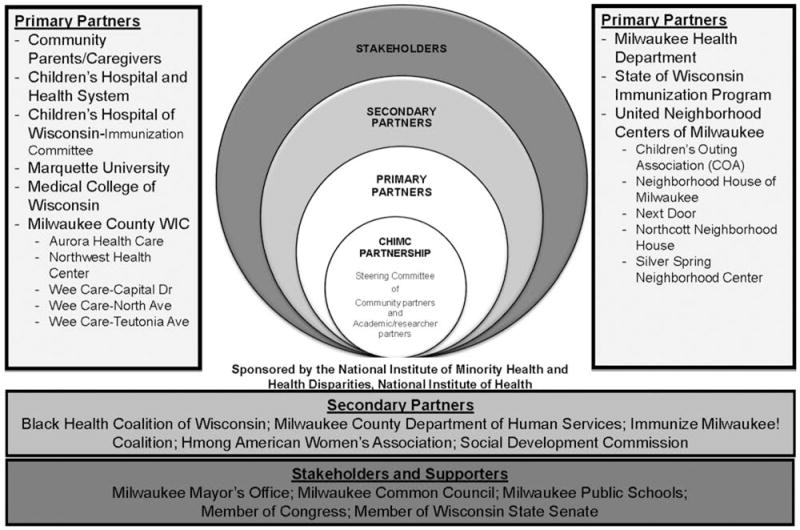
Community Health Improvement for Milwaukee’s Children (CHIMC) Infrastructure, 2005–2016
A 26-partner Steering Committee (SC; 18 community and 8 academic representatives) met 6 times annually to revise the intervention protocols, and make changes to governance and policies for operation of this project that would align with, and support local interventions. The SC approved workgroups activities, strategies, tactics, and interpretation of data. Community residents (self-identified as the Community Forward Team [CFT]), were convened to provide input into all phases of this research initiative. Primary partner agencies employed the majority of the CHIMC staff and the partnership maintained a 2:1 ratio in community to academic representation. Remaining CHIMC members were community agency representatives and academic partners (clinicians, researchers, and staff). Co-learning opportunities were offered at SC meetings to foster community buy-in and engagement in advocacy-related activities. To demonstrate bidirectional learning, community residents assisted academic partners in the understanding of culturally relevant language in relation to immunizations (i.e., using immunizations or vaccines instead of shots).
Community residents involved in the CHIMC project consisted of individuals who lived in or were referred from local organizations (e.g., nonprofit community organizations as family resource centers, child care agencies, or the Milwaukee Police Department) in the targeted areas and/or expressed a strong interest in being involved in CHIMC. To demonstrate respect for their investments and promote sustainability of community voices and expertise, CFTs received an hourly honorarium. In addition, CFTs demonstrated commitment to the project by volunteering unpaid time beyond the hours allotted in the budget.
A total of four CHIMC workgroups were established and co-led by community and academic partners to develop, monitor, and implement CHIMC interventions: 1) Curriculum and Development, 2) Recruitment and Retention, 3) Research, Design, and Intervention, and 4) Evaluation and Dissemination. All members of the CHIMC team were encouraged to join at least two workgroups, but many chose to engage in more than two. Power sharing was established through the selection of community and academic co-chairs for workgroups and the SC. These leaders worked with CHIMC staff to set meeting agendas and present and/or propose recommendations for discussion of research-related concerns to the SC. Final recommendations were revised and ratified by the SC votes at bimonthly meetings to ensure shared decision making and consensus among partners. Consultants with expertise in focus groups, community-based initiatives, and social marketing campaigns were invited to facilitate several retreats. Leaders from community organizations contributed their expertise as in-kind to CHIMC processes; in particular, they advocated that a randomized, controlled trial not be used and emphasized the incorporation of quantitative and qualitative data.
All three phases of CHIMC included a variety of data collection tools as outlined in Figure 2. CHIMC staff collected participants’ immunization data from the Wisconsin Immunization Registry (WIR), a computerized Internet database application that records dates of immunizations for Wisconsin’s children and adults. When available, CHIMC staff collected parents’/caregivers’ immunization records for comparisons with WIR records. CFTs and community agencies have been actively engaged in dissemination of findings to community via local newspapers, radio shows, newsletters, community forums, academic conferences, a chapter in a book, and grand rounds. They have also been strong advocates for voicing the benefits of CHIMC to the local communities and have attended outreach activities along with CHIMC staff to acquire an understanding of community resources that can be shared with participants enrolled in the project.
Figure 2.
