Abstract
We present a case of neck pain in a middle-aged woman, initially attributed to a retropharyngeal infection and treated with urgent intubation. With the help of computed tomography, the diagnosis was later revised to acute prevertebral calcific tendinitis, a self-limiting condition caused by abnormal calcium hydroxyapatite deposition in the longus colli muscles. It is critical to differentiate between these two disease entities due to dramatic differences in management. A discussion of acute prevertebral calcific tendinitis and its imaging findings is provided below.
Keywords: acute prevertebral calcific tendinitis, acute calcific tendinitis of the longus colli muscle, calcific retropharyngeal tendinitis, retropharyngeal edema, computed tomography of the neck
CASE REPORT
A 41 year old woman presented to a peripheral hospital with acute onset of sore throat, mild dysphagia, and neck tenderness. There was no preceding history of trauma, upper respiratory tract infection, or dental infection. She was in no distress, afebrile and with a mild leukocytosis of 12.3 × 103 cells/mm3. A lateral nasopharyngeal radiograph demonstrated nonspecific retropharyngeal thickening (Figure 1). A contrast enhanced computed tomographic (CT) examination of the neck (Figure 2) revealed edema within the retropharyngeal space without cervical lymphadenopathy. Subtle calcifications within the tendinous fibers of the longus colli muscles were not commented upon. The patient was urgently intubated for the presumed infection to secure the airway prior to the development of respiratory distress. She was transferred to a tertiary centre to the otolaryngology service and she was treated with IV antibiotic therapy for presumed retropharyngeal abscess. After three days in the intensive care unit, a repeat CT of the neck with contrast was obtained showing the same findings. Upon recognition of the longus colli tendinous calcifications, a diagnosis of acute prevertebral calcific tendinitis was made. The patient was extubated without issue and discharged home on oral non-steroidal anti-inflammatory drugs (NSAIDs) and antibiotics. Two month CT and three month radiographic follow-up images (Figure 3) prior to the clinical follow-up demonstrated resolution of the effusion and near complete resolution of the longus colli muscle calcifications, consistent with the diagnosis of acute prevertebral calcific tendinitis. At the 3-month clinical follow-up appointment, the patient had a full recovery without any swallowing or airway difficulties. She had a few intermittent episodes of pain, which were controlled with ibuprofen and acetaminophen.
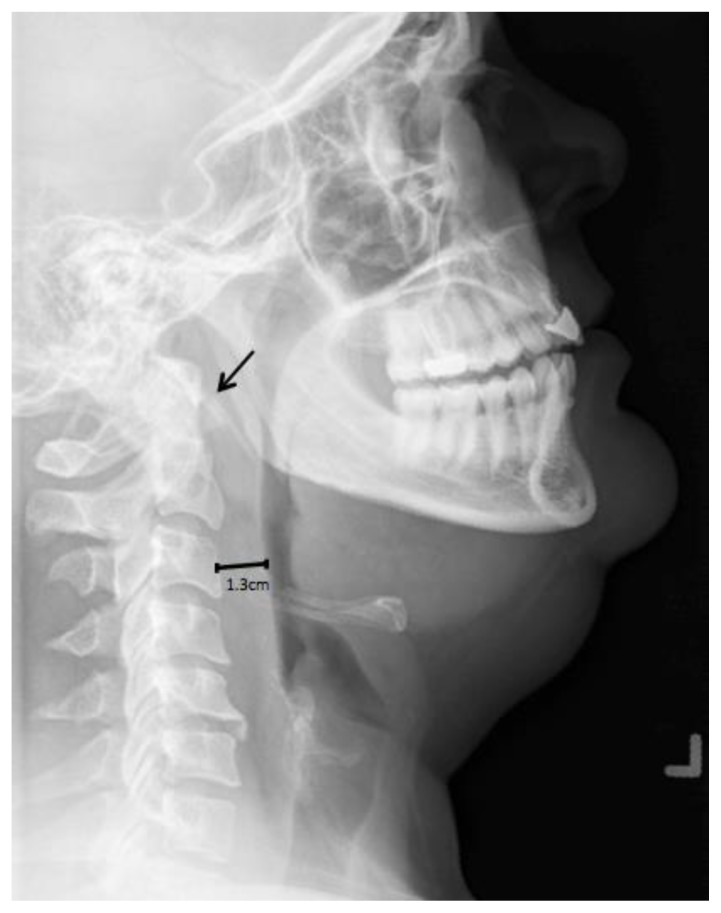
Figure 1.
41 year old woman with acute prevertebral calcific tendinitis, which was initially diagnosed as a retropharyngeal abscess. Lateral radiograph (18 mAs, 66 kV, Philips) of the nasopharynx demonstrates nonspecific prevertebral soft tissue swelling (measuring 1.3 cm at C3) and calcifications anterior to C1 and C2 (arrow).
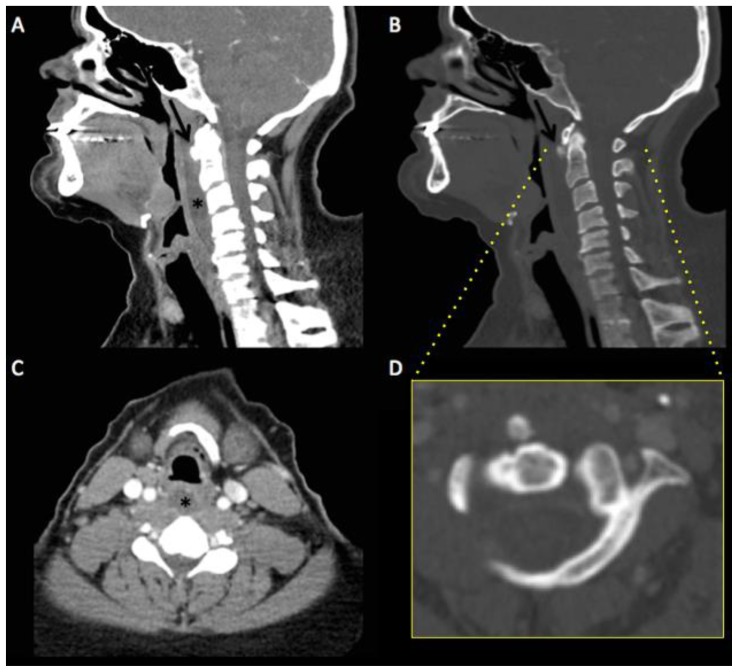
Figure 2.
41 year old woman with acute prevertebral calcific tendinitis, which was initially diagnosed as a retropharyngeal abscess. Sagittal (A, B) and axial (C, D) images in soft tissue (A, C) and bone windows (B, D) from a contrast enhanced CT of the neck in the venous phase (250 mAs, 120 kV, 0.6 mm slice thickness, 80 mL of Omnipaque contrast, Toshiba Aquilion) demonstrates calcific density in the upper oblique fibres of the longus colli muscle tendon at the level of C1–2 (arrow) as well as non-enhancing retropharyngeal edema (asterisk) measuring approximately 25 HU. The edema results in smooth expansion of the retropharyngeal space in every direction, accounting for the prevertebral thickening seen on the radiograph.
DISCUSSION
ETIOLOGY & DEMOGRAPHICS
The longus colli muscle is a bilateral paired neck flexor located in the prevertebral area consisting of upper oblique, vertical and lower oblique fibers. It originates from the transverse processes of C3–C5 and the C5–T3 vertebral bodies, while it inserts on the anterior arch of C1 and the C2–C4 vertebral bodies. Along with the longus capitis muscle, it forms the bulk of the prevertebral space. Acute prevertebral calcific tendinitis, or calcific retropharyngeal tendinitis, is a clinical syndrome that was first described in 1964 [1]. Most affected individuals are between the ages of 30 and 60 years (range of 21–65) with a ratio of two men for every three women [2, 3]. It is an uncommon condition (exact incidence is unknown) with slightly more than 70 documented cases in the English literature [2]. It is caused by calcium hydroxyapatite deposition and inflammation in the longus colli tendon and muscle, respectively. The exact pathophysiology and etiology of calcium hydroxyapatite deposition is not known. Several hypotheses, including repeated trauma and tendinous degeneration, have been proposed [2,4,5]. Oliva et al. proposed that acute or chronic tendon injury results in an abnormal healing process mediated by macrophages, osteoclasts, and erroneously differentiated tendon-derived stem cells resulting in calcific tendinopathy [5]. Subsequent aseptic inflammatory response to the calcium deposition results in reactive fluid within the retropharyngeal space [2].
