Abstract
Background Occupational edema is reported to occur in healthy individuals after working in a sitting or standing position for extensive periods of time. It can be associated with feelings of tiredness, heaviness of the legs, and pain. Three licensed medical devices were compared in their management of occupational edema.
Subjects and Methods A total of 10 subjects were recruited from a clinical workspace. Right leg volume and great saphenous vein diameter was measured in the morning, and 6 hours later. On subsequent separate days, grade 2 graduated compression stockings (Active Compression Socks, Mediven, United Kingdom), geko (Firstkind Ltd, United Kingdom), and Revitive (Actegy Ltd, United Kingdom) were used bilaterally according to manufacturer's instructions.
Results Leg volumes increased by median 41 mL (p < 0.05) with no intervention. Percentage increase in leg volume was found to be significantly reduced by stockings compared with control (−1.7%, p < 0.01), and were more effective than electrical devices. Changes in vein diameter poorly correlate with leg volume changes.
Conclusion Occupational edema can occur over as little as 6 hours. All devices were well tolerated and reduced leg swelling. Stockings were the only device to significantly reduce leg swelling in this small trial.
Keywords: swelling, leg, edema, electrical stimulation, NMES, compression
Occupational edema is reported to occur in healthy individuals after working in a sitting or standing position for extensive periods of time.1 Activation of the calf muscle pump during walking, or recumbent position, allows limbs to empty, and intra-/extravascular pressures return to normal.2 Occupational edema is usually asymptomatic, but it can be associated with feelings of tiredness, heaviness of the legs, and pain.1 3 4
Previously, the efficacy of graduated compression stockings (GCS) has been investigated in the preventative management of occupational edema.1 2 4 5 The pressure applied by GCS is thought to increase the efficacy of the calf muscle pump. Activation of the calf muscle pump can also be achieved by applying electricity to the muscles and/or nerves of the leg (neuromuscular electrical stimulation [NMES]), and several new portable systems have been released in the last few years.6 These are available in the open market and marketed for the management of leg swelling, and improving circulation in the legs.
In this study, the effect of GCS on leg swelling is compared with these new NMES devices. Changes in great saphenous vein (GSV) diameter, and its correlation with leg swelling will also be monitored, as this has been linked to severity in chronic venous disease.7 8 Subjective measures of comfort and tolerability will also be noted.
Subjects and Methods
Participants
This pilot interventional crossover study trial included 10 participants (10 legs). Participants were recruited from clinical offices at Charing Cross Hospital. An information sheet was provided beforehand to all the participants, and written consent was obtained. The inclusion criteria were age 18 years or above, and ability to provide informed consent.
The subjects were excluded if they had a history of peripheral vascular disease, or renal/hepatic/cardiac failure. They were also excluded if they needed to walk or cycle to another work site during the day.
Ethical approval was obtained from the Imperial College Research Ethics Committee (ICREC 13/6/5).
Measurement Tools
Ultrasound: A clinical ultrasound system (Philips iU22 xMATRIX) and an L9–L3 vascular venous linear transducer with venous protocol were used. The GSV of the right leg was identified, and reflux (> 0.5 second) was excluded using a series of calf squeezes with color Doppler evaluation. A section of vein two fingers breadth below the knee joint was identified and marked. If this section was extrafascial, then the left leg was used. Two orthogonal diameter measurements were taken, and an average calculated. Two researchers measured ultrasound GSV diameters. Reproducibility readings of orthogonal diameter measurements were taken, two sets of 15 consecutive readings for each observer. Coefficients of variation (n = 30) were 3.61 and 2.75%. The intra- and interobserver Bland Altman graphs are shown in Fig. 1.
Fig. 1.