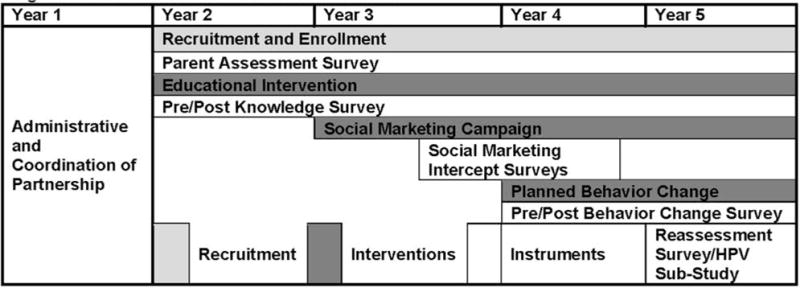
CHIMC–SLI Intervention Phase Schema
Intervention
Enrollment and Baseline Data Collection
CFTs and community partners completed the Collaborative Institutional Training Initiative training and actively engaged CHIMC’s project participants through recruitment and outreach efforts. They referred eligible parents/caregivers to CHIMC staff, assisted with parent workshop series, and represented community issues in project planning. The CHIMC staff recruited and enrolled CHIMC participants, provided additional resources for community participants (e.g., referrals to agencies providing assistance with housing, food access, or health insurance), and assisted in tracking information for the project, such as immunization records.
CHIMC staff and CFTs canvassed the community and attended community-wide events in the targeted areas to recruit participants into this project. A cross-sectional sample of eligible families consisted of those residing in the project’s targeted areas with at least one child 0 to 14 years of age. Parents/caregivers were enrolled following Children’s Hospital of Wisconsin Institutional Review Board approval of the protocol. Enrolled parents/caregivers completed a 110-item survey that consisted of questions addressing demographics, immunization attitudes and beliefs, and psychosocial factors (e.g., perceived racism, neighborhood cohesion, and self-efficacy). CHIMC staff was trained and gained access to the WIR registry to assess if participants were UTD, late up-to-date, or behind on their immunizations.
Intervention 1: Educational Intervention
After consenting and completing the 110-item survey, CHIMC staff administered pre-knowledge surveys to participants followed by administration of an educational presentation on immunizations according to their preferences (e.g., individual vs. group settings, location, and time). After this, a post-knowledge survey was used to evaluate the value of the educational intervention. Survey data was collected via paper survey forms that were scanned and stored in Remark software. Quarterly, immunization records were obtained from the WIR and entered into CoCASA, a community tracking database. Data were exported to SPSS (Version 20) for analysis. A two-step cluster analysis was used as an exploratory tool to reveal natural groupings of participants in clusters for attitudes and beliefs about immunizations. Gust categorization included parents/caregivers paired with the youngest child in the family, using the sample from October 2011 (n = 465), to categorize parents/caregivers into such groups as Health Advocates/Immunization Advocates (HA/HI), Fence Sitters (FS), Go-Along-to-Get-Along (GATGA), and Skeptics.13 A nonparametric Mann–Whitney test was used to compare the two groups and the Kruskal–Wallis test was used to compare multiple groups. The McNemar and Fisher exact tests were conducted on the pre/post-knowledge dichotomized questions and immunization rates. No adjustment was made for multiple testing. A p < 0.05 was reported as statistically significant.
Intervention 2: Social Marketing Campaign
During the Social Marketing Campaign (SMC), responses from the parent questionnaire defined the marketing mix (product, place, price, and promotion) and were used to develop social marketing strategies, messages, and materials. This was accomplished via the following steps: 1) collaborated with partners to develop images and concepts, 2) developed focus group processes, 3) recruited and enrolled residents, 4) conducted focus groups, 5) analyzed focus group results, and 6) created the final message. These steps resulted in a number of potential SMC messages that were identified for testing in the community and can be reviewed in Table 2.
Table 2.
Optional Immunization Messages for Community Health Improvement for Milwaukee Children Social Marketing Campaign
| 1. Two out of 3 children in Milwaukee are not fully immunized. Could your child be one of them? |
| 2. Parenting is a juggling act! You don’t want to drop the ball on immunizations. |
| 3. Take Control! Check your child’s immunization records. |
| 4. Think your child has all his shots? Be Sure! |
| 5. Protect your child’s health. Immunize! |
| 6. Get your child immunized on time. Every time! |
| 7. Have you talked to your doctor about your child’s immunizations? |
Convenience samples of 15 community residents were selected from the existing CHIMC enrollees to assess SMC messages and suggested materials. A social marketing consultant, with support of CHIMC staff and CFTs, conducted two focus group discussions. Feedback from the focus groups was analyzed by the local consultant and shared as social marketing strategies and messages. Based upon feedback from the focus groups and analysis by the consultant, the final message was “Take Control! Protect Your Child with Immunizations” accompanied with a photo of a young mother, baby, and health professional.
