Abstract
Study Design
Sequential cross-sectional analysis.
Objective
To document vertebroplasty rates and costs.
Summary of Background Data
Little is known about interstate variation in rates or about nation-wide costs associated with the growing use of percutaneous vertebroplasty.
Methods
Using specific CPT-4 billing codes, we reviewed aggregate Medicare Part B fee-for-service claims data (cross-stratified by physician specialty and treatment setting) on thoracolumbar vertebroplasties performed from 2001–2005. Vertebroplasty rates for individual states were expressed per 100,000 Part B fee-for-service enrollees. Nation-wide facility and physician charges (combining expected contributions from all sources) allowed by Medicare for vertebroplasties and associated imaging guidance procedures were applied to observed vertebroplasty volumes. These charges (reflecting direct medical costs from an all-payer perspective) were expressed in 2005 dollars using the Producer Price Index.
Results
Vertebroplasty rates for individual states rose but varied considerably, ranging from 0.0 to 515.6/100,000 Medicare Part B fee-for-service enrollees in 2001 (median state rate = 35.4), and from 9.8 to 849.5 in 2005 (median state rate = 75.0). On average, 1.3 vertebral levels were treated per procedure, varying by treatment site and physician specialty. Fluoroscopic rather than CT guidance was used in 98.7% of cases. Total nation-wide inflation-adjusted charges rose from $76.0 million for 14,142 cases performed in 2001 to $152.3 million for 29,090 cases in 2005. While vertebroplasty was predominantly an outpatient procedure, inpatient cases generated most of the charges. Increasing volumes and costs were associated with cases performed in ambulatory surgery centers and physicians’ offices.
Conclusions
Nation-wide vertebroplasty volumes and inflation-adjusted charges doubled from 2001 to 2005 in this Medicare population. Procedure rates varied considerably by state. Almost all cases involved fluoroscopic guidance; procedures treating multiple vertebral levels were not uncommon. Procedures performed in free-standing facilities are of growing importance. Given the issues surrounding appropriate vertebroplasty use, future practice patterns and outcomes should be closely tracked.
Keywords: vertebroplasty, thoracic, lumbar, costs, rates, Medicare, health service research
INTRODUCTION
Some observational studies1 and newer randomized trial data2 suggest, that percutaneous vertebroplasty3 may be effective for treating osteoporotic vertebral compression fractures. As noted elsewhere,4 technology assessments performed abroad5–8 had generally supported vertebroplasty use, but decried the scarcity of solid comparative evidence of its effectiveness. Later US-based assessments9,10 found the available evidence to be largely inconclusive. In 2005, the Centers for Medicare & Medicaid Services (CMS)’s Coverage Advisory Committee11 reached no conclusions regarding vertebroplasty’s effectiveness and generated no national coverage decisions. Nevertheless, many state-level Medicare contractors12 and private insurers13 have covered vertebroplasty under various circumstances since at least 2001. For Medicare Part B fee-for-service (FFS) patients, we describe subsequently observed interstate variation in vertebroplasty rates, along with nationwide payer-perspective direct medical costs.
MATERIALS AND METHODS
Case Selection
Effective January 2001, thoracic and lumbar (but not cervical) vertebroplasty and associated imaging procedures were assigned unique Current Procedure Terminology-(CPT) billing codes14 (see below). Using these codes, we obtained aggregate data on vertebroplasty claims from the CMS Part B Extract and Summary System (BESS)15 for 2001–2005. (Leo Porter, Center for Medicare Management, CMS, Baltimore, MD. Personal communication, 9/05–7/06). BESS is populated from the Physician Supplier Procedure Summary Master File, which contains data for all accepted fee-for-service claims for physician care provided to Medicare enrollees of all ages. BESS does not capture denied claims, claims of Medicare Advantage (managed care) patients or Part A claims.
Data Collection
Claims for primary thoracic (CPT code 22520) and lumbar (CPT code 22521) vertebroplasties captured all accepted claims for primary thoracic or lumbar vertebroplasties. Claims for CPT code 22522 captured all additional vertebral levels treated during primary procedures. Using aggregate BESS data cross-stratified by the billing physician’s reported specialty and by the listed place of service, we classified cases by places of service, namely: inpatient hospital, other outpatient hospital settings (including the <0.5% of cases coded as Emergency Department [ED] procedures), office settings, and ambulatory surgery centers (ASCs). The remaining (<0.1%) procedures coded as having been performed in nursing homes, at home or elsewhere were categorized as outpatient hospital based procedures. We grouped physician specialties into five categories: diagnostic/interventional radiology, orthopedic surgery, neurosurgery, anesthesiology/pain management, and “other” (including neurologists, physiatrists, internists, ED physicians, physicians identified only as members of multi-specialty groups, and non-physicians).
Population-Based Procedure Rates
BESS claims identify the state or “state-equivalent” jurisdiction in which care was provided. Hereafter, the term “state” refers to 52 such jurisdictions: 49 states (since CMS enrollee data combine North and South Dakota), Washington, DC, the Commonwealth of Puerto Rico, and the Railroad Retirement Board (which processes claims for eligible enrollees regardless of state of residence). We obtained numbers of Part B fee-for-service and Medicare Advantage enrollees for each state directly from CMS. (Pamela Pope, Office of Research, Development, and Information, CMS, Baltimore, MD. Personal communication, 7/06), and calculated rates per 100,000 Part B fee-for-service enrollees.
