Abstract
Background
The management of meniscus tears identified at the time of primary ACL reconstruction is highly variable and includes repair, meniscectomy, and non-treatment.
Hypothesis/Purpose
The purpose of this study is to determine the reoperation rate for meniscus tears left untreated at the time of ACL reconstruction with minimum follow-up of 6 years. We hypothesize that small, peripheral tears identified at the time of ACL reconstruction managed with “no treatment” will have successful clinical outcomes.
Study Design
Retrospective study of a prospective cohort; Level of Evidence, 3
Methods
Patients with meniscus tears left untreated at the time of primary ACL reconstruction were identified from a multicenter study group with minimum 6-year follow-up. Patient, tear, and reoperation data were obtained for analysis. Need for reoperation was used as the primary endpoint, with analysis performed to determine patient and tear characteristics associated with reoperation.
Results
There were 194 patients with 208 meniscus tears (71 medial; 137 lateral) left in situ without treatment with complete follow-up for analysis. Of these, 97.8% of lateral and 94.4% of medial untreated tears required no reoperation. Sixteen tears (7.7%) left in situ without treatment underwent subsequent reoperation: 9 tears (4.3%) underwent reoperation in the setting of revision ACL reconstruction and 7 tears (3.4%) underwent reoperation for isolated meniscus pathology. Patient age was significantly lower in patients requiring reoperation, while tears measuring ≥ 10 mm more frequently required reoperation.
Conclusions
Lateral and medial meniscus tears left in situ at the time of ACL reconstruction did not require reoperation at minimum 6-year follow-up for 97.8% and 94.4% of tears, respectively. These findings reemphasize the low reoperation rate following non-treatment of small, peripheral lateral meniscus tears while noting less predictable results for medial meniscus tears left without treatment.
Key Terms: meniscus, anterior cruciate ligament (ACL) reconstruction, non-treatment, in situ
Introduction
Acute anterior cruciate ligament (ACL) tears are frequently accompanied by meniscal injury.5, 18, 30 The management of these associated meniscal lesions varies substantially and includes meniscal repair, partial meniscectomy, as well as leaving tears in situ without treatment at the time of ACL reconstruction. The knowledge of the anatomy and blood supply of the meniscus, as well as the location, length, tear type, and inherent stability of the tear, often guide management of meniscal lesions identified at the time of arthroscopy.2, 9, 23, 28
The meniscus plays an important role in load transmission and contact stress in the knee.3 The goals of meniscal treatment at the time of ACL reconstruction are to create a favorable environment for knee stability while preventing subsequent articular cartilage damage. Due to this fact, as well as the clinical and radiographic deterioration of knees over time following partial meniscectomy,6, 11, 13 meniscal preservation is favored when possible. Therefore, determining which tears are amenable to nonoperative management, meniscectomy, or repair is essential for successful outcomes in patients who undergo ACL reconstruction with concomitant meniscal tears noted at the time of surgery.
Previous studies suggest that certain meniscal tears left in situ without treatment at the time of ACL reconstruction produce consistently positive clinical results.4, 7, 9, 12, 20, 23, 26, 28, 34, 37 However, clinical outcomes vary depending on meniscal tear characteristics. Classically, meniscal tear “failures” are defined by subsequent reoperation. A systematic review revealed that lateral meniscal tears left in situ without treatment undergo subsequent reoperation in 4-22% of cases while medial meniscal tears undergo subsequent reoperation in 10-66% of cases.21 Additionally, tear length and the location of the tear within the meniscus itself have been shown to influence outcomes as measured by clinical outcome scores and subsequent reoperation.23, 26, 28 Several authors have suggested that longitudinal, peripheral one-third tears of the lateral meniscus measuring less than 10 mm in length can be left untreated at the time of ACL reconstruction with a predictably low reoperation rate.9, 20, 22, 23, 34 Interestingly, lateral meniscal tears left in situ at the time of ACL reconstruction have been identified as a positive prognostic indicator,7 while outcomes of medial meniscal tears left in situ without treatment are less predictable, particularly when measuring greater than 10 mm in length.20, 24, 26, 37
To date, there have been few studies to prospectively report the outcome of meniscal tears left in situ without treatment at the time of ACL reconstruction. The primary purpose of this study is to determine the rate of subsequent reoperation of meniscal tears left in situ without treatment at the time of ACL reconstruction with a minimum 6-year follow-up utilizing a previously established, prospectively collected and longitudinally followed, multicenter cohort. As a secondary aim, we describe patient and tear characteristics that led to leaving tears in situ without treatment at the time of primary ACL reconstruction using the same cohort. We hypothesize that small peripheral tears in the meniscus identified at the time of ACL reconstruction managed with “no treatment” will have successful outcomes while also requiring less frequent reoperation.
Material and Methods
Data Sources
Data on ACL reconstructions was prospectively collected at 7 centers (University of Iowa, Washington University in St. Louis, Vanderbilt University, Cleveland Clinic, The Ohio State University, University of Colorado, and Hospital for Special Surgery) between January 1, 2002 and December 31, 2004. The initial cohort included all patients who underwent unilateral primary or revision ACL reconstruction. Institutional review board (IRB) approval was obtained from all centers prior to enrollment and informed consent was obtained from all participants included in this study. Funding for the project was provided by the National Institutes of Health. The general methodology of the cohort has been described previously.27, 36 Briefly, each patient completed a 13-page questionnaire including patient demographics, health status, comorbidities, injury characteristics, prior surgeries, and sports participation at the time of enrollment as well as 6-year follow-up.
At the time of the index procedure, surgeons completed a 49-page questionnaire detailing examinations under anesthesia, descriptions of meniscal injuries, and surgical techniques. Upon completion, all patient and surgeon questionnaires were sent to the data coordinating center (Vanderbilt University) where the information was scanned using Teleform software (Cardiff Software Inc, Vista, California, USA) and exported to an electronic database.
Study Design
The database was queried to specifically identify patients who underwent unilateral, primary ACL reconstructions with meniscal tears identified at the time of surgery and left in situ without treatment between January 1, 2002 and December 31, 2004 using the previously described cohort. Treatment decisions at the time of surgery were made by the 12 participating surgeons included in the multicenter study and no specific treatment algorithms or guidelines for meniscal tears were provided. Previous research using this cohort has indicated that surgeons consistently agree upon descriptive tear characteristics and treatment choice when independently evaluating meniscal tears.8 Exclusion criteria for this study included patients undergoing simultaneous bilateral ACL reconstructions, revision ACL reconstructions, multi-ligament injuries requiring operation at the time of ACL reconstruction. For the primary aim, patients with tears left in situ without treatment in the same compartment as a tear treated with excision and/or repair, and patients with incomplete 6-year follow-up data (Figure 1) were also excluded. Patient demographic variables and comorbidities were obtained in addition to meniscal tear characteristics (compartment involvement, length, type of tear) and information regarding subsequent surgery. Patients with meniscal contusions without tears and those treated with abrasion and/or trephination were excluded. For the secondary aim, all tears were considered for analysis, regardless of other treatment in the same compartment or follow-up status in order to determine tear characteristics that led to the decision to leave a tear in situ without treatment.
