Abstract
The purpose of this study was to evaluate the central axis dose in the build-up region and the surface dose of a 6 MV and 10 MV flattened photon beam (FB) and flattening filter free (FFF) therapeutic photon beam for different square field sizes (FSs) for a Varian Truebeam linear accelerator using parallel-plate ionization chamber and Gafchromic film. Knowledge of dosimetric characteristics in the build-up region and surface dose of the FFF is essential for clinical care. The dose measurements were also obtained empirically using two different commonly used dosimeters: a p-type photon semiconductor dosimeter and a cylindrical ionization chamber. Surface dose increased linearly with FS for both FB and FFF photon beams. The surface dose values of FFF were higher than the FB FSs. The measured surface dose clearly increases with increasing FS. The FFF beams have a modestly higher surface dose in the build-up region than the FB. The dependence of source to skin distance (SSD) is less significant in FFF beams when compared to the flattened beams at extended SSDs.
Keywords: Flattening filter-free, Gafchromic films, NACP chamber, photon beams, surface dose
Introduction
The dose at the skin surface is the sum of the two component doses; the first results from contaminant electrons from the air, in the collimator, and in the scattering material in the beam path,[1,2,3,4,5] and the second component comes from secondary electrons[6] produced in the irradiated patient. The dose from secondary electrons generated in the patient depends primarily on the field size (FS) of the irradiated field but reaches an asymptotic value for large fields with sufficiently deep backscattering material to produce a lateral electron equilibrium.[1] However, the dose from contaminant electrons from the head depends strongly on clinical setup, such as FS, beam modifier (wedge), tray, block, and source-to-surface distance (SSD).[7,8,9,10,11]
In previous studies, the surface dose from therapeutic photon beams was investigated by using one of the various types of dosimeter, such as a thermoluminescence dosimeter,[12,13,14] radiochromic film,[15,16,17,18] and many types of parallel-plate ionization chambers.[19,20,21,22,23] Fixed-electrode separation (parallel-plate) chambers are now commonly available and are also convenient for measuring the surface dose in clinical situations. However, their accuracy in the build-up region remains in doubt because a cavity perturbation from the chamber volume causes excess ionizations. To obtain an accurate surface measurement, the ionization reading must be corrected by considering the perturbation conditions. Velkley et al.[24] proposed using the correction factors derived from aluminum-walled extrapolation-chamber measurements obtained by adjusting the depth dose curves in the build-up region from several types of fixed parallel-plate ionization chambers. Recently, Gerbi and Khan[21] have provided a modified approach in accurate estimation of surface dose.
In recent times, interest has increased in the use of flattening filter-free (FFF)[25] X-ray photons. When the flattening filter is removed from the X-ray beam path, photon production should be far more efficient, and dose rate should increase substantially at the treatment target, which is especially beneficial for high-dose per-fraction delivery techniques, such as stereotactic radiosurgery (SRS) and stereotactic body radiation therapy (SBRT). Use of the FFF mode for SBRT[26] in lung-cancer treatment can significantly reduce beam-on time and can facilitate breath-hold or respiratory gating[27] for more precise management of organ motion. In addition, FFF X-rays are thought to offer dosimetric advantages[25] such as reduced peripheral doses, out-of-field scattered dose,[28,29,30] and head scatter.[31,32] The FFF beams contain more low-energy components and have softer energy spectra than the corresponding flattened beams, which can lead to increased dose in the build-up region. Meanwhile, the FFF photons undergo less head scatter[33] because the flattening filter is absent from gantry head of the linear accelerator, which may decrease the dose in the build-up region. In the build-up region where longitudinal electronic disequilibrium exists, these two competing factors determine the build-up dosimetric characteristics of the FFF photons. The first factor can reduce dmax, given that the mean energy of primary photons is reduced in the FFF beams. However, the second factor will increase dmax because of the reduced contamination by head scattering of the FFF photons. The dose in the build-up region due to FFF photons thus becomes interesting and may differ from that due to conventional flattened photons. Numerous publications discuss on the surface dose measurements for FFF beams from Varian and Elekta accelerators.[25,26,27,28,29,30,31,32,33,34,35,36,37] However, relatively few dosimetric studies consider Gafchromic film-based surface dose measurements of FFF photon beams.
The surface dose is machine dependent and can be affected by many parameters, including the FS, the source-to-surface distance, the presence of beam modifiers, and the angle of beam incidence. Because of the steep dose gradient near the surface as well as in the build-up region, careful considerations are required in the selection of detectors. Generally, the size of the detector along the beam direction should be as small as possible. Extrapolation chambers are the detectors of choice for surface dose. However, its availability is limited and its use in surface dose measurements is very time-consuming. Instead, fixed-separation plane-parallel chambers are commonly used for surface dose and the dose in the build-up region. Because of their relatively large separation compared with the extrapolation chamber and their small guard ring, the plane-parallel chambers show an over-response in the build-up region and especially at the surface.
