Abstract
Background and Aims:
Air-Q intubating laryngeal mask airway (ILA) is used as a supraglottic airway device and as a conduit for endotracheal intubation. This study aims to assess the efficacy of the Air-Q ILA regarding ease of insertion, adequacy of ventilation, rate of successful intubation, haemodynamic response and airway morbidity.
Methods:
Sixty patients presenting for elective surgery at our Medical College Hospital were selected. Following adequate premedication, baseline vital parameters, pulse rate and blood pressure were recorded. Air-Q size 3.5 for patients 50-70 kg and size 4.5 for 70-100 kg was selected. After achieving adequate intubating conditions, Air-Q ILA was introduced. Confirming adequate ventilation, appropriate sized endotracheal tube was advanced through the Air-Q blindly to intubate the trachea. Placement of the endotracheal tube in trachea was confirmed.
Results:
Air-Q ILA was successfully inserted in 88.3% of patients in first attempt and 11.7% patients in second attempt. Ventilation was adequate in 100% of patients. Intubation was successful in 76.7% of patients with Air-Q ILA. 23.3% of patients were intubated by direct laryngoscopy following failure with two attempts using Air-Q ILA. Post-intubation the change in heart rate was statistically significant (P < 0.0001). 10% of patients were noted to have a sore throat and 5% of patients had mild airway trauma.
Conclusion:
Air-Q ILA is a reliable device as a supraglottic airway ensuring adequate ventilation as well as a conduit for endotracheal intubation. It benefits the patient by avoiding the stress of direct laryngoscopy and is also superior alternative device for use in a difficult airway.
Keywords: Air-Q intubating laryngeal airway, endotracheal intubation, supraglottic airway device
INTRODUCTION
Airway management is the cornerstone of safe anaesthetic practice. Tracheal intubation with the aid of a rigid laryngoscope, although a gold standard in securing a definitive airway, triggers adverse haemodynamic stress response.[1]
In instances when the procedure or the patient need not be subjected to endotracheal intubation, which is an invasive technique, the use of supraglottic airway devices is a superior alternative.[2,3] The use of supraglottic airway device has also proven to be lifesaving in the management of airway crisis.[4]
Since the introduction of laryngeal mask airways, an array of supraglottic airway devices have been designed and some of these devices have been modified to be used as conduits for endotracheal intubation.
The Air-Q® Intubating Laryngeal Airway (ILA™, Cookgas® LLC, Mercury Medical, Clearwater, FL, USA) was introduced by Daniel Cook in 2005 as an aid for airway maintenance and as a conduit for tracheal intubation during general anaesthesia.[5] At present, the Air-Q ILA is available in 7 sizes (0.5, 1, 1.5, 2, 2.5, 3.5 and 4.5) in both disposable as well as the reusable form.[6]
The aim of this study was to evaluate the efficacy of Air-Q ILA with respect to ease of insertion, characteristics of ventilation, intubating conditions, haemodynamic response to endotracheal intubation and identifying any airway morbidity subsequent to its use.
METHODS
A prospective observational study of new supraglottic airway device, Air-Q ILA was undertaken in our medical college hospital. After obtaining Institutional Ethics Committee approval, along with informed consent, 60 patients of either sex presenting for routine elective surgery under general anaesthesia were randomly selected.
Inclusion criteria consisted of patients belonging to American Society of Anaesthesiologists physical status I and II, weighing 50-100 kg in the age group of 18-70 years with Mallampatti airway classification class I and class II.
Exclusion criteria included subjects with unknown nil per oral status, patients posted for emergency surgery, pregnant females, patients with pathology of oropharynx and larynx and patients with pre-existing comorbid conditions such as endocrine, cardiac and hypertensive disorders.
A detailed clinical assessment of the patient including that of the airway was done the previous day. All patients were advised to fast on the night before surgery. All patients were advised tab. Alprazolam 0.5 mg and tab. ranitidine 150 mg the night before the proposed surgery. On arrival in the operating theatre, a multi-channel monitor was connected to record electrocardiography, non-invasive blood pressure, capnograph and pulse oximetry. The baseline vital parameters were recorded.