Cost Estimation
BESS’ allowed charge data reflect Medicare-approved amounts that physicians could collect from all sources (including Medicare, supplemental insurance and patient copayments/deductibles). As this does not include amounts that hospitals or other facilities would separately receive for care of Medicare patients, we used other data to estimate this component of vertebroplasty charges. For vertebroplasties performed on Medicare patients, total Medicare-allowed charges represented total payments expected from all sources, and therefore reflected total direct medical costs from the perspective of all payers (including the patient). From this perspective, the terms “allowed charges,” “payments,” and “costs” could be used interchangeably.
Inpatient Procedures
We used allowed physician charges for primary thoracic and lumbar procedures, and for all added levels treated. CPT codes 76012 and 76013 respectively capture the fluoroscopic or computed tomography (CT) guidance associated with each level treated. However, combined fluoroscopy and CT claims volumes did not match the numbers of levels treated (see Results), and BESS data do not link imaging claims to individual vertebroplasties. Therefore, to calculate the physician component of charges for associated imaging guidance, we multiplied the yearly overall mean of allowed physician charges for vertebroplasty imaging (weighted by fluoroscopy versus CT volumes) by the total number of levels treated.
CMS directs that hospitals bill for inpatient vertebroplasties under Diagnosis Related Group (DRG) 233 or DRG 234 (Other Musculoskeletal System and Connective Tissue Operating Room Procedures, with or without Complicating Conditions, respectively). Therefore, we estimated annual inpatient hospital payments (including those for imaging) by multiplying the appropriate DRG weights by the national average operating costs (average labor + non-labor + capital amounts) from Tables 1A and 1D in the annual Hospital Inpatient Prospective Payment System Final Rule. While BESS data do not list DRGs, Medicare annually tallies twice as many discharges under DRG 233 as under DRG 234.16 Therefore, to calculate aggregate annual inpatient hospital payments, we multiplied the average payments/admission for these two DRGs (weighted 2:1 for DRG 233 versus DRG 234) by total numbers of inpatient claims.
Table 1.
Volumes and Rates of Vertebroplasty Among Medicare Part B Fee-for-Service Enrollees, 2001–2005
| YEAR | |||||
|---|---|---|---|---|---|
| 2001 | 2002 | 2003 | 2004 | 2005 | |
| Nation-wide Medicare Part B fee-for-service enrollment population | 31,912,051 | 32,946,811 | 33,662,744 | 34,077,252 | 34,243,425 |
| Nation-wide vertebroplasty procedure volume | 14,142 | 19,341 | 24,556 | 27,549 | 29,090 |
| Overall nation-wide vertebroplasty rate | 45.0 | 59.5 | 74.9 | 82.8 | 86.0 |
| Median state vertebroplasty rate | 35.4 | 53.8 | 61.9 | 74.9 | 75.0 |
| Lowest state vertebroplasty rate * | 0.0 | 0.0 | 0.2 | 1.5 | 9.8 |
| Highest state vertebroplasty rate ** | 515.6 | 719.2 | 959.5 | 841.2 | 849.5 |
Puerto Rico had the lowest rate every year.
Washington, DC had the highest rate every year.
Note: Data on annual nationwide vertebroplasty volumes and overall rates also appear in Gray et al.23
Outpatient Hospital-Based Procedures
We calculated aggregate allowable physician charges for vertebroplasty and imaging as was done for inpatient cases. We based hospital component costs on Ambulatory Payment Classification (APC) prospective payment amounts reflecting expected contributions from CMS and elsewhere. Vertebroplasty was assigned to APC 049 for 200117 and APC 050 thereafter.18 As stipulated by Medicare rules, hospital payments for additional vertebral levels were calculated at 50% of the base APC rate. Both fluoroscopy and CT guidance fall under APC 0274, with full payment allowed for each level imaged.
Office-Based Procedures
Physician payments for office-based vertebroplasties and imaging procedures incorporate any allowances provided for the facility’s costs. Therefore, BESS-allowed payment amounts listed for office-based vertebroplasties were considered the total payment amounts for the interventional procedure. Additional physician payments for imaging guidance were calculated as was done for inpatients. However, these imaging payments represented total payments (including those for imaging equipment use) allowed for outpatient imaging.
Ambulatory Surgery Center (ASC) Procedures
Per CMS policies in effect before 2007,19 we calculated costs for vertebroplasties performed in ASCs as though they occurred in office settings.
Inflation Adjustment
As the Consumer Price Index20 actually excludes Medicare costs from its calculations, we considered the producer price index to better capture inflation seen in allowed charges that would mainly be paid by Medicare. Therefore, dollar amounts for 2001–2004 were converted to 2005 dollars using producer price index ratios specifically calculated for costs of care provided to Medicare patients treated in general medical and surgical hospitals.21
Statistical Analysis
As we had no specified a priori hypotheses regarding vertebroplasty rates or costs, we performed no power calculations. As we captured 100% of applicable cases, there were no larger populations to which results might be extrapolated. Therefore, we performed no tests of statistical significance and generated no confidence intervals. Data were analyzed using Microsoft Excel.22
RESULTS
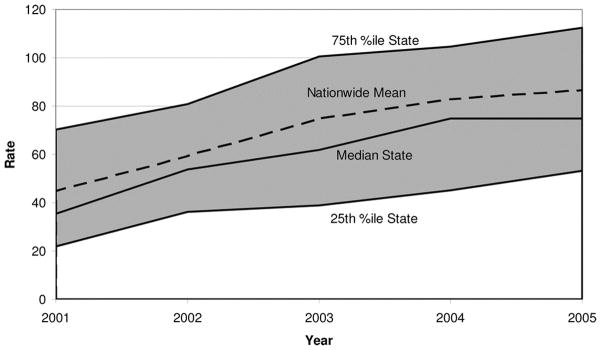
Nationwide vertebroplasty volumes and rates doubled from 2001 to 2005. However, state rates varied considerably. Puerto Rico and Washington, DC respectively had the lowest and highest rates seen each year (Table 1). Excluding these outliers, 2001 rates ranged from 3.6 per 100,000 Part B fee-for-service enrollees in New Jersey to 117.8 in Indiana. Rates from 2005 ranged from 15.2 in New York to 310.3 in Kansas. The median state varied from year to year. Interquartile ranges appear in Figure 1. In 2001, rates for 17 states were below 25.0/100,000, and only Washington, DC exceeded 149.9/100,000 (Figure 2). In 2005, only 7 states had rates below 25.0/100,000, whereas rates for 7 other states exceeded 149.9/100,000 (Figure 3).
