Abstract
Epidemiological differences exist between Mycobacterium africanum (Maf)- and Mycobacterium tuberculosis (Mtb)-infected patients, but to date, contributing host factors have not been characterised. We analysed clinical outcomes, as well as soluble markers and gene expression profiles in unstimulated, and ESAT6/CFP-10-, whole-Maf- and Mtb-stimulated blood samples of 26 Maf- and 49 Mtb-HIV-negative tuberculosis patients before, and after 2 and 6 months of anti-tuberculosis therapy. Before treatment, both groups had similar clinical parameters, but differed in few cytokines concentration and gene expression profiles. Following treatment the body mass index, skinfold thickness and chest X-ray scores showed greater improvement in the Mtb- compared to Maf-infected patients, after adjusting for age, sex and ethnicity (p = 0.02; 0.04 and 0.007, respectively). In addition, in unstimulated blood, IL-12p70, IL12A and TLR9 were significantly higher in Maf-infected patients, while IL-15, IL-8 and MIP-1α were higher in Mtb-infected patients. Overnight stimulation with ESAT-6/CFP-10 induced significantly higher levels of IFN-γ and TNF-α production, as well as gene expression of CCL4, IL1B and TLR4 in Mtb- compared to Maf-infected patients. Our study confirms differences in clinical features and immune genes expression and concentration of proteins associated with inflammatory processes between Mtb- and Maf-infected patients following anti-tuberculosis treatment These findings have public health implications for treatment regimens, and biomarkers for tuberculosis diagnosis and susceptibility.
Author Summary
In the Gambia tuberculosis is caused my two major lineages within the Mycobacterium tuberculosis complex (MTBC), M. tuberculosis lineages 4 and M. africanum lineage 6. Our analysis of 26 M. africanum- and 49 M. tuberculosis -HIV-negative tuberculosis patients’ clinic parameters and antigen-stimulated blood cytokines concentration and genes expression reveal that heterogeneous response to standard anti-tuberculosis treatment might depend on the diversity of MTBC lineages. Before treatment, the two groups of patients had similar clinical parameters, but greater improvement was observed in M. tuberculosis- compared to M. africanum -infected patients post-treatment. This was supported by higher production of inflammation-associated cytokines and genes in unstimulated blood samples from M. africanum-infected patients compared to those infected with M. tuberculosis, who instead had higher level of disease resolution cytokines. In contrast, there were lower cytokine responses in antigen-stimulated blood samples of M. africanum- compared to M. tuberculosis-infected patients post-treatment indicating a poorly recovered immune profile. Our results suggest that M. africanum patients respond relatively poorly to the standard anti-tuberculosis treatment or might have a pre-existing defective immune profile; this could explain why they succumb to less virulent mycobacteria.
Introduction
Mycobacterium africanum (Maf) is an ancient lineage of the Mycobacterium tuberculosis (Mtb) Complex (MTBC), mostly found in West Africa where it causes up to half of all tuberculosis (TB) cases [1]. Apart from descriptions of the epidemiological differences between Maf and Mtb infection in the human population, differences in underlying immune responses, clinical course and outcome of TB therapy have not been described [2]. Other authors have recently attempted to define biomarkers that are able to predict treatment outcome and if validated, these biomarkers could significantly shorten trials of new TB regimens [3–5]. Ultimately, the performance of such biomarkers might be influenced by the infecting mycobacterial lineage. Previous studies that have assessed whether the rate of response to treatment differs between infecting MTBC lineages obtained conflicting results [6–13], but data from our own laboratory and others [6,12,13] indicate that their responses to treatment are heterogeneous. Different MTBC lineages may have been responsible for the heterogeneous response to the shorter TB treatment regimen containing Gatifloxacin recently tested in West Africa [14].
We have previously shown that although the proportion of activated T cells were similar in Maf- and Mtb-infected patients pre-treatment, they decreased significantly in Mtb-infected patients, while those of Maf-infected patients were persistently high but consisted of poorly functional T cells post-treatment [15]. In addition, the transcriptomic and metabolic profiles of Maf- and Mtb-infected patients while similar at baseline significantly differed by lineage post-treatment mainly due to changes in Mtb-infected but not in Maf-infected patients [13]. These results suggest that intrinsic host factors determine the immune response to TB and/or differential effect of the standard anti-TB treatment on the two lineages.
This study was conducted to investigate the changes in the host immune response and clinical outcomes following treatment in a larger cohort of Maf- and Mtb-infected tuberculosis patients before, during and after standard anti-TB treatment. Although we found no differences in the clinical parameters measured and found differences in only few cytokines concentration and gene expression profiles between Maf- and Mtb-infected patients pre-treatment, many of these showed significant differences post-treatment suggesting either intrinsic lineage-specific difference in response to standard anti-TB therapy and/or in the underlying host immunity.
Methods
Ethics statement
Ethical approval was obtained from The Joint Gambian Government/Medical Research Council (MRC) Ethics Committee in The Gambia and the London School of Hygiene & Tropical Medicine Ethics Committee. All patients provided written informed consent.
Study participants
Sputum smear and culture positive TB patients were recruited at the TB Clinic, MRC Unit, Fajara, The Gambia. On recruitment, we recorded clinical symptoms using a questionnaire that included duration of cough, weight lost, night sweats, and fever; routine clinical assessment including anthropometry (weight, height, skinfold thickness (SFK) and body mass index (BMI)), and tuberculin skin test (TST), as previously reported [16]. Sputum was sent for TB smear and culture. The genotypes of the infecting bacilli in sputum were determined by spoligotyping analysis and assessing the presence or absence of lineage defining Large Sequence Polymorphisms (LSP) RD702 and TbD1 as previously described [15,17]. All patients were HIV-negative with no history of previous TB disease and were enrolled before anti-TB treatment. All patients received conventional therapy of 2 months intensive treatment with Isoniazid, Rifampicin, Pyrazinamide, Ethambutol, followed by a second phase of four months with only Isoniazid and Rifampicin (2HRZE/4HR) [18]. They were actively followed-up at 2 and 6 months of treatment, during which chest x-ray (CXR), haematological and sputum smear examination, and anthropometric measurements were done, and heparinized blood samples collected. All patients were confirmed sputum smear negative at the end of the 6 months treatment.
Whole blood stimulation and multiplex cytokine assays
Undiluted whole blood (180 μL) was incubated overnight (16 hours) in duplicate with 20 μL of medium alone or phytohaemagglutinin (PHA-L, Sigma-Aldrich, UK; 5 μg/ml), purified protein derivative (Mtb-PPD; Staten Serum Institute, Denmark; 10 μg/ml), ESAT-6/CFP-10 peptides pool [(EC, ProImmune, UK; 2.5 μg/mL/peptides), EC amino acid sequence is identical in Maf and Mtb lineages [19], or whole mycobacteria Mtb H37Rv and Maf GM041182 used both live [final multiplicity of infection (MOI) 1:2 (bacteria: monocytes) and heat-killed (6 x 105 cfu/mL)] [15].
After overnight culture, supernatants were collected from each well, TriReagent (Ambion, Foster City, USA) was added to the pellet, and both were stored at -20°C till analysis. The supernatants were analysed using a Bio-Plex Pro 27-plex kit (cat# M50OKCAFOY, BIO-RAD Laboratories; Belgium) for IL-1β, IL-1RA, IL-2, IL-4, IL-5, IL-6, IL-7, IL-8 (CXCL8), IL-9, IL-10, IL-12p70, IL-13, IL-15, IL-17A, Eotaxin (CCL11), Basic FGF, granulocyte colony-stimulating factor [G-CSF], granulocyte-macrophage CSF [GM-CSF], IFN-γ, IP-10 (CXCL10), MCP-1 (CCL2), MIP-1α (CCL3), MIP-1β (CCL4), PDGF-ββ, RANTES (CCL5), TNF-α, and VEGF following the standard protocol provided by the manufacturers. Plates were immediately read on the Bio-Plex reader using Bio-Plex Manager software (version 4.1.1; Bio-Rad, USA) with five-parameter logistic (5-PL) algorithms and a low PMT setting. All standards were run in duplicate. OOR> and OOR< values were assigned the highest and lowest standard values multiplied or divided by 2 respectively.
