Summary
Since the beginning of the 1980s, 33 emerging tick-borne agents have been identified in mainland China, including eight species of spotted fever group rickettsiae, seven species in the family Anaplasmataceae, six genospecies in the complex Borrelia burgdorferi sensu lato, 11 species of Babesia, and the virus causing severe fever with thrombocytopenia syndrome. In this Review we have mapped the geographical distributions of human cases of infection. 15 of the 33 emerging tick-borne agents have been reported to cause human disease, and their clinical characteristics have been described. The non-specific clinical manifestations caused by tick-borne pathogens present a major diagnostic challenge and most physicians are unfamiliar with the many tick-borne diseases that present with non-specific symptoms in the early stages of the illness. Advances in and application of modern molecular techniques should help with identification of emerging tick-borne pathogens and improve laboratory diagnosis of human infections. We expect that more novel tick-borne infections in ticks and animals will be identified and additional emerging tick-borne diseases in human beings will be discovered.
Introduction
Ticks were the first arthropods to be recognised as vectors that can transmit pathogens to human beings and are second only to mosquitoes as vectors of infectious diseases in the world.1 Tick-borne infections are zoonoses with pathogens maintained in natural cycles involving tick vectors and animal hosts. Human beings are occasional hosts for ticks and are usually viewed as dead-end hosts that have no role in maintaining tick-borne agents in nature.2 Different tick species favour distinct biotopes or environments, which define their geographical distribution and, consequently, the areas of risk for human tick-borne infections. In the past three decades, tick-borne pathogens have emerged worldwide and become a great threat to human health.1, 3
China is the largest developing country in the world and has made tremendous progress in the control and prevention of infectious diseases; however, emerging infectious diseases are the new challenge now facing China.4 Although outbreaks of severe acute respiratory syndrome and H5N1 and H7N9 avian influenza virus infections have attracted great attention, emerging tick-borne diseases have generally been neglected by primary health-care providers and clinicians. Although an increasing number of tick-borne infections have been reported in mainland China, no comprehensive review of this substantial public health problem has been undertaken. We will provide an overview of the type and distribution of emerging tick-borne infections in tick vectors, animal hosts, and human beings. We will describe the clinical characteristics of human tick-borne diseases, and discuss possible factors contributing to their emergence.
Emergence of tick-borne infections in mainland China
Since 1982, 33 emerging tick-associated agents have been identified in mainland China, including eight species of spotted fever group rickettsiae (SFGR);5, 6, 7, 8, 9, 10, 11 three species of Ehrlichia,12, 13, 14 three species of Anaplasma,15, 16, 17 and Candidatus Neoehrlichia mikurensis18 in the family Anaplasmataceae; six genospecies in the complex Borrelia burgdorferi sensu lato;19, 20, 21, 22, 23 11 species of Babesia;24, 25, 26, 27, 28, 29, 30, 31, 32, 33 and severe fever with thrombocytopenia syndrome virus (SFTSV).34 The location and year in which each emerging tick-borne agent was first identified are shown in the appendix. Most (19 of 33) were initially detected in ticks; however, six were identified in domestic animals (sheep, goat, buffalo, and dog), two in wild animals (Chinese white-bellied rat and Chinese hare), and six in people. Detailed information regarding the identification of these emerging tick-borne infections is summarised in table 1 .
Table 1.
First identification and origin of emerging tick-borne infections in mainland China since 1982
| First identified origin* | First identified province (year)† | Reference (subsequent investigations) | ||
|---|---|---|---|---|
| Spotted fever group rickettsiae | ||||
| Rickettsia heilongjiangiensis | Dermacentor silvarum | Heilongjiang (1982) | 5 (6,8,35–45) | |
| Rickettsia sibirica sp BJ-90 | Dermacentor sinicus | Beijing (1990) | 7 (46) | |
| Rickettsia sibirica sp mongolotimonae | Hyalomm asiaticum kozlovi | Inner Mongolia (1991) | 7 | |
| Rickettsia monacensis | Ixodes persulcatus | Henan, Anhui, and Hubei provinces (2006) | 8 (44,47) | |
| Rickettsia raoultii | D silvarum | Xinjiang (2011) | 9 (48–50) | |
| Rickettsia slovaca | D silvarum | Xinjiang (2011) | 9 (50,51) | |
| Candidatus Rickettsia hebeiii | Haemaphysalis longicornis | Hebei (2011) | 10 (52) | |
| Candidatus Rickettsia tarasevichiae | Man (I persulctus) | Heilongjiang (2012) | 11 | |
| Anaplasmataceae | ||||
| Ehrlichia chaffeensis | Amblyomma testudinarium | Yunan (1996) | 12 (32,36,53–62) | |
| Ehrlichia canis | Rhipicephalus sanguineus sensu stricto | Guangdong (1997) | 13 (16,57,63) | |
| Ehrlichia sp Tibet | Rhipicephalus microplus | Tibet (2000) | 14 | |
| Anaplasma phagocytophilum | I persulcatus | Heilongjiang (1997) | 15 (36,51,53–55,62–75) | |
| Anaplasma platys | Dog | Guangdong (1998) | 16 (63) | |
| Anaplasma capra‡ | Goat | Heilongjiang (2014) | 17 | |
| Candidatus Neoehrlichia mikurensis | Man (I persulctus) | Heilongjiang (2010) | 18 (76,77) | |
| Borrelia burgdorferi sensu lato | ||||
| Borrelia garinii | Man (I persulcatus) | Heilongjiang (1986) | 19 (21,23,36,54,78–91) | |
| Borrelia valaisiana | Ixodes granulatus (Apodemus agrarius) | Zhejiang (1997) | 20 (86,92) | |
| Borrelia sinica | Niviventer confucianus | Chongqing (1997) | 20 | |
| Borrelia afzelii | Man | Heilongjiang (2000) | 21 (36,78,79,81,83–85,90) | |
| Borrelia valaisiana-related genospecies | I granulatus, H longicornis (A agrarius) | Guizhou (2006) | 22 (78,83,86,88) | |
| Borrelia burgdorferi sensu stricto | Caprolagus sinensis | Hunan (2010) | 23 (92) | |
| Babesia spp | ||||
| Babesia ovis | Sheep | Sichuan (1982) | 24 (93) | |
| Babesia major | H longicornis (cattle) | Henan (1988) | 25 (94) | |
| Babesia ovata | Cattle | Henan (1990) | 26 (95) | |
| Babesia orientalis | Buffalo | Hubei (1997) | 27 (96,97) | |
| Babesia motasi | Sheep | Gansu (1997) | 28 (98,99) | |
| Babesia caballi | D silvarum, Dermacentor nuttalli | Gansu (1998) | 29 (100–102) | |
| Babesia sp Kashi | Hyalomma anatolicum | Xinjiang (2005) | 30 (103) | |
| Babesia sp Xinjiang | R sanguineus sensu stricto, H anatolicum | Xinjiang (2007) | 31 (103) | |
| Babesia microti | I persulcatus, Haemaphysalis concinna | Heilongjiang (2007) | 32 (36,104–107) | |
| Babesia divergens | I persulcatus, H concinna, Haemaphysalis japonica (A agrarius) | Heilongjiang (2007) | 32 (36,108) | |
| Babesia venatorum‡ | Man | Xinjiang (2012) | 33 (109) | |
| SFTSV | Man | Henan (2009) | 34 (110–118) | |
SFTSV=severe fever with thrombocytopenia syndrome virus.
First identified origin of each emerging tick-associated agent, including man, domestic animal, rodent, and tick. The agent that was simultaneously identified from other hosts or ticks is shown in parentheses.
Provinces include autonomous regions and metropolis.
Not been formally described in taxonomic papers.
Among the 33 newly recognised tick-associated agents, 15 have been reported to cause human infection, including: four species of SFGR;11, 35, 46, 48 an Ehrlichia species,53 two Anaplasma species,17, 53 and Candidatus N mikurensis;18 three genospecies of B burgdorferi sensu lato;19, 21, 78 three species of Babesia;33, 104, 108 and SFTSV (table 2 ).34 Six of the tick-borne pathogens were first identified in febrile patients (Candidatus Rickettsia tarasevichiae, Candidatus N mikurensis, Borrelia garinii, Borrelia afzelii, Babesia venatorum [not yet formally described], and SFTSV) and then shown to be associated with ticks (table 1). The other nine human pathogens were initially detected in ticks or animals and subsequently shown to infect human beings (Rickettsia heilongjiangiensis, Rickettsia sibirica sp BJ-90, Rickettsia raoultii, Ehrlichia chaffeensis, Anaplasma phagocytophilum, Anaplasma capra, Borrelia valaisiana-related genospecies, Babesia microti, and Babesia divergens). Among these 15 emerging tick-borne diseases, severe fever with thrombocytopenia syndrome (SFTS) was first identified in mainland China34 and subsequently reported in South Korea and Japan.134, 135 A disease similar to SFTS has been reported in the USA.136 Human infections with R sibirica sp BJ-90, Candidatus R tarasevichiae, A capra, and B valaisiana-related genospecies have been exclusively diagnosed in mainland China.11, 17, 46, 78 Human infections of Candidatus N mikurensis, Ba venatorum, and R raoultii, which have been detected in China, were first identified in Europe.18, 33, 48 Five tick-borne pathogens have been detected in ticks or reservoir hosts, or both, but have not yet been reported to cause infection in human beings in China. They include Rickettsia monacensis, Rickettsia slovaca, Rickettsia sibirica sp mongolotimonae, B valaisiana, and B burgdorferi sensu stricto.137, 138, 139, 140, 141 Additionally, a Rickettsia species (Candidatus Rickettsia hebeiii), two Ehrlichia species (Ehrlichia canis and Ehrlichia sp Tibet), an Anaplasma species (Anaplasma platys), a genospecies of B burgdorferi sensu lato (Borrelia sinica), and eight Babesia species (Babesia ovis, Babesia ovata, Babesia orientalis, Babesia major, Babesia motasi, Babesia caballi, Babesia sp Kashi, and Babesia sp Xinjiang) have been identified in ticks or animals, but their pathogenicity to human beings is unknown.
Table 2.
