Abstract
A self-contained, self-fitting hearing aid (SFHA) is a device that enables the user to perform both threshold measurements leading to a prescribed hearing aid setting and fine-tuning, without the need for audiological support or access to other equipment. The SFHA has been proposed as a potential solution to address unmet hearing health care in developing countries and remote locations in the developed world and is considered a means to lower cost and increase uptake of hearing aids in developed countries. This article reviews the status of the SFHA and the evidence for its feasibility and challenges and predicts where it is heading. Devices that can be considered partly or fully self-fitting without audiological support were identified in the direct-to-consumer market. None of these devices are considered self-contained as they require access to other hardware such as a proprietary interface, computer, smartphone, or tablet for manipulation. While there is evidence that self-administered fitting processes can provide valid and reliable results, their success relies on user-friendly device designs and interfaces and easy-to-interpret instructions. Until these issues have been sufficiently addressed, optional assistance with the self-fitting process and on-going use of SFHAs is recommended. Affordability and a sustainable delivery system remain additional challenges for the SFHA in developing countries. Future predictions include a growth in self-fitting products, with most future SFHAs consisting of earpieces that connect wirelessly with a smartphone and providers offering assistance through a telehealth infrastructure, and the integration of SFHAs into the traditional hearing health-care model.
Keywords: hearing aid, self-fitting, amplification, hearing health care, hearing apps, teleaudiology
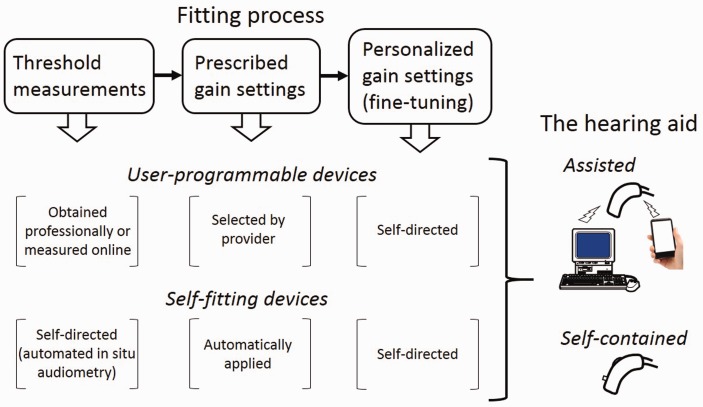
Five years ago, we introduced the concept of a self-contained self-fitting hearing aid (SFHA), where self-contained implies that the hearing aids can be adjusted without requiring access to other hardware and connection to the Internet, and self-fitting implies that the fitting process (i.e., obtaining the initial hearing aid setting from threshold data) is managed by the user without assistance from a hearing health professional (Figure 1). The concept was based on a behind-the-ear (BTE) style hearing aid that was equipped with an on-board tone-generator, fitting algorithm, and training algorithm, and that could be connected to an instant-fit ear tip (Convery, Keidser, Dillon, & Hartley, 2011a). Using on-board controls, the tone generator can be activated to run an automated in-situ hearing threshold test. The resulting thresholds are then used as input to the fitting algorithm that determines the initial, prescribed settings of the hearing aid. The training algorithm enables the user to fine-tune the hearing aid over time (Dillon et al., 2006; Zakis, Dillon, & McDermott, 2007), if the prescribed setting is not satisfactory. We suggested that such a hearing aid might be a viable solution to address a large unmet demand for hearing care in developing countries and underserved areas in developed countries where resources are sparse. Although there were then commercial hearing aids available that could be purchased without visiting a hearing health-care professional and that could be fine-tuned by the user, we argued that none of these aids met the criteria for a SFHA as professionally measured audiometric data had to be supplied prior to purchase of the hearing aid. Furthermore, none of these alternatives could be managed by the user without accessing other equipment, meaning that they were not self-contained hearing aids either. Both these factors would make them less suitable for developing countries.
Figure 1.
An overview of the processes associated with fitting a hearing aid, and how each process is achieved in devices classified as “user-programmable” and “self-fitting.” The processes can be managed either from an Software application (“assisted” devices) or via on-board buttons (“self-contained” devices). Currently, all commercial products are assisted devices.
In Convery et al. (2011a), we further discussed what we considered were the potential advantages and limitations of a SFHA. Lower cost achieved by avoiding the need for professional assistance, and increased psychological ownership resulting from the time and effort invested in the self-fitting process were listed as the major potential benefits of the device. In other health areas, active participation in the treatment of chronic conditions has been found to lead to improved adherence and better outcomes (Kralik, Koch, Price, & Howard, 2004; Lawn et al., 2007; Meng, Friedberg, & Castora-Binkley, 2014; Richardson et al., 2013). The suggested disadvantages of the SFHA included the failure to identify pathologies, such as impacted wax, active infection, and otalgia, that are contraindicative to hearing aid fitting, and the risk of the user not adhering to the self-fitting protocol resulting in inappropriate gain-frequency responses and output levels that could lead to reduced speech discrimination due to upward spread of masking, and temporary or permanent threshold shift, respectively. We also acknowledged that in order for our concept of a self-contained SFHA to be successful in developing countries, some support system needs to be in place that as a minimum serves as supplier of renewable ear tips and batteries and provide simple repairs.
A preliminary feasibility study was also presented at this time. This study looked at how well the self-fitting concept was perceived and how one small step, such as selecting appropriately sized tubing and ear tips and connecting them together, and attaching them to a hearing aid body, could be managed by 80 hearing-impaired people in one developed country (Convery, Keidser, & Hartley, 2011b; Convery et al., 2011c). The study suggested that people were generally positive toward the concept, and volunteered similar potential advantages and disadvantages of the device to those identified by the researchers. Specifically, the ability to self-manage was the most frequently suggested advantage (36% of participants), while not having professional guidance and fearing an inferior fitting result were the most frequently suggested disadvantages (26% and 19% of participants, respectively). Despite the positive reaction, not all participants (40%) felt the concept would be of personal benefit, and many, as indicated earlier, would prefer to see a professional. The study also demonstrated that it was possible to guide hearing aid users through the task of selecting and connecting hearing aid components by help of a set of written illustrated instructions, although less than 40% completed the task accurately against strict audiological criteria. In most cases, however, the mistakes made did not severely compromise the ability to continue the self-fitting process. This preliminary data encouraged us to continue our investigations into the feasibility of a SFHA.
Five years on, we take stock of the development of commercial self-fitting, including self-contained self-fitting, devices, review what we now know about a lay person’s ability to manage a SFHA, present our current view on the feasibility and challenges of the device and discuss its potential future in developed and developing countries.
Commercial Self-Fitting Devices and Self-Managing Alternatives
A key feature of the SFHA is that the process of fitting and fine tuning is managed entirely by the user (Figure 1), which makes the device particularly suitable for direct-to-consumer device sale and for distribution in areas with a limited audiological infrastructure, such as developing countries. In 2011, we identified four companies (America Hears, Australia Hears, DIY Hearing Aids, and HearSource) that offered hearing aids online that could be considered partly self-fitting; that is, they were pre-programmed by the providers but were user-programmable (Figure 1) by help of a computer program if the user purchased a proprietary programming interface and cables to connect the hearing aids to a computer. The pre-programming of these devices was based on a user-supplied audiogram, which in the United States had to be obtained professionally and within the past 6 months to comply with Food and Drug Administration (FDA) requirements. Clients of Australia Hears could also obtain a hearing aid without a previous audiogram, in which case they were required to obtain the associated fitting software and make adjustments from a non-prescribed baseline response. The hearing aids are described in more details in Convery et al. (2011a).
