Abstract
Prior glaucoma severity staging systems were mostly concerned with visual field function and retinal nerve fiber layer, but did not include intraocular pressure or medications to capture resistance to treatment. We recently introduced a simple index that combines pressure, medications, and visual field damage and applied it to stratify outcomes of trabectome surgery. This microincisional glaucoma surgery removes the primary resistance to outflow in glaucoma, the trabecular meshwork, and has been mostly used in mild glaucoma. Traditional glaucoma surgeries have a relatively high complication rate and have been reserved for more advanced disease stages. In the analysis presented here we include our data of trabectome combined with cataract surgery. This is a common practice pattern as both occur in the same age group with increasing frequency. For patients in higher glaucoma index (GI) groups, the intraocular pressure (IOP) reduction was 2.34+/-0.19 mmHg more than those in a GI group one level lower while holding everything else constant. Those who had undergone trabectome combined with phacoemulsification had an IOP reduction that was 1.29+/-0.39 mmHg less compared to those with trabectome alone. No statistically significant difference was found between genders and age groups while holding everything else constant. Hispanics had a 3.81+/-1.08 mmHg greater IOP reduction. Pseudoexfoliation and steroid glaucoma patients had an IOP reduction that was greater by 2.91+/-0.56 and 3.86+/-0.81 mmHg, respectively, than those with primary open angle glaucoma. These results suggest a role for trabectome-mediated ab interno trabeculectomy beyond mild forms of glaucoma. Additionally, the multifactorial glaucoma index demonstrates a role in staging patients when comparing glaucoma surgical modalities.
Keywords: glaucoma, outflow, surgery, trabectome, ab interno trabeculectomy, disease index
Introduction
Due to an increasing human lifespan, chronic diseases that manifest later in life, such as glaucoma and cataracts, have an increasing incidence and often occur in the same individuals 1. In addition, medications used to treat glaucoma 2 or interventions to reduce intraocular pressure (IOP) 3 can cause cataracts or accelerate their occurrence. Traditional glaucoma surgery consists of trabeculectomy or tube shunt implantation, both of which have a relatively high frequency of serious complications. Ab interno trabeculectomy with the trabectome, a plasma surgical modality that ionizes and aspirates the trabecular meshwork with minimal energy transfer to surrounding tissues, was first introduced in 2004 4 and is considered a more mature microincisional glaucoma surgery. Trabectome surgery, similar to other surgeries in this family, has a favorable safety profile 5 but is often only performed in ocular hypertension or mild glaucoma stages 6.
The primary outflow resistance in glaucoma is the trabecular meshwork 7. However, more recent insight has also demonstrated a significant contribution to elevated pressure in glaucoma by an outflow resistance that is downstream of the trabecular meshwork 8– 10. According to the Goldmann equation, the limiting factor in pressure reduction from ab interno trabeculectomy with the trabectome is this residual resistance and the pressure of the episcleral veins 11, and this may vary depending on glaucoma type 12 and severity. Glaucoma severity can be described by visual field 13, optic nerve damage, and also by the number of medications needed to achieve a target IOP 14.
We recently examined the amount of IOP reduction that is due to phacoemulsification at the time of trabectome surgery and found this to be relatively clinically insignificant 9. We also noted that trabectome surgery performed after failed trabeculectomy caused patients with more advanced visual field damage to have on average a greater pressure reduction despite similar medications 10. In the current study we have consequently combined data of trabectome and phaco-trabectome surgery patients and stratified them by a glaucoma severity index. By combining both trabectome and phaco-trabectome surgery data, a more complete picture can be obtained to guide surgeons on whether ab interno trabeculectomy may be an appropriate primary intervention.
