Abstract
Introduction
Congenital high airway obstruction syndrome (CHAOS) is a rare, usually lethal abnormality characterized by complete or near-complete intrinsic obstruction of the fetal airway. Laryngeal atresia is the most frequent cause, but other etiologies include laryngeal or tracheal webs, laryngeal cyst, subglottic stenosis or atresia, tracheal atresia and laryngeal or tracheal agenesis. When antenatal diagnosis of possible upper airway obstruction is made, specific type of obstruction is rarely determined making the term CHAOS introduced by Hedrick et al in 1994 more appropriate.
USG Characteristics
Sonographic findings in CHAOS are characteristic and are secondary to high airway obstruction. The lungs are symmetrically enlarged, echogenic and homogenous. The distended lungs have mass effect on the diaphragm, which appears flattened or inverted, and the heart is displaced anteriorly in the midline. The heart often appears dwarfed by the surrounding enlarged lungs.
Discussion
The primary abnormality is an intrinsic obstruction of the upper airway. Normal lung development involves a continuous efflux of fluid from the fetal lungs. Laryngeal atresia/CHAOS stops the efflux of this fluid, and this retained fluid distends the alveoli with fluid giving the lungs voluminous echogenic appearance and inverting the diaphragm. Isolated airway obstruction without hydrops has a relatively favorable prognosis. CHAOS with associated anomalies and with early presentation of hydrops is an ominous sign with a high rate of fetal demise and a poor survival rate even with the ex utero intrapartum treatment (EXIT) procedure.
Keywords: Laryngeal atresia, Antenatal, Sonography
Introduction
CHAOS (congenital high airway obstruction syndrome) is a rare, usually lethal abnormality characterized by complete or near-complete intrinsic obstruction of the fetal airway. Laryngeal atresia is the most frequent cause, but other etiologies include laryngeal or tracheal webs, laryngeal cyst, subglottic stenosis or atresia, tracheal atresia and laryngeal or tracheal agenesis. When antenatal diagnosis of possible upper airway obstruction is made, specific type of obstruction is rarely determined making the term CHAOS introduced by Hedrick et al. [1] more appropriate.
The true incidence of high airway obstruction in the fetus is not known because this is a rare and life-threatening condition with high mortality and morbidity. Survival is dependent on early prenatal diagnosis, close prenatal follow-up and fetal or immediate postnatal intervention. If unrecognized before delivery, the reported mortality is 80–100 % [2].
The precise cause is not known; most authors claim that this malformation is related to an arrest of the sixth brachial arch at different gestational stages during normal embryological development. Sporadic, genetic and vascular causes have been proposed. In most cases, the subglottic portion of the airway (laryngeal) or proximal trachea is atretic, stenotic, or there may be a thick web obstructing the proximal airway. It is even more rare for the obstruction to occur distally in the trachea, although this has been described.
Pathologically the obstructed airway results in decreased clearance of fluid produced by the fetal lungs as well as an increase in intratracheal pressure resulting in lung hyper-expansion and abnormal development [1, 3]. In addition, there is thinning of the alveolar walls, a decreased number of type 2 pneumocytes and a resulting decreased surfactant proportional to the duration of the tracheal obstruction. The hyper-expanded lungs cause compression of the heart and IVC, decreasing venous return and leading to non-immune hydrops [1, 3, 4]. These series of events are responsible for the prenatal imaging characteristics of CHAOS.
