Abstract
Various types of shunt valves have been developed during the past 50 years, most of which can be classified into the following categories: (1) fixed differential pressure valves; (2) fixed differential pressure (DP) valves with an antisiphon mechanism; (3) programmable DP valves; (4) programmable DP valves with an antisiphon mechanism; and (5) programmable antisiphon valves. When considering the myriad of possible postoperative condition changes, such as the onset of accidental non-related diseases or trauma in adults, and changes in normal physiological development or anticipation of future shunt removal in children, it has become standard to use the programmable valve as a first choice for cerebrospinal fluid shunting. However, it is still unclear what type of shunt valve is suitable for each individual case. Based on the results of SINPHONI and more recently SINPHONI 2 trials, the programmable DP valve is recommended as the first line shunt valve. The programmable DP valve with an antisiphon mechanism is thought to be beneficial for tall, slender patients, who have a tendency for easily developing complications of overdrainage, however, this type of valve must be used cautiously in obese patients because of the increased risk of underdrainage. Although the current evidence is still insufficient, the programmable antisiphon valve, which costs the same as the programmable DP valve, is also thought to be the first line shunt valve. The quick reference table is applicable for most shunt valves, and for patients with either the ventriculoperitoneal or the lumboperitoneal shunt.
Keywords: cerebrospinal fluid shunting, programmable shunt valve, antisiphon mechanism, hydrocephalus, quick reference table
Introduction
Cerebrospinal fluid (CSF) shunting is one of the oldest neurosurgical procedures, first developed in ancient Greece. Since then, various trials of CSF shunting have been attempted, all resulting in poor outcomes. The history of shunting has been described in previous articles.1,2) The modern shunt procedure was established in the 1960s, with the advent of silicone materials for catheters and valves. Shunt valves at that stage can be categorized as fixed differential pressure (DP) valves, which can be considered as the first generation valves.
Although the first generation valve brought acceptable surgical outcomes, management of the siphon effect was recognized as a necessity for further improvement of shunt outcome. For this purpose, two different types of shunt valves were developed which were classified as the second generation valves. One was the programmable DP valve (Sophy valve and Sophysa Polaris valve (SPV), Sophysa, Orsay, France; Codman-Hakim programmable valve (CHPV), Codman and Shurtleff, Ryanham, Massachusetts, USA; Strata no siphon control (NSC) valve, Medtronic Neurosurgery, Goleta, California, USA), and the other was the DP valve with an antisiphon mechanism [Orbis-Sigma valve, Integra NeuroSciences, Sophia Antipolis, France; Dual switch valve (DSV), Aesculap-Miethke, Potsdam, Germany; Delta valve, Medtronic Neurosurgery; Gravity assisted valves (GAVs), Aesculap-Miethke].
Before long, the two mechanisms of the second generation valves were united into a programmable DP valve with an antisiphon mechanism (CHPV with siphon guard (CHPV-SG), Codman and Shurtleff; Strata II valve, Medtronic Neurosurgery; and ProGAV, Aesculap-Miethke), which can be classified as the third generation valve.
Recently, the antisiphon mechanism has become controllable (ProSA, Aesculap-Miethke), which should rightly be classified as the fourth generation valve.
Incidentally, later generation valves do not directly equate with a better functioning valves. Rather, the most important thing to consider when choosing valves is to select the type of valve on an individual basis according to the type of hydrocephalus in each patient as well as the anticipated postoperative management needs. In this article, I want to describe the unique characteristics of each valve and respective recommendations for its management.
Valve Characteristics
The shunt valve intrinsically functions as a kind of resistance mechanism within the shunt system, which serves to control intracranial pressure (ICP) in patients with hydrocephalus. The main characteristics of each valve are shown as follows:
I. First generation valves: the fixed DP valve
This conventional type of valve usually has three DP ranges (low, medium, and high), which in fact are thought to be insufficient for selecting a proper valve for each patient, and consequently the occurrence of inappropriate choice of DP valve typically results in shunt reoperation.
II. Second generation valves
A. The DP valve with antisiphon mechanism
1. Orbis-Sigma valve: This valve was designed to produce a constant flow (20–30 ml/hour) under a fixed range of DP (8–35 cmH2O).3) However, this feature may lead to underdrainage complications especially in patients with high pressure hydrocephalus.
2. Delta valve: This valve consists of a DP valve with a delta chamber which is a membrane type of antisiphon device. The DP valve has four pressure ranges described as performance levels (PLs) ranging from PL0.5, PL1.0, PL1.5, and PL2.0, which are equivalent to 1.5–2.5, 3.5–5.5, 7–9, and 10.5–12.5 cmH2O levels, respectively. The delta chamber provides an additional source of resistance (about 1.5 cmH2O) in the upright position. The ratio of inlet and outlet area in the delta chamber is designed as 20:1 in order to avoid underdrainage.
