Abstract
Objective
To characterize health disparities in common chronic diseases among adults with socioeconomic status (SES) and ethnicity in a mixed rural-urban community of the United States
Patients and Methods
This was a cross-sectional study to assess the association of prevalence of the five most burdensome chronic diseases in adults with SES and ethnicity and their interaction. The Rochester Epidemiology Project medical records linkage system was used to identify prevalence of coronary heart disease (CHD), asthma, diabetes, hypertension, and mood disorder using ICD-9 codes recorded between January 1, 2005, through December 31, 2009 among all adult residents of Olmsted County, Minnesota, on April 1, 2009. For SES measure, individual HOUsing-based SocioEconomic Status index (termed HOUSES) derived from real property data was used. Logistic regression models were used to examine the association of prevalence of chronic diseases with ethnicity and HOUSES and their interaction.
Results
There were 88,010 eligible adults with HOUSES available, of whom 55% were female, 92% Non-Hispanic White, and the median age (interquartile range) was 46 (30 – 58) years. Overall and in the subgroup of Non-Hispanic White subjects, SES measured by HOUSES was inversely associated with the prevalence of all of five chronic diseases independent of age, gender, and ethnicity (P-values < .001). While association of ethnicity with the prevalence was observed for all the chronic diseases, SES modified the effect of ethnicity for clinically less overt conditions (interaction P-value < .05 for each condition [diabetes, hypertension, and mood disorder]), but not for CHD, a clinically more overt condition.
Conclusion
In a mixed rural-urban setting with predominant Non-Hispanic White population, health disparities in chronic diseases still exist across different SES. The extent to which SES modifies the effect of ethnicity on the risk of chronic diseases may depend on nature of disease.
As health disparities across socioeconomic status (SES) and ethnicity have been well documented in the US and elsewhere, reduction of health disparities has been consistently one of the overarching goals of the Healthy People in the United States since 1990.1–9 The 2003 Institute of Medicine Report and the 2013 National Healthcare Disparities Report suggest prevailing disparities in health care access and health outcomes across income and ethnicity.10,11 The geographic and temporal trends of health disparities among people with different SES and ethnic backgrounds have persisted, and may have worsened over time.11–15 For example, the National Health and Nutrition Examination Survey, 1999 to 2006 showed that control of blood pressure and glucose and cholesterol levels has improved since 1999 for adults with cardiovascular disease and diabetes, but gaps in ethnic or socioeconomic disparities have not significantly declined.14 Another recent cross-sectional study among Medicare enrollees in 2006 and 2011 showed similar ethnic disparities in control of the same measures as well as significant regional variation.15
Despite the regional variation of health disparities across ethnicity categories in the US, little is known about the degree and nature of health disparities in a mixed rural-urban setting that mitigates factors known to contribute to health disparities, such as a relatively affluent community, a higher proportion of people working in the health care system (higher access to health care services), lower prevalence of environmental issues (air pollution, pest infestation, etc.), homogeneous distribution of people with different ethnicity in the community (lower dissimilarity index), and higher health insurance coverage.16–20 Given these potentially mitigating factors for health disparities at a community level, assessing health disparities in common chronic diseases in a community characterized by these attributes is likely to provide important insight into the degree and nature of health disparities in chronic diseases in a non-inner city setting. Using data from such a setting, we determined whether significant health disparities in chronic diseases among people with different ethnicity and SES existed in our community given the mitigating factors at a community level.
In addressing this question, the literature is limited as few population-based studies using a well-defined cohort in a mixed rural-urban setting are available. Particularly, most previous studies were based on self-reported SES measures and health outcomes.3–9 One important barrier to large-scale health disparities research based on clinical or administrative datasets is the lack of SES measures even during the electronic medical record era. To overcome this barrier, we applied our recently developed individual housing-based SES index (termed HOUSES) to a population-based cohort including nearly all Olmsted County, Minnesota, residents, instead of relying on self-reported SES measures.21–26 Olmsted County, Minnesota, is a suitable study setting for conducting a population-based study such as this since the health care environment is self-contained and medical records for nearly all residents are available for clinical research. Using these unusual resources, we examined the degree and nature of health disparities in five common chronic diseases among adults with different SES and ethnicity.