The purpose of this study was to evaluate the central axis dose in the build-up region and the surface dose delivered by a flattened photon beam (FB) and FFF beam (6 MV and 10 MV) for different square FSs with an ionization chamber and Gafchromic film. The dose measurements were also obtained with different source to skin distance (SSD) for a Varian Truebeam linear accelerator using NACP-02. Article TG-106[38] highly recommended that the surface dose measurements should not be carried out with a scanning device, but in our study, we used cylindrical ionization chamber (CC13) cylindrical chamber to measure the surface doses of FB and FFF photon beams to compare (scanning and nonscanning) surface doses values measured with NACP-02, Gafchromic film, and a p-type photon semiconductor dosimeter (PFD).
Materials and Methods
In this study, 6 and 10 MV FB and FFF beams of Truebeam (Varian Medical System, Palo Alto, CA, USA) linear accelerator were used. Based on our commissioning data with a standard source to skin distance (SSD) of 100 cm and FS of 10 cm × 10 cm, dmax is 1.5 and 2.4 cm for 6 MV and 10 MV FB and 1.4 and 2.2 cm for 6 MV and 10 MV FFF, respectively.
The surface doses delivered by the FB, and FFF beams were measured using a plane-parallel ionization chamber (NACP-02, IBA-Scanditronix, Germany) with DOSE 1 (IBA, Germany) electrometer in a solid water-equivalent phantom with adequate backscattering material. The solid water phantom has a physical density of 1.04 g/cm3. The NACP-02 chamber has a Mylar foil and graphite window with a combined thickness of 0.6 mm (104 mg/cm2). The electrode spacing is 2.0 mm, and the collecting electrode diameter is 10 mm. The surface dose measurements were done with the FB and FFF beams aligned along the central axis with square FSs of 5 cm × 5 cm, 8 cm × 8 cm, 10 cm × 10 cm, 15 cm × 15 cm, 20 cm × 20 cm, and 30 cm × 30 cm at 100 cm source-to-surface distances and with build-up depths extending from the surface to just beyond the maximum depth.
The perturbation effect was corrected using a method proposed by Gerbi and Khan.[21] To account for polarity effects, the measurements were done at both positive and negative voltage (+300 V and −300 V) for FB and FFF beams.
EBT2 (Gafchromic) films were irradiated in a 30 cm × 30 cm × 30 cm solid water phantom. The doses in the surface and build-up region dose were measured with the film sandwiched tightly between slabs and irradiated while oriented parallel to the beam axis. The film pieces themselves were 6 cm × 25 cm. Each irradiation step delivered 200 monitor units. All films were scanned 24 h after irradiation. An Epson 10000XL (Epson America, Inc., Long Beach, USA) flatbed document scanner was used to scan the films following the manufacturer scanning protocol and recommendations. Epson software was used for scanning the films in transmission mode with a resolution of 75 dpi and with all image enhancements turned off. The images were saved as 48-bit tag image file format files for further analysis. The surface dose of the scanned images was calculated by using OmniPro – I'mRT software (Version 1.6; IBA dosimetry, Germany).
Surface dose was also measured using two common dosimeters: A p-type photon PFD and a CC13. The readings from each detector were assigned to the effective point of measurement for each individual detector. For CC13 chamber, the effective point was determined automatically by the computerized scanning system. The effective points of measurement, when measuring with the PFD dosimeter and with the NACP-02 chamber, were assumed to be at front surface and at the bottom of the entrance-window electrode, respectively.
Results
All the results given below for point-dose measurements are mean values from at least five repeated measurements. The standard deviations are <1.5% and also partly crosschecked on different days to confirm the initial results remain at least within ±1.5%.