USG Characteristics
Sonographic findings in CHAOS are characteristics and are secondary to high airway obstruction. This abnormality has been detected in the fetus as early as 16 weeks. The lungs are symmetrically enlarged, echogenic and homogenous. This appearance is due to the fluid distension of the tiny air spaces, which are too small to be perceived as cysts on the sonogram. The distended lungs have mass effect on the diaphragm, which appears flattened or inverted, and the heart is displaced anteriorly in the midline. The heart often appears dwarfed by the surrounding enlarged lungs. In many fetuses, the two fluid-filled main bronchi and trachea, distended by lung fluid, can be visualized. Neither the precise level of obstruction nor etiology (web vs stenosis vs atresia) can be determined accurately with sonography. One can safely assume, however, that the high airway obstruction is severe if the lungs are enlarged and diaphragm is flattened [1, 4, 5]. Fetal ascites is nearly universal at the time of diagnosis but may not be associated with other findings of hydrops. Poly- and oligohydramnios are reported. Presumably, polyhydramnios is caused by esophageal compression. Oligohydramnios is not fully understood due to cardiac compromise or diminished lung fluid efflux into the amnia.
More than 50 % of fetus with laryngeal obstruction have additional anomalies. Most common associated anomalies in the literature are renal, cranio-spinal, tracheo-esophageal atresia, vertebral defects, imperforate anus, ambiguous genitals, tracheo-esophageal fistula, hemi-diaphragmatic defect, duodenal atresia, syndactyly and single umbilical artery. Laryngeal atresia may occur as part of Fraser syndrome [6].
We report here two cases of laryngeal atresia leading to indirect inference of CHAOS with associated anomalies. Both cases had type 2 laryngeal atresia (infraglottic obstruction).
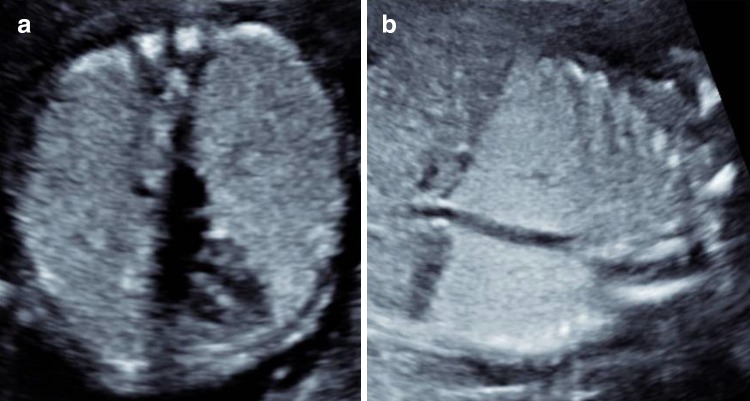
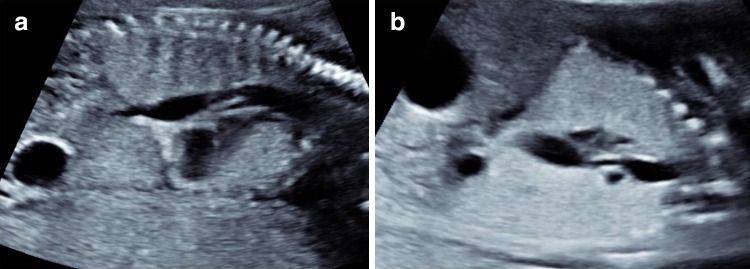
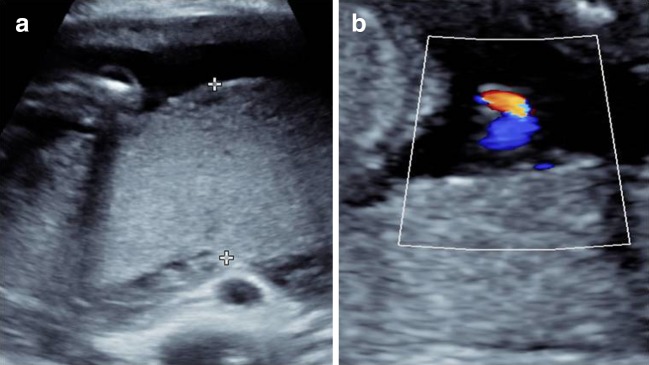
A 25-year-old woman, G2P1, was referred at 20 weeks of gestation for routine obstetric ultrasound examination. The ultrasound examination showed increased thoracic diameter and circumference due to bilateral symmetrically enlarged and homogenously echogenic lungs. Diaphragms were flattened, and heart appeared compressed and shifted anteriorly in midline (Fig. 1). There was a fluid-filled tubular structure in posterior mediastinum, supposed to be trachea. It showed branching into bronchi, and also through a small narrow channel, it was connected to dilated fluid-filled distal esophagus suggestive of a tracheo-esophageal fistula (Fig. 2). Stomach and proximal duodenum were dilated with typical double bubble sign signifying duodenal atresia (Fig. 3). There were a single umbilical artery and placentomegaly (Fig. 4). An inference of duodenal atresia, tracheo-esophageal fistula and CHAOS was made. Poor prognosis was explained to the parents, and after counseling, they opted for termination of pregnancy.