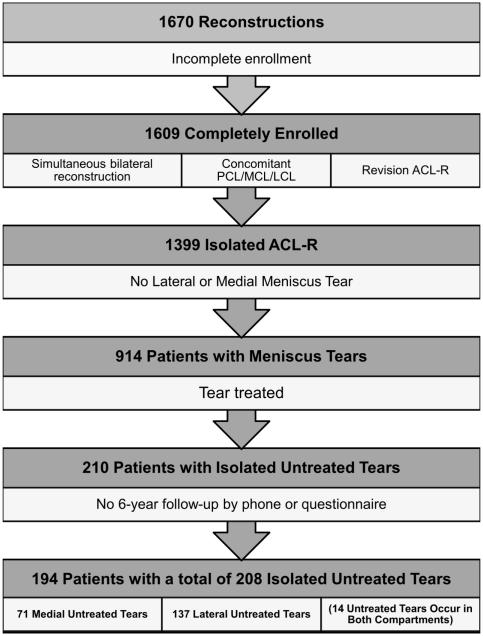
Figure 1.
Flow diagram of meniscus tears identified at the time of primary ACL reconstruction. Inclusion and exclusion criteria yield cohort of patients with untreated meniscus tears with minimum 6-year follow-up.
Statistical Analysis
Demographic variables (including patient sex, age, smoking status, body mass index (BMI), ethnicity) and meniscal tear characteristics (including compartment(s) involved, partial versus complete tears, anterior-posterior location, coronal location, tear type, tear length, and degenerative tear status) were compared between patients who did and did not undergo reoperation for meniscal pathology within the same compartment. Based on previous literature9, 21, 22, 23, tears were stratified by medial or lateral compartment involvement throughout the analysis. Reoperation for meniscal pathology was defined as any subsequent meniscal repair or meniscectomy within the same compartment, medial or lateral, as the meniscal tear left in situ without treatment at the time of the index ACL reconstruction. For patients with meniscal tears left in situ without treatment in both the medial and lateral compartments at the time of the index ACL reconstruction, any subsequent meniscal repair or meniscectomy was considered a reoperation for meniscal pathology regardless of the compartment(s) involved. Reoperation for meniscal pathology was further categorized into any reoperation, including meniscal reoperations with concomitant revision ACL reconstruction, as well as reoperation for isolated meniscal pathology, which excluded meniscal reoperations in the setting of concomitant revision ACL reconstructions. Univariate analysis, including chi-square testing for categorical variables and Student’s t-test for continuous variables, was performed to compare the two cohorts. Fisher’s exact test was used in place of chi-square testing when categorical counts were < 5. This portion of the statistical analysis was performed using IBM SPSS version 21.0 (IBM Corporation, Armonk, New York, USA).
As a secondary aim, we utilized the entire dataset in order to better understand what predicted treatment, including cases of meniscal excision and/or repair, or no treatment for meniscus tears identified at the time of primary ACL reconstruction. Nomograms were created using patient and tear characteristics to help predict subsequent treatment. Medial and lateral tears were separated for the purpose of this analysis, and unlike previous analyses, tears left in situ without treatment that existed within the same compartment as treated tears were included for analysis. A proportional odds model was created for lateral and medial meniscus tears separately in order to determine the likelihood that tears were left in situ without treatment given several patient and tear characteristics. Patient and tear characteristics incorporated in the models included patient age and BMI as well as tear length, partial versus complete tears, tear type (longitudinal; bucket handle; complex; horizontal; oblique; radial), and tear location (peripheral third; central/middle third). This portion of the statistical analysis was performed with R version 3.1.1 (R Foundation for Statistical Computing, Vienna, Austria).
Patients who had both a treated tear and tear left in situ without treatment in the same compartment at the time of primary ACL reconstruction were considered as having been treated within the flow diagram (Figure 1) since we were unable to distinguish which tear subsequently underwent reoperation, the primary outcome. However, multiple tears within the same compartment at the time of primary ACL reconstruction were treated independently for the purpose of prediction of treatment during formulation of the nomograms since the data for each individual tear was collected separately at the time of primary ACL reconstruction.
Results
Between 2002 and 2004, 1399 isolated, unilateral primary ACL reconstructions were listed in the multicenter study database. There were 914 patients (65.3%) who had concomitant meniscal tears at the time of their index ACL reconstruction. Of these, 210 patients (23.0%) had meniscal tears left in situ without treatment at the time of surgery, with 194 patients (totaling 208 untreated meniscus tears in unique compartments) completing 6-year follow-up (92.4%) (Figure 1).