Figure 1.
Nation-wide and State specific primary vertebroplasty rates per 100,000 Part B Fee-For-Service Enrollees
Figure 2.
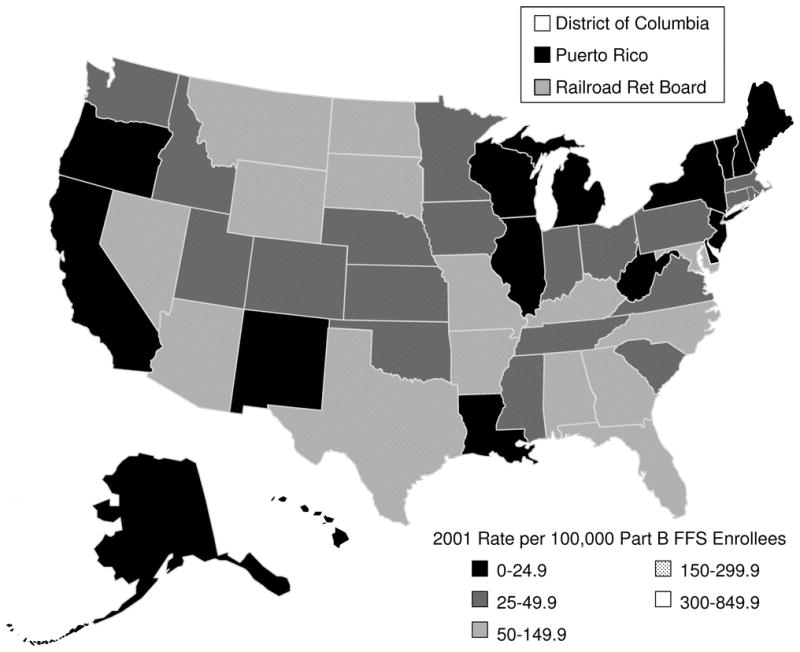
State-wide primary vertebroplasty rates per 100,000 Part B Fee-For-Service Enrollees for 2001.
Figure 3.
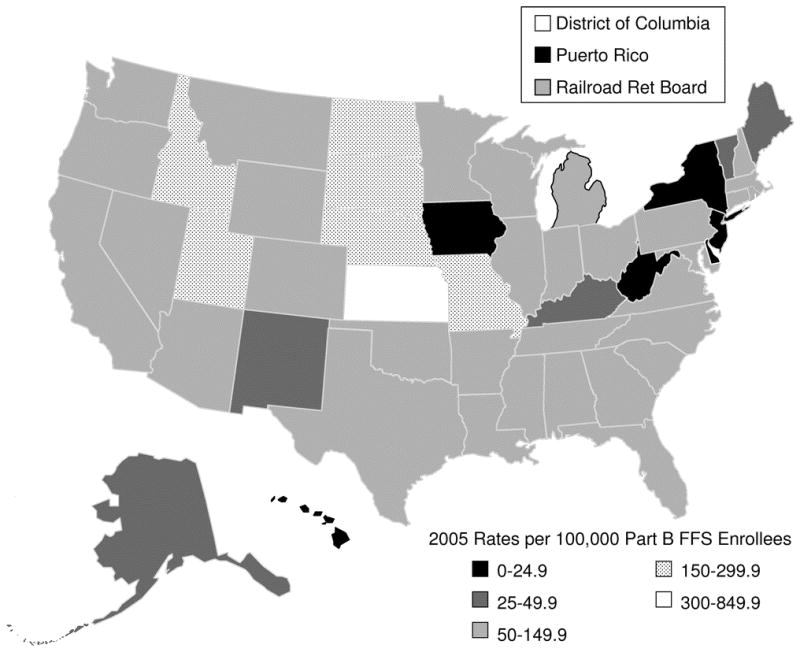
State-wide primary vertebroplasty rates per 100,000 Part B Fee-For-Service Enrollees for 2005.
When estimating vertebroplasty costs based on total numbers of vertebral levels treated, we noted that mean numbers of levels treated per procedure dropped slightly from 1.34 in 2001 to 1.24 in 2005. For all years combined, this figure ranged from 1.18 for ASC cases to 1.30 for inpatient cases. Mean numbers of levels treated varied slightly more by specialty, ranging from 1.25 for radiologists to 1.42 for orthopedic surgeons.
The 14,501 imaging claims from 2001 slightly exceeded the number of vertebroplasty encounters, 14,142 but also did not match the total of 18,911 levels treated. By 2005, numbers of imaging claims exceeded numbers of vertebral levels treated by roughly 15%. Imaging charge calculations also reflected the proportions of imaging claims for fluoroscopy relative to CT. Fluoroscopy accounted for 97.4% of imaging claims from 2001, versus 99.7% to 99.0% in subsequent years.