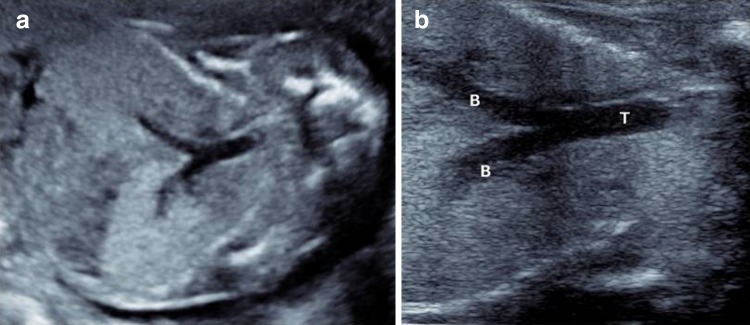
Fig. 1.
a, b (Axial and coronal)Echogenic voluminous lungs with flattening of diaphragm. Heart is in midline, compressed and displaced anteriorly
Fig. 2.
a, b (Sagittal and coronal)Dilated trachea and lower esophagus with tracheo-esophageal fistula
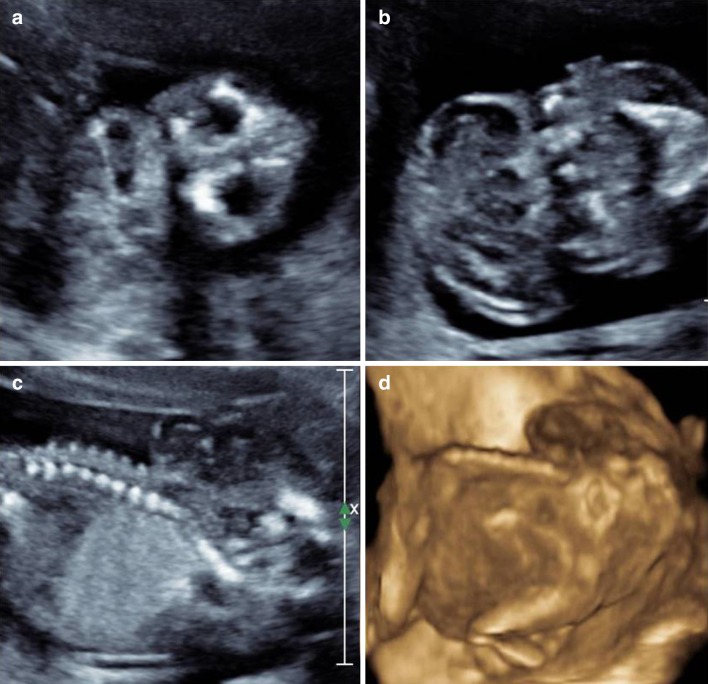
Fig. 3.
a (Coronal) Dilated lower esophagus and ‘double bubble sign’ in upper abdomen. b (Axial) Continuity of stomach with duodenum confirming duodenal atresia
Fig. 4.
a, b Placentomegaly (4.8 cm in thickness) and single umbilical artery (two-vessel cord)
Fetus was delivered in obstetric department of our hospital and showed no external defect; autopsy of 160 g fetus was carried out at forensic department which revealed voluminous lungs with rib markings on the surface consistent with CHAOS. The fetus had laryngeal stenosis type 2. There was esophageal atresia with type III tracheo-esophageal fistula. Single umbilical artery and duodenal atresia were also confirmed.