Methods
This retrospective analysis was approved (PRO14100026) by the Institutional Review Board of the University of Pittsburgh in accordance with the Declaration of Helsinki and the Health Insurance Portability and Accountability Act. Because of the retrospective nature, no consent was required. Glaucoma patients who received trabectome with or without phacoemulsification were enrolled, except in the following circumstances: history of glaucoma surgery, any subsequent cataract or glaucoma surgery in the follow-up period, and short term followup (less than 12 months). Patients were divided into four groups (from mild to severe) according to a glaucoma index (GI), an indicator of glaucoma severity based on visual field, numbers of glaucoma medication, and preoperative IOP 14. GI group 1 = mild, GI group 2 = moderate, GI group 3 = advanced, and GI4 = severe were defined based on glaucoma index scores of “≤4”, “4<GI≤8”, “8<GI≤16”, and “>16,” respectively. The main outcome measure was the reduction of IOP. Secondary outcome measures included reduction of medication and a Kaplan-Meier survival analysis. Baseline characteristics were analyzed by the Kruskal-Wallis and chisquare tests for continuous and categorical variables between GI groups, respectively. Univariate linear regression was performed first and those demographics found to be statistically significant were included into the multivariate regression analysis. Kaplan-Meier was used for survival-curve analyses. Surgical success was defined as IOP≤21 mmHg or at least 20% IOP reduction from baseline in any two consecutive visits after three months and no secondary glaucoma surgery. Log-rank test was used to compare survival distributions of GI groups.
Results
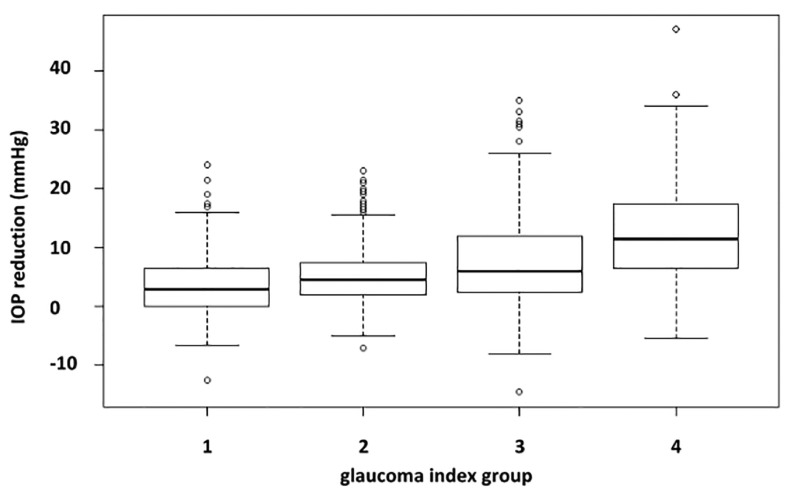
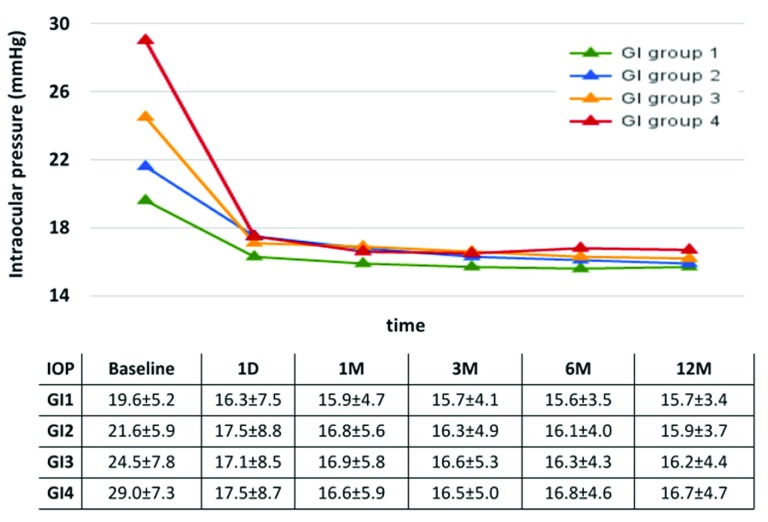