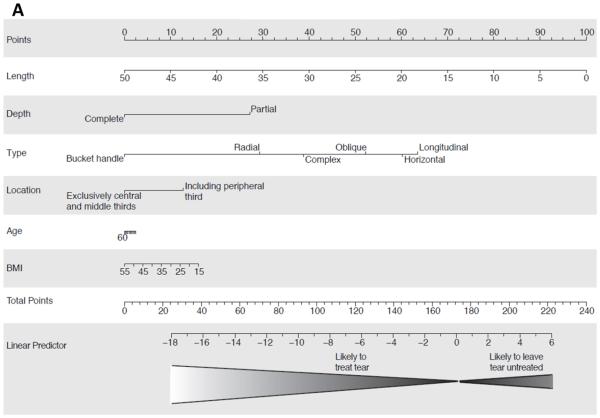
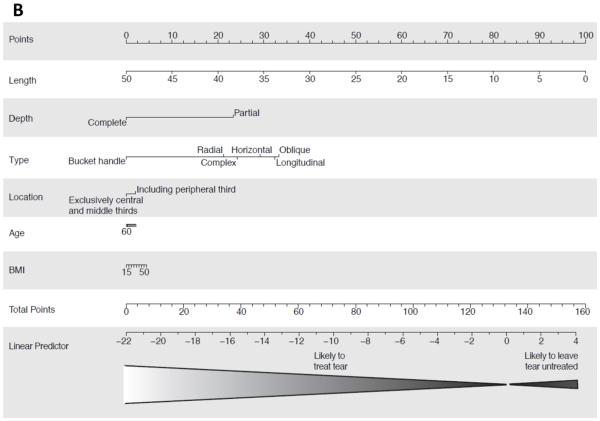
In order to determine the likelihood that meniscus tears were left in situ without treatment or treated with excision and/or repair, proportional odds models were created utilizing several patient and tear characteristics. There were 719 lateral meniscus tears (532 treated; 187 no treatment) and 545 medial meniscus tears (464 treated; 81 no treatment) included for this model. All meniscal treatment decisions made at the time of primary ACL reconstruction were made by the treating surgeon without specific exclusion or inclusion criteria limiting treatment choices. On the lateral side, tear length (p < 0.001), partial versus complete tear (p < 0.001), tear type (longitudinal versus radial/ complex/oblique; p < 0.001), and tear location (including peripheral third versus exclusively central/middle third; p < 0.001) were identified as significant predictors of treatment type. Specifically, for each 1 mm increase in tear length, the odds of leaving a tear in situ without treatment decreased by 22% (95% Confidence Interval [CI]: 15-28%). Partial tears as compared to complete tears (Odds Ratio [OR] = 27.3; 95% CI: 1.6 – 51.0), tears including the peripheral third as compared to tears exclusively in the central/middle third (OR = 4.7; 95% CI: 2.5 – 8.9), and longitudinal tears as compared to oblique (OR = 3.9; 95% CI: 1.9 – 8.3), complex (OR = 20.6; 95% CI: 6.1 – 68.9), or radial tears (OR = 65.2; 95% CI: 17.6 – 242.0) were all significantly (p < 0.001) more likely to be left in situ without treatment at the time of primary ACL reconstruction. There was no significant difference between the odds of longitudinal tears or horizontal tears to be left in situ without treatment (p = 0.7). All bucket handle tears were treated. On the medial side, only tear length (p < 0.001) and complete versus partial tear type (p < 0.001) were significant predictors of treatment type. Specifically, for each 1 mm increase in tear length, the odds of leaving a tear in situ without treatment decreased by 28% (95% CI: 18 – 38%), while partial tears as compared to complete tears (OR = 47.9; 95% CI: 18.0 – 127.5) were more likely to be left in situ without treatment at the time of primary ACL reconstruction (Figure 2). All other factors were not statistically significant for the medial compartment (p ≥ 0.05).
Figure 2.
Nomogram for predicting which meniscus tears are left in situ without treatment at the time of primary ACL reconstruction within the (A) lateral and (B) medial compartments. A vertical line is drawn independently for each variable of interest (tear length, depth, type, location, patient age, BMI), intersecting the “Points” row. The values for each variable of interest are then added and the corresponding value located on the “Total Points” row located. A vertical line is then drawn from this point to the “Linear Predictor” row in order to determine whether a tear was more likely to be treated or left in situ without treatment.
Tears left untreated were located in the lateral compartment in 123 patients (63.4%), medial compartment in 57 patients (29.4%), and both the lateral and medial compartment in 14 patients (7.2%). The average age of patients with meniscus tears left untreated was 24.9 ± 10.7 years, with female patients accounting for 49.0% of the cohort (Table 1). Overall, 208 meniscus tears were left untreated, 137 lateral (65.9%) and 71 medial (34.1%), within unique compartments. Lateral tears left without treatment were more frequently complete tears as compared to tears left without treatment in the medial compartment (18.2 vs. 5.6%; p = 0.013). Otherwise, no differences in tear characteristics were identified between lateral and medial compartment tears (Table 2).
Table 1.
Demographic Characteristics for Patients with Meniscus Tears left without treatment at the time of Primary ACL Reconstruction†
| n | 194 |
| Sex | |
| Male | 99 (51.0) |
| Female | 95 (49.0) |
| Age (years)* | 24.9 ± 10.7 |
| Smoking Status | |
| No | 160 (82.5) |
| Quit | 18 (9.3) |
| Yes | 14 (7.2) |
| Unknown | 2 (1.0) |
| BMI‡ (n = 189)* | 24.8 ± 4.3 |
| Ethnicity | |
| White | 168 (86.6) |
| Black | 16 (8.2) |
| Other | 10 (5.2) |
| Compartment(s) Involved | |
| Medial | 57 (29.4) |
| Lateral | 123 (63.4) |
| Both | 14 (7.2) |
Values listed as number (%) except where noted.
Body mass index (kg/m2)
Listed as mean ± standard deviation.
Table 2.
Characteristics of Tears Left Untreated following Primary ACL Reconstruction, separated by Compartment†
| Medial |
Lateral |
p-value |
Combined |
|
| n (%) | 71 (34.1) | 137 (65.9) | 208 (100) | |
| Partial vs. Complete | 0.013!! | |||
| Partial | 67 (94.4) | 112 (81.8) | 179 (86.1) | |
| Complete | 4 (5.6) | 25 (18.2) | 29 (13.9) | |
| Anterior-Posterior Location | 0.086 | |||
| Anterior | 2 (2.8) | 0 (0) | 2 (1.0) | |
| Anterior + Posterior | 0 (0) | 2 (1.5) | 2 (1.0) | |
| Posterior | 69 (97.2) | 135 (98.5) | 204 (98.1) | |
| Coronal Location | 0.083 | |||
| Central + Middle + Peripheral Third | 0 (0) | 4 (2.9) | 4 (1.9) | |
| Central + Middle Third | 1 (1.4) | 10 (7.3) | 11 (5.3) | |
| Central Third | 5 (7.0) | 8 (5.8) | 13 (6.3) | |
| Middle + Peripheral Third | 5 (7.0) | 14 (10.2) | 19 (9.1) | |
| Middle Third | 15 (21.1) | 39 (28.5) | 54 (26.0) | |
| Peripheral Third | 45 (63.4) | 62 (45.3) | 107 (51.4) | |
| Tear Type | 0.091 | |||
| Complex | 1 (1.4) | 6 (4.4) | 7 (3.4) | |
| Horizontal | 0 (0) | 1 (0.7) | 1 (0.5) | |
| Longitudinal(vertical) | 64 (90.1) | 105 (76.6) | 169 (81.3) | |
| Oblique | 3 (4.2) | 21 (15.3) | 24 (11.5) | |
| Radial | 3 (4.2) | 4 (2.9) | 7 (3.4) | |
| Length, mm (continuous)* | 9.2 ± 2.9 | 9.5 ± 3.9 | 0.520 | 9.4 ± 3.6 |
| Length (categorical) | 0.314 | |||
| < 10 mm | 29 (40.8) | 66 (48.2) | 95 (45.7) | |
| ≥ 10 mm | 42 (59.2) | 71 (51.8) | 113 (54.3) | |
| Degenerative Tear | 0.450 | |||
| No | 67 (94.4) | 132 (97.1) | 199 (96.1) | |
| Yes | 4 (5.6) | 4 (2.9) | 8 (3.9) |
Values listed as number (%) except where noted.
