Abstract
Purpose
On RTOG 0630, a study of IGRT for primary soft tissue sarcomas of the extremity, six imaging modalities were used. We analyzed all daily patient-repositioning data collected in this trial to determine the impact of daily IGRT on CTV-to-PTV margin.
Methods and Materials
Daily repositioning data, including shifts in right-left (RL), superior-inferior (SI), anterior-posterior (AP) directions and rotations, for 98 patients enrolled in RTOG 0630 from 18 institutions were analyzed. Patients were repositioned daily based on bony anatomy using the pretreatment images, including KV-orthogonal images (KVorth), MV-orthogonal images, KV fan-beam CT, KV cone-beam, MV fan-beam CT (MVCT), and MV cone-beam CT. Mean and standard deviations (SD) for each shift and rotation were calculated for each patient and for each IGRT modality. The t-tests and F-tests were performed to analyze the differences in the means and SDs. Necessary CTV-to-PTV margins were estimated.
Results
The repositioning shifts and day-to-day variations were large and generally similar for the 6 imaging modalities. Of the two most commonly used modalities, MVCT and KVorth, there were no statistically significant differences in the shifts and rotations (p=0.15 and 0.59 for RL and SI shifts, respectively, and p=0.22 for rotation), except for shifts in AP direction (p=0.002). The estimated CTV-to-PTV margins in RL, SI and AP directions would be 13.0, 10.4, and 11.7 mm from MVCT data, and 13.1, 8.6, and 10.8 mm from KVorth data, indicating that margins substantially larger than 5mm used with daily IGRT would be required in the absence of IGRT.
Conclusion
The observed large daily repositioning errors as well as the large variations among institutions imply that the daily IGRT is necessary for this tumor site, particularly in multi-institutional trials. Otherwise, a CTV-to-PTV margin of 1.5 cm is required to account for daily setup variations.
Introduction
Preoperative radiotherapy (RT) is one of the standard options in the management of soft tissue sarcoma (STS) of the extremities for improvement in local control. Clinical data indicate that preoperative RT with smaller treatment volumes results in reduced toxicity compared to postoperative RT (1–3). Advanced RT delivery technologies, such as image-guided radiotherapy (IGRT) and in particular image-guided intensity modulated radiotherapy (IG-IMRT), have the capability of delivering highly conformal doses to the targets while sparing the adjacent organs at risk (OAR) (4–6). During IGRT, patient treatment position is adjusted prior to the delivery of the radiation dose based on imaging acquired immediately prior to treatment delivery, minimizing interfractional variations including set up errors and anatomic changes. IGRT may benefit treatment of STS of the extremities as the extremity may not be in a rigid immobilization device during RT and daily setup error can be significant in irradiating sarcomas of certain sites. Moreover, a large field size is often required for conventional RT of extremity sarcoma so that sparing of the surrounding normal structures such as the adjacent normal tissues, bone, testis, femoral head/neck, external genitalia, anus, joints, spinal cord, lungs, kidneys, ovary, subcutaneous tissues and strip of skin is challenging. Thus, reducing targeting uncertainty (margin) during the delivery is highly desirable (7). It is conceivable that, by decreasing the margin required for setup error [margin from clinical target volume (CTV) to planning target volume (PTV)], IGRT could result in improved treatment outcomes by reducing side effects and improving quality of life. With this rationale, a multicenter phase II trial of preoperative IGRT for STS of the extremity, Radiation Therapy Oncology Group (RTOG) 0630 trial, was conducted. The primary endpoint of this trial was to determine the effect of reduced RT volume with IGRT on late radiation morbidity at 2 years from the start of RT. This trial was successfully completed in 2010 and a significant reduction of late toxicities was observed in a recent analysis of the outcome data collected in the trial (8).
Six different commonly available IGRT modalities were used in the RTOG 0630 trial among the 18 participating institutions. The purpose of this work is to analyze the daily patient-repositioning data collected in the trial to determine the impact of daily image guidance with the different IGRT technologies and to estimate CTV-to-PTV margins that would be required with and without IGRT.