A new search in 2015 revealed three new developments, including the introduction of the following: (a) self-administered hearing tests, either provided online or embedded in the hearing device, used to pre-program the devices; (b) applications (apps) for tablets or smartphones to drive the user-adjustments; and (c) hearing apps that can be downloaded to tablets and smartphones to turn these devices into a hearing-assisting device. The first development means that fully self-fitting devices are now available. An overview of some of the devices that enable the user to self-manage the fine-tuning process (user-programmable devices) or the entire fitting and fine-tuning process (self-fitting devices) are shown in Tables 1 and 2, respectively. Among these products, some are categorized as Personal Sound Amplification Products (PSAPs); that is, they are devices that do not have regulatory approval to be marketed as a hearing aid in the United States, although they can offer sophisticated signal processing similar to that found in approved hearing aids. None of the products listed in Table 2 meet our vision of a self-contained, self-fitting device as they require access to additional hardware or a smartphone.
Table 1.
Examples of User-Programmable Devices That Are Currently Available on the Direct-to-Consumer Market.
| Company | Website (http://) | Device styles | Price per device, or app | User requirements |
|
|---|---|---|---|---|---|
| Hearing test | Fine-tuning | ||||
| HearSource | www.hearsource.com | BTE, RIC | US$995 | Professional audiogram | App for Windows, USB programmer and cables |
| America Hears | www.americahears.com | BTE, RIC, ITE | US$699–1499a | Professional audiogram | App for Windows, USB programmer and cables |
| Blamey Saunders Hears | www.blameysaunders.com.au | BTE, RIC | US$1050-1650 | Online speech-based test or professional audiogram | App for Windows, Android, or iOS, Bluetooth enabled programmer |
| SoundHawk | www.soundhawk.com/ | Bluetooth like earpieces | US$350 | Not applicable | App for Android or iOS |
Note. Prices are correct as of December 2015. BTE = behind-the-ear; RIC = receiver-in-canal; ITE = in-the-ear; app = application; OS = operating system.
Price not disclosed for all devices.
Table 2.
Examples of Self-Fitting Devices That Are Currently Available on the Direct-to-Consumer Market.
| Company | Website (http://) | Device styles | Price per device, or app | User requirements |
|
|---|---|---|---|---|---|
| Hearing test | Fine-tuning | ||||
| SoundWorld Solutions | www.soundworldsolutions.com | Bluetooth like earpieces, RIC | US$349–449 | App for Windows, Mac OS, Android, or iOS | App for Windows, Mac OS, Android, or iOS |
| iHear Medical | www.ihearmedical.com | Earbuds | From US$199 | App for Windows, or Mac OS, USB programmer and cables | App for Windows, or Mac OS, USB programmer and cables |
| Audientes | www.audientes.com | Processing unit + earbuds | Not available | The processing unit | The processing unit |
Note. Prices are correct as of December 2015. RIC = receiver-in-canal; app = application; OS = operating system.
User-Programmable Devices
Of the companies listed in Table 1 that offer user-programmable hearing aids, three were also in operation in 2011: America Hears, Blamey Saunders Hears (previously Australia Hears), and HearSource. As in 2011, these companies offer customers hearing aids that are pre-programmed by the providers from a user-supplied audiogram, along with an interface and programming cables to enable fine-tuning of the devices via a computer program. Blamey Saunders Hears now additionally invites their clients to do a proprietary hearing test (Blamey, 2012) online, the result of which can be used to pre-program the hearing aids. Furthermore, the application from Blamey Saunders Hears that enables clients to fine-tune their hearing aid is now available to be downloaded on tablets and smartphones too. An interface and cables still need to be purchased separately to access this feature. In 2011, only HearSource offered coaching with the fine-tuning process. Today, all three companies offer remote programming support. This development is interesting, as it seems incompatible with the self-fitting concept, and we will further discuss this later in the article.
A new device in this category is the SoundHawk, which is a PSAP that looks like a Bluetooth earpiece. Instead of requiring a proprietary interface to access manipulation options, this product links wirelessly via Bluetooth to a smartphone or tablet, as well as to an accompanying microphone that can be worn by a conversational partner. The device, which offers directionality and noise cancelling technology, comes with four pre-set programs for listening in various environments. Each program can be personalized from an accompanying app by running a finger over a two-dimensional space on the screen to achieve a “brighter and fuller audio.” The ear pieces and handheld microphone runs on batteries that are rechargeable via an accompanying charging case with a micro-USB port. Due to the integrated Bluetooth technology, the product is ready for use with Bluetooth enabled phones.
Self-Fitting Devices
Among the first self-fitting products are the Bluetooth-headset-look-alike PSAPs launched in 2013 by SoundWorld Solutions, see Table 2. The products include a rechargeable battery and Bluetooth technology that enables the user to pair their device with a computer, tablet, or smartphone to access a free app. The app provides access to a self-administered pure-tone test, used to automatically pre-program the device, and an equalizer for further fine-tuning. The devices, which offer the main features of conventional hearing aids, such as multi-channel wide dynamic range compression (WDRC), directional microphones, noise suppression, and feedback cancellation, also give the user access to three separate programs that can be independently fine-tuned for different environments. If the user does not have the technology that provides access to the app, one of three pre-programmed settings can be selected through an on-board push-button. More recently, SoundWorld Solutions has added an FDA-approved receiver-in-the-canal BTE hearing aid to their range of products that offer the same features as their PSAPs but has the advantage of being better suited for bilateral fittings and usage. This is probably the world’s first SFHA. SoundWorld Solutions products can be used with Bluetooth enabled phones and can stream audio signals from other Bluetooth enabling devices. A potential downside of this asset is the need for a large battery that results in their BTE being twice the size of conventional small BTEs.
Other current self-fitting products in Table 2 include a PSAP from iHear Medical that enables pre-programming from an FDA-approved self-administered hearing test, and fine-tuning from a computer program via a proprietary interface and programming cables. It provides four-channel WDRC, ambient noise suppression, and adaptive feedback cancellation. The device is an in-the-ear (ITE) style device that looks like an earbud and is only suitable for people with milder hearing loss.
In this category, it is also worth noting Self-fit from 2Pi GmbH, which is an app for hearing aid fitting that enables a screening of hearing loss, the result of which leads to an initial gain-frequency response setting, and interactive fine-tuning of gain. While the company also produces and sells signal processing algorithms for hearing aids, it does not deliver the chip and associated hardware. A hearing aid supported by the Self-fit app would be a SFHA. At the time of writing, this app is the only product that to our knowledge is undergoing clinical evaluation.
Emerging Self-Contained SFHAs
None of the earlier mentioned devices classify as a self-contained SFHA as manipulations require access to other hardware. Audientes (see Table 2) is advertising a device that consists of a sound processing unit which is wired to a set of earbuds. The unit uses a battery that can be recharged via a microUSB. From the sound processing unit, a self-administered hearing test is initiated that leads to the initial settings of the device. There are currently no details on the hearing test or the signal processing capabilities of the device. Furthermore, it is not clear if the user will be able to further fine-tune the device. If fine-tuning by the user from the signal processing unit will be a feature of this device, it could become the first self-contained self-fitting product, albeit in the form of a body worn device. The device is expected to be for sale from September 2016.
Hearing Applications
A relatively new low-cost and self-manageable alternative offered to hearing-impaired people is an app that turns a smartphone or tablet into an assistive hearing device. In 2012, there were a couple of hearing enhancement apps to choose from (Galster, 2012). Today, there are numerous apps available that may provide a boost of volume, simple gain-frequency shaping, or fitting with a sophisticated sound processing algorithm according to the individual hearing loss; all followed by user-controlled fine-tuning. Generally, the apps apply a pre-set or user-manipulated amplification characteristic to the sound picked up by the external microphone of the phones or tablets, delivering the processed sound to the user’s ears through the chosen headset. For optimum sound quality, it is recommended to use earbuds, or other headsets that fit tightly in or around the ear, and to mute any microphone on the headset. Essentially, the phone or tablet is turned into a monophonic body worn sound processing device, which acoustically is a large step backwards for hearing-impaired people. However, including the cost of the phone or tablet, this alternative is cheaper than any of the user-programmable devices listed in Tables 1 and 2, and they do have the advantage of not requiring frequent replacement of batteries. It is impossible to review all the available apps here. A handful is listed in Table 3 that are somewhat arbitrarily chosen to show the variety. It should be noted that unless the app allows for independent adjustment of gain for left and right ears or provides non-linear amplification to boost softer sounds relative to louder sounds, these apps provide no advantage over the device’s external volume control to the user when streaming audio.