Surface dose versus field size
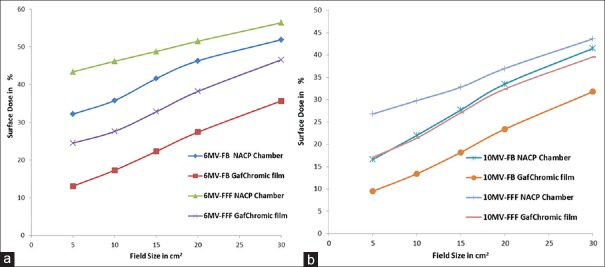
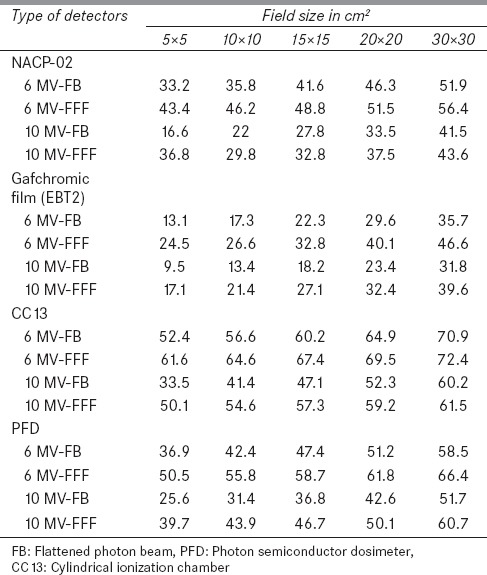
The surface dose within the build-up region increases linearly with the FS by about 1% per cm2 for both the FB and FFF photon beams. The surface dose for any FS is defined as the dose measured at surface for that field size divided by the dose at dmax at a 10 cm × 10 cm field. The relative surface dose is defined as the fractional surface dose divided by Dmax for the corresponding field for which the dose was measured. The surface dose for FB and FFF beams for various FSs was measured using the NACP-02 chamber and EBT2 film, and the results are shown in Figure 1a and b. For the 6 MV-FB (6 MV-FFF) beam, the surface dose ranges from 13.1% to 35.7% (24.5% to 46.6%) when measured by EBT2 film for FSs from 5 cm × 5 cm to 30 cm × 30 cm (SSD is 100 cm for phantom surface). For the 10 MV-FB (10 MV-FFF) beam, the surface dose ranges from 9.5% to 31.8% (17.1% to 39.6%) when measured by EBT2 film for FSs from 5 cm × 5 cm to 30 cm × 30 cm (SSD is 100 cm for phantom surface). The surface doses for the FFF beams are consistent with those for the FB beam for FSs from 5 cm × 5 cm to 30 cm × 30 cm. However, as the FS was increased from 5 cm × 5 cm to 30 cm × 30 cm, increases in the values of surface dose were observed for both FB and FFF.
Figure 1.
Surface dose of flattened photon beam and FFF beam as a function of field size at a 100 cm SSD. (a) For 6 MV and (b) for 10 MV
Doses at different build-up depths
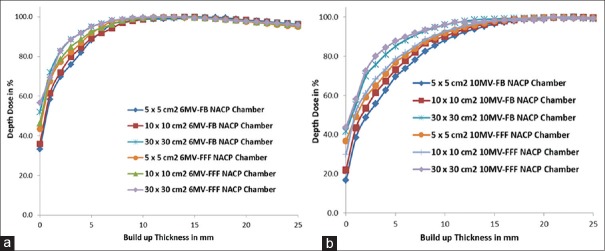
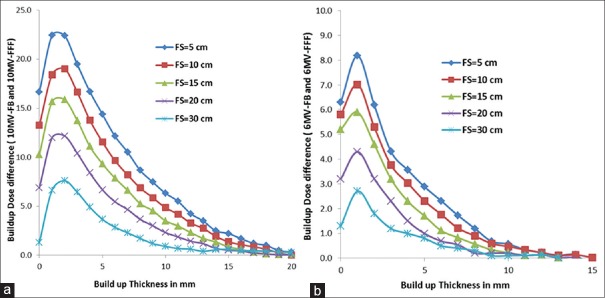
The build-up dose was modestly higher than that of the FB photons for build-up depth at FS of 5 cm × 5 cm to 30 cm × 30 cm [Figure 2a and b]. For 6 MV-FB and 6 MV-FFF with a FS of 10 cm × 10 cm, the surface dose increased from 17.3% to 89.1% and 26.6% to 92.5% in the first 5 mm build-up depths and 17.3% to 98.7% and 26.6% to 99.1%, respectively, in the first 10 mm build-up depths. Figure 3 shows that the surface dose increased from 13.4–73.1% to 21.4–78.5% in the first 5 mm build-up depths and 13.4–90.3% and 21.4–92.7%, respectively, in the first 10 mm build-up depths for 10 MV-FB and 10 MV-FFF with a FS of 10 cm × 10 cm. The difference in build-up dose between 6 MV-FB and 6 MV-FFF beams range from 8.8% to 1.5% for FSs 5 cm × 5 cm to 30 cm × 30 cm [Figure 4a]. The maximum differences were observed in the smaller field size and minimum build-up dose differences were observed in the largest FS.
Figure 2.
Build-up dose of FFF beam is modestly higher than the flattened photon beam photons for different build-up depths at various field sizes. (a) 6 MV and (b) 10 MV
Figure 3.