3. Dual switch valve: This valve has high and low pressure chambers. In the upright position, the high pressure circuit is activated by blocking the low pressure circuit by a tantalum ball dropping with gravity. Three types of functioning pressures are designated for each chamber (10, 13, 16 cmH2O for the low pressure chamber, and 30, 40, 50 cmH2O for the high pressure chamber).
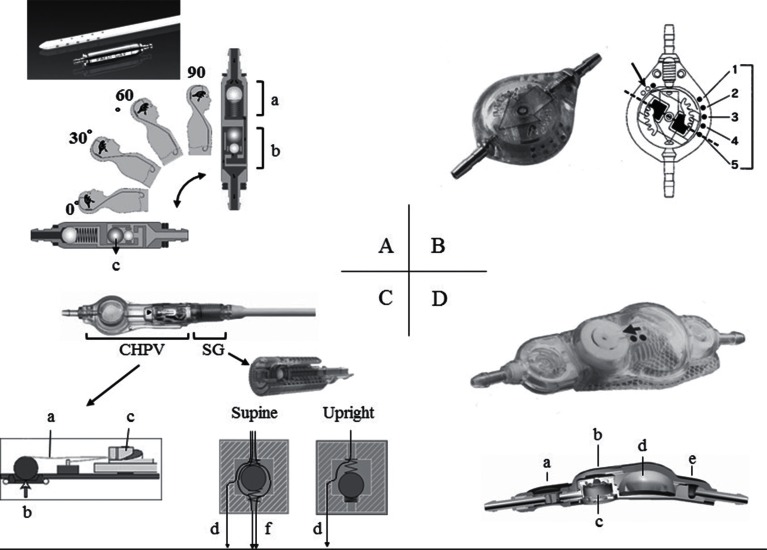
4. GAV (Fig. 1A): This valve is composed of a ball-in-cone valve and a gravity valve. The ball-in-cone valve acts as a DP valve. Two types of functioning pressures (4 and 9 cmH2O) are available. The gravity valve acts as an antisiphon device. Three types of the opening pressures (10, 15, 20 cmH2O) are available. Total opening pressure of GAV is described by the following formula: DP pressure + Sin “position angle” (0 degree (lying) to 90 degrees (upright)) × maximum pressure of gravity valve. Six types of GAV (4/14, 4/19, 4/24, 9/19, 9/24, 9/29 cmH2O) are in the lineup. The gravity valve part is also available as a solo device (shunt assistant: SA).
Fig. 1.
The outer appearance and cut surface of the popular shunt valves. A: Gravity assisted valve. a: Ball-in-cone valve, b: Gravity valve (SA: shunt assistant), c: Tantalum ball B: Sophysa Polaris valve (SPV). Arrow indicates the type of SPV. The right side dots indicate the pressure setting (1: lowest, and 5: highest). C: Codman Hakim Programmable Valve with Siphon Guard (CHPV-SG). a: Leaf spring, b: Ruby ball and Ruby seat, c: CAM, d: Second pathway, e: Main pathway D: Strata II valve. a: Delta chamber, b: Distal occluder, c: Valve mechanism, d: Reservoir, e: Proximal occluder.
5. Siphon X (Sophysa): This valve employs a gravity type of antisiphon mechanism, providing 20 cmH2O of resistance only in the upright position.
B. Programmable (adjustable) DP valves
1. Sophy valve: This was the first programmable valve in the world. This valve has a ball-in-cone mechanism, where a ruby ball at the valve inlet, compressed by a leaf spring, acts as a shunt resistance. The strength of the leaf spring is magnetically changeable in eight steps by the position of a rotor.
2. SPV (Fig. 1B): This valve has a rocking mechanism, so that the pressure setting never changes even in 3.0 tesla magnetic fields. The standard SPV can be programmed in five steps (3, 7, 11, 15, 20 cmH2O) by the same mechanism as used in the Sophy valve. Other types of SPVs including the SPV-140 (1, 4, 8, 11, 14 cmH2O), SPV-300 (5, 10, 15, 22, 30 cmH2O), and SPV-400 (8, 15, 23, 33, 40 cmH2O) are also available. The pressure settings of the Sophy valve and SPV can be programmed and identified by an exclusive adjustment kit after implantation.
3. CHPV: This valve also has a ball-in-cone mechanism, where a ruby ball at the inlet of the valve is compressed by a leaf spring, which acts to provide shunt resistance. The DP of CHPV can be adjusted electromagnetically from 3 to 20 cmH2O by 1 cmH2O intervals (18 steps) using an exclusive programmer.
4. Strata NSC valve: This valve was developed by simply removing the delta chamber from the Strata II valve. The DP valve in this system can be magnetically programmed in five steps (PL0.5, PL1.0, PL1.5, PL2.0, and PL 2.5). Each PL is equivalent to 1.5–3.5, 3.5–5.5, 9–11, 14.5–16.5, and 20–22 cmH2O, respectively. These settings are relatively higher than those of the Strata II valve. The pressure settings for the valve can be programmed and identified by an exclusive instrument (Varius system).