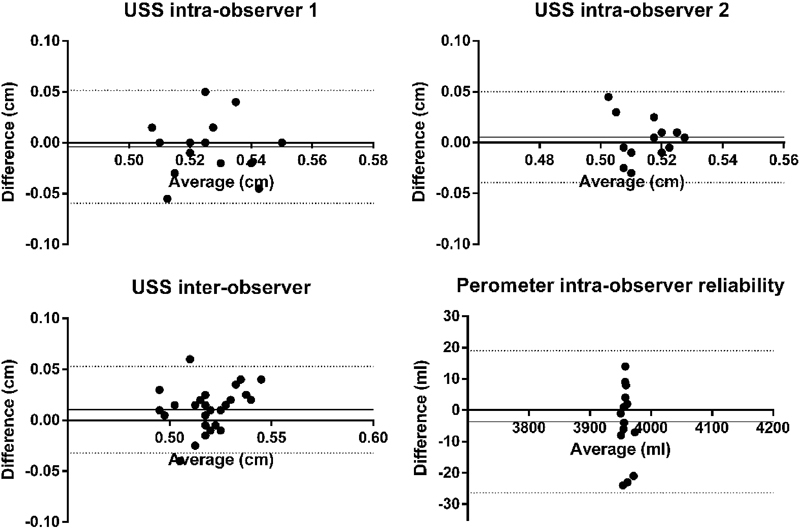
Bland–Altman graphs for both ultrasound and perometer measurements. USS, ultrasound scans.
For the protocol, three repeat sets of measurements of were recorded and averaged, as per Abraham et al.9 The trial room conditions were kept as constant as possible, without the facility for climate control.
Perometer: The perometer is an optoelectric limb volume measurement system (type 35 S, Pero-system Messgeräte GmbH, Germany, using PeroPlus 2000 software). It uses a circular arrangement of infrared light transmitters and photosensors on a rigid frame to create an electronic image of the presented limb.10 The perometer has been previously validated for limb volume measurements.11 The subjects were seated on a standard office chair, positioned with their leg extended and foot placed flat on the footplate. Care was taken to minimize space between sole and footplate, and relax the leg as much as possible to minimize leg muscle contraction. A baseline scan was taken and the length of footplate to middle of patella noted. All successive measurements of volume used this length value as a standardized cutoff, particular to that trial subject. One observer took all perometer scans. Reliability testing coefficient of variation (n = 30) was 0.2%, and intraobserver Bland–Altman plots are shown in Fig. 1. For the protocol, five repeat measurements were taken for each scan and averaged.
Devices
Graduated Compression Stockings
Compression stockings (Active Compression Socks, Mediven, United Kingdom): These grade 2 graduated below-knee stockings were fitted according to manufacturer's instructions, on the appropriate test day, applied immediately after the morning scans. They were removed at the time of the evening scan.
NMES 1
The geko T-1 (Firstkind Ltd, United Kingdom) is a small, disposable, internally powered, neuromuscular stimulation device (27 mA, 1Hz, 70–560 µs pulse width). Applied transcutaneously, it stimulates the common peroneal nerve as it wraps around the neck of the fibula, thereby engaging the foot and calf venous muscle pumps (tibialis anterior, peroneus longus, and lateral gastrocnemius). A device was worn on each leg for 4 hours at the minimum level to stimulate definite dorsiflexion movement of the foot, as per manufacturer's instructions.
NMES 2
Revitive IX device with Isorocker (Actegy Ltd, United Kingdom) induces contraction of the muscles of the foot and calf through the plantar surface of the feet when rested on a set of footpads. The device delivers a 30-minute program of pulses with varying frequencies (range, 20–50 Hz), patterns, and durations (range, 4–9 seconds). Ankle movement is facilitated by passive device rocking (± 15 degree forward and backward tilt relative to the central axis of the footpad) when calf muscles contract. Stimulation intensity was zeroed, and then increased until muscle contraction occurred (motor threshold). The preprogrammed stimulation cycle of 30 minutes was applied during the trial subject's lunch break, at double motor threshold intensity (or if not tolerated, then at the maximum tolerated level).
Protocol
The first scan of the day was performed in the morning after arrival at work, followed by a second set of readings 6 hours later, or before leaving work. Subjects were positioned standing upright with a nonweight-bearing heel, and GSV diameter measurements were taken. Subjects were then seated, and the volume of the same leg was measured. The first day was taken as a control. Over subsequent days different interventions were applied in different orders (subject-to-subject) in an effort to reduce application (Table 1).