Although mean unadjusted for vertebroplasty rose from 2001 to 2005 (Table 2), overall mean charges remained relatively stable when expressed in inflation-adjusted dollars (bottom row of Table 2). Total inflation-adjusted costs of vertebroplasty rose from $76.0 million in 2001 to $152.3 million in 2005 (Figure 4), reflecting a doubling of procedure volumes. Charges varied considerably by treatment site. Although inpatient procedures comprised roughly 40% of procedure volumes each year (Table 2), they accounted for 77.8% of annual costs for 2001, and 71.5% in 2005 (Figure 4). As both volumes and costs per case performed in physicians’ offices and ASCs rose over time (Table 2), the proportions of total costs accounted for by cases performed in these settings also rose (Figure 4).
Table 2.
Nationwide Physician, Facility and Non-Facility Mean Payer Perspective Medical Costs ($2005) for Vertebroplasty and Imaging Guidance, 2001–2005
| Year | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2001 | 2002 | 2003 | 2004 | 2005 | ||||||
| N | Mean Cost (original $) | N | Mean Cost (original $) | N | Mean Cost (original $) | N | Mean Cost (original $) | N | Mean Cost (original $) | |
| Inpatient Procedures | 5932 | $8575 | 8466 | $8741 | 10,724 | $9049 | 11,508 | $9022 | 11,597 | $9386 |
| Hospital-based outpatient procedures | 7889 | $1805 | 10,657 | $2307 | 13,558 | $2232 | 14,979 | $2426 | 15,098 | $2478 |
| Office-based procedures | 173 | $585 | 151 | $573 | 194 | $577 | 757 | $3321 | 1884 | $2531 |
| Ambulatory surgery center procedures | 48 | $645 | 67 | $577 | 80 | $559 | 305 | $3343 | 511 | $2449 |
| All procedures | 14,142 | $4626 | 19341 | $5104 | 24,556 | $5190 | 27,549 | $5216 | 29,090 | $5235 |
| PPI Ratio | ----- | 1.16 | ---- | 1.13 | ---- | 1.07 | ---- | 1.04 | ---- | 1.00 |
| All Procedures ($2005) | 14,142 | $5371 | 19,341 | $5768 | 21,556 | $5577 | 27,549 | $5410 | 29,090 | $5235 |
Note: Data on annual vertebroplasty volumes by treatment site also appear in Gray et al23
Figure 4.
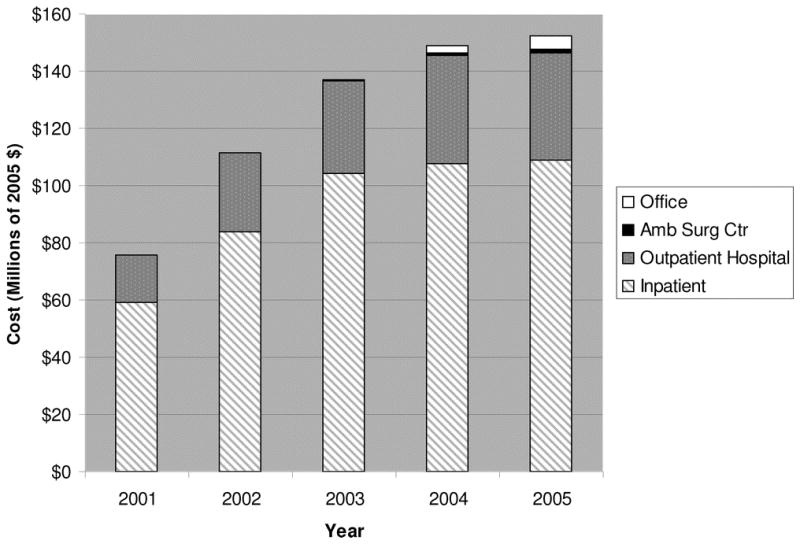
Nationwide aggregate payer-perspective costs of vertebroplasty in 2005 dollars, 2001–2005.
DISCUSSION
Our data on vertebroplasty rates extend work that we recently published23 and partly corroborate other shorter-term findings24 based on related data. Population-based vertebroplasty rate calculations required excluding patients enrolled in Part A alone from the denominator, since BESS numerator data do not include claims of such patients. The higher Medicare enrollment denominator figures for 2001–2003 used by Morrison et al24 may not have excluded such Part A enrollees. This would explain why our rates were higher, despite being based on essentially the same procedure volumes.
To our knowledge, ours is the first study to document the interstate variation seen in vertebroplasty rates. These calculations required restricting rate denominators to Part B fee-for-service enrollees, since BESS data also do not capture Medicare Advantage claims. This was especially important because the penetrance of Medicare Advantage varied considerably by state. For example, although 14.7% of US Part B enrollees were Medicare Advantage patients in 2005, percentages ranged from 0.2% in Maine to 36.9% in Rhode Island.
Significant geographic variation has been seen in rates of other musculoskeletal procedures.25 While the underlying incidence of osteoporotic fractures may vary somewhat by region, we doubt that this accounts for much of the vertebroplasty rate variation we saw. Instead, the observed variation presumably reflects some combination of local differences in factors such as clinical opinion regarding vertebroplasty, practice patterns, expressed patient demand, and financial incentives based on Medicare contractor coverage policies. FDA Public Health Notices from 2002–200426 regarding potentially serious complications associated with PMMA use in vertebroplasty and the alternative kyphoplasty approach27,28 may have had variable effects on local provider and Medicare contractor enthusiasm for vertebroplasty.
When calculating costs, we noted that mean numbers of vertebral levels treated per procedure declined slightly from 2001 to 2005 for unknown reasons. Mean numbers of vertebral levels treated per inpatient case slightly exceeded figures for all other treatment sites, presumably reflecting preferential admission of cases requiring more extensive procedures. The basis for the slightly greater variation seen across physician specialties is unclear. It is possible that surgeons see more cases with extensive osteoporosis, and/or that they are more inclined to treat multiple levels during one procedure.