III. Third generation valves: programmable (adjustable) DP valves with antisiphon mechanisms
1. CHPV with siphon guard (CHPV-SG, Fig. 1C): The siphon guard works as an overflow limiter. The main pathway of the SG begins to close by excessive CSF flow (beyond approximately 1 ml/min) and CSF is drained toward the second pathway running along the SG wall spirally. Until the main pathway is completely closed, the SG acts as an additional resistor regardless of the patient’s posture. Because the shunt flow in the stable condition is approximately 0.6 ml/min, the SG is thought to offer additional resistance rather than serve as an overflow limiter.
2. Strata II valve (Fig. 1D): This valve can be described as a programmable Delta valve. The mechanism of the DP valve is the same as with the Strata NSC valve. Each PL is equivalent to 1.5–2.5, 3.5–5.5, 7–9, 10.5–12.5, and 13.5–15.5 cmH2O, respectively. The delta chamber provides additional resistance (about 1.5 cmH2O) for each PL in the upright position. The pressure settings of the valve can be adjusted and identified by the Varius system.
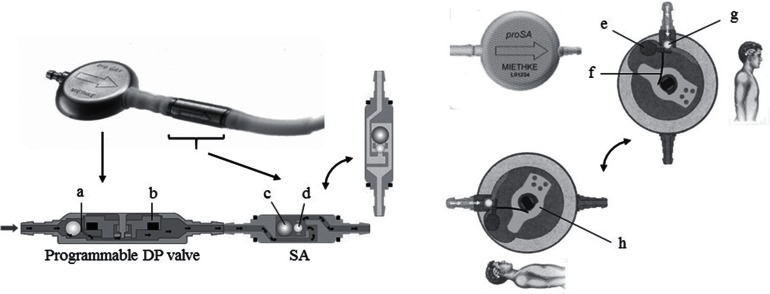
3. ProGAV (Fig. 2 left): This valve is composed of a programmable DP valve and SA. The DP valve can be programmed in 21 steps (0–20 cmH2O in 1 cmH2O intervals) magnetically. The SA acts as an antisiphon device. Six types of maximum opening pressures, 10, 15, 20, 25, 30, and 35 cmH2O, are currently available. ProGAV also has a rock mechanism, which is stable under 3.0 tesla magnetic fields. Valve pressure can be identified and programmed using the exclusive pencil-type instrument. ProGAV 2.0 is a newly developed valve, in which the rocking mechanism contains a modified version of the ProGAV. In order to reset the ProGAV 2.0, a doughnut-type exclusive adjustment tool is applied to the valve, which aligns the target value of opening pressure with the direction of the valve inlet, and then the center of the valve is compressed by manual finger compression. With this maneuver, the rocking mechanism is released, and the opening pressure is set to the target value. Release of the rocking mechanism is confirmed by an auditory clicking sound and a tactile finger sensation. The pencil-type adjuster for the ProGAV also can be used for the ProGAV 2.0.
Fig. 2.
The outer appearance and cut surface of the ProGAV (left) and ProSA (right). SA: shunt assistant. a: Spring, b: Magnet, c: Tantalum ball, d: Sapphire ball, e: Tantalum ball, f: Leaf spring, g: Sapphire ball, h: Rotor.
IV. Fourth generation valves: the programmable (adjustable) antisiphon valve
1. ProSA (Fig. 2 right): This is the first valve system which has the capability of programming for variable degrees of antisiphon control. When the rotor does not push the leaf spring connected to a tantalum ball, maximum gravity is obtained. Compression of the leaf spring increases by rotating the rotor, which acts to cancel the tantalum gravity. In this way, the opening pressure of the ProSA can be controlled continuously from 0 cmH2O to 40 cmH2O only in the upright position. Each opening pressure changes automatically from 0 cmH2O (in the recumbent position) to the maximum setting (in the upright position) depending on the postural angle. If the programmable DP valve is used in combination with the ProSA, the opening pressures in both the recumbent and upright positions can be controlled independently. ProSA also has a rocking mechanism, so the pressure setting is stable under 3.0 tesla magnetic fields. Valve pressure can be visualized and programmed using the exclusive pencil-type instrument for the ProSA. Characteristics of programmable shunt valves are summarized in Table 1. As for the Delta valve, Strata NSC valve, and Strata II valve, the Bioglide type (a type of hydrophilic processing) is also available. All programmable shunt valves settings can be adjusted within a certain depth under the skin. The standard workable depth for each valve is approximately 8–10 mm, however, these values are only reference data and not guaranteed by the manufactures.
Table 1.
