Abstract
Multilocular thymic cysts are rare and acquired lesions induced by an inflammatory arising within the thymus. We report a rare case of multilocular thymic cyst with follicular lymphoid hyperplasia in a 59-year-old female. Chest CT and MRI revealed a large multilocular cystic mass, which contains thick septa and nodules in the thymus. F-18 FDG PET/CT showed almost no FDG uptake of the multilocular cystic mass but moderate FDG uptake of the solid nodules. Extended total thymectomy was performed. Histopathological findings revealed follicular lymphoid hyperplasia of thymic tissue but no neoplastic lesion. Based on these findings, diagnosis of multilocular thymic cyst with follicular lymphoid hyperplasia was made. This is a rare case that preoperatively was difficult to diagnose.
Keywords: Thymic cyst, Lymphoid hyperplasia, F-18 FDG, Positron-emission tomography, Computed tomography
Introduction
Thymic cysts account for 1 %–2 % of all anterior mediastinal masses, and most thymic cysts are congenital. Congenital cysts are typically unilocular and show no evidence of inflammation. Acquired thymic cysts, in contrast, result from an inflammatory process. They are usually multilocular, hence the commonly used term, multilocular thymic cyst [1]. Multilocular thymic cysts may be associated with other diseases, such as thymoma, thymic carcinoma, malignant lymphoma (including MALT lymphoma), Hodgkin lymphoma, germ cell tumor, HIV infection, or lymphoid hyperplasia [2, 3]. However, a preoperative diagnosis is difficult. Herein, we report a rare case of a multilocular thymic cyst with follicular lymphoid hyperplasia in a 59-year-old female, with radiologic findings on F-18 FDG PET/CT and histopathologic features.
Case Report
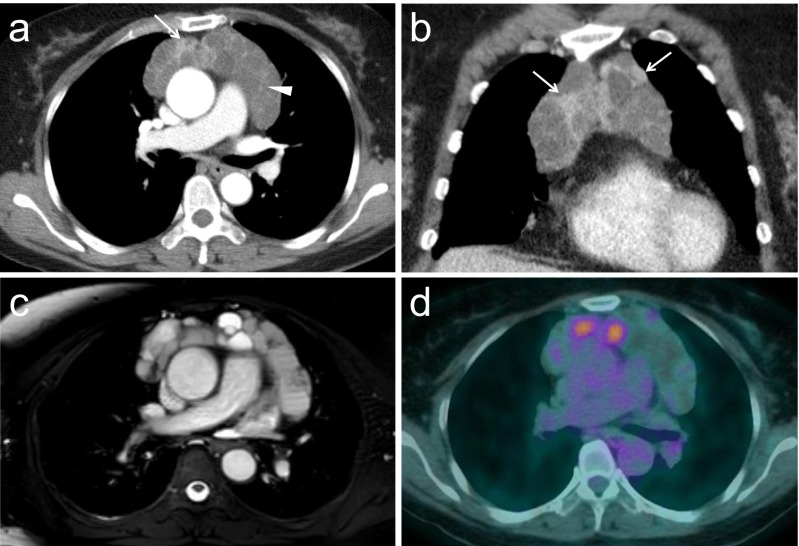
A 59-year-old female with a history of hypertension, old pulmonary tuberculosis, hyperlipidemia, and angina was incidentally found to have a mediastinal mass. Chest CT and MRI revealed a large anterior mediastinal mass that measured approximately 10 × 3.7 × 7 cm and featured multilocular cysts. CT with contrast enhancement showed partially enhancing nodules and septa in the lesion (Fig. 1a,b). MRI images revealed different degrees of signal intensity in each of the cystic compartments (Fig. 1c), and contrast enhancement of the solid nodules. No calcifications or fatty components were seen. The serum levels of carcinoembryonic antigen, alpha-fetoprotein, and anti-acetylcholine receptor antibody were not elevated. A multilocular thymic cyst, cystic thymoma, cystic teratoma, or thymic carcinoma were suspected.
Fig. 1.
Radiological imaging findings of the multilocular thymic cyst. a,b) Axial and coronal contrast enhanced chest CT show multicystic mass in anterior mediastinum. The mass contains multiple internal septa (arrowhead) and enhancing soft tissue attenuation components (arrow). c) Fat-suppressed MR image shows the different degree of signal intensity of the cystic compartments. d) F-18 FDG PET/CT scan shows moderate uptake of FDG corresponding to solid nodules of multicystic anterior mediastinal mass (SUVmax = 3.6)
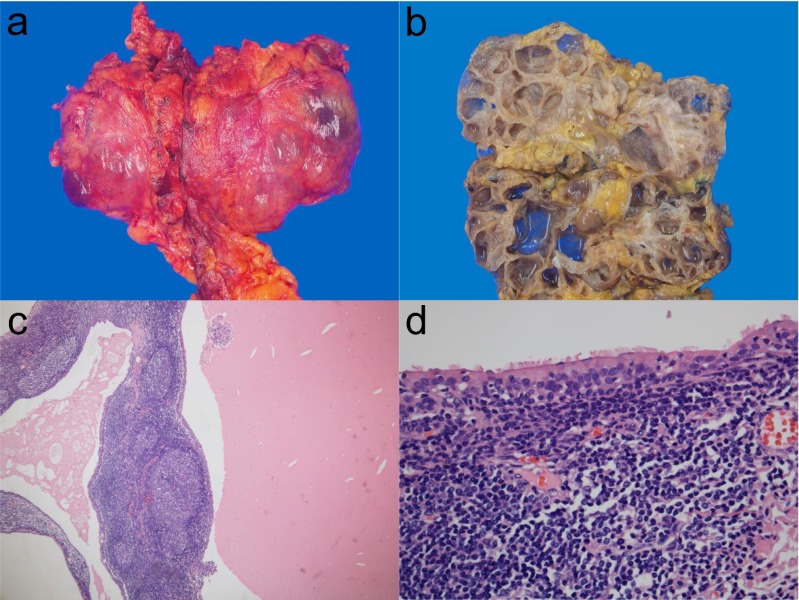
F-18 FDG PET/CT (Gemini TF, Philips Healthcare, OH, USA) was carried out for further evaluation, and revealed almost no FDG uptake in the multilocular cystic mass but moderate FDG uptake in the solid nodules (SUVmax = 3.6) (Fig. 1d). Extended total thymectomy was performed. The resected specimen measured 15 × 14 × 8 cm and weighed 300 g. The mass itself measured 14 × 8 × 6 cm and was well-demarcated from the surrounding thymic adipose tissue, with focal adhesion to the pericardium. The cut surface showed multilocular cysts separated by fibrous walls of varying thickness, and there were centrally nodular lesions. The cysts contained clear fluid and gelatinous material (Fig. 2a,b). Microscopically, the cysts were lined by flattened cuboidal cells or ciliated columnar cells, and some cystic lumens contained eosinophilic material. The fibrous walls exhibited prominent lymphoid hyperplasia with well-developed germinal centers. Central nodular lesions showed a similar morphology of fibrous septa. The lymphocytes were small and mature, and the epithelium showed no atypia. Several small cholesterol granulomas within the lumen and walls of the cysts were seen (Fig. 2c,d). Immunohistochemically, the lining epithelia of the cyst were positive for cytokeratin AE1/AE3 and no epithelial proliferation was seen in the nodular lesions; the findings eliminated the possibility of thymoma. CD20-positive B cells in germinal centers and CD3-positive T cells in interfollicular areas showed organized mixed distribution, which suggested polyclonal lymphocytes expansion. BCL-2 was negative in the germinal center of lymphoid follicles. Based on these findings, a diagnosis of multilocular thymic cyst with follicular lymphoid hyperplasia was made.
Fig. 2.