Patients were positioned supine with a pillow under the head. After securing intravenous (IV) cannula, IV fluid infusion was initiated. Patients were pre-medicated with inj. ondansetron 4 mg, injection glycopyrrolate 0.2 mg, injection midazolam 0.02 mg/kg, injection fentanyl 2 μg/kg administered IV.
The appropriate size of the Air-Q was selected for each patient, size 3.5 for patients weighing 50-70 kg and size 4.5 for 70-100 kg. The ILA was prepared by completely deflating the cuff and application of 2% lignocaine jelly on the posterior surface of the mask bowl. Size 7.0 endotracheal tube for Air-Q 3.5 and size 8.0 endotracheal tube for Air-Q sized 4.5 was selected and was pre-lubricated with 2% lignocaine jelly before induction of general anaesthesia.
All patients were pre-oxygenated for 3 min with 100% oxygen using a fresh gas flow of 8 L/min using a conventional facemask and Bain circuit. General anaesthesia was induced with injection propofol 2 mg/kg IV and muscle relaxant injection succinylcholine 1.5 mg/kg IV was administered.
After achieving an adequate depth of anaesthesia and muscle relaxation, patient's mouth was opened and the tongue displaced using a disposable sterile wooden tongue depressor to facilitate the passage of the Air-Q. Air-Q ILA was introduced with a gentle inward and downward pressure using the curvature of the device as a guide till a fixed resistance to further advancement was felt. The cuff was inflated with air as per manufacturer's recommendation, 18 mL for size 3.5 and 25 mL for size 4.5.
The proximal connector of the Air-Q ILA was connected to EtCO2 probe along with the breathing circuit. Initiating positive pressure ventilation, proper insertion of device was confirmed by observing bilateral chest rise along with audible breath sounds on auscultation and capnographic trace on the monitor. The vital parameters (pulse rate, blood pressure, peripheral oxygen saturation [SpO2]) were recorded after successful insertion of the Air-Q ILA.
The pre-lubricated appropriate size endotracheal tube was then advanced through the Air-Q ILA blindly to intubate the trachea. The endotracheal tube was then connected to EtCO2 probe along with the breathing circuit and placement of the endotracheal tube in trachea was again confirmed by auscultation of breath sounds along with bilateral chest rise and capnographic trace. On the first attempt, if trachea was not intubated, the endotracheal tube was withdrawn up to 18 cm mark for number 7.0 endotracheal tube and 20 cm mark for number 8.0 endotracheal tube followed by re-advancement of the endotracheal tube with adequate external laryngeal manoeuvre over the cricoid cartilage.[6]
After confirmation of endotracheal placement, the connector of endotracheal tube was removed and the tube was stabilised using the Air-Q removal stylet. The cuff of the Air-Q was deflated and Air-Q withdrawn over the endotracheal tube-stylet assembly. The placement of endotracheal tube was reconfirmed to rule out endobronchial advancement and then the tube was secured.
After removal of Air-Q following tracheal intubation, the device was observed for visible macroscopic blood stains to rule out airway trauma.
The following data were recorded: Number of attempts to insert Air-Q, post-insertion heart rate (HR), blood pressure and SpO2, number of attempts to intubate the trachea, post-intubation HR, systolic (SBP), diastolic (DBP) and mean arterial pressures (MAP) recorded at 1 min, 3 min and 5 min intervals and airway trauma and post-operatively, airway morbidity was recorded.
Failure to intubate the trachea was defined as the inability to advance the endotracheal tube into the trachea on manipulation respectively. In patients where intubation with Air-Q as a conduit was unsuccessful, the patients were intubated with direct laryngoscopy using Macintosh laryngoscope.
Statistical analysis was performed using. IBM SPSS Statistics for Windows, Version 20.0. (Armonk, NY: IBM Corp.IBM Corp.Released 2011). Repeated measure ANOVA was used to analyse the variations in HR SBP, DBP and MAP. Chi-square test was used to assess the number of attempts for tracheal intubation and analysis of airway morbidity associated with the use of the Air-Q ILA.
RESULTS
A total of 60 patients were enrolled in this study. The demographics of the study group was as follows: Age (33.63 ± 10.78 years), weight (58.73 ± 9.88 kg) and 18 male and 42 female subjects. As assessed during pre-operative airway examination 27 patients had Grade I and 33 had Grade II Mallampati grading. Based on American Society of Anesthesiologists (ASA) risk grading, 49 patients belonged to ASA Grade I, and 11 patients to ASA Grade II.