Emerging tick-borne diseases of human beings reported in mainland China as of May 31, 2015
| Pathogen | Number of patients | Diagnostic methods*(reference) | |
|---|---|---|---|
| Rickettsiosis | Rickettsia heilongjiangiensis | 34 | A and B (35), B and C (43), A and C (45) |
| Rickettsiosis | Rickettsia sibirica sp BJ-90 | 1 | A and B (46) |
| Rickettsiosis | Rickettsia raoultii | 2 | A and B (48) |
| Rickettsiosis | Candidatus Rickettsia tarasevichiae | 5 | B (11) |
| Rickettsiosis | Uncharacterised Rickettsia spp | 37 | C (119–121), B (122), A and C (123), E (124) |
| Human monocytic ehrlichiosis | Ehrlichia chaffeensis | 12 | B (53,55) |
| Human granulocytic anaplasmosis | Anaplasma phagocytophilum | 104 | B (53,55,74,75), A, B, and C (73), A and B (64), E (71) |
| Human infection with Anaplasma capra† | A capra† | 28 | A, B, and C (17) |
| Human infection with Candidatus Neoehrlichia mikurensis | Candidatus N mikurensis | 7 | B (18) |
| Lyme disease | Borrelia garinii | 30 | B (21,23,78,90,91) |
| Lyme disease | Borrelia afzelii | 8 | B (21,23,78,90), C (125) |
| Lyme disease | Borrelia valaisiana-related genospecies | 1 | B (78) |
| Lyme disease | Uncharacterised Borrelia burgdorferi sensu lato | 2691 | A (126–130), E (131) |
| Babesiosis | Babesia divergens | 2 | B (108) |
| Babesiosis | Babesia microti | 11 | B and D (104,107) |
| Babesiosis | Babesia venatorum† | 49 | A, B, and C (33), B, C, and D (109) |
| Babesiosis | Uncharacterised Babesia spp | 3 | D (132,133) |
| SFTS | SFTSV | 2543 | A, B, and C (34,117), A or B or C (113,118), A or B (114), B and C (115), B (116) |
SFTS=severe fever with thrombocytopenia syndrome. SFTSV=severe fever with thrombocytopenia syndrome virus.
Diagnostic methods: (A) a four-fold increase in titre of specific antibodies in blood sera collected from the acute and convalescent stages of illness, or a seroconversion of specific antibodies; (B) molecular detection and sequence determination; (C) isolation of pathogens from clinical samples; (D) light or electronic micrograph identification for thin blood smear; and (E) methods were not provided.
Not been formally described in taxonomic papers.
Emerging SFGR infections
Eight novel species of SFGR have been recorded in mainland China since 1982 (table 1).5, 6, 7, 8, 9, 10, 11 These species are mainly distributed in northern China (north of 36° north latitude).
Tick and animal infections
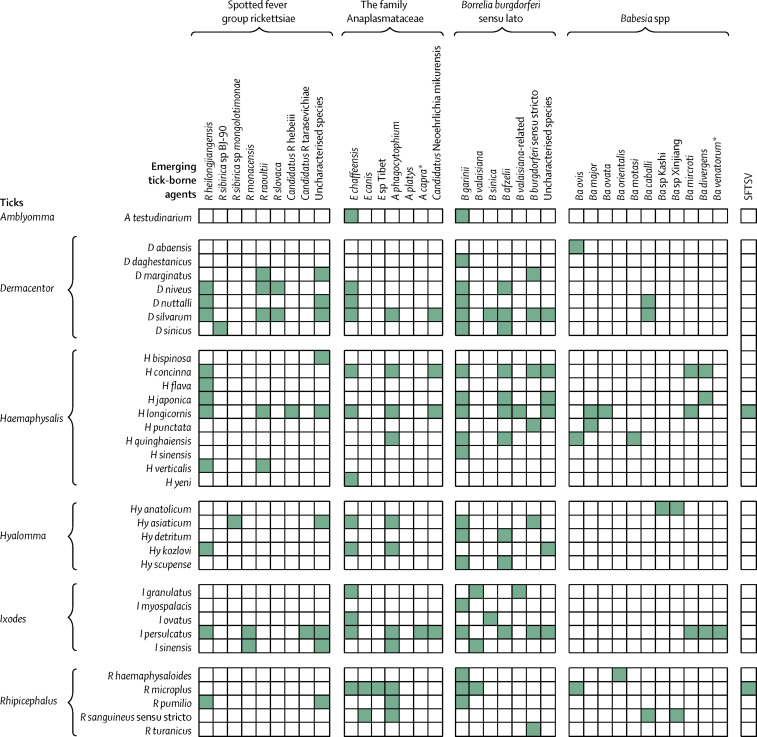
The eight emerging species and uncharacterised species of SFGR have been shown to be associated with 16 tick species (figure 1 ). R heilongjiangiensis has been proven to infect a range of tick species, three rodent species, and goats (appendix). In northeastern China, R heilongjiangiensis was detected in nine tick species and two rodent species from Heilongjiang Province,36, 37, 38 and in Haemaphysalis spp ticks from Jilin Province.38 In Inner Mongolia, R heilongjiangiensis has been reported in Haemaphysalis verticalis, Detmacentor niveus, Hyalomma asiaticum kozlovi, Rhipicephalus pumilio, and Detmacentor nuttalli ticks.39 In northwestern China, R heilongjiangiensis has been detected in Dermacentor silvarum ticks from Qinghai Province.40 In southern China, R heilongjiangiensis has been detected in Haemaphysalis longicornis ticks from Guangdong Province,41 in goats from Yunnan Province,42 and in chestnut white-bellied rats from Hainan Province.43 In central and eastern China, R heilongjiangiensis was identified in Haemaphysalis flava ticks from Henan, Anhui, and Hubei provinces,8 and in H longicornis from Zhejiang Province.44 R sibirica sp BJ-90 was detected in Dermacentor sinicus ticks from a Beijing suburb.7 R raoultii was detected in Dermacentor species ticks, including D silvarum and Dermacentor marginatus, in western China,9, 49 in H verticalis collected from Inner Mongolia, in D silvarum from Heilongjiang Province, and in H longicornis from Liaoning Province.48, 39, 50, 51 Four species, including R sibirica sp mongolotimonae, R monacensis, R slovaca, and Candidatus R hebeiii, have not been proven to infect human beings. Data regarding infected ticks and animal hosts are shown in figure 1 and the appendix.7, 8, 9, 10, 47, 52, 54, 119, 142, 143, 144, 145, 146, 147
Figure 1.
Matrix of emerging tick-associated agents and tick species in mainland China
*Not yet formally described. SFTSV=severe fever with thrombocytopenia syndrome virus.
Human infections
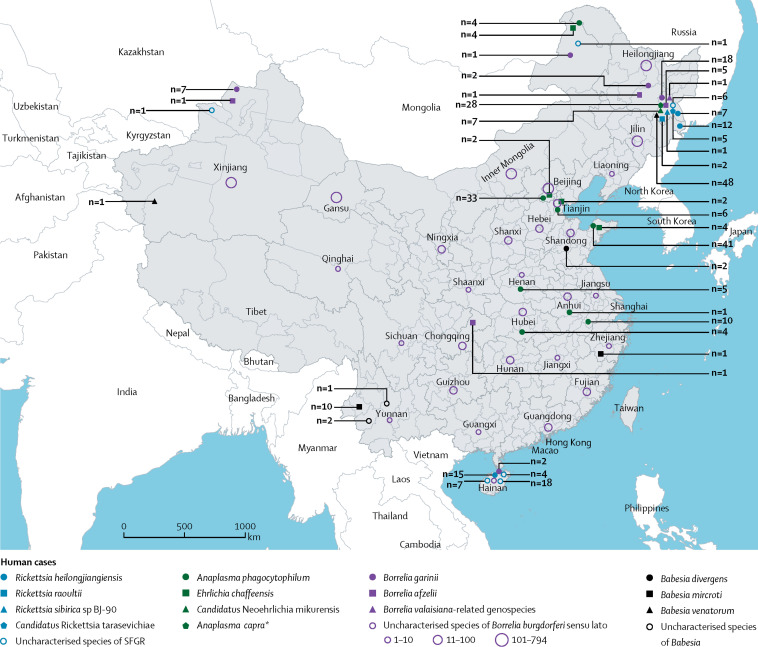
Four species of emerging SFGR have been reported to infect human beings, including R heilongjiangiensis, Candidatus R tarasevichiae, R sibirica sp BJ-90, and R raoultii (table 2; figure 2 ). Of 34 people infected with R heilongjiangiensis, 19 were diagnosed in forested areas of northeastern China in the 1990s.35, 45 The other 15 cases of infection were reported on the island of Hainan Province in 2008.43 In 2012, we undertook an active surveillance for human SFGR infections at the Mudanjiang Forestry Central Hospital of Heilongjiang Province in northeastern China, and eight cases of SFGR infection (including five infected by Candidatus R tarasevichiae, one by R sibirica sp BJ-90, and two by R raoultii) were identified by molecular detection and sequence determination. The presence of antibody against SFGR antigen in serum samples detected by immunofluorescence assay lent support to the diagnosis of SFGR.46, 48 Additionally, 37 patients were reported to have been infected with uncharacterised species of SFGR, including one in Inner Mongolia, one in Xinjiang Autonomous Region, 29 in Hainan Province, and six in Heilongjiang Province (figure 2).119, 120, 121, 122, 123, 124 The clinical manifestations of SFGR infections mainly include fever, eschar, headache, malaise, asthenia, anorexia, nausea, and lymphadenopathy. A few patients had rash and neurological manifestations such as coma, neck stiffness, and Kernig's sign.11, 35, 43, 45, 46, 48, 119, 120, 121, 122, 123, 124 Detailed information about the clinical and laboratory characteristics of patients infected with each of the emerging SFGR species are summarised in the appendix.
Figure 2.
Geographical distribution of emerging tick-borne diseases in mainland China
Human cases of SFGR infections are shown in blue; patients infected with agents in the family Anaplasmataceae in green; patients infected with agents in the complex Borrelia burgdorferi sensu lato in purple; and patients infected with agents in the genus Babesia in black. SFGR=spotted fever group rickettsiae. *Not yet formally described.
Emerging infections with agents in the family Anaplasmataceae
Seven species in the family Anaplasmataceae have been identified in mainland China, including E chaffeensis, E canis, Ehrlichia sp Tibet, A phagocytophilum, A capra, A platys, and Candidatus N mikurensis (table 1).
