Abstract
Background and Aims:
Oropharyngeal colonisation followed by aspiration of contaminated secretions is the major cause for ventilator-associated pneumonia (VAP). Pooled secretions present in the sub-glottic area above inflated endotracheal tube cuff may be aspirated into the lower airways. It was hypothesised that intermittent suctioning of sub-glottic secretions would prevent VAP.
Methods:
Group I (n = 50) patients were intubated with HiLo Evac™ endotracheal (ET) tube with facility for sub-glottic suctioning, and Group II (n = 50) patients were intubated with HiLo Contour™ ET tube without such facility. In the Group I, sub-glottic suctioning was performed every 2 h. Incidence of VAP, mean ventilator days, Intensive Care Unit (ICU) stay and mortality were compared. Qualitative variables were reported as percentages and were compared by Chi-square test or unpaired two-tailed, Fisher's exact test, as appropriate, to analyse the significance of difference between the two groups.
Results:
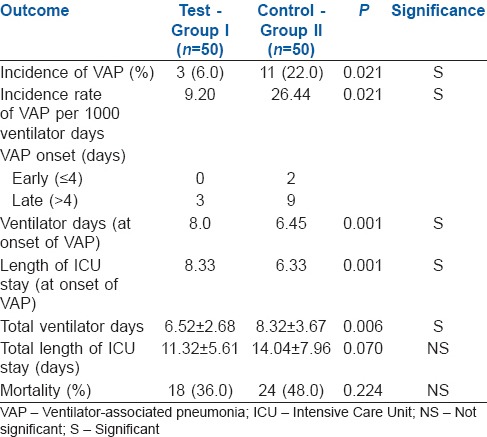
The two groups were similar with respect to demographic characteristics. VAP was seen in 6% of patients in Group I and 22% of patients in Group II (P = 0.021). Both early- and late-onset VAPs were significantly reduced in Group I. Both ventilator days (8.0 vs. 6.45; P = 0.001) and ICU stay (8.33 vs. 6.33; P = 0.001) on the day of onset of VAP were significantly more in the Group I. Total ventilator days were significantly less (6.52 vs. 8.32; P = 0.006) with lower incidence of mortality (36% vs. 48%; P = 0.224) in the Group I.
Conclusion:
Intermittent sub-glottic suctioning reduces the incidence of VAP including late-onset VAP.
Keywords: Aspiration, intubation, mechanical ventilation, sub-glottic secretion drainage, ventilator-associated pneumonia
INTRODUCTION
Hospital-acquired pneumonia (HAP) accounts for up to 25% of all Intensive Care Unit (ICU) infections and more than 50% of the antibiotics prescribed. The development of HAP 48 h after endotracheal intubation and initiation of mechanical ventilation is known as ventilator-associated pneumonia (VAP). The prevalence of VAP ranges from 8 to 28% in ICU patients receiving mechanical ventilation depending on the patient population.[1,2] VAP that occurs within 48-96 h after tracheal intubation is termed early-onset pneumonia and often results from aspiration during intubation.[1] VAP that occurs after this period is defined as late-onset pneumonia which is mostly caused by high-risk pathogens and is associated with excess mortality.[2] Mortality rates in patients with VAP range from 20 to 50% and may reach more than 70% when the infection is caused by multidrug resistant and invasive pathogens.[3] The incidence of VAP-attributable mortality is difficult to quantify due to the possible confounding effect of associated conditions, but VAP is thought to increase the mortality of the underlying disease by about 30%.[3] VAP is also associated with considerable morbidity including prolonged length of ICU stay, prolonged mechanical ventilation and increased costs of hospitalisation.[3] Two processes are considered essential for the development of VAP; bacterial colonisation of the oropharynx followed by aspiration of contaminated oropharyngeal secretions and leakage around the endotracheal tube into the lower airways. The presence of an invasive medical device (endotracheal tube) is an important contributor to the colonisation of the oropharynx and the tracheobronchial tree.[4] Pooled secretions are also present in the sub-glottic area above the inflated endotracheal tube cuff. Sub-glottic secretions accumulated above the endotracheal cuff may progress, descending along the channels within the folds of the cuff wall, into the lower respiratory tract.[5] Continuous micro-aspiration of microorganisms from the oropharynx or secretions around the cuff of the endotracheal tube into the lower airways are the most common mechanisms for development of VAP.[5] While oropharyngeal secretions are amenable for suctioning, the sub-glottic secretions are inaccessible for the same. Using an endotracheal tube which incorporates a separate dorsal lumen ending in the sub-glottic area, above the cuff, for drainage of sub-glottic secretions therefore should result in reduction in the development of VAP. Many studies have been carried out, some with negative results. However, this intervention needs to be formally tested in a setting with a high baseline incidence of VAP.