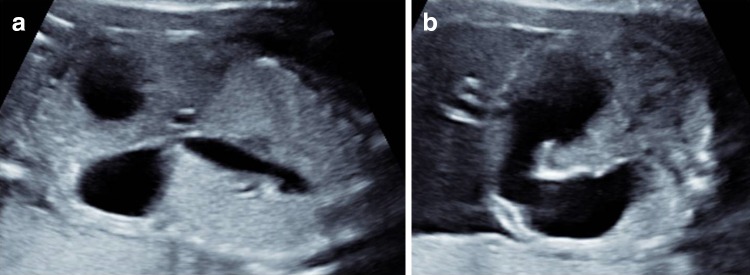
Second case was a 22-year-old woman, primigravida, referred at 18 weeks of gestation. The ultrasound examination showed increased thoracic diameter and circumference due to bilateral, voluminous, homogenously echogenic lungs. Diaphragms were everted, and heart appeared compressed and shifted anteriorly in midline. The trachea and bronchi were dilated (Fig. 5). The ribs appear short and faintly echogenic. There was an absence of calvarium. Brain tissue was seen exposed to amniotic fluid and appeared disorganized. Fetal face was normal (Fig. 6). There was an absence of cervical vertebrae and rachischisis of upper thoracic vertebrae. There was persistent retroflexion of neck (Fig. 7). Mild ascites was noted in the abdomen. An inference of CHAOS with iniencephaly and acalvaria–anencephaly sequence was made. Poor prognosis was explained to the parents, and they opted for termination of pregnancy. Fetus was delivered in obstetric department and showed anencephaly and iniencephaly (Fig. 8a, b) with normal limbs.
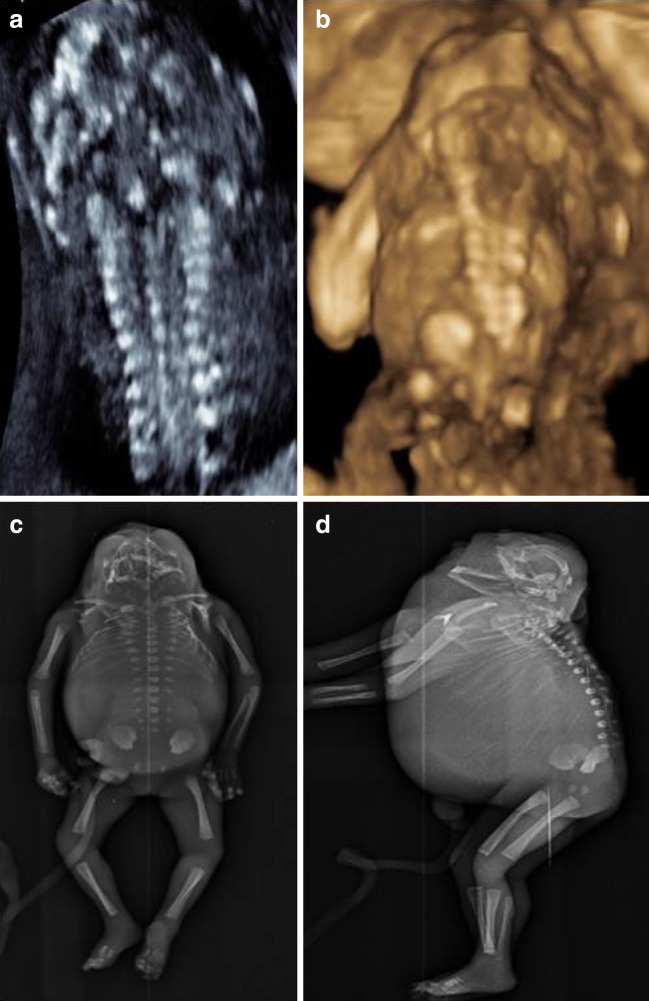
Fig. 5.