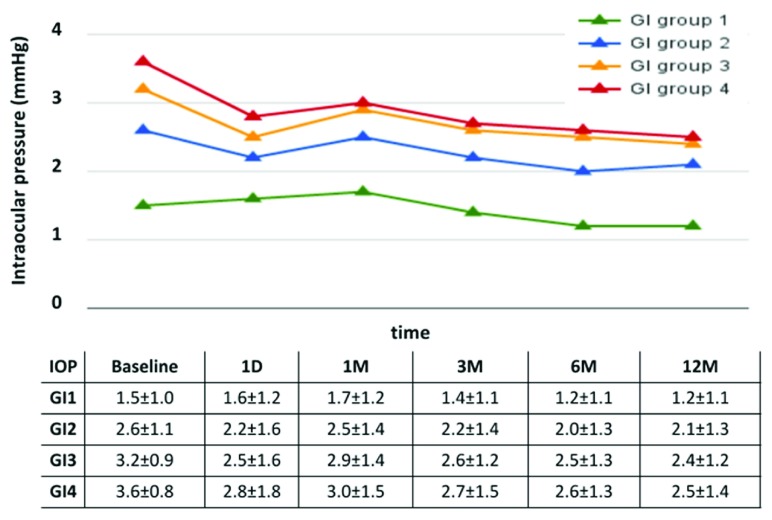
A total of 1340 cases of glaucoma patients were enrolled in the study and most of them were primary open angle glaucoma (POAG). The distribution across glaucoma severity groups was relatively even in number and average ages ( Table 1). There was a slight preponderance of female patients in the mild and moderate groups. The ethnicity of most patients was Caucasian followed by Asian. POAG and pseudoexfoliation glaucoma were the most common diagnoses. The cup disc ratio increased by glaucoma index group and more patients were phakic than pseudophakic. More patients in the higher GI groups had a trabectome surgery that was combined with cataract surgery. Patients with a higher GI group had a more profound IOP reduction ( Figure 1). At one year, the mean IOP reduction was 3.57±5.01, 5.34±5.40, 7.75±7.40, 12.09±8.08 mmHg for GI group 1 to 4, respectively. This pressure decrease occurred already on day 1 and remained relatively stable ( Figure 2). Similarly, patients with more severe glaucoma experienced a larger reduction in medications which were tapered more gradually ( Figure 3). When we stratified the overall IOP reduction by glaucoma severity, patients with worse glaucoma had the largest decrease.
Figure 1. Reduction of intraocular pressure at 1 year.
More severe glaucoma was associated with a larger pressure reduction.
Figure 2. Intraocular pressure over time by glaucoma index group.
Patients with a higher group had the largest decrease (average and standard deviation).
Figure 3. Medications by glaucoma index group.
Patients in the severe and advanced groups had the largest medication reduction (average and standard deviation).
Table 1. Demographics.
Glaucoma index (GI); GI1 Mild: GI≤4; GI2 Moderate: 4<GI≤8; GI3 Advanced: 8<GI≤16; GI4 Severe: GI>16.