After receiving input on SMC message in partnership with the Children’s Community Health Plan of Children’s Hospital and Health System, the CHIMC implemented its SMC message in conjunction with the ongoing educational intervention. SMC messages were disseminated throughout the targeted areas using billboards, posters on buses, and in doctor’s offices. In addition, CHIMC staff and CFTs distributed brochures, pens, pencils, bags, t-shirts and magnets at outreach events as mobile billboards. To test the penetration of the SMC, two rounds of intercept survey data was collected from individuals recruited from bus stops and outside community locations.14 Final datasets were exported into SPSS (version 20) for analysis. A nonparametric Mann–Whitney and Fisher exact test were used to compare pre and post results. A paired analysis could not be done because the responses at each meeting were anonymous. No adjustment was made for multiple testing. A p < 0.05 was reported as statistically significant.
Intervention 3: PBC
The PBC intervention was guided by strategies that emphasize learning from observation, experience, reinforcement, mastery, and communication within social contexts.15 Goals for the PBC, as established by CHIMC Research, Design, and Intervention and Evaluation and Dissemination workgroups, included 1) identifying barriers that prevent parents/caregivers from keeping their children’s UTD immunization status, 2) exploring and addressing the discrepancy between parents/caregivers’ perceptions versus actual immunization status of their child, 3) teaching parents/caregivers how to access children’s immunization records through existing resources such as WIR, and 4) modeling, rehearsing, and reinforcing effective health care navigating behaviors, such as self-advocacy, negotiating health systems and social service agencies, and leveraging support from significant others to increase self-efficacy in monitoring and maintaining their children’s UTD immunization status. Content for PBC sessions is summarized in Table 3.
Table 3.
Community Health Improvement for Milwaukee Children Planned Behavior Change Sessions Content
| 1. Orientation (introductions, relationship building, intervention overview, pre-survey) |
| 2. Health Care System Navigation (barriers to UTD immunizations, personal stories of health care experiences, brainstorming strategies for addressing health care barriers) |
| 3. Communicating with Health Care Providers (overview of communication, barriers for effective communication and strategies for improved communication) |
| 4. Accessing Immunization Records through the WIR (describe WIR, how to interpret records, and how to access records online) |
| 5. Social Networking (overview of social support, understanding social support systems, how to build social support systems) |
| 6. Action Planning for Immunization Compliance (overview of setting specific, measurable, attainable, realistic and timely goals, setting individual goals) |
| Next Steps and Wrap-Up |
| Review of barriers and strategies to overcome barriers, review key concepts, post-intervention survey |
Abbreviations: UTD, up-to-date; WIR, Wisconsin Immunization Registry.
Enrolled CHIMC participants were invited to participate in 7 weekly, 90-minute PBC sessions if they had at least one child who was less than 5 years old. Sessions entailed discussion and skills practice between facilitators (CHIMC staff and CFTs) and participants (parents/caregivers enrolled in CHIMC). Full participation in the intervention was defined as completion of pre and post surveys and participation in four of the five middle sessions as these sessions contained the majority of the intervention content. Sixty-four parents/caregivers consented to participate in a total of seven cohorts and 35 participants completed the PBC intervention (attended at least four of five required sessions).
Parents’/caregivers’ perceptions of barriers and/or facilitators were discussed in all sessions and recorded by CHIMC staff. At the beginning of each session, parents/caregivers identified the barriers that prevented them from keeping their child(ren)’s immunizations UTD. At the end of each session, parents/caregivers identified facilitators that advanced their child(ren)’s immunizations UTD status. Five cohorts with a total of 48 parents/caregivers were assessed to identify changes in their perceptions of barriers and facilitators in each session based on transcribed notes from each session to assess changes.