a Dilated trachea and bronchi with echogenic voluminous lungs causing mass effect on diaphragm leading to eversion. b Zoomed view of trachea and bronchi
Fig. 6.
a, b (Axial sections) c, d (sagittal sections) Normal-appearing orbits and face but with absence of calvarium, marked retroflexion at neck and disorganized brain tissue displaced caudally and seen overlying upper torso
Fig. 7.
a (Coronal section spine), b (7d Image), c and d (Radiograph spine AP and Lat.) Absence of cervical vertebrae and rachischisis of upper thoracic vertebrae
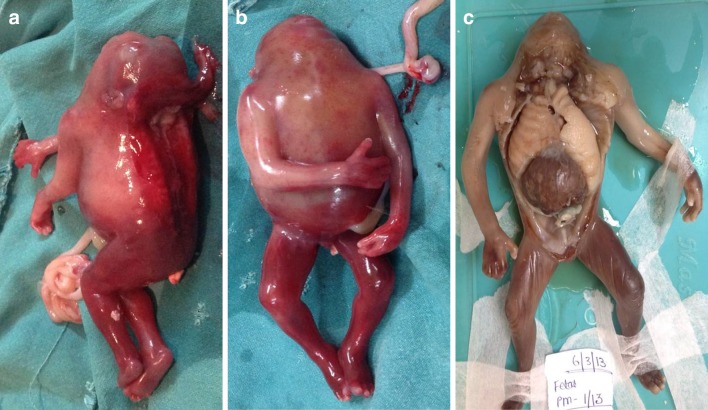
Fig. 8.
a, b Post-abortion 18-week fetus showing features of iniencephaly and anencephaly. c Autopsy specimen showing hyperinflated lungs with costal impressions
Autopsy of 145 g fetus was carried out which revealed voluminous lungs with rib markings on the surface. The fetus had laryngeal stenosis type 2. There was an absence of cervical vertebrae and spina bifida of upper thoracic vertebrae and absence of calvarial bones with disorganized brain tissue and marked retroflexion of neck. Autopsy confirmed the prenatal ultrasound findings (Fig. 8c).
Discussion
Congenital high airway obstruction sequence is a rare condition characterized by a single identifiable abnormality leading to a pattern of severe life-threatening abnormalities in the affected fetuses. The primary abnormality is an intrinsic obstruction of the upper airway. Normal lung development involves a continuous efflux of fluid from the fetal lungs. Laryngeal atresia/CHAOS stops the efflux of this fluid, and this retained fluid distends the alveoli with fluid giving the lungs voluminous echogenic appearance and inverting the diaphragm.
CHAOS is characterized by a number of sonographic structural secondary changes. Fetal lung size is increased, and the lungs are hyperechoic bilaterally. The hyperplastic lungs are edematous but otherwise histologically normal. The increased number of tissue–fluid interfaces produces the hyperechoic appearance of the lungs on ultrasound. The fetal heart is compressed and assumes a more central position; diaphragms are flattened or everted. In the absence of tracheal atresia, an enlarged fluid-filled trachea can be demonstrated. Using color Doppler, one can demonstrate the absence of flow in the trachea during fetal breathing and in some cases even localize the level of obstruction. The enlarged lungs may compress the superior vena cava, thoracic duct and heart, impeding venous return and causing ascites, non-immune fetal hydrops and placentomegaly. Oligohydramnios may be present early in pregnancy, due to the absence of lung liquid contribution to the total volume of amniotic fluid. Oligohydramnios is also present in cases with associated renal anomalies. Hydramnios may also develop, usually later in pregnancy, from compression on the esophagus and decreased fetal swallowing.