METHODS
The study was conducted in a tertiary care hospital after approval from the Institutional Ethical Committee for this study and 100 ICU patients who were expected to require mechanical ventilation for more than 48 h were studied. After admission to the ICU, informed written consent was obtained from the next of kin of the patient. Then, all the patients were assessed for degree of morbidity by acute physiology and chronic health evaluation (APACHE) II score[6] which was recorded. A total of 157 patients were assessed for eligibility, out of which 47 were excluded for not meeting the criteria. The remaining 110 were randomised by sealed envelope method and 54 were allocated to Group I and 56 to Group II, out of which 4 and 6 died before 48 h, respectively, and hence were not considered in our study [Figure 1]. Group I (n = 50) patients were intubated with HiLo™ Evac endotracheal tube (Mallinckrodt, Tyco Healthcare, Pleasanton, CA 94588, USA) [Figure 2] which incorporates a separate dorsal lumen ending in the sub-glottic area, above the cuff, for sub-glottic secretion drainage. Group II patients (n = 50) were intubated with HiLo™ Contour endotracheal tube (Mallinckrodt, Tyco Healthcare, Pleasanton, CA 94588, USA) without such facility for drainage of sub-glottic secretions. In Group I, sub-glottic secretions were suctioned manually with a 10 ml syringe intermittently at an intended frequency of one suction manoeuvre every 2 h. Sub-glottic suctioning was not performed in the Group II. Because of the nature of the intervention, physicians and nurses could not be blinded to the randomisation arm. In both the groups, measures for the prevention of VAP were followed which included semi-recumbent body positioning and changes in body position every 4 h, stress ulcer prophylaxis with sucralfate, and endotracheal suctioning with closed suctioning system every 4 h or whenever there was an increase in airway resistance; or when there was any audible or visible secretions in the endotracheal tube. The endotracheal tube cuff pressure was maintained between 20 and 30 cm H2O which was measured every 4 h using HiLo™ H and pressure gauge. With base line incidence of VAP considered as 22% and assuming a reduction of incidence of VAP by 25% to be significant, the sample size for 95% Confidence Interval and power of 80% was calculated to be 511 per group. Since number of patients ventilated annually at our institution is around 150, a convenience sample size of 110 only could be hence drawn.
Figure 1.