Characteristics of programmable shunt valves available in Japan
| Type | Setting range (cmH2O) | Setting steps | Lock mechanism | MRI artifact *1 | Workable depth (mm) *2 | Antisiphon mechanism | Availability in LP shunt | |
|---|---|---|---|---|---|---|---|---|
| Sophy | SM8/SM8–140 SM8–300/SM8–400 |
3–20/1–14 5–30/8–40 |
8 | − | L | 10 | – | + |
| Polaris | SPV/ SPV-140 SPV-300/ SPV-400 |
3–20/1–14 5–30/8–40 |
5 | + | L | 8 | – | + |
| CHPV | Standard/in-line | 3–20 | 18 | − | S | 18 | – | + |
| CHPV-SG | Right angle/micro | 3–20 | 18 | − | S | 18 | Siphon guard | + |
| StrataNSC | Regular/small/LP | PL 0.5–2.5 | 5 | − | M | 10 | – | + |
| Strata II | Regular/small | PL 0.5–2.5 | 5 | − | M | 10 | Delta chamber | − |
| ProGAV | ProGAV/ProGAV2.0 | 0–20 | 21 | + | S-M | 10 | Shunt assistant | ± |
| ProSA | ProSA | 0–40 | continuous | + | S-M | 10 | ProSA | ± |
*1: S, M, L means small, medium, and large respectively,
*2: values are reference data, and are not guaranteed by maker,
CHPV-SG: Codman-Hakim programmable valve siphon guard, GAV: gravity assisted valve, LP: lumboperitoneal, MRI: magnetic resonance imaging, NSC: no siphon control, PL: performance level, SPV: Sophysa Polaris valve.
Postural Changes in ICP and Shunt Flow
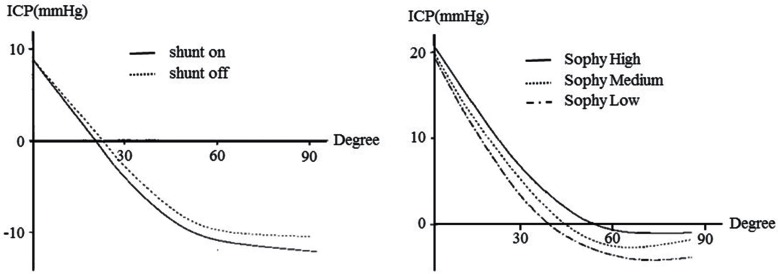
The authors previously reported on the postural ICP changes among patients with shunt-off, Sophy high, Sophy medium, and Sophy low settings,4) as shown in Fig. 3. The ICP decreases rapidly with postural changes from the recumbent position (0 degree) to the upright position (90 degrees), even in the shunt-off condition (Fig. 3 left). The ICP in the upright position becomes lower as the Sophy valve setting is lowered (Fig. 3 right). There may be some misunderstandings that excessive shunt flow continues throughout the upright position, which causes overdrainage symptoms. However, excessive shunt flow occurs just after postural change from the recumbent position to the upright position. Shunt flow decreases very quickly in accordance with a rapid ICP decrease and stabilizes around 0.6 ml/min, which is thought to be equal to the CSF production rate.
Fig. 3.
A comparison of postural ICP changes between shunt on and shunt off condition (left) and among Sophy high, medium and low conditions (right). (Revised from “Miyake H, Ohta T, Nagasawa S, et al: Clinical Experience with a New Ventriculo-Peritoneal Shunt Using a Telemetric Intraventricular Pressure Sensor, an On-Off Flushing Reservoir and a Sophy’s Programmable Hydrostatic Pressure Valve. Current Tr Hyd (Tokyo), 1991. 1: p. 79–84.”)
Basic Concepts for Shunt Control
The most important factor in shunt management is control of ICP, not shunt flow. Some consider that overdrainage symptoms are effectively controlled by preventing excessive shunt flow as a result of gradual decreases in ICP. However, shunt flow itself decreases very quickly without a flow regulating device and is self-limiting, never exceeding the CSF production rate during the stable postural condition. Furthermore, overdrainage symptoms do not occur during postural changes, rather they tend to occur during the stable upright conditions usually 20–30 minutes after postural changes, which proves that excessive shunt flow and speed of ICP decrease do not affect overdrainage symptoms. Even in healthy individuals without CSF shunting, ICP decreases rapidly with postural change (Fig. 3 left). Only excessive lowering of ICP in the stable condition after postural change to the upright position influences the occurrence of overdrainage symptoms. In our experience, overdrainage symptoms increase from the upright ICP below −30 cmH2O with reference to the frontal skull surface.
We formerly showed that the pressure environment of shunted patients in the upright position could be described by the following formula: perfusion pressure (PP) = hydrostatic pressure (HP) + ICP − intraabdominal pressure (IAP).5,6) The stable condition is thought to be a condition where PP equalizes with valve pressure. In other words, ICP decreases until PP becomes equal to valve pressure. Because PP and valve pressure are balanced, shunt flow in the stable condition is minimal, similar to titration at approximately 0.6 ml/min.