In an effort to reduce barriers (e.g., time commitment of multiple sessions, transportation, childcare) to participation in all sessions, childcare was provided. In addition, participants were compensated for their time, transportation (e.g., rides or bus passes) was available as needed, and light meals were served for participants and children. CFTs agreed to provide childcare support for these sessions. Reported barriers and/or facilitators to getting children immunized were recorded for each session and were transcribed into Diction 6.0 text analysis software (2012) for latent analysis to compare the general understanding (tone) of all identified barriers and/or facilitators. Notes were documented and transcribed by three CHIMC staff members. A member of the CHIMC team with qualitative research expertise conducted coding of barrier/facilitator variables. Quotations contained personal and situational attributions to explain the barriers and facilitators of their child(ren)’s immunization status. A word frequency count identified words about barriers and/or facilitators that occurred two or more times. Word frequencies of one or fewer occurrences were eliminated from this count. An open reading of quotations that could not be coded with the initial codes resulted in the development of additional codes. Resulting codes were merged into groups based on similarities in content. Information gathered from this intervention was analyzed and compiled after workshops to be included as a component of future web-based toolkit, available on the CHIMC website at www.chimcmke.org.
RESULTS
Baseline Assessment: Demographics
CHIMC team enrolled and surveyed 565 parents/caregivers with 1,533 children. Parent/caregiver participants were predominantly female (89.4%), African American (91.4%), unemployed (63.5%), residing in single-headed households (70.5%), and had a mother/child relationship to the child participants (78.3%). Median age of parents/caregivers in CHIMC-Save Lives-Immunize! was 30 years (range, 17–72). Median age of their children was 6.18 years, ranging from birth to 15 years, distributed as follows: 12.9% were 0 to 18 months; 12.3% were 19 to 35 months; 8.3% were 36 to 48 months; 12.9% were 4 to 6 years; 26.1% were 7 to 10 years; and 18.5% were 11 to 14 years.
Years that families resided within the targeted areas were less than 1 year, 31.9%; 1 to 5 years, 37.1%; and more than 5 years, 29.7%. Only 11% were college graduates. Primarily mothers (82.3%) made the immunization decisions within each household. Parents/caregivers reported that the medical provider or public health official (90.8%) was a very important source of immunization information; parents/friends (63.1%) and school nurses or officials (66.4%) followed. For children enrolled in the project, 98% had documented immunizations within the WIR. CHIMC project’s overall retention rates were high (80%).
Intervention 1: Educational Intervention
Gust categories were used to quantify attitudes and beliefs about immunizations ranging from 1 (strongly disagree) to 5 (strongly agree). Four groups were identified using the two-step cluster analysis, distributed as follows: 45% GATGA, 42% HA/IA, 11% FS, and 2% Skeptics. Among these groups, self-efficacy was significantly different (p ≤ 0.001). HA/IA had a median of 4.2 (range, 1.1–5), the FS had a median of 3.9 (range, 1.6–5); and the GATGA had a median of 3.9 (range, 1.3–5.0). HA/IA exhibited higher self-efficacy than other groups. Perception of racism was statistically different among the four groups (p ≤ 0.001). HA/IA had a median of 2.0 (range, 1–5), the FS had a median of 3 (range, 1–4.4), and the GATGA had a median of 2 (range, 1–5). FS perceived more racism than the HA/IA and the GATGA. Although the research team was able to categorize participants into these groups and determine differences among psychosocial factors, this information was not related to UTD immunization status.
Pre/post knowledge assessments revealed a significant increase in knowledge as illustrated by variables documented in Table 4. As of August 2012, children whose parents/caregivers completed the educational program, demonstrated in Figure 3, demonstrated significantly higher actual WIR UTD immunization status (p < 0.05) from baseline. Consistently, parents/caregivers perceived their child(ren) to have a higher immunization status than the actual immunization status documented in WIR. Further analysis revealed that there is a significant difference between baseline data and age-specific Healthy People 2020 goals (Table 5). However, the difference between parents’/caregivers’ perceptions and Healthy People 2020 goals are not different. Therefore, parents/caregivers may not seek immunizations believing that their children are UTD. Among children whose parents completed the education section, the 0- to 18-month group had significantly higher UTD immunization status than baseline (p = 0.048). Children 4 years of age or younger had the greatest disparities from the Healthy People 2020 goals and from parents’/caregivers’ perceptions of immunization status.
Table 4.
