Patients with a systemic neurological disease can often first present with symptoms and signs affecting the hand. With limited time to review patients in clinic, the symptoms can often be attributed to common hand disorders, such as carpal tunnel syndrome (Figure 1). The aim of this article is to review a few of the common systemic neurological disorders that may first present with manifestations in the hand. A secondary goal would be to prevent the surgical treatment of hand conditions that are more amenable to systemic treatment if appropriately managed.
Figure 1.
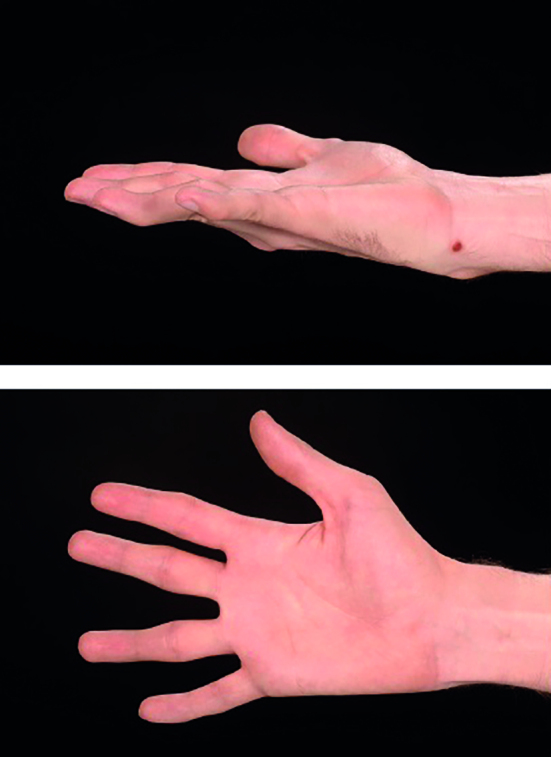
An anteroposterior and lateral clinical photograph of the right hand of a patient with Charcot-Marie Tooth disease. Note the thenar flattening with preservation of hypothenar muscle bulk. Sensory deficit was most notable in the radial three digits. The changes were unilateral. An initial diagnosis of carpal tunnel syndrome had been made.
MOTOR NEURONE DISEASE
Motor neurone disease (MND) can present with both upper and lower motor neurone signs. The terminology attributed to the disorder is subdivided between upper (primary lateral sclerosis) and lower motor neurone (progressive and spinal musclular atrophies) or both (amyotrophic lateral sclerosis). Onset of the disease is usually in the mid-50s with an incidence of 1–2:100 000.
In the hand, the lower and combined motor neurone types may first present with wasting of the thenar muscles. Typically it is the abductor pollicis brevis (APB) muscle that is first to be affected. Based on such a presentation, it would be understandable for the diagnosis of carpal tunnel syndrome to be made despite the absence of sensory signs.
Subsequent to the weakening of the thenar muscles, the first dorsal interosseous (FDI) muscle is next affected.1 This is referred to as the ‘split hand’ as the radial aspect of the hand is far more affected than the ulna aspect.2 The muscle atrophy eventually progresses proximally with diminished tendon reflexes.
HEREDITARY NEUROPATHY WITH LIABILITY TO PRESSURE PALSIES (HNPP)
This condition typically presents between 30 and 40 years of age. As a result of the deletion of a segment of chromosome 17p11.2-12 there is inadequate production of myelin with reduced myelination of both sensory and motor nerves.3 Minor trauma such as stretching or pressure from traction or repetitive movement results in focal demyelination. As a result of the myelin deficiency repair is poor and the nerve is then more susceptible to further injury. In the upper limb the median and ulna nerves are commonly affected. Symptoms can be as mild as occasional numbness but can progress to true sensory deficit with motor weakness.
The diagnosis can be confirmed through genetic testing and nerve conduction testing. Electromyographs confirm the disease with the bilateral slowing of sensory and motor nerve conduction at the carpal tunnel with at least one additional abnormal finding for motor conduction in one peroneal nerve.4
The importance of clarifying the diagnosis is that decompression is controversial and may only provide short-lived relief. Patients are likely to experience recurrent symptoms following decompression and may undergo further unnecessary surgery if there is concern that incomplete decompression has been performed. On a final note, if the patient is undergoing anaesthesia meticulous attention must be paid to prevent pressure on any nerves that may cause further palsies.