When setting the programmable DP valve, one DP value must be selected which is suitable for either the upright position or the recumbent position. The DP suitable for the upright position may cause underdrainage during sleep, and DP for the recumbent position may cause overdrainage in the upright position. Our concept is to select a DP setting suitable for the upright position, because people spend longer time in the upright position and overdrainage usually occurs in the upright position.6) The quick reference table (QRT, Table 2) was designed from the former equation, assuming HP from the patient’s height, IAP from the body mass index, and the ideal sitting ICP as −26 cmH2O in reference to the frontal skull surface.7) Consequently, the QRT must not be used for mostly recumbent bed-ridden patients.
Table 2.
Revised quick reference table for initial pressure setting of programmable differential pressure valve
| Men | BW (kg) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ht (cm) | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | 95 | 100 | 105 | 110 |
| 140 | 16 | 12 | 9 | 6 | 3 | |||||||||||
| 145 | 19 | 16 | 13 | 10 | 7 | 4 | ||||||||||
| 150 | 23 | 19 | 16 | 13 | 10 | 7 | 4 | |||||||||
| 155 | 26 | 23 | 20 | 17 | 14 | 12 | 9 | 6 | 3 | |||||||
| 160 | 29 | 27 | 24 | 21 | 18 | 16 | 13 | 11 | 8 | 5 | 3 | |||||
| 165 | 33 | 30 | 27 | 24 | 20 | 18 | 16 | 14 | 12 | 10 | 8 | 5 | 1 | |||
| 170 | 36 | 34 | 31 | 28 | 25 | 23 | 20 | 18 | 15 | 13 | 11 | 9 | 6 | 4 | ||
| 175 | 39 | 37 | 34 | 31 | 29 | 27 | 24 | 20 | 18 | 16 | 14 | 12 | 10 | 8 | 5 | 3 |
| 180 | 42 | 40 | 37 | 35 | 33 | 31 | 28 | 26 | 23 | 20 | 18 | 16 | 14 | 12 | 10 | 8 |
| Women | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BW (kg) | ||||||||||||||||
| Ht (cm) | 35 | 40 | 45 | 50 | 55 | 60 | 65 | 70 | 75 | 80 | 85 | 90 | 95 | 100 | 105 | 110 |
| 145 | 20 | 18 | 15 | 12 | 9 | 6 | 3 | |||||||||
| 150 | 23 | 20 | 18 | 15 | 12 | 9 | 6 | 4 | 1 | |||||||
| 155 | 26 | 23 | 21 | 19 | 16 | 14 | 11 | 8 | 5 | 3 | ||||||
| 160 | 29 | 27 | 24 | 21 | 19 | 17 | 14 | 12 | 9 | 6 | 4 | 1 | ||||
| 165 | 32 | 30 | 27 | 24 | 22 | 20 | 18 | 16 | 14 | 11 | 8 | 6 | 4 | 1 | ||
| 170 | 35 | 33 | 31 | 28 | 25 | 23 | 21 | 19 | 16 | 14 | 12 | 10 | 7 | 5 | 2 | |
| 175 | 38 | 36 | 34 | 31 | 29 | 27 | 25 | 23 | 20 | 18 | 16 | 14 | 12 | 10 | 7 | 5 |
| 180 | 41 | 39 | 37 | 34 | 32 | 30 | 28 | 25 | 23 | 21 | 19 | 17 | 15 | 13 | 11 | 9 |
| 185 | 44 | 41 | 39 | 37 | 35 | 33 | 31 | 29 | 26 | 24 | 22 | 20 | 19 | 18 | 16 | 15 |
All quick reference table values are shown in cmH2O. Bold: original part, others: new postscription calculating by the original method, BW: body weight, Ht: height.
Revised from Miyake H, Kajimoto Y, Tsuji M, Ukita T, Tucker A, Ohmura T: Development of a quick reference table for setting programmable pressure valves in patients with idiopathic normal pressure hydrocephalus. Neurol Med Chir (Tokyo) 48: 427–432, 2008.
Various approaches for determining the initial pressure of programmable DP valves have been reported. Reinprecht et al.8) and Bergsneider et al.9) recommended setting the opening pressure at the highest setting initially, followed by decreases depending on the patient’s clinical condition. This method is usually best for reducing overdrainage complications, however, hospitalization time may be prolonged, and symptoms remain unchanged until a suitable setting is achieved. Zemack et al. proposed setting the initial pressure based on the patient’s age, duration of the underlying disease, ventricular size, and results of the lumbar infusion test.10) This method is not strictly quantitative, and is too complicated and invasive for clinical use. In contrast to these methods, use of the QRT is very simple, and determination of the appropriate pressure value is performed by locating the intersecting value derived from the height in the horizontal axis with body weight in the vertical axis. The QRT has proven to be useful not only because of its ease of use but also because of favorable objective outcomes with less overdrainage complications as demonstrated in SINPHONI11,12) and SINPHONI-2.13)
Surgical methods and shunt valves
1. Ventriculoperitoneal (VP) shunt: All available shunt valves can be used with VP shunting. All valves except valves with membrane-type antisiphon mechanisms can be implanted in any location in VP shunts. Valves with membrane-type antisiphon mechanisms (Strata II valves and Delta valves) must be implanted in the retroauricular region, in order to achieve an adequate antisiphon effect.