| GI Group 1
n=368 |
GI Group 2
n=322 |
GI Group 3
n=370 |
GI Group 4
n=280 |
p-value | |
|---|---|---|---|---|---|
| Age | 0.02 | ||||
| Mean±SD | 71±11 | 68±13 | 69±15 | 66±18 | |
| Range | 18 – 92 | 18 – 90 | 18 – 96 | 18 – 96 | |
| Gender | <0.01 | ||||
| Female | 225 (61%) | 181 (56%) | 183 (49%) | 135 (48%) | |
| Male | 139 (38%) | 139 (43%) | 184 (50%) | 136 (49%) | |
| NR | 4 (1%) | 2 (1%) | 3 (1%) | 9 (3%) | |
| Race | <0.01 | ||||
| African American | 29 (8%) | 16 (5%) | 17 (5%) | 14 (5%) | |
| Asian | 98 (27%) | 86 (27%) | 115 (31%) | 107 (38%) | |
| Caucasian | 203 (55%) | 177 (55%) | 202 (55%) | 124 (44%) | |
| Hispanic | 23 (6%) | 16 (5%) | 17 (5%) | 21 (8%) | |
| Other | 15 (4%) | 27 (8%) | 19 (5%) | 14 (5%) | |
| Glaucoma Diagnosis | <0.01 | ||||
| Primary open angle | 288 (78%) | 241 (75%) | 257 (69%) | 179 (64%) | |
| Pseudoexfoliation | 28 (8%) | 37 (11%) | 59 (16%) | 41 (15%) | |
| Pigment Dispersion | 18 (5%) | 10 (3%) | 11 (3%) | 6 (2%) | |
| Steroid | 10 (3%) | 18 (6%) | 28 (8%) | 39 (14%) | |
| Open angle type not
specified |
24 (7%) | 16 (5%) | 15 (4%) | 15 (5%) | |
| Visual Acuity (logMAR) | <0.01 | ||||
| Mean±SD | 0.31±0.34 | 0.28±0.35 | 0.37±0.52 | 0.47±0.61 | |
| Range | -0.19 – 2.12 | -0.19 – 2.00 | -0.19 – 3.00 | -0.19 – 3.00 | |
| Cup/Disc Ratio | <0.01 | ||||
| Mean±SD | 0.69±0.18 | 0.74±0.15 | 0.75±0.17 | 0.83±0.12 | |
| Range3 | 0.1 – 1.9 | 0.3 – 1.00 | 0.1 – 1.00 | 0.25 – 1.00 | |
| Lens Status | <0.01 | ||||
| Phakic | 296 (80%) | 231 (72%) | 240 (65%) | 159 (57%) | |
| Pseudophakic | 56 (15%) | 78 (24%) | 116 (31%) | 104 (37%) | |
| Aphakic | 1 (0%) | 1 (0%) | 0 (0%) | 3 (1%) | |
| Not recorded | 15 (4%) | 12 (4%) | 14 (4%) | 14 (5%) | |
| Shaffer Grade | 0.47 | ||||
| I | 5 (1%) | 6 (2%) | 4 (1%) | 2 (1%) | |
| II | 23 (6%) | 25 (8%) | 20 (5%) | 27 (10%) | |
| III | 107 (29%) | 99 (31%) | 121 (33%) | 85 (30%) | |
| IV | 192 (52%) | 146 (45%) | 172 (46%) | 134 (48%) | |
| NR | 41 (11%) | 46 (14%) | 53 (14%) | 32 (11%) | |
| Combined Surgeries | <0.01 | ||||
| Trabectome+Phaco | 164 (45%) | 202 (63%) | 260 (70%) | 216 (77%) | |
| Trabectome Alone | 204 (55%) | 120 (37%) | 110 (30%) | 64 (23%) |
In the univariate regression analysis, age was slightly negatively correlated with the amount of IOP reduction ( Table 2) but this was not noted in the multivariate regression ( Table 3) while male gender had a positive correlation in the univariate but not anymore in the multivariate regression. For patients in the higher GI group, the IOP reduction was 2.34±0.19 mmHg more than those in one level lower GI group while holding everything else constant. Hispanics experienced a pressure drop larger by 3.81±1.08 mmHg than other ethnicities as did patients with a diagnosis of pseudoexfoliation and steroid induced glaucoma ( Table 3). IOP reduction was 2.91±0.56 and 3.86±0.81 mmHg more than in POAG patients. Interestingly, cataract surgery was associated with a slightly worse IOP reduction by 1.29+/-0.39 mmHg ( Table 3).