Tick and animal infections
The seven emerging agents in the family Anaplasmataceae are known to be associated with 17 tick species (figure 1). E chaffeensis was first detected in Amblyomma testudinarium ticks from Yunnan Province in 1996.12 Several surveys report that it infects various tick species, and is widely dispersed in mainland China.31, 54, 55, 56, 57, 58 Furthermore, E chaffeensis was detected in dogs from Shandong Province, in long-tailed ground squirrels (Citellus undulates Pallas) and gerbils from Xinjiang Autonomous Region, in the striped field mouse (Apodemus agrarius) from Heilongjiang Province, and in rodents (Rattus norvegicus, Rattus losea, Rattus flavipectus, Rattus niviventer, Mus musculus, Niviventer confucianus, and Rattus edwardsi) and hares (Lepus sinensis) from Fujian and Zhejiang provinces (appendix).36, 55, 59, 60, 61, 62 A phagocytophilum was first detected in Ixodes persulcatus from Heilongjiang Province in 1997,15 and is now the most widely encountered species in the family Anaplasmataceae over broad areas where multifarious tick species are vectors (figure 1). Additionally, A phagocytophilum infects domestic and wild animals, including cattle, sheep, goats, horses, dogs, hare, yaks, and 24 species of rodents (appendix).36, 51, 54, 55, 62, 64, 65, 66, 67, 68, 69, 70, 71, 72 A capra was first recognised in goats (Capra aegagrus hircus) and provisionally named by our group, but has since been detected in I persulcatus ticks in Heilongjiang Province.17 Although Candidatus N mikurensis was initially identified in I persulcatus and Haemaphysalis concinna ticks,18 it was subsequently detected in D silvarum, H longicornis, and various rodents from many areas of mainland China.18, 76, 77 Three other species, including E canis, Ehrlichia sp Tibet, and A platys, have not been proven to infect human beings. Data regarding infected ticks and animal hosts are shown in figure 1 and the appendix.13, 14, 16, 57, 63
Human infections
Four species of Anaplasmataceae have been identified to cause human infections in mainland China: E chaffeensis, A phagocytophilum, A capra, and Candidatus N mikurensis. The first human case of monocytic ehrlichiosis was diagnosed in a forested area of Inner Mongolia in 1999.53 Of the 12 human cases of monocytic ehrlichiosis reported, four were recorded in Inner Mongolia, two in Beijing, two in Tianjin, and four in Shandong Province (figure 2).53, 55 A cluster of ten cases of human granulocytic anaplasmosis caused by nosocomial transmission was identified in Anhui Province in 2006.73 An additional 94 cases of human granulocytic anaplasmosis have been reported, including 33 in Beijing, six in Tianjin, 41 in Shandong Province, one in Anhui Province, and four to five each in Henan and Hubei provinces and Inner Mongolia (figure 2).53, 55, 64, 74, 75 In 2015, 28 patients were reported to be infected with A capra in Heilongjiang Province.17 Seven cases of Candidatus N mikurensis infection were identified from 622 febrile patients in the same location in 2010.18 Patients with infections caused by species from the Anaplasmataceae family showed undifferentiated clinical manifestations, mainly including fever, malaise, myalgia, arthralgia, and gastrointestinal symptoms (diarrhoea, nausea, vomiting, and anorexia). Laboratory abnormalities included leucopenia, thrombocytopenia, and raised hepatic aminopherase, lactate dehydrogenase, and blood urea nitrogen (appendix).17, 18, 53, 55, 64, 73, 74, 75
Emerging infections with B burgdorferi sensu lato
B burgdorferi sensu lato was first detected in human beings and I persulcatus in China (Heilongjiang Province) in 1986.19 This isolate was later classified as B garinii by molecular biological methods in our laboratory. Five other genospecies were subsequently identified, including B valaisiana, B sinica, B afzelii, B valaisiana-related genospecies, and B burgdorferi sensu stricto (table 1).
Tick and animal infections
Over a wide geographical distribution of 25 provinces in mainland China, 26 tick species have been shown to carry B burgdorferi sensu lato (figure 1). B garinii is the most common genospecies and has been identified in many tick species (figure 1).54, 79, 80, 81, 82, 83, 84, 85, 86 B garinii has been detected in rodents from many endemic areas,23, 36, 79, 85, 87, 88 in dogs from Yunnan Province, in sheep keds (Melophagus ovinus) from Tibet, and in hares from Gansu Province (appendix).89 B afzelii is the second most common genospecies, and has been identified in the same ticks and rodents as B garinii with a similar distribution.36, 79, 81, 83, 84, 85 B valaisiana-related genospecies (a genetically related but distinct genospecies of B valaisiana) was detected in Ixodes granulatus and H longicornis from Guizhou Province, and in rodents from Guizhou and Zhejiang provinces.22, 83 Three other genospecies that have not been reported to infect human beings include B valaisiana, B sinica, and B burgdorferi sensu stricto. Data regarding infected ticks and animal hosts are shown in figure 1 and the appendix.20, 23, 86, 92, 148, 149, 150, 151, 152, 153, 154, 155, 156
Human infections
After the identification of B burgdorferi sensu lato in ticks and animals, human cases of B burgdorferi sensu lato infection have been reported frequently in almost all provinces in mainland China, except for Tibet and Shanghai metropolis (figure 2). B garinii, B afzelii, and B valaisiana-related genospecies have been reported to cause human infections (table 2).19, 21, 23, 78, 90, 91, 125 The genospecies causing thousands of cases of Lyme disease in mainland China have not been characterised.126, 127, 128, 129, 130, 131 All the uncharacterised human cases in figure 2 were classified as B burgdorferi sensu lato infections irrespective of their actual genospecies. Infections with different genospecies of B burgdorferi sensu lato might result in slightly different clinical manifestations, including erythema migrans, arthritis or arthralgia, fever, headache, and fatigue.19, 21, 23, 78, 90, 91, 125, 126, 127, 128, 129, 130, 131 Generally, clinical manifestations in mainland China are mild compared with those in USA and Europe.78
Emerging Babesia species infections
Since 1982, 11 Babesia species have been discovered in mainland China, including Ba ovis, Ba major, Ba ovata, Ba orientalis, Ba motasi, Ba caballi, Babesia sp Kashi, Babesia sp Xinjiang, Ba microti, Ba divergens, and Ba venatorum (table 1).
Tick and animal infections
The transmission of babesia is associated with 13 tick species (figure 1). Ba microti, Ba divergens, and Ba venatorum have been proven to infect human beings. Ba microti was identified in I persulcatus and H concinna ticks and in striped field mice and reed voles (Microtus fortis) from forested areas of Heilongjiang Province, in H longicornis ticks and dogs from Henan Province, and in rodents from Fujian, Zhejiang, Henan, and Heilongjiang provinces.32, 36, 58, 105, 106 Ba divergens was detected in I persulcatus, H concinna, and Haemaphysalis japonica ticks and striped field mice in several areas of Heilongjiang Province.32, 36 Ba venatorum was reported in I persulcatus ticks from forested areas of northeastern China.109 Other species of Babesia that have not been shown to infect human beings include Ba ovis, Ba major, Ba ovata, Ba orientalis, Ba motasi, Ba caballi, Babesia sp Kashi, and Babesia sp Xinjiang. Data regarding their infected ticks and animals are shown in figure 1 and the appendix.24, 25, 26, 27, 28, 29, 30, 31, 93, 94, 95, 96, 97, 98, 99, 100, 101, 102, 103
Human infections
Ba microti, Ba divergens, and Ba venatorum have been reported to cause human infections in mainland China (figure 2). A patient was diagnosed with Ba microti infection by peripheral blood and bone marrow smears and PCR assay in Zhejiang Province in 2011.104 By use of PCR, Ba microti infections were identified in an additional ten patients among 449 febrile patients with malaria-like symptoms in Yunnan Province during 2012–13.107 One patient was co-infected with Plasmodium vivax and another was co-infected with Plasmodium falciparum. Two cases of Ba divergens infection were detected from 377 patients with anaemia in Shandong Province in 2009.108 A case of babesiosis caused by Ba venatorum was reported in a child from Xinjiang Autonomous Region.33 Between 2011 and 2014, 48 cases of Ba venatorum infection were reported through our active surveillance at a sentinel hospital in forested areas of northeastern China. Among them, 32 were confirmed cases, and 16 were probable cases.109 These infections were the first report of endemic human Ba venatorum disease anywhere in the world. Additionally, two cases of babesiosis caused by uncharacterised Babesia species were reported in Yunnan Province of southwestern China in 1982 and one in 2008 (figure 2).132, 133 Clinical manifestations for patients with Babesia species infections included fever, fatigue, anaemia, chills, and high levels of hepatic aminopherase and C-reactive protein.33, 108, 104, 109, 107, 132, 133 Detailed information about the clinical manifestations of each of these species of Babesia infections is summarised in the appendix.
Emerging SFTSV infections
SFTSV is a novel member of the genus Phlebovirus in the Bunyaviridae family, and was first identified in China. The identification of SFTSV infections was made possible by enhanced active surveillance in selected provinces of China.34 Since a systematic review on the epidemiology, clinical signs, pathogenesis, diagnosis, treatment, and prevention of human infection with SFTSV has been published,157 we provide only a brief description and some new information about the infection.
Tick and animal infections
SFTSV have been reported to infect H longicornis and Rhipicephalus microplus ticks, with a higher prevalence of infection in H longicornis (4–9%) compared with in R microplus (0–6%).34, 110 Various animals, including goats, cattle, dogs, pigs, rodents, chickens, geese, and hedgehogs, might be infected by this pathogen.110, 111 Studies in Shandong, Jiangsu, and Hubei provinces showed that goats and cattle had the highest seropositive rate. Furthermore, big animals usually had higher seropositive rates than small animals.111, 112
Human infections
As of 2013, 2543 human SFTS infections have been reported to the China Center For Disease Control And Prevention, including 154 deaths.34, 113, 114, 115, 116, 117, 118 Incidence hotspots are located in Henan, Hubei, Anhui, and Shandong provinces of middle-eastern China, in addition to Liaoning Province of northeastern China (appendix). Clinical manifestations in patients with SFTS are non-specific with major symptoms including respiratory tract symptoms, sudden onset of fever up to 38–41°C, headache, fatigue, myalgia, and gastrointestinal symptoms (loss of appetite, nausea, vomiting, and diarrhoea). Multiple organ failure develops rapidly in most patients (with raised concentrations of serum alanine aminotransferase, aspartate aminotransferase, creatine kinase, and lactate dehydrogenase; and proteinuria and haematuria), and is usually accompanied by thrombocytopenia, leucocytopenia, and lymphadenopathy.34, 117
Factors contributing to the emergence of tick-borne infections
Beyond doubt, advances in and application of molecular technologies have resulted in the discovery of novel agents and helped to identify human infections caused by agents previously detected in ticks. Thus, to some extent, the emergence of tick-borne infections has resulted from the discovery of novel pathogens through the use of more sensitive and reliable detection methods. However, various biological factors, such as tick and host population dynamics, which have caused an increase in the transmission and dissemination of tick-borne zoonotic diseases, are probably the main reasons for the emergence of these infections.3
Changes in land use have affected the emergence of tick-borne zoonotic diseases by altering the interactions and abundance of ticks, wild and domestic hosts, and human exposure to pathogens.158 An example is the emergence of Lyme disease in northeastern USA. Reforestation of this region during the 20th century is thought to have increased the population of white-tailed deer, which greatly amplified the number of Ixodes scapularis. Consequentially, vector tick densities grew and expanded, contributing substantially to the emergence of Lyme disease in the USA.159 Fragmentation of forests in eastern regions of Canada and the USA might have increased the relative abundance of small mammals because of a reduction in predator communities, leading to an increase in B burgdorferi sensu lato infection rates in I scapularis nymphs. Ultimately, people in these areas were confronted with a higher risk of Lyme disease.160, 161
Since the mid-1990s, the Chinese central government has initiated the Greening Program to regain forests and grasslands from former agricultural lands.162 Reforestation and grass replanting with high-quality vegetative cover could have increased the abundance and diversity of ticks and animal hosts, and favoured the re-establishment of pre-existing tick vector enzootic cycles in these areas. One example described in our study was in the most severely endemic region of SFTS. Our findings showed that the incidence of SFTS is significantly associated with vegetation-rich lands. A 10% increase in shrub, forest, and rain-fed cropland areas resulted in increased human SFTS incidence rates of 51%, 51%, and 90%, respectively.163
Additionally, urbanisation has affected the emergence and increasing incidence of tick-borne diseases. Studies in Europe suggest that encroachment into forested and uncultivated areas, and protection of existing green spaces in the process of urbanisation, have created opportunities for ticks to survive in urban and especially suburban environments. The presence of many pets and domestic animals, which can serve as tick hosts and pathogen reservoirs, might help tick transmission of various human and animal pathogens.164, 165 In the past three decades, China has gone through the most rapid urbanisation in its history. This rapid urbanisation, followed by widespread rural-to-urban migration of the human population, intensive long-distance trade, and explosive short-term travel for shopping, has led to substantial health risks including air pollution, occupational and traffic hazards, and altered diets and activity.166 All of these changes in human activity, together with increased contact between human beings and their pets and nature, have probably contributed to the increasing abundance of tick exposure, as reported in other developed countries.164 Further investigation is needed to show the relation between emerging tick-borne diseases and urbanisation in mainland China.