Community Health Improvement for Milwaukee Children’s Parents/Caregivers Pre/Post Immunization Knowledge Results
| Immunization Knowledge (N = 447) | Pre % Correct | Post % Correct | p Value |
|---|---|---|---|
| Vaccines decrease your body’s ability to fight disease. | 53 | 60 | 0.016 |
| Current research shows that vaccines cause certain illnesses like cancer, autism, meningitis, and deafness. | 48 | 79 | ≤0.001 |
| If most people get their shots, others who have not been vaccinated will be protected. | 21 | 68 | ≤0.001 |
| Getting vaccinated against measles will not give you that disease. | 52 | 74 | ≤0.001 |
| Common reactions to vaccines are seizures and high fever (>105°F). | 37 | 55 | ≤0.001 |
| Vaccines against genital warts (HPV) and yellow jaundice (hepatitis B) protect against different types of cancer | 24 | 56 | ≤0.001 |
| Flu (influenza) vaccine is not recommended for children. | 71 | 88 | ≤0.001 |
| Te WIR provides secure access to your child’s immunization records. | 71 | 96 | ≤0.001 |
| How Each Disease is Spread | |||
| Chicken Pox by coughing/sneezing | 26 | 61 | ≤0.001 |
| Lockjaw (tetanus) by cuts and tears in the skin | 19 | 35 | ≤0.001 |
| Yellow jaundice (hepatitis B) by blood and sexual contact | 37 | 45 | 0.008 |
| Measles by coughing and sneezing | 24 | 47 | ≤0.001 |
| Genital warts (HPV) by sexual contact | 64 | 74 | ≤0.001 |
| Whooping cough (pertussis) by coughing and sneezing | 79 | 87 | ≤0.001 |
Abbreviations: HPV, human papilloma virus; WIR, Wisconsin Immunization Registry.
Figure 3.
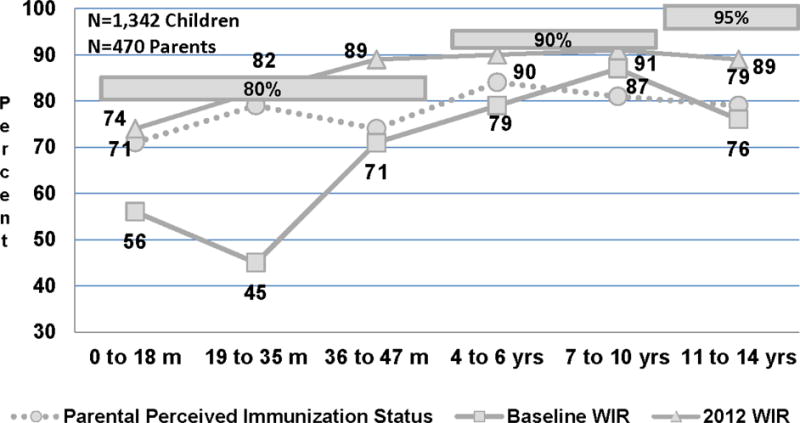
Comparisons of Enrolled Children’s UTD Immunization Status Post-CHIMC’s Educational Interventions to Parents’/Caregivers/Perceptions, Baseline WIR-Verified Rates, and Healthy People 2020 Goals by Age Group
Note. Shaded areas are Helthy People 2020 Goals.
Table 5.
Comparisons of Children Up-to-date Immunization Status to Baseline Levels, Parents’/Caregivers’ Perceptions, and Healthy People 2020 Goals by Age Group for the Youngest Child in Households
| Age | n | 2020 Goal | Baseline at Enrollment | p Value | Parents’/Caregivers’ Perceptions of UTD Immunization Status at Enrollment | p Value | Actual Rate (August 2012) | p Value |
|---|---|---|---|---|---|---|---|---|
| 0–18 months | 159 | 80% | 54% | <0.001 | 76% | 0.046 | 64% | <0.001 |
| 19–35 months | 92 | 80% | 41% | <0.001 | 86% | 0.001 | 76% | 0.433 |
| 36–47 months | 43 | 80% | 72% | <0.001 | 81% | 0.650 | 88% | 0.323 |
| 4–6 years | 74 | 95% | 82% | <0.001 | 85% | <0.001 | 88% | 0.043 |
| 7–10 years | 70 | 95% | 81% | <0.001 | 83% | <0.001 | 89% | 0.081 |
| 11–14 years | 25 | 90% | 72% | <0.001 | 75% | <0.001 | 86% | 0.760 |
p Values demonstrate statistical significance between the column immediately to the left and the Healthy People 2020 goals.
Nine parental/caregiver factors (e.g., transportation accessibility, high self-efficacy) were significantly associated with positively influencing parents’/caregivers’ perception of children’s immunization status and four protective factors (e.g., safety of vaccines, helpful staff at healthcare provider office) for documented immunization status (WIR verified) were identified (Table 6). Comparisons were made between the 2012 UTD status and the U.S. Centers for Disease Control and Prevention reporting baseline status. One of the questions considered very significant was: “All childhood vaccinations that are recommended by my child’s regular doctor are safe.” Of those children who were UTD, 22% of the parents/caregivers disagreed that vaccines were safe as recommended by their doctor, whereas for children who were behind, 33% of the parents/caregivers disagreed that vaccines were safe as recommended by their doctor (p = 0.007). Three other factors related to psychosocial factors were identified as self-efficacy, ease of access to doctor’s office, and friendliness of clinical staff (p < 0.05).