Methods and Materials
A total of 98 patients were enrolled in RTOG 0630 trial from 18 institutions. Patients were treated with IGRT using six commonly-available imaging modalities: (i) kilovoltage (KV) fan-beam CT (KVCT), (ii) megavoltage (MV) fan-beam CT (MVCT) (Tomotherapy, Accuray Inc, Sunnyvale, CA), (iii) KV cone-beam (KVCB), (iv) MV cone-beam (MVCB) (MVision, Siemens Med), (v) KV orthogonal images (KVorth), and (vi) MV orthogonal images (MVorth), which were used for a total of 12, 26, 6, 2, 45 and 7 patients, respectively. The first 4 modalities are 3-dimensional (3D) imaging, while the fifth and sixth are 2D imaging. Except for MVCT and MVCB, the other four modalities are available from multiple vendors.
Patients were immobilized in stable and comfortable positions to allow accurate repositioning from treatment to treatment and to minimize movement during treatments. In each treatment fraction, the patient was repositioned based on a rigid body registration of the bony anatomy adjacent to the gross tumor target between the planning CT and the daily image acquired immediately prior to the treatment using one of six imaging modalities. With use of daily image guidance, the daily set up errors should be small (< 5 mm) (6). The other inter- and intra-fraction variations (e.g., organ motion) should also be small due to the relatively rigid anatomy of the extremities. Based on these considerations, RTOG 0630 protocol used a small margin of 5 mm to expand the CTV to the PTV.
The daily patient repositioning data, including shifts in x (right-left, RL), y (superior-inferior, SI) and z (anterior-posterior, AP) directions and rotations in pitch, roll and yaw for patients were collected and analyzed in this study. The mean and standard deviations (SD) for each shift and rotation were calculated for each patient and for each IGRT modality. For the two most commonly used modalities, MVCT (26/98) and KVorth (45/98), t-test and F-test were performed to analyze the differences in their means and SDs. Based on the daily shift data (e.g., set up errors and anatomic changes), the margin (M) from CTV to PTV were estimated as (9):
| (1) |
where Σ is the combined standard deviation (SD) of all systematic variations, and σ is the combined SD of all setup random variations as
| (2) |
where σi (i = 1, 2, 3..) is the ith random error (e.g., setup error, anatomic motion). The same rule applies to Σ. This margin should be used in the absence of daily IGRT to account for the inter- and intra-fractional variations.
Results
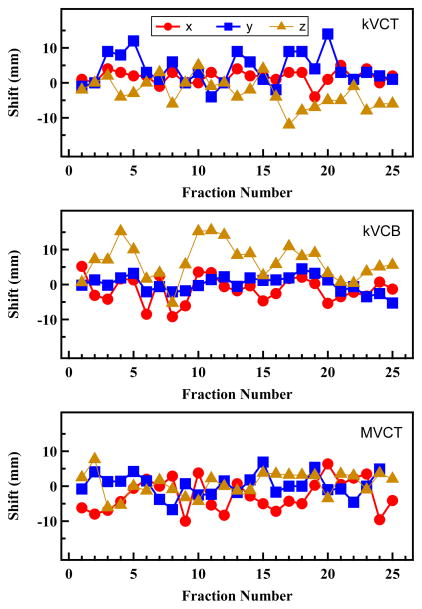
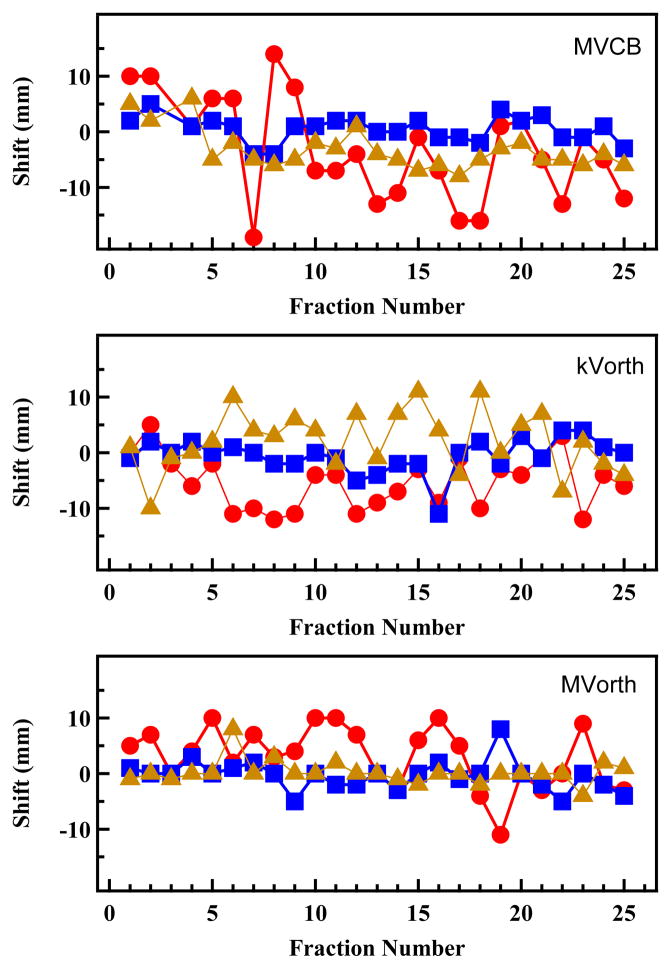
Figure 1 shows examples of daily translational shifts in the x, y and z directions for each of the six IGRT modalities for six representative cases, indicating that day-to-day set up errors of up to 20 mm could occur in one or more directions if image-guided patient repositioning was not performed.