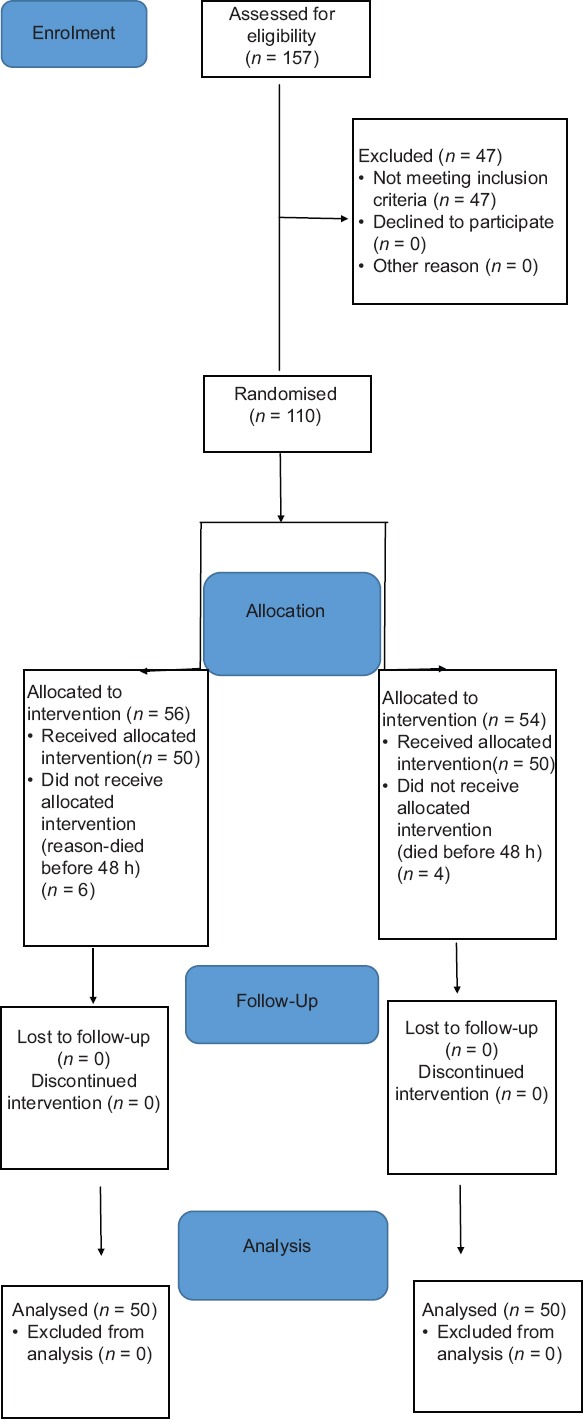
Consort flowchart
Figure 2.
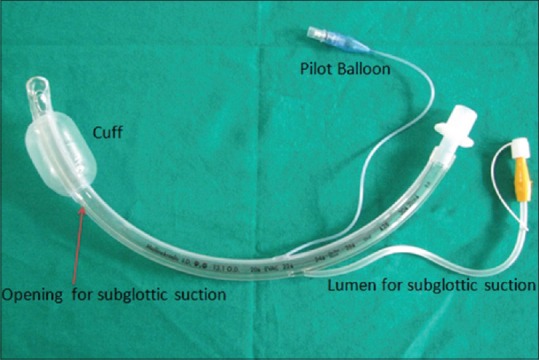
HiLo Evac™ endotracheal tube
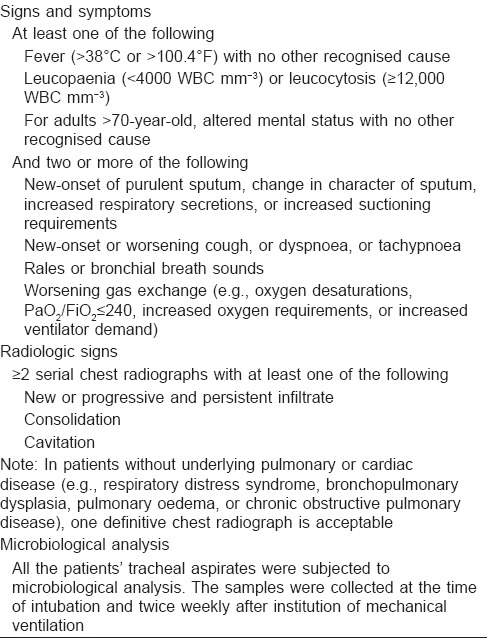
The following outcome parameters were measured in each of these cases: Presence of VAP [Table 1], day of onset of VAP after instituting mechanical ventilation, length of mechanical ventilation, length of ICU stay and mortality.
Table 1.
Criteria for diagnosis of ventilator-associated pneumonia (centers for disease control and prevention, surveillance, definition for clinical diagnosis of health care associated pneumonia)
Qualitative variables were reported as percentages and were compared by Chi-square test or unpaired two-tailed, Fisher's exact test, as appropriate, to analyse the significance of difference between the two groups. Univariate analysis was used to compare the variables for the outcome groups. Continuous variables were compared using Student's t-test for normally distributed variables. We confirmed the results of these tests, with logistic regression analysis, using statistics software (SPSS 16.0, SPSS Inc., and Chicago, Illinois, USA). For all statistical tests used, a P < 0.05 was considered statistically significant.