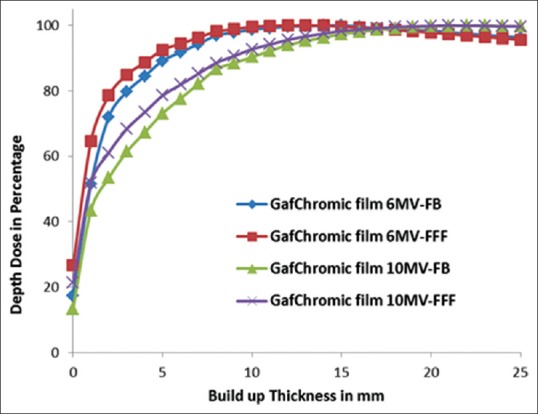
Relative surface dose of flattened photon beam and FFF photon energy as a function of field size at a SSD of 100.0 cm measured with EDT2 film
Figure 4.
Build-up dose difference between FFF and flattened photon beam photons for various field sizes. (a) 6 MV and (b) 10 MV
The difference in build-up dose between 10 MV-FB and 10 MV-FFF beams ranges from 22.4% to 6.6% for FSs 5 cm × 5 cm to 30 cm × 30 cm [Figure 4b]. The maximum differences were observed in the smaller FS and minimum build-up dose differences were observed in the largest FS. The build-up dose difference between the FB and FFF photon beams remains same for the different energies, but the quantitative value is higher in the higher energy.
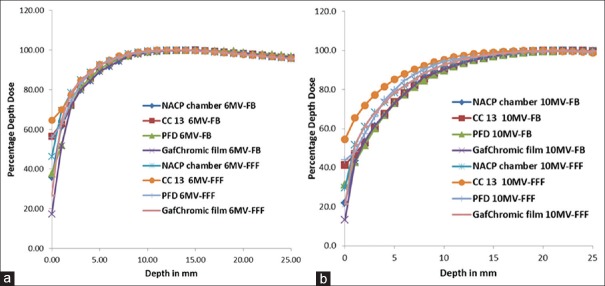
Figure 5a and b compares the depth-dose curves for the FB and FFF beams measured with various detectors for a 10 cm × 10 cm field. The three detectors measured the percent depth dose for the depth beyond the build-up region, and the results from the different detectors are consistent with each other, and these results are consistent with that of Das et al.[38] However, near the surface, the results of the three detectors differ significantly from the measured depth dose obtained with the EBT2 film.
Figure 5.
The percentage depth dose curves obtained using the Gafchromic film, cylindrical ionization chamber, photon semiconductor dosimeter, and NACP-02 chamber for the flattened photon beam and FFF photon beams with 10 cm × 10 cm field size. (a) 6 MV and (b) 10 MV
The surface dose measured with CC13 is 21.5% and 18.3% greater than when measured with NACP-02 for the 6 MV-FB and 6 MV-FFF beams, respectively, and 20.2% and 13.2% greater than measured with NACP-02 for the 10 MV-FB and 10 MV-FFF beams, respectively, for a 10 cm × 10 cm FS, at 100 cm SSD. The surface dose measured by PFD is 6.4% and 9.7% greater than when measured by NACP-02 for the 6 MV-FB and 6 MV-FFF beams, respectively, and 11.3% and 14.1% higher than the NACP-02 measured surface dose of 10MV-FB and 10 MV-FFF, respectively, for a 10 cm × 10 cm FS, at 100 cm SSD. The surface dose measured by EBT2 film is 17.3% and 19.2% less than when measured by NACP-02 for the 6 MV-FB and 6 MV-FFF beams, respectively, and 9.7% and 8.4% less than when measured by NACP-02 for the 10 MV-FB and 10 MV-FFF beams, respectively, for 10 cm × 10 cm FS, at 100 cm SSD.
Surface dose at different SSD
The FS was defined at 100 cm SSD for all the different SSD clinical setups. The surface dose increases slightly with decreasing SSDs, although this effect is relatively small with <2% change when going from 100 cm to 80 cm for a field size of 10 cm x 10 cm and for both FB and FFF photon beams. The skin dose increased rapidly as the SSD decreased for both FB and FFF photon beams, especially in larger fields. For example, the decrease in SSD can increase the skin dose up to 8% for large fields (30 cm × 30 cm) for both FB and FFF photon beams. The surface doses decrease slightly with increasing SSDs, although this effect is relatively small with <1.0% change when going from 100 cm to 120 cm for both FB and FFF photon beams for a field size of 10 cm × 10 cm. Thus, we can expect a large difference of skin dose between SSD and source-to-axis clinical setup.
Discussion
Although previous studies comprehensively described FFF beam dosimetric characteristics,[22,25,26,27,28,29,30,31,32,33,34,35,37] the dose in the build-up region nevertheless is well worth quantifying, and its clinical impact is worth pursuing. For high-energy photons used in conventional radiotherapy, skin dose may be less of a concern because of the skin-sparing effect, which allows high-energy photons to be delivered to deep-seated tumors without exceeding the tolerance of the skin. However, for the unconventional hypofractionated[26,27] (SBRT, SRS) delivery where the fractional dose is extremely high, an acute skin reaction can occur. Therefore, it is clinically important to analyze and compare the characteristics of the build-up dose for the both FB and FFF photons.