Table 1. Order of device applicationa .
| Subject | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
|---|---|---|---|---|---|---|---|---|---|---|
| Day 1 | Control | Control | Control | Control | Control | Control | Control | Control | Control | Control |
| Day 2 | GCS | NMES1 | NMES1 | NMES2 | GCS | NMES1 | NMES2 | NMES2 | GCS | NMES1 |
| Day 3 | NMES1 | GCS | NMES2 | GCS | NMES2 | GCS | NMES1 | GCS | NMES1 | NMES2 |
| Day 4 | NMES2 | NMES2 | GCS | NMES1 | NMES1 | NMES2 | GCS | NMES1 | NMES2 | GCS |
Abbreviations: GCS, graduated compression stockings; NMES, neuromuscular electrical stimulation.
NMES1, bilateral geko application; NMES2: Revitive.
Preference Questionnaire
On completion of the protocol subjects were asked to rate the three devices in order of preference in the following domains: comfort, ease of use, and perceived effectiveness; scale 3 (best) to worst (1). This was then scaled to a percentage.
Statistical Analysis
All statistical analyses were performed using Prism 6 (Graphpad Software Inc., CA, version 6.01), on an intention-to-treat basis, with significance taken at p < 0.05.
Results
Four females and six males were recruited, screened, and completed the protocol in full. Participants had a mean age 29.2 years, and body mass index 25.3 kg/m2. Time between scans varied according to subject workload and schedule, mean 371 minutes ± 43 (standard deviation).
In one subject, NMES1 was unable to elicit dorsiflexion, despite multiple fitting attempts. This could not be linked to any anatomical variation seen on ultrasound or known physiological abnormality.
Morning measurements of leg volume and GSV diameter varied over 4 days, maximum coefficients of variation 1.58 and 19.5%, respectively. Absolute change in leg volume over control days was median 41 mL (interquartile range [IQR], 7.7–74.0; p = 0.01; Wilcoxon-matched pairs signed rank). Absolute change in GSV diameter over the control day was −0.4 mm (range, −1 to 0.4; p = 0.32).
When compared with control, leg volumes changed by −1.7% (p < 0.01, Mann–Whitney U-test), −0.06% (ns) and −0.22% (ns) in the GCS, NMES1, and NMES2 groups respectively; while GSV diameters decreased by 2.5% (ns), 3.1% (ns), and 8.5% (ns), respectively (Table 2). Correlation of percentage changes in GSV diameter and leg volume was poor (Spearman r = 0.10, p = 0.56), and is shown graphically in Fig. 2.
Table 2. Change in measurements over trial protocola .
| Absolute leg volume change (mL) | Percentage change relative to control | GSV diameter absolute change (mm) | Percentage change relative to control | |
|---|---|---|---|---|
| Control | 41.0 (7.7 to 74.3) | −0.4 (−1 to 0.4) | ||
| GCS | −16.6 (−52.2 to 20.3) | −1.7** | −0.2 (−0.6 to 0.4) | 2.51 |
| NMES 1 | 40.6 (7.5 to 80.5) | −0.06 | −0.3 (−0.4 to 0.5) | 3.13 |
| NMES 2 | 30.7 (5.9 to 66.1) | −0.22 | −0.1 (−0.8 to 0.2) | 8.48 |
Abbreviations: GCS, graduated compression stockings; GSV, great saphenous vein; NMES, neuromuscular electrical stimulation.
Median and interquartile range, **p < 0.01, Mann–Whitney U-test for significance compared with control.
Fig. 2.