Table 6.
Odds Ratios for Factors Influencing Parents’/Caregivers’ Perceptions of Children’s UTD Immunization Status and Actual UTD Status
| Parental/Caregiver Response | OR | 95% CI | p Value* |
|---|---|---|---|
| Perceived Immunization Status | |||
| Intention to immunize | 9.24 | 3.07–28.90 | ≤0.0001 |
| Youngest child visited doctor in past 12 months | 7.66 | 2.23–26.36 | 0.003 |
| Transportation accessibility | 5.70 | 2.94–11.08 | ≤0.0001 |
| Personal healthcare provider for routine care | 4.11 | 1.58–10.64 | 0.007 |
| Healthcare provider source of good health information | 3.96 | 1.96–8.00 | ≤0.0001 |
| Healthcare provider explanations are understandable | 3.68 | 1.68–8.03 | 0.002 |
| High self-efficacy | 3.16 | 1.58–6.30 | 0.002 |
| High coping abilities | 3.08 | 1.61–5.89 | 0.001 |
| Good relationship with healthcare provider | 2.68 | 1.33–5.38 | 0.009 |
| Actual Immunization Status | |||
| Agree or strongly agree that all childhood vaccinations that are recommended by my child’s regular doctor are safe. | 1.16* | 1.46–1.31 | 0.007 |
| Agee or strongly agree that it is easy for me to get to the clinic/doctor’s office to have my child vaccinated. | 1.11 | 1.01–1.22 | 0.02 |
| Agee or strongly agree that it is easy for me to stick to my aims and accomplish my goals. | 1.10 | 1.00–1.21 | 0.03 |
| Often or very often in the last 12 months, how often were clerks and receptionists at your child(ren)’s doctor as helpful as your through they should be. | 1.14 | 1.01–1.29 | 0.03 |
All items are statistically significant with p ≤ 0.010 (owing to multiple comparisons).
Intervention 2: Social Marketing Campaign
A total of 408 respondents participated in the CHIMC Intercept Survey. Without visual prompting, 51% of this group (n = 408) recalled a health message about children, but only 5 (2%) of these participants recalled CHIMC’s Take Control message. However, when given the visual prompting, 84.5% respondents (n = 290) recalled CHIMC SMC messages in the past 3 months the CHIMC Take Control! message.14 Furthermore, survey respondents identified the location of the message as buses (35%), billboards (15%), TV/newspapers (15%), children’s hospital sites (10%), and doctor’s offices (10%). Among respondents who reported that immunizations were important for children (96%), approximately 97% indicated that they were likely to immunize their children.
Intervention 3: PBC
Results from the qualitative analysis of the PBC sessions revealed that the most frequently mentioned barriers were hospital personnel (e.g., doctor’s attitude, medical terminology) and resources (e.g., problems with insurance, getting time off work, not having transportation). The most frequently mentioned facilitative factors were parents (e.g., speaking up, keeping records, switching doctors to get a good fit, getting kids ready for office visit the night before), resources (bring someone to support, free clinics, reliable transportation service), and hospital personnel (e.g., good relationship with provider, early morning appointments, reminder calls).
DISCUSSION
Immunization coverage (UTD) status at baseline for CHIMC participants was significantly lower than the recommended Healthy People 2020 goals, confirming the need for culturally tailored and population-specific interventions. At the most recent follow-up, statistical tests indicated that there were no longer differences between CHIMC participants and the Healthy People 2020 Goals, except in children ages of 0 to 18 months lagged behind the older age groups. Using multilayered interventions (educational, social marketing campaign and PBC models), the CHIMC project successfully increased the proportion of children with UTD immunization status. However, among children whose parents completed the education section, the 0- to 18-months age group had significantly higher UTD immunization status than baseline. Parents’/caregivers’ perceptions of immunization for preschoolers were inconsistent with baseline immunization status at the time of enrollment. It is possible that the older age groups receive more immunization support owing to state immunization laws and immunization enforcement upon annual enrollment into schools or daycare settings. Therefore, improving the immunization rates for this 0- to 18-months age group requires awareness and removal of barriers (parental education about the safety and efficacy of immunizations, transportation, and health care providers cultural sensitive engagement). This reinforces the notion that culturally tailored programmatic support is necessary to overcome healthcare systems barriers.3,16,17 This support may be extensive educational outreach and dissemination of immunization information, or it may come in the form of enrollment requirements via daycare and school environments.