RNA extraction and dual colour Reverse Transcription Multiplex Ligation-dependent Probe Amplification (dcRT-MLPA)
RNA was isolated from stimulated blood pellets lysed in TriReagent (Ambion, Foster City, USA) using a Chloroform/RNeasy (Qiagen, Crawley, UK) protocol following manufacturer’s instructions. Dual colour RT-MLPA was performed as described previously [20,21]. Briefly, 100–150 ng RNA was reverse transcribed using 80nM of target-specific RT primers, 1x MMLV reverse transcriptase and 0.4 mM of each dNTP. cDNA was denatured and hybridized overnight at 60°C with 4 nM of probe mix containing left- and right-hand probes of 85 genes. After ligating the hybridized probes with ligase-65 for 15 min at 54°C, PCR amplification of the ligation products was performed with specific SALSA FAM-labelled MLPA primers, HEX-labelled MAPH primers (1 μL of 2 μM each, forward primer 5’-GGCCGCGGGAATTCGATT-3’ and reverse primer 5’-GCCGCGAATTCACTAGTG-3’), 14.75 μL H20 and 0.25 μL SALSA polymerase. Primers and probes were from Sigma-Aldrich Chemie (Zwijndrecht, The Netherlands) and MLPA SALSA reagents from MRC-Holland (Amsterdam, The Netherlands). Thermal cycling conditions were 33 cycles of 30s at 95°C, 30s at 58°C and 60s at 72°C, followed by 1 cycle of 20min at 72°C. PCR products were diluted 1:10 in HiDi formamide containing 400 HD ROX size standard and analysed on an Applied Biosystems 3730 capillary sequencer in GeneScan mode (Applied Biosystems, Foster City, USA).
Data were analysed using GeneMapper 4.0 software package (Applied Biosystems, Warrington, UK) and peak areas were exported to a Microsoft Excel file for downstream analysis. Data were subsequently normalized to GAPDH housekeeping gene and signals below the threshold value for noise cut-off (peak area #200) were assigned threshold value for noise cut-off. A positive control that encompassed the complement reverse sequence of the combined target-specific sequences of the left and right hand half-probes was used for all runs.
Statistical analysis
Demographic and clinical characteristics were compared between Maf- and Mtb-infected patients using Mann-Whitney test for continuous variables and Fisher’s exact test for categorical variables. BMI, skinfold thickness and haematology parameters were logarithmically transformed. No transformation was needed for the chest X-ray score [16], and all were analysed using a random intercept model based on restricted maximum likelihood (REML) estimation.
The cytokine responses were positively skewed and contained zero as values. We first added a constant 0.5 to all cytokine responses as suggested by Yamamura [22], then used a base-2 logarithmic transformation to reduce skewness. Three-level random-intercept model (time points nested in cytokines nested in patients) was fitted to account for the dependence of the cytokine responses within subject and between time points. The model included triple interaction terms between cytokines, lineages, stimulants and time points to estimate the difference in infecting lineages effect on cytokine production in blood incubated with medium alone, as well as the incremental difference in infecting lineages effect induced by each stimulant at each treatment time points. This approach did not require any background subtraction. Contrast analysis was used to estimate differences in infecting lineages effect on cytokine production with Sidak multiple comparison correction [23].
Gene expression data were available for each subject at the same time points as for the cytokines. At each time point, the effect of the four culture conditions (Medium, ESAT-6/CFP-10, live Maf and live Mtb) on the expression of 85 selected immune-related genes were assessed. Thirty (30) genes showed expression data above the cut-off value (200) for ≤1% of the patients and were discarded from the analysis to avoid inflation of the cut-off value. The remaining 55 genes were log2 transformed and analysed as described for cytokines’ data.
Predicted values of clinical outcomes, cytokines production and genes expression from the constructed model were used to study kinetics following anti-TB treatment for each group and plotted using R software. We tested for interaction between lineages and treatment time points using the Wald test. All analyses were adjusted for age, gender and ethnicity and performed using STATA 12.1 (StataCorp, USA). Statistical significance was considered at p-value ≤0.05.
Results
Study participants
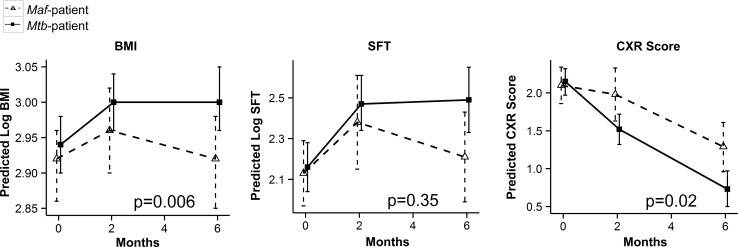
Seventy-five HIV-negative TB patients were enrolled in this study, 26 were infected with Maf-lineage 6 and 49 with Mtb-lineage 4. Before treatment, Maf- and Mtb-infected patients had similar clinical symptoms, age, sex, ethnicity, sputum smear microscopy grade and TST results (Table 1). The BMI, skinfold thickness and CXR scores were also similar in both groups at enrolment, but following treatment these were more significantly improved in Mtb- compared to Maf-infected patients post-treatment after adjusting for age, sex and ethnic group (p = 0.02, p = 0.04 and p = 0.007 respectively; Table 1). The BMI and CXR scores were significantly affected by the infecting lineages following treatment (interaction p = 0.006 and p = 0.02 respectively; Fig 1). Mean corpuscular volume (MCV) was significantly higher in Mtb- compared to Maf-infected patients before and post-treatment after adjusting for the mentioned potential confounders (p = 0.02 and p = 0.03; respectively), while all other measured haematology parameters were similar between the groups (Table 1). The monocytes/lymphocytes (M:L) ratio was similar before treatment but higher in Maf- compared to Mtb-infected patients post-treatment after adjusting for confounders (p = 0.05 respectively; Table 1).
Table 1. Demographic, clinical and haematology characteristics of M. africanum and M. tuberculosis patients.
| M. africanum | M. tuberculosis | Unadjusted | Adjusted | |||||
|---|---|---|---|---|---|---|---|---|
| n | Positive | n | Positive | ED (95%CI) | P | AED (95%CI) | P | |
| Number of cases at enrolmenta | 26 (35) | 49 (65) | ||||||
| Age in years, median (range) | 26 | 30.5 (19–66) | 49 | 27 (15–79) | 0.39 | |||
| Sex (%) (Female) | 26 | 8 (27) | 49 | 20 (38) | 0.40 | |||
| Ethnicity (%) | 26 | 49 | 0.50 | |||||
| Mandinka | 8 (27) | 23 (43) | ||||||
| Jola | 10 (33) | 5 (9) | 0.084 | |||||
| Fula | 4 (13) | 10 (19) | 0.89 | |||||
| Wolof | 3 (10) | 6 (12) | 0.79 | |||||