Table 3.
Examples of Assistive Hearing Applications.
| Company | Website (http://) | Price per device, or app | User requirements |
|
|---|---|---|---|---|
| Hearing test | Fine-tuning | |||
| Petralex | Petralex.pro | Free | Android or iOS | External VC |
| BioAid | bioaid.org.uk | Free | Not applicable | iOS |
| EarMachine | www.earmachine.com/ | Free | Not applicable | iOS |
| HearingAid | tiau.de/TiAu_Engineering_UG_(Haftungsbeschrankt)/Apps.html | US$1.99 | Not applicable | Not applicable |
| HearingCorrector or HearingHelp | www.ind-technik.eu/ software/hearinghelp/index.php | US$9.99 | Manual entry | iOS |
| Enhanced Ear Hearing Aid | www.bxtel.com/enhanced. html | US$6.99 | iOS | ? |
Note. Prices are correct as of December 2015. OS = operating system; VC = volume control.
Petralex by IT ForYou, EarMachine by Ear Machine LLC, and BioAid by Nicholas Clark are all free apps. Petralex enables the user to create customized programs for different listening environments. This is done through a self-administered hearing test that is taken in the environment for which the program is intended to be used. During the test, the user is presented with pure tones that slowly rise in volume until the user presses a button to indicate that the tone has just become audible (reaction time will affect the result here). After the creation of each program further fine-tuning of the response shape is not possible but overall gain can be changed by a volume control. EarMachine and BioAid are designed by hearing scientists from the United States and England, respectively. None of the apps require an audiogram to be entered or a hearing test to be taken. By entering a simple profile, including age, gender, and perceived hearing status, the EarMachine will suggest a suitable amplification setting based also on the listening environment picked up by the microphone. The selected setting can be personalized by the user through loudness and “fine-tuning” adjustments. BioAid is promoted as a research tool and the developers encourage users to try out a range of pre-programmed settings called “flat boost,” “gradual HF boost,” “sharp HF boost,” “1-kHz boost,” “2-kHz boost,” and “1- and 2-kHz boost,” designed for common types of hearing impairment, and to select the one that seems best suited to the user. For each pre-programmed filter shape, the user can choose between one of four settings of overall gain and compression strength. The various processing schemes are claimed to be based on the current “understanding of the biology of hearing.” The user can subsequently manipulate volume and select the rejection level of background noise.
For less than US$10.00, the interested can, for example, try out Hearing Aid by TiAu Engineering UK, an app that is designed to boost hearing during conversations by reducing ambient noise by “filtering out the frequencies outside of the human voice range”; Hearing help by IND (Ingenieurbüro für Nachrichten-und Datentechnik), which requires the user to first enter an audiogram before providing an equalizer for fine-tuning of the response shape; and Enhanced Ears Hearing Aid by Bxtel, that guides the user through a hearing test, the data of which are used to create a customized amplification for the user’s specific hearing loss. It is not clear if the user is able to subsequently fine-tune the response, but two different sets of gain-frequency response can be stored on one device.
While the range of user-programmable and self-fitted devices available through direct sales is growing in developed countries and meeting the expectation of reduced cost, there is yet limited data available about their clinical validity; that is, on how outcomes with these devices and hearing apps compare to outcomes achieved with professionally fitted devices. Performance and satisfaction were compared between two smartphone hearing apps and a bare-bones (advanced features were deactivated) hearing aid in 18 hearing-impaired people (Amlani, Taylor, Levy, & Robbins, 2013). Aided performance on a speech-in-noise test and rated sound quality related to clarity, own voice, naturalness, and localization, were similar across devices. According to the International Outcome Inventory for Hearing Aids, test participants reported significantly greater benefit with the hearing apps, but they were significantly more satisfied with the hearing aid and were more likely to recommend the latter to family and friends. Specifically, the participants favored the hearing aid for being less visible, whereas battery charging and manipulation were thought to be better with the hearing apps. Overall, the authors concluded that the hearing apps may serve well as an introduction to amplification. Convery, Keidser, Seeto, and McLelland (in review) investigated to what extent 20 experienced and 20 inexperienced hearing aid users could follow instructions that were devised by the researchers to self-fit a prototype of the SFHA from SoundWorld Solutions. The self-fitting process included completion of an automated in situ pure tone test and fine-tuning of overall loudness and gain in the low-, mid-, and high-frequency bands, all managed from an app downloaded on a tablet. Disregarding any problems with using the tablet, which was a new tool for many participants, 45%, equally distributed across experienced and inexperienced participants, demonstrated some problems with the self-fitting process. Some of the problems were attributed to the device and have since been rectified by the manufacturer. However, this data, together with clinical reports that some people present at brick-and-mortar hearing centers requesting assistance with their devices purchased in the direct sales market, suggest that current implementations pose challenges to some hearing aid candidates. Below, we summarize what is currently known about the feasibility of SFHAs, especially related to self-management, and point out areas that need particular attention to make SFHAs a viable option.
Empirical Data on Feasibility of the SFHA
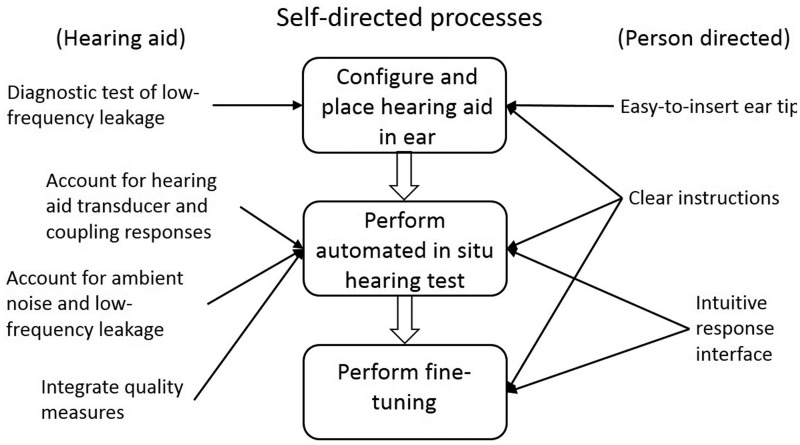
To successfully fit and use a SFHA, the hearing aid candidate has to navigate through three distinct and different steps: (a) configure and place the hearing aid in the ear, (b) perform an automated hearing test, and (c) fine-tune the settings, if unsatisfactory. At the time, the investigations referred to below were carried out; there was no SFHA available that incorporated all three steps. Consequently, the feasibility of each of these steps has so far been investigated in isolation.