2. Lumboperitoneal (LP) shunt: In Japan, use of LP shunts is increasing remarkably especially for the treatment of idiopathic normal pressure hydrocephalus. All valves except valves with a membrane-type antisiphon mechanism can be implanted in any location in LP shunts. Use of valves with membrane-type antisiphon mechanisms is unnecessary because the siphon effect is negligible in LP shunts. Valves with a gravity-type antisiphon mechanism (GAV, ProGAV, and ProSA) must be implanted along the vertical axis, which is difficult to apply for use in the LP shunt. All shunt valves for LP shunts, are recommended for implantation in the back, because excessive movement of the shunt valve with implantation in the abdomen can cause stress at the connection site between the lumbar catheter and the valve, resulting in lumbar catheter rupture, as well as dislodgement of both the lumbar catheter from the lumbar canal and abdominal catheter from the abdominal cavity. Furthermore, overturn of the valve in the subcutaneous tissue or excessively deep subcutaneous valve implantation may cause difficulties in postoperative setting changes.
3. Ventriculoatrial (VA) shunt: All shunt valves are available for VA shunts. However, the merit of the valve with a membrane-type antisiphon mechanism is minimal because the siphon effect itself is small in the VA shunt.
4. Lumbar subarachnoid-lumbar epidural (LL) shunt: Recently, Takeuchi et al. reported the usefulness of the LL shunt in patients with idiopathic normal pressure hydrocephalus.14) Although evidence for this surgical method is insufficient, the procedure can be completed under local anesthesia, which is beneficial for high risk patients. Valves with a membrane-type antisiphon mechanism are not recommended for use, because the siphon effect itself is minimal in this method. Takeuchi et al. recommended starting the CHPV setting at 20 cmH2O, since a higher setting of the programmable valve may be necessary because the lumbar epidural space is thought to have a negative pressure. The CHPV-SG, ProGAV, and ProSA are thought to be better for this purpose.
Postoperative Management of the Programmable Shunt Valve in Adults
The shunt environments of the VP shunt and the LP shunt are thought to be the same.15,16) Therefore the QRT is also applicable for patients with an LP shunt. In conditions when considerable amounts of subdural fluid collection/chronic subdural hematoma are observed, the valve setting must be raised immediately to the highest level. Otherwise, a pressure readjustment of 3 cmH2O/time is recommended.9,17)
In performing the LP shunt procedure there is a discrepancy in diameters between the puncture needle and lumbar catheter, which may result in side leakage.18) This is thought to be a cause of overdrainage immediately after surgery. Such overdrainage symptoms (mostly low pressure headache) usually resolve within a couple of days spontaneously, or by upward resetting of the shunt valve alone. Because of the possibility of this side leakage in patients with LP shunts, immediate postoperative setting at the highest level followed by resetting according to the QRT at discharge is an alternative solution.
Furthermore, the QRT can be applicable for the initial pressure setting of other programmable valves. As for the Strata II valve, the QRT can be used by making adjustments in reference to the opening pressure of each PL in the upright position.
The CHPV and use of the QRT for making appropriate shunt settings have shown favorable outcomes in SINPHONI.12) Likewise, most patients whose QRT value falls between 0 cmH2O and 20 cmH2O can be controlled well by the simple programmable DP valves or Strata II valve, both of which have almost the same opening pressure range as the CHPV in the upright position. The CHPV-SG which has slightly higher opening pressures may be better for patients whose QRT value falls between 15 cmH2O and 20 cmH2O, in order to allow for leeway in upward pressure resetting. For patients with QRT values of greater than 20 cmH2O, the use of ProGAV or ProSA may be an effective option.
As for the ProGAV, the opening pressure in the upright position is the sum of the programmable DP valve pressures and the SA pressure. The SA pressure is equivalent to the minimum opening pressure of the ProGAV in the upright position, so excessively high SA pressures may cause underdrainage. In my personal opinion, selection of an SA pressure which is close to the value of subtracting 10 from the QRT value [(QRT –10) cmH2O), is recommended in order to avoid underdrainage. After selection of that SA, next I recommend setting the programmable DP valve by subtracting the selected SA pressure from QRT value [(QRT value – SA pressure) cmH2O].
As for the ProSA, programmable SA pressure settings can be made using the QRT values. The opening pressure in the recumbent position is always 0 cmH2O with the ProSA alone. This is not a major problem, because overdrainage complications seldom occur in the recumbent position. On the other hand, most overdrainage and underdrainage complications are thought to be controllable by resetting alone, because SA pressure can be programmed from 0 cmH2O to 40 cmH2O continuously.