The effect of worldwide climate change on the emergence of most vector-borne zoonotic diseases (including tick-borne diseases) is thought to be less important than changes in land use, animal host communities, human living conditions, and societal factors.3 Although the effects of climate on transmission of infectious diseases are thought to be non-linear and act in opposing directions in different climate regions, the seasonal dynamics of tick vectors are largely defined by climate conditions, which might further affect the seasonal pattern of tick-borne diseases. An increase in winter temperatures is known to cause the northward extension and increased abundance of Ixodes ricinus, which subsequently raises the risk of tick-borne disease dissemination.167, 168, 169 Although this topic is still under debate, climatic change could have a role in the emergence of tick-borne diseases in China. Further studies are needed to better elucidate this issue.
Perspectives
Ticks are thought to be second only to mosquitoes as worldwide vectors of human infectious diseases.170 Up to now, more than 120 tick species have been identified in China, including over 100 species in the Ixodidae (so-called hard tick) family and 19 species in the Argasidae (soft tick) family.171 They transmit several pathogens when feeding on a range of animals, including human beings as accidental hosts. About 30 tick species are reported to feed on human beings.172, 173 The diverse geographical distribution and abundance of ticks are dependent on optimum environmental conditions and biotopes for each tick species, which define the risk areas for corresponding tick-borne zoonoses.3 In addition to the emerging tick-borne infections, previously documented and well established tick-borne diseases are a continuing threat to human health, including tick-borne encephalitis in northeastern China, Crimean-Congo haemorrhagic fever in northwestern China, tularaemia and north-Asia tick-borne spotted fever in northern China, and Q fever, which is widely distributed throughout China.174, 175, 176, 177, 178, 179, 180, 181, 182, 183
The non-specific clinical manifestations caused by tick-borne pathogens, such as SFGR, Anaplasma species, B burgdorferi sensu lato, Babesia species, and SFTSV, present a major diagnostic challenge. Most physicians are unfamiliar with the many tick-borne diseases that present with non-specific symptoms in the early stages of the illness. The wide distributions of the 33 emerging tick-associated agents and their tick vectors, in addition to the diversity of tick species throughout mainland China, imply that reported cases of infection might be only the tip of the iceberg in regard to the actual number of tick-borne diseases. To develop a reasonable differential diagnosis and identify a specific pathogen, laboratory diagnostic methods that are rapid, convenient, and practical are urgently needed for these emerging tick-borne diseases. Although great progress has been made in mainland China in the detection and identification of various tick-borne pathogens and diagnosis of the infections they cause, the necessary technologies are still unavailable in most general hospitals. Unfortunately, the importance of tick-borne diseases to human and animal health has not been sufficiently recognised as a result of inaccessibility to laboratory tests for aetiological diagnosis and inadequate surveillance activities.
In China, 18 tick-borne agents have been detected in ticks or animals, including four Rickettsia species, two Ehrlichia species, an Anaplasma species, three genospecies of B burgdorferi sensu lato, and eight Babesia species; however, the full effect of their pathogenicity to human beings is still to be established. Despite increasing knowledge about their geographical distribution, the natural cycle of these agents and the natural history of their infection in tick vectors and animal hosts have yet to be elucidated. Identifying human infections after potentially pathogenic agents are identified in ticks could take many years, in part because the microbial loads are much lower in human blood than in arthropods.184 For example, R sibirica sp BJ-90 was first identified in D sinicus ticks in China in 1990,7 but was not discovered to infect human beings until 22 years later.46 Similarly, A phagocytophilum was initially detected in China in 1997;15 however, nosocomial transmission of human granulocytic anaplasmosis was not recognised until 10 years later.73 As such, the 18 tick-associated agents that have been recognised in China in either ticks or animals represent potential candidates for new tick-borne human diseases. Likewise, a search for potential new pathogens in ticks is essential for the discovery of emerging tick-borne diseases in human beings.
Conclusion
33 tick species belonging to six genuses have been reported to be naturally infected with the emerging pathogenic agents described in this Review (figure 1). Except for eight species (Dermacentor abaensis, Dermacentor daghestanicus, Haemaphysalis bispinosa, H flava, Haemaphysalis sinensis, Haemaphysalis yeni, Ixodes myospalacis, and Rhipicephalus turanicus), most species carry two or more agents. Conversely, some emerging agents such as R heilongjiangensis, E chaffeensis, A phagocytophilum, and B garinii can infect several tick species. Additionally, tick-borne pathogens that infect domestic animals might eventually cause human disease. A representative example is B divergens, which has long been recognised to cause cattle babesiosis in Europe, and was subsequently identified as a human pathogen.185 In China, a wide range of emerging tick-borne agents are known to infect various domestic animals (appendix), and their potential capability to infect humans warrants great attention and further investigation. With the continued emergence of tick-borne diseases in mainland China, improving our understanding of the existence and health burden of these diseases is essential for China and for the rest of the world.
Search strategy and selection criteria
We searched PubMed and ISI Web of Science for articles published in English, and WanFang database, China National Knowledge Infrastructure, and Chinese Scientific Journal Database for articles published in Chinese between Jan 1, 1980, and May 31, 2015. We used the following search terms: “tick-borne disease”, “tick-borne zoonosis”, “tick-borne zoonotic disease”, “tick-associated agent”, “tick-associated microbe”, and “China”, in combination with each of the five genera of tick-borne agents. We did a secondary manual search of the references cited in these articles to find relevant articles. We investigated all the articles related to detection, identification, or infections of these five genera of tick-borne microbes in human beings, ticks, and animals. We contacted the corresponding authors for detailed information such as the time of discovery, location, and origin of tick-borne agents if any of this information was missing in the articles.
Contributors
L-QF, SL, XFY, GCG, PJK, and W-CC initiated the original ideas for the review. KL, X-LL, H-WY, RXS, YS, and W-JC contributed to the literature search and extracted data. KL, X-LL, H-WY, YY, SL, S-QZ, M-JM, HL, J-FJ, and WL assessed the data. L-QF, KL, X-LL, H-WY, R-XS, YS, W-JC, and W-CC created the figures. L-QF, GCG, and W-CC wrote the draft, and all authors contributed to the review and revision of the paper.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
This work was supported by the Natural Science Foundation of China (81290344, 81130086, and 81172728), the Special Program for Prevention and Control of Infectious Diseases in China (number 2013ZX10004218), the Basic Work on Special Program for Science & Technology Research (2013FY114600), and National Institutes of Health–National Institute of Allergy and Infectious Diseases (5R01AI083640 to XFY). The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Contributors
L-QF, SL, XFY, GCG, PJK, and W-CC initiated the original ideas for the review. KL, X-LL, H-WY, RXS, YS, and W-JC contributed to the literature search and extracted data. KL, X-LL, H-WY, YY, SL, S-QZ, M-JM, HL, J-FJ, and WL assessed the data. L-QF, KL, X-LL, H-WY, R-XS, YS, W-JC, and W-CC created the figures. L-QF, GCG, and W-CC wrote the draft, and all authors contributed to the review and revision of the paper.
Declaration of interests
We declare no competing interests.