PATIENTS AND METHODS
Study Setting and Population
Olmsted County, Minnesota, is a mixed rural-urban setting containing both urban and rural areas defined by the United States Census (16% of rural population and 91% of rural area) with low White/Black dissimilarity index of 29.5 in 2010 (versus 82.5 for Chicago, Illinois).20,27 According to the 2010 Census, the population of Olmsted County was 85.7% White, 4.7% African American, 5.4% Asian, and 4.2% Hispanic.16 Our community has a higher median family income ($66,252 in 2009–2013) than the national average ($53,046) and a larger proportion of Rochester residents working in the health care industry (22%).18,19,28 Accordingly, Olmsted County is not a Medically Underserved Area.29 The level of poverty in Minnesota and the United States has steadily increased since 2008 (11.9% in Minnesota and 15.9% throughout the nation in 2011), but poverty levels in Olmsted County remain considerably below national and state levels hovering around 8% over the last five years. 95% of Olmsted County adults currently have health insurance (vs. 85% in the US) and 66% routinely seek medical care.30
The Rochester Epidemiology Project (REP) links data on medical care delivered to the population of Olmsted County, Minnesota.31–33 The majority of medical care in this community is currently provided by the Mayo Clinic and its two affiliated hospitals, and the Olmsted Medical Center and its affiliated hospitals with limited care provided through the two clinicians of the Rochester Family Medicine Clinic which has recently closed. The health care records from these institutions are linked together through the REP records linkage system.32,33 Patients are categorized as residents or non-residents of Olmsted County at the time of each health care visit on the basis of their address. The population counts obtained by the REP census are similar to those obtained by the US Census, indicating that virtually the entire population of the county is captured by the system.32,33 For this study, we used the REP census to identify all individuals who resided in Olmsted County on April 1, 2009, but we excluded those individuals who had refused medical record research authorization in at least one health care institution.32
Study design
This was a cross-sectional study to assess the association of 5-year prevalence (i.e., January 1, 2005, through December 31, 2009) of the five most burdensome chronic diseases in adults with different socioeconomic status (SES) and ethnicity and their interaction.
The five most burdensome chronic diseases
We assessed the prevalence of the five most burdensome chronic diseases as identified by the Agency for Healthcare Research and Quality (AHRQ) among adults over 18 years of age identified by the REP dataset.34 These diseases included coronary heart disease (CHD), asthma, diabetes, hypertension, and mood disorder. Detail identification algorithms for each disease were previously described.35 In brief, the diagnostic indices of the REP were searched electronically to extract the International Classification of Diseases, Ninth Revision (ICD-9) codes of these five chronic diseases in the medical records of the Olmsted County population ever assigned by any health care institution from January 1, 2005, through December 31, 2009 (i.e., 5-year prevalence with a single ICD code). These ICD-9 codes were grouped into clinical classification codes (CCCs) proposed by the AHRQ-Healthcare Cost and Utilization Project.36,37
Individual socioeconomic status measured by HOUSES
Socioeconomic status of our study population was measured by individual housing-based SES index (HOUSES).21–26 Development and initial testing of the index were completed in both Olmsted County, Minnesota, and Jackson County, Missouri, and the index was applied to a study, which was conducted in Sioux Falls, South Dakota. Briefly, in formulating HOUSES, addresses of the eligible subjects in April 2009 were geocoded. Geocoding allowed us to match the study subject’s address to geographic reference data and real property data from the Assessor’s Office of the county government. Our original research work for development and validation of HOUSES (principal components factor analysis) identified four real property feature variables including housing value, square footage of housing unit, number of bedrooms, and number of bathrooms in a same factor sharing the underlying construct (SES). We then formulated a standardized HOUSES index score by summing their z-scores for each variable (i.e., standardized index). The higher the HOUSES (z-score), the higher the SES. Our prior work has demonstrated that HOUSES is associated with health outcomes in children and adults such as the risk of low birth weight, obesity, smoking exposure at home, asthma control status, risk of pneumococcal diseases, post-MI mortality, and risk of rheumatoid arthritis (RA) and post-RA mortality.21–26