DYSTONIA
This condition involves an initial repetitive involuntary movement followed by abnormal posturing of muscles and can involve the face (blepharospasm), neck (spasmodic torticollis), and hands. It is thought that the balance between the excitation and inhibition of muscles is disrupted and this then leads to the co-contraction of antagonistic muscles.5 This can be painful during as well as after the abnormal posturing.
In the hand this condition is usually task specific and can be so debilitating that it may cause a patient to lose their job. These occupations include guitar playing, piano playing, writing, and typing.6 It is unclear what the exact aetiology for the condition is but there is a genetic as well as an occupational or repetitive task disposition to it. It is a clinical diagnosis and does not require special tests.
The management of this condition includes therapy with retraining of muscles as well as mirror box exercises. This can be combined with behavioural sessions. Botulinum toxin is also used under EMG guidance to weaken the antagonistic muscles.
MULTIPLE SCLEROSIS
This complex disease has a frequency of 100 per 100 000 people. It is thought to be related to central demyelination and it can have multiple presentations from acute progressive to chronic and relapsing types. A key point is that a patient may present with symptoms and signs that are disseminated in time and anatomical location.
Multiple sclerosis can affect both the sensory and motor systems. It is possible that the first area to be affected is the hand. Again, the diagnosis of median or ulnar nerve compression could be made at this presentation, thus delaying the underlying diagnosis. Other hand signs include an intention and postural tremor, and there may also be clonus and spasm. Careful evaluation for other systemic neurological symptoms or signs should be undertaken. Management is predominantly medical and surgery should not be attempted without a definite achievable goal.
CONCLUSION
At medical school, students are often taught to begin a systematic examination by looking at the hands. In the case of a patient presenting with neurological symptoms affecting the hand the reverse is true. The clinician should consider the possible diagnoses of a systemic neurological disease such as those presented. Careful history and examination supplemented with appropriate investigations such as electromyography, nerve conduction studies, and magnetic resonance imaging can aid the diagnosis. In reality, most apparent compressive neuropathies and radicular pains will prove to be just that. However, in those patients with a systemic neurological disease, a systematic approach can avoid patients undergoing unnecessary operative procedures. Instead, patients can be correctly diagnosed and treated at the earliest possible opportunity.
Acknowledgments
Mr Elliot Sorene and Miss Emma Taylor — for their support during the completion of the Diploma in Hand Surgery.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Kuwabara S, Sonoo M, Komori T, et al. Dissociated small hand muscle atrophy in amyotrophic lateral sclerosis: frequency, extent, and specificity. Muscle Nerve. 2008;37(4):426–430. doi: 10.1002/mus.20949. [DOI] [PubMed] [Google Scholar]
- 2.Wilbourn AJ. The ‘split hand syndrome’. Muscle Nerve. 2000;23(1):138. doi: 10.1002/(sici)1097-4598(200001)23:1<138::aid-mus22>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 3.Meier C, Moll C. Hereditary neuropathy with liability to pressure palsies. Report of two families and review of the literature. J Neurol. 1982;228(2):73–95. doi: 10.1007/BF00313754. [DOI] [PubMed] [Google Scholar]
- 4.Mouton P, Tardieu S, Gouider R, et al. Spectrum of clinical and electrophysiologic features in HNPP patients with the 17p11.2 deletion. Neurology. 1999;52(7):1440–1446. doi: 10.1212/wnl.52.7.1440. [DOI] [PubMed] [Google Scholar]
- 5.Lin PT, Hallett M. The pathophysiology of focal hand dystonia. J Hand Ther. 2009;22(2):109–113. doi: 10.1016/j.jht.2008.10.008. quiz 114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Frucht SJ. Focal task-specific dystonia of the musicians’ hand — a practical approach for the clinician. J Hand Ther. 2009;22(2):136–142. doi: 10.1016/j.jht.2008.11.006. quiz 143. [DOI] [PubMed] [Google Scholar]