RESULTS
The differences in distribution with respect to age, gender and BMI of patients in Groups I and II were non-significant; however, APACHE II score was significantly more in Group II with P = 0.034 [Table 2]. A regression analysis was done to see the confounding effect of APACHE II which did not reveal any significance of VAP in both groups. Association of risk factors were found to be non-significant (P = 0.475) in both groups. The overall incidence of VAP in both the groups was 14, (incidence of 18.9 episodes per 1000 ventilator days). Patients randomised to intermittent sub-glottic suctioning had a statistically lower incidence of VAP than patients intubated with the conventional endotracheal tube (6% vs. 22%; P = 0.021). Use of sub-glottic suctioning resulted in an absolute event reduction of 16%, indicating that 16 occurrences of VAP could be avoided for every 100 patients treated with sub-glottic secretion drainage. Incidence of VAP was 9.20 and 26.44 episodes of VAP per 1000 ventilator days in the Group I and Group II, respectively. The probability of remaining free of VAP over the duration of mechanical ventilation was significantly higher in the Group I compared with the Group II. Adjustment analysis for APACHE II scores, which was more in patients randomised to the Group II, showed that it did not alter the results of the study. Both early- and late-onset VAPs were significantly reduced in the patients undergoing intermittent sub-glottic secretion drainage compared with the control patients (early-onset, 0.0 vs. 6.0%; late-onset, 4.0 vs. 18.0%). The duration of mechanical ventilation (8.0 vs. 6.45; P = 0.001) and length of ICU stay (8.33 vs. 6.33; P = 0.001) on the day of onset of VAP were significantly more in Group I compared to Group II. Total ventilator days are significantly less in Group I when compared to Group II (6.52 vs. 8.32; P = 0.006). Total length of ICU stay was also less in Group I when compared to the Group II (11.32 vs. 14.04; P = 0.070) though not statistically significant it shows a trend towards reduction in duration of ICU stay in patients of Group I receiving intermittent sub-glottic suctioning. Incidence of mortality was higher in Group II (48.0%) compared to Group I (36.0%) with P = 0.224, but this was not statistically significant [Table 3]. The overall use of antibiotic therapy before the onset of VAP was similar in the two groups (80.0% in Group I vs. 84.0% in Group II ; P = 0.799, not significant).
Table 2.
Patient characteristics
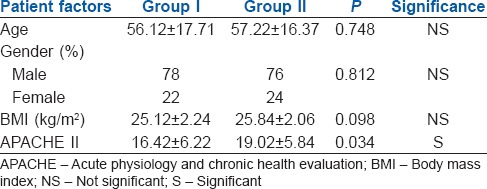
Table 3.