The measurements on the surface area with a parallel-plane ionization chamber, however, overestimate the surface dose because the chamber is perturbed in methods and materials. Upon applying the correction factor, the open field doses measured for both 6 and 10 MV FB beams and 10 cm × 10 cm fields decrease from 44.9% and 31.1% to 35.8% and 22.0%, respectively, and for both 6 and 10 MV FFF beams, surface doses decrease from 55.3% and 38.9% to 46.2% and 29.8%, respectively. The corrected values for 6 MV-FB are similar to the surface doses of 33.4% measured by Ishmael Parsai et al.,[39] with an extrapolation chamber at a depth of 0.5 mm and with the same FS energy.
The surface dose increases linearly with FS for both 6 MV-FB and 10 MV-FB, and 6 MV-FFF and 10 MV-FFF beams, which is due to increased electron emission from the collimator and from air. The measured surface dose for the 6 MV-FB and 10 MV-FB, and 6 MV-FFF and 10 MV-FFF beams plotted in Figure 1 against equivalent square shows statistically significant difference between the FB and FFF modes for both NACP chamber and EBT2 film measured surface doses. These results reveal the important contribution of the flattening filter to the surface dose for FSs exceeding 10 cm × 10 cm. Removal of flattening filter leads to decrease in head scatter (Sc)[28,29,32,33] for FSs above 10 cm × 10 cm.
The beam-hardening effect imposed by the flattening filter helps reduce the surface or skin dose. However, the filter also produces a large amount of scattered radiation that tends to deposit energy at shallow depths, thereby adding to the surface dose, and this effect depends strongly on FS. Dalaryd et al.[40] and Kragl et al.[37] found that the build-up dose increases with depth in solid water and the surface dose and build-up region dose delivered by the FFF beam produced by an Elekta Precise linac slightly exceeds that delivered by the FB from the same source. These results agree with our data. The photon spectrum of the FFF beam contains a greater proportion of low energy photons (<1 MeV) and lesser proportion of high energy photons compared to the FB photon beam due to the loss of beam hardening occurring through the filter.[25,41]
For both the FB and FFF photon beams, the surface dose clearly increases with increasing FS, regardless of the detector used to make the measurement. This result is mainly due to the increasing number of scattered electrons in the air and collimator. The surface dose measured by PFD dosimeter and the CC13 chamber differ greatly from that measured by the NACP-02 chamber. For a 10 cm × 10 cm FS, the PFD and CC13 dosimeters measured high percentage surface doses of about 37.8% and 56.6% for 6 MV-FB and 55.8% and 64.6% for 6 MV-FFF and 31.4% and 41.4% for 10 MV-FB and 44.0% and 54.6% for 10 MV-FFF photon beams, respectively.
A very large discrepancy was found when using the PFD dosimeter and the CC13 chamber for surface dose measurements compared to NACP-2 measured values. The higher surface doses observed with the PFD and CC13 dosimeter with the 10 cm × 10 cm FS were about 37.8% and 56.6% for 6 MV-FB and 55.8% and 64.6% for 6 MV-FFF and 31.4% and 41.4% for 10 MV-FB and 44.0% and 54.6% for 10 MV-FFF photon beams, respectively. Lukkana Apipunyasopon et al.,[41] reported scale down in the over-response of the measured surface dose by using correction factors of 0.294 and 0.378 for CC13 chamber and PFD respectively for a field size of 10 × 10 cm2. Upon applying the correction factors, the surface dose delivered by the 6 MV-FB, 6 MV-FFF, 10 MV-FB and 10 MV-FFF were 14.3%, 21.1%, 11.9% and 16.6% for PFD and 16.3%, 19.0%, 12.2% and 16.1% for CC13, respectively, for 10 cm × 10 cm FS. These corrected surface doses are consistent with published values.
The high spatial resolution and low spectral sensitivity provided by radiochromic films make them ideal for measuring dose distributions in regions in which a radiation field produces a high-dose gradient. As expected, surface dose increases with FS due to extra electron contamination and photon head scatter. Table 1 shows the surface dose for various FSs as measured by EBT2 Gafchromic film and by the NACP-02 chamber. The NACP-02 chamber overestimates the dose by 20% compared with the EBT2 Gafchromic film for both FB and FFF. We compared these results with those of Butson et al.,[42] who measured surface dose with Gafchromic film type MD-55. The data obtained in the present work are consistent with the results obtained with the Attix chamber to within 3% for 6 MV high-energy photon beams. The surface dose measured by Gafchromic film models HD-810, EBT, HS, and XR for a 6 MV photon beam was investigated more comprehensively by Devic et al.[43]
Table 1.