Supplementary Material
References
- 1.Dantas-Torres F, Chomel BB, Otranto D. Ticks and tick-borne diseases: a One Health perspective. Trends Parasitol. 2012;28:437–446. doi: 10.1016/j.pt.2012.07.003. [DOI] [PubMed] [Google Scholar]
- 2.Socolovschi C, Mediannikov O, Raoult D, Parola P. The relationship between spotted fever group Rickettsiae and ixodid ticks. Vet Res. 2009;40:34. doi: 10.1051/vetres/2009017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kilpatrick AM, Randolph SE. Drivers, dynamics, and control of emerging vector-borne zoonotic diseases. Lancet. 2012;380:1946–1955. doi: 10.1016/S0140-6736(12)61151-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang L, Wang Y, Jin S. Emergence and control of infectious diseases in China. Lancet. 2008;372:1598–1605. doi: 10.1016/S0140-6736(08)61365-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lou D, Wu YM, Wang B. A new specie in Rickettsia: isolation and identification of Rickettsia heilongjiangii. Chin J Microbiol Immunol. 1985;5:250. (in Chinese). [Google Scholar]
- 6.Zhang L, Raoult D, Fournier PE. ‘Rickettsia hulinii’ belongs to the Rickettsia heilongjiangensis species. Clin Microbiol Infect. 2009;15(suppl 2):340–342. doi: 10.1111/j.1469-0691.2008.02267.x. [DOI] [PubMed] [Google Scholar]
- 7.Yu X, Jin Y, Fan M, Xu G, Liu Q, Raoult D. Genotypic and antigenic identification of two new strains of spotted fever group rickettsiae isolated from China. J Clin Microbiol. 1993;31:83–88. doi: 10.1128/jcm.31.1.83-88.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li W, Liu L, Jiang X. Molecular identification of spotted fever group Rickettsiae in ticks collected in central China. Clin Microbiol Infect. 2009;15(suppl 2):279–280. doi: 10.1111/j.1469-0691.2008.02235.x. [DOI] [PubMed] [Google Scholar]
- 9.Tian ZC, Liu GY, Shen H, Xie JR, Luo J, Tian MY. First report on the occurrence of Rickettsia slovaca and Rickettsia raoultii in Dermacentor silvarum in China. Parasit Vectors. 2012;5:19. doi: 10.1186/1756-3305-5-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou Y, Wang Q, Fu Z. Detection of spotted fever group Rickettsia in Haemaphysalis longicornis from Hebei Province, China. J Parasitol. 2011;97:960–962. doi: 10.1645/GE-2751.1. [DOI] [PubMed] [Google Scholar]
- 11.Jia N, Zheng YC, Jiang JF, Ma L, Cao WC. Human infection with Candidatus Rickettsia tarasevichiae. N Engl J Med. 2013;369:1178–1180. doi: 10.1056/NEJMc1303004. [DOI] [PubMed] [Google Scholar]
- 12.Cao WC, Gao YM, Zhang PH. Identification of Ehrlichia chaffeensis by nested PCR in ticks from Southern China. J Clin Microbiol. 2000;38:2778–2780. doi: 10.1128/jcm.38.7.2778-2780.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pan H, Chen XR, Ma YH. Ehrlichia canis DNA found in ticks in the south of China. Chin J Zoonoses. 1999;15:3–6. (in Chinese). [Google Scholar]
- 14.Wen B, Jian R, Zhang Y, Chen R. Simultaneous detection of Anaplasma marginale and a new Ehrlichia species closely related to Ehrlichia chaffeensis by sequence analyses of 16S ribosomal DNA in Boophilus microplus ticks from Tibet. J Clin Microbiol. 2002;40:3286–3290. doi: 10.1128/JCM.40.9.3286-3290.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cao WC, Zhao QM, Zhang PH. Granulocytic Ehrlichiae in Ixodes persulcatus ticks from an area in China where Lyme disease is endemic. J Clin Microbiol. 2000;38:4208–4210. doi: 10.1128/jcm.38.11.4208-4210.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hua P, Yuhai M, Shide T, Yang S, Bohai W, Xiangrui C. Canine ehrlichiosis caused simultaneously by Ehrlichia canis and Ehrlichia platys. Microbiol Immunol. 2000;44:737–739. doi: 10.1111/j.1348-0421.2000.tb02557.x. [DOI] [PubMed] [Google Scholar]
- 17.Li H, Zheng YC, Ma L. Human infection with a novel tick-borne Anaplasma species in China: a surveillance study. Lancet Infect Dis. 2015;15:663–670. doi: 10.1016/S1473-3099(15)70051-4. [DOI] [PubMed] [Google Scholar]
- 18.Li H, Jiang JF, Liu W. Human infection with Candidatus Neoehrlichia mikurensis, China. Emerg Infect Dis. 2012;18:1636–1639. doi: 10.3201/eid1810.120594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ai CX, Wen YX, Zhang YG. Clinical manifestations and epidemiological characteristics of Lyme disease in Hailin county, Heilongjiang Province, China. Ann N Y Acad Sci. 1988;539:302–313. doi: 10.1111/j.1749-6632.1988.tb31864.x. [DOI] [PubMed] [Google Scholar]
- 20.Masuzawa T, Takada N, Kudeken M. Borrelia sinica sp. nov., a lyme disease-related Borrelia species isolated in China. Int J Syst Evol Microbiol. 2001;51:1817–1824. doi: 10.1099/00207713-51-5-1817. [DOI] [PubMed] [Google Scholar]
- 21.Shi CX, Zhang ZF, Wan KL. Analyzing clinical samples of Lyme disease with 5s-23s rRNA gene spacer RFLP analysis. Chin J Zoonoses. 2000;16:21–23. (in Chinese). [Google Scholar]
- 22.Chu CY, Liu W, Jiang BG. Novel genospecies of Borrelia burgdorferi sensu lato from rodents and ticks in southwestern China. J Clin Microbiol. 2008;46:3130–3133. doi: 10.1128/JCM.01195-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hao Q, Hou X, Geng Z, Wan K. Distribution of Borrelia burgdorferi sensu lato in China. J Clin Microbiol. 2011;49:647–650. doi: 10.1128/JCM.00725-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Chen DM. Investigation report on sheep babesiosis with Piroplasma ovis infection. Chin J Vet Sci Technol. 1982;12:31–32. (in Chinese). [Google Scholar]
- 25.Lv WS, Yin H, Lv WX, Yu F, Zhang QC, Dou HF. Detection of Babesia major and the identification of its tick vector in mainland China. Chin J Vet Sci Technol. 1988;18:11–14. (in Chinese). [Google Scholar]
- 26.Bai Q, Liu GY, Zhang L, Zhang JY. Discovery and isolation of Babesia ovata in China. Chin J Vet Sci Technol. 1990;20:2–4. (in Chinese). [Google Scholar]
- 27.Liu ZL, Zhao JL, Ma LH, Yao BA. Babesia orientalis sp. nov. parasitized in buffalo Bubalus bubalis in China (Piroplasmida: Babesiidae) Acta Veterinaria et Zootechnica Sinica. 1997;28:84–89. (in Chinese). [Google Scholar]
- 28.Yin H, Luo JX, Lv WS. Isolation and configuration observation of Babesia motasi and Babesia ovis in mainland China. Chin J Vet Sci Technol. 1997;27:7–9. (in Chinese). [Google Scholar]
- 29.Li YZ, Lu WY, Song JG. Studies on etiology and integrated control measures of difficult equine diseases in Gansu Province, China. J Chin Agric Univ. 1998;S2:130. (in Chinese). [Google Scholar]
- 30.Luo J, Yin H, Liu Z. Molecular phylogenetic studies on an unnamed bovine Babesia sp. based on small subunit ribosomal RNA gene sequences. Vet Parasitol. 2005;133:1–6. doi: 10.1016/j.vetpar.2005.02.014. [DOI] [PubMed] [Google Scholar]
- 31.Liu AH, Yin H, Guan GQ. At least two genetically distinct large Babesia species infective to sheep and goats in China. Vet Parasitol. 2007;147:246–251. doi: 10.1016/j.vetpar.2007.03.032. [DOI] [PubMed] [Google Scholar]
- 32.Yang LW, Hou Y, Li M, Wen ZQ, Yang J, Fan DH. Study of tick-borne pathogens at Heilongjiang Port. Chin Front Health Q. 2007;30:77–82. (in Chinese). [Google Scholar]
- 33.Sun Y, Li SG, Jiang JF. Babesia venatorum infection in child, China. Emerg Infect Dis. 2014;20:896–897. doi: 10.3201/eid2005.121034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yu XJ, Liang MF, Zhang SY. Fever with thrombocytopenia associated with a novel bunyavirus in China. N Engl J Med. 2011;364:1523–1532. doi: 10.1056/NEJMoa1010095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wu YM, Wei AM, Hu LM. Study on aetiology of Rickettsia heilongianggii tick borne spotted fever. Chin Public Health. 2001;7:28–30. (in Chinese). [Google Scholar]
- 36.Hu MX, Zhang J, Fan DH, Fu WM, Sun XF, Yang LW. Detection of rodent infected by new tick pathogens in Suifenhe and Dongning Ports. Chin J Vector Biol Control. 2009;20:573–576. (in Chinese). [Google Scholar]
- 37.Sun XF, Ding SL, Hu MX, Guo XM, Zhao G. Study on tick-borne Rickettsia dermacentroxenus infection at Heilongjiang Port. Chin Front Health Q. 2007;30:154–156. (in Chinese). [Google Scholar]
- 38.Wu YM, Liu GP, Wei AM. Investigation of spotted fever group Rickettsia in the northeastern China. Chin J Public Health. 2003;19:1043–1044. (in Chinese). [Google Scholar]
- 39.Hao GF, Li H, Sun Y. Detection of tick and tick-borne pathogen in some ports of Inner Mongolia. Zhonghua Liu Xing Bing Xue Za Zhi. 2009;30:365–367. (in Chinese). [PubMed] [Google Scholar]
- 40.Li Y, Li ZK, Chen G, Kang M, Liu DX, Zhang YM. Identification and phylogenetic analysis of spotted fever group Rickettsia isolated from Qinghai province. Chin J Vet Sci. 2014;34:1956–1961. (in Chinese). [Google Scholar]
- 41.Zhang LJ, Zhang JS, Fu XP, Luan MC. First identification of a Rickettsia closely related to R. heilongjiangii and R. massilliae in South China. Infect Dis Inf. 2006;19:65–67. (in Chinese). [Google Scholar]
- 42.Liang CW, Zhao JB, Li J. Spotted fever group Rickettsia in Yunnan Province, China. Vector Borne Zoonotic Dis. 2012;12:281–286. doi: 10.1089/vbz.2011.0835. [DOI] [PubMed] [Google Scholar]
- 43.Jin YM, Zhang LJ, Sun LY. Epidemiological investigation of emerging spotted fever in Chengmai County, Hainan Province. Dis Surveill. 2011;26:18–22. (in Chinese). [Google Scholar]
- 44.Sun J, Lin J, Gong Z. Detection of spotted fever group Rickettsiae in ticks from Zhejiang Province, China. Exp Appl Acarol. 2015;65:403–411. doi: 10.1007/s10493-015-9880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu YM, Wei AM, Hu LM. Identification of spotted fever group (SFG) H-5 strain isolated from the patient's blood samples. Chin J Zoonoses. 1998;14:23–26. (in Chinese). [Google Scholar]
- 46.Jia N, Jiang JF, Huo QB, Jiang BG, Cao WC. Rickettsia sibirica subspecies sibirica BJ-90 as a cause of human disease. N Engl J Med. 2013;369:1176–1178. doi: 10.1056/NEJMc1303625. [DOI] [PubMed] [Google Scholar]