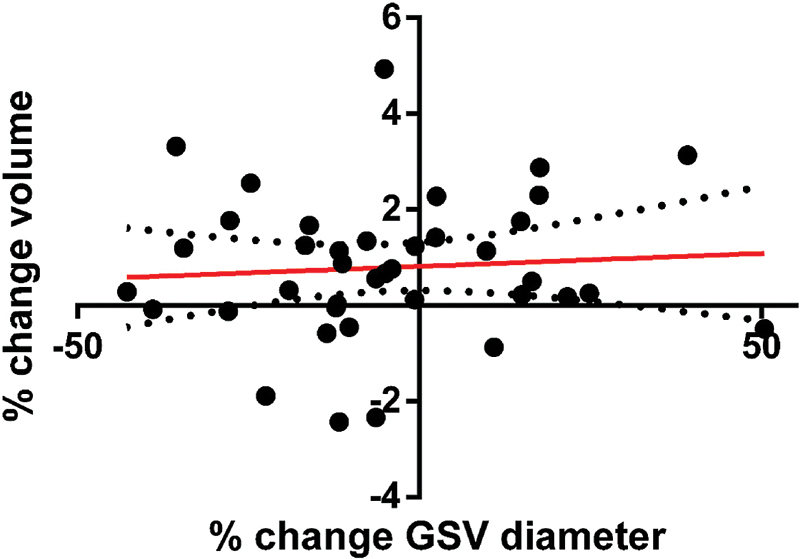
Percentage changes in great saphenous vein diameter plotted against percentage changes in leg volume. Line of best fit is shown (r 2 < 0.01) with 95% confidence intervals. GSV, great saphenous vein.
The results of preference questionnaires are shown in Table 3. GCS were preferred for subjective effectiveness and comfort, while NMES1 was felt to be easiest to apply and operate.
Table 3. Summed subject preference scores for the devicesa .
| Comfort | Ease of use | Effectiveness | |
|---|---|---|---|
| GCS | 47 | 32 | 47 |
| NMES1 | 28 | 36 | 28 |
| NMES2 | 25 | 32 | 25 |
| Total | 100 | 100 | 100 |
Abbreviations: GCS, graduated compression stockings; NMES, neuromuscular electrical stimulation.
Expressed as percentages.
Discussion
This study has shown that over a representative sedentary office-based working day, there is a significant change in leg volume in healthy individuals, reproducing results from other studies.1 This can be attributed to decreased movements of the leg with insufficient calf muscle pump activity.4 12
Occupational edema can be managed using medical devices such as compression stockings and neuromuscular devices, although there is little evidence in the literature to support this in a healthy population. They both promote calf muscle pump efficacy, peak venous velocity, and venous return, thereby reducing ambulatory venous pressures, interstitial fluid volume, and leg volume.5 6 13 14
Compression stockings were most effective at reducing percentage leg volume increase, with neuromuscular stimulation devices reducing swelling but not reaching statistical significance in this trial.
NMES cause muscular contraction of the calf muscle pump, above what would normally occur in an average sedentary working day, but body position may affect the efficacy of such measures. Flexed hips and knees may increase resistance to blood and lymph flow from the lower extremities. Compression stockings apply graduated pressure from the ankle to knee, both increasing interstitial space pressures, and assisting resistance to muscle expansion with contraction.15 This allows the calf muscle pumps to perform more efficiently, but relying on the wearer to activate the leg muscles. In an office-based environment, we expected NMES to outperform GCS because of the increased muscle activity. The two NMES devices are new to the market and still undergoing pilot trials, and as such, clear guidance on their most efficacious use has not been published. A different NMES protocol may give different results.
There is little to no correlation between GSV diameter and leg swelling, nor does it change significantly in any of the interventions compared with control. In our pilot trial, subjects were healthy, whereas the literature has shown relationships between GSV diameter and severity of clinical symptoms in populations with venous disease.7 8 In a trial population of healthy subjects with competent valves this relationship appears to be absent. This is supported by Barros et al, who have shown a strong correlation between severity of reflux analyzed using air plethysmography, and GSV diameter.16
Differences in tolerability of the devices did not lead to poor compliance, and all subjects completed the whole protocol. A preference for compression stockings in healthy subjects over NMES is noted, although this did vary from person to person.
Efforts were taken not to restrict normal subject activity over the working day, in an effort to produce results applicable to the general population. Common tasks performed during the day involved sitting at a desk typing, clinical duties in outpatient clinic (taking histories, clinical examination, and dictation), with minimal walking. Distances walked were not recorded. Fluid intake, bathroom breaks, environmental temperature and subject working position were not controlled, and this could have skewed our results. Overall, 40% of our sample was female, and variation in hormonal profile (particularly progesterone) may have had a confounding effect. Our small sample size also makes us prone to both types 1 and 2 statistical errors.