Other variables
Both Olmsted County and Minnesota’s minority populations accounted for 14.7% of the population in 2010.38 For this study, we grouped the self-reported ethnicity into 4 groups, which include non-Hispanic White, African American, Asian, and Hispanic according to the suggested racial and ethnic categories by the NIH.15,39 As suggested by a previous study, we grouped the other/unknown category with the non-Hispanic White category because we presumed that most of the patients in the other/unknown category were non-Hispanic White (85.7% of the Olmsted County’s population self-reported White in the 2010 census).35
Statistical Analysis
Descriptive statistics were used to summarize demographic characteristics of the study population. Association between demographic variables and HOUSES in quartiles (Q1 – Q4) was assessed by Chi-square tests. To assess the association of HOUSES with the prevalence of each chronic condition (CHD, asthma, diabetes, hypertension, and mood disorder), logistic regression models were used among subjects in the overall cohort, adjusting for age, gender, and ethnicity. Additional multivariate logistic models further adjusted for pertinent risk factors for CHD (diabetes, hypertension, hyperlipidemia, and obesity) and diabetes (hyperlipidemia and obesity). Similar analysis was carried out among non-Hispanic White subjects only. Stratified logistic regression models were used to assess associations of different ethnicity groups with each chronic disease. In addition, an interaction effect between ethnicity and HOUSES on prevalence of each disease was tested under the framework of logistic regression, by adding an interaction term between ethnicity group and HOUSES quartiles. Statistical analyses were performed using the SAS software package (SAS Institute, Cary, NC). All tests were two-sided and p-values <0.05 were considered statistically significant.
RESULTS
Characteristics of study subjects
Of the eligible REP cohort (n=130,078), we excluded 9,455 subjects due to institutionalized subjects (n=330), PO Box (n=1,186), unverifiable addresses (n=6,099), and unavailable real property data (n=1,840) leaving 120,623 (93%) subjects who were successfully geocoded. Of the 120,623 subjects, 88,010 were adults; 55% were female and the median age (interquartile range, IQR) was 46 (IQR 30 – 58) years (Table 1). The proportions of non-Hispanic White, African American, Asian, and Hispanic subjects were 91.7%, 3.0%, 3.5%, and 1.8%, respectively. The median (IQR) of HOUSES was −0.38 (−2.28 – 1.84).
Table 1.
Sociodemographic characteristics and prevalence of the five most burdensome chronic diseases
| Variables | (N=88,010) |
|---|---|
| Age, years | |
| Median (IQR) | 45 (30, 58) |
|
| |
| Age group (years), n (%) | |
| 18–45 | 45,450 (51.6) |
| 46–65 | 29,011 (33.0) |
| >65 | 13,549 (15.4) |
|
| |
| Gender, n (%) | |
| Male | 39,924 (45.4) |
| Female | 48,086 (54.6) |
|
| |
| Ethnicity, n (%) | |
| Non-Hispanic White | 80,699 (91.7) |
| African American | 2,650 (3.0) |
| Asian | 3,065 (3.5) |
| Hispanic | 1,596 (1.8) |
|
| |
| HOUSES | |
| Median (IQR) | −0.38 (−2.28, 1.84) |
|
| |
| Prevalence of five chronic diseases, n (%) | |
| Coronary Heart Disease (CHD) | 9,585 (10.9) |
| Asthma | 7,601 (8.6) |
| Diabetes | 7,824 (8.9) |
| Hypertension | 22,513 (25.6) |
| Mood Disorder | 2,2263 (25.3) |
SES as measured by HOUSES and demographic characteristics
Overall, higher SES was observed among subjects aged between 46 and 65 years and males (Table 2). In addition, Non-Hispanic White subjects had higher SES than their African American and Hispanic counterparts, whereas Asian subjects showed relatively similar SES as Non-Hispanic White subjects in this community (percent of subjects in the highest SES quartile (Q4) was 25.9% for Non-Hispanic White subjects, 7.5% for African American subjects, 10% among Hispanic subjects, and 24.3% for Asian subjects).
Table 2.