Clinical outcome in patients receiving mechanical ventilation >48 h
DISCUSSION
In our study, intermittent sub-glottic secretion drainage resulted in a significant reduction in the overall incidence of VAP and the incidence of early- and late-onset VAPs in an unselected population of ICU patients. Moreover, the absolute risk reduction in our patients indicates that 16 occurrences of VAP could be avoided for every 100 patients treated with intermittent sub-glottic suctioning. The strengths of our study include the concealment of the allocation process, complete follow-up of included patients and high compliance with the planned sub-glottic suctioning procedure. We also carefully ensured that potentially confounding factors, including compliance with preventive measures for VAP other than sub-glottic suctioning, use of antibiotics and tracheal cuff pressure, were equally distributed between the two groups. These confounding factors were not taken into account in other studies review.[7,8,9] Furthermore, APACHE II score and risk factors for VAP which may be confounding the results were proved by regression analysis that they did not influence the results of the study. A randomised multicentre trial[10] on VAP prevention was published while the present study was being performed which concluded that sub-glottic secretion drainage is effective in preventing both early- and late-onset VAPs. Our finding of a protective role for sub-glottic secretion drainage in late-onset VAP is consistent with a randomised trial assessing the simultaneous use of sub-glottic secretion drainage and a new polyurethane cuff.[11] In our study and previous two studies,[7,10] manual intermittent suctioning was used to aspirate sub-glottic secretions. Although other suctioning techniques including automatic intermittent[8] or continuous suctioning[9,12,13] have also been proposed, to date, the most effective technique to remove sub-glottic secretions remains unclear and is to be further evaluated. In our study, in addition to a marked decrease in the incidence of VAP, there was also a significant delay in the onset of VAP in terms of both ventilatory days and ICU stay in group I [Table 3]. The meta-analysis by Dezfulian et al.,[14] which pooled the results of the first five trials of sub-glottic secretion drainage, demonstrated a significant reduction in duration of mechanical ventilation and ICU stay which is consistent with the results of our study. Our results are in agreement with several other earlier studies.[7,8,10] A randomised controlled clinical trial[10] conducted at four centres included a total of 333 adult patients intubated with a tracheal tube allowing drainage of sub-glottic secretions and expected to require mechanical ventilation for >48 h. Primary outcome was the overall incidence of VAP based on quantitative culture of distal pulmonary samplings performed after each clinical suspicion. Other outcomes studied included incidence of early- and late-onset VAPs, duration of mechanical ventilation and hospital mortality. No significant group differences were observed in duration of mechanical ventilation and hospital mortality. This study did not include length of ICU stay and specific mortality of patients receiving mechanical ventilation, both of which, in our study showed a trend towards reduction in patients receiving intermittent sub-glottic suctioning. Smulders et al.[8] included 150 patients with an expected duration of mechanical ventilation >72 h and were randomised to intermittent sub-glottic secretion drainage or control group. Patients randomised to intermittent sub-glottic secretion drainage had a statistically lower incidence of VAP than patients intubated with the conventional endotracheal tube. No statistical differences were found in the duration of mechanical ventilation, length of ICU stay, length of hospital stay and mortality. Our study showed significant reduction in duration of mechanical ventilation and a trend towards reduction in length of ICU stay and mortality in patients receiving intermittent sub-glottic suctioning though not statistically significant. In contrast to these results, Kollef et al.[9] studied 343 patients undergoing cardiac surgery and requiring mechanical ventilation. This study did not show statistically significant reduction in VAP in the study group. Bouza et al.[12] studied total of 714 randomised patients who had received mechanical ventilation for >48 h, 359 in continuous aspiration of sub-glottic secretion group and 331 in control group. These results are consistent with our study results. In a recent meta-analysis[15] which included 13 studies, 12 reported a reduction in VAP rates in the sub-glottic secretion drainage arm, with overall risk ratio of 0.55 (P < 0.00001) with no heterogeneity. The use of sub-glottic secretion drainage was associated with reduced ICU length of stay (−1.52 days; P = 0.03), decreased duration of mechanical ventilation (−1.08 days; P = 0.03) and increased time to first episode of VAP (2.66 days; P = 0.001). Although these results are consistent with our study with respect to incidence of VAP, duration of mechanical ventilation and length of ICU stay, in contrast to our study, there was no effect on mortality.
Ours being a tertiary care government hospital where patients do not pay for the treatment, economic evaluation was not carried out, which is the limitation of our study.