- 47.Ye X, Sun Y, Ju W, Wang X, Cao W, Wu M. Vector competence of the tick Ixodes sinensis (Acari: Ixodidae) for Rickettsia monacensis. Parasit Vectors. 2014;7:512–518. doi: 10.1186/s13071-014-0512-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jia N, Zheng YC, Ma L. Human infections with Rickettsia raoultii, China. Emerg Infect Dis. 2014;20:866–868. doi: 10.3201/eid2005.130995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Sun X, Zhang GL, Liu R, Liu XM, Zhao Y, Zheng Z. Molecular epidemiological study of Rickettsia raoultii in ticks from Xinjiang, China. Zhonghua Liu Xing Bing Xue Za Zhi. 2013;34:756–757. (in Chinese). [PubMed] [Google Scholar]
- 50.Zhuang L, Wang CY, Tong YG. Discovery of Rickettsia species in Dermacentor niveus Neumann ticks by investigating the diversity of bacterial communities. Ticks Tick Borne Dis. 2014;5:564–568. doi: 10.1016/j.ttbdis.2014.04.004. [DOI] [PubMed] [Google Scholar]
- 51.Dong X, Chen XP, Liu N, Dumler SJ, Zhang YZ. Co-circulation of multiple species of Rickettsiales bacteria in one single species of hard ticks in Shenyang, China. Ticks Tick Borne Dis. 2014;5:727–733. doi: 10.1016/j.ttbdis.2014.05.011. [DOI] [PubMed] [Google Scholar]
- 52.Feng S, Wu H, Zhang LW. Molecular epidemiological study of tick-borne spotted fever group Rickettsia in western mountain area of Hebei Province, China. Chin J Vector Biol Control. 2013;24:308–312. (in Chinese). [Google Scholar]
- 53.Gao D, Cao W, Zhang X. Investigations on human ehrlichia infectious people in Daxingan Mountains. Zhonghua Liu Xing Bing Xue Za Zhi. 2001;22:137–141. (in Chinese). [PubMed] [Google Scholar]
- 54.Sun X, Zhang GL, Liu XM, Zhao Y, Zheng Z. Investigation of tick species and tick-borne pathogens in Hoxud County of Xinjiang Uyghur Autonomous Region, China. Chin J Vector Biol Control. 2013;24:5–10. (in Chinese). [Google Scholar]
- 55.Dong T, Qu Z, Zhang L. Detection of A. phagocytophilum and E. chaffeensis in patient and mouse blood and ticks by a duplex real-time PCR assay. PLoS One. 2013;8:e74796. doi: 10.1371/journal.pone.0074796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Li HM, Jiang BG, He J. Detection and identification of Ehrlichia sp. in Boophilus microplus ticks from Xiamen of Fujian Province. J Pathog Biol. 2006;1:174–176. (in Chinese). [Google Scholar]
- 57.Meng QL, Qiao J, Sheng JL. Survey on tick-borne Anaplasmataceae in the south edge of Gurbantunggut desert. Chin J Vet Sci. 2012;32:1158–1163. (in Chinese). [Google Scholar]
- 58.Chen Z, Liu Q, Liu JQ. Tick-borne pathogens and associated co-infections in ticks collected from domestic animals in central China. Parasit Vectors. 2014;7:237. doi: 10.1186/1756-3305-7-237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhang L, Cui F, Wang L. Investigation of anaplasmosis in Yiyuan County, Shandong Province, China. Asian Pac J Trop Med. 2011;4:568–572. doi: 10.1016/S1995-7645(11)60148-X. [DOI] [PubMed] [Google Scholar]
- 60.Zhao QL, Huang L, Yang X. 16s rRNA sequence analysis of Anaplasma and Ehrlichia in rodents from parts area of Xinjiang. Chin J Zoonoses. 2013;29:743–747. (in Chinese). [Google Scholar]
- 61.Gao YM, Zhang XT, Cao WC. Detection of Ehrlichia chaffeensis in ticks and rodents using semi-nested PCR. Chin J Zoonoses. 2000;16:25–28. (in Chinese). [Google Scholar]
- 62.Xu Z, Xu XH, Zhou YL. Comprehensive surveillance of tick-borne diseases in Jiande, Zhejiang province, China. Chin J Vector Biol Control. 2014;25:350–353. (in Chinese). [Google Scholar]
- 63.Li Y, Chen Z, Liu Z. Molecular survey of Anaplasma and Ehrlichia of red deer and sika deer in Gansu, China in 2013. Transbound Emerg Dis. 2015 doi: 10.1111/tbed.12335. published online Feb 7. [DOI] [PubMed] [Google Scholar]
- 64.Zhang L, Wang G, Liu Q. Molecular analysis of Anaplasma phagocytophilum isolated from patients with febrile diseases of unknown etiology in China. PLoS One. 2013;8:e57155. doi: 10.1371/journal.pone.0057155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhang L, Liu H, Xu B. Anaplasma phagocytophilum infection in domestic animals in ten provinces/cities of China. Am J Trop Med Hyg. 2012;87:185–189. doi: 10.4269/ajtmh.2012.12-0005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Li GH, Yu Q, Zhang QX. Molecular epidemiology regarding Anaplasma phagocytophilum in Dermacentor silvarum in Ningwu county, Shanxi province. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33:642–643. (in Chinese). [PubMed] [Google Scholar]
- 67.Jiang JF, Jiang BG, Yu JH. Anaplasma phagocytophilum infection in ticks, China–Russia border. Emerg Infect Dis. 2011;17:932–934. doi: 10.3201/eid1705.101630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Li Y, Kang FY, Yang JF, Sun CQ, Liu ZJ, Yin H. Prevalence and coexistence of Anaplasma phagocytophilum and Borrelia burgdorferi sensu lato in ticks in Gansu, Hunan and Guangdong provinces, China. Chin J Zoonoses. 2013;29:117–121. (in Chinese). [Google Scholar]
- 69.Yang J, Liu Z, Guan G. Prevalence of Anaplasma phagocytophilum in ruminants, rodents and ticks in Gansu, north-western China. J Med Microbiol. 2013;62:254–258. doi: 10.1099/jmm.0.046771-0. (in Chinese). [DOI] [PubMed] [Google Scholar]
- 70.Cao WC, Zhao QM, Zhang PH. Prevalence of Anaplasma phagocytophila and Borrelia burgdorferi in Ixodes persulcatus ticks from northeastern China. Am J Trop Med Hyg. 2003;68:547–550. doi: 10.4269/ajtmh.2003.68.547. [DOI] [PubMed] [Google Scholar]
- 71.Zhang HL, Sun Y, Wang JJ. Investigation on foci severe fever with thrombocytopenia syndrome and human granulocytic anaplasmosis in Lujiang County. Chin J Dis Control Prev. 2015;19:273–276. (in Chinese). [Google Scholar]
- 72.Zhang YZ, Wang Y, Yang WH. Seroprevalence and molecular biological investigation of commonly known Rickettsia species in rodents in Qujing Prefecture, Yunnan Province, China. Chin J Zoonoses. 2015;31:35–40. (in Chinese). [Google Scholar]
- 73.Zhang L, Liu Y, Ni D. Nosocomial transmission of human granulocytic anaplasmosis in China. JAMA. 2008;300:2263–2270. doi: 10.1001/jama.2008.626. [DOI] [PubMed] [Google Scholar]
- 74.Wang S, Kou ZQ, Wang M. A survey and identification of co-infection of Anaplasma phagocytophilum and Ehrlichia chaffeensis in Shandong. Dis Surveill. 2012;27:642–643. (in Chinese). [Google Scholar]
- 75.Li Z, Ding SJ, Lv H, Chen Y, Hou PQ, Wang XJ. Investigation of one case of human granulocytic anaplasmosis in Shandong Province. Infect Dis Inf. 2009;22:165–168. (in Chinese). [Google Scholar]
- 76.Li H, Jiang J, Tang F. Wide distribution and genetic diversity of “Candidatus Neoehrlichia mikurensis” in rodents from China. Appl Environ Microbiol. 2013;79:1024–1027. doi: 10.1128/AEM.02917-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lu QY, Cheng SY, Peng WL, Zhao JL, Jiang LP, Ge JH. Candidatus Neoehrlichia mikurensis infection on animals and related 16S rRNA gene analysis in Zhejiang province. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33:993–994. (in Chinese). [PubMed] [Google Scholar]
- 78.Ni XB, Jia N, Jiang BG. Lyme borreliosis caused by diverse genospecies of Borrelia burgdorferi sensu lato in northeastern China. Clin Microbiol Infect. 2014;20:808–814. doi: 10.1111/1469-0691.12532. [DOI] [PubMed] [Google Scholar]
- 79.Li M, Masuzawa T, Takada N. Lyme disease Borrelia species in northeastern China resemble those isolated from far eastern Russia and Japan. Appl Environ Microbiol. 1998;64:2705–2709. doi: 10.1128/aem.64.7.2705-2709.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jiang B, Yao H, Tong Y. Genome sequence of Borrelia garinii strain NMJW1, isolated from China. J Bacteriol. 2012;194:6660–6661. doi: 10.1128/JB.01844-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Chu CY, Jiang BG, He J. Genetic diversity of Borrelia burgdorferi sensu lato isolates from Northeastern China. Vector Borne Zoonotic Dis. 2011;11:877–882. [PubMed] [Google Scholar]
- 82.Shi SG, Zhang F, Liu ZJ. Molecular epidemiological studies on Borrelia burgdorferii in ticks collected from several provinces and autonomous regions of northwestern China. Chin J Zoonoses. 2011;27:461–463. (in Chinese). [Google Scholar]
- 83.Chu CY, Jiang BG, Liu W. Presence of pathogenic Borrelia burgdorferi sensu lato in ticks and rodents in Zhejiang, south-east China. J Med Microbiol. 2008;57:980–985. doi: 10.1099/jmm.0.47663-0. (in Chinese). [DOI] [PubMed] [Google Scholar]
- 84.Wang HW, He J, Chu CY. Detection and genotyping of Borrelia burgdorferi sensu lato in ticks from some areas of China. J Pathog Biol. 2006;1:81–85. (in Chinese). [Google Scholar]
- 85.Zhang JJ, Zhang F, Li L, Liu ZJ. Borrelia burgdorferi infection and their genotypes in ticks and rodents collected from Maijishan region, Gansu Province, China. Chin J Zoonoses. 2015;31:357–360. (in Chinese). [Google Scholar]
- 86.Hou J, Ling F, Chai C. Prevalence of Borrelia burgdorferi sensu lato in ticks from eastern China. Am J Trop Med Hyg. 2015;92:262–266. doi: 10.4269/ajtmh.14-0587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Chu CY, He J, Zhao QM. Molecular epidemiological studies on Borrelia burgdorferi in rodents collected in the forest area of several provinces and autonomous regions of China. Chin J Zoonoses. 2006;22:817–820. (in Chinese). [Google Scholar]
- 88.Hou XX, Geng Z, Hao Q, Zhang Y, Wan KL. Rats, the primary reservoir hosts of Borrelia burgdorferi in six representative provinces, China. Chin J Zoonoses. 2010;26:1034–1036. (in Chinese). [Google Scholar]
- 89.Zhan L, Chu CY, Zuo SQ. Anaplasma phagocytophilum and Borrelia burgdorferi in rabbits from southeastern China. Vet Parasitol. 2009;162:354–356. doi: 10.1016/j.vetpar.2009.03.003. [DOI] [PubMed] [Google Scholar]
- 90.Tan YH, Liu Y, Wan KL. Molecular epidemiological study of Borrelia burgdorferi infection among population in Xinjiang, China. Chin J Vector Biol Control. 2013;24:297–300. (in Chinese). [Google Scholar]