| Other | 5 (17) | 9 (17) | 0.89 | |||||
| Maximum smear grade (%) | 26 | 49 | 0.18 | |||||
| 1+ | 5 (19) | 3 (6) | ||||||
| 2+ | 6 (23) | 18 (37) | 0.066 | |||||
| 3+ | 15 (58) | 28 (57) | 0.16 | |||||
| TST | 13 | 12 (92) | 28 | 24 (89) | 0.40 | |||
| BMI, median (range) | ||||||||
| Enrolment | 26 | 18.6 (13–22) | 49 | 18.6 (13–32) | 0.04 (-0.04,0.12) | 0.28 | 0.04 (-0.05,0.13) | 0.39 |
| 6 months | 14 | 18.6 (17–21) | 25 | 20.2 (17–36) | 0.12 (0.04,0.2) | 0.004 | 0.11 (0.02,0.20) | 0.02 |
| Skinfold thickness median (range) in mm | ||||||||
| Enrolment | 26 | 8 (3–20) | 49 | 8 (3–20) | 0.08 (-0.08,0.25) | 0.33 | 0.03 (-0.17,0.23) | 0.76 |
| 6 months | 14 | 8.5 (3–20) | 27 | 14 (2–25) | 0.2 (0.07,0.4) | 0.006 | 0.28 (-0.01,0.55) | 0.04 |
| Chest X-Ray (Moderate & Severe Disease) | ||||||||
| Enrolment | 26 | 21 (81) | 48 | 44 (92) | 0.009 (-0.2,0.3) | 0.94 | 0.05 (-0.25,0.35) | 0.74 |
| 6 months | 11 | 7 (64) | 18 | 2 (11) | -0.55 (-0.8, -0.3) | 0.000 | -0.55 (-0.95, -0.15) | 0.007 |
| Haematology parameter median (range) | ||||||||
| Haemoglobin (mg/dL) Enrolment | 26 | 11.5 (8.7–14.6) | 43 | 10.7 (7.5–14.2) | -0.06 (0.13, -003) | 0.06 | -0.06 (-0.12, 0.01) | 0.09 |
| 6 months | 20 | 13.4 (11.5–16.8) | 30 | 13.7 (11.3–23.1) | 0.01 (-0.06, 0.08) | 0.80 | 0.01 (-0.06, 0.08) | 0.74 |
| WBC (x109/L) Enrolment | 26 | 7.2 (3.8–19.4) | 43 | 7.6 (3.6–15.3) | 0.1 (-0.06, 0.26) | 0.20 | 0.10 (-0.07, 0.26) | 0.24 |
| 6 months | 20 | 5.2 (3.2–7.8) | 30 | 4.9 (2.4–8.4) | -0.04 (-0.23, 0.14) | 0.63 | -0.05 (-0.24, 0.13) | 0.56 |
| Granulocytes (x109/L) Enrolment | 26 | 4.3 (1.2–15.8) | 43 | 5.5 (1.4–11.4) | 0.21 (-0.07, 0.49) | 0.13 | 0.19 (-0.10, 0.47) | 0.20 |
| 6 months | 20 | 3 (0.9–13.1) | 30 | 3.4 (1.4–5.7) | -0.02 (-0.33, 0.29) | 0.89 | -0.03 (-0.34, 0.29) | 0.87 |
| Lymphocytes (x109/L) Enrolment | 26 | 1.5 (0.3–8.1) | 43 | 1.7 (0.6–4.2) | 0.08 (-0.16, 0.33) | 0.50 | 0.09 (-0.17, 0.34) | 0.50 |
| 6 months | 20 | 2.8 (0.8–6.3) | 30 | 3.7 (1.6–8.6) | 0.03 (-0.25, 0.32) | 0.82 | 0.02 (-0.28, 0.31) | 0.91 |
| Monocytes (x109/L) Enrolment | 26 | 0.5 (0.3–1.4) | 43 | 0.5 (0.1–1.2) | 0.008 (-0.20, 0.21) | 0.93 | -0.004 (-0.22, 0.21) | 0.97 |
| 6 months | 20 | 0.7 (0.3–1.4) | 30 | 0.6 (0.3–1.4) | -0.20 (-0.43, 0.04) | 0.1 | -0.21 (-0.45, 0.03) | 0.08 |
| M:L ratio Enrolment | 26 | 0.31 (0.12–1.14) | 43 | 0.29 (0.06–0.87) | -0.06 (-0.30, 0.18) | 0.64 | -0.06 (-0.30, 0.19) | 0.65 |
| 6 months | 20 | 0.23 (0.11–0.62) | 30 | 0.18 (0.08–0.45) | -0.27 (-0.55, -0.001) | 0.049 | -0.27 (-0.54, 0.005) | 0.05 |
| MCV (fL) Enrolment | 25 | 77.8(59.2–92.5) | 42 | 79.6 (60.6–92.9) | 0.02 (-0.02, 0.07) | 0.29 | 0.05 (0.004, 0.09) | 0.03 |
| 6 months | 20 | 83.7 (67.6–94.8) | 30 | 85.1 (69.3–97.9) | 0.04 (-0.01, 0.08) | 0.15 | 0.06 (0.01, 0.10) | 0.02 |
| Platelets (x109/L) Enrolment | 26 | 376 (131–678) | 43 | 410 (101–663) | 0.09 (-0.08, 0.26) | 0.30 | 0.09 (-0.09, 0.26) | 0.33 |
| 6 months | 20 | 238 (161–355) | 30 | 230 (74–387) | -0.06 (-0.25, 0.13) | 0.51 | -0.07 (-0.26, 0.13) | 0.50 |
a Total number of patients recruited = 75.
Abbreviations: BMI, body mass index; CXR, chest X-ray; 1+, 2+ & 3+ = Density of Mycobacteria into patient sputum; TST: tuberculin skin test, Maf = M. africanum; Mtb = M. tuberculosis; WBC = white blood cells, MCV = mean corpuscular volume, M:L: monocytes/lymphocytes ratio, ED = Estimated Difference between Mtb vs. Maf-infected patients, AED = Adjusted ED.
Significant p-values are highlighted in bold.
Fig 1. Kinetics of the clinical outcomes in Maf- and Mtb-infected patients following treatment.
Line plots show the predicted mean and its 95% CI of Log transformed Body Mass Index (BMI) and Skinfold Thickness (SFT) in Maf- and Mtb-infected groups at 0, 2 and 6 months of treatment, Chest X-ray (CXR) was not Log transformed. Wald test through contrasts analysis following a random-intercept model adjusted for age, sex and ethnicity was used to assess interaction between lineage group and time point on clinical response. Maf group (dashed lines) and Mtb group (solid lines) respectively. P-values of the interactions are shown.
Maf- and Mtb-infected patients’ cytokine response to stimulants differs after treatment
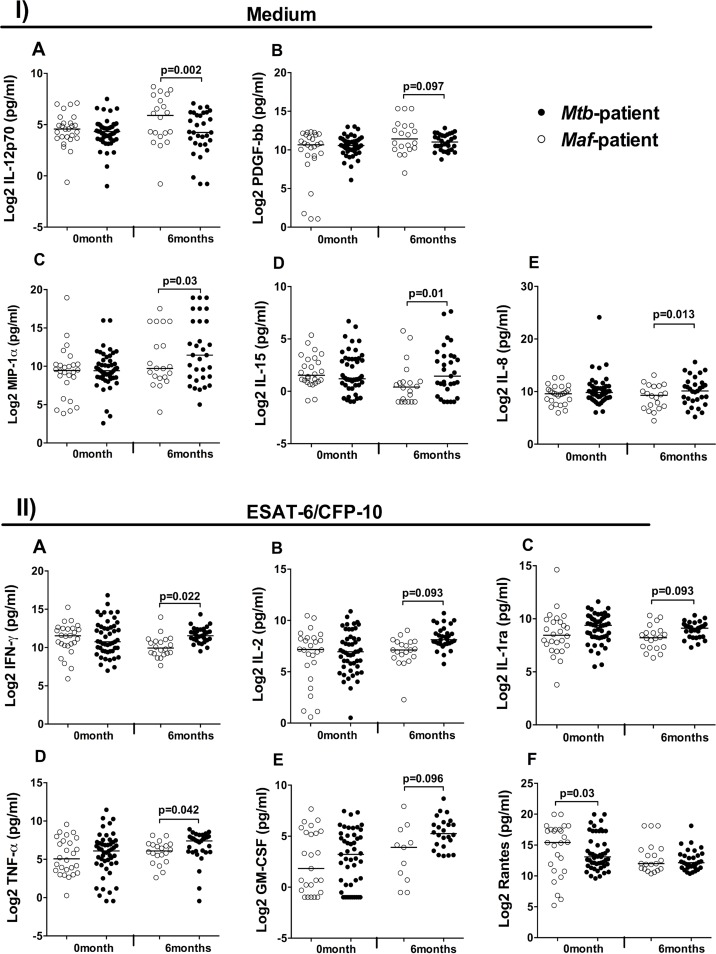
Before treatment, only stimulation with ESAT-6/CFP-10 induced a significant difference and this was seen only for RANTES (CCL5) production, which was higher in Maf- compared to Mtb-infected patients (p = 0.03; Fig 2; S1 Table). In contrast, many cytokines showed significantly different responses between Mtb- and Maf-infected patients post-treatment. In unstimulated blood supernatants, concentrations of IL-8 (p = 0.013), IL-15 (p = 0.01) and MIP-1α (p = 0.027) were significantly higher in Mtb- compared to Maf-infected patients (Fig 2; S2 Table), whereas IL-12p70 (p = 0.002) and PDGF-β (p = 0.097) were higher in Maf- compared to Mtb-infected patients. Stimulation with ESAT-6/CFP-10 induced the greatest differences in cytokines production between the two groups. IFN-γ (p = 0.022), TNF-α (p = 0.042), IL-2 (p = 0.093), IL-1ra (p = 0.093), and GM-CSF (p = 0.096) were higher in Mtb- compared to Maf-infected patients after Sidak multiple comparisons correction (Fig 2; S2 Table).
Fig 2. Differential cytokine production between Maf- and Mtb-infected patients before and after treatment.
Whole blood incubated overnight with medium only (I), revealed differences in the concentrations of IL12p70 (A), PDGF-ββ (B), MIP-1α (C), IL-15 (D) and IL-8 (E) between Mtb- and Maf-infected patients at 6 month of treatment. (II) Only ESAT-6/CFP-10 stimulation induced significant differences in cytokine production between Mtb- and Maf-infected patients above the background level of IFN-γ (A), IL-2 (B), IL-1ra (C), TNF-α (D), GM-CSF (E) and Rantes (F). Dot plots show log-2 transformed cytokine concentrations measured with Bio-Plex assay. Horizontal bars indicate median cytokine concentration by lineage groups, Maf-infected patients (closed circles, n = 26 and 20) and Mtb-infected patients (open circles, n = 49 and 31) respectively at 0 and 6 months of TB treatment. Log-2 transformed cytokine concentrations were compared between lineage groups using a random-intercept model adjusted for age, sex and ethnicity, and Sidak multiple comparison correction. Contrasts analysis was used after estimation to compute the difference in each cytokine concentration between lineage groups and used Wald test for assessing the significance at each time point. P-values of the differences are shown.