Calculations of imaging costs reflected the fact that vertebroplasty generally involved fluoroscopic rather than CT guidance. As over 90% of vertebroplasties were performed in hospital-based settings, this distribution is unlikely to reflect restricted access to CT in the treatment setting. Instead, this may reflect the perceived advantages of using real-time fluoroscopy for this procedure. These calculations also adjusted for the observed discordance between numbers of imaging claims and of vertebral levels treated (See Results). Although imaging claim short-falls seen for 2001–2003 may reflect early coding issues, imaging claim volumes for 2004–2005 exceeded those of vertebral levels treated. As CT accounted for only ~1% of imaging claims, the excess is unlikely to reflect many cases where both CT and fluoroscopy were used. This more likely reflects the use of vertebroplasty imaging codes in kyphoplasty cases. Our cost calculations adjusted for this discordance by basing imaging costs on numbers of vertebral levels treated.
The increasing use of free-standing facilities we observed may reflect growing provider and patient familiarity with this approach, combined with changing financial incentives. These incentives include significant increases in Medicare-allowed charges for procedures performed in offices and, by extension, in ASCs as of 2004.29 These increases included allowance for so-called “non-facility” (i.e., non-hospital) charges for overhead and other expenses not previously permitted. These increases combined with rising procedure volumes to expand free-standing facilities’ shares of procedure costs for 2004–2005 (Table 2). It is unclear how many of these procedures were performed in free-standing imaging centers, which have no unique CMS designation.
In any case, inpatient procedures accounted for most costs, due to their much higher volumes and higher DRG-based reimbursement per case (Table 2). For patients originally admitted for other reasons, ascribing all costs incurred during the procedure admission to vertebroplasty may overestimate the provider costs actually attributable to the procedure. However, DRG-based reimbursement does represent payer costs, and does not capture entrained post discharge costs of treating any immediate complications associated with inpatient vertebroplasty. Therefore, this seemed like a reasonable approach on balance.
Limitations of this study included the potential for coding errors in administrative databases. However, we previously found a high degree of concordance between medical record data on invasive spinal procedures and administrative data from one statewide database.30 Although transitory shortfalls in Medicare’s capture of surgical cases have been identified,31 overall concordance of 90% to 98% previously seen between medical records and Medicare data on various procedures32,33 affirms the research value of such data.
As BESS data do not include patient-level information, we could not stratify data by demographic or clinical variables. We also could not link multiple procedures (e.g., imaging or additional levels treated) billed during a given encounter, identify multiple encounters for individual patients or determine whether or not increased vertebroplasty volumes were clustered among large or small numbers of providers. However, these shortcomings would not affect our ability to track procedure rates or aggregate costs. Unlike vertebroplasty’s listed CPT codes, those for other potentially related care components (e.g., anesthesia, ED care, epidural venography, inpatient management/consultation) are not unique to this procedure. The fact that we could not use BESS data to identify claims also submitted for such care provided to vertebroplasty patients makes our cost estimates more conservative.
The availability of CPT codes specific for vertebroplasty allowed us to track trends in use of this procedure alone. However, we could not capture vertebroplasties billed under older “unspecified procedure” codes, nor could we identify denied claims for vertebroplasties that were actually performed. This may also make our esti mates of vertebroplasty volumes, rates and costs conservative. However, as kyphoplasty did not receive specific CPT codes until 2006, we could not exclude kyphoplasties that had actually been billed as vertebroplasties. Differences in frequencies of these potential procedure misclassifications may have contributed to the rate variations we observed over time and across states.
Numerators for our vertebroplasty rates reflect the states in which procedures were performed, while denominators track Medicare enrollees by states of residence. Interstate migration would not affect nation-wide rates and we doubt that net migration accounts for much of the interstate rate variation we observed. However, it is possible that net in-or out-migration contributed to the very high or low rates seen in some jurisdictions.
Our data may provide limited insight regarding vertebroplasty use in patients other than Medicare Part B fee-for-service enrollees. Legally, Medicare Advantage enrollees have access to various services (e.g., vertebroplasty) equal to that of FFS enrollees. However, possible differences in health status or age distribution between Medicare Part B FFS enrollees and those with Medicare Advantage or Part A coverage alone might still limit the applicability of our rates to these groups. Our rates may also not apply to younger non-Medicare populations where vertebroplasty indications might be more likely to include neoplastic disease, for example. Finally, the absence of CPT codes for kyphoplasty precluded tracking patterns of vertebral augmentation as a whole.
The allowed payment amounts we used in our cost estimates combine payments expected from Medicare, patients, and any supplemental insurance. Although allowed payment amounts ideally approximate provider costs,34 activity-based provider costs do differ from Medicare reimbursement for some radiology procedures.35–37 In addition our figures on payments allowed rather than payments actually made reflect expected rather than observed payer-perspective costs; some calculations involved combining overlapping fiscal and calendar year costs. Our figures also do not include non-medical costs (e.g., those of travel or lost productivity) ideally incorporated in more comprehensive analyses of societal costs.38 Nevertheless, our study has several important implications. We know of no US data that would consistently capture vertebroplasties regardless of patient age, treatment setting, or payer. For example, inpatient data (.e.g., from AHRQ’s Healthcare Cost and Utilization Project or HCUP)39 on vertebroplasty are limited because its ICD-9-CM procedure code40 only became effective in October of 2004 and because this code does not distinguish among cervical, thoracic and lumbar procedures. HCUP data on outpatient surgical procedures41 are only available for select states. In addition, such data do not include office-based procedures and vary considerably in their capture of procedures performed in radiology suites or ASCs.