The most significant parental/caregiver factor influencing UTD status was the perception that vaccines recommended by doctors are safe. This highlights the importance of trust between health care professionals and parents/caregivers as a way to facilitate acceptance of the idea that vaccinations are essential. Positive interactions with health care professionals were also more likely to result in higher immunization rates. Other suggestive factors were self-efficacy and access to healthcare clinics/offices. Lack of these factors (low access, poor doctor–patient relationship, etc.) were identified as barriers. Lack of resources, such as transportation, was an additional barrier to be considered by insurers and health care professionals.
This project was designed and positioned to overcome many of these barriers and to promote trust in preventive primary care based on a participatory approach with community residents. Educational sessions served to improve self-efficacy, which is expected to result in higher immunization compliance. Understanding the importance of immunizations, as promoted in the CHIMC educational sessions, was associated with higher UTD immunization status.
LIMITATIONS
There are a number of potential limitations with this project. The use of non-probability sampling may have skewed findings, because those who volunteered may be different than the general population. However, as discussed, it was important to the community partners that randomized controlled trials not be used in this project. Community partners raised ethical concerns about withholding interventions to any potential participants based on the fact that they would be randomized to a non-intervention group. Additionally, the use of the Gust questionnaire did not predict immunization UTD or behind status. In other words, the cluster analysis did not demonstrate predictability between Gust’s categorizations or attitudes and beliefs about immunizations versus actual immunization status as documented in WIR and parents’/caregivers’ records. Further studies on how to correlate parents’/caregivers’ attitudes and beliefs as it relates to immunization status may be warranted, especially for high-risk populations.
NEXT STEPS/SUSTAINABILITY
CHIMC will continue to focus on the development of interactive information about immunizations using technology in community-based locations to ensure broader dissemination. Immunization information can be provided on a broader scale by using a web-based platform. These resources will be organized into a CHIMC toolkit and will be available on www.chimcmke.org. Evaluation of this web-based Toolkit, inclusive of a custom-designed eLearning Café, will be established to provide sustainability of immunization and be accessible via mobile smart phones to promote knowledge exchange beyond the grant-funded period. A dissemination plan has been proposed as the next phase of this CBPR approach. Furthermore, it is noteworthy that the Milwaukee community immunization rates also increased beyond the baseline reported in 2005 likely owing in part to collective community efforts with CHIMC partners. This has culminated into the establishment of a local coalition titled: IMMUNIZE MILWAUKEE COALITION. CHIMC team continues to actively collaborate with this Coalition and share findings.
CONCLUSIONS
By partnering with community organizations and using a CBPR approach, CHIMC successfully promoted factors that led to higher immunization rates among targeted populations. The ability of this project to elevate immunization awareness and increase access to the WIR for parents/caregivers was enhanced by the CBPR approach. Culturally tailored social marketing messages designed in partnership with lower socioeconomic populations can be quite effective. Initiatives such as CHIMC can successfully decrease childhood immunization rate disparities by reaching larger targeted audiences and could be adapted for other public health conditions and challenges.
Although protective factors are suggestive of positive relationships with UTD immunization status in children, these factors require focused promotion to eliminate disparities among vulnerable populations. Enrollment in CHIMC encouraged these protective factors and contributed to UTD immunization status. Analysis of protective factors associated with perceived and actual UTD (WIR-verified) status suggests that these improvements may be multifactorial. These factors could include increased promotion of the importance of immunizations, heightened parents’/caregivers’ self-efficacy through knowledge exchange, increased advocacy and navigation of the health care systems. The CBPR approach could be utilized to address other immunization challenges, such as lower coverage of human papilloma virus vaccines.