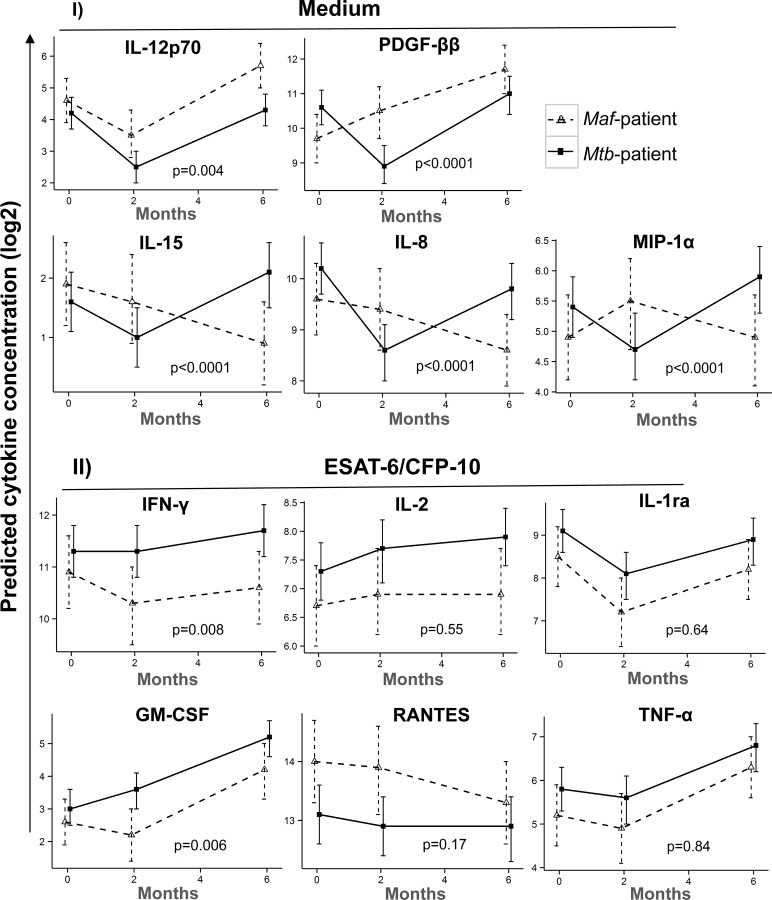
Kinetics of specific cytokines production following treatment of Mtb- and Maf-infected patients
The kinetics of differentially produced cytokines between the groups was assessed in order to understand the effect of treatment on cytokine responses in each group. In the unstimulated samples, the patterns of IL-12p70 and IL-15 were similar at 2 months, but differed significantly at 6 months of treatment, whereas those of IL-8, MIP-1α and PDGF-ββ differed already at 2 months of treatment between the groups (interaction p<0.001; Fig 3A). In response to ESAT-6/CFP-10 stimulation, the patterns of IFN-γ and GM-CSF were significantly different between the groups at 2 months of treatment (interaction p<0.01; Fig 3B).
Fig 3. Kinetics of cytokines production between Maf- and Mtb-infected groups following treatment.
The kinetics of cytokine expression showing either strong or weak evidence of difference between lineage groups following overnight incubation with Medium alone (I) or ESAT-6/CFP-10 (II). Line plots show the predicted mean and its 95% confidence interval (95% CI) of log-2 transformed cytokines concentration in Maf- and Mtb-infected groups at 0, 2 and 6 months of treatment. Wald test through contrasts analysis following a random-intercept model adjusted for age, sex and ethnicity was used to assess interaction between lineage group and time point on cytokine production. The legend shows Maf-infected group (dashed lines) and Mtb-infected group (solid lines) respectively. P-values of the interactions are shown.
Differences in gene expression profiles between Maf- and Mtb-infected patients following treatment
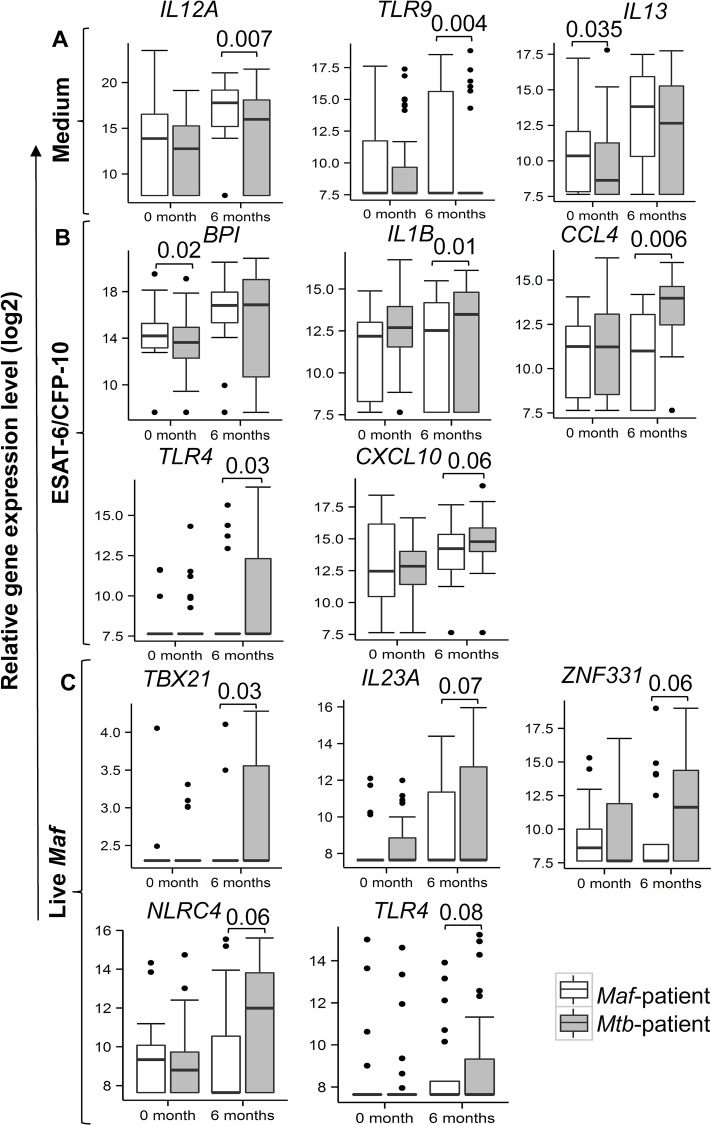
Prior to treatment, there were significantly higher expression of IL13 in unstimulated (p = 0.035), and BPI in ESAT-6/CFP-10 stimulated (p = 0.02) whole blood samples in Maf- compared to Mtb-infected patients (Fig 4, S3 Table). Likewise, post-treatment, TLR9 and IL12A expression were significantly higher in Maf- compared to Mtb-infected patients in the unstimulated whole blood (p = 0.004 and p = 0.007 respectively; Fig 4, S4 Table). ESAT-6/CFP-10 stimulation induced significantly higher expression of IL1B (p = 0.01), CCL4 (p = 0.006), TLR4 (p = 0.03) and CXCL10 (p = 0.06) in Mtb- compared to Maf-infected patients. Furthermore, stimulation with live Maf induced higher expression of TBX21 (p = 0.03), NLRC4 (p = 0.06), ZNF331 (p = 0.06), IL23A (p = 0.07) and TLR4 (p = 0.08) in Mtb- than Maf-infected patients (Fig 4, S4 Table).
Fig 4. Gene expression profiles differ between Maf- and Mtb-infected patients before and after treatment.
dcRT-MLPA was performed on RNA extracted from whole blood incubated overnight with medium only (A), ESAT-6/CFP-10 (B) and live Maf (C). Median gene expression levels (peak areas normalized to GAPDH and log2 transformed) of the indicated genes are shown in box-and-whisker plots. Equal number of samples were analysed at 0 and 6 months of treatment in each group of Maf-infected (n = 20; white boxes) and Mtb-infected (n = 31; grey boxes) patients, respectively. Log-2 transformed gene expression data were compared between the groups using contrast analysis following a random-intercept model adjusted for age, sex and ethnicity, and Sidak multiple comparison correction. Wald test was used to assess the significance at each time point. P-values of significant differences are shown.
Kinetics of gene expression in Maf- and Mtb-infected patients following treatment
In unstimulated whole blood, the patterns of TLR9 and IL12A expression were significantly different between Maf and Mtb-infected patients at 2 months of treatment (interaction p = 0.004 and p = 0.0005 respectively; Fig 5A). In ESAT-6/CFP-10 stimulated whole blood, the kinetics of CXCL10 expression differed between the groups at 2 months of treatment (interaction p = 0.04; Fig 5B), while following live Maf stimulation, the kinetics of NLRC4 expression was significantly different at 2 month of treatment between the groups (interaction p = 0.0007; Fig 5C).
Fig 5. Kinetics of gene expression in Maf- and Mtb-infected groups following treatment.
The expression kinetics of genes that showed significant differences between Maf- and Mtb-infected groups following overnight incubation with Medium alone (A), ESAT-6/CFP-10 (B) and live Maf (C). Line plots show the predicted mean and its 95% CI of log2 transformed gene expression levels in Maf- and Mtb-infected groups at 0, 2 and 6 months of treatment. Wald test through contrasts analysis following a random-intercept model adjusted for age, sex and ethnicity was used to assess interaction between lineage group and time point on gene expression. The legend shows Maf-infected group (dashed lines) and Mtb-infected group (solid lines) respectively. P-values of the interactions are shown.