Association between demographic characteristics and HOUSES as both continuous scale and quartiles (Q1 – Q4)
| HOUSES median (IQR) | HOUSES (quartile) | ||||
|---|---|---|---|---|---|
| Q1 (lowest), n (%) | Q2, n (%) | Q3, n (%) | Q4 (highest), n (%) | ||
| Age, years | [P <.001]a | ||||
| 18–45 | −0.57 (−2.74, 1.65) | 12,999 (28.6) | 10,594 (23.3) | 11,022 (24.3) | 10,835 (23.8) |
| 46–65 | 0.22 (−1.72, 2.57) | 5,454 (18.8) | 6,853 (23.6) | 7,598 (26.2) | 9,106 (31.4) |
| >65 | −0.95 (−2.32, 0.75) | 3,551 (26.2) | 4,556 (33.6) | 3,382 (25.0) | 2,060 (15.2) |
|
| |||||
| Gender | [P <.001]a | ||||
| Male | −0.17 (−2.12, 2.02) | 9,283 (23.3) | 9,862 (24.7) | 10,274 (25.7) | 10,505 (26.3) |
| Female | −0.54 (−2.40, 1.69) | 12,721 (26.5) | 12,141 (25.2) | 11,728 (24.4) | 11,496 (23.9) |
|
| |||||
| Ethnicity | [P <.001]a | ||||
| Non-Hispanic | |||||
| White | −0.24 (−2.11, 1.96) | 18,519 (22.9) | 20,754 (25.7) | 20,525 (25.4) | 20,901 (25.9) |
| African | |||||
| American | −4.56 (−5.15, −0.44) | 1,603 (60.5) | 390 (14.7) | 461 (17.4) | 196 (7.5) |
| Asian | −0.41 (−3.21, 1.74) | 956 (31.2) | 586 (19.1) | 778 (25.4) | 745 (24.3) |
| Hispanic | −3.51 (−4.97, −0.43) | 926 (58.0) | 273 (17.1) | 238 (14.9) | 159 (10.0) |
p-value from Chi-square test
SES and the prevalence of common chronic diseases
Overall, lower SES was associated with higher prevalence of each of the five chronic conditions controlling for age, gender, ethnicity, and additional pertinent risk factors. The results are summarized in Table 3 (P-values < .001), and a similar pattern was found in the subgroup of Non-Hispanic White subjects. The impact of SES on prevalence tended to be greater in diabetes, hypertension, and mood disorder, compared to CHD and asthma. For example, the adjusted odds ratio for the highest SES group, compared to the lowest SES group was 0.56 (95% CI 0.52 – 0.60) for diabetes, and 0.74 (95% CI 0.69 – 0.80) for CHD.
Table 3.
Association between HOUSES and prevalence of chronic diseases in overall cohort and among Non-Hispanic White
| HOUSES (quartile) | Overall | Non-Hispanic White | ||
|---|---|---|---|---|
|
| ||||
| (N=88,010), n (%) | adj. OR (95% CI) | (N=80,699), n (%) | adj. OR (95% CI) | |
| CHD | ||||
|
| ||||
| Q1 (lowest SES) | 2,535 (11.5) | 1.0 (Reference) [P <.001] a | 2,357 (12.7) | 1.0 (Reference) [P <.001] d |
| Q2 | 2,867 (13.0) | 0.87 (0.81, 0.93) | 2,784 (13.4) | 0.84 (0.78, 0.90) |
| Q3 | 2,429 (11.0) | 0.86 (0.80, 0.92) | 2,331 (11.4) | 0.87 (0.81, 0.94) |
| Q4 (highest SES) | 1,754 (8.0) | 0.74 (0.69, 0.80) | 1,693 (8.1) | 0.81 (0.75, 0.88) |
|
| ||||
| Asthma | ||||
|
| ||||
| Q1 (lowest SES) | 2,112 (9.6) | 1.0 (Reference) [P <.001] b | 1,849 (10.0) | 1.0 (Reference) [P <.001] e |
| Q2 | 1,950 (8.9) | 0.90 (0.84, 0.96) | 1,850 (8.9) | 0.91 (0.85, 0.97) |
| Q3 | 1,840 (8.4) | 0.85 (0.80, 0.91) | 1,739 (8.5) | 0.86 (0.80, 0.92) |
| Q4 (highest SES) | 1,699 (7.7) | 0.78 (0.73, 0.83) | 1,627 (7.8) | 0.78 (0.73, 0.84) |
|
| ||||
| Diabetes | ||||
|
| ||||
| Q1 (lowest SES) | 2,330 (10.6) | 1.0 (Reference) [P <.001] c | 2,004 (10.8) | 1.0 (Reference) [P <.001] f |
| Q2 | 2,303 (10.5) | 0.84 (0.78, 0.89) | 2,176 (10.5) | 0.83 (0.78, 0.89) |