Listed as mean ± standard deviation.
Indicates statistical significance.
Subsequent ipsilateral knee surgery, including meniscus repair or excision within the same compartment of meniscus tears left untreated at the time of primary ACL reconstruction, was performed for 16 tears (7.7%) at an average follow-up of 22.3 ± 19.7 months. Of these, 9 tears underwent meniscal reoperation in the setting of revision ACL reconstruction at average follow-up 0f 23.8 ± 21.1 months, leaving 7 tears (3.4%) that underwent isolated treatment of meniscal pathology, excluding treatment of tears in the setting of revision ACL reconstruction, at an average follow-up of 20.4 ±17.6 months. Surgery to address any meniscal pathology in these cases included excision for 13 tears (6.3%) and repair for 3 tears (1.4%) including meniscal surgery in the setting of revision ACL reconstruction. All lateral compartment tears left untreated that required subsequent surgery measured ≥ 10 mm, while several medial compartment tears that required reoperation measured < 10 mm (Table 3).
Table 3.
Characteristics of Tears Left Untreated following Primary ACL Reconstruction Requiring Reoperation†
| Any Reoperation‡ | Isolated Meniscus Reoperation!! | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| Medial |
Lateral |
Combined |
Medial |
Lateral |
Combined |
|
| n (%) | 71 (34.1) | 137 (65.9) | 208 (100) | 71 (34.1) | 137 (65.9) | 208 (100) |
| Partial vs. Complete | ||||||
| Partial | 9 (12.7) | 5 (3.6) | 14 (6.7) | 4 (5.6) | 2 (1.5) | 6 (2.9) |
| Complete | 0 (0) | 2 (1.5) | 2 (1.0) | 0 (0) | 1 (0.7) | 1 (0.5) |
| Anterior-Posterior Location | ||||||
| Anterior | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Anterior + Posterior | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Posterior | 9 (12.7) | 7 (5.1) | 16 (7.7) | 4 (5.6) | 3 (2.2) | 7 (3.4) |
| Coronal Location | ||||||
| Central + Middle + Peripheral Third | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Central + Middle Third | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Central Third | 2 (2.8) | 0 (0) | 2 (1.0) | 1 (1.4) | 0 (0) | 1 (0.5) |
| Middle + Peripheral Third | 0 (0) | 2 (1.5) | 2 (1.0) | 0 (0) | 2 (1.5) | 2 (1.0) |
| Middle Third | 1 (1.4) | 3 (2.2) | 4 (1.9) | 0 (0) | 1 (0.7) | 1 (0.5) |
| Peripheral Third | 6 (8.5) | 2 (1.5) | 8 (3.8) | 3 (4.2) | 0 (0) | 3 (1.4) |
| Tear Type | ||||||
| Complex | 0 (0) | 1 (0.7) | 1 (0.5) | 0 (0) | 0 (0) | 0 (0) |
| Horizontal | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Longitudinal(vertical) | 9 (12.7) | 5 (3.6) | 14 (6.7) | 4 (5.6) | 2 (1.5) | 6 (2.9) |
| Oblique | 0 (0) | 1 (0.7) | 1 (0.5) | 0 (0) | 1 (0.7) | 1 (0.5) |
| Radial | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Length, mm (continuous) | 9.7 ± 2.3 | 11.4 ± 2.2 | 10.4 ± 2.4 | 9.3 ± 3.4 | 10.7 ± 1.2 | 9.9 ± 2.6 |
| Length (categorical) | ||||||
| < 10 mm | 3 (4.2) | 0 (0) | 3 (1.4) | 2 (2.8) | 0 (0) | 2 (1.0) |
| ≥ 10 mm | 6 (8.5) | 7 (5.1) | 13 (6.3) | 2 (2.8) | 3 (2.2) | 5 (2.4) |
| Degenerative Tear | ||||||
| No | 9 (12.7) | 7 (5.1) | 16 (7.7) | 4 (5.6) | 3 (2.2) | 7 (3.4) |
| Yes | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Treatment Type | ||||||
| Excision | 9 (12.7) | 4 (2.9) | 13 (6.3) | 3 (4.2) | 3 (2.2) | 6 (2.9) |
| Repair | 0 (0) | 3 (2.2) | 3 (1.4) | 1 (1.4) | 0 (0) | 1 (0.5) |
Values listed as number (%) except where noted.
Listed as mean ± standard deviation.
Any reoperation for meniscal pathology.
Excludes meniscus reoperation in setting of revision ACL reconstruction
Univariate analysis of patient demographic variables and meniscal tear characteristics was performed to determine variables associated with increased rates of all reoperation and reoperation not in the setting of revision ACL reconstruction. Including all reoperations, there was a trend toward increased reoperation in medial compartment tears as compared to lateral compartment tears left untreated (12.7 vs. 5.1%; p = 0.052) (Table 4). This trend was less apparent when excluding patients that underwent reoperation with concomitant revision ACL reconstruction. Including all reoperations, tears measuring ≥ 10 mm underwent reoperation more frequently than tears measuring < 10 mm (11.5 vs. 3.2%; p = 0.035). This relationship was not seen when excluding tears treated in the setting of concomitant revision ACL reconstruction. Not including reoperation in the setting of revision ACL reconstruction, patients who underwent reoperation for meniscus tears left untreated at the time of primary ACL reconstruction were significantly younger compared to those patients who did not require reoperation (18.6 vs. 25.1 years; p = 0.026).
Table 4.