As Medicare Part B FFS patients should contribute significantly to vertebroplasty volumes, ours may be the most comprehensive US data currently available on this procedure. Our figures should be considered in light of estimates that up to 200,000 American women aged 50 and over suffer new clinically-evident vertebral fractures annually.42 Future demand for vertebroplasty may increase among these patients and their male counterparts, with potentially significant clinical and resource use implications. The frequency of outpatient vertebroplasty may mirror earlier trends seen in the growth of outpatient lumbar spine surgery.43 Concerns about the need for post-procedural monitoring after outpatient spinal43 procedures may be especially relevant to the growing use of free-standing facilities for performing vertebroplasty. Hopefully, our study provides useful background data for future studies that may facilitate the appropriate evidence-based diffusion of vertebroplasty
Key Points.
We reviewed aggregate Medicare Part B fee-for-service claims data on thoracolumbar vertebroplasties performed from 2001–2005.
Vertebroplasty rates in individual states grew to varying degrees, ranging from 0.0–515.6/100,000 in 2001 (median state rate=35.4), to 9.8–849.5 in 2005 (median state rate=75.0).
While vertebroplasty was predominantly an outpatient procedure, inpatient cases generated most of the charges. Increasing volumes and costs were associated with cases performed in ambulatory surgery centers and physicians’ offices.
From an all-payer perspective, inflation-adjusted nation-wide direct medical costs rose from $76 million in 2001 to $154 million in 2005.
Acknowledgments
We thank Leo Porter, formerly of CMS for providing the BESS data on which this study was based. We also thank Pamela Pope of CMS for Part B fee-for-service enrollee data. We thank Doctors William Munier, Artyom Sedrakyan and Chunliu Zhan of AHRQ and Dr Richard A Deyo, formerly of the University of Washington, for their helpful comments on prior versions of this manuscript. This work was partially supported by grants (P60 AR48093 and 5R01AR049373-04) from the National Institute for Arthritis, Musculoskeletal and Skin Diseases. Doctors Gray and Onwudiwe performed this work while employed by the US Agency for Healthcare Research and Quality (AHRQ). The views expressed herein are not necessarily those of AHRQ, CMS, or the Department of Health and Human Services.
Our study was deemed exempt from formal review by the Agency for Healthcare Research and Quality (AHRQ)’s Institutional Review Board.
Contributor Information
Darryl T. Gray, Center for Quality Improvement and Patient Safety, Agency for Healthcare Research and Quality, Rockville, MD.
William Hollingworth, Department of Social Medicine, University of Bristol, Bristol, UK.
Nneka Onwudiwe, Pharmaceutical Health Services Research, University of Maryland School of Pharmacy, Baltimore, MD; Center for Quality Improvement and Patient Safety, Agency for Healthcare Research and Quality, Rockville, MD.
Jeffrey G. Jarvik, Departments of Radiology, Neurosurgery and Health Services, University of Washington, Seattle, WA.
References
- 1.Diamond TH, Champion B, Clark WA. Management of acute osteoporotic vertebral fractures: a nonrandomized trial comparing percutaneous vertebroplasty with conservative therapy. Am J Med. 2003;114:257–65. doi: 10.1016/s0002-9343(02)01524-3. [DOI] [PubMed] [Google Scholar]
- 2.Voormolen MH, Mali WP, Lohle PN, et al. Percutaneous vertebroplasty compared with optimal pain medication treatment: short-term clinical outcome of patients with subacute or chronic painful osteoporotic vertebral compression fractures. The VERTOS study. AJNR Am J Neuroradiol. 2007;28:555–60. [PMC free article] [PubMed] [Google Scholar]
- 3.Galibert P, Deramond H, Rosat P, Le Gars Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neuro chirurgie. 1987;33:166–8. In French; abstract in English. [PubMed] [Google Scholar]
- 4.Hollingworth W, Jarvik J. Evidence on the effectiveness and cost-effectiveness of vertebroplasty: a review of policy makers’ responses. Acad Radiol. 2006;13:550–5. doi: 10.1016/j.acra.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Muggli EE. The safety and efficacy of percutaneous vertebroplasty in symptomatic osteoporotic vertebral compression fractures. Clayton, Australia: Center for Clinical Effectiveness; 2002. [Accessed 9/27/2006]. p. 24. [web site] Available at: http://areastematicas.com/www/areatematicadme/contenidos/3/Osteoporosis/809.pdf. [Google Scholar]
- 6.Fisher A. Percutaneous vertebroplasty: A Bon Cement Procedure for spinal pain relief. Ottawa, Canada: the Canadian Coordinating Office for Health Technology Assessment (CCOHTA), 2002. Issues Emerg Health Technol. 2002;31:1–4. [PubMed] [Google Scholar]
- 7.National Institute for Clinical Excellence (NICE) Interventional procedure guidance 12. London, UK: NICE; 2003. Nov, [Accessed 1/6/2005]. Percutaneous vertebroplasty. [web site] Available at: http://www.nice.org.uk/page.aspx?o85733. [Google Scholar]
- 8.Sundhedsstyrelsen. Medicinsk Teknologivurdering 2004. 2. Vol. 6. Copenhagen, Denmark: Center for Evaluering og Medicinsk Teknologivurdering; 2004. [Accessed 9/27/2006]. Perkutan vertebroplastik: En medicinsk teknologivurdering. Smertebehandling af osteoporotiske knoglebrud i ryghvirvler. In Danish; Executive Summary in English. [web site] Available at: http://www.sst.dk/publ/Publ2004/perkutan_vertebroplastik.pdf. [Google Scholar]
- 9.Institute for Clinical Systems Improvement. Technology Assessment Report. Bloomington, MN: Institute for Clinical Systems Improvement; 2003. [Accessed 9/27/2006]. Vertebroplasty and Balloon-Assisted Vertebroplasty for the Treatment of Osteoporotic Compression Fractures. [web site] Available at: http://ww.icsi.org/knowledge/detail.asp?catID=107&itemID=1355. [Google Scholar]
- 10.Blue Cross and Blue Shield Association Technology Evaluation Center. Percutaneous Vertebroplasty for Vertebral Fractures Caused by Osteoporosis or Malignancy. Blue Cross and Blue Shield Association Technology Evaluation Center; Chicago, IL: Aug, 2005. [Accessed 10/10/2005]. [web site] Available at: http://www.bcbs.com/tec/vol20/20_06.html. [Google Scholar]
- 11.Medicare Coverage Advisory Committee (MCAC) Meeting. Treatments for Vertebral Body Compression Fractures. Centers for Medicare & Medicaid Services; Baltimore MD: May 24, 2005. [Accessed 10/6/05]. [web site] Available at: http://www.cms.hhs.gov/mcd/viewmcac.asp?whereindex&mid=29. [Google Scholar]
- 12.Empire Medicare Services (Medicare Part A Contractor for New York, CT, DE, MA; Part B Contractor for New Jersey and New York) [Accessed 9/13/2006];Medicare News Update MEDICARE Local Medical Review Policy Percutaneous Vertebroplasty Issue 2001–8. 2001 Aug; [web site] Available at: http://www.empiremedicare.com/newsupda/2001-08/vertebroplasty.htm.