| Q3 | 1,905 (8.7) | 0.75 (0.70, 0.80) | 1,741 (8.5) | 0.74 (0.69, 0.80) |
| Q4 (highest SES) | 1,286 (5.8) | 0.56 (0.52, 0.60) | 1,178 (5.6) | 0.56 (0.52, 0.61) |
|
| ||||
| Hypertension | ||||
|
| ||||
| Q1 (lowest SES) | 5,672 (25.8) | 1.0 (Reference) [P <.001] b | 5,180 (28.0) | 1.0 (Reference) [P <.001] e |
| Q2 | 6,789 (30.9) | 0.96 (0.91, 1.01) | 6,558 (31.6) | 0.96 (0.90, 1.01) |
| Q3 | 5,651 (25.7) | 0.80 (0.76, 0.85) | 5,352 (26.1) | 0.78 (0.74, 0.83) |
| Q4 (highest SES) | 4,401 (20.0) | 0.64 (0.61, 0.68) | 4,209 (20.1) | 0.64 (0.60, 0.67) |
|
| ||||
| Mood disorder | ||||
|
| ||||
| Q1 (lowest SES) | 6,534 (29.7) | 1.0 (Reference) [P <.001] b | 5,872 (31.7) | 1.0 (Reference) [P <.001] e |
| Q2 | 5,737 (26.1) | 0.78 (0.75, 0.81) | 5,520 (26.6) | 0.79 (0.76, 0.83) |
| Q3 | 5,309 (24.1) | 0.72 (0.69, 0.75) | 5,057 (24.6) | 0.72 (0.69, 0.75) |
| Q4 (highest SES) | 4,683 (21.3) | 0.61 (0.58, 0.63) | 4,531 (21.7) | 0.61 (0.59, 0.64) |
adjusted for age, gender, ethnicity, hypertension, diabetes, hyperlipidemia, and obesity;
adjusted for age, gender and ethnicity;
adjusted for age, gender, ethnicity, hyperlipidemia, and obesity;
adjusted for age, gender, hypertension, diabetes, hyperlipidemia, and obesity;
adjusted for age and gender;
adjusted for age, gender, hyperlipidemia, and obesity
Ethnicity and the prevalence of chronic diseases
The association between ethnicity and prevalence of chronic diseases varied in magnitude but showed no consistent patterns for distinguishing clinically more versus less overt diseases. The results are summarized in Table 4. While mood disorder was more prevalent in Non-Hispanic White subjects than in minority groups, odds of diabetes were at least two-fold higher among minority groups compared with Non-Hispanic White subjects adjusting for age and gender (and obesity for comparison of diabetes). In comparison to Non-Hispanic White subjects, Hispanic subjects had a reduced rate of both hypertension and CHD while African American subjects had increased odds of both diseases adjusting for pertinent risk factors. Both Asian and Hispanic, but not African American subjects, showed lower rates of asthma compared to Non-Hispanic White subjects.
Table 4.
Association between ethnicity and prevalence of chronic diseases (adj. OR (95% CI) [p-value]a)
| Ethnicity | CHDb | Asthmac | Diabetesd | Hypertensionc | Mood Disorderc |
|---|---|---|---|---|---|
|
| |||||
| [P= .01] | [P <.001] | [P <.001] | [P <.001] | [P <.001] | |
| African American | 1.25 (1.04, 1.50) | 1.04 (0.91, 1.19) | 2.22 (1.94, 2.55) | 1.38 (1.23, 1.55) | 0.62 (0.56, 0.69) |
| Asian | 1.00 (0.84, 1.18) | 0.61 (0.52, 0.71) | 2.09 (1.83, 2.39) | 0.86 (0.77, 0.97) | 0.44 (0.40, 0.49) |
| Hispanic | 0.71 (0.53, 0.97) | 0.61 (0.49, 0.75) | 1.97 (1.64, 2.38) | 0.86 (0.72, 1.01) | 0.63 (0.56, 0.72) |
All listed p-values are for comparisons among different ethnicity for risk of each chronic disease;
Adjusted for age, gender, hypertension, diabetes, hyperlipidemia, and obesity;
Adjusted for age and gender;
Adjusted for age, gender, hyperlipidemia, and obesity; all compared with non-Hispanic White.