Patient and Tear Characteristics for Meniscus Tears that Did and Did Not Require Reoperation†
| Any Reoperation!! | Isolated Meniscus Reoperation€ | |||||
|---|---|---|---|---|---|---|
|
|
||||||
| No |
Yes |
p-value |
No |
Yes |
p-value |
|
| Patient Characteristics (n = 194) | ||||||
| Sex | 0.338 | 0.659 | ||||
| Male | 89 (89.9) | 10 (10.1) | 96 (97.0) | 3 (3.0) | ||
| Female | 89 (93.7) | 6 (6.3) | 91 (95.8) | 4 (4.2) | ||
| Age (years)* | 25.2 ± 10.8 | 20.7 ± 8.6 | 0.062 | 25.1 ± 10.8 | 18.6 ± 5.9 | 0.026Ω |
| Smoking Status | 0.640 | 0.848 | ||||
| No | 146 (91.3) | 14 (8.8) | 154 (96.3) | 6 (3.8) | ||
| Quit | 16 (88.9) | 2 (11.1) | 17 (94.4) | 1 (5.6) | ||
| Yes | 14 (100) | 0 (0) | 14 (100) | 0 (100) | ||
| Unknown | 2 (100) | 0 (0) | 2 (100) | 0 (100) | ||
| BMI‡ (n = 190)* | 24.8 ± 4.4 | 24.0 ± 3.3 | 0.483 | 24.8 ± 4.4 | 24.1 ± 3.8 | 0.685 |
| Ethnicity | 0.939 | 0.570 | ||||
| White | 154 (91.7) | 14 (8.3) | 161 (95.8) | 7 (4.2) | ||
| Black | 15 (93.8) | 1 (6.2) | 16 (100) | 0 (0) | ||
| Other | 9 (90.0) | 1 (10.0) | 10 (100) | 0 (0) | ||
| Location of Tear(s) | 0.080 | 0.150 | ||||
| Medial | 49 (86.0) | 8 (14.0) | 53 (93.0) | 4 (7.0) | ||
| Lateral | 117 (95.1) | 6 (4.9) | 121 (98.4) | 2 (1.6) | ||
| Both | 12 (85.7) | 2 (1.4) | 13 (92.9) | 1 (7.1) | ||
| Tear Characteristics (n = 208) | ||||||
| Compartment | 0.052 | 0.233 | ||||
| Medial | 62 (87.3) | 9 (12.7) | 67 (94.4) | 4 (5.6) | ||
| Lateral | 130 (94.9) | 7 (5.1) | 134 (97.8) | 3 (2.2) | ||
| Partial vs. Complete | 0.862 | 1.000 | ||||
| Partial | 165 (92.12) | 14 (7.8) | 173 (96.6) | 6 (3.4) | ||
| Complete | 27 (93.1) | 2 (6.9) | 28 (96.6) | 1 (3.4) | ||
| Anterior-Posterior Location | 0.844 | 0.931 | ||||
| Anterior | 2 (100) | 0 (0) | 2 (100) | 0 (0) | ||
| Anterior + Posterior | 2 (100) | 0 (0) | 2 (100) | 0 (0) | ||
| Posterior | 188 (92.2) | 16 (7.8) | 197 (96.6) | 7 (3.4) | ||
| Coronal Location | 0.767 | 0.447 | ||||
| Central + Middle + Peripheral Third | 4 (100) | 0 (0) | 4 (100) | 0 (0) | ||
| Central + Middle Third | 11 (100) | 0 (0) | 11 (100) | 0 (0) | ||
| Central Third | 11 (84.6) | 2 (15.4) | 12 (92.3) | 1 (7.7) | ||
| Middle + Peripheral Third | 17 (89.5) | 2 (10.5) | 17 (89.5) | 2 (10.5) | ||
| Middle Third | 50 (92.6) | 4 (7.5) | 53 (98.1) | 1 (1.9) | ||
| Peripheral Third | 99 (92.5) | 8 (7.5) | 104 (97.2) | 3 (2.8) | ||
| Tear Type | 0.808 | 0.964 | ||||
| Complex | 6 (85.7) | 1 (14.3) | 7 (100) | 0 (0) | ||
| Horizontal | 1 (100) | 0 (0) | 1 (100) | 0 (0) | ||
| Longitudinal(vertical) | 155 (91.7) | 14 (8.3) | 163 (96.4) | 6 (3.6) | ||
| Oblique | 23 (95.8) | 1 (4.2) | 23 (95.8) | 1 (4.2) | ||
| Radial | 7 (100) | 0 (0) | 7 (100) | 0 (0) | ||
| Length, mm (continuous)* | 9.3 ± 3.6 | 10.4 ± 2.4 | 0.233 | 9.4 ± 3.6 | 9.9 ± 2.6 | 0.740 |
| Length (categorical) | 0.035Ω | 0.458 | ||||
| < 10 mm | 92 (96.8) | 3 (3.2) | 93 (97.9) | 2 (2.1) | ||
| ≥ 10 mm | 100 (88.5) | 13 (11.5) | 108 (95.6) | 5 (4.4) | ||
| Degenerative Tear | 1.000 | 1.000 | ||||
| No | 183 (92.0) | 16 (8.0) | 192 (96.5) | 7 (3.5) | ||
| Yes | 8 (100) | 0 (0) | 8 (100) | 0 (0) | ||
Values listed as number (%) except where noted.
Body mass index (kg/m2)
Listed as mean ± standard deviation.
Any reoperation for meniscal pathology
Excludes meniscus reoperation in setting of revision ACL reconstruction.
Denotes statistical significance.
Discussion
The primary purpose of this study was to determine the rate of subsequent reoperation of meniscal tears left in situ without treatment at the time of primary ACL reconstruction using a well-established, multicenter ACL reconstruction database. Several studies have previously reported clinical outcomes and reoperation rates for meniscus tears left untreated at the time of ACL reconstruction,4, 9, 20, 23, 26, 28, 34, 37, 38 but to date, no studies have provided clinical data at minimum 6-year follow-up in a prospectively collected cohort. In the present study, 91.8% of patients did not require reoperation for meniscal pathology at 6-year follow-up. Excluding meniscal reoperations performed in the setting of revision ACL reconstruction, an even greater number of patients, 96.4%, did not require reoperation for meniscal pathology. This reoperation rate compares favorably with the reoperation rate for intact menisci at the time of ACL reconstruction using the same dataset, with 97.4% of intact menisci not requiring reoperation at minimum 6-year follow-up.35 Meniscus tears left in situ without treatment measuring ≥ 10 mm in length underwent a higher rate of reoperation, with a trend toward increased reoperation in medial meniscus tears left in situ without treatment as compared to lateral meniscus tears when using any reoperation that addressed meniscal pathology as an endpoint. However, the overall low number of reoperations, and subsequently low statistical power, must be considered when evaluating these comparisons. Excluding meniscal reoperation in the setting of concomitant revision ACL reconstructions, patients who underwent reoperation of meniscus tears left in situ at the time of primary ACL reconstruction were significantly younger compared to their counterparts.
Failure following meniscal repair, meniscectomy, or leaving tears in situ without treatment at the time of ACL reconstruction has classically been defined and reported throughout the literature as the need for reoperation. While this definition allows for simple comparisons to be made between reoperation rates reported in the literature, it fails to acknowledge the ultimate goal when treating meniscal pathology at the time of ACL reconstruction which is to create a favorable environment for knee stability while preventing subsequent articular cartilage damage. Additionally, re-injury to the previously reconstructed ACL may be considered a separate injury event, and reporting meniscal reoperations in this setting may unnecessarily increase the reporting of reoperation rates. In the largest report on the outcome of stable lateral meniscus tears, defined as those tears that could not be moved with a probe into the intercondylar notch, left in situ at the time of ACL reconstruction provided by Shelbourne et al,23 reoperation rates were categorized by tear type and location. Posterior horn and posterior, peripheral tears were noted to have a reoperation rate < 3%, while radial flap tears underwent reoperation in 6% of patients. These findings expanded upon the previous literature on lateral meniscus tears provided by Fitzgibbons et al9 which reported successful outcomes following “aggressive” non-treatment of lateral meniscal tears during ACL reconstruction. Talley et al26 noted similar results to Shelbourne and colleagues when leaving lateral meniscal tears in situ, with 4% of patients undergoing reoperation for meniscal pathology. In a systematic review of meniscal tears left in situ at the time of ACL reconstruction, Pujol et al21 reported reoperation rates ranging from 0-22% with an average rate of failure of 4.8% at minimum 16-month follow-up. The results of the present study are consistent with those previously reported and may provide even more optimism for leaving certain lateral compartment tears in situ without treatment at the time of primary ACL reconstruction, given the reported 5.1% reoperation rate for lateral meniscus tears treated in any setting and reoperation rate of 2.2% reported for treatment of lateral meniscus tears not in the setting of revision ACL reconstruction at minimum 6-year follow-up.