- 91.Zhu X, Zhang L, Hou XB. Investigation on Lyme disease of patients with arthrities or neurological disorders in Hainan province, China. Chin J Zoonoses. 2015;31:353–356. (in Chinese). [Google Scholar]
- 92.Zhang L, Wang Y, Chen C. Isolation of Borrelia burgdorferi in ixodes from four counties, in North Xinjiang. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35:262–265. (in Chinese). [PubMed] [Google Scholar]
- 93.Li W, Peng HS, Li XM. Diagnosis and treatment of a goat infected with Babesia ovis. Contemp Anim Hus. 2015;1:12–13. (in Chinese). [Google Scholar]
- 94.Luo JX, Yin H, Liu GY. Collection and identification of piroplasma infected to cattle and sheep in China. Chin J Parasitol Parasit Dis. 2006;24:S48–S52. (in Chinese). [Google Scholar]
- 95.Bai Q, Liu G, Han G, Hui Y. Isolation and complementary transmission of Babesia ovata in Zhangjiachuan of Gansu Province. Chin J Vet Sci Technol. 1994;24:9–10. (in Chinese). [Google Scholar]
- 96.He L, Feng HH, Zhang WJ. Occurrence of Theileria and Babesia species in water buffalo (Bubalus babalis, Linnaeus, 1758) in the Hubei province, South China. Vet Parasitol. 2012;186:490–496. doi: 10.1016/j.vetpar.2011.11.021. [DOI] [PubMed] [Google Scholar]
- 97.Liu Q, Zhou YQ, Zhou DN. Semi-nested PCR detection of Babesia orientalis in its natural hosts Rhipicephalus haemaphysaloides and buffalo. Vet Parasitol. 2007;143:260–266. doi: 10.1016/j.vetpar.2006.08.016. [DOI] [PubMed] [Google Scholar]
- 98.Niu Q, Luo J, Guan G. Detection and differentiation of ovine Theileria and Babesia by reverse line blotting in China. Parasitol Res. 2009;104:1417–1423. doi: 10.1007/s00436-009-1344-x. [DOI] [PubMed] [Google Scholar]
- 99.Sun C, Liu Z, Gao J. Investigations into the natural infection rate of Haemaphysalis qinghaiensis with piroplasma using a nested PCR. Exp Appl Acarol. 2008;44:107–114. doi: 10.1007/s10493-008-9133-2. [DOI] [PubMed] [Google Scholar]
- 100.He SD, Che FM, Liu WQ. Investigation of Babesia caballi in areas around Qinghai Lake, China. Chin Anim Health Insp. 2007;24:28. (in Chinese). [Google Scholar]
- 101.Wang XS, Liu JY, Zhang L, Feng LG. Case report of horse Babesia caballi infection. Anim Breed Feed. 2014;12:56–57. (in Chinese). [Google Scholar]
- 102.Yi CY, Guo QY, Xue H, Peng C, Ba YCH. Detection of pathogen DNA of Babesia caballi from Rhipicephalus sanguineus and Dermacentor nuttalli. Heilongjiang Anim Sci Vet Med. 2014;11:38–40. (in Chinese). [Google Scholar]
- 103.Guan G, Ma M, Moreau E. A new ovine Babesia species transmitted by Hyalomma anatolicum anatolicum. Exp Parasitol. 2009;122:261–267. doi: 10.1016/j.exppara.2009.05.001. [DOI] [PubMed] [Google Scholar]
- 104.Lei YL, Wang XG, Yao LN. Case report of human Babesia infections. Chin J Health Lab Technol. 2012;22:651–652. (in Chinese). [Google Scholar]
- 105.Sun Y, Liu G, Yang L, Xu R, Cao W. Babesia microti-like rodent parasites isolated from Ixodes persulcatus (Acari: Ixodidae) in Heilongjiang Province, China. Vet Parasitol. 2008;156:333–339. doi: 10.1016/j.vetpar.2008.05.026. [DOI] [PubMed] [Google Scholar]
- 106.Zhao XG, Li H, Sun Y. Dual infection with Anaplasma phagocytophilum and Babesia microti in a Rattus norvegicus, China. Ticks Tick Borne Dis. 2013;4:399–402. doi: 10.1016/j.ttbdis.2013.04.002. [DOI] [PubMed] [Google Scholar]
- 107.Zhou X, Li SG, Chen SB. Co-infections with Babesia microti and Plasmodium parasites along the China–Myanmar border. Infect Dis Poverty. 2013;2:24. doi: 10.1186/2049-9957-2-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Qi C, Zhou D, Liu J. Detection of Babesia divergens using molecular methods in anemic patients in Shandong Province, China. Parasitol Res. 2011;109:241–245. doi: 10.1007/s00436-011-2382-8. [DOI] [PubMed] [Google Scholar]
- 109.Jiang JF, Zheng YC, Jiang RR. Epidemiological, clinical, and laboratory characteristics of 48 cases of “Babesia venatorum” infection in China: a descriptive study. Lancet Infect Dis. 2015;15:196–203. doi: 10.1016/S1473-3099(14)71046-1. [DOI] [PubMed] [Google Scholar]
- 110.Zhang YZ, Zhou DJ, Qin XC. The ecology, genetic diversity, and phylogeny of Huaiyangshan virus in China. J Virol. 2012;86:2864–2868. doi: 10.1128/JVI.06192-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Zhao L, Zhai S, Wen H. Severe fever with thrombocytopenia syndrome virus, Shandong Province, China. Emerg Infect Dis. 2012;18:963–965. doi: 10.3201/eid1806.111345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Li Z, Hu J, Bao C. Seroprevalence of antibodies against SFTS virus infection in farmers and animals, Jiangsu, China. J Clin Virol. 2014;60:185–189. doi: 10.1016/j.jcv.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 113.Ding F, Zhang W, Wang L. Epidemiologic features of severe fever with thrombocytopenia syndrome in China, 2011–2012. Clin Infect Dis. 2013;56:1682–1683. doi: 10.1093/cid/cit100. [DOI] [PubMed] [Google Scholar]
- 114.Gai Z, Liang M, Zhang Y. Person-to-person transmission of severe fever with thrombocytopenia syndrome bunyavirus through blood contact. Clin Infect Dis. 2012;54:249–252. doi: 10.1093/cid/cir776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Yu L, Yu P, Liu DH, Hou J, Chen YF. Surveillance of syndrome of fever with thrombocytopenia in Dalian, 2012–2013. Study Trace Elem Health. 2014;31:5–6. (in Chinese). [Google Scholar]
- 116.Bao CJ, Guo XL, Qi X. A family cluster of infections by a newly recognized bunyavirus in eastern China, 2007: further evidence of person-to-person transmission. Clin Infect Dis. 2011;53:1208–1214. doi: 10.1093/cid/cir732. [DOI] [PubMed] [Google Scholar]
- 117.Gai ZT, Zhang Y, Liang MF. Clinical progress and risk factors for death in severe fever with thrombocytopenia syndrome patients. J Infect Dis. 2012;206:1095–1102. doi: 10.1093/infdis/jis472. [DOI] [PubMed] [Google Scholar]
- 118.Liu K, Zhou H, Sun RX. A national assessment of the epidemiology of severe fever with thrombocytopenia syndrome, China. Sci Rep. 2015;5:9679. doi: 10.1038/srep09679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Fan MY, Walker DH, Liu QH. Rickettsial and serologic evidence for prevalent spotted fever rickettsiosis in inner Mongolia. Am J Trop Med Hyg. 1987;36:615–620. doi: 10.4269/ajtmh.1987.36.615. [DOI] [PubMed] [Google Scholar]
- 120.Lin BH, Sun XJ, Zhan ZN, Lin YZ, Li WG. Serological and etiological studies on undefined rickettsiosis on Hainan Island. J Hainan Med College. 1997;3:97–102. (in Chinese). [Google Scholar]
- 121.Lin YZ, Sun XJ, Zhan ZN. Serological and etiological studies on rickettsiosis in Hainan Island. Chin J Zoonoses. 1999;15:90–91. (in Chinese). [Google Scholar]
- 122.Shi H, Wang Y, Han H. Analysis of 92 patients with tick-borne diseases in Mudanjiang. Chin J Vector Biol Control. 2013;24:295–300. (in Chinese). [Google Scholar]
- 123.Fan MY, Wang JG, Jiang YX, Zong DG, Lenz B, Walker DH. Isolation of a spotted fever group rickettsia from a patient and related ecologic investigations in Xinjiang Uygur Autonomous Region of China. J Clin Microbiol. 1987;25:628–632. doi: 10.1128/jcm.25.4.628-632.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Wu J, Wang SL, Jin YM. Detection of groEL gene in spotted fever group Rickettsia of patients with fever in Hainan province. Mod Prev Med. 2014;41:2417–2419. (in Chinese). [Google Scholar]
- 125.Jiang BG, Zheng YC, Tong YG. Genome sequence of Borrelia afzelii Strain HLJ01, isolated from a patient in China. J Bacteriol. 2012;194:7014–7015. doi: 10.1128/JB.01863-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Geng Z, Hou XX, Hao Q, Hu GL, Wan KL. Anti-Borrelia burgdorferi antibody response in 827 patients with suspected Lyme disease. Chin J Vector Biol Control. 2007;18:219–221. (in Chinese). [Google Scholar]
- 127.Zhou XY. The epidemiological and clinical analysis of Lyme disease in Mudanjiang from 1996 to 2003. Chin J Parasit Dis Control. 2005;18:159. (in Chinese). [Google Scholar]
- 128.Peng FB, Zhang WF, Zhou GP, Zhang SY, Yuan YM, Wu YY. The detection and clinical study on Lyme disease in Beijing. Chin J Epidemiol. 1994;15:10–13. (in Chinese). [Google Scholar]
- 129.Huang ZY, Hou XX, Wan KL. An investigation of Lyme disease in Pingjiang County, Hunan Province, China. Chin J Vector Biol Control. 2001;12:293–294. (in Chinese). [Google Scholar]
- 130.Li YL, Hao JG, Zhang ZF. The investigation of Lyme disease in Nanchuan County, Sichuan Province, China. Chin J Vector Biol Control. 1991;2:54–56. (in Chinese). [Google Scholar]
- 131.Jin SW, Hao Q, Tian Z. Analysis of surveillance on Lyme disease in Xinjiang prospecting region of Henan oil prospecting bureau. Chin J Zoonoses. 2005;21:501–502. (in Chinese). [Google Scholar]
- 132.Li JF, Meng DB, Wang QF, Dong XR, Wang JY. The discovery of human babesiosis. Chin Vet. 1984;6:19–20. (in Chinese). [Google Scholar]
- 133.Wang HX. A case of human babesiosis in southwest region of China. Int J Med Parasit Dis. 2012;39:190–192. (in Chinese). [Google Scholar]
- 134.Kim KH, Yi J, Kim G. Severe fever with thrombocytopenia syndrome, South Korea, 2012. Emerg Infect Dis. 2013;19:1892–1894. doi: 10.3201/eid1911.130792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Takahashi T, Maeda K, Suzuki T. The first identification and retrospective study of severe fever with thrombocytopenia syndrome in Japan. J Infect Dis. 2014;209:816–827. doi: 10.1093/infdis/jit603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.McMullan LK, Folk SM, Kelly AJ. A new phlebovirus associated with severe febrile illness in Missouri. N Engl J Med. 2012;367:834–841. doi: 10.1056/NEJMoa1203378. [DOI] [PubMed] [Google Scholar]