Table 2. Univariate regression.
| Coefficient | Standard
Error |
p-value | |
|---|---|---|---|
| Age | -0.06 | 0.02 | <0.01 |
| Male | 1.12 | 0.40 | 0.01 |
| Ethnicity | |||
| Asian | 0.45 | 0.90 | 0.61 |
| Caucasian | 0.12 | 0.87 | 0.89 |
| Hispanic | 4.45 | 1.16 | <0.01 |
| Other | -0.57 | 1.26 | 0.66 |
| Diagnosis | |||
| Open angle type not
specified |
0.78 | 0.90 | 0.39 |
| Pigmentary Dispersion | 0.41 | 1.12 | 0.71 |
| Pseudoexfoliation
Glaucoma |
3.44 | 0.59 | <0.01 |
| Steroid Glaucoma | 5.38 | 0.88 | <0.01 |
| Cup/Disc Ratio | -2.30 | 1.34 | 0.09 |
| Shaffer Grade | -0.38 | 0.31 | 0.21 |
| Lens | |||
| Aphakic | 0.59 | 3.10 | 0.85 |
| Pseudophakic | 0.66 | 0.49 | 0.18 |
| Combined with phaco | -3.20 | 0.41 | <0.01 |
Table 3. Multivariate Regression.
| Coefficient | Standard
Error |
p-value | |
|---|---|---|---|
| Glaucoma index group | 2.34 | 0.19 | <0.01 |
| Age | -0.02 | 0.02 | 0.11 |
| Male | 0.60 | 0.38 | 0.12 |
| Ethnicity | |||
| Asian | -0.57 | 0.84 | 0.50 |
| Caucasian | 0.10 | 0.84 | 0.90 |
| Hispanic | 3.81 | 1.08 | <0.01 |
| Other | -0.30 | 1.05 | 0.78 |
| Diagnosis | |||
| Open angle type not
specified |
1.30 | 0.79 | 0.10 |
| Pigmentary Dispersion | 0.54 | 1.10 | 0.62 |
| Pseudoexfoliative
Glaucoma |
2.91 | 0.56 | <0.01 |
| Steroid Glaucoma | 3.86 | 0.81 | <0.01 |
| Combined with phaco | -1.29 | 0.39 | <0.01 |
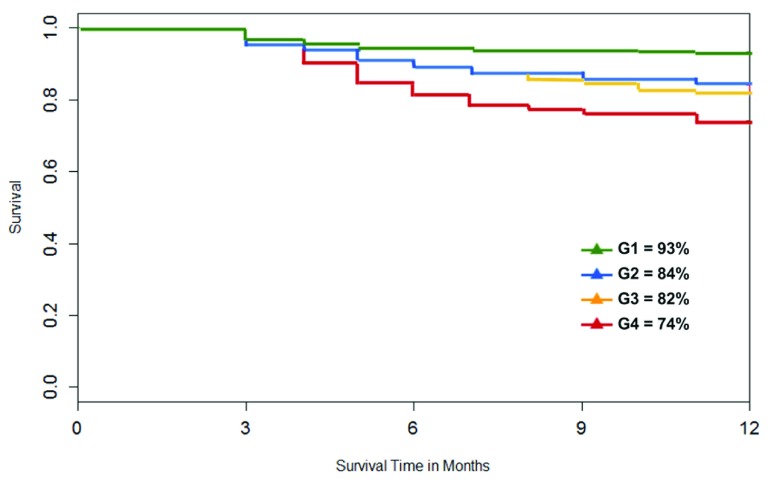
Survival rate at 12 months was 93%, 84%, 82% and 74% for GI group 1 to 4 ( Figure 4). Log-rank test indicated statistically significant differences between the GI groups and patients in the lower GI groups had a higher survival rate than those in higher GI groups.
Figure 4. Survival plot by GI groups.
The highest GI group with more advanced glaucoma (GI4, red) had the worst survival.
Discussion
The results of the current study are confirmatory of our prior study where we examined the impact of a glaucoma severity index on the results of trabectome surgery when done as a standalone procedure 14. The larger number of patients involved here allowed discovery of additional factors. We included here phaco-trabectome patients, who have a different, mixed indication that often includes visually significant cataract as the primary motivator while presenting with a relatively stable glaucoma. We did so after demonstrating by a rigorous statistical matching method, coarsened exact matching 15, that phacoemulsification does not contribute significantly to IOP reduction when done at the same time 9 or in a surgery prior to trabectome surgery 16.