The results following non-treatment of medial meniscus tears have been consistently less satisfying in previous literature. Compared to his lateral meniscus cohort, Shelbourne et al24 reported a 10.8% rate of reoperation for patients with medial meniscus tears left in situ, compared to a 13.6% and 6% reoperation rate for tears treated with repair or abrasion and trephination, respectively. The authors concluded that medial meniscus tears, especially tears measuring ≥ 10 mm, are best treated with abrasion and trephination. Vermesan et al28 reported equivalent outcomes between medial and lateral meniscus tears left in situ. However, lateral meniscus tears were longer than medial meniscus tears in the study and were more often accompanied by severe chondromalacia at the time of surgery. Results of a systematic review21 report reoperation rates for medial meniscus tears left in situ from 0-33%, with an average failure rate of 14.8% at minimum 16-month follow-up. The results of the present study are consistent with those previously reported, with a reoperation rate of 12.7% for medial meniscal tears in any setting and 5.6% when excluding meniscal reoperation in the setting of revision ACL reconstruction, with both values higher than those reported for lateral tears left in situ without treatment.
While the discrepancy in reoperation rates between medial and lateral tears left without treatment at the time of ACL reconstruction have been previously reported, determining with certainty which tears can be left without treatment has proven more difficult to predict. Previous studies have noted that peripheral, lateral meniscus tears that measure less than 10 mm and do not extend anteriorly have predictably low reoperation rates.9, 20, 21, 23 Reoperation rates after leaving medial meniscus tears in situ without treatment have been much less predictable.24, 26, 37 The findings of the present study are in agreement with previous reports, with no reoperations reported for lateral tears measuring < 10 mm, while finding the fate of medial meniscus tears left in situ at the time of ACL reconstruction to be less predictable. Furthermore, while excluding meniscal reoperation in the setting of concomitant revision ACL reconstruction, we found that patients requiring reoperation were significantly younger than those who did not require reoperation. While younger patient age has been identified as a risk factor for graft failure1, 32, 33 and revision surgery10 following ACL reconstruction in addition to need for reoperation following isolated meniscal repair16, this finding has not been previously reported when evaluating meniscus tears left untreated at the time of primary ACL reconstruction and warrants further investigation.
Moving forward, future directions for evaluation of meniscus treatment must coincide with the primary goal of meniscus treatment at the time of ACL reconstruction, which is to create a favorable environment for knee stability while preventing subsequent articular cartilage damage. While the importance of the meniscus in transmitting loads across the knee has been well established,3, 29 the long-term effects of meniscus treatment strategies on the preservation of articular cartilage have been less conclusive. Meniscal repair techniques continue to improve and serve as an attempt to restore the load bearing characteristics of the native meniscus. While early results of meniscus repair have been promising,15, 25 particularly when performed at the same time as ACL reconstruction,19, 31 there is some concern that clinical, as well as radiographic results, may deteriorate over time, particularly for tears within the medial compartment.7, 14, 17, 35 Whether or not leaving meniscus tears in situ without treatment serves as a viable long-term option for preservation of articular cartilage has yet to be established as well.
Assessing non-operatively managed meniscal tears provides several points to consider. As is the case with much of the literature regarding non-treatment of meniscus tears, a great deal of surgeon selection bias may come into play when choosing meniscal tears to leave in situ without treatment. It is frequently reported that stable meniscus tears, particularly those involving the lateral meniscus, can reliably be left in situ without treatment with good clinical results. Several authors have attempted to define what encompasses a stable tear,24, 26, 34 but there is little consistency between definitions. Additionally, we believe that meniscal reoperation in the setting of revision ACL reconstruction, and presumed recurrent instability, differs from isolated meniscal surgery. While we elected to distinguish these two unique cohorts, this is not consistently done throughout the literature. While a randomized design would help eliminate this shortcoming, previous research has indicated that surgeons consistently agree upon treatment choice when independently evaluating tears.8 In light of this, we elected to provide analysis from surgeons participating in the multicenter study as to which types of tears are most likely to be left in situ without treatment at the time of primary ACL reconstruction. For lateral meniscus tears, we identified decreasing tear length, partial tears, longitudinal tears, and tears including the peripheral third as predictors of leaving tears in situ without treatment, while decreasing tear length and partial tears predicted leaving tears in situ without treatment within the medial compartment. While we acknowledge that these findings are limited to the current cohort in question and guided by the treatment decisions made by the participating surgeons at the time of ACL reconstruction, the generally favorable results for both lateral and medial meniscus tears left in situ without treatment could potentially help guide surgeons in the future while serving as a baseline for future comparative studies.
The present study does have several limitations. Failure in the present study and throughout the majority of the existing literature is defined by reoperation. More specific to the present study, failure was defined as any reoperation focused on meniscus pathology within the same compartment, medial or lateral, as the meniscal tear left in situ without treatment at the time of the index ACL reconstruction due to symptomatic failure, although the exact symptomatology necessitating reoperation is not implicitly defined within the database. This definition fails to address the primary goal of meniscus repair at the time of ACL reconstruction which is to provide a stable knee with preservation of articular cartilage. The present study does not report clinical outcome data on meniscus tears left in situ without treatment at the time of ACL reconstruction, as this subset of data has previously been reported by the multicenter study.7 As such, clinically symptomatic knees that have not undergone reoperation may not be captured. Lastly, this paper was not designed to compare different treatment strategies for meniscus tears found at the time of ACL reconstruction and such comparisons are beyond the scope of this paper. An idealized situation would allow randomization of treatment options using an algorithmic approach based on tear length, location, and chronicity. The multicenter study has reported on multivariate analysis of outcomes following ACL reconstruction, and treatment of meniscus and cartilage pathology is only one of many factors influencing outcomes after ACL reconstruction.7
Conclusion
Utilizing a prospectively collected multicenter database with minimum 6-year follow-up, the present study reemphasizes the low reoperation rate following non-treatment of small, peripheral lateral meniscus tears at the time of ACL reconstruction while noting less predictable results for medial meniscus tears left without treatment the time of ACL reconstruction. While the decision to treat or leave tears in situ without treatment may be at least partially surgeon-dependent, we have identified several tear characteristics that predict leaving meniscus tears in situ without treatment at the time of primary ACL reconstruction. Further studies should aim to better characterize appropriate tears to leave without treatment at the time of ACL reconstruction while also studying the role age plays on outcomes for meniscal tears left in situ without treatment.