- 137.Jado I, Oteo JA, Aldámiz M. Rickettsia monacensis and human disease, Spain. Emerg Infect Dis. 2007;13:1405–1407. doi: 10.3201/eid1309.060186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.de Sousa R, Pereira BI, Nazareth C. Rickettsia slovaca infection in humans, Portugal. Emerg Infect Dis. 2013;19:1627–1629. doi: 10.3201/eid1910.130376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Pretorius AM, Birtles RJ. Rickettsia mongolotimonae infection in South Africa. Emerg Infect Dis. 2004;10:125–126. doi: 10.3201/eid1001.020662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Ryffel K, Péter O, Rutti B, Suard A, Dayer E. Scored antibody reactivity determined by immunoblotting shows an association between clinical manifestations and presence of Borrelia burgdorferi sensu stricto, B. garinii, B. afzelii, and B. Valaisiana in humans. J Clin Microbiol. 1999;37:4086–4092. doi: 10.1128/jcm.37.12.4086-4092.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.van Dam AP, Kuiper H, Vos K. Different genospecies of Borrelia burgdorferi are associated with distinct clinical manifestations of Lyme borreliosis. Clin Infect Dis. 1993;17:708–717. doi: 10.1093/clinids/17.4.708. [DOI] [PubMed] [Google Scholar]
- 142.Zhang HL, Yang H, Zhang PH. Spotted fever group Rickettsia DNA was detected in wild rodents and ticks in Dali, Yunnan Province, China. Chin J Vector Biol Control. 2004;15:461–462. (in Chinese). [Google Scholar]
- 143.Huang HN, Ding Z, He J. Study on the coinfection status of Borrelia burgdorferi sensu lato and spotted fever group Rickettsia in ticks from Hunchun, Jilin province. Zhonghua Liu Xing Bing Xue Za Zhi. 2006;27:379–383. (in Chinese). [PubMed] [Google Scholar]
- 144.Jiang LP, Mo SH, Zheng SG. Spotted fever group rickettsiae DNA was first detected in ticks in Zhejiang Province. Chin J Vector Biol Control. 2006;17:484–485. (in Chinese). [Google Scholar]
- 145.Wang Z, Liu XG, Luo Y. Investigation of tick-borne spotted fever group Rickettsia in northwestern Liaoning Province, China. Anim Hus Vet Med. 2015;47:143–144. (in Chinese). [Google Scholar]
- 146.Chai CL, Sun JM, Lu QY. A cross-sectional study on tick-borne Rickettsiae infections among murine-like animals. Zhejiang Prev Med. 2014;26:659–663. (in Chinese). [Google Scholar]
- 147.Wang Z, Yu M, Yang SJ. Epidemiological survey of spotted fever group Rickettsia in rodents in northeastern China. Chin Pre Med. 2015;16:184–186. (in Chinese). [Google Scholar]
- 148.Wang DM, Hao Q, Cai XH, Wan KL, Wang ZX, Chen J. Study on ribotyping of Lyme borreliosis spirochete in Guizhou province. Zhonghua Liu Xing Bing Xue Za Zhi. 2003;24:1129–1131. (in Chinese). [PubMed] [Google Scholar]
- 149.Yang Y, Zhang XL, Qiao S. Investigation on tick-borne pathogens at Ganqimaodu Port between Sino-Mongolia border. Chin Front Health Q. 2011;34:339–342. (in Chinese). [Google Scholar]
- 150.Zuo SY, Tang K, Li Y. DNA detection and sequence analysis of Borrelia burgdorferi sensu lato in rodents from Helongjiang and forest region. Zhonghua Liu Xing Bing Xue Za Zhi. 2012;33:643–644. (in Chinese). [PubMed] [Google Scholar]
- 151.Yang XF, Wan KL, Lu JP. Investigation of geographical epidemiology and etiological studies on Lyme disease in Inner Mongolia. Chin J Zoonoses. 1999;15:98. (in Chinese). [Google Scholar]
- 152.Yang XJ, Wan KL, Wang CS. Etiological studies on Lyme disease in Jilin Province. Chin J Health Lab Technol. 2006;16:1355–1362. (in Chinese). [Google Scholar]
- 153.Zhang DC, Hong Y, Zhang ZQ. Isolation of Borrelia burgdorferi in ticks and rodents in Liaoning Province. Chin J Vector Biol Control. 1992;3:19. (in Chinese). [Google Scholar]
- 154.Tian WC, Moldenhauer S, Li MQ. The first detection of Borrelia burgdorferi in H. japonica. Chin J Zoonoses. 1995;11:22–25. (in Chinese). [Google Scholar]
- 155.Zhang ZC, Tian WC, Guo YX. Investigation of Lyme disease in Hebei Province. Chin J Public Health. 1995;11:253–254. (in Chinese). [Google Scholar]
- 156.Wang LJ, Chen ZL, Wan KL. First isolation and identification of Lyme disease spirochete in Shandong Province. Chin J Vector Biol Control. 1997;8:127–128. (in Chinese). [Google Scholar]
- 157.Liu Q, He B, Huang SY, Wei F, Zhu XQ. Severe fever with thrombocytopenia syndrome, an emerging tick-borne zoonosis. Lancet Infect Dis. 2014;14:763–772. doi: 10.1016/S1473-3099(14)70718-2. [DOI] [PubMed] [Google Scholar]
- 158.Lambin EF, Tran A, Vanwambeke SO, Linard C, Soti V. Pathogenic landscapes: interactions between land, people, disease vectors, and their animal hosts. Int J Health Geogr. 2010;9:54. doi: 10.1186/1476-072X-9-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Barbour AG, Fish D. The biological and social phenomenon of Lyme disease. Science. 1993;260:1610–1616. doi: 10.1126/science.8503006. [DOI] [PubMed] [Google Scholar]
- 160.Levi T, Kilpatrick AM, Mangel M, Wilmers CC. Deer, predators, and the emergence of Lyme disease. Proc Natl Acad Sci USA. 2012;109:10942–10947. doi: 10.1073/pnas.1204536109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.LoGiudice K, Duerr ST, Newhouse MJ, Schmidt KA, Killilea ME, Ostfeld RS. Impact of host community composition on Lyme disease risk. Ecology. 2008;89:2841–2849. doi: 10.1890/07-1047.1. [DOI] [PubMed] [Google Scholar]
- 162.Liu J, Li S, Ouyang Z, Tam C, Chen X. Ecological and socioeconomic effects of China's policies for ecosystem services. Proc Natl Acad Sci USA. 2008;105:9477–9482. doi: 10.1073/pnas.0706436105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Liu K, Cui N, Fang LQ. Epidemiologic features and environmental risk factors of severe fever with thrombocytopenia syndrome, Xinyang, China. PLoS Negl Trop Dis. 2014;8:e2820. doi: 10.1371/journal.pntd.0002820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Uspensky I. Tick pests and vectors (Acari: Ixodoidea) in European towns: introduction, persistence and management. Ticks Tick Borne Dis. 2014;5:41–47. doi: 10.1016/j.ttbdis.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 165.Uspensky I. Ticks (Acari: Ixodoidea) as urban pests and vectors with special emphasis on ticks outside their geographical range. In: Robinson WH, Bajomi D, editors. Proceedings of the Sixth International Conference on Urban Pests. OOK-Press Kft; Hungary: 2008. pp. 333–347. [Google Scholar]
- 166.Gong P, Liang S, Carlton EJ. Urbanisation and health in China. Lancet. 2012;379:843–852. doi: 10.1016/S0140-6736(11)61878-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Parola P. Tick-borne rickettsial diseases: emerging risks in Europe. Comp Immunol Microbiol Infect Dis. 2004;27:297–304. doi: 10.1016/j.cimid.2004.03.006. [DOI] [PubMed] [Google Scholar]
- 168.Altizer S, Ostfeld RS, Johnson PT, Kutz S, Harvell CD. Climate change and infectious diseases: from evidence to a predictive framework. Science. 2013;341:514–519. doi: 10.1126/science.1239401. [DOI] [PubMed] [Google Scholar]
- 169.Harrus S, Baneth G. Drivers for the emergence and re-emergence of vector-borne protozoal and bacterial diseases. Int J Parasitol. 2005;35:1309–1318. doi: 10.1016/j.ijpara.2005.06.005. [DOI] [PubMed] [Google Scholar]
- 170.Parola P, Raoult D. Ticks and tickborne bacterial diseases in humans: an emerging infectious threat. Clin Infect Dis. 2001;32:897–928. doi: 10.1086/319347. [DOI] [PubMed] [Google Scholar]
- 171.Yang XJ, Chen Z, Liu JZ. Advances in systematics of ticks. Acta Entomologica Sinica. 2007;50:941–949. (in Chinese). [Google Scholar]
- 172.Meng YC. Ticks, acari, and human diseases. 1st edn. China Sci Tech Press; Hefei: 1995. p. 43. (in Chinese). [Google Scholar]
- 173.Cao WC, Zhang XT, Xu RM. The medical significance of tick and tick-borne disease in public health. Chin J Public Health. 1999;15:221–222. (in Chinese). [Google Scholar]
- 174.Wu XB, Na RH, Wei SS, Zhu JS, Peng HJ. Distribution of tick-borne diseases in China. Parasit Vectors. 2013;6:119. doi: 10.1186/1756-3305-6-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Zhao JW, Wang HY, Wang Y. Regional distribution profiles of tick borne pathogens in China. Chin J Biol Control. 2012;18:45–48. (in Chinese). [Google Scholar]
- 176.Zhan L, Cao WC, Jiang JF. Anaplasma phagocytophilum from rodents and sheep, China. Emerg Infect Dis. 2010;16:764–768. doi: 10.3201/eid1605.091293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Wang YY, Li J, Wang S, Hu M, Lu FL. Tick-borne infectious diseases. Infect Dis Inf. 2011;24:58–61. (in Chinese). [Google Scholar]
- 178.Lu Z, Bröker M, Liang G. Tick-borne encephalitis in mainland China. Vector Borne Zoonotic Dis. 2008;8:713–720. doi: 10.1089/vbz.2008.0028. [DOI] [PubMed] [Google Scholar]
- 179.Xia H, Li P, Yang J. Epidemiological survey of Crimean-Congo hemorrhagic fever virus in Yunnan, China, 2008. Int J Infect Dis. 2011;15:e459–e463. doi: 10.1016/j.ijid.2011.03.013. [DOI] [PubMed] [Google Scholar]
- 180.Wang Y, Peng Y, Hai R. Diversity of Francisella tularensis subsp. holarctica lineages, China. Emerg Infect Dis. 2014;20:1191–1194. doi: 10.3201/eid2007.130931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Chen M, Fan MY. A review on the research of North-Asia tick-borne spotted fever. Chin Public Health. 1997;6:373–376. (in Chinese). [Google Scholar]
- 182.Liu YF, Zhang Y. The study progress of Q fever and Ehrlichiosis. Med Recap. 2008;6:864–867. (in Chinese). [Google Scholar]
- 183.Süss J. Tick-borne encephalitis 2010: epidemiology, risk areas, and virus strains in Europe and Asia - an overview. Ticks Tick Borne Dis. 2011;2:2–15. doi: 10.1016/j.ttbdis.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 184.Parola P, Paddock CD, Socolovschi C. Update on tick-borne rickettsioses around the world: a geographic approach. Clin Microbiol Rev. 2013;26:657–702. doi: 10.1128/CMR.00032-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Colwell DD, Dantas-Torres F, Otranto D. Vector-borne parasitic zoonoses: emerging scenarios and new perspectives. Vet Parasitol. 2011;182:14–21. doi: 10.1016/j.vetpar.2011.07.012. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.