Fig. 1.
Daily translational shifts in lateral (x), longitudinal (y) and vertical (z) directions for 6 IGRT modalities for 6 representative patients.
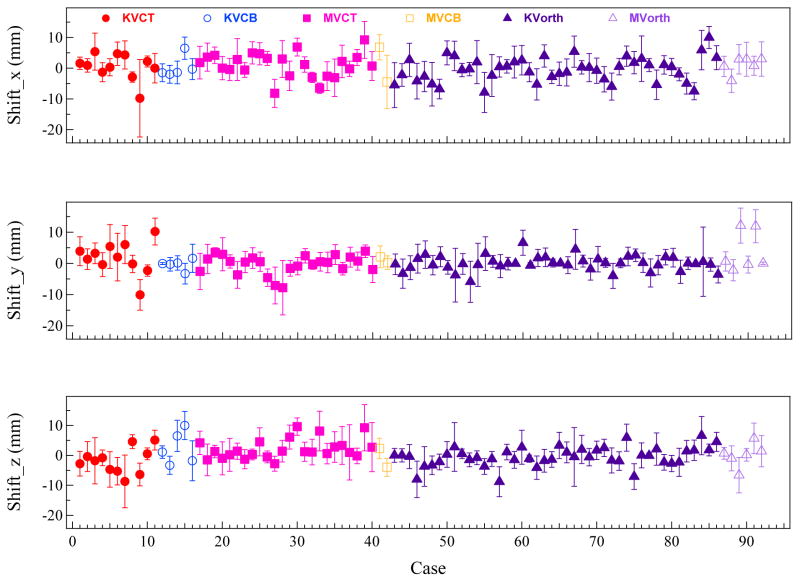
Figure 2 compares the average shifts in the x, y, and z directions for each patient during the entire course of treatment delivery for each of the six modalities. The mean set up errors are mostly less than 10 mm, and their values in the x and z directions are generally larger than those in the y (SI) direction. The large shift variations for different patients using the same imaging modality may be due in part to practice differences among the participating institutions.
Fig. 2.
A comparison of the mean shifts in righ-left lateral (x), superior-inferior (y), and anterior-posterior (z) directions for each patient during the entire course of treatment delivery between the six IGRT modalities.
Table 1 presents the means and SDs of daily repositioning shifts in the x, y and z directions for all patients treated with each of the six image modalities. Because the number of patients treated with four of the six imaging modalities is small, it was not possible to statistically compare the daily shift data for all six modalities, but there was no major difference between the data from the six IGRT modalities. For the two most commonly used modalities, MVCT (26 cases) and KVorth (45 cases), the mean ± SD of pitch rotations were −0.1±1.0 and 0.4±1.3 degree, respectively (not shown in Table 1). Between these two modalities, there was no statistically significant difference in the RL and SI shifts or rotations (p=0.15 and 0.59 for RL and SI shifts, respectively, and p=0.22 for rotation). Difference in the AP direction was statistically significant (2.2 vs −0.5 mm, p=0.002). The SDs between these two modalities are comparable, indicating that the both 2D/KV and 3D/MV imaging performed equally well for the IGRT of STS of the extremities and that alignment to bony anatomy rather than soft tissue may be sufficient.
Table 1.