Medico-economic Evaluation of Shunt Valves in Japan
1. Comparison between fixed DP valves and programmable DP valves
In SINPHONI, 42 patients from 80 shunt responders underwent valve setting change during the follow-up period. Among these 42 patients, setting changes of more than 6 cmH2O/time were performed 19 times in 17 patients. Furthermore, among the remaining 25 patients, setting changes of more than 6 cmH2O compared to the initial setting were done in 2 patients. Assuming that the case with setting changes of more than 6 cmH2O requires reoperation with a programmable DP valve, these 19 (= 17 + 2) patients were thought to be the cases who required reoperation, if the patients in SINPHONI had undergone a shunt operation with a fixed DP valve initially. In Japan, the costs of a fixed DP valve and a programmable DP valve are 69,700 yen and 181,000 yen, respectively. Therefore if 80 patients are operated on with fixed DP valves, the initial valve costs are 8,904,000 yen less than the cases with programmable DP valves, however, 19 patients would require reoperation with a programmable DP valve, which would cost approximately 21,560,000 yen in our hospital (The average total cost for an LP shunt in our hospital was approximately 1,135,000 yen/patient in the last year. This fee varies slightly according to each hospital.). Considering these estimates, it can be concluded more economical to use a programmable DP valve in the initial shunt operation.
2. Comparison among programmable DP valves, programmable DP valves with antisiphon mechanisms, and programmable antisiphon valves
In SINPHIONI, all patients were treated by VP shunts with CHPV. In SINPHONI-2, all patients were treated by LP shunts with CHPV-SG. The percentage of patients with favorable outcome in both studies showed no significant difference (69% in SINPHONI and 63% in SINPHONI-2). Overdrainage complications in SINPHONI were observed in 18 cases (low pressure headache: 7, subdural fluid collection: 8, chronic subdural hematoma: 5), most of which improved only by upward resetting of the CHPV, and only 1 CSDH case required burr hole irrigation.11) On the other hand, overdrainage complications in SINPHONI-2 were observed in 25 cases (low pressure headache: 21, subdural fluid collection: 5, chronic subdural hematoma: 5), most of which improved only by upward resetting of CHPV-SG, and 3 cases of CSDH required burr hole irrigation.13) These results do not support the superiority of CHPV-SG compared with CHPV.
ProGAV shows better results in reducing overdrainage complications compared with CHPV in the SVASONA study,19) however, the study design is quite questionable. In this study, both ProGAV and CHPV were set at 10 cmH2O initially, and were decreased to 7 cmH2O at 3 months after VP shunt operation. In this design, the opening pressures of both valves in the recumbent position were the same, but the opening pressures in the upright position, which mostly affect overdrainage complications, were quite different. Consequently, if the initial CHPV pressure was chosen according to the QRT, the outcome of CHPV group would have been much better as the results showed in SINPHONI, and the outcomes of both groups would have shown no significant differences.
Because CHPV-SG and ProGAV (programmable DP valves with anti-siphon mechanisms) costs 67.100 yen higher than CHPV (simple programmable DP valve) in Japan, it is recommended to use them not for every patients, but for selected cases, such as tall, slender patients, who are thought to easily develop complications of overdrainage.
As for the ProSA, the opening pressure can be programmed between 0 cmH2O and 40 cmH2O continuously, which offers a wider range of controllability than other programmable valves and the cost is the same as the simple programmable DP valve. The ProSA may be useful as a first line shunt valve for cases using VP and VA shunts.20)
Conclusion
The characteristics of shunt valves available in Japan were described.
The programmable DP valve is recommended as a first line shunt valve not only because of its superior efficacy but also from a medico-economic standpoint.
The most important goal in shunt management is to control ICP, not to control shunt flow.
The QRT can be applied both in VP shunts and LP shunts.
Most shunt valves can be programmed using the QRT algorithm.
The ProSA is theoretically thought to be useful as a first line shunt valve.