Configuration and Placement of the Aid
Assuming that ITE style devices require custom-made moulds, which currently are incompatible with the notion of the hearing aid being managed by the user without needing to see a hearing health professional, a traditional BTE hearing aid has been the centre of investigations. It has been assumed that the first step would include the selection of an appropriately sized ear tip and tube that are connected to the hearing aid body. The ear tip then has to be correctly inserted in the ear canal with the hearing aid body placed behind the ear. These tasks were found to be manageable from written illustrated instructions by a wide cross-section of the population, when the instructions were carefully designed for people with low health-literacy, and when a trusted partner could be consulted as needed (Convery et al., 2011c, 2013). In these investigations, the approach taken to guide people through the step was to make people start with the tube length and ear tip size assumed to fit the average ear of their gender, and then get them to troubleshoot the fit for tightness and looseness. While it was possible to obtain acceptable outcomes with this procedure, there is no doubt that a more generic solution would ease this step tremendously in terms of both reducing the parts that otherwise need to be provided with the hearing aid body and eliminating handling tasks that may be challenging for people with poor dexterity, vision, and cognition (Erber, 2003; Kricos, 2006; Singh, Pichora-Fuller, Hayes, von Schroeder, & Carnahan, 2013). We note that SoundWorld Solutions has introduced a retractable tube that is attached to the hearing aid body and that can be locked into position at different lengths. More recently, a completely ITE style device, Eargo, which is held in place in the ear canal via a fan of soft medical grade silicone fibers (patented and trademarked as Flexi Fibers), has entered the direct-to-consumer market. The device is modeled on a fishing fly and the flexibility of the fan of fibers means that the device fits a wide range of ear canal sizes while still allowing air to circulate in and out of the ear canal. Despite its tip flexibility, two sizes of the device are offered for sale to cover the wide range of ear canal sizes in prospective users. Furthermore, as the design is open, it is suitable only for those with mild or moderate hearing loss. While both these inventions pose some limitations, they are important steps in making the SFHA more accessible and easy to use, and more innovation in the design of the form and plumbing parts of the hearing aid is desirable. In the experiments reported by Convery et al. (2011c, 2013), the final insertion depth of the ear tip was not critical, but this factor is clearly important for the following step of the self-fitting process (see below) and daily usage of the device. Many people have a tendency, at least initially, to place an unfamiliar tip in an excessively shallow position causing potential leakage problems during the threshold testing. We suggest that a diagnostic test of low-frequency leakage (U.S. Patent no 9,113,267, 2015) should be included in the design of SFHAs to assist in getting an adequately fitting ear tip prior to threshold testing. This idea has to our knowledge not yet been fully explored.
Automated In Situ Threshold Measurements
A self-directed, automated in situ threshold test is fundamental for obtaining an appropriate baseline response with the SFHA. As pointed out in 2011, there is sufficient support in the literature for the reliability and validity of both automated audiometry and in situ threshold measurements, see Keidser, Dillon, Zhou, and Carter (2011) for a review. The evidence in support of automated audiometry has in the meantime been strengthened by a meta-analysis (Mahomed, Swanepoel, Eikelboom, & Soer, 2013), and the key to valid in situ thresholds is the application of hearing aid transducer and coupling specific correction factors (O’Brien, Keidser, Yeend, Hartley, & Dillon, 2010). The issues requiring further investigation at that time were identified to be: (a) confirming reliability and validity of self-directed automated in situ threshold measurements, (b) identifying the combination of transducer and coupling that enable the widest range of thresholds to be tested, (c) controlling for ambient noise, and (d) detecting medical contraindication/s to hearing aid fitting.
Validity and reliability of self-directed automated in situ threshold measurements have been verified among participants who followed the prescribed process correctly (Convery, Keidser, Seeto, Yeend, & Freeston, 2015). In this study, 40 participants produced 120 audiograms; one for each ear and a repeat for one ear. Of these audiograms, 30%, involving half of the participants, were incomplete. The causes for incomplete audiograms were identified to be due to a combination of the instructions and the hardware used, the algorithm supporting the automated measurements, and erratic response behaviors. In the first category, shallow insertions of the ear tip (an open dome) and incorrect use of the buttons on a remote control, used both to activate the threshold measurements and as response mechanism during measurements, accounted for most of the problems. The problem with shallow insertions supports the need for developing an ear tip that is easy to insert at an appropriate depth and a method that can alert the user when the ear tip is too loose, as discussed earlier. The remote control, originally used for changing programs and volume in hearing aids, had had the buttons modified to activate new functions, although the button symbols remained related to their original functions. This clearly caused confusion among some participants and using a control with button symbols that more specifically align with the intended function of each button would likely increase chances for an accurate performance. A more recent study that had participants perform an automated in situ hearing test using a commercial product (Convery et al., in review), showed that some hearing aid candidates, even experienced hearing aid users, needed some practice before confidently managing the hearing test, suggesting that earlier test frequencies should be repeated. Convery et al. (2015) further suggested randomizing the order of test frequencies in a balanced way to avoid presenting the highest frequencies consecutively to reduce the chance of an extended period of silence in cases where the threshold at high frequencies is at or beyond the highest level the hearing aid can produce. Erratic response behaviors are related to the person and would be difficult to accommodate for in the test algorithm. However, integrating quality measures in line with those described by Margolis, Saly, Le, and Laurence (2007) would hopefully capture some of these behaviors and generally improve outcomes with, and ensure validity of, automated threshold tests.
The potential impact of using a combination of transducer and coupling unsuitable for the hearing loss and not controlling for ambient noise on hearing aid fittings have been explored and discussed (Kiessling et al., 2015). Of these two issues, the former is the more challenging and makes the SFHA a less attractive solution in environments with little support, when no data are available to guide the client to the most suitable device. The latter should be manageable by enabling the hearing aid microphone to monitor the ambient noise level and comparing those levels with test levels. A similar concept has been successfully implemented in a head set developed for audiometric testing (Swanepoel, Maclennan-Smith, & Hall, 2013) and has shown to provide valid thresholds when testing in low level background noise (Storey, Munoz, Nelson, Larsen, & White, 2014).
Two characteristics that may require medical attention and that are easily detected during manual audiometry are asymmetrical thresholds and a conductive component to the hearing loss. In a self-contained self-fitting device, wireless communication between two devices; a feature that is fast becoming standard in hearing aid chips would be required to detect an asymmetrical loss. Communication between two devices would make it possible to directly compare threshold data between ears and to enable masking in the contralateral ear as needed. It is likely that when measuring in situ thresholds, air transmitted low frequency sound is a greater problem than bone transmitted sound in cases where the ear tips are not fully occluding. To overcome this problem, the incoming sound to the contralateral ear could be analyzed, and if identified to be a pure tone, appropriate masking applied. If the threshold test is driven from a computer, tablet, or smartphone, a comparison of thresholds and the application of masking should be easily managed by the app. The reliability and validity of an automated threshold test that compares thresholds across ears and applies masking as required have been demonstrated by Margolis, Glasberg, Creeke, and Moore (2010).
As for detecting a conductive hearing loss, Convery et al. (2014) introduced an air conduction test in which tones are presented in a continuous background of temporally and spectrally modulated narrowband noise and demonstrated that outcomes on this test in combination with pure-tone thresholds obtained in quiet could predict the presence of a conductive loss with reasonable accuracy. The rationale behind the test is that people with pure sensorineural hearing loss are expected to show elevated thresholds on both tests while people with conductive loss are expected to show elevated thresholds in quiet, but are likely able to take advantage of gaps in the noise to perform similarly to normal-hearing listeners on the tone-in-noise detection test. The sensitivity and specificity of the test battery increased with decreasing test frequency and increasing air-bone gap. Data were obtained using automated procedures for running both air conduction tests; however, both tests were presented through calibrated EAR insert earphones and done under the supervision of a qualified audiologist. Thus, it is currently unknown to what extent the accuracy of the test battery is maintained if the test battery is performed self-directed and in situ. Most likely the factors influencing outcomes would be the same as those that influenced automated in situ threshold measurements as discussed above. Consequently, if the algorithm together with response mechanism and instructions are carefully designed, the proposed method should be feasible for capturing the more significant cases of conductive hearing loss. It also remains to be seen if illustrated written instructions can be produced that successfully guide the user through the entire process, and if users possess the patience to perform the entire test battery in one sitting. For people with symmetrical hearing loss, some time may be saved by using information about thresholds measured in the first ear to determine the starting levels for testing in the second ear. Additionally, time could be saved by omitting the tone in noise test whenever the audiometric configuration of the tone in quiet test is one that only ever occurs for a purely sensorineural loss. A method for detecting active infection and investigating otalgia remains a challenge for the SFHA.