Interaction between SES and Ethnicity in relation to the prevalence of chronic diseases
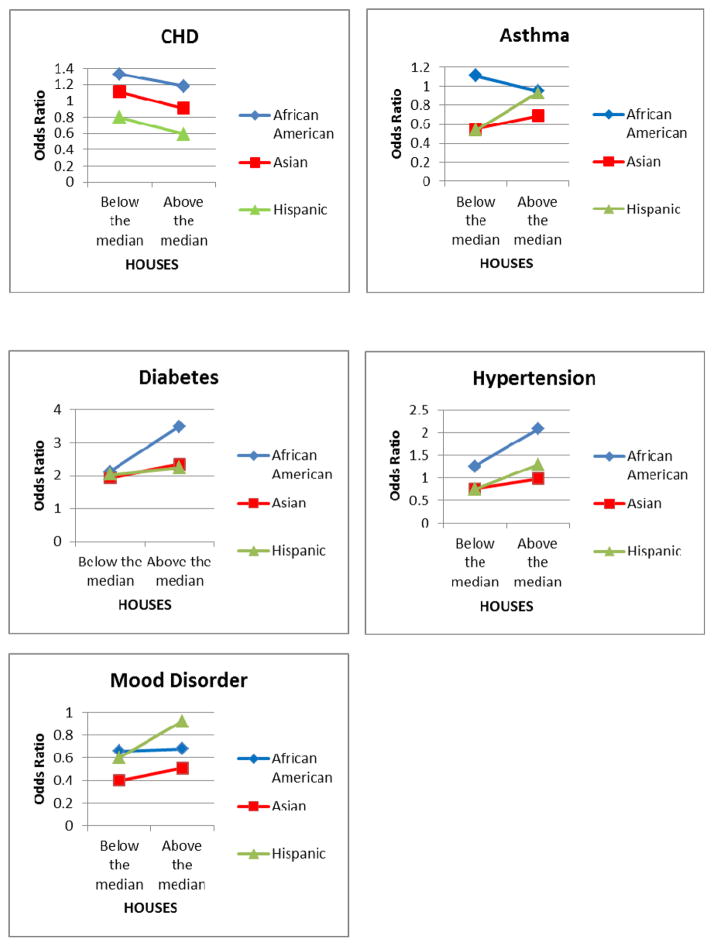
SES modified the effect of ethnicity on the prevalence of chronic diseases, and the interaction between SES and ethnicity depended on the nature of the disease. The results are summarized in Figure 1 and Supplemental Table. Specifically, the patterns in which SES modified the effect of ethnicity observed among minority groups were comparatively different for diabetes, hypertension, and mood disorder from CHD. As shown in Figure 1 and Supplemental Table, odds of diabetes, hypertension, and mood disorder were generally increased with higher SES (above the median of HOUSES) in the minority subjects, especially African American subjects, relative to Non-Hispanic White subjects, controlling for age, gender, ethnicity, and additional pertinent risk factors for diabetes (i.e., obesity and hyperlipidemia). However, such patterns appeared to be reversed for CHD.
Figure 1. Comparison of odds ratios of each chronic condition by ethnicity between different SES group (reference: Non-Hispanic White subjects).
SES modified the effect of ethnicity on the prevalence of chronic diseases, and the interaction between SES and ethnicity depended on the nature of the disease. Specifically, the patterns in which SES modified the effect of ethnicity observed among minority groups were comparatively different for diabetes, hypertension, and mood disorder from CHD. In this Figure 1, odds of diabetes, hypertension, and mood disorder were generally increased with higher SES (above the median of HOUSES) in the minority subjects, especially African American subjects, relative to Non-Hispanic White subjects, controlling for age, gender and additional pertinent risk factors. However, such patterns appeared to be reversed for CHD.
DISCUSSION
Significant health disparities still existed among Non-Hispanic White residents and overall adult population with different SES in a mixