Abstract
Food oral processing and pharyngeal food passage cannot be observed directly from the outside of the body without instrumental methods. Videofluoroscopy (x-ray video recording) reveals the movement of oropharyngeal anatomical structures in two dimensions. By adding a radiopaque contrast medium, the motion and shape of the food bolus can be also visualized, providing critical information about the mechanisms of eating, drinking, and swallowing. For quantitative analysis of the kinematics of oral food processing, radiopaque markers are attached to the teeth, tongue or soft palate. This approach permits kinematic analysis with a variety of textures and consistencies, both solid and liquid. Fundamental mechanisms of food oral processing are clearly observed with videofluoroscopy in lateral and anteroposterior projections.
Introduction
Food oral processing and pharyngeal food passage cannot be seen directly from the outside of the body. To analyze the kinesiology and physiology of mastication and swallowing, it is important to visualize the food passage through the oral cavity and pharynx and the movement of those structures. Videofluoroscopy (VFS) is the optimal instrumental assessment tool to visualize the movement of the structures and food with a contrast medium simultaneously, as it allows understanding the mechanisms of eating solid food and drinking liquid.
VFS is a dynamic radiographic examination (x-ray video recording) with recordings of fluoroscopic images in subjects eating or swallowing radiopaque materials (Fig. 1). VFS was developed as an alternative to cineradiography (x-ray movie recording), an older technique that in use since the 1890s; clinical application of cineradiography to visualize swallowing and oral function began during the 1950s [1], but its use was limited to the relatively high radiation exposure. VFS provides comparable images with a much lower dose of radiation; it has been used routinely to study dysphagia (swallowing difficulty) since the 1970s [2]. VFS or the videofluorographic swallowing study is regarded as the gold standard in the assessment of dysphagia in clinical settings. During the VFS, the patient ingests radiopaque foods and liquids, and oral, pharyngeal, and esophageal stages of swallowing are evaluated. It has then broadly applied to clinical and basic research fields.
Figure 1.

A subject sitting in the videofluoroscopic apparatus in lateral and anteroposterior projections.
Food oral processing and swallowing are in a sequential process of eating food. VFS enables to visualize the entire sequence. The examination area can reach from the lips to the upper esophageal sphincter (Fig. 2). The main feature of videofluoroscopic analysis is to assess the kinesiology of food bolus and oropharyngeal structures using temporal and spatial measurements. Moreover, synchronizing VFS with the other physiological assessments such as electromyography [3], manometry [4], respiratory measurements[5, 6](airflow or plethysmography), enables analysis of the integrated physiology of eating, drinking, swallowing, and breathing.
Figure 2.


Videofluoroscopic images in lateral and anteroposterior projections.
VFS has many advantages in visualization of food processing and swallowing, but there are some limitations. Since images acquired with VFS are limited to two dimensions information, laterality of function or food passage cannot be evaluated adequately in the lateral projection alone. Therefore, especially in clinical settings, imaging in both lateral and anteroposterior projections is essential. Radiation exposure is also one of the limitations of VFS. However, the radiation dose for swallowing examination is quite low, such as 1.05 mSV in five minutes exposure, and is rarely a limiting factor in adults [7, 8].
VFS Equipment settings and techniques
VFS equipment
The VFS equipment includes standard fluoroscopy apparatus, a seating chair to allow the subject to sit fully upright or recline as needed. Recent VFS systems incorporate high resolution digital imaging with acquisition rates from 15 to 30 frames per second. Review of images after recording is often required, thus storage of the video images with capacity for playback is essential. Sound recording with a microphone and an amplifier is useful to document activities. A video timer to measure the actual time or frame number on each image is essential for temporal analysis (Fig. 2).
Food preparation
Since VFS can visualize only radiopaque materials, use of a radiopaque contrast medium is essential to visualize the bolus. Barium sulfate is the most common contrast medium, and is commercially available as a powder or a suspension of barium in water (so-called liquid barium). Foods are readily mixed with radiopaque material. Liquids are rendered radiopaque by mixing with barium powder. Thickening agent is added if thicker liquids are needed. As standardized viscosity and concentration are essential for reliable physiologic measurements, pre-thickened standardized barium liquids with five levels of viscosity (thin, nectar, thin honey, honey, and pudding) are manufactured in North America (Fig. 3). For solid food, hard food like cookie is usually coated with barium powder or paste, and soft foods like purees or chicken salad are mixed with barium powder in advance of the examination. By using the contrast media, the timing and extent of bolus flow, including timing of oropharyngeal bolus transport and swallow can be measured [9, 10]. If the study subjects are patients with dysphagia, the mechanism of swallowing dysfunction can be assessed. Phenomena such as bolus misdirection (e.g., nasopharyngeal regurgitation, laryngeal penetration, or aspiration) and residue after swallowing can be observed. Laryngeal penetration is defined as contrast entering the larynx but not passing through the vocal folds (glottis). Aspiration is defined as contrast passing through the vocal folds to enter the trachea. Anatomical abnormalities seen on VFS including webs, to the tooth surface with dental cement, and are observed, as are opening and closing of the esophageal sphincters (upper and lower).
Figure 3.

Pre-thickened standardized barium liquid (Varibar, Bracco diagnostic inc., NJ, USA)
Marker preparation
Motions of the soft and hard tissues related to eating and swallowing can be observed with VFS. The movements of calcified tissues such as the jaw or hyoid bone can be traced on VFS recordings. However, for quantitative kinematic analysis, radiopaque markers should be attached to tooth surfaces [11]. Soft tissues, including the tongue or soft palate, are visible in VFS and their contours readily observed. However, kinematic measures are simplified by attaching small radiopaque markers on the mucosal surface. This technique enables to trace the movements of the tongue or soft palate [5, 11–13]. In our previous studies, small lead discs (5-mm diameter) were used as the radiopaque markers, and were attached to the tooth surface with dental cement, and to the tongue surface with medical adhesive [14] (Fig. 4). For soft palate marker, a small metal pellet marker glued to the tip of a flexible rubber tube was passed transnasally with a guidewire, and was positioned on the upper surface of the soft palate [5] (fig. 5). For posterior pharyngeal wall marker, the small metal suction cups (4-mm diameter) attached to a flexible plastic tube was passed transnasally, and the markers were attached to the pharyngeal wall by applying suction to the end of the tube with a 5-mL syringe[15, 16]. The detailed explanation of these preparations has been described in previous literature [5, 14].
Figure 4.
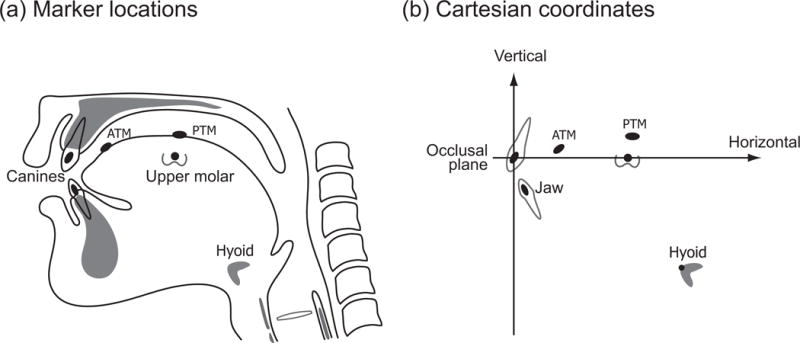
Tongue markers from Matsuo paper
Figure 5.
Soft palate markers from Matsuo10 paper.
Food processing seen in VFS
The movements of food in the oral cavity and oropharynx differ substantially between eating solid food and drinking liquid, while bolus passage through the hypopharynx and esophagus is less variable across food consistencies. Thus, the physiology of eating solid food and drinking liquid has been widely studied with VFS based on two paradigmatic models: the Four Stage Model for swallowing a liquid bolus, and the Process Model for eating solid food. The normal swallow in humans is described with a four-stage sequential model. In this model, the swallowing process was depicted as having oral preparatory, oral propulsive, pharyngeal, and esophageal stages that are sequential and rapid [2, 17]. For eating of solid food, the food processing in the oral cavity, oro-pharyngeal food transport and bolus accumulation in the oropharynx can occur simultaneously before swallowing. Thus eating is not well-described with the four-stage model. Therefore, optimal model for eating solid was proposed as the Process Model [18, 19]. The Process Model explains the feeding sequence with stage I transport, processing, stage II transport, and swallowing. While the stages are sequential in the Four-stage model, stages can overlap in the Process model.
Liquid Processing on VFS
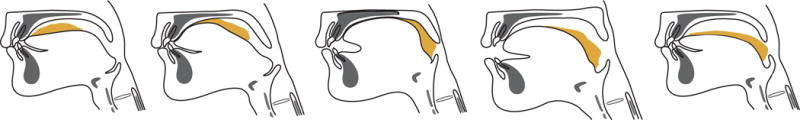
The schematic images of a liquid swallow in lateral projection of VFS are shown in Fig. 6. The liquid bolus is first held in the anterior part of the floor of the mouth or on the tongue surface against the hard palate. The oral cavity is sealed posteriorly by the soft palate and tongue contact to prevent the liquid bolus leaking into the oropharynx before the swallow. Once oral propulsion starts, the tongue tip rises, touching the alveolar ridge of the hard palate just behind the upper teeth, while the posterior tongue drops to open the back of the oral cavity. The area of tongue-palate contact gradually expands from front to back, squeezing the bolus backward. Pharyngeal swallow immediately follows oral propulsion. The soft palate elevates, closing the nasopharynx at about the same time that the bolus head comes into the pharynx. The base of the tongue retracts, pushing the bolus downward and backward against the pharyngeal walls. The pharyngeal constrictor muscles contract sequentially from the top to the bottom, squeezing the bolus downward. The upper esophageal sphincter (UES) opens, often before the bolus reaches the UES. The UES remains closed between swallows due to tonic muscle contraction.
Figure 6.

Schematic images of a liquid swallow in lateral projection of VFS.
Several influencing factors change the bolus flow. Viscosity is known to alter swallow initiation and bolus flow in liquid swallows [20]. Increased bolus viscosity slows bolus flow, thus the oral transit time is extended [21, 22]. The time of initiation of the pharyngeal swallow is correspondingly delayed and a bolus position at swallow initiation is higher up in the pharynx [21, 23]. Taste and chemesthesis can facilitate swallow initiation. Sour taste promotes initiation of swallowing more effectively than the other tastes [24, 25]. Chemesthesis is the feeling of irritation responsible for the perception of the hotness of capsaicin (for example, in hot peppers), coolness of menthol, and tingling with carbonated beverages via the transient receptor potential vanilloid 1 and ankyrin 1 (TRPV1 and TRPA1, respectively) [26, 27]. These receptors are widely distributed in the human oropharynx. Chemesthetic stimuli facilitate swallow initiation and may improve swallow response [28–30].
Solid food processing on VFS
When eating solid food, the food is first transported to the occlusal surfaces of the postcanine dentition (stage I transport). Then, in chewing, the food is reduced in size and lubricated with saliva (food processing). During chewing the food, the triturated food is transported to the oropharynx (stage II transport) and collects there (bolus aggregation) until swallow onset.
After food ingestion, the food is transported to the postcanine region of the teeth backward movement of the tongue surface (Stage I transport). This process of carrying the food posteriorly on the surface of the tongue is called a “pullback” mechanism of intraoral food transport. The tongue also rotates to push the food bolus onto the occlusal surfaces. Stage I transport can be observed with VFS in lateral [19, 31, 32] and AP projections [14, 33]. During stage I transport, the mandible opened and the tongue and hyoid bone moved posteriorly and inferiorly. The initial food size and consistency affects the duration and frequency of stage I transport. Okada et al., [32] reported that stage I transport is closely bound to the recognition process when humans take natural food eating rice sticks freely.
After food is transported to the postcanine region, food processing begins. During food processing, both mechanical and enzymatic digestion are initiated. Food particles are reduced in size by mastication and softened by saliva for bolus formation. Masticatory jaw motion continues until swallowing, but food processing depends on not only the motions of the jaw and teeth, but also the coordinated motions of the tongue, cheek, and soft palate [5, 11, 33–36].
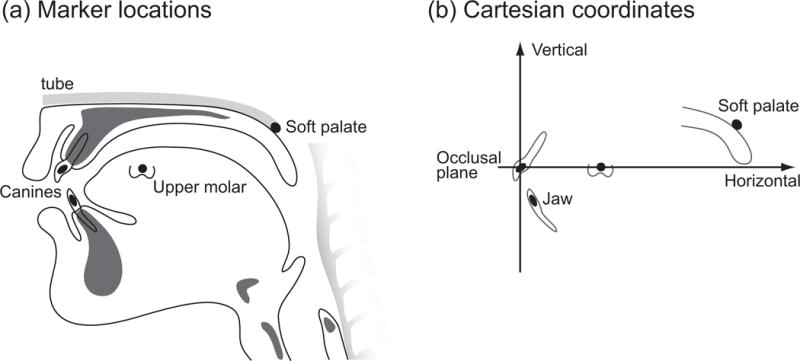
Tongue kinematics during mastication has been studied with VFS recordings using radiopaque tongue markers. Tongue motion is temporally and spatially linked with cyclic jaw movement in food processing [11]. The tongue continuously moves both anteroposteriorly and mediolaterally, during chewing; it also rotates on its three spatial axes during chewing [11, 14](Fig. 7). Those tongue movements reposition the food on the occlusal surfaces before each closing stroke of the teeth [33].
Figure 7.
Vertical motion of (a) the tongue and (b) soft palate during eating of solid food. (a) When eating solid food, the tongue moves cyclically in vertical dimensions. Tongue movement showed tight temporospatial linkage to jaw and hyoid movements during feeding. (b) Motion of the soft palate is temporally linked to jaw movement but not in every motion cycle. The soft palate moves upward as the jaw opens, and moves downward as the jaw closes.
Cyclical motion of the soft palate during mastication is seen on VFS in about 50% of individuals. This movement is temporally linked to jaw movement [5, 37] (Fig. 7). During processing, the soft palate moves upward as the jaw opens and downward as the jaw closes. Since the soft palate and tongue moves continuously, the fauces are not closed during food processing. This permits air to flow between the oral and nasal cavities during mastication, providing access for odorants in food within the oral cavity to reach smell receptors on the nasal mucosa. Indeed, the perception of flavor requires the sensations of both smell and taste.
Stage II transport is readily observed with VFS in the lateral projection. When a portion of the masticated food in the oral cavity is ready for swallowing, triturated food is propelled back through the fauces to the oropharynx by the tongue squeezing it against the palate (stage II transport, Fig. 8) [19, 38]. Stage II transport usually occurs in the later chewing cycles of mastication [19, 39]. During stage II transport, the tongue surface raises, gradually expanding the area of tongue-palate contact from anterior to posterior, squeezing the bolus back along the palate and into the pharynx. The tongue motion during stage II transport is different from that during chewing [14]. In AP projection VFS, the tongue moves mediolaterally and rotates during chewing, but moves upward and remains medial during stage II transport. The frequency of stage II transport is greater with hard than soft food.
Figure 8.
Schematic images of stage II transport in lateral projection of VFS.
The number of chewing cycles and chewing duration to prepare a food for swallowing increases with hardness of food. The duration that the masticated food is aggregated on the pharyngeal surface of the tongue is also longer with greater hardness of the food [19].
New Computed Tomography techniques for swallowing analysis
Although VFS is still regarded as the gold standard for visualizing swallowing mechanisms, the image of VFS is limited to two dimensions. In recent rapid advances in imaging techniques, dynamic area detector computed tomography (ADCT) has been emerging in swallowing evaluation. The recent ADCT detectors of 320 rows with 0.5-mm thickness can scan the area of 160-mm width during 0.275 msec per image. The scanned area can cover the whole oro-pharyngeal region from the nasopharynx to the cervical esophagus. This high speed scanning enables to visualize not only the static 3D oropharyngeal morphology but also oropharyngeal swallowing dynamics with acquisition rate of 10 images/sec (Fig. 9). Radiation exposure is relatively higher compared to VFS, but thanks to recent low dose image reconstruction technique, the dose has decreased substantially. ADCT and VFS provide complementary information, thus ADCT is intended to supplement rather than to replace VFS.
Figure 9.

320 row area detected computed tomography and a swallowing examination chair.
Swallowing analysis with 320-ADCT (swallowing CT) has brought the understandings of 3 dimensional change of oropharynx during swallowing from any angles, which has been never seen with VFS (Fig. 10). Swallowing CT analyzes quantitatively the changes in volume of the pharynx, area of the upper esophageal sphincter, or timing of vocal folds closure, all of which have not able to been observed by VFS. Swallowing CT also has reveal the laterality of pharyngeal contraction in 3D in patients with dysphagia. Swallowing CT is an important development in swallowing research with potential application in patient care.
Figure 10.
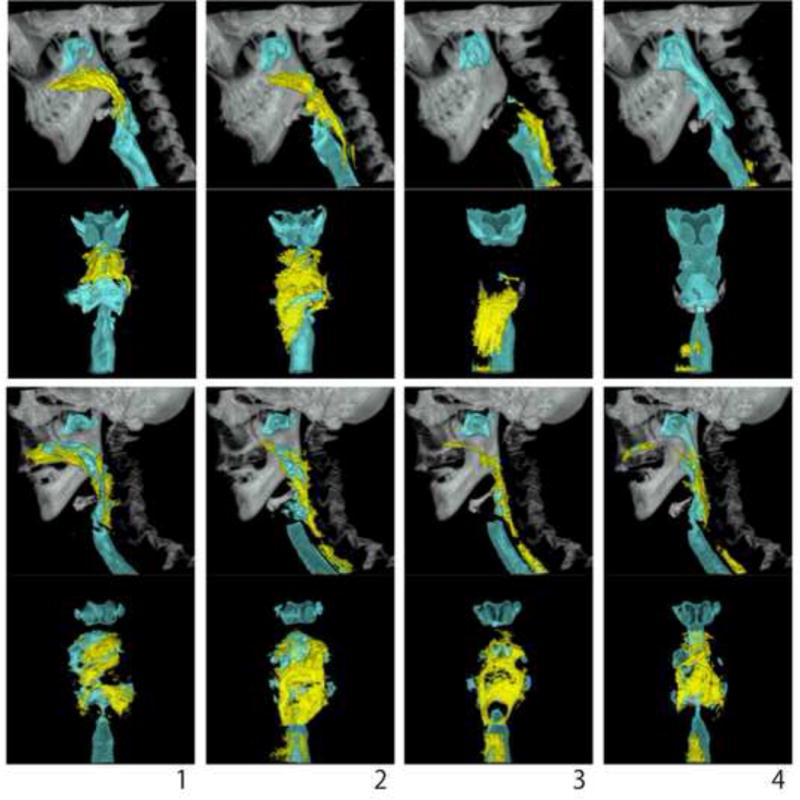
Swallow-CT images of normal adult swallowing 10ml nectar thick barium from lateral and posterior 3D view.
Conclusion
The movements of food in the oral cavity and oropharynx differ substantially between eating solid food and drinking liquid. VFS analyses with lateral and anteroposterior projections have revealed the fundamental mechanisms of food oral processing and swallowing for eating and drinking. By adding a radiopaque contrast medium to liquid or solid food, the motion and shape of the food bolus can be visualized. By applying radiopaque markers to the teeth, tongue or soft palate, quantitative kinematic analysis of the oropharyngeal structures is enabled. Swallowing CT will help understand more 4 dimensional change of food oral processing in the future.
Highlights.
Videofluoroscopy reveals the movement of oropharyngeal structures in two dimensions
Videofluoroscopy permits quantitative kinematic analysis of oral food processing
Imaging in both lateral and AP projections allows understanding the 3D information
Acknowledgments
Supported by USPHS Award R01 DC02123 from the National Institute on Deafness and other Communication Disorders, and KAKENHI (26463200) from the Ministry of Education, Culture, Sports, Science, and Technology, Japan of Japan
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Rushmer RF, Hendron JA. The act of deglutition; a cinefluorographic study. J Appl Physiol. 1951;3:622–30. doi: 10.1152/jappl.1951.3.10.622. [DOI] [PubMed] [Google Scholar]
- 2.Logemann JA. Evaluation and treatment of swallowing disorders. 2nd. Austin Texas: Pro-Ed; 1998. [Google Scholar]
- 3.Inokuchi H, Gonzalez-Fernandez M, Matsuo K, Brodsky MB, Yoda M, Taniguchi H, et al. Electromyography of swallowing with fine wire intramuscular electrodes in healthy human: activation sequence of selected hyoid muscles. Dysphagia. 2014;29:713–21. doi: 10.1007/s00455-014-9566-1. [DOI] [PubMed] [Google Scholar]
- 4.Nativ-Zeltzer N, Kahrilas PJ, Logemann JA. Manofluorography in the evaluation of oropharyngeal dysphagia. Dysphagia. 2012;27:151–61. doi: 10.1007/s00455-012-9405-1. [DOI] [PubMed] [Google Scholar]
- 5.Matsuo K, Metani H, Mays KA, Palmer JB. Effects of respiration on soft palate movement in feeding. J Dent Res. 2010;89:1401–6. doi: 10.1177/0022034510377336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6*.Matsuo K, Palmer JB. Coordination of oro-pharyngeal food transport during chewing and respiratory phase. Physiol Behav. 2015;142:52–6. doi: 10.1016/j.physbeh.2015.01.035. This study demonstrated that stage II tranposrt during chewing occurerd more during expiration than during inspiration, suggesting the temporal linkage between stage II transport movement and respiration. [DOI] [PubMed] [Google Scholar]
- 7.Chan CB, Chan LK, Lam HS. Scattered radiation level during videofluoroscopy for swallowing study. Clin Radiol. 2002;57:614–6. doi: 10.1053/crad.2001.0904. [DOI] [PubMed] [Google Scholar]
- 8.Wright RE, Boyd CS, Workman A. Radiation doses to patients during pharyngeal videofluoroscopy. Dysphagia. 1998;13:113–5. doi: 10.1007/PL00009554. [DOI] [PubMed] [Google Scholar]
- 9.Molfenter SM, Steele CM. Temporal variability in the deglutition literature. Dysphagia. 2012;27:162–77. doi: 10.1007/s00455-012-9397-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Molfenter SM, Steele CM. Physiological variability in the deglutition literature: hyoid and laryngeal kinematics. Dysphagia. 2011;26:67–74. doi: 10.1007/s00455-010-9309-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Palmer JB, Hiiemae KM, Liu J. Tongue-jaw linkages in human feeding: a preliminary videofluorographic study. Arch Oral Biol. 1997;42:429–41. doi: 10.1016/s0003-9969(97)00020-4. [DOI] [PubMed] [Google Scholar]
- 12.Matsuo K, Palmer JB. Kinematic linkage of the tongue, jaw, and hyoid during eating and speech. Arch Oral Biol. 2010;55:325–31. doi: 10.1016/j.archoralbio.2010.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hiiemae KM, Palmer JB, Medicis SW, Hegener J, Scott Jackson B, Lieberman DE. Hyoid and tongue surface movements in speaking and eating. Arch Oral Biol. 2002;47:11–27. doi: 10.1016/s0003-9969(01)00092-9. [DOI] [PubMed] [Google Scholar]
- 14*.Taniguchi H, Matsuo K, Okazaki H, Yoda M, Inokuchi H, Gonzalez-Fernandez M, et al. Fluoroscopic evaluation of tongue and jaw movements during mastication in healthy humans. Dysphagia. 2013;28:419–27. doi: 10.1007/s00455-013-9453-1. The study quantitatively described tongue movement during food oral processing and stage II transport during eating of solid food using VFS in anteroposterior projection. [DOI] [PubMed] [Google Scholar]
- 15.Palmer JB, Tanaka E, Siebens AA. Motions of the posterior pharyngeal wall in swallowing. Laryngoscope. 1988;98:414–7. doi: 10.1288/00005537-198804000-00012. [DOI] [PubMed] [Google Scholar]
- 16.Palmer JB, Tanaka E, Ensrud E. Motions of the posterior pharyngeal wall in human swallowing: a quantitative videofluorographic study. Arch Phys Med Rehabil. 2000;81:1520–6. doi: 10.1053/apmr.2000.17829. [DOI] [PubMed] [Google Scholar]
- 17.Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. Am J Roentgenol. 1990;154:953–63. doi: 10.2214/ajr.154.5.2108569. [DOI] [PubMed] [Google Scholar]
- 18.Palmer JB, Rudin NJ, Lara G, Crompton AW. Coordination of mastication and swallowing. Dysphagia. 1992;7:187–200. doi: 10.1007/BF02493469. [DOI] [PubMed] [Google Scholar]
- 19.Hiiemae KM, Palmer JB. Food transport and bolus formation during complete feeding sequences on foods of different initial consistency. Dysphagia. 1999;14:31–42. doi: 10.1007/PL00009582. [DOI] [PubMed] [Google Scholar]
- 20*.Steele CM, Alsanei WA, Ayanikalath S, Barbon CE, Chen J, Cichero JA, et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30:2–26. doi: 10.1007/s00455-014-9578-x. This detailed review article presented swallowing physiolgy and function modied by food texture and liquid consistency for solid and liquid. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee SI, Yoo JY, Kim M, Ryu JS. Changes of timing variables in swallowing of boluses with different viscosities in patients with dysphagia. Arch Phys Med Rehabil. 2013;94:120–6. doi: 10.1016/j.apmr.2012.07.016. [DOI] [PubMed] [Google Scholar]
- 22.Troche MS, Sapienza CM, Rosenbek JC. Effects of bolus consistency on timing and safety of swallow in patients with Parkinson’s disease. Dysphagia. 2008;23:26–32. doi: 10.1007/s00455-007-9090-7. [DOI] [PubMed] [Google Scholar]
- 23.Hiss SG, Strauss M, Treole K, Stuart A, Boutilier S. Effects of age, gender, bolus volume, bolus viscosity, and gustation on swallowing apnea onset relative to lingual bolus propulsion onset in normal adults. J Speech Lang Hear Res. 2004;47:572–83. doi: 10.1044/1092-4388(2004/044). [DOI] [PubMed] [Google Scholar]
- 24.Pelletier CA, Lawless HT. Effect of citric acid and citric acid-sucrose mixtures on swallowing in neurogenic oropharyngeal dysphagia. Dysphagia. 2003;18:231–41. doi: 10.1007/s00455-003-0013-y. [DOI] [PubMed] [Google Scholar]
- 25.Leow LP, Huckabee ML, Sharma S, Tooley TP. The influence of taste on swallowing apnea, oral preparation time, and duration and amplitude of submental muscle contraction. Chem Senses. 2007;32:119–28. doi: 10.1093/chemse/bjl037. [DOI] [PubMed] [Google Scholar]
- 26.Dessirier JM, Simons CT, Carstens MI, O’Mahony M, Carstens E. Psychophysical and neurobiological evidence that the oral sensation elicited by carbonated water is of chemogenic origin. Chem Senses. 2000;25:277–84. doi: 10.1093/chemse/25.3.277. [DOI] [PubMed] [Google Scholar]
- 27.Green BG, Alvarez-Reeves M, George P, Akirav C. Chemesthesis and taste: evidence of independent processing of sensation intensity. Physiol Behav. 2005;86:526–37. doi: 10.1016/j.physbeh.2005.08.038. [DOI] [PubMed] [Google Scholar]
- 28.Yamasaki M, Ebihara S, Ebihara T, Yamanda S, Arai H, Kohzuki M. Effects of capsiate on the triggering of the swallowing reflex in elderly patients with aspiration pneumonia. Geriatrics & gerontology international. 2010;10:107–9. doi: 10.1111/j.1447-0594.2009.00566.x. [DOI] [PubMed] [Google Scholar]
- 29*.Rofes L, Arreola V, Martin A, Clave P. Natural capsaicinoids improve swallow response in older patients with oropharyngeal dysphagia. Gut. 2013;62:1280–7. doi: 10.1136/gutjnl-2011-300753. This study presented the effect of TRPV1 by capsaicinoids on facilitation of swallowing fuctions in dysphagic patients. [DOI] [PubMed] [Google Scholar]
- 30.Ebihara S, Kohzuki M, Sumi Y, Ebihara T. Sensory stimulation to improve swallowing reflex and prevent aspiration pneumonia in elderly dysphagic people. Journal of pharmacological sciences. 2011;115:99–104. doi: 10.1254/jphs.10R05CP. [DOI] [PubMed] [Google Scholar]
- 31.Mikushi S, Seki S, Brodsky MB, Matsuo K, Palmer JB. Stage I intraoral food transport: Effects of food consistency and initial bolus size. Arch Oral Biol. 2014;59:379–85. doi: 10.1016/j.archoralbio.2014.01.002. [DOI] [PubMed] [Google Scholar]
- 32.Okada A, Honma M, Nomura S, Yamada Y. Oral behavior from food intake until terminal swallow. Physiol Behav. 2007;90:172–9. doi: 10.1016/j.physbeh.2006.09.032. [DOI] [PubMed] [Google Scholar]
- 33.Mioche L, Hiiemae KM, Palmer JB. A postero-anterior videofluorographic study of the intra-oral management of food in man. Arch Oral Biol. 2002;47:267–80. doi: 10.1016/s0003-9969(02)00007-9. [DOI] [PubMed] [Google Scholar]
- 34.Hiiemae KM, Palmer JB. Tongue movements in feeding and speech. Crit Rev Oral Biol Med. 2003;14:413–29. doi: 10.1177/154411130301400604. [DOI] [PubMed] [Google Scholar]
- 35.Hori K, Ono T, Nokubi T. Coordination of tongue pressure and jaw movement in mastication. J Dent Res. 2006;85:187–91. doi: 10.1177/154405910608500214. [DOI] [PubMed] [Google Scholar]
- 36.Casas MJ, Kenny DJ, Macmillan RE. Buccal and lingual activity during mastication and swallowing in typical adults. J Oral Rehabil. 2003;30:9–16. doi: 10.1046/j.1365-2842.2003.00983.x. [DOI] [PubMed] [Google Scholar]
- 37.Matsuo K, Hiiemae KM, Palmer JB. Cyclic motion of the soft palate in feeding. J Dent Res. 2005;84:39–42. doi: 10.1177/154405910508400106. [DOI] [PubMed] [Google Scholar]
- 38.Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Physical medicine and rehabilitation clinics of North America. 2008;19:691–707. doi: 10.1016/j.pmr.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yamashita S, Sugita D, Matsuo K. Relationship between stage II transport and number of chewing strokes as mastication progresses. Physiol Behav. 2013;122:100–3. doi: 10.1016/j.physbeh.2013.08.030. [DOI] [PubMed] [Google Scholar]