Comparison of relative surface doses measured with different types of dosimeter for 6 MV-flattened photon beam and 6 MV-flattening filter free photon beam and 10 MV-flattened photon beam and 10 MV-flattening filter free photon beam
In general, with respect to the SSD increase, skin dose is more pronounced for 6 MV-FB than for 10 MV-FB beams and for small fields as compared to large fields.[44,45] The effect of extended SSD (at 120 cm) dependence is less significant in FFF beams compared to FB photon beams. This is due to the loss of beam hardening occurring through the filter.
Conclusions
The FFF beams for both energies have a modestly higher surface dose in the build-up region compared to FB. The surface dose increases with increasing FS, regardless of the detector and photon beams with or without flattening filter. The dependence of SSD is less significant in FFF beams compared to the FB in extended SSDs. However, the difference is not substantial and may be clinically insignificant. Knowledge of the dosimetric characteristics in the buildup region and of the surface dose delivered by 6 MV & 10 MV-FFF beams is useful for implementations of IMRT, SRS, and SBRT techniques.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bjärngard BE, Vadash P, Zhu T. Doses near the surface in high-energy x-ray beams. Med Phys. 1995;22:465–8. doi: 10.1118/1.597477. [DOI] [PubMed] [Google Scholar]
- 2.Ling CC, Biggs PJ. Improving the buildup and depth-dose characteristics of high energy photon beams by using electron filters. Med Phys. 1979;6:296–301. doi: 10.1118/1.594585. [DOI] [PubMed] [Google Scholar]
- 3.Mackie TR, Scrimger JW. Contamination of a 15-MV photon beam by electrons and scattered photons. Radiology. 1982;144:403–9. doi: 10.1148/radiology.144.2.6806853. [DOI] [PubMed] [Google Scholar]
- 4.Nilsson B, Brahme A. Electron contamination from photon beam collimators. Radiother Oncol. 1986;5:235–44. doi: 10.1016/s0167-8140(86)80053-6. [DOI] [PubMed] [Google Scholar]
- 5.Beauvais H, Bridier A, Dutreix A. Characteristics of contamination electrons in high energy photon beams. Radiother Oncol. 1993;29:308–16. doi: 10.1016/0167-8140(93)90149-3. [DOI] [PubMed] [Google Scholar]
- 6.Nizin PS. Electronic equilibrium and primary dose in collimated photon beams. Med Phys. 1993;20:1721–9. doi: 10.1118/1.596959. [DOI] [PubMed] [Google Scholar]
- 7.McCullough EC. A measurement and analysis of buildup region dose for open field photon beams (cobalt-60 through 24 MV) Med Dosim. 1994;19:5–14. doi: 10.1016/0958-3947(94)90027-2. [DOI] [PubMed] [Google Scholar]
- 8.Fontenla DP, Napoli JJ, Hunt M, Fass D, McCormick B, Kutcher GJ. Effects of beam modifiers and immobilization devices on the dose in the build-up region. Int J Radiat Oncol Biol Phys. 1994;30:211–9. doi: 10.1016/0360-3016(94)90537-1. [DOI] [PubMed] [Google Scholar]
- 9.Klein EE, Purdy JA. Entrance and exit dose regions for a Clinac-2100C. Int J Radiat Oncol Biol Phys. 1993;27:429–35. doi: 10.1016/0360-3016(93)90256-u. [DOI] [PubMed] [Google Scholar]
- 10.McParland BJ. The effects of a universal wedge and beam obliquity upon the central axis dose buildup for 6-MV x-rays. Med Phys. 1991;18:740–3. doi: 10.1118/1.596733. [DOI] [PubMed] [Google Scholar]
- 11.Jani SK, Pennington EC. Depth dose characteristics of 24-MV x-ray beams at extended SSD. Med Phys. 1991;18:292–4. doi: 10.1118/1.596673. [DOI] [PubMed] [Google Scholar]
- 12.Nilsson B, Sorcini B. Surface dose measurements in clinical photon beams. Acta Oncol. 1989;28:537–42. doi: 10.3109/02841868909092265. [DOI] [PubMed] [Google Scholar]
- 13.Stathakis S, Li JS, Paskalev K, Yang J, Wang L, Ma CM. Ultra-thin TLDs for skin dose determination in high energy photon beams. Phys Med Biol. 2006;51:3549–67. doi: 10.1088/0031-9155/51/14/018. [DOI] [PubMed] [Google Scholar]