Fine-Tuning
It has been reported that in approximately 50% of listening situations, hearing aid users fitted with prescribed environmentally adaptive devices found loudness to be softer or louder than preferred (Keidser, 2009). Therefore, enabling fine-tuning in SFHAs is desirable because an unsatisfactory baseline response could deter the owner from using the aid, or at least reduce wear time (Saunders, Lewis, & Forsline, 2009). A fine-tuning process managed entirely by the user requires access to controls that will manipulate the amplification characteristic. Volume controls have long been provided on hearing aids to enable users to make in situ changes to overall gain. The software and apps associated with current user-programmable hearing aids enable users to also manipulate such parameters as the gain or frequency response shape, maximum output, and noise management technologies, but unless the programming unit is mobile, the adjustments cannot be performed in situ. One advantage of performing fine-tuning in situ is that the changes made to the amplification can be linked to simultaneous acoustic measures of the environment to provide environment-specific changes to the hearing aid settings. Changes made in situ could be applied permanently by either having the user making the decision and pressing an “apply” button, or by having the hearing aid monitoring the changes made over time in each environment by a training, or learning, algorithm built in to the hearing aid. The algorithm will then incrementally move the amplification to the preferred setting, provided the changes made by the user in a given environment have at least some consistency. When the amplification has moved to the preferred setting, no further adjustments would be necessary. Training the hearing aid to learn a user’s preferred setting in different environments has been found to be manageable and reasonably reliable among hearing aid users with mild to moderately severe hearing loss (Keidser & Alamudi, 2013; Zakis et al., 2007). Although test participants in previous studies were primed about the training feature and its function, it is likely that only instructions on how to manipulate the available controls need to be conveyed to users of SFHAs for the training to occur successfully, but this needs to be confirmed.
There has been some discussion about the need to carefully match prescriptive targets during hearing aid fitting when the devices are subsequently fine-tuned to meet individual preferences (Dillon & Keidser, 2003). As empirical data have demonstrated that some gain-frequency response shapes are better for speech understanding than others (Byrne & Cotton, 1988; Keidser & Grant, 2001), it seems desirable to ensure that the device produces an appropriate baseline response shape based on threshold measurements, as there is no evidence that all users will want to perform the additional steps related to fine-tuning. Furthermore, several studies have observed that final self-adjusted variations are highly influenced by the baseline response, especially in gain-frequency response shape (Dreschler, Keidser, Convery, & Dillon, 2008; Keidser, Dillon, & Convery, 2008; Mueller, Hornsby, & Weber, 2008).
Outcomes
Figure 2 shows an overview of the factors that have been identified to increase the likelihood of a successful outcome with a SFHA. The ultimate evidence for the feasibility of SFHAs is that they produce outcomes that are not inferior to those achieved with professionally fitted devices. A useful by-product of self-fitting may be increased self-efficacy and psychological ownership that may lead to increased usage time and satisfaction with the hearing aids. In one study, experienced hearing aid users who managed to self-fit a hearing aid with a satisfactory result; that is, their fine-tuned responses were acceptable to their hearing loss when compared with the NAL-NL2 prescription, further tried the hearing aid in the field for 6 weeks (Convery et al., in review). After 6 weeks, a series of outcomes measures were obtained in the laboratory, and compared with measures obtained when the participants were wearing their own aid. For various reasons, only five participants completed the full test battery, but in this small cohort, no significant differences were seen in outcomes. This limited observation is encouraging but needs to be verified in a much larger and diverse sample.
Figure 2.
Overview of the steps managed by the user when self-fitting a hearing aid, and the hearing aid and person-directed factors that should increase the likelihood of a successful outcome.
Challenges
The Self-Fitting Hearing Aid
Overall, the empirical evidence collected so far and the emerging self-fitting products support the viability of a SFHA in terms of the technical implementation of the required processes. Table 4 summarizes the different steps of the self-fitting process that have been identified as needing further investigation or development. Remaining challenges for the SFHA seem to revolve around making it more user-friendly. For example, there is a call for a novel hearing aid design that eases the initial steps of configuring the device and inserting it correctly and sufficiently deeply in the ear. We applaud the initiatives described earlier that have so far been introduced by SoundWorld Solutions and Eargo and look forward to seeing other inventors “thinking outside the square.”
Table 4.
Self-Fitting Hearing Aid Issues That Currently Need Further Investigation or Development.
| Step in self-fitting process | Issues to be further investigated | Issues to be solved |
|---|---|---|
| 1. Configure and place hearing aid in the ear. | Devising a method to detect leakage associated with a shallow ear tip insertion or fitting with an ear tip that is too small, and use the measurement to adjust transfer functions used to measure hearing thresholds and adjust amplification. | Improving the form and plumbing system to make it easier to achieve correct placement of the aid and insertion of the tip. Guiding users to the correct insertion of the tip. |
| 2. Perform automated in situ hearing test. | Using the hearing aid microphone to monitor ambient noise levels. Establishing validity and reliability of a test battery designed to detect threshold asymmetry and a conductive component to the hearing loss when testing is self-administered and performed in situ. | Guiding users to the most suitable transducer/coupling combination for their hearing loss. Guiding users through the hearing test. Developing an effective algorithm with quality control for self-directed threshold measurements. Designing on-board buttons that are easily identifiable by the user for the various functions required to fit and fine-tune the hearing aid when placed in the ear. |
| 3. Fine-tune hearing aid settings. | Establishing that hearing aid users can be guided by written illustrated instructions to perform permanent fine-tuning | Developing a mechanism for saving instant adjustments to the response from on-board controls. |
Note. Issues that are specific to the self-contained self-fitting hearing aid are shown in italics.
There is also a need to provide better instructions that increase the chances of successful completion of the self-fitting process and ongoing usage of the device. There is relatively little information available about hearing aid users’ ability to manage a hearing aid from written instructions without any prior face-to-face education. The fitting process is traditionally managed entirely by the hearing health professional, who also educates the user in the daily use and management of the hearing aids. As we have learned through our research activities over the past 5 years, guiding a layperson through these processes using illustrated written instructions is not a trivial matter. Health literacy, which is distinct from literacy by referring specifically to the ability to read and understand information in a health-related context (Mayer & Villaire, 2007), is limited in a significant proportion of older adults (Kutner, Greenberg, & Paulsen, 2006). For this reason, it is recommended that text related to health management be written at a reading level between the third and sixth grades (Doak, Doak, & Root, 1996; Osborne, 2005), and that the information is coherent, well-organized, and minimized using easy to read typography, layout, and graphics (for a review, see Caposecco, Hickson, & Meyer, 2011). Research has demonstrated that better hearing aid management results were obtained when instructions adhered to such criteria (Caposecco, Hickson, Meyer, & Khan, 2016). Even when instructions on processes associated with self-fitting were designed in line with best-practice health literacy principles; people with low cognition still had difficulty with the described tasks (Convery et al., 2013, 2015). Convery et al. (in review) further observed that assistance from another lay person did not improve the chance of successfully completing self-directed audiometric threshold testing. An alternative solution may be to provide assistance services through telehealth. For the services associated with self-fitting, the assistant may not need to be a qualified hearing health professional but could be a person trained to guide users through the steps of the self-fitting process. The idea of “front-line clinical service providers” who had received training in some of the more basic hearing services has previously been entertained (Clark & Swanepoel de, 2014) and as mentioned earlier in this article, some of the more established direct-to-consumer providers, who previously offered no support, have introduced remote coaching to assist their clients with the fine-tuning process and on-going management of their devices. Services provided ad hoc and by less qualified personnel should still keep the cost of hearing care well below the service-bundled prices that are often charged in traditional hearing health-care systems, an original selling point of the SFHA. More information about the mediating effect of accessing a trained or knowledgeable person during the self-fitting process on hearing aid usage and outcomes is currently needed. There is also scope for exploring the use of videos to guide users through the varied processes.
The Self-Contained SFHA
The self-contained SFHA is a device where all the self-fitting processes, including starting and performing the hearing test, applying a prescription to the measured thresholds, and performing fine-tuning, are all managed from on-board controls. This would eliminate the need for accessing other instruments and the Internet. So far research activities, which have been limited to evaluating each self-fitting step in isolation, have also taken advantage of accessing controls for threshold testing and fine-tuning from either a dedicated remote control or a body-worn processor. Only in a preliminary study, in which participants performed the automated in situ threshold test under supervision of an audiologist, was the procedure tested using both an on-board toggle switch and a remote control. This study revealed no difference in validity and reliability of the threshold measurements with the two modes of control, but participants overwhelmingly preferred to use the remote control (Convery et al., 2015). This observation supports the trends in current commercial products of enabling control of self-fitting procedures using an interface. It is well known that many older hearing aid users experience difficulty managing on-board hearing aid controls (Bertoli et al., 2009; Desjardins & Doherty, 2009; Doherty & Desjardins, 2012; Pothier & Bredenkamp, 2006; Upfold, May, & Battaglia, 1990). The number of on-board controls that can be fitted on a hearing aid is limited and enabling both threshold testing and fine-tuning to be done from a small set of controls that are not in view of the user, adds to the complexity of managing the self-fitting process. This abstract problem needs further investigation but also appears to be the greatest barrier to the self-contained SFHA. From this perspective, the increasing prevalence of smartphone ownership and the development of apps for interactive manipulation of hearing aids are appealing, although marrying the SFHA with an app would make the device inaccessible for hearing aid candidates who do not own a computer, smartphone, or tablet. Currently, ownership of at least smartphones is lowest among the older population (Pew Research Center, 2015) for whom hearing loss is most prevalent (Cruickshanks et al., 1998; Hartley, Rochtchina, Newall, Golding, & Mitchell, 2010). In the future, this problem is likely to diminish as technology-savvy generations grow older.
Developing Countries
Originally, we introduced the idea of a self-contained SFHA as a means of meeting the current large unmet demand in underserved areas, particularly in developing countries. Two studies investigating the ability to configure a hearing aid from different parts and to complete a self-directed, automated in situ audiometry test, conducted with Australian hearing-impaired participants, were repeated in two developing countries: China and South Africa. The former study demonstrated that apart from low health literacy, cultural differences must also be taken into account when designing instructions for how to complete the self-fitting task (Convery et al., 2013). Specifically, many of the participants from China did not comply with the self-driven task of configuring the hearing aid, with 58% not reading the instructions fully or even opening the instruction booklet. In the latter study, it was necessary to target people with mild or moderate hearing loss that could be captured within the dynamic test range of the research hearing aid. While it was no problem to find 40 experienced hearing aid users in Australia that met the audiometric criteria, it proved very difficult to find similar numbers in China and South Africa. In these countries, the population who presented to the recruiting hospitals for help with their hearing problems generally had severe hearing loss; that is, their thresholds fell below the lowest levels measurable with the test device. This observation parallels the experience obtained by the Affordable Hearing Aid Project, launched early in this century in India (Seelman & Werner, 2014). Eventually, data collection in both countries had to be abandoned with a total of 15 and 14 completed participants, respectively (unpublished data). The experience highlights the need for both a transducer that can handle moderately severe to profound hearing loss and a method for guiding the user to the transducer and coupling combination that is most suitable for their hearing loss. Despite some improvements being implemented to the overall design of the algorithm for measuring in situ thresholds and the accompanying instructions, validity and reliability of the self-directed threshold measurements obtained in the developing countries were slightly poorer than those obtained in Australia. In the Australian population, 91% of valid threshold data obtained via the hearing aid were within ±10 dB of the manually recorded thresholds, and 97% of valid test and retest thresholds measured with the hearing aid met the ±10 dB criterion. The corresponding figures were 86% and 93% for the Chinese participants and 73% and 90% for the South African participants. The low validity observed for the South African population was primarily due to three participants who consistently produced lower or higher thresholds across frequencies and ears. No personal or other factors were found to explain their results.
In addition to the challenges discussed earlier that are pertinent to the device, the major challenges of SFHAs (whether self-contained or not) in developing countries continue to be affordability and a sustainable delivery model (Caccamo, Voloshchenko, & Dankyi, 2014). Some success has been had with the donor model, in which non-governmental organizations obtain and deliver hearing aids in developing countries, often equipping and training local staff in providing the most basic services in the process (Carkeet, Pither, & Anderson, 2014). However, if the organization is unable to provide continuing support to local staff, this model is a short-term solution at best (Seelman & Werner, 2014). According to Seelman and Werner (2014) the model that is most likely to succeed in the mid- to long-term is the partnership model; that is, a model in which international, public, and private sector and non-governmental organizations work together to provide the needed service, devices, and equipment, while the local government provides a workable health and legal infrastructure. The authors do acknowledge that this model can be bureaucratically complex.
Future Predictions
We said in 2011 that things in this area are set to change, and they have. In a span of 5 years, self-fitting devices and self-manageable hearing apps have become readily available, although they are as yet mostly accessible through a highly unregulated direct-to-consumers market, and are unsupported by evidence-based data. We predict that both technologies are here to stay and that they will merge; that is, the future SFHA will be an aid (that may look more like an ear bud than the current BTEs) that is wirelessly connected with, and manipulated from, a smartphone. Hopefully, efforts will also be made to ensure that these devices are as effective as professionally fitted hearing aids. According to a recent survey on Internet access conducted by the UK Office for National Statistics (2015), people are increasingly purchasing goods and looking for health-related information online. We anticipate that in the future, the smartphone will also connect the user of a SFHA with either a hearing health professional, or a trained assistant, who from a remote point could access informative data logged in the hearing aid, as needed. This concept is already applied in other health areas; for example, cardio-diabetic patients can use an app to measure their ECG, blood glucose, pulse rate, calories burnt, and activity counts from any location and to obtain feedback through remote monitoring from a physician (Anantharaman, 2015). Overall, combining SFHAs with a telehealth structure has a strong appeal and would seem like a suitable solution particularly for people living in underserved areas.
With the current calls in the USA to urgently improve hearing for older adults by approving direct-to-consumer sale of hearing aids, including SFHAs, allowing PSAPs to be advertised as products for hearing-impaired people (President’s Council of Advisors on Science and Technology (PCAST) Report, 2015), and unbundling the cost of hearing services to address consumer’s concerns about the affordability, transparency, and accessibility of hearing health care (PCAST Report, 2015; Shaw, 2015; Sjoblad, 2015), we also believe that the SFHA will soon be available in the traditional and regulated hearing health-care model. In the traditional model, the benefits of the SFHA are two fold; it can be as follows: (a) reduce the time clinicians currently spend on testing and fitting to allow them more time to see more clients, to provide alternative rehabilitation options, and to support longer term, higher level client needs (i.e., the clinician can spend more time providing patient-centred care, Grenness, Hickson, Laplante-Levesque, & Davidson, 2014a, 2014b, where needed); and (b) reduce the cost for clients for whom a hearing aid is identified to be the preferred rehabilitation option. With unbundled prices in place, clients who purchase a SFHA may only need to incur additional service costs if a session on getting started with the self-fitting process, or support with ongoing hearing aid management, is needed.