The results of this study match established risk factors and findings from other studies. Steroid glaucoma and pseudoexfoliation often produce very high IOPs and the primary pathology is located in the trabecular meshwork. As a result, ablating the meshwork reduces intraocular pressure very effectively 17.
In that study we found that a larger pressure reduction is achieved in more severe glaucoma consisting of a more advanced visual field damage, a higher pre-intervention IOP and more medications. We had previously found that cup disc ratio, Hispanic ethnicity and diagnosis of steroid-induced glaucoma are related to a larger IOP reduction 14. In addition to steroid induced glaucoma, pseudoexfoliation glaucoma confers a larger IOP reduction in the present study. Although phacoemulsification was negatively correlated with IOP reduction in this analysis, something that has been described for combined traditional trabeculectomy 18, 19, it is important to recall that this study was not designed to formally compare outcomes of combined versus trabectome-alone as we have done before 9. The number of patients analyzed here is significantly higher than in the two separate studies but we note similar results in the regression analysis allowing to discover additional factors.
The Goldmann equation describes that the limiting factor to IOP reduction after removal of the trabecular meshwork, the substrate of the main outflow resistance, is the episcleral venous pressure and uveoscleral outflow 11. The data presented here indicate that that this is mostly true also for more advanced glaucoma and consistent with two prior studies that demonstrated that significant conventional outflow can be recovered even after failed tube shunts 20 and after failed trabeculectomy 10. Small differences of the eventually achieved pressures could be explained by an episcleral venous pressures that is higher in glaucoma 12. Overall, the data presented here suggest that ab interno trabeculectomy might be an appropriate surgery to attempt to control more than mild glaucoma.
Data availability
The data referenced by this article are under copyright with the following copyright statement: Copyright: © 2016 Dang Y et al.
The raw datasets could not be made available because the data could not be sufficiently anonymised to protect patient confidentiality. No individuals other than the investigators or research staff involved in the conduct of this research study and authorized representatives of the University Research Conduct and Compliance Office (RCCO) are permitted access to research data or documents (including medical record information) associated with the conduct of this research study. Institutional IRB rules are available on the following University of Pittsburgh OSIRIS website: http://www.osiris.pitt.edu/osiris. The approval permit number for this study is PRO14100026.
Funding Statement
This study was funded by the Eye and Ear Foundation of Pittsburgh.
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 1; referees: 3 approved]
References
- 1. Guedes G, Tsai JC, Loewen NA: Glaucoma and aging. Curr Aging Sci. 2011;4(2):110–7. 10.2174/1874609811104020110 [DOI] [PubMed] [Google Scholar]
- 2. Chandrasekaran S, Cumming RG, Rochtchina E, et al. : Associations between elevated intraocular pressure and glaucoma, use of glaucoma medications, and 5-year incident cataract: the Blue Mountains Eye Study. Ophthalmology. 2006;113(3):417–24. 10.1016/j.ophtha.2005.10.050 [DOI] [PubMed] [Google Scholar]
- 3. Patel HY, Danesh-Meyer HV: Incidence and management of cataract after glaucoma surgery. Curr Opin Ophthalmol. 2013;24(1):15–20. 10.1097/ICU.0b013e32835ab55f [DOI] [PubMed] [Google Scholar]
- 4. Minckler DS, Baerveldt G, Alfaro MR, et al. : Clinical results with the Trabectome for treatment of open-angle glaucoma. Ophthalmology. 2005;112(6):962–7. 10.1016/j.ophtha.2004.12.043 [DOI] [PubMed] [Google Scholar]
- 5. Kaplowitz K, Bussel II, Honkanen R, et al. : Review and meta-analysis of ab-interno trabeculectomy outcomes. Br J Ophthalmol. 2016. pii: bjophthalmol-2015-307131. 10.1136/bjophthalmol-2015-307131 [DOI] [PubMed] [Google Scholar]
- 6. Kaplowitz K, Schuman JS, Loewen NA: Techniques and outcomes of minimally invasive trabecular ablation and bypass surgery. Br J Ophthalmol. 2014;98(5):579–85. 10.1136/bjophthalmol-2013-304256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ethier CR, Kamm RD, Palaszewski BA, et al. : Calculations of flow resistance in the juxtacanalicular meshwork. Invest Ophthalmol Vis Sci. 1986;27(12):1741–50. [PubMed] [Google Scholar]
- 8. Schuman JS, Chang W, Wang N, et al. : Excimer laser effects on outflow facility and outflow pathway morphology. Invest Ophthalmol Vis Sci. 1999;40(8):1676–80. [PubMed] [Google Scholar]
- 9. Parikh HA, Bussel II, Schuman JS, et al. : Coarsened Exact Matching of Phaco-Trabectome to Trabectome in Phakic Patients: Lack of Additional Pressure Reduction from Phacoemulsification. PLoS One. 2016;11(2):e0149384. 10.1371/journal.pone.0149384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bussel II, Kaplowitz K, Schuman JS, et al. : Outcomes of ab interno trabeculectomy with the trabectome after failed trabeculectomy. Br J Ophthalmol.BMJ Publishing Group Ltd.2015;99(2):258–62. 10.1136/bjophthalmol-2013-304717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Brubaker RF: Goldmann’s equation and clinical measures of aqueous dynamics. Exp Eye Res. 2004;78(3):633–7. 10.1016/j.exer.2003.07.002 [DOI] [PubMed] [Google Scholar]
- 12. Selbach JM, Posielek K, Steuhl KP, et al. : Episcleral venous pressure in untreated primary open-angle and normal-tension glaucoma. Ophthalmologica. 2005;219(6):357–61. 10.1159/000088378 [DOI] [PubMed] [Google Scholar]
- 13. Ng M, Sample PA, Pascual JP, et al. : Comparison of visual field severity classification systems for glaucoma. J Glaucoma. 2012;21(8):551–61. 10.1097/IJG.0b013e31821dac66 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Loewen RT, Roy P, Parikh HA, et al. : Impact of a Glaucoma Severity Index on Results of Trabectome Surgery: Larger Pressure Reduction in More Severe Glaucoma. PLoS One. 2016;11(3):e0151926. 10.1371/journal.pone.0151926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Iacus SM, King G, Porro G: Causal Inference without Balance Checking: Coarsened Exact Matching. Polit Anal. 2012;20(1):1–24. 10.1093/pan/mpr013 [DOI] [Google Scholar]
- 16. Bussel I, Neiweem A, Schuman J, et al. : Glaucoma Surgery Calculator: Limited Additive IOP Effect of Phacoemulsification on Ab Interno Trabeculectomy. F1000Res. 2016;5 [cited 2016 Mar 20]. 10.7490/f1000research.1111456.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Widder RA, Dinslage S, Rosentreter A, et al. : A new surgical triple procedure in pseudoexfoliation glaucoma using cataract surgery, Trabectome, and trabecular aspiration. Graefes Arch Clin Exp Ophthalmol. 2014;252(12):1971–5. 10.1007/s00417-014-2795-z [DOI] [PubMed] [Google Scholar]
- 18. Naveh N, Kottass R, Glovinsky J, et al. : The long-term effect on intraocular pressure of a procedure combining trabeculectomy and cataract surgery, as compared with trabeculectomy alone. Ophthalmic Surg. 1990;21(5):339–45. [PubMed] [Google Scholar]
- 19. Kosmin AS, Wishart PK, Ridges PJ: Long-term intraocular pressure control after cataract extraction with trabeculectomy: phacoemulsification versus extracapsular technique. J Cataract Refract Surg.Elsevier;1998;24(2):249–55. 10.1016/S0886-3350(98)80207-1 [DOI] [PubMed] [Google Scholar]
- 20. Mosaed S, Chak G, Haider A, et al. : Results of Trabectome Surgery Following Failed Glaucoma Tube Shunt Implantation: Cohort Study. Medicine (Baltimore). 2015;94(30):e1045. 10.1097/MD.0000000000001045 [DOI] [PMC free article] [PubMed] [Google Scholar]