The Air-Q was successfully inserted in all the patients (100%) [Figure 1]. The first attempt for insertion of the Air-Q was successful in 53 patients and in 7 patients, a second attempt was required. Ventilation was found to be adequate in all patients in our study with size 3.5 and 4.5 Air-Q ILA [Table 1].
Figure 1.
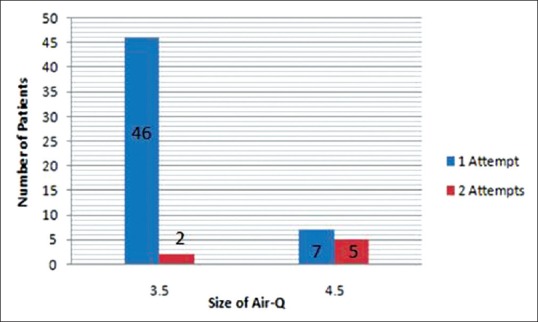
Number of attempts for successful insertion of the Air-Q laryngeal mask airway
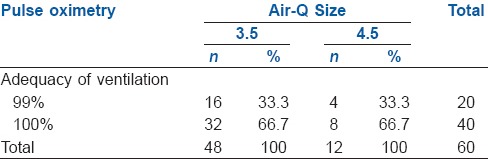
Table 1.
Adequacy of ventilation
Tracheal intubation was successful in 46 patients (76.7%). Overall, 34 patients (56.7%) were successfully intubated in the first attempt; Figure 2 shows the analysis for the successful tracheal intubation with size 3.5 and size 4.5 Air-Q ILA, wherein we observed that frequency of successful intubation at second attempt was higher when size 4.5 Air-Q ILA was used to pass size 8.0 mm endotracheal tube.
Figure 2.
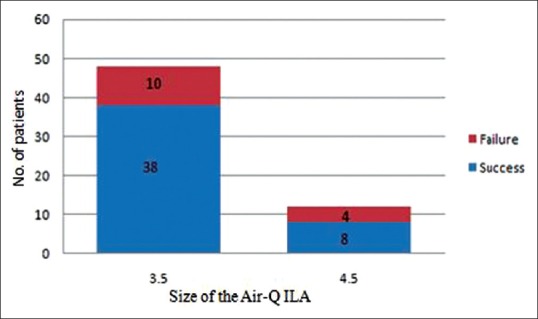
Rate of succesful endotracheal intubation
Haemodynamic response to insertion of Air-Q ILA and tracheal intubation [Table 2] showed significant reduction of SBP, DBP and MAP after the induction of general anaesthesia and insertion of the Air-Q compared to the pre-induction values (P < 0.0001). The rise in HR after insertion of the Air-Q and 1 min after intubation was significant (P < 0.0001) when compared with pre-induction values of HR.
Table 2.
Perioperative haemodynamic response
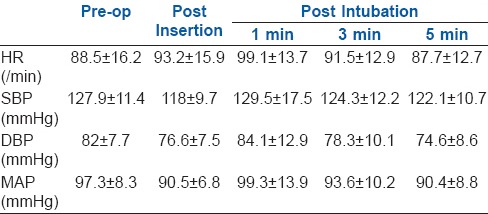
Immediately after tracheal intubation, there was a significant rise in the systolic, diastolic and MAP compared to the pre-intubation values. A gradual decline was observed between 1 min, 3 min and 5 min post-intubation. Three patients (5%) had minor airway trauma as deduced by observation of macroscopic blood on the device after its removal and 6 patients (10%) reported having sore throat after removal of the endotracheal tube at the end of surgery [Figure 3].
Figure 3.