- 13.Blue Cross and Blue Shield of North Carolina. [Accessed 11/7/07];Corporate Medical Policy: Vertebroplasty and Kyphoplasty Percutaneous. [web site] Available at: http://www.bcbsnc.com/services/medical-policy/pdf/vertebroplasty_and_kyphoplasty_percutaneous.pdf.
- 14.CPT® (Current Procedural Terminology) American Medical Association; Chicago, IL: [Accessed 9/1/2005]. [web site] Available at: http://www.ama-assn.org/ama/pub/category/3113.html. [Google Scholar]
- 15.Part B Extract and Summary System (BESS) Centers for Medicare & Medicaid Services; Baltimore MD: [Accessed 8/30/06]. [web site] Available at: http://www.cms.hhs.gov/NonIdentifiableDataFiles/03_PartBExtractSummarySystem.asp#TopOfPage. [Google Scholar]
- 16.Centers for Medicare & Medicaid Services. Baltimore MD. [Accessed 4/30/2007];MEDICARE PROSPECTIVE PAYMENT SYSTEM SELECTED PERCENTILE LENGTHS OF STAY FY2005 MEDPAR UPDATE 12/05 GROUPER V24.0. [web site] Available at http://www.cms.hhs.gov/AcuteInpatientPPS/FFD/itemdetail.asp?filterType_none&filterByDID__99&sortByDID_2&sortOrder_ascending&itemID_CMS061851.
- 17.Centers for Medicare & Medicaid Services. Baltimore MD. [Accessed 9/1/2006];PR001A. Update of Calendar Year 2001 Hospital Outpatient Payment Rates and Coinsurance Amounts. 2001 May 4; [web site] Available at: http://www.cms.hhs.gov/HospitalOutpatientPPS/HORD/itemdetail.asp?filterType=none&filterByDID=99&sortByDID=3&sortOrder=descending&itemID=CMS048313.
- 18.Centers for Medicare & Medicaid Services. Baltimore MD. [Accessed 4/21/2007];PR001A. Update of Calendar Year 2001 Hospital Outpatient Payment Rates and Coinsurance Amounts. 2001 May 4; [web site] Available at: http://www.cms.hhs.gov/HospitalOutpatientPPS/AU/itemdetail.asp?filterType=none&filterByDID==99&sortByDID=1&sortOrder=descending&itemID=CMS061134.
- 19.Centers for Medicare & Medicaid Services. Baltimore MD. [Accessed 9/1/2006];Medicare Program Memorandum. 2001 Jul 18; [web site] Available at:. http://www.cms.hhs.gov/manuals.
- 20.US Department of Labor Bureau of Labor Statistics. Archived Consumer Price Index Detailed Report Tables. US Department of Labor Bureau of Labor Statistics; Washington, DC: 2005. [Accessed 9/30/2005]. [web site] Available at: http://www.bls.gov/cpi/cpi_dr.htm#2001. [Google Scholar]
- 21.US Department of Labor Bureau of Labor Statistics. Producer Price Index Industry Data. US Department of Labor Bureau of Labor Statistics; Washington, DC: [Accessed 9/1/2006]. [web site] Available at: http://data.bls.gov/cgi-bin/dsrv?pc. [Google Scholar]
- 22.Microsoft Excel [computer program]. Version 10.4302.4219 for PC. Redmond, WA: Microsoft Corp; 2002. [Google Scholar]
- 23.Gray DT, Hollingworth W, Onwudiwe N, et al. Thoracic and lumbar vertebroplasties performed in US Medicare enrollees, 2001–2005. JAMA. 2007;298:1760–1762. doi: 10.1001/jama.298.15.1760-b. [DOI] [PubMed] [Google Scholar]
- 24.Morrison WB, Parker L, Frangos AJ, et al. Vertebroplasty in the United States: guidance method and provider distribution, 2001–2003. Radiology. 2007;243:166–70. doi: 10.1148/radiol.2431060045. [DOI] [PubMed] [Google Scholar]
- 25.Weinstein JN, Bronner KK, Morgan TS, et al. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood) 2004;(Suppl Web Exclusives):VAR81–9. doi: 10.1377/hlthaff.var.81. [DOI] [PubMed] [Google Scholar]
- 26.Center for Devices and Radiological Health. US Food and Drug Administration, Rockville, MD. [Accessed 9/12/2006];FDA Public Health Web Notification: Complications Related to the Use of Bone Cement and Bone Void Fillers in Treating Compression Fractures of the Spine. Updated: May 7, 2004. [web site] Available at: http://www.fda.gov/cdrh/safety/bonecement.html.