Overall, we believe that in developed countries, the SFHA will soon challenge providers of hearing health care to change the structure and content of their services, governments and other bodies to reconsider the metrics used to judge outcomes and the need for funding, and university programs to change the training of audiologists. In developing countries, the app-driven SFHA should have a bright future among those who can afford a smartphone and can access the Internet. Unless manipulated from a remote processor as proposed by Audientes, we do have some doubt about the self-contained SFHA from a user-management perspective; particularly among older adults, and predict that this device is unlikely to emerge any time soon.
Other Statements
Unpublished studies referred to in this article were approved by the Australian Hearing Human Research Ethics Committee and conformed in all respects to the Australian government’s National Statement on Ethical Conduct in Human Research (National Health and Medical Research Council, 2007).
Acknowledgments
The views presented in this article are solely those of the authors and are not necessarily shared by the funding sources. The authors would like to thank Professors Lena Wong from Hong Kong University and De Wet Swanepoel from the University of Pretoria for their assistance with organizing the collection of unpublished data in China and South Africa, and Professor Harvey Dillon for his input to the various projects conducted at NAL and valuable comments to an earlier draft of this article.
Declaration of Conflicting Interests
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The authors acknowledge the financial support of the HEARing Cooperative Research Centre, established and supported under the Business Cooperative Research Centres Programme, and the Commonwealth Department of Health and Ageing.
References
- Amlani A. M., Taylor B., Levy C., Robbins R. (2013) Utility of smartphone-based hearing aid applications as a substitute to traditional hearing aids. The Hearing Review 20: 16–23. [Google Scholar]
- Anantharaman K. (2015) Let’s turn your smart phone to a smart physician. Journal of Novel Physiotherapy and Physical Rehabilitation 2(1): 8–9. [Google Scholar]
- Bertoli S., Staehelin K., Zemp E., Schindler C., Bodmer D., Probst R. (2009) Survey on hearing aid use and satisfaction in Switzerland and their determinants. International Journal of Audiology 48(4): 183–195. [DOI] [PubMed] [Google Scholar]
- Blamey, P. (2012). An alternative to the audiogram for hearing aid fitting. Poster presented at the International Hearing Aid Research Conference, Lake Tahoe.
- Byrne D., Cotton S. (1988) Evaluation of the national acoustic laboratories’ new hearing aid selection procedure. Journal of Speech and Hearing Research 31(2): 178–186. [DOI] [PubMed] [Google Scholar]
- Caccamo S., Voloshchenko A., Dankyi N. Y. (2014) The importance of creating a social business to produce low-cost hearing aids. Disability and Rehabilitation. Assistive Technology 9(5): 368–373. [DOI] [PubMed] [Google Scholar]
- Caposecco A., Hickson L., Meyer C. (2011) Assembly and insertion of a self-fitting hearing aid: Design of effective instruction materials. Trends in Amplification 14(4): 184–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caposecco A., Hickson L., Meyer C., Khan A. (2016) Evaluation of a modified user guide for hearing aid management. Ear and Hearing 37(1): 27–37. [DOI] [PubMed] [Google Scholar]
- Carkeet D., Pither D., Anderson M. (2014) Service, training and outreach – The EARS Inc. Model for a self sustainable hearing program in action. Disability and Rehabilitation. Assistive Technology 9(5): 383–390. [DOI] [PubMed] [Google Scholar]
- Clark J. L., Swanepoel de W. (2014) Technology for hearing loss – As we know it, and as we dream it. Disability and Rehabilitation. Assistive Technology 9(5): 408–413. [DOI] [PubMed] [Google Scholar]
- Convery E., Keidser G., Caposecco A., Swanepoel de W., Wong L. L., Shen E. (2013) Hearing-aid assembly management among adults from culturally and linguistically diverse backgrounds: Toward the feasibility of self-fitting hearing aids. International Journal of Audiology 52(6): 385–393. [DOI] [PubMed] [Google Scholar]
- Convery E., Keidser G., Dillon H., Hartley L. (2011a) A self-fitting hearing aid: Need and concept. Trends in Amplification 15(4): 157–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Convery E., Keidser G., Hartley L. (2011b) Perception of a self-fitting hearing aid among urban-dwelling hearing-impaired adults in a developed country. Trends in Amplification 15(4): 175–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Convery E., Keidser G., Hartley L., Caposecco A., Hickson L., Meyer C. (2011c) Management of hearing aid assembly by urban-dwelling hearing-impaired adults in a developed country: Implications for a self-fitting hearing aid. Trends in Amplification 15(4): 196–208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Convery E., Keidser G., Seeto M., Freeston K., Zhou D., Dillon H. (2014) Identification of conductive hearing loss using air conduction tests alone: Reliability and validity of an automatic test battery. Ear and Hearing 35(1): e1–e8. doi:10.1097/AUD.0b013e31829e058f. [DOI] [PubMed] [Google Scholar]
- Convery, E., Keidser, G., Seeto, M., & McLelland, M. (in review). Evaluation of the self-fitting process with a commercially available hearing aid. Journal of the American Academy of Audiology. [DOI] [PubMed]
- Convery E., Keidser G., Seeto M., Yeend I., Freeston K. (2015) Factors affecting reliability and validity of self-directed automatic in situ audiometry: Implications for self-fitting hearing AIDS. Journal of the American Academy of Audiology 26(1): 5–18. [DOI] [PubMed] [Google Scholar]
- Cruickshanks K. J., Wiley T. L., Tweed T. S., Klein B. E., Klein R., Mares-Perlman J. A., Nondahl D. M. (1998) Prevalence of hearing loss in older adults in beaver dam, Wisconsin. The Epidemiology of Hearing Loss Study. American Journal of Epidemiology 148(9): 879–886. [DOI] [PubMed] [Google Scholar]
- Desjardins J. L., Doherty K. A. (2009) Do experienced hearing aid users know how to use their hearing AIDS correctly? American Journal of Audiology 18(1): 69–76. [DOI] [PubMed] [Google Scholar]
- Dillon H., Keidser G. (2003) Arguments for and against using probe-mic measurments. The Hearing Journal 56(10): 28–30. [Google Scholar]
- Dillon H., Zakis J., McDermott H. J., Keidser G., Dreschler W. A., Convery E. (2006) The trainable hearing aid: What will it do for clients and clinicians? The Hearing Journal 59(4): 30–36. [Google Scholar]
- Doak C., Doak L., Root J. (1996) Teaching patients with low literacy levels, Philadelphia, PA: JB Lippincott. [Google Scholar]
- Doherty K. A., Desjardins J. L. (2012) The practical hearing aids skills test-revised. American Journal of Audiology 21(1): 100–105. [DOI] [PubMed] [Google Scholar]
- Dreschler W. A., Keidser G., Convery E., Dillon H. (2008) Client-based adjustments of hearing aid gain: The effect of different control configurations. Ear and Hearing 29(2): 214–227. [DOI] [PubMed] [Google Scholar]
- Erber N. P. (2003) Use of hearing aids by older people: Influence of non-auditory factors (vision, manual dexterity). International Journal of Audiology 42(Suppl 2): 2S21–25. [PubMed] [Google Scholar]
- Galster J. (2012) Apps for audiology. Audiology Practices 4(3): 16–19. Retrieved from http://galster.net/wp-content/uploads/2012/11/Galster-2012-Audiology-Practices-Apps-for-Audiology.pdf. [Google Scholar]