Gross and microscopic findings of multilocular thymic cyst. a, b) The mass is a 14 × 8 × 6 cm sized multilocular cyst separated by fibrous wall. c) Cyst contains eosiophilic material and fibrous wall shows diffuse lymphoid follicles with germinal centers. d) Cysts are lined by ciliated columnar cells in some areas
Discussion
Thymic cysts can be divided into two types—congenital cysts and acquired cysts. Congenital cysts are typically unilocular, without inflammatory changes. In contrast, acquired thymic cysts are multilocular lesions induced by an inflammatory process. It is important to differentiate a multilocular thymic cyst from a unilocular one, because the multilocular type may recur postoperatively and coexist with a thymic epithelial tumor [1].
Multilocular thymic cysts can occur at any age, and their etiology is generally unknown. They have been associated with certain infections (e.g., human immunodeficiency virus and syphilis) [4, 5], autoimmune disease (Sjögren’s syndrome, systemic lupus erythematosus, myasthenia gravis), and malignancy. Associated malignancies include thymic neoplasia (thymoma and thymic carcinoma), malignant lymphoma (MALT lymphoma and Hodgkin lymphoma), and germ cell tumor [2, 3]. Multilocular thymic cysts are often found incidentally on imaging of asymptomatic patients [7]. However, presenting symptoms may include chest pain, dyspnea, or superior vena cava syndrome and fever secondary to a severe inflammatory process [3].
The diagnosis of multilocular thymic cysts cannot be made by imaging alone. Cystic thymic pathology can be benign or malignant. Squamous cell carcinoma, cystic degeneration of thymoma, thymus with nodular sclerotic Hodgkin’s lymphoma, and seminoma all display similar radiologic features [8]. Choi et al. analyzed CT examinations of eight patients with multilocular thymic cysts, and revealed that CT cannot be used to reliably distinguish neoplastic from non-neoplastic soft tissue components [6]. As a result, CT or MRI can still be nonspecific, given the overlapping nature between multilocular thymic cysts and other thymic pathologies.
To our best knowledge, there are only two reports regarding the F-18 FDG PET/CT features of multilocular thymic cysts, and they both reported that multilocular thymic cysts exhibit FDG uptake [9, 10]. In our case, FDG uptake (SUVmax = 3.6) of the solid thymic components was seen. On the histopathologic examination, these solid components were nodules with lymphoid tissue, without atypia. It is well known that increased FDG uptake can be observed not only in malignancies but also in inflammation [11]. F-18 FDG PET/CT can be helpful in ruling out malignancies, such as thymic carcinoma and Hodgkin lymphoma, because FDG uptake of these tumors is higher than in multilocular thymic cysts, including in our case [12, 13]. However, F-18 FDG PET/CT cannot exclude thymomas and lymphomas with low to moderate FDG uptake, such as MALT lymphoma [12, 14]. To this end, tissue biopsy remains the hallmark of the diagnosis. A less invasive percutaneous CT-guided biopsy may be optimal, or open biopsy can be performed. If the biopsy does not provide conclusive results, complete removal is necessary, as in our case. Thus, complete surgical resection for extensive histopathologic sampling and therapy is recommended. Incomplete resection of multilocular thymic cysts due to fibrous adhesions may, in some cases, result in recurrence of the disease [9]. Our case showed fibrous adhesion to the adjacent pericardium, so pericardial resection was performed.
In conclusion, our patient was symptom-free, and it was difficult to determine whether a multilocular thymic cyst coexisted with a thymic malignancy using any method except for histological examination. When treating multilocular thymic cysts, complete surgical resection should be performed to prevent recurrence. Careful pathological examinations are also essential to exclude coexisting malignancies.
Compliance with Ethical Standards
Conflict of Interest
Jin-Suk Kim and Eun Jung Cha declare that they have no conflict of interest.
Ethical Statement
All procedures followed were performed in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration of 1975, as revised in 2013. The study design and exemption of informed consent were approved by the Institutional Review Board of the Konyang University Hospital.