- 27.Deen HG, Aranda-Michel J, Reimer R, et al. Balloon kyphoplasty for vertebral compression fractures in solid organ transplant recipients: results of treatment and comparison with primary osteoporotic vertebral compression fractures. Spine. 2006;6:494–9. doi: 10.1016/j.spinee.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 28.Hulme PA, Krebs J, Ferguson SJ, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine. 2006;31:1983–2001. doi: 10.1097/01.brs.0000229254.89952.6b. [DOI] [PubMed] [Google Scholar]
- 29.Centers for Medicare & Medicaid Services (CMS), HHS. Medicare Program; Changes to Medicare Payment for Drugs and Physician Fee Schedule Payments for Calendar Year 2004. Addendum B. Relative Value Units (RVUS) and Related Information. [Accessed 4/23/2007];Federal Register. 2004 Jan 7;69(4):1127, 1203. [web site] Available at: http://www.gpoaccess.gov/fr/advanced.html. [PubMed] [Google Scholar]
- 30.Cherkin DC, Deyo RA. Nonsurgical hospitalization for low back pain is it necessary? Spine. 1993;18:1728–35. doi: 10.1097/00007632-199310000-00003. [DOI] [PubMed] [Google Scholar]
- 31.Gray DT, Hodge DO, Ilstrup DM, et al. The concordance between clinical and Medicare data on population-based cataract surgery utilization in Olmsted County, MN. Am J Epidemiol. 1997;145:1123–26. doi: 10.1093/oxfordjournals.aje.a009075. [DOI] [PubMed] [Google Scholar]
- 32.Javitt JC, McBean AM, Sastry SS, et al. Accuracy of coding in Medicare Part B claims: cataract as a case study. Arch Ophthalmol. 1993;111:605–7. doi: 10.1001/archopht.1993.01090050039024. [DOI] [PubMed] [Google Scholar]
- 33.Du X, Freeman JL, Warren JL, et al. Accuracy and completeness of Medicare claims data for surgical treatment of breast cancer. Med Care. 2000;38:719–27. doi: 10.1097/00005650-200007000-00004. [DOI] [PubMed] [Google Scholar]
- 34.Medicare Payment Advisory Commission. Report to the Congress: Medicare Payment Policy. Washington, DC: Medicare Payment Advisory Commission; 1999. [Google Scholar]
- 35.Saini S, Seltzer SE, Bramson RT, et al. Technical cost of radiologic examinations: analysis across imaging modalities. Radiology. 2000;216:269–72. doi: 10.1148/radiology.216.1.r00jl18269. [DOI] [PubMed] [Google Scholar]
- 36.Nisenbaum HL, Birnbaum BA, Myers MM, et al. The costs of CT procedures in an academic radiology department determined by an activity based costing (ABC) method. J Comput Assist Tomogr. 2000;24:813–23. doi: 10.1097/00004728-200009000-00026. [DOI] [PubMed] [Google Scholar]
- 37.Gray DT, Hollingworth W, Blackmore CC, et al. Conventional radiography, rapid magnetic resonance and conventional magnetic resonance imaging for low back pain: activity-based costs and reimbursement. Radiology. 2003;227:669– 80. doi: 10.1148/radiol.2273012213. [DOI] [PubMed] [Google Scholar]
- 38.Russell LB, Gold MR, Siegel JE, et al. The role of cost-effectiveness analysis in health and medicine. Panel on Cost-Effectiveness in Health and Medicine. JAMA. 1996;276:1172–7. [PubMed] [Google Scholar]
- 39.HCUP Databases. Healthcare Cost and Utilization Project (HCUP); Agency for Healthcare Research and Quality; Rockville, MD: Dec, 2004. [Accessed 10/10/2006]. [web site] Available at: http://www.hcup-us.ahrq.gov/sidoverview.jsp. [PubMed] [Google Scholar]
- 40.ICD-9-CM. Centers for Medicare & Medicaid Services; Baltimore MD: [Accessed 10/6/2005]. [web site] Available at: http://cms.hhs.gov/paymentsystems/icd9. [Google Scholar]
- 41.HCUP Databases. Healthcare Cost and Utilization Project (HCUP); Agency for Healthcare Research and Quality; Rockville, MD: Dec, 2004. [Accessed 10/10/2006]. [web site] Available at: http://www.hcup-us.ahrq.gov/sasdoverview.jsp. [PubMed] [Google Scholar]
- 42.Melton LJ, III, Kallmes DF. Epidemiology of vertebral fractures: implications for vertebral augmentation. Acad Radiol. 2006;13:538– 45. doi: 10.1016/j.acra.2006.01.005. [DOI] [PubMed] [Google Scholar]
- 43.Gray DT, Deyo RA, Kreuter W, et al. Population based trends in volumes and rates of ambulatory lumbar spine surgery. Spine. 2006;31:1957–63. doi: 10.1097/01.brs.0000229148.63418.c1. [DOI] [PubMed] [Google Scholar]
- 44.Katz JN. Commentary on: “Gray DT, Deyo RA, Kreuter W, Mirza SK, Heagerty PJ, Comstock BA, Chan L. Population-based trends in volumes and rates of ambulatory lumbar spine surgery”. Spine. 2006;31:1964. doi: 10.1097/01.brs.0000229148.63418.c1. [DOI] [PubMed] [Google Scholar]