CONCLUSION
This clinical study demonstrated that intermittent sub-glottic suctioning significantly reduces the incidence of VAP including late-onset VAP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Chastre J, Fagon JY. Ventilator-associated pneumonia. Am J Respir Crit Care Med. 2002;165:867–903. doi: 10.1164/ajrccm.165.7.2105078. [DOI] [PubMed] [Google Scholar]
- 2.Klompas M. Does this patient have ventilator-associated pneumonia? JAMA. 2007;297:1583–93. doi: 10.1001/jama.297.14.1583. [DOI] [PubMed] [Google Scholar]
- 3.Heyland DK, Cook DJ, Griffith L, Keenan SP, Brun-Buisson C. The attributable morbidity and mortality of ventilator-associated pneumonia in the critically ill patient. The Canadian Critical Trials Group. Am J Respir Crit Care Med. 1999;159(4):1249–56. doi: 10.1164/ajrccm.159.4.9807050. [DOI] [PubMed] [Google Scholar]
- 4.Safdar N, Crnich CJ, Maki DG. The pathogenesis of ventilator-associated pneumonia: Its relevance to developing effective strategies for prevention. Respir Care. 2005;50:725. [PubMed] [Google Scholar]
- 5.Seegobin RD, van Hasselt GL. Aspiration beyond endotracheal cuffs. Can Anaesth Soc J. 1986;33(3):273–9. doi: 10.1007/BF03010737. [DOI] [PubMed] [Google Scholar]
- 6.Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Crit Care Med. 1985;13:818–29. [PubMed] [Google Scholar]
- 7.Mahul P, Auboyer C, Jospe R, Ros A, Guerin C, el Khouri Z, et al. Prevention of nosocomial pneumonia in intubated patients: Respective role of mechanical subglottic secretions drainage and stress ulcer prophylaxis. Intensive Care Med. 1992;18:20–5. doi: 10.1007/BF01706421. [DOI] [PubMed] [Google Scholar]
- 8.Smulders K, van der Hoeven H, Weers-Pothoff I, Vandenbroucke-Grauls C. A randomized clinical trial of intermittent subglottic secretion drainage in patients receiving mechanical ventilation. Chest. 2002;121:858–62. doi: 10.1378/chest.121.3.858. [DOI] [PubMed] [Google Scholar]
- 9.Kollef MH, Nikolaos J, Thoralf M. A randomized clinical trial of continuous aspiration of subglottic secretions in cardiac surgery patients. Chest. 1999;116:1339–46. doi: 10.1378/chest.116.5.1339. [DOI] [PubMed] [Google Scholar]
- 10.Lacherade JC, De Jonghe B, Guezennec P, Debbat K, Hayon J, Monsel A, et al. Intermittent subglottic secretion drainage and ventilator-associated pneumonia: A multicenter trial. Am J Respir Crit Care Med. 2010;182:910–7. doi: 10.1164/rccm.200906-0838OC. [DOI] [PubMed] [Google Scholar]
- 11.Lorente L, Lecuona M, Jiménez A, Mora ML, Sierra A. Influence of an endotracheal tube with polyurethane cuff and subglottic secretion drainage on pneumonia. Am J Respir Crit Care Med. 2007;176:1079–83. doi: 10.1164/rccm.200705-761OC. [DOI] [PubMed] [Google Scholar]
- 12.Vallés J, Artigas A, Rello J, Bonsoms N, Fontanals D, Blanch L, et al. Continuous aspiration of subglottic secretions in preventing ventilator-associated pneumonia. Ann Intern Med. 1995;122:179–86. doi: 10.7326/0003-4819-122-3-199502010-00004. [DOI] [PubMed] [Google Scholar]
- 13.Bouza E, Pérez MJ, Muñoz P, Rincón C, Barrio JM, Hortal J. Continuous aspiration of subglottic secretions in the prevention of ventilator-associated pneumonia in the postoperative period of major heart surgery. Chest. 2008;134:938–46. doi: 10.1378/chest.08-0103. [DOI] [PubMed] [Google Scholar]
- 14.Dezfulian C, Shojania K, Collard HR, Kim HM, Matthay MA, Saint S. Subglottic secretion drainage for preventing ventilator-associated pneumonia: A meta-analysis. Am J Med. 2005;118:11–8. doi: 10.1016/j.amjmed.2004.07.051. [DOI] [PubMed] [Google Scholar]
- 15.Muscedere J, Rewa O, McKechnie K, Jiang X, Laporta D, Heyland DK. Subglottic secretion drainage for the prevention of ventilator-associated pneumonia: A systematic review and meta-analysis. Crit Care Med. 2011;39:1985–91. doi: 10.1097/CCM.0b013e318218a4d9. [DOI] [PubMed] [Google Scholar]