What is known about the subject
There is limited data on reoperation rates of meniscus tears left untreated at the time of ACL reconstruction beyond 6-year follow-up.
What this study adds to existing knowledge
This is the first prospective multicenter study to report outcomes with minimum 6-year follow-up for meniscus tears left untreated at the time of ACL reconstruction.
Acknowledgment
The authors thank Samuel K. Nwosu, MS, for his contribution to the statistical methods for this manuscript.
References
- 1.Andernord D, Desai N, Björnsson H, Ylander M, Karlsson J, Samuelsson K. Patient Predictors of Early Revision Surgery After Anterior Cruciate Ligament Reconstruction A Cohort Study of 16,930 Patients With 2-Year Follow-up. Am J Sports Med. 2015;43(1):121–7. doi: 10.1177/0363546514552788. [DOI] [PubMed] [Google Scholar]
- 2.Arnoczky SP, Warren RF. The microvasculature of the meniscus and its response to injury An experimental study in the dog. Am J Sports Med. 1983;11(3):131–141. doi: 10.1177/036354658301100305. [DOI] [PubMed] [Google Scholar]
- 3.Baratz ME, Fu FH, Mengato R. Meniscal tears: The effect of meniscectomy and of repair on intraarticular contact areas and stress in the human knee: A preliminary report. Am J Sports Med. 1986;14(4):270–275. doi: 10.1177/036354658601400405. [DOI] [PubMed] [Google Scholar]
- 4.Beaufils P, Bastos R, Wakim E, Cho S, Petit-Jouvet C. Meniscal injury in the plastic reconstruction of the anterior cruciate ligament. Meniscal suture or abstention. Rev Chir Orthop Reparatrice Appar Mot. 1991;78(5):285–291. [PubMed] [Google Scholar]
- 5.Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW, Albright JP, Allen CR, Amendola A, Anderson AF. Intra-articular Findings in Primary and Revision Anterior Cruciate Ligament Reconstruction Surgery A Comparison of the MOON and MARS Study Groups. Am J Sports Med. 2011;39(9):1889–1893. doi: 10.1177/0363546511406871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burks RT, Metcalf MH, Metcalf RW. Fifteen-year follow-up of arthroscopic partial meniscectomy. Arthroscopy. 1997;13(6):673–679. doi: 10.1016/s0749-8063(97)90000-1. [DOI] [PubMed] [Google Scholar]
- 7.Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD, Wright RW, Kaeding CC, Marx RG, Amendola A. Are Articular Cartilage Lesions and Meniscus Tears Predictive of IKDC, KOOS, and Marx Activity Level Outcomes After Anterior Cruciate Ligament Reconstruction? A 6-Year Multicenter Cohort Study. Am J Sports Med. 2014;42(5):1058–1067. doi: 10.1177/0363546514525910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dunn WR, Wolf BR, Amendola A, Andrish JT, Kaeding C, Marx RG, McCarty EC, Parker RD, Wright RW, Spindler KP. Multirater agreement of arthroscopic meniscal lesions. Am J Sports Med. 2004;32(8):1937–1940. doi: 10.1177/0363546504264586. [DOI] [PubMed] [Google Scholar]
- 9.Fitzgibbons RE, Shelbourne KD. "Aggressive" Nontreatment of Lateral Meniscal Tears Seen During Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 1995;23(2):156–9. doi: 10.1177/036354659502300205. [DOI] [PubMed] [Google Scholar]
- 10.Hettrich CM, Dunn WR, Reinke EK, Spindler KP, Parker RD, Andrish JT, Kaeding CC, Amendola A, Wright RW, Marx RG. The Rate of Subsequent Surgery and Predictors After Anterior Cruciate Ligament Reconstruction Two-and 6-Year Follow-up Results From a Multicenter Cohort. Am J Sports Med. 2013;41(7):1534–1540. doi: 10.1177/0363546513490277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoser C, Fink C, Brown C, Reichkendler M, Hackl W, Bartlett J. Long-term results of arthroscopic partial lateral meniscectomy in knees without associated damage. J Bone Joint Surg Br. 2001;83(4):513–516. doi: 10.1302/0301-620x.83b4.11364. [DOI] [PubMed] [Google Scholar]
- 12.Ihara H, Miwa M, Takayanagi K, Nakayama A. Acute torn meniscus combined with acute cruciate ligament injury: second look arthroscopy after 3-month conservative treatment. Clin Orthop Relat Res. 1994;307:146–154. [PubMed] [Google Scholar]
- 13.Jaureguito JW, Elliot JS, Lietner T, Dixon LB, Reider B. The effects of arthroscopic partial lateral meniscectomy in an otherwise normal knee: a retrospective review of functional, clinical, and radiographic results. Arthroscopy. 1995;11(1):29–36. doi: 10.1016/0749-8063(95)90085-3. [DOI] [PubMed] [Google Scholar]
- 14.Lee GP, Diduch DR. Deteriorating outcomes after meniscal repair using the meniscus arrow in knees undergoing concurrent anterior cruciate ligament reconstruction increased failure rate with long-term follow-up. Am J Sports Med. 2005;33(8):1138–1141. doi: 10.1177/0363546505275348. [DOI] [PubMed] [Google Scholar]
- 15.Logan M, Watts M, Owen J, Myers P. Meniscal repair in the elite athlete results of 45 repairs with a minimum 5-year follow-up. Am J Sports Med. 2009;37(6):1131–1134. doi: 10.1177/0363546508330138. [DOI] [PubMed] [Google Scholar]
- 16.Lyman S, Hidaka C, Valdez AS, Hetsroni I, Pan TJ, Do H, Dunn WR, Marx RG. Risk Factors for Meniscectomy After Meniscal Repair. Am J Sports Med. 2013;41(12):2772–8. doi: 10.1177/0363546513503444. [DOI] [PubMed] [Google Scholar]
- 17.Nepple JJ, Dunn WR, Wright RW. Meniscal Repair Outcomes at Greater Than Five YearsA Systematic Literature Review and Meta-Analysis. J Bone Joint Surg Am. 2012;94(24):2222–2227. doi: 10.2106/JBJS.K.01584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paletta GA, Levine DS, O'Brien SJ, Wickiewicz TL, Warren RF. Patterns of meniscal injury associated with acute anterior cruciate ligament injury in skiers. Am J Sports Med. 1992;20(5):542–547. doi: 10.1177/036354659202000510. [DOI] [PubMed] [Google Scholar]