Interactions of cytokines and genes differentially expressed between Maf- and Mtb-infected patients
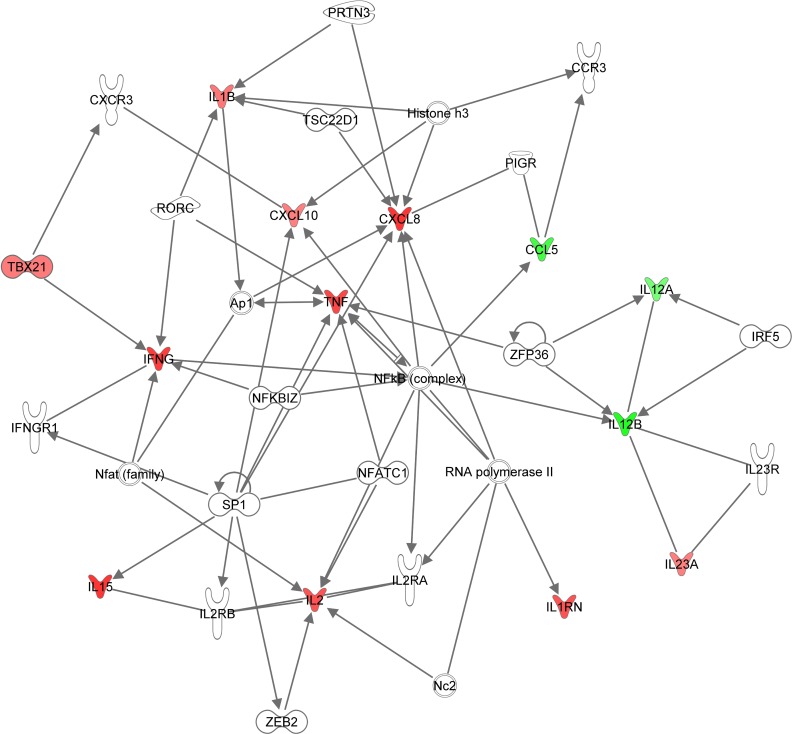
The direct relationship among the 23 cytokines and genes differentially expressed between the Maf and Mtb-infected patients was analysed using the Ingenuity Pathway Analysis (IPA, QIAGEN Redwood City, USA, www.qiagen.com/ingenuity). Ingenuity canonical pathway analysis identified a high enrichment in the communication between innate and adaptive immune cells. Analysis of the upstream regulators revealed a very high enrichment (p = 6.6 x 10−21) of the nuclear factor NF-kappa-B p65 subunit (RELA) that regulates more than half (n = 12) of the differentially expressed cytokines and genes between Maf- and Mtb-infected patients post-treatment. Interestingly, all the cytokines fitted into 2 network functions with the top one containing 13 of the 23 markers and centred on the NFκB complex (Fig 6).
Fig 6. Ingenuity network of direct relationship among genes and cytokines differentially expressed between Maf- and Mtb-infected patients.
Ingenuity network showing 13 of the 23 pro-inflammatory cytokines and genes that were differentially expressed between Maf- and Mtb- infected patients, centred on NF-κ complex. Genes or cytokines that were higher in Mtb- compared to Maf- infected patients are depicted in red, those that were lower in green.
Discussion
We report here a comparison of clinical and immunological responses before and following standard anti-TB treatment between TB patients infected by Maf and Mtb lineages of the MTBC in The Gambia. We used an unbiased rigorous statistical approach that accounted for both intra and inter patient’s group variation, experimental condition variability, repeated measurement over time and corrected for multiple comparison to identify biomarkers that are associated with MTBC lineage-specific pathogenesis and response to anti-TB treatment. Overall, before treatment there were no differences in clinical parameters and differences in very few cytokine concentrations and gene expression profiles between Maf- and Mtb-infected patients. However, after treatment the BMI, CXR, skinfold thickness and immunological responses were more significantly improved in Mtb- than in Maf-infected patients.
The high similarity in the peripheral blood cells populations, clinical presentation, cytokines production and genes expression profiles before treatment between Maf- and Mtb-infected patients further support uniformity in host responses after succumbing to infection, irrespective of the infecting lineage of MTBC as previously reported [13,15]. This result also suggests that Maf and Mtb lineages differences may not affect diagnosis of active TB based on the measurement of soluble cytokines.
The pattern of the changes after treatment are indicative of a quicker recovery from disease in Mtb-infected patients, which might be due to their stronger host immunity and/or a better immediate response to treatment of the Mtb-lineage 4 [10]. In contrast, the poorer improvement in the clinical outcome following treatment of Maf-infected patients could be related to the immune profile. Higher ratio of monocytes/lymphocytes following treatment has been attributed to unresolved infection with on-going inflammation [24]. The high IL-12p70 production in Maf-patients correlates with the higher expression of IL12A gene, which encodes IL-12p35, a subunit of IL-12p70 produced by macrophages to induce production of inflammatory cytokines from T helper-1 (Th1) and Th17 cells [25,26]. In addition, the increased TLR9 expression also induces IL-12 production [27] that will further promote prolonged inflammatory processes, which could lead to poor weight gain [28,29] as seen in our Maf-infected patients.
IL-15 is a pleiotropic cytokine produced mainly by macrophages, activates a broad range of cells including T and NK cells [30], and promotes the survival of BALB/c mice infected with Mtb [31]. Increased MIP-1α levels in unstimulated plasma of HIV-negative TB patients were associated with favourable treatment outcomes [32]. Therefore, the increased IL-15 and MIP-1α in Mtb-infected patient after 2 months of treatment could reflect a better response to treatment in contrast to the Maf-infected patients.
The significantly higher CCL5 (RANTES) level and IL13 and BPI expression in Maf- compared to Mtb-infected patients before treatment was not seen post-treatment, implying that treatment did not amplify the differences in the markers already detected pre-treatment but rather revealed new markers. Abundance of IL13 has predicted progression to active tuberculosis disease in high-risk groups [33], suggesting higher susceptibility as well as a lower ability to mount adequate immune response to recover from disease in our Maf-infected patients. This is in line with our previous report of immune exhaustion, and higher prevalence among HIV-positive, severely malnourished and older individuals, of Maf-infected patients [1,15,16,34,35], implying that Maf mainly causes diseases in a permissive host environment.
ESAT-6/CFP-10 stimulation induced the greatest differences in cytokines concentration and genes expressed between the groups post-treatment. These were mainly pro-inflammatory markers that have previously been associated with protection, such as IFN-γ, and were all significantly higher in Mtb- than Maf-infected patients. This suggests that the immune system of Mtb-infected patients were more capable of mounting a robust response to ESAT-6/CFP-10 on recovering following anti-TB treatment as previously described [15,36,37]. However, other studies have reported the opposite [38,39]. Lower cytokine response post-treatment in Maf-infected patients may reflect a poor immune recovery due to an ineffective response to treatment in this group, or a pre-TB immune suppressed state. This is further supported by a generally lower cytokine profile in response to all stimulants in this study, as well as corroborates with the previous finding of increased proportion of HIV-infected amongst patients with Maf-caused tuberculosis [34].
The enrichment of NF-κB activation-related genes among the differentially expressed biomarkers between the groups post-treatment is similar to previous reports [40,41]. NF-κB is a key nuclear transcription factor of pro-inflammatory genes activation [41], which corroborates our identified cytokines. We have previously reported high enrichment of HNF4-α, which regulated about 15% of all genes differentially expressed between Maf- and Mtb-infected patients post-treatment [13]. Low HNF4-α expression has been associated with worst prognosis of hepatocellular carcinoma (HCC) through a robust activation of RELA, whereas higher HNF4-α expression inhibited NF-κB expression and improved HCC outcome [42]. The enrichment of HNF4-α and NF-κB in our datasets is very interesting. Although we cannot yet establish a direct connection based on our current data, this might suggests that the dampened Maf-infected patient’s pro-inflammatory response to antigen stimulation post-treatment occurs through the inhibition of NF-κB pathway.
Our study was nested within a platform that has a commendable record of treatment monitoring and completion. [43]. Although both Mtb and Maf-infected patients had negative smears for AFB by the end of the follow up, differences may not have been observed due to poor sensitivity of the microscopy method used [44]. The more sensitive culture conversion method is not used to monitor treatment in The Gambia and was therefore not used in our study. In addition, although the drug resistance profile of the infecting organisms was not tested, The Gambia has a very low prevalence of TB drug resistance determined in the last survey performed in 2003 [45]. It is therefore unlikely that the different immune profiles observed post-treatment between the groups was due to drug resistance. Moreover, previous studies from West Africa showed that Maf is less likely to develop drug resistance compared to Mtb [46–48]. However, future studies should include systematic mycobacterial culture to monitor anti-TB treatment response and mycobacterial drug susceptibility testing in order to strengthen this evidence.