There are significant differences between the three medical devices tested here, and may be more suitable for certain lifestyles or population groups. GCS needs to be properly fitted to be efficacious, whereas the Revitive device can be used straight from the box. The geko can take a few minutes to position properly over the appropriate anatomical landmarks, and did not work in one of our healthy trial subjects. The reason for this is unknown. The Revitive requires the user to be stationary in a chair for 30 minutes, whereas the geko and GCS allow full mobility throughout. The two NMES devices work through slightly different mechanisms, one working anterograde through the common peroneal nerve, the other retrograde through the plantar muscles and plexus of nerves. This may or may not be significant in different populations. GCS reported compliance in chronic disease has been poor, often being described as uncomfortable and restrictive.17 18 The long-term tolerability of NMES device such as the geko and Revitive has yet to be evaluated. From small pilot trials using NMES in healthy subjects, it does seem that the maximum tolerated level does seem to be efficacious for producing maximum positive results while limiting discomfort.6 It has also been shown that exposure over time to neuromuscular stimulation leads to tolerance of higher stimulation settings and experience of lower levels of discomfort.19 However, in this trial, we did not explore a range or grade of stimulation settings allowing subjects to select their own intensity settings. This may have affected the comparison with GCS.
Previous studies combining NMES (DUO Stim or BMR Neurotech) with GCS have shown an additive enhancement of hemodynamic flow measurements.19 20 This may translate into added clinical benefit with combined use of NMES devices with GCS in future interventional trials.
Conclusion
In this pilot trial, all devices were well tolerated and reduced leg swelling. GCS were the only device to statistically reduce leg swelling in this small trial. Further evaluation of combinations of GCS and NMES devices are warranted, as are interventional trials in the management of venous and lymphatic disease.
Acknowledgments
This research was supported by the National Institute for Health Research (NIHR) Biomedical Research Centre, based at Imperial College Healthcare NHS Trust and Imperial College London. The views expressed are those of the authors and not necessarily those of the NHS, NIHR, or Department of Health. The research was funded by the European Venous Forum, Royal Society of Medicine, the Graham-Dixon Charitable Trust, and the Royal College of Surgeons of England. We also acknowledge Mediven, Firstkind Ltd, and Actegy Ltd, for providing the devices for the trial. The trial was registered at www.clinicaltrials.gov (NCT02241343).
Note
This article was previously presented as a poster at the Annual Meeting of the Society of Academic and Research Surgery, Durham, January 2015 (prize winner).
References
- 1.Blättler W, Kreis N, Lun B, Winiger J, Amsler F. Leg symptoms of healthy people and their treatment with compression hosiery. Phlebology. 2008;23(5):214–221. doi: 10.1258/phleb.2008.008014. [DOI] [PubMed] [Google Scholar]
- 2.Mosti G, Partsch H. Occupational leg oedema is more reduced by antigraduated than by graduated stockings. Eur J Vasc Endovasc Surg. 2013;45(5):523–527. doi: 10.1016/j.ejvs.2013.01.032. [DOI] [PubMed] [Google Scholar]
- 3.de Boer E M, Broekhuijsen R W, Nieboer C. et al. Lycra Support Tights: Are They Effective? Phlebology. 1999;14(4):162–166. [Google Scholar]
- 4.Jungbeck C, Peterson K, Danielsson G. et al. Effects of Compression Hosiery in Female Workers with a Standing Profession. Phlebology. 2002;16(3):117–120. [Google Scholar]