- 19.Paxton ES, Stock MV, Brophy RH. Meniscal repair versus partial meniscectomy: a systematic review comparing reoperation rates and clinical outcomes. Arthroscopy. 2011;27(9):1275–1288. doi: 10.1016/j.arthro.2011.03.088. [DOI] [PubMed] [Google Scholar]
- 20.Pierre A, Hulet C, Locker B, Schiltz D, Delbarre J, Vielpeau C. Outcome of 95 stable meniscal tears left in place after reconstruction of the anterior cruciate ligament. Rev Chir Orthop Reparatrice Appar Mot. 2001;87(7):661–668. [PubMed] [Google Scholar]
- 21.Pujol N, Beaufils P. Healing results of meniscal tears left in situ during anterior cruciate ligament reconstruction: a review of clinical studies. Knee Surg Sports Traumatol Arthrosc. 2009;17(4):396–401. doi: 10.1007/s00167-008-0711-y. [DOI] [PubMed] [Google Scholar]
- 22.Shelbourne KD, Gray T. Meniscus tears that can be left in situ, with or without trephination or synovial abrasion to stimulate healing. Sports Med Arthrosc. 2012;20(2):62–67. doi: 10.1097/JSA.0b013e318243265b. [DOI] [PubMed] [Google Scholar]
- 23.Shelbourne KD, Heinrich J. The long-term evaluation of lateral meniscus tears left in situ at the time of anterior cruciate ligament reconstruction. Arthroscopy. 2004;20(4):346–351. doi: 10.1016/j.arthro.2004.01.029. [DOI] [PubMed] [Google Scholar]
- 24.Shelbourne KD, Rask BP. The sequelae of salvaged nondegenerative peripheral vertical medial meniscus tears with anterior cruciate ligament reconstruction. Arthroscopy. 2001;17(3):270–274. doi: 10.1053/jars.2001.19978. [DOI] [PubMed] [Google Scholar]
- 25.Steenbrugge F, Verdonk R, Hürel C, Verstraete K. Arthroscopic meniscus repair: inside-out technique vs. Biofix meniscus arrow. Knee Surg Sports Traumatol Arthrosc. 2004;12(1):43–49. doi: 10.1007/s00167-003-0446-8. [DOI] [PubMed] [Google Scholar]
- 26.Talley MC, Grana WA. Treatment of partial meniscal tears identified during anterior cruciate ligament reconstruction with limited synovial abrasion. Arthroscopy. 2000;16(1):6–10. doi: 10.1016/s0749-8063(00)90120-8. [DOI] [PubMed] [Google Scholar]
- 27.Toman CV, Dunn WR, Spindler KP, Amendola A, Andrish JT, Bergfeld JA, Flanigan D, Jones MH, Kaeding CC, Marx RG. Success of meniscal repair at anterior cruciate ligament reconstruction. Am J Sports Med. 2009;37(6):1111–1115. doi: 10.1177/0363546509337010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vermesan D, Prejbeanu R, Laitin S, Georgianu V, Haragus H, Nitescu S, Tatullo M, Tattoli M, Caprio M, Cagiano R. Meniscal tears left in situ during anatomic single bundle anterior cruciate ligament reconstruction. Eur Rev Med Pharmacol Sci. 2014;18(2):252–256. [PubMed] [Google Scholar]
- 29.Walker PS, Erkiuan MJ. The role of the menisci in force transmission across the knee. Clin Orthop Relat Res. 1975;109:184–192. doi: 10.1097/00003086-197506000-00027. [DOI] [PubMed] [Google Scholar]
- 30.Warren RF, Levy IM. Meniscal lesions associated with anterior cruciate ligament injury. Clin Orthop Relat Res. 1983;172:32–37. [PubMed] [Google Scholar]
- 31.Wasserstein D, Dwyer T, Gandhi R, Austin PC, Mahomed N, Ogilvie-Harris D. A matched-cohort population study of reoperation after meniscal repair with and without concomitant anterior cruciate ligament reconstruction. Am J Sports Med. 2013;41(2):349–355. doi: 10.1177/0363546512471134. [DOI] [PubMed] [Google Scholar]
- 32.Wasserstein D, Khoshbin A, Dwyer T, Chahal J, Gandhi R, Mahomed N, Ogilvie-Harris D. Risk Factors for Recurrent Anterior Cruciate Ligament Reconstruction A Population Study in Ontario, Canada, With 5-Year Follow-up. Am J Sports Med. 2013;41(9):2099–2107. doi: 10.1177/0363546513493580. [DOI] [PubMed] [Google Scholar]
- 33.Webster KE, Feller JA, Leigh WB, Richmond AK. Younger patients are at increased risk for graft rupture and contralateral injury after anterior cruciate ligament reconstruction. Am J Sports Med. 2014;42(3):641–7. doi: 10.1177/0363546513517540. [DOI] [PubMed] [Google Scholar]
- 34.Weiss CB, Lundberg M, Hamberg P, DeHaven K, Gillquist J. Non-operative treatment of meniscal tears. J Bone Joint Surg Am. 1989;71(6):811–822. [PubMed] [Google Scholar]
- 35.Westermann RW, Wright RW, Spindler KP, Houston LJ, Wolf BR, Cox CL, Kaeding CC, Flanigan DC, Magnussen RA, Matava MJ. Meniscal Repair With Concurrent Anterior Cruciate Ligament Reconstruction Operative Success and Patient Outcomes at 6-Year Follow-up. Am J Sports Med. 2014;42(9):2184–92. doi: 10.1177/0363546514536022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wright R, Spindler K, Huston L, Amendola A, Andrish J, Brophy R, Carey J, Cox C, Flanigan D, Jones M. Revision ACL reconstruction outcomes: MOON cohort. J Knee Surg. 2011;24(4):289–294. doi: 10.1055/s-0031-1292650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yagishita K, Muneta T, Ogiuchi T, Sekiya I, Shinomiya K. Healing potential of meniscal tears without repair in knees with anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32(8):1953–1961. doi: 10.1177/0363546504263702. [DOI] [PubMed] [Google Scholar]
- 38.Zemanovic JR, McAllister DR, Hame SL. Nonoperative treatment of partial-thickness meniscal tears identified during anterior cruciate ligament reconstruction. Orthopedics. 2004;27(7):755–759. doi: 10.3928/0147-7447-20040701-17. [DOI] [PubMed] [Google Scholar]