There was a striking similarity in the kinetics of cytokines and genes expression between Mtb- and Maf-infected patients during the first two months, but significant differences at 6 months of treatment. These together with the clinical responses provide a coherent and robust evidence of differential responses to treatment in Maf- and Mtb-infected patients. This pattern may indicate that the interval for differences to emerge between the groups by 2 months was short and the difference at 6 month of treatment may reflect a slower rate of clinical and immunological disease resolution of Maf-infected TB patients. The fact that most differences between the two groups only emerge after 2 months of treatment suggest that Maf-infected patient may require longer intensive treatment phase, a longer treatment regimen overall, or reveals the pre-TB disease immune profile of the individuals. These results suggest that Maf leaves a permissive host profiles after treatment with poor lung function and health quality in general, which might promotes the susceptibility to future disease. It becomes important to investigate Maf-infected patients long-term recovery post-treatment and their risk of relapse or re-infection as a permissive host immunity could favour TB disease from Maf, which remains a less virulent bacillus [49] but yet has not been outcompeted by other Mtb lineages according to recent report in West Africa [35,48,50–56]. Moreover, Maf causes up to half of all tuberculosis cases in West Africa where the same treatment regimen is given irrespective of the infecting MTBC lineage. New host-directed therapeutic approaches that aim to reduce inflammatory responses associated with immunopathology might be proven useful for these patients [57,58]. Furthermore, these results demonstrate that the identification and evaluation of immunological biomarkers to monitor anti-tuberculosis treatment response in West Africa should consider the diversity of MTBC lineages.
Studies in Maf non-endemic regions have shown heterogeneous response to TB treatment depending on the infecting MTBC lineages [6,10,59]. However, other studies in highly heterogeneous populations found no effect of MTBC lineages, but rather patient ethnicity was a significant determinant for difference in treatment response [9,11]. Clearly, host and bacteria factors are important determinants for treatment response, therefore stratified approaches to TB treatment that account for MTBC lineages is required to improve treatment outcome especially now with clinical trials of shorter drug treatment regimen for TB [14,60].
In conclusion, our data show differences in clinical parameters and immune genes and proteins associated with inflammatory processes recovery between Mtb- and Maf-infected patients following anti-tuberculosis treatment. This profile may be an indication of differences in the resolution of disease or the pre-tuberculosis status of the host immune system. These findings may have public health relevance for therapeutic and biomarker discovery purposes, and warrant further investigation for the use of the identified biomarkers as potential targets for preventive or therapeutic intervention against tuberculosis.
Supporting Information
List of pages and paragraphs containing keys information about this study. The pages and paragraphs numbers responding to the specific questions of the STROBE Checklist are provided to ease the reading of this manuscript and understanding the study.
(DOC)
Show the Estimated Difference (ED) of cytokines production in blood incubated with Medium only and the Estimated Incremental Difference (EID) of cytokines production above the baseline induced by the respective stimulants between Mtb and Maf-infected patients before treatment. The statistical analyses were done using a random intercept model based on restricted maximum likelihood (REML) and adjusted for age, gender and ethnicity as well as applying Sidak multiple comparison correction. Statistical significant ED and EID are highlighted in bold.
(DOCX)
Show the Estimated Difference (ED) of cytokines production in blood incubated with Medium only and the Estimated Incremental Difference (EID) of cytokines production above the baseline induced by the respective stimulants between Mtb and Maf-infected patients at 6 months of treatment. The statistical analyses were done using a random intercept model based on restricted maximum likelihood (REML) and adjusted for age, gender and ethnicity as well as applying Sidak multiple comparison correction. Statistical significant ED and EID are highlighted in bold.
(DOCX)
Show the Estimated Difference (ED) of genes expression in blood incubated with Medium only and the Estimated Incremental Difference (EID) of genes expression above the baseline induced by the respective stimulants between Mtb and Maf-infected patients before treatment. The statistical analyses were done using a random intercept model based on restricted maximum likelihood (REML) and adjusted for age, gender and ethnicity as well as applying Sidak multiple comparison correction. Statistical significant ED and EID are highlighted in bold.
(XLSX)
Show the Estimated Difference (ED) of genes expression in blood incubated with Medium only and the Estimated Incremental Difference (EID) of genes expression above the baseline induced by the respective stimulants between Mtb and Maf-infected patients at 6 months of treatment. The statistical analyses were done using a random intercept model based on restricted maximum likelihood (REML) and adjusted for age, gender and ethnicity as well as applying Sidak multiple comparison correction. Statistical significant ED and EID are highlighted in bold.
(XLSX)
Acknowledgments
We thank the Gambian National Leprosy and Tuberculosis Programme for their continuing collaboration. We are also grateful to study participants, field workers, especially K Kanyi, M. Davies and O Ceesay for performing sample collection, MRC TB clinical staff and P Camara for obtaining consent and enrolling participants, TB immunology and TB diagnostic laboratory staff, and P Owiafe, A Bojang, J Mendy, J Otu and F Mendy for laboratory assistance. We also thank T Togun for clinical examination of some study patients.
Data Availability
Our data are from study patients and are sensitive to disclosure therefore cannot be made publicly available according to the MRC/LSHTM ethic policy. However, the anonymised data is available to share upon request to the MRC Unit the Gambia under the supervision of the Head of Data Management and Archives Mr. Bai Lamin Dondeh who is not an author on our manuscript. To have the data, please email our e-data repository (edatarepository@mrc.gm), which is widely accessible by our data management and archives staffs who will rapidly reply to any request.
Funding Statement
The study was funded by the MRC Unit, The Gambia as a PhD fellowship awarded to LDT. Financial support for these studies was obtained from projects EC FP7 IDEA, EC FP7 ADITEC, EC FP7 NEWTBVAC and EC HOR2020 TBVAC2020. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.de Jong BC, Antonio M, Gagneux S. Mycobacterium africanum-review of an important cause of human tuberculosis in West Africa. PLoS Negl Trop Dis. 2010; 4(9):e744 10.1371/journal.pntd.0000744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gagneux S. Host-pathogen coevolution in human tuberculosis. Philosophical transactions of the Royal Society of London Series B, Biological sciences. 2012; 367(1590):850–9. 10.1098/rstb.2011.0316 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bloom CI, Graham CM, Berry MP, Wilkinson KA, Oni T, Rozakeas F, et al. Detectable changes in the blood transcriptome are present after two weeks of antituberculosis therapy. PLoS One. 2012; 7(10):e46191 10.1371/journal.pone.0046191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cliff JM, Lee JS, Constantinou N, Cho JE, Clark TG, Ronacher K, et al. Distinct phases of blood gene expression pattern through tuberculosis treatment reflect modulation of the humoral immune response. J Infect Dis. 2013; 207(1):18–29. 10.1093/infdis/jis499 [DOI] [PubMed] [Google Scholar]
- 5.Cliff JM, Kaufmann SH, McShane H, van Helden P, O'Garra A. The human immune response to tuberculosis and its treatment: a view from the blood. Immunol Rev. 2015; 264(1):88–102. 10.1111/imr.12269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Click ES, Winston CA, Oeltmann JE, Moonan PK, Mac Kenzie WR. Association between Mycobacterium tuberculosis lineage and time to sputum culture conversion. Int J Tuberc Lung Dis. 2013; 17(7):878–84. 10.5588/ijtld.12.0732 . [DOI] [PubMed] [Google Scholar]
- 7.Coscolla M, Gagneux S. Consequences of genomic diversity in Mycobacterium tuberculosis. Seminars in immunology. 2014; 26(6):431–44. 10.1016/j.smim.2014.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gumbo T. Biological variability and the emergence of multidrug-resistant tuberculosis. Nat Genet. 2013; 45(7):720–1. 10.1038/ng.2675 [DOI] [PubMed] [Google Scholar]
- 9.Coussens AK, Wilkinson RJ, Nikolayevskyy V, Elkington PT, Hanifa Y, Islam K, et al. Ethnic variation in inflammatory profile in tuberculosis. PLoS Pathog. 2013; 9(7):e1003468 10.1371/journal.ppat.1003468 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford CB, Shah RR, Maeda MK, Gagneux S, Murray MB, Cohen T, et al. Mycobacterium tuberculosis mutation rate estimates from different lineages predict substantial differences in the emergence of drug-resistant tuberculosis. Nat Genet. 2013; 45(7):784–90. 10.1038/ng.2656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pareek M, Evans J, Innes J, Smith G, Hingley-Wilson S, Lougheed KE, et al. Ethnicity and mycobacterial lineage as determinants of tuberculosis disease phenotype. Thorax. 2013; 68(3):221–9. 10.1136/thoraxjnl-2012-201824 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nahid P, Bliven EE, Kim EY, Mac Kenzie WR, Stout JE, Diem L, et al. Influence of M. tuberculosis lineage variability within a clinical trial for pulmonary tuberculosis. PLoS One. 2010; 5(5):e10753 10.1371/journal.pone.0010753 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tientcheu LD, Maertzdorf J, Weiner J, Adetifa IM, Mollenkopf HJ, Sutherland JS, et al. Differential transcriptomic and metabolic profiles of M. africanum- and M. tuberculosis-infected patients after, but not before, drug treatment. Genes Immun. 2015; 16(5):347–55. 10.1038/gene.2015.21 ; [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merle CS, Fielding K, Sow OB, Gninafon M, Lo MB, Mthiyane T, et al. A four-month gatifloxacin-containing regimen for treating tuberculosis. N Engl J Med. 2014; 371(17):1588–98. 10.1056/NEJMoa1315817 . [DOI] [PubMed] [Google Scholar]
- 15.Tientcheu LD, Sutherland JS, de Jong BC, Kampmann B, Jafali J, Adetifa IM, et al. Differences in T-cell responses between Mycobacterium tuberculosis and Mycobacterium africanum-infected patients. Eur J Immunol. 2014; 44(5):1387–98. 10.1002/eji.201343956 . [DOI] [PubMed] [Google Scholar]
- 16.de Jong BC, Hill PC, Aiken A, Jeffries DJ, Onipede A, Small PM, et al. Clinical presentation and outcome of tuberculosis patients infected by M. africanum versus M. tuberculosis. Int J Tuberc Lung Dis. 2007; 11(4):450–6. . [PubMed] [Google Scholar]
- 17.de Jong BC, Antonio M, Awine T, Ogungbemi K, de Jong YP, Gagneux S, et al. Use of spoligotyping and large sequence polymorphisms to study the population structure of the Mycobacterium tuberculosis complex in a cohort study of consecutive smear-positive tuberculosis cases in The Gambia. J Clin Microbiol. 2009; 47(4):994–1001. 10.1128/JCM.01216-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.WHO. Treatment of tuberculosis GUIDELINES Fourth edition World Health Organisation. 2010. http://apps.who.int/iris/bitstream/10665/44165/1/9789241547833_eng.pdf [PubMed]
- 19.Galagan JE, Sisk P, Stolte C, Weiner B, Koehrsen M, Wymore F, et al. TB database 2010: overview and update. Tuberculosis (Edinb). 2010; 90(4):225–35. . [DOI] [PubMed] [Google Scholar]
- 20.Joosten SA, Goeman JJ, Sutherland JS, Opmeer L, de Boer KG, Jacobsen M, et al. Identification of biomarkers for tuberculosis disease using a novel dual-color RT-MLPA assay. Genes Immun. 2012; 13(1):71–82. 10.1038/gene.2011.64 . [DOI] [PubMed] [Google Scholar]
- 21.Satti L, Ikram A, Abbasi S, Malik N, Mirza IA, Martin A. Evaluation of thin-layer agar 7H11 for the isolation of Mycobacterium tuberculosis complex. Int J Tuberc Lung Dis. 2010; 14(10):1354–6. . [PubMed] [Google Scholar]
- 22.Reuter MA, Pecora ND, Harding CV, Canaday DH, McDonald D. Mycobacterium tuberculosis promotes HIV trans-infection and suppresses major histocompatibility complex class II antigen processing by dendritic cells. J Virol. 2010; 84(17):8549–60. 10.1128/JVI.02303-09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sidak Z. Rectangular confidence regions for the means of multivariate normal distributions. J Amer Stat Assoc 1967; 62:626–33. [Google Scholar]
- 24.Wang J, Yin Y, Wang X, Pei H, Kuai S, Gu L, et al. Ratio of monocytes to lymphocytes in peripheral blood in patients diagnosed with active tuberculosis. Braz J Infect Dis. 2015; 19(2):125–31. 10.1016/j.bjid.2014.10.008 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Khader SA, Pearl JE, Sakamoto K, Gilmartin L, Bell GK, Jelley-Gibbs DM, et al. IL-23 compensates for the absence of IL-12p70 and is essential for the IL-17 response during tuberculosis but is dispensable for protection and antigen-specific IFN-gamma responses if IL-12p70 is available. J Immunol. 2005; 175(2):788–95. 175/2/788 [pii]. . [DOI] [PubMed] [Google Scholar]
- 26.Kay MK, Linke L, Triantis J, Salman MD, Larsen RS. Evaluation of DNA extraction techniques for detecting Mycobacterium tuberculosis complex organisms in Asian elephant trunk wash samples. J Clin Microbiol. 2011; 49(2):618–23. 10.1128/JCM.00807-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bafica A, Scanga CA, Feng CG, Leifer C, Cheever A, Sher A. TLR9 regulates Th1 responses and cooperates with TLR2 in mediating optimal resistance to Mycobacterium tuberculosis. J Exp Med. 2005; 202(12):1715–24. 10.1084/jem.20051782 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.O'Sullivan DM, McHugh TD, Gillespie SH. Mapping the fitness of Mycobacterium tuberculosis strains: a complex picture. J Med Microbiol. 2010; 59(12):1533–5. [DOI] [PubMed] [Google Scholar]
- 29.Yu CC, Chang CY, Liu CE, Shih LF, Hsiao JH, Chen CH. Drug resistance pattern of Mycobacterium tuberculosis complex at a medical center in central Taiwan, 2003–2007. J Microbiol Immunol Infect. 2010; 43(4):285–90. 10.1016/S1684-1182(10)60045-X . [DOI] [PubMed] [Google Scholar]
- 30.Umemura M, Nishimura H, Hirose K, Matsuguchi T, Yoshikai Y. Overexpression of IL-15 in vivo enhances protection against Mycobacterium bovis bacillus Calmette-Guerin infection via augmentation of NK and T cytotoxic 1 responses. J Immunol. 2001; 167(2):946–56. . [DOI] [PubMed] [Google Scholar]
- 31.Maeurer MJ, Trinder P, Hommel G, Walter W, Freitag K, Atkins D, et al. Interleukin-7 or interleukin-15 enhances survival of Mycobacterium tuberculosis-infected mice. Infect Immun. 2000; 68(5):2962–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mihret A, Abebe M, Bekele Y, Aseffa A, Walzl G, Howe R. Impact of HIV co-infection on plasma level of cytokines and chemokines of pulmonary tuberculosis patients. BMC Infect Dis. 2014; 14:125 10.1186/1471-2334-14-125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shakoor S, Ahsan T, Jabeen K, Raza M, Hasan R. Use of p-nitrobenzoic acid in 7H10 agar for identification of Mycobacterium tuberculosis complex: a field study. Int J Tuberc Lung Dis. 2010; 14(12):1644–6. . [PubMed] [Google Scholar]
- 34.de Jong BC, Hill PC, Brookes RH, Otu JK, Peterson KL, Small PM, et al. Mycobacterium africanum: a new opportunistic pathogen in HIV infection? AIDS. 2005;19(15):1714–5. 00002030-200510140-00030. . [DOI] [PubMed] [Google Scholar]
- 35.de Jong BC, Adetifa I, Walther B, Hill PC, Antonio M, Ota M, et al. Differences between tuberculosis cases infected with Mycobacterium africanum, West African type 2, relative to Euro-American Mycobacterium tuberculosis: an update. FEMS Immunol Med Microbiol. 2010; 58(1):102–5. 10.1111/j.1574-695X.2009.00628.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jackson-Sillah D, Cliff JM, Mensah GI, Dickson E, Sowah S, Tetteh JK, et al. Recombinant ESAT-6-CFP10 Fusion Protein Induction of Th1/Th2 Cytokines and FoxP3 Expressing Treg Cells in Pulmonary TB. PLoS One. 2013; 8(6):e68121 10.1371/journal.pone.0068121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Mensah GI, Addo KK, Tetteh JA, Sowah S, Loescher T, Geldmacher C, et al. Cytokine response to selected MTB antigens in Ghanaian TB patients, before and at 2 weeks of anti-TB therapy is characterized by high expression of IFN-gamma and Granzyme B and inter- individual variation. BMC Infect Dis. 2014; 14:495 10.1186/1471-2334-14-495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mattos AM, Almeida Cde S, Franken KL, Alves CC, Abramo C, de Souza MA, et al. Increased IgG1, IFN-gamma, TNF-alpha and IL-6 responses to Mycobacterium tuberculosis antigens in patients with tuberculosis are lower after chemotherapy. Int Immunol. 2010;22(9):775–82. 10.1093/intimm/dxq429 [DOI] [PubMed] [Google Scholar]
- 39.Kaneko Y, Nakayama K, Kinoshita A, Kurita Y, Odashima K, Saito Z, et al. Relation between recurrence of tuberculosis and transitional changes in IFN-gamma release assays. Am J Respir Crit Care Med. 2015; 191(4):480–3. 10.1164/rccm.201409-1590LE . [DOI] [PubMed] [Google Scholar]