- 5.Partsch H Winiger J Lun B Compression stockings reduce occupational leg swelling Dermatol Surg 2004305737–743., discussion 743 [DOI] [PubMed] [Google Scholar]
- 6.Zhang Q, Styf J, Ekström L, Holm A K. Effects of electrical nerve stimulation on force generation, oxygenation and blood volume in muscles of the immobilized human leg. Scand J Clin Lab Invest. 2014;74(5):369–377. doi: 10.3109/00365513.2014.898323. [DOI] [PubMed] [Google Scholar]
- 7.Navarro T P, Delis K T, Ribeiro A P. Clinical and hemodynamic significance of the greater saphenous vein diameter in chronic venous insufficiency. Arch Surg. 2002;137(11):1233–1237. doi: 10.1001/archsurg.137.11.1233. [DOI] [PubMed] [Google Scholar]
- 8.Lane T RA, Shepherd A C, Gohel M. et al. Big Veins, Big Deal - Vein Diameter Affects Disease Severity, not Quality of Life. Journal of Vascular Surgery: Venous and Lymphatic Disorders. 2013;1:101. doi: 10.1016/j.jvsv.2012.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Abraham P, Leftheriotis G, Desvaux B, Saumet M, Saumet J L. Diameter and blood velocity changes in the saphenous vein during thermal stress. Eur J Appl Physiol Occup Physiol. 1994;69(4):305–308. doi: 10.1007/BF00392035. [DOI] [PubMed] [Google Scholar]
- 10.Tan C W, Coutts F, Bulley C. Measurement of lower limb volume: agreement between the vertically oriented perometer and a tape measure method. Physiotherapy. 2013;99(3):247–251. doi: 10.1016/j.physio.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Stanton A W, Northfield J W, Holroyd B, Mortimer P S, Levick J R. Validation of an optoelectronic limb volumeter (Perometer) Lymphology. 1997;30(2):77–97. [PubMed] [Google Scholar]
- 12.Hirai M, Iwata H, Miyazaki K. et al. Effect of gaiters on muscle pump activity in healthy volunteers. Phlebology. 2013;28(6):293–298. doi: 10.1258/phleb.2012.012007. [DOI] [PubMed] [Google Scholar]
- 13.Tucker A, Maass A, Bain D. et al. Augmentation of venous, arterial and microvascular blood supply in the leg by isometric neuromuscular stimulation via the peroneal nerve. Int J Angiol. 2010;19(1):e31–e37. doi: 10.1055/s-0031-1278361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Williams K, Moore H, Davies A. Haemodynamic changes with the use of neuromuscular electrical stimulation compared to intermittent pneumatic compression. Phlebology. 2015;30(5):365–372. doi: 10.1177/0268355514531255. [DOI] [PubMed] [Google Scholar]
- 15.Morris R J, Woodcock J P. Evidence-based compression: prevention of stasis and deep vein thrombosis. Ann Surg. 2004;239(2):162–171. doi: 10.1097/01.sla.0000109149.77194.6c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barros M V, Labropoulos N, Ribeiro A L, Okawa R Y, Machado F S. Clinical significance of ostial great saphenous vein reflux. Eur J Vasc Endovasc Surg. 2006;31(3):320–324. doi: 10.1016/j.ejvs.2005.08.017. [DOI] [PubMed] [Google Scholar]
- 17.Ziaja D, Kocełak P, Chudek J, Ziaja K. Compliance with compression stockings in patients with chronic venous disorders. Phlebology. 2011;26(8):353–360. doi: 10.1258/phleb.2010.010086. [DOI] [PubMed] [Google Scholar]
- 18.Raju S, Hollis K, Neglen P. Use of compression stockings in chronic venous disease: patient compliance and efficacy. Ann Vasc Surg. 2007;21(6):790–795. doi: 10.1016/j.avsg.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 19.Corley G J, Breen P P, Bîrlea S I, Serrador J M, Grace P A, Ólaighin G. Hemodynamic effects of habituation to a week-long program of neuromuscular electrical stimulation. Med Eng Phys. 2012;34(4):459–465. doi: 10.1016/j.medengphy.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 20.Lyons G M, Leane G E, Grace P A. The effect of electrical stimulation of the calf muscle and compression stocking on venous blood flow velocity. Eur J Vasc Endovasc Surg. 2002;23(6):564–566. doi: 10.1053/ejvs.2002.1652. [DOI] [PubMed] [Google Scholar]