Acknowledgments
The authors acknowledge the following for their contributions to the work described in this manuscript: Sumaiyah Clark, Cathy Edwards, Jo Ann Gray-Murray, Tiffanie Henderson, Sheri Johnson, Carol Keintz, Mary Ann Kiepczynski, Meggan Leary, Norma Magallanes, John Meurer, Emmanuel Ngui, Katie Swank Watt, Ann White, Kevin Glatt, members of the CFT, and parents and caregivers who shared their information as participants in the research. Research reported in this publication was supported by the National Institute On Minority Health And Health Disparities of the National Institutes of Health under Award Number R24MD001812. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Szilagyi PG, Bordley C, Vann JC, Chelminski A, Kraus RM, Margolis PA, et al. Effect of patient reminder/recall interventions on immunization rates: A review. JAMA. 2000 Oct;284(14):1820–7. doi: 10.1001/jama.284.14.1820. [DOI] [PubMed] [Google Scholar]
- 2.Bardenheier BH, Yusuf HR, Rosenthal J, Santoli JM, Shefer AM, Rickert DL, et al. Factors associated with underimmunization at 3 months of age in four medically underserved areas. Public Health Rep. 2004 Oct;119(5):479–85. doi: 10.1016/j.phr.2004.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosenthal J, Rodewald L, McCauley M, Berman S, Irigoyen M, Sawyer M, et al. Immunization coverage levels among 19- to 35-month-old children in 4 diverse, medically underserved areas of the United States. Pediatrics. 2004 Apr;113(4):e296–302. doi: 10.1542/peds.113.4.e296. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Department of Health and Human Services [Internet] Topics and Objectives. [updated 2014 Jul 7; cited 2013 Jun 18]. Available from: http://www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=23.
- 5.Walker AT, Smith PJ, Kolasa MK. Reduction of Racial/Ethnic Disparities in Vaccination Coverage, 1995–2011. MMWR Morb Mortal Wkly Rep. 2014 Apr;63(01):7–12. [PubMed] [Google Scholar]
- 6.Brown KF, Kroll JS, Hudson MJ, Ramsay M, Green J, Long SJ, et al. Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine. 2010;28:4235–4248. doi: 10.1016/j.vaccine.2010.04.052. [DOI] [PubMed] [Google Scholar]
- 7.Lau A, Sintchenko V, Crimmins J, Magrabi F, Gallego B, Coiera E. Protocol for a randomised controlled trial examining the impact of a web-based personally controlled health management system on the uptake of influenza vaccination rates. BMC Health Serv Res. 2012 Apr;12(1):86. doi: 10.1186/1472-6963-12-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Orenstein WA, Hinman AR. The immunization system in the United States: The role of school immunization laws. Vaccine. 1999;17:S19–S24. doi: 10.1016/s0264-410x(99)00290-x. [DOI] [PubMed] [Google Scholar]
- 9.Lawlor EM. Kindergarten immunization coverage survey school year 2012–13. Kansas Health Department of Health and Environment; 2013. [Internet] [cited 2015 Jan 9]. Available from: http://www.kdheks.gov/immunize/download/Kindergarten_2012–13.pdf. [Google Scholar]
- 10.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 11.Israel BA, Eng E, Schulz AJ, Parker EA. Introduction to methods for CBPR for health. In: Israel BA, Eng E, Schulz AJ, Parker EA, editors. Methods for community-based participatory research for health. 2nd. San Francisco: Jossey-Bass; 2013. pp. 4–42. [Google Scholar]
- 12.Kennedy E, Sofaer S. Coalition self-assessment survey Allies Against Asthma. University of Michigan; Ann Arbor: Available from: http://www.policyarchive.org/handle/10207/21651. [Google Scholar]
- 13.Gust D, Brown C, Sheedy K, Hibbs B, Weaver D, Nowak G. Immunization Attitudes and Beliefs Among Parents: Beyond a Dichotomous Perspective. Am J Health Behav. 2005;29(1):81–92. doi: 10.5993/ajhb.29.1.7. [DOI] [PubMed] [Google Scholar]
- 14.Ngui EM, Ha Census milton C, Nugent M, Simpson P, Willis E. The effect of a social marketing campaign to increase awareness of immunization for urban low-income children. Wisc Med J. 2014;114(10):10–5. [PMC free article] [PubMed] [Google Scholar]
- 15.Montaño DE, Kasprzyk D. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model. In: Glanz K, Rimer BK, Viswanath K, editors. Health behavior and health education: theory research and practice. 4th. San Francisco: John Wiley & Sons, Inc; 2008. pp. 67–92. [Google Scholar]
- 16.Merrill R, Kelley T, Cox E, Layman AB, Layton BJ, Lindsay R. Factors and barriers influencing influenza vaccination among students at Brigham Young University. Med Sci Monit. 2010 Feb;16(2):PH29–34. [PubMed] [Google Scholar]
- 17.Dixon-Woods M, Brown H, Arthur A, Matthews R, Jagger C. Organising services for influenza vaccination for older people. J Health Serv Res Policy. 2004 Apr;9(2):85–90. doi: 10.1258/135581904322987490. [DOI] [PubMed] [Google Scholar]