Our first case was associated with T.O. fistula and duodenal atresia. CHAOS coexisting with T.O. fistula alone leads to decompression of lungs, making diagnosis more challenging. Our second case had, in association with type 2 laryngeal atresia, anencephaly and iniencephaly. To the best of our knowledge, no such case in the literature has been reported.
Isolated airway obstruction without hydrops has a relatively favorable prognosis. CHAOS with associated anomalies and with early presentation of hydrops is an ominous sign with a high rate of fetal demise and a poor survival rate even with the ex utero intrapartum treatment (EXIT) procedure. In recent years, fetoscopic tracheoscopy has been performed to eliminate the cause of obstruction. It was possible to create a pharyngo-tracheal fistula for the decompression of the lung. However, further studies are necessary to determine the long-term effects and safety of fetoscopic tracheoscopy [7].
But before applying these advanced treatment options, other congenital anomalies incompatible with life (such as in our cases) must be ruled out. Our own cases as well as extensive review of the literature show that laryngeal atresia has been reported with varying anomalies and there is no definite pattern of associations. Hence, the careful investigation for other associated anomalies is mandatory. If other major anomalies are ruled out, level of obstruction must be ascertained, and then, these advanced options can be used.
Dr. Aman Gupta
is presently a Professor and Head, Department Of Radiodiagnosis at Sri Aurobindo Medical College and PG Institute, Indore (MP). He did his graduation and postgraduation in Radiodiagnosis from MGM Medical College, Indore. He has 15 publications in indexed journals to his name. He has guided/co-guided 28 MD thesis. His fields of interest include conventional radiography and ultrasonography.
Compliance with Ethical Standards
Conflict of interest
None.
Footnotes
Dr. Aman Gupta is a MD; Dr. Chandrajeet Yadav is a MD; Dr. Sandeep Dhruw is a MD; Dr. Divyangi Mishra is a MBBS; and Dr. Abhijeet Taori is a MBBS at Department of Radiodiagnosis, Sri Aurobindo Medical College and PG Institute, Indore, MP, India
References
- 1.Hedrick MH, Ferro MM, Filly RA, et al. Congenital high airway obstruction syndrome(CHAOS): a potential for perinatal intervention. J Pediatr Surg. 1994;29:271–274. doi: 10.1016/0022-3468(94)90331-X. [DOI] [PubMed] [Google Scholar]
- 2.Cho HJ, Kim YM, Lee HY, et al. A case of congenital high airway obstruction syndrome caused by complete tracheal obstruction with associated anomalies. Korean J Obstet Gynecol. 2012;55(2):115–118. doi: 10.5468/KJOG.2012.55.2.115. [DOI] [Google Scholar]
- 3.Lim FY, Crombleholme TM, Hedrick HL, et al. Congenital high airway obstruction syndrome: natural history and management. J Pediatr Surg. 2003;38:940–945. doi: 10.1016/S0022-3468(03)00128-3. [DOI] [PubMed] [Google Scholar]
- 4.Onderoglu L, Saygan Karamursel B, Bulun A, et al. Prenatal diagnosis of laryngeal atresia. Prenat Diagn. 2003;23:277–280. doi: 10.1002/pd.565. [DOI] [PubMed] [Google Scholar]
- 5.Biyyam Deepa R, Chapman Teresa, Ferguson Mark R, et al. Congenital lung abnormalities: embryologic features, prenatal diagnosis, and postnatal radiologic-pathologic correlation. RadioGraphics. 2010;30:1721–1738. doi: 10.1148/rg.306105508. [DOI] [PubMed] [Google Scholar]
- 6.Eskander BS, Shehata BM. Fraser syndrome: a new case report with review of the literature. Fetal Pediatr Pathol. 2008;27:99–104. doi: 10.1080/15513810802077628. [DOI] [PubMed] [Google Scholar]
- 7.Paek BW, Callen PW, Kitterman J, et al. Successful fetal intervention for congenital high airway obstruction syndrome. Fetal Diagn Ther. 2002;17:272–276. doi: 10.1159/000063179. [DOI] [PubMed] [Google Scholar]