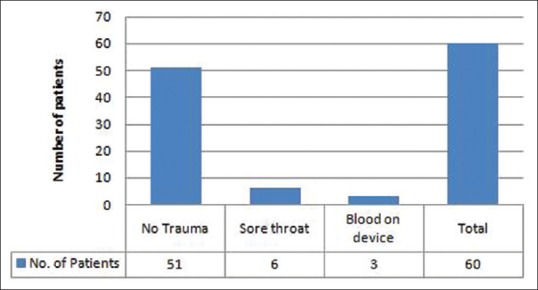
Assesment of airway morbidity
DISCUSSION
Tracheal intubation with the aid of a rigid laryngoscope, although a gold standard in securing a definitive airway, is an invasive technique. The stimulus of direct laryngoscopy to visualise the vocal cords triggers adverse haemodynamic stress response in the form of tachycardia and hypertension. Although the severity of this response depends on the duration of laryngoscopy, operator expertise and the level of anaesthesia, it can prove hazardous in patients with myocardial insufficiency and cerebrovascular disease, especially in the geriatric age group.[1,7]
The Air-Q® Intubating Laryngeal Airway (ILA™, Cookgas® LLC, Mercury Medical, Clearwater, FL, USA) is a new supraglottic airway device designed for airway maintenance and also as a conduit for endotracheal intubation during general anaesthesia. The major advantage of the device design is that conventional PVC endotracheal tube can be passed through the Air-Q ILA to intubate the trachea (up to 7.5 and 8.5 mm ID through Air-Q size 3.5 and 4.5, respectively) without the use of conventional laryngoscope.[8] Armoured endotracheal tubes can also be used with Air-Q ILA as conduit.[9]
Air-Q design when compared to LMA Unique™ includes a shorter airway tube with an integrated bite block and a larger inner diameter enabling passage of larger standard cuffed tracheal tubes, ensuring tracheal tube cuff placement below the level of the vocal cords in the mid-trachea and also facilitating safe removal of the Air-Q ILA after endotracheal intubation.[5,10,11] This airway tube also has a tethered, removable standard 15 mm circuit adapter. The advancement of appropriately sized endotracheal tube is also favoured by the absence of grill at the ventilating orifice which is in the form of a keyhole shaped aperture. The absence of grill at the ventilating orifice also favours the utility of device for fibreoptic endoscope assisted endotracheal intubation.[12] The ventilating orifice is accompanied by an auxiliary hole that improves ventilation. Air-Q does not have an epiglottis elevating bar which is an important factor in prevention of haemodynamic stress response caused by stimulation of the epiglottis and the periepiglottic structures, an advantage over the LMA Fastrach.[13,14,15] In case of failure to intubate the trachea, the Air-Q ILA can be used as a definitive airway, also a major advantage over the LMA Fastrach.[16] Furthermore, LMA Fastrach requires a special expensive silicon endotracheal tube and it is not available in paediatric sizes.[17]
Air-Q ILA when compared to other supraglottic airway devices such as LMA Classic Excel™ and LMA Unique™ provides a better fibreoptic view of the larynx and also provides a conduit for larger diameter endotracheal tube.[18]
The use of predictive scores in a scenario of anticipated difficult airway does not include any parameter that has been validated for predicting difficulties in blind intubation through a ILA. Thus, the development of more specific parameter awaits further development.[19]
In this study, in a 70-year-old female patient with loose and maloccluded teeth, Air-Q ILA was successfully inserted in a single smooth attempt, thus supporting the fact that insertion of Air-Q is not hindered by less than optimal mouth opening [Video 1]. The manufacturer recommended optimal mouth opening for successful supraglottic placement of the device is 23 mm for size 3.5 and 25 mm for size 4.5 Air-Q ILA.[6,20,21]
The successful tracheal intubation (56.7%) in the first attempt and overall (76.7%) is comparable to the results obtained by E.J. Bakker et al. in their pilot study where it was 58% and 74%, respectively.[8]
External laryngeal manipulation was employed to facilitate alignment for tracheal intubation in our study. The use of this manoeuvre along with conventional endotracheal tube's rigid tip pushing against the anterior portion of the glottis may have led to the observed incidents of airway trauma and/or failed intubation. There was no statistically significant difference in the occurrence of airway trauma based on the size of Air-Q used. There was no incidence of any nerve injury often associated with use of supraglottic airway device.
In a comparative study of cobra perilaryngeal airway (PLA) and Air-Q ILA, the Cobra PLA showed a significantly higher incidence of airway trauma and post-operative sore throat.[22]
After the introduction of the Air-Q ILA, there has been further refinement in the design of the device and newer modifications have been introduced.