CLINICAL AND IMAGING FINDINGS
The clinical presentation (acute onset neck pain, dysphagia, odynophagia, and sometimes low-grade fever [6]) is nonspecific and similar to the presentation of retropharyngeal infection. Laboratory investigations may demonstrate nonspecific signs of acute inflammation (mild leukocytosis and elevated erythrocyte sedimentation rate or c-reactive protein). Diagnostic imaging is essential to differentiate infection from calcific tendinitis (see table 2). CT findings are subtle yet can be pathognomonic. They include curvilinear calcific (non-osseous) density along the longus colli muscle, particularly in the upper oblique fibers, at the C1 to C2 level with associated soft tissue swelling. The presence of retropharyngeal edema or fluid has been less commonly reported but, when it occurs, it smoothly expands the retropharyngeal space in all directions [7]. Plain radiographs are less sensitive than CT for these calcifications and may show only nonspecific prevertebral swelling [8], with the upper limits of normal for adult prevertebral/retropharyngeal space thickness is usually 7 mm at C3 and 18 mm at C7 [9]. Magnetic resonance imaging is not usually necessary for diagnosis but can show prevertebral edema and low-signal calcifications in the longus colli muscle tendons [7]. MRI may be useful in differentiating an abscess from edema as the abscess will demonstrate restricted diffusion and often have an enhancing wall following contrast administration (in contrast to edema which will not restrict or have a rim of enhancement) [10].
Table 2.
Differential diagnosis table for acute prevertebral calcific tendinitis
| X-ray | CT | MRI | |
|---|---|---|---|
| Acute prevertebral calcific tendinitis |
|
|
|
| Median atlantoaxial degenerative change |
|
|
|
| Retropharynge al infection |
|
|
|
TREATMENT AND PROGNOSIS
The condition is self-limiting and symptomatic treatment is simple and non-invasive. NSAIDs are first line therapy. Useful adjunct therapies include corticosteroids, opioids, and immobilization [11]. Prognosis is excellent.
DIFFERENTIAL DIAGNOSES
RETROPHARYNGEAL INFECTION
Retropharyngeal infection usually occurs in children, immunocompromised patients and those who have sustained penetrating neck trauma. Its presenting symptoms are similar to acute prevertebral calcific tendinitis as described above, but may also include higher-grade fever and trismus. Key CT features that suggest retropharyngeal infection include the presence of rim-enhancement, suppurative retropharyngeal lymph nodes, asymmetric retropharyngeal edema and the absence of calcification in the longus colli muscle tendon [7].
MEDIAN ATLANTOAXIAL DEGENERATIVE CHANGE
The calcific densities at the C1 to C2 level seen on CT in acute prevertebral calcific tendinitis should not be confused with median atlantoaxial degenerative change. The main features of this entity are: osteophytes arising from the anterior arch of the atlas (either superior or inferior), odontoid apex, or median facet of the atlas; small ossicles within or adjacent to the atlantoodontoid joint; subchondral cysts; and calcification of the transverse ligament [12].
TEACHING POINT
Radiologists should be familiar with the computed tomography (CT) characteristics of acute prevertebral calcific tendinitis including curvilinear calcific (non-osseous) density along the longus colli muscle, particularly in the upper oblique fibers, at the C1 to C2 level with associated soft tissue swelling; and possible retropharyngeal edema that smoothly expands the retropharyngeal space in all directions. It is important for radiologists and otolaryngologists to differentiate between these findings and those of retropharyngeal infection, in order to institute appropriate treatment and avoid invasive therapies such as intubation and surgical drainage.
Table 1.