Means and standard deviations (mean ± SD) of daily repositioning shifts in x, y, and z directions for all patients treated with each of the 6 image modalities.
| Modality | Right-Left (x) (mm) | Superior-Inferior (y) (mm) | Anterior-Posterior (z) (mm) |
|---|---|---|---|
| KVCT | 0.5±4.2 | 1.7±5.2 | −1.9±4.3 |
| KVCB | 0.35±3.5 | −0.4±1.8 | 2.5±5.6 |
| MVCT | 1.0±4.0 | −0.4±3.1 | 2.2±3.3 |
| MVCB | 1.1±8.0 | 1.2±1.3 | −0.9±4.4 |
| KVorth | −0.5±4.0 | 0.0±2.3 | −0.5±3.2 |
| MVorth | 1.0±2.7 | 3.7±6.5 | 0.1±4.0 |
Table 2 presents the systematic and random errors in x, y and z directions calculated based on the daily shifts for the six imaging modalities. The CTV-to-PTV margins estimated using Eqs. (1) and (2) based on these systematic and random errors were also included in the table. The margins based on the data for the two most commonly used imaging modalities, MVCT and KVorth, are statistically meaningful due to the sufficient number of cases used in the calculation with these two modalities. These data indicate that a margin of approximate 15 mm would be required if daily image guidance was not used in a multi-institutional study, which is substantially larger than the 5 mm margin used in the RTOG 0630 trial as a consequence of the daily IGRT. The use of IGRT in this trial permitted a smaller CTV to PTV expansion with greater sparing of adjacent normal tissues, resulting in the reduced toxicity as recently observed (8).
Table 2.
The systematic and random errors and the CTV-to-PTV margins in lateral (x), longitudinal (y) and vertical (z) directions, estimated based on the daily shifts for the 6 imaging modalities.
| IGRT Modality | Systematic Error (Σ) | Random Error (σ) | Margin | ||||||
|---|---|---|---|---|---|---|---|---|---|
| x(mm) | y(mm) | Z(mm) | x(mm) | y(mm) | z(mm) | x(mm) | y(mm) | z(mm) | |
| KVCT | 4.2 | 5.2 | 4.3 | 5.1 | 4.8 | 5.0 | 14.2 | 16.5 | 14.3 |
| KVCB | 3.5 | 1.8 | 5.6 | 3.3 | 2.9 | 4.6 | 11.1 | 6.5 | 17.3 |
| MVCT | 4.0 | 3.1 | 3.3 | 4.2 | 3.8 | 4.9 | 13.0 | 10.4 | 11.7 |
| MVCB | 8.0 | 1.3 | 4.4 | 6.8 | 2.9 | 3.2 | 24.6 | 5.3 | 13.2 |
| KVorth | 4.0 | 2.3 | 3.2 | 4.5 | 4.0 | 4.1 | 13.1 | 8.6 | 10.8 |
| MVorth | 2.7 | 6.5 | 4.0 | 4.5 | 3.8 | 4.4 | 10.0 | 19.0 | 13.0 |
Discussions
Soft-tissue sarcomas of the extremity are rare tumors that can be challenging to treat. In this secondary analysis of RTOG 0630, we observed significant inter-institutional variation in set-up errors that were corrected with daily IGRT. These results emphasize the importance of optimal immobilization for extremity sarcomas and suggest that in many institutions daily IGRT is needed unless large (1.5 cm) CTV to PTV margins are employed, which would likely increase long-term toxicity (8).
The data generated in this analysis are limited by the relatively small number of patients enrolled in the study. In addition, the daily rotation corrections which were submitted by some, but not all participating institutions. Although the image registration software tools used by these institutions can directly provide the rotation correction angles based on the image registration, these rotation corrections (mostly in the pitch direction) were not actually performed prior to treatment for practical reasons (e.g., lack of capacity of 6 degree of freedom on the treatment couch. To calculate the translational shifts, the rotation corrections should be set to zero. However, as the rotation corrections were mostly less than 1.5 degrees based on the collected data, the associated errors in patient position and the impact on CTV-to-PTV margin should be small.
In the absence of IGRT, we estimate that a CTV to PTV margin of 1.5 cm would be necessary to adequately cover the CTV based on the MVCT and KVorth data in Table 2, which have sufficient sample sizes for statistical analysis. The estimate of a 1.5 cm uniform PTV margin assumes that no IGRT is performed. In routine clinical practice, however, weekly IGRT is commonly utilized even if daily IGRT is not used. It is possible that with less-frequent use of IGRT a PTV margin less than 1.5 cm would be sufficient.