The Air-Q™ sp has a self-pressurising cuff which inflates to adequate pressure during positive pressure ventilation thus eliminating the adverse effects of cuff over inflation associated with the use of supraglottic airway device with an inflatable cuff.[23]
The Air-Q blocker is another recent modification which has an integrated channel which allows the passage of a naso-gastric tube thereby reducing the risk of pulmonary aspiration of gastric content. Further studies are awaited on the utilities of the devices.
The learning curve associated with the operative understanding of a novel airway device caused initial failures in attempts at blind tracheal intubation with Air-Q ILA as a conduit. With increasing experience and practice, the Air-Q ILA proved to be a reliable supraglottic airway device with an added advantage of its utility as a conduit for tracheal intubation.
The selection of size of the Air-Q for an individual as recommended by the manufacturer is based on the body weight and mouth opening. This aspect needs to be further validated based on the physiology and anatomy of the patient and the selection needs to be individualised for each patient. This would reduce the incidence of airway morbidity associated with the use of Air-Q ILA.
The Air-Q ILA is designed to cause minimal stimulation of the periglottic structures; as a conduit for blind endotracheal intubation, it attenuates the haemodynamic stress response associated with intubation.
CONCLUSION
Air-Q ILA is a reliable supraglottic airway device ensuring adequate ventilation consistently and could also prove to be a lifesaving alternative as a rescue device in difficult airway scenario. It provides a conduit for endotracheal intubation thereby providing a valuable alternative to conventional laryngoscopy-aided tracheal intubation. The safety of Air-Q ILA in regular management of the airway needs further assessment considering the number of second attempts required for successfully intubating the trachea.
Video Available on: www.ijaweb.org
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bashandy GM, Boules NS. Air-Q the intubating laryngeal airway: Comparative study of hemodynamic stress responses to tracheal intubation via air-Q and direct laryngoscopy. Egypt J Anaesth. 2012;28:95–100. [Google Scholar]
- 2.Benumof JL. Laryngeal mask airway. Indications and contraindications. Anesthesiology. 1992;77:843–6. doi: 10.1097/00000542-199211000-00001. [DOI] [PubMed] [Google Scholar]
- 3.White P, Smith I. Laryngeal mask airway. In: Benumof JL, editor. Airway Management Principles and Practice. St. Louis: Mosby; 1995. pp. 353–73. [Google Scholar]
- 4.Parmet JL, Colonna-Romano P, Horrow JC, Miller F, Gonzales J, Rosenberg H. The laryngeal mask airway reliably provides rescue ventilation in cases of unanticipated difficult tracheal intubation along with difficult mask ventilation. Anesth Analg. 1998;87:661–5. doi: 10.1097/00000539-199809000-00032. [DOI] [PubMed] [Google Scholar]
- 5.Abbas DN, Abdghaffar EM. Comparison of the air-Q intubating laryngeal airway versus the modified Williams intubating airway as aids for training in fiberoptic tracheal intubation. Ain Shams J Anaesthesiol. 2013;6:134–9. [Google Scholar]
- 6.The Air- Q® Intubating Laryngeal Airway (ILA™, Cookgas® LLC, Mercury Medical, Clearwater, FL USA): Information for Use [Package insert] [Last accessed on 2016 Apr 1]. Available from: http://mercurymed.com/pdf/air-Q_dfu.pdf .