Summary table of acute prevertebral calcific tendinitis
| Etiology | Uncertain. Proposed hypotheses include calcium hydroxyapatite deposition from repeated trauma and tendinous degeneration |
| Incidence | Unknown, but thought to be higher than in the era previous to the advent of CT. |
| Gender ratio | 2 men : 3 women |
| Age predilection | Mean of ~42 years; age range from 21–65 |
| Risk factors | None known. |
| Treatment | Non-steroidal anti-inflammatories +/− corticosteroids, opioids, and immobilization |
| Prognosis | Excellent |
| Findings on Imaging | Curvilinear calcifications along the longus colli muscle tendon at C1–C2 with symmetric retropharyngeal edema |
ABBREVIATIONS
- CT
Computed Tomography
- NSAIDs
Non-Steroidal Anti-Inflammatory Drugs
- MRI
Magnetic Resonance Imaging
REFERENCES
- 1.Hartley J. Acute cervical pain associated with retropharyngeal calcium deposit: a case report. J Bone Joint Surg. 1964;46-A:1753–1754. [PubMed] [Google Scholar]
- 2.Park R, Halpert DE, Baer A, Kunar D, Holt PA. Retropharyngeal calcific tendinitis: case report and review of the literature. Semin Arthritis Rheum. 2009;39(6):504–509. doi: 10.1016/j.semarthrit.2009.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan MJ, Eavey RD. Calcific tendinitis of the longus colli muscle. Ann Otol Rhinol Laryngol. 1984;93:215–219. doi: 10.1177/000348948409300305. [DOI] [PubMed] [Google Scholar]
- 4.Chung T, Rebello R, Gooden EA. Retropharyngeal calcific tendinitis: case report and review of literature. Emerg Radiol. 2005;11(6):375–380. doi: 10.1007/s10140-005-0427-y. [DOI] [PubMed] [Google Scholar]
- 5.Oliva F, Via AG, Maffulli N. Physiopathology of intratendinous calcific deposition. BMC Med. 2012;10(1):95. doi: 10.1186/1741-7015-10-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Omezzine SJ, Hafsa C, Lahmar I, Driss N, Hamza H. Calcific tendinitis of the longus colli: diagnosis by CT. Joint Bone Spine. 2008;75:90–91. doi: 10.1016/j.jbspin.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Eastwood JD, Hudgins PA, Malone D. Retropharyngeal effusion in acute calcific prevertebral tendinitis: diagnosis with CT and MR imaging. AJNR Am J Neuroradiol. 1998 Oct;19(9):1789–92. [PMC free article] [PubMed] [Google Scholar]
- 8.Artenian DJ, Lipman JK, Scidmore GK, Brant-Zawadzki M. Acute neck pain due to tendinitis of the longus colli: CT and MRI findings. Neuroradiology. 1989;31:166–169. doi: 10.1007/BF00698847. [DOI] [PubMed] [Google Scholar]
- 9.Rojas CA, Vermess D, Bertozzi JC, Whitlow J, Guidi C, Martinez CR. Normal thickness and appearance of the prevertebral soft tissues on multidetector CT. AJNR. 2009;30(1):136–41. doi: 10.3174/ajnr.A1307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoang JK, Branstetter BF, Eastwood JD, Glastonbury CM. Multiplanar CT and MRI of Collections in the Retropharyngeal Space: Is it an Abscess? AJR. 2011;196:W426–432. doi: 10.2214/AJR.10.5116. [DOI] [PubMed] [Google Scholar]
- 11.Ring D, Vaccaro AR, Scuderi G, Pathria MN, Garfin SR. Acute calcific retropharyngeal tendinitis. Clinical presentation and pathological characterization. J Bone Joint Surg Am. 1994;76(11):1636–1642. doi: 10.2106/00004623-199411000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Genez BM, Willis JJ, Lowrey CE, Lauerman WC, Woodruff W, Diaz MJ, Higgs JB. CT findings of degenerative arthritis of the atlantoodontoid joint. 1990;154:315–318. doi: 10.2214/ajr.154.2.2105022. [DOI] [PubMed] [Google Scholar]