- 14.Hsu SH, Roberson PL, Chen Y, Marsh RB, Pierce LJ, Moran JM. Assessment of skin dose for breast chest wall radiotherapy as a function of bolus material. Phys Med Biol. 2008;53:2593–606. doi: 10.1088/0031-9155/53/10/010. [DOI] [PubMed] [Google Scholar]
- 15.Butso MJ, Cheung T, Yu PK, Webb B. Variations in skin dose associated with linac bed material at 6 MV x-ray energy. Phys Med Biol. 2002;47:N25–30. doi: 10.1088/0031-9155/47/1/404. [DOI] [PubMed] [Google Scholar]
- 16.Paelinck L, De Wagter C, Van Esch A, Duthoy W, Depuydt T, De Neve W. Comparison of build-up dose between Elekta and Varian linear accelerators for high-energy photon beams using radiochromic film and clinical implications for IMRT head and neck treatments. Phys Med Biol. 2005;50:413–28. doi: 10.1088/0031-9155/50/3/002. [DOI] [PubMed] [Google Scholar]
- 17.Price S, Williams M, Butson M, Metcalfe P. Comparison of skin dose between conventional radiotherapy and IMRT. Australas Phys Eng Sci Med. 2006;29:272–7. doi: 10.1007/BF03178577. [DOI] [PubMed] [Google Scholar]
- 18.Devic S, Seuntjens J, Abdel-Rahman W, Evans M, Olivares M, Podgorsak EB, et al. Accurate skin dose measurements using radiochromic film in clinical applications. Med Phys. 2006;33:1116–24. doi: 10.1118/1.2179169. [DOI] [PubMed] [Google Scholar]
- 19.Nilsson B, Montelius A. Fluence perturbation in photon beams under nonequilibrium conditions. Med Phys. 1986;13:191–5. doi: 10.1118/1.595895. [DOI] [PubMed] [Google Scholar]
- 20.Mellenberg DE., Jr Determination of build-up region over-response corrections for a Markus-type chamber. Med Phys. 1990;17:1041–4. doi: 10.1118/1.596579. [DOI] [PubMed] [Google Scholar]
- 21.Gerbi BJ, Khan FM. Measurement of dose in the buildup region using fixed-separation plane-parallel ionization chambers. Med Phys. 1990;17:17–26. doi: 10.1118/1.596522. [DOI] [PubMed] [Google Scholar]
- 22.Lamb A, Blake S. Investigation and modelling of the surface dose from linear accelerator produced 6 and 10 MV photon beams. Phys Med Biol. 1998;43:1133–46. doi: 10.1088/0031-9155/43/5/006. [DOI] [PubMed] [Google Scholar]
- 23.Carl J, Vestergaard A. Skin damage probabilities using fixation materials in high-energy photon beams. Radiother Oncol. 2000;55:191–8. doi: 10.1016/s0167-8140(00)00177-8. [DOI] [PubMed] [Google Scholar]
- 24.Velkley DE, Manson DJ, Purdy JA, Oliver GD., Jr Build-up region of megavoltage photon radiation sources. Med Phys. 1975;2:14–9. doi: 10.1118/1.594158. [DOI] [PubMed] [Google Scholar]
- 25.Georg D, Knöös T, McClean B. Current status and future perspective of flattening filter free photon beams. Med Phys. 2011;38:1280–93. doi: 10.1118/1.3554643. [DOI] [PubMed] [Google Scholar]
- 26.Wang Y, Golden N, Ting JY. Treatment Planning Study: Flattening Filter Free X-Rays vs. Conventional Flattened X-Rays for Stereotactic Body Radiation Therapy of Stage 1A Non-Small Cell Lung Cancer (NSCLC). Presented at the Annual Meeting of the Radiological Society of North America; Chicago, IL. 2011. [Google Scholar]
- 27.Vassiliev ON, Kry SF, Chang JY, Balter PA, Titt U, Mohan R. Stereotactic radiotherapy for lung cancer using a flattening filter free Clinac. J Appl Clin Med Phys. 2009;10:2880. doi: 10.1120/jacmp.v10i1.2880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kragl G, Baier F, Lutz S, Albrich D, Dalaryd M, Kroupa B, et al. Flattening filter free beams in SBRT and IMRT: dosimetric assessment of peripheral doses. Z Med Phys. 2011;21:91–101. doi: 10.1016/j.zemedi.2010.07.003. [DOI] [PubMed] [Google Scholar]
- 29.Kry SF, Vassiliev ON, Mohan R. Out-of-field photon dose following removal of the flattening filter from a medical accelerator. Phys Med Biol. 2010;55:2155–66. doi: 10.1088/0031-9155/55/8/003. [DOI] [PubMed] [Google Scholar]
- 30.Vassiliev ON, Titt U, Pönisch F, Kry SF, Mohan R, Gillin MT. Dosimetric properties of photon beams from a flattening filter free clinical accelerator. Phys Med Biol. 2006;51:1907–17. doi: 10.1088/0031-9155/51/7/019. [DOI] [PubMed] [Google Scholar]