- 7.Xue FS, Zhang GH, Li XY, Sun HT, Li P, Li CW, et al. Comparison of hemodynamic responses to orotracheal intubation with the GlideScope videolaryngoscope and the Macintosh direct laryngoscope. J Clin Anesth. 2007;19:245–50. doi: 10.1016/j.jclinane.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 8.Bakker EJ, Valkenburg M, Galvin EM. Pilot study of the air-Q intubating laryngeal airway in clinical use. Anaesth Intensive Care. 2010;38:346–8. doi: 10.1177/0310057X1003800217. [DOI] [PubMed] [Google Scholar]
- 9.Khan RM, Kaul NK, Neelakanthan PH, Sharma PK. Evaluation of three adjusting manoeuvres and type of endotracheal tube in the success of air-Q aided tracheal intubation. South Afr J Anaesth Analg. 2012;18:157–60. [Google Scholar]
- 10.Abdel-Halim TM, El Enin MA, Elgoushi MM, Afifi MG, Atwa HS. Comparative study between air-Q and intubating laryngeal mask airway when used as conduit for fiber-optic. Egypt J Anaesth. 2014;30:107–13. [Google Scholar]
- 11.Schebesta K, Karanovic G, Krafft P, Rössler B, Kimberger O. Distance from the glottis to the grille: The LMA unique, Air-Q and CobraPLA as intubation conduits: A randomised trial. Eur J Anaesthesiol. 2014;31:159–65. doi: 10.1097/EJA.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 12.Elganzouri AR, Marzouk S, Youssef MM, Abdelalem N. The use of air-Q as conduit for fiberoptic endotracheal intubation in adult paralyzed patients. Egypt J Anaesth. 2012;28:249–55. [Google Scholar]
- 13.Kihara S, Watanabe S, Taguchi N, Suga A, Brimacombe JR. Tracheal intubation with the Macintosh laryngoscope versus intubating laryngeal mask airway in adults with normal airways. Anaesth Intensive Care. 2000;28:281–6. doi: 10.1177/0310057X0002800305. [DOI] [PubMed] [Google Scholar]
- 14.Shimoda O, Yoshitake A, Abe E, Koga T. Reflex responses to insertion of the intubating laryngeal mask airway, intubation and removal of the ILMA. Anaesth Intensive Care. 2002;30:766–70. doi: 10.1177/0310057X0203000608. [DOI] [PubMed] [Google Scholar]
- 15.Choyce A, Avidan MS, Harvey A, Patel C, Timberlake C, Sarang K, et al. The cardiovascular response to insertion of the intubating laryngeal mask airway. Anaesthesia. 2002;57:330–3. doi: 10.1046/j.1365-2044.2002.02463.x. [DOI] [PubMed] [Google Scholar]
- 16.Badawi R, Mohamed NN, Al-Haq MM. Tips and tricks to increase the success rate of blind tracheal intubation through the air-Q versus the intubating laryngeal mask airway Fastrach. Egypt J Anaesth. 2014;30:59–65. [Google Scholar]
- 17.Sanchez GJ, López Correa T, Sastre Corner JA. Tracheal intubation ‘blind’ to mask air-Q® (ILA-Cookgas). Comparison with ILMA intubation LMA-Fastrach™. Span J Anesthesiol. 2014;61:190–5. doi: 10.1016/j.redar.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 18.Lee AY, Benumof JL. Fiberoptic intubation through adapter removable supraglottic airways; comparison of the air-Q ILA TM, LMA classic excel TM, and LMA unique TM. Open J Anesthesiol. 2014;4:111–8. [Google Scholar]
- 19.Erlacher W, Tiefenbrunner H, Kästenbauer T, Schwarz S, Fitzgerald RD. CobraPLUS and Cookgas air-Q versus Fastrach for blind endotracheal intubation: A randomised controlled trial. Eur J Anaesthesiol. 2011;28:181–6. doi: 10.1097/EJA.0b013e328340c352. [DOI] [PubMed] [Google Scholar]
- 20.Neoh EU, Choy YC. Comparison of the air-Q ILA and the LMA-Fastrach in airway management during general anaesthesia. South Afr J Anaesth Analg. 2012;18:150–5. [Google Scholar]
- 21.Preis C, Czerny C, Preis I, Zimpfer M. Variations in ILMA external diameters: Another cause of device failure. Can J Anaesth. 2000;47:886–9. doi: 10.1007/BF03019669. [DOI] [PubMed] [Google Scholar]
- 22.Girgis KK, Youssef MM, ElZayyat NS. Comparison of the air-Q intubating laryngeal airway and the cobra perilaryngeal airway as conduits for fiber optic-guided intubation in pediatric patients. Saudi J Anaesth. 2014;8:470–6. doi: 10.4103/1658-354X.140841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Goyal R. Small is the new big: An overview of newer supraglottic airways for children. J Anaesthesiol Clin Pharmacol. 2015;31:440–9. doi: 10.4103/0970-9185.169048. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