References
- 1.Müller NL, Silva CIS. Imaging of the chest. Philadelphia: Saunders/Elsevier; 2008. pp. 1513–4. [Google Scholar]
- 2.Izumi H, Nobukawa B, Takahashi K, Kumasaka T, Miyamoto H, Yamazaki A, et al. Multilocular thymic cyst associated with follicular hyperplasia: clinicopathologic study of 4 resected cases. Hum Pathol. 2005;36:841–4. doi: 10.1016/j.humpath.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 3.Suster S, Rosai J. Multilocular thymic cyst: an acquired reactive process. Study of 18 cases. Am J Surg Pathol. 1991;15:388–98. doi: 10.1097/00000478-199104000-00008. [DOI] [PubMed] [Google Scholar]
- 4.Avila NA, Mueller BU, Carrasquillo JA, et al. Multilocular thymic cysts: imaging features in children with human immunodeficiency virus infection. Radiology. 1996;201:130–4. doi: 10.1148/radiology.201.1.8816533. [DOI] [PubMed] [Google Scholar]
- 5.Leonidas JC, Berdon WE, Valderrama E, et al. Human immunodeficiency virus infection and multilocular thymic cysts. Radiology. 1996;198:377–9. doi: 10.1148/radiology.198.2.8596835. [DOI] [PubMed] [Google Scholar]
- 6.Choi YW, McAdams HP, Jeon SC, et al. Idiopathic multilocular thymic cyst: CT features with clinical histopathologic correlation. AJR Am J Roentgenol. 2001;117:881–5. doi: 10.2214/ajr.177.4.1770881. [DOI] [PubMed] [Google Scholar]
- 7.Schmalz SL, Reddy PR, Hutchens KA, Liu J. Multilocular thymic cyst presenting as acute chest pain. Am J Med. 2008;121:5–6. doi: 10.1016/j.amjmed.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 8.Wick MR, et al. The mediastinum. In: Mills SE, Carter D, Greenson JA, et al., editors. Sternberg’s diagnostic surgical pathology. Fourth. Philadelphia: Lippincott, Williams & Wilkins; 2004. pp. 1254–9. [Google Scholar]
- 9.Kasirye Y, Talsness S, Walters MP, Douglas-Jones JW, Resnick JM, Mazza JJ, et al. Multilocular thymic cyst with epithelioid granulomata of unknown etiology: a radiologic and histopathologic correlation. Ann Diagn Pathol. 2012;16:38–42. doi: 10.1016/j.anndiagpath.2010.11.009. [DOI] [PubMed] [Google Scholar]
- 10.Hiroshi H, Kinoshita E, Nakada S, Nojima T, Tanaka M, Usuda K, et al. Thymic lymphoid hyperplasia with multilocular thymic cysts diagnosed before the Sjögren syndrome diagnosis. Diagn Pathol. 2015;10:103. doi: 10.1186/s13000-015-0332-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gorospe L, Raman S, Echeveste J, Avril N, Herrero Y, Herna NS. Whole-body PET/CT; spectrum of physiological variants, artifacts and interpretative pitfalls in cancer patients. Nucl Med Commun. 2005;26:671–87. doi: 10.1097/01.mnm.0000171779.65284.eb. [DOI] [PubMed] [Google Scholar]
- 12.Sung YM, Lee KS, Kim BT, Choi JY, Shim YM, Yi CA. 18F-FDG PET/CT of thymic epithelial tumors: usefulness for distinguishing and staging tumor subgroups. J Nucl Med. 2006;47:1628–34. [PubMed] [Google Scholar]
- 13.Tsukamoto N, Kojima M, Hasegawa M, Oriuchi N, Mastsushima T, Yokohama A, et al. The usefulness of 18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET) and a comparison of 18F-FDG-PET with 67Gallium scintigraphy in the evaluation of lymphoma; relation to Histologic subtypes based on the world health organization classification. Cancer. 2007;110:652–9. doi: 10.1002/cncr.22807. [DOI] [PubMed] [Google Scholar]
- 14.Hoffmann M, Wöhrer S, Becherer A, Chott A, Streubel B, Kletter K, et al. 18F-Fluoro-deoxy glucose positron emission tomography in lymphoma of mucosa-associated lymphoid tissue: histology makes the difference. Ann Oncol. 2006;17:1761–5. doi: 10.1093/annonc/mdl295. [DOI] [PubMed] [Google Scholar]