- Grenness C., Hickson L., Laplante-Levesque A., Davidson B. (2014a) Patient-centred audiological rehabilitation: Perspectives of older adults who own hearing aids. International Journal of Audiology 53(Suppl 1): S68–S75. [DOI] [PubMed] [Google Scholar]
- Grenness C., Hickson L., Laplante-Levesque A., Davidson B. (2014b) Patient-centred care: A review for rehabilitative audiologists. International Journal of Audiology 53(Suppl 1): S60–S67. [DOI] [PubMed] [Google Scholar]
- Hartley D., Rochtchina E., Newall P., Golding M., Mitchell P. (2010) Use of hearing AIDS and assistive listening devices in an older Australian population. Journal of the American Academy of Audiology 21(10): 642–653. [DOI] [PubMed] [Google Scholar]
- Keidser G. (2009) Many factors are involved in optimizing environmentally adaptive hearing aids. The Hearing Journal 62(1): 26–32. [Google Scholar]
- Keidser G., Alamudi K. (2013) Real-life efficacy and reliability of training a hearing aid. Ear and Hearing 34(5): 619–629. [DOI] [PubMed] [Google Scholar]
- Keidser G., Dillon H., Convery E. (2008) The effect of the base line response on self-adjustments of hearing aid gain. Journal of the Acoustical Society of America 124(3): 1668–1681. [DOI] [PubMed] [Google Scholar]
- Keidser G., Dillon H., Zhou D., Carter L. (2011) Threshold measurements by self-fitting hearing aids: Feasibility and challenges. Trends in Amplification 15(4): 167–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keidser G., Grant F. (2001) Comparing loudness normalization (IHAFF) with speech intelligibility maximization (NAL-NL1) when implemented in a two-channel device. Ear and Hearing 22(6): 501–515. [DOI] [PubMed] [Google Scholar]
- Kiessling J., Leifholz M., Unkel S., Pons-Kuhnemann J., Jespersen C. T., Pedersen J. N. (2015) A comparison of conventional and in-situ audiometry on participants with varying levels of sensorineural hearing loss. Journal of the American Academy of Audiology 26(1): 68–79. [DOI] [PubMed] [Google Scholar]
- Kralik D., Koch T., Price K., Howard N. (2004) Chronic illness self-management: Taking action to create order. Journal of Clinical Nursing 13(2): 259–267. [DOI] [PubMed] [Google Scholar]
- Kricos P. B. (2006) Audiologic management of older adults with hearing loss and compromised cognitive/psychoacoustic auditory processing capabilities. Trends in Amplification 10(1): 1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kutner M., Greenberg E. Y. J., Paulsen C. (2006) The health literacy of America’s adults: Results from the 2003 national assessment of adult literacy (NCES 2006483), Washington, DC: National Center for Education Statistics, US Department of Education. [Google Scholar]
- Lawn S., Battersby M. W., Pols R. G., Lawrence J., Parry T., Urukalo M. (2007) The mental health expert patient: Findings from a pilot study of a generic chronic condition self-management programme for people with mental illness. The International Journal of Social Psychiatry 53(1): 63–74. [DOI] [PubMed] [Google Scholar]
- Mahomed, F., Swanepoel, D. W., Eikelboom, R. H., & Soer, M. (2013). Validity of automated threshold audiometry: A systematic review and meta-analysis. Ear and Hearing. doi:10.1097/AUD.0b013e3182944bdf. [DOI] [PubMed]
- Margolis R. H., Glasberg B. R., Creeke S., Moore B. C. J. (2010) AMTAS®: Automated method for testing audiotory sensitivity: Validation studies. International Journal of Aduiology 49(3): 185–194. [DOI] [PubMed] [Google Scholar]
- Margolis R. H., Saly G. L., Le C., Laurence J. (2007) Qualind: A method for assessing the accuracy of automated test. Journal of the American Academy of Audiology 18(1): 78–89. [DOI] [PubMed] [Google Scholar]
- Mayer G., Villaire M. (2007) Health literacy in primary care: A clinician’s guide, New York, NY: Springer. [Google Scholar]
- Meng H., Friedberg F., Castora-Binkley M. (2014) Cost-effectiveness of chronic fatigue self-management versus usual care: A pilot randomized controlled trial. BioMed Central Family Practice 15: 184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller H. G., Hornsby B. W., Weber J. E. (2008) Using trainable hearing aids to examine real-world preferred gain. Journal of the American Academy of Audiology 19(10): 758–773. [DOI] [PubMed] [Google Scholar]
- O’Brien A., Keidser G., Yeend I., Hartley L., Dillon H. (2010) Validity and reliability of in-situ air conduction thresholds measured through hearing aids coupled to closed and open instant-fit tips. International Journal of Audiology 49(12): 868–876. [DOI] [PubMed] [Google Scholar]
- Osborne H. (2005) Health literacry from A to Z, Boston, MA: Jones and Bartlett. [Google Scholar]
- Pew Research Center. (2015). The smartphone difference. Retrieved from http://www.pewinternet.org/2015/04/01/us-smartphone-use-in-2015/.
- Pothier D. D., Bredenkamp C. (2006) Hearing aid insertion: Correlation between patients’ confidence and ability. The Journal of Laryngology and Otology 120(5): 378–380. [DOI] [PubMed] [Google Scholar]
- President’s Council of Advisors on Science and Technology Report. (2015). Retrieved from https://www.whitehouse.gov/sites/default/files/microsites/ostp/PCAST/pcast_hearing_tech_letterreport_final.pdf.
- Richardson G., Epstein D., Chew-Graham C., Dowrick C., Bentall R. P., Morriss R. K. FINE Trial Writing group on behalf of the FINE Trial group (2013) Cost-effectiveness of supported self-management for CFS/ME patients in primary care. BioMed Central Family Practice 14: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders G. H., Lewis M. S., Forsline A. (2009) Expectations, prefitting counseling, and hearing aid outcome. Journal of the American Academy of Audiology 20(5): 320–334. [DOI] [PubMed] [Google Scholar]
- Seelman K. D., Werner R. (2014) Technology transfer of hearing aids to low and middle income countries: Policy and market factors. Disability and Rehabilitation. Assistive Technology 9(5): 399–407. [DOI] [PubMed] [Google Scholar]
- Shaw G. (2015) Unbundling hearing health care pricing: Up-front work pays off. The Hearing Journal 68: 28–32. [Google Scholar]
- Singh G., Pichora-Fuller M. K., Hayes D., von Schroeder H. P., Carnahan H. (2013) The aging hand and the ergonomics of hearing aid controls. Ear and Hearing 34(1): e1–e13. doi:10.1097/AUD.0b013e31825f9bba. [DOI] [PubMed] [Google Scholar]
- Sjoblad, S. (2015). A model of evidence-based practice with itemized billing. Institute of Medicine Committee on Accessble and Affordable Hearing Health Care for Adults, University of North Carolina: Chapel Hill.
- Storey K. K., Munoz K., Nelson L., Larsen J., White K. (2014) Ambient noise impact on accuracy of automated hearing assessment. International Journal of Audiology 53(10): 730–736. [DOI] [PubMed] [Google Scholar]
- Swanepoel D., Maclennan-Smith F., Hall J. W. (2013) Diagnostic pure-tone audiometry in schools: Mobile testing without a sound-treated environment. Journal of the American Academy of Audiology 24(10): 992–1000. [DOI] [PubMed] [Google Scholar]
- UK Office for National Statistics. (2015, August 6). Internet access – Households and individuals 2015. Statistical Bulletin. Retrieved from http://www.ons.gov.uk/ons/rel/rdit2/internet-access—households-and-individuals/2015/stb-ia-2015.html.
- Upfold L. J., May A. E., Battaglia J. A. (1990) Hearing aid manipulation skills in an elderly population: A comparison of ITE, BTE, and ITC aids. British Journal of Audiology 24(5): 311–318. [DOI] [PubMed] [Google Scholar]
- Usher, J., & Keady, J. P. (2015). Acoustic sealing analysis system. U.S. Patent no 9,113,267.
- Zakis J. A., Dillon H., McDermott H. J. (2007) The design and evaluation of a hearing aid with trainable amplification parameters. Ear and Hearing 28(6): 812–830. [DOI] [PubMed] [Google Scholar]