References
- 1). Drake JM, Sainte-Rose C: The Shunt Book. Cambridge, Blackwell Science Inc, 1995. [Google Scholar]
- 2). Miyake H: The present status and problems associated with shunt treatment for hydrocephalus. Nervous System in Children 33: 507– 517, 2008. [Google Scholar]
- 3). Sainte-Rose C, Hooven MD, Hirsch JF: A new approach in the treatment of hydrocephalus. J Neurosurg 66: 213– 226, 1987. [DOI] [PubMed] [Google Scholar]
- 4). Miyake H, Ohta T, Nagasawa S, Takatsuka H, Yamashita M, Osaka K: Clinical experience with a new ventriculo-peritoneal shunt using a telemetric intraventricular pressure sensor, an on-off flushing reservoir and a Sophy’s programmable hydrostatic pressure valve. Current Tr Hyd (Tokyo) 1: 79– 84, 1991. [Google Scholar]
- 5). Kajimoto Y, Ohta T, Miyake H, Matsukawa M, Ogawa D, Nagao K, Kuroiwa T: Posture-related changes in the pressure environment of the ventriculoperitoneal shunt system. J Neurosurg 93: 614– 617, 2000. [DOI] [PubMed] [Google Scholar]
- 6). Miyake H, Ohta T, Kajimoto Y, Nagao K: New concept for the pressure setting of a programmable pressure valve and measurement of in vivo shunt flow performed using a microflowmeter. Technical note. J Neurosurg 92: 181– 187, 2000. [DOI] [PubMed] [Google Scholar]
- 7). Miyake H, Kajimoto Y, Tsuji M, Ukita T, Tucker A, Ohmura T: Development of a quick reference table for setting programmable pressure valves in patients with idiopathic normal pressure hydrocephalus. Neurol Med Chir (Tokyo) 48: 427– 432; discussion 432, 2008. [DOI] [PubMed] [Google Scholar]
- 8). Reinprecht A, Czech T, Dietrich W: Clinical experience with a new pressure-adjustable shunt valve. Acta Neurochir (Wien) 134: 119– 124, 1995. [DOI] [PubMed] [Google Scholar]
- 9). Bergsneider M, Black PM, Klinge P, Marmarou A, Relkin N: Surgical management of idiopathic normal-pressure hydrocephalus. Neurosurgery 57: S29– S39; discussion ii–v, 2005. [DOI] [PubMed] [Google Scholar]
- 10). Zemack G, Romner B: Adjustable valves in normal-pressure hydrocephalus: a retrospective study of 218 patients. Neurosurgery 51: 1392– 1400; discussion 1400–1402, 2002. [PubMed] [Google Scholar]
- 11). Hashimoto M, Ishikawa M, Mori E, Kuwana N, Study of INPH on Neurological Improvement (SINPHONI) : Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res 7: 18, 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12). Miyake H, Kajimoto Y, Murai H, Nomura S, Ono S, Okamoto Y, Sumi Y: Assessment of a quick reference table algorithm for determining initial postoperative pressure settings of programmable pressure valves in patients with idiopathic normal pressure hydrocephalus: SINPHONI subanalysis. Neurosurgery 71: 722– 728; discussion 728, 2012. [DOI] [PubMed] [Google Scholar]
- 13). Kazui H, Miyajima M, Mori E, Ishikawa M, SINPHONI-2 Investigators : Lumboperitoneal shunt surgery for idiopathic normal pressure hydrocephalus (SINPHONI-2): an open-label randomised trial. Lancet Neurol 14: 585– 594, 2015. [DOI] [PubMed] [Google Scholar]
- 14). Takeuchi T, Fukushima S, Misaki D, Shibata S: Lumbosubarachnoid-lumboepidural shunting in patients with idiopathic normal-pressure hydrocephalus: surgical procedures and follow-up study of five cases. Neurol Med Chir (Tokyo) 53: 638– 643, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15). Nakajima M, Miyajima M, Ogino I, Sugano H, Akiba C, Domon N, Karagiozov KL, Arai H: Use of external lumbar cerebrospinal fluid drainage and lumboperitoneal shunts with Strata NSC valves in idiopathic normal pressure hydrocephalus: a single-center experience. World Neurosurg 83: 387– 393, 2015. [DOI] [PubMed] [Google Scholar]
- 16). Tarnaris A, Toma AK, Watkins LD, Kitchen ND: Is there a difference in outcomes of patients with idiopathic intracranial hypertension with the choice of cerebrospinal fluid diversion site: a single centre experience. Clin Neurol Neurosurg 113: 477– 479, 2011. [DOI] [PubMed] [Google Scholar]
- 17). Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M, Nakajima M, Hashimoto M, Kuriyama N, Tokuda T, Ishii K, Kaijima M, Hirata Y, Saito M, Arai H, Japanese Society of Normal Pressure Hydrocephalus : Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir (Tokyo) 52: 775– 809, 2012. [DOI] [PubMed] [Google Scholar]
- 18). Kaijima M, Fukuda H, Yamamoto K: [Post-operative complications peculiar to lumboperitoneal shunt: possible consequences due to side leakage of CSF from around the inserted spinal tube into the lumbar epidural space]. No Shinkei Geka 39: 497– 504, 2011. [PubMed] [Google Scholar]
- 19). Lemcke J, Meier U, Müller C, Fritsch MJ, Kehler U, Langer N, Kiefer M, Eymann R, Schuhmann MU, Speil A, Weber F, Remenez V, Rohde V, Ludwig HC, Stengel D: Safety and efficacy of gravitational shunt valves in patients with idiopathic normal pressure hydrocephalus: a pragmatic, randomised, open label, multicentre trial (SVASONA). J Neurol Neurosurg Psychiatr 84: 850– 857, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20). Kehler U, Kiefer M, Eymann R, Wagner W, Tschan CA, Langer N, Rohde V, Ludwig HC, Gliemroth J, Meier U, Lemcke J, Thomale UW, Fritsch M, Krauss JK, Mirzayan MJ, Schuhmann M, Huthmann A: PROSAIKA: a prospective multicenter registry with the first programmable gravitational device for hydrocephalus shunting. Clin Neurol Neurosurg 137: 132– 136, 2015. [DOI] [PubMed] [Google Scholar]