- 31.Wang Y, Gajdos S, Tendulkar R, Vassil A, Bayouth J, Xis P. Application of non flat beams for breast radiotherapy using direct aperture optimization. Med Phys. 2010;37:3215. [Google Scholar]
- 32.Ashokkumar S, Nambi Raj NA, Sinha SN, Yadav G, Thiyagarajan R, Raman K, et al. Comparison of head scatter factor for 6MV and 10MV flattened (FB) and unflattened (FFF) photon beam using indigenously designed columnar mini phantom. J Med Phys. 2014;39:184–91. doi: 10.4103/0971-6203.139010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ashokkumar S, Nambiraj A, Sinha SN, Yadav G, Raman K, Bhushan M, et al. Measurement and comparison of head scatter factor for 7 MV unflattened (FFF) and 6 MV flattened photon beam using indigenously designed columnar mini phantom. Rep Pract Oncol Radiother. 2015;20:170–80. doi: 10.1016/j.rpor.2015.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Javedan K, Feygelman V, Zhang RR, Moros EG, Correa CR, Trotti A, et al. Monte Carlo comparison of superficial dose between flattening filter free and flattened beams. Phys Med. 2014;30:503–8. doi: 10.1016/j.ejmp.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 35.Sahani G, Sharma SD, Sharma PK, Deshpande DD, Negi PS, Sathianarayanan VK, et al. Acceptance criteria for flattening filter-free photon beam from standard medical electron linear accelerator: AERB task group recommendations. J Med Phys. 2014;39:206–11. doi: 10.4103/0971-6203.144482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang Y, Khan MK, Ting JY, Easterling SB. Surface dose investigation of the flattening filter-free photon beams. Int J Radiat Oncol Biol Phys. 2012;83:e281–5. doi: 10.1016/j.ijrobp.2011.12.064. [DOI] [PubMed] [Google Scholar]
- 37.Kragl G, af Wetterstedt S, Knäusl B, Lind M, McCavana P, Knöös T, et al. Dosimetric characteristics of 6 and 10MV unflattened photon beams. Radiother Oncol. 2009;93:141–6. doi: 10.1016/j.radonc.2009.06.008. [DOI] [PubMed] [Google Scholar]
- 38.Das IJ, Cheng CW, Watts RJ, Ahnesjö A, Gibbons J, Li XA, et al. Accelerator beam data commissioning equipment and procedures: report of the TG-106 of the Therapy Physics Committee of the AAPM. Med Phys. 2008;35:4186–215. doi: 10.1118/1.2969070. [DOI] [PubMed] [Google Scholar]
- 39.Ishmael Parsai E, Shvydka D, Pearson D, Gopalakrishnan M, Feldmeier JJ. Surface and build-up region dose analysis for clinical radiotherapy photon beams. Appl Radiat Isot. 2008;66:1438–42. doi: 10.1016/j.apradiso.2008.02.089. [DOI] [PubMed] [Google Scholar]
- 40.Dalaryd M, Kragl G, Ceberg C, Georg D, McClean B, af Wetterstedt S, et al. A Monte Carlo study of a flattening filter-free linear accelerator verified with measurements. Phys Med Biol. 2010;55:7333–44. doi: 10.1088/0031-9155/55/23/010. [DOI] [PubMed] [Google Scholar]
- 41.Apipunyasopon L, Srisatit S, Phaisangittisakul N. An investigation of the depth dose in the build-up region, and surface dose for a 6-MV therapeutic photon beam: Monte Carlo simulation and measurements. J Radiat Res. 2013;54:374–82. doi: 10.1093/jrr/rrs097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Butson MJ, Yu PK, Metcalfe EM. Extrapolated surface dose measurements with radiochromic film. Med Phys. 1999;26:485–7. [Google Scholar]
- 43.Devic S, Seuntjens J, Abdel-Rahman W, Evans M, Olivares M, Podgorsak EB, et al. Accurate skin dose measurements using radiochromic film in clinical applications. Med Phys. 2006;33:1116–24. doi: 10.1118/1.2179169. [DOI] [PubMed] [Google Scholar]
- 44.De Ost B, Vanregemorter J, Schaeken B, Van den Weyngaert D. The effect of carbon fibre inserts on the build-up and attenuation of high energy photon beams. Radiother Oncol. 1997;45:275–7. doi: 10.1016/s0167-8140(97)00118-7. [DOI] [PubMed] [Google Scholar]
- 45.Higgins DM, Whitehurst P, Morgan AM. The effect of carbon fiber couch inserts on surface dose with beam size variation. Med Dosim. 2001;26:251–4. doi: 10.1016/s0958-3947(01)00071-1. [DOI] [PubMed] [Google Scholar]