The data indicate that both KVorth and MVCT imaging modalities performed equally well for IGRT of STS of the extremities. Based on this observation, a simple IGRT modality with less radiation exposure may be considered for daily IGRT of this tumor site. If a 2D modality (e.g., KVorth) is used daily, a 3D IGRT modality (e.g., KVCT, KVCB, MVCT) may be performed less frequently (e.g., weekly) to assess tumor growth or shrinkage that may prompt adaptive planning.
Conclusions
The setup errors and their daily variations during the delivery of radiation therapy for soft tissue sarcoma of the extremities were large in this multi-institutional study. Daily image-guided repositioning with one of the available imaging modalities can substantially reduce setup errors and day-to-day variations justifying daily IGRT as necessary when a 5 mm margin is utilized. The 2D (KVorth) and 3D (MVCT) imaging modalities performed equally well. For extremity STS, simple IGRT modality with low radiation exposure such as 2D/KV may be considered for daily repositioning. However, 3D imaging remains appropriate to image soft tissue sarcomas to assess for tumor growth or shrinkage that may require re-planning. If daily IGRT is not used, a large CTV-to-PTV margin of 1.5 cm would be required to account for the large inter-and intra-fractional variations due to daily setup errors and anatomic changes.
Acknowledgments
This project was supported by grants U10CA21661, U10CA180868, U10CA180822, U10 CA37422, U24CA180803 from the National Cancer Institute (NCI).
Footnotes
This work was presented in part at the 2014 American Society for Radiation Oncology Annual Meeting.
Conflict of interest: none
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Davis AM, O’Sullivan B, Turcotte R, et al. Late radiation morbidity following randomization to preoperative versus postoperative radiotherapy in extremity soft tissue sarcoma. Radiother Oncol. 2005;75(1):48–53. doi: 10.1016/j.radonc.2004.12.020. [DOI] [PubMed] [Google Scholar]
- 2.O’Sullivan B, Davis AM, Turcotte R, et al. Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. Lancet. 2002;359(9325):2235–41. doi: 10.1016/S0140-6736(02)09292-9. [DOI] [PubMed] [Google Scholar]
- 3.O’Sullivan B, Griffin AM, Dickie CI, et al. Phase 2 study of preoperative image-guided intensity-modulated radiation therapy to reduce wound and combined modality morbidities in lower extremity soft tissue sarcoma. Cancer. 2013;119(10):1878–84. doi: 10.1002/cncr.27951. [DOI] [PubMed] [Google Scholar]
- 4.Jaffray DA. Emergent technologies for 3-dimensional image-guided radiation delivery. Semin Radiat Oncol. 2005;15:208–16. doi: 10.1016/j.semradonc.2005.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Mackie TR, Kapatoes J, Ruchala K, et al. Image guidance for precise conformal radiotherapy. Int J Radiat Oncol Biol Phys. 2003;56:89–105. doi: 10.1016/s0360-3016(03)00090-7. [DOI] [PubMed] [Google Scholar]
- 6.Li XA, Qi XS, Pitterle M, Kalakota K, Mueller K, Jursinic PA, Erickson BA, Wang D, Schultz CJ, Firat SY, Wilson JF. Inter-fractional variations in patient setup and anatomic change assessed by daily CT from helical tomotherapy. Int J Radiat Oncol Biol Phys. 2007;68:581–591. doi: 10.1016/j.ijrobp.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 7.Bradley J, Kainz K, Li XA, DeLaney T, Wang D. The Role of Image Guided Radiotherapy in the Treatment of Soft Tissue Sarcoma. Cancer Therapy Review. 2010;6(3):207–213. [Google Scholar]
- 8.Wang D, Zhang Q, Eisenberg BL, Kane JM, Li XA, Lucas D, Petersen IA, DeLaney TF, Freeman CR, Finkelstein SE, Hitchcock YJ, Bedi M, Singh AK, Dundas G, Kirsch DG. Significant Reduction of Late Toxicities in Patients With Extremity Sarcoma Treated With Image-Guided Radiation Therapy to a Reduced Target Volume: Results of Radiation Therapy Oncology Group RTOG-0630 Trial. J Clin Oncol. 2015 Feb 9; doi: 10.1200/JCO.2014.58.5828. pii: JCO.2014.58.5828 Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Van Herk M, Remeijer P, Rasch C, Lebesque JV. The probability of correct target dosage: dose-population histograms from deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys. 2000;47:1121–1135. doi: 10.1016/s0360-3016(00)00518-6. [DOI] [PubMed] [Google Scholar]