- 40.Kaewseekhao B, Naranbhai V, Roytrakul S, Namwat W, Paemanee A, Lulitanond V, et al. Comparative Proteomics of Activated THP-1 Cells Infected with Mycobacterium tuberculosis Identifies Putative Clearance Biomarkers for Tuberculosis Treatment. PLoS One. 2015; 10(7):e0134168 10.1371/journal.pone.0134168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Huang KH, Wang CH, Lin CH, Kuo HP. NF-kappaB repressing factor downregulates basal expression and Mycobacterium tuberculosis induced IP-10 and IL-8 synthesis via interference with NF-kappaB in monocytes. Journal of biomedical science. 2014; 21:71 10.1186/s12929-014-0071-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ning BF, Ding J, Liu J, Yin C, Xu WP, Cong WM, et al. Hepatocyte nuclear factor 4alpha-nuclear factor-kappaB feedback circuit modulates liver cancer progression. Hepatology. 2014. 10.1002/hep.27177 . [DOI] [PubMed] [Google Scholar]
- 43.WHO. Global Tuberculosis Report 2015. World Health Organization; 2015;20th Edition http://apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf [Google Scholar]
- 44.Horne DJ, Royce SE, Gooze L, Narita M, Hopewell PC, Nahid P, et al. Sputum monitoring during tuberculosis treatment for predicting outcome: systematic review and meta-analysis. Lancet Infect Dis. 2010; 10(6):387–94. 10.1016/S1473-3099(10)70071-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Adegbola RA, Hill P, Baldeh I, Otu J, Sarr R, Sillah J, et al. Surveillance of drug-resistant Mycobacterium tuberculosis in The Gambia. Int J Tuberc Lung Dis. 2003; 7(4):390–3. [PubMed] [Google Scholar]
- 46.Yeboah-Manu D, Asante-Poku A, Bodmer T, Stucki D, Koram K, Bonsu F, et al. Genotypic diversity and drug susceptibility patterns among M. tuberculosis complex isolates from South-Western Ghana. PLoS One. 2011; 6(7):e21906 10.1371/journal.pone.0021906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Traore B, Diarra B, Dembele BP, Somboro AM, Hammond AS, Siddiqui S, et al. Molecular strain typing of Mycobacterium tuberculosis complex in Bamako, Mali. Int J Tuberc Lung Dis. 2012; 16(7):911–6. 10.5588/ijtld.11.0397 [DOI] [PubMed] [Google Scholar]
- 48.Winglee K, Manson McGuire A, Maiga M, Abeel T, Shea T, Desjardins CA, et al. Whole Genome Sequencing of Mycobacterium africanum Strains from Mali Provides Insights into the Mechanisms of Geographic Restriction. PLoS Negl Trop Dis. 2016; 10(1):e0004332 10.1371/journal.pntd.0004332 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Via LE, Weiner DM, Schimel D, Lin PL, Dayao E, Tankersley SL, et al. Differential virulence and disease progression following Mycobacterium tuberculosis complex infection of the common marmoset (Callithrix jacchus). Infect Immun. 2013; 81(8):2909–19. 10.1128/IAI.00632-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Lawson L, Zhang J, Gomgnimbou MK, Abdurrahman ST, Le Moullec S, Mohamed F, et al. A molecular epidemiological and genetic diversity study of tuberculosis in Ibadan, Nnewi and Abuja, Nigeria. PLoS One. 2012; 7(6):e38409 10.1371/journal.pone.0038409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Asante-Poku A, Yeboah-Manu D, Otchere ID, Aboagye SY, Stucki D, Hattendorf J, et al. Mycobacterium africanum Is Associated with Patient Ethnicity in Ghana. PLoS Negl Trop Dis. 2015; 9(1):e3370 10.1371/journal.pntd.0003370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gomgnimbou MK, Refregier G, Diagbouga SP, Adama S, Kabore A, Ouiminga A, et al. Spoligotyping of Mycobacterium africanum, Burkina Faso. Emerg Infect Dis. 2012; 18(1):117–9. 10.3201/eid1801.110275 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Thumamo BP, Asuquo AE, Abia-Bassey LN, Lawson L, Hill V, Zozio T, et al. Molecular epidemiology and genetic diversity of Mycobacterium tuberculosis complex in the Cross River State, Nigeria. Infect Genet Evol. 2012; 12(4):671–7. 10.1016/j.meegid.2011.08.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Affolabi D, Anyo G, Faihun F, Sanoussi N, Shamputa IC, Rigouts L, et al. First molecular epidemiological study of tuberculosis in Benin. Int J Tuberc Lung Dis. 2009; 13(3):317–22. [PubMed] [Google Scholar]
- 55.Gehre F, Antonio M, Faihun F, Odoun M, Uwizeye C, de Rijk P, et al. The first phylogeographic population structure and analysis of transmission dynamics of M. africanum West African 1-combining molecular data from Benin, Nigeria and Sierra Leone. PLoS One. 2013; 8(10):e77000 10.1371/journal.pone.0077000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gehre F, Kumar S, Kendall L, Ejo M, Secka O, Ofori-Anyinam B, et al. A Mycobacterial Perspective on Tuberculosis in West Africa: Significant Geographical Variation of M. africanum and Other M. tuberculosis Complex Lineages. PLoS Negl Trop Dis. 2016; 10(3):e0004408 PMCID: 4786107. 10.1371/journal.pntd.0004408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Zumla A, Maeurer M, Host-Directed Therapies N, Chakaya J, Hoelscher M, Ntoumi F, et al. Towards host-directed therapies for tuberculosis. Nature reviews Drug discovery. 2015; 14(8):511–2. 10.1038/nrd4696 . [DOI] [PubMed] [Google Scholar]
- 58.Zumla A, Rao M, Wallis RS, Kaufmann SH, Rustomjee R, Mwaba P, et al. Host-directed therapies for infectious diseases: current status, recent progress, and future prospects. Lancet Infect Dis. 2016; 16(4):e47–63. 10.1016/S1473-3099(16)00078-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Click ES, Moonan PK, Winston CA, Cowan LS, Oeltmann JE. Relationship between Mycobacterium tuberculosis phylogenetic lineage and clinical site of tuberculosis. Clin Infect Dis. 2012; 54(2):211–9. 10.1093/cid/cir788 [DOI] [PubMed] [Google Scholar]
- 60.Gillespie SH, Crook AM, McHugh TD, Mendel CM, Meredith SK, Murray SR, et al. Four-month moxifloxacin-based regimens for drug-sensitive tuberculosis. N Engl J Med. 2014; 371(17):1577–87. 10.1056/NEJMoa1407426 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
List of pages and paragraphs containing keys information about this study. The pages and paragraphs numbers responding to the specific questions of the STROBE Checklist are provided to ease the reading of this manuscript and understanding the study.
(DOC)
Show the Estimated Difference (ED) of cytokines production in blood incubated with Medium only and the Estimated Incremental Difference (EID) of cytokines production above the baseline induced by the respective stimulants between Mtb and Maf-infected patients before treatment. The statistical analyses were done using a random intercept model based on restricted maximum likelihood (REML) and adjusted for age, gender and ethnicity as well as applying Sidak multiple comparison correction. Statistical significant ED and EID are highlighted in bold.
(DOCX)
Show the Estimated Difference (ED) of cytokines production in blood incubated with Medium only and the Estimated Incremental Difference (EID) of cytokines production above the baseline induced by the respective stimulants between Mtb and Maf-infected patients at 6 months of treatment. The statistical analyses were done using a random intercept model based on restricted maximum likelihood (REML) and adjusted for age, gender and ethnicity as well as applying Sidak multiple comparison correction. Statistical significant ED and EID are highlighted in bold.
(DOCX)
Show the Estimated Difference (ED) of genes expression in blood incubated with Medium only and the Estimated Incremental Difference (EID) of genes expression above the baseline induced by the respective stimulants between Mtb and Maf-infected patients before treatment. The statistical analyses were done using a random intercept model based on restricted maximum likelihood (REML) and adjusted for age, gender and ethnicity as well as applying Sidak multiple comparison correction. Statistical significant ED and EID are highlighted in bold.
(XLSX)
Show the Estimated Difference (ED) of genes expression in blood incubated with Medium only and the Estimated Incremental Difference (EID) of genes expression above the baseline induced by the respective stimulants between Mtb and Maf-infected patients at 6 months of treatment. The statistical analyses were done using a random intercept model based on restricted maximum likelihood (REML) and adjusted for age, gender and ethnicity as well as applying Sidak multiple comparison correction. Statistical significant ED and EID are highlighted in bold.
(XLSX)
Data Availability Statement
Our data are from study patients and are sensitive to disclosure therefore cannot be made publicly available according to the MRC/LSHTM ethic policy. However, the anonymised data is available to share upon request to the MRC Unit the Gambia under the supervision of the Head of Data Management and Archives Mr. Bai Lamin Dondeh who is not an author on our manuscript. To have the data, please email our e-data repository (edatarepository@mrc.gm), which is widely accessible by our data management and archives staffs who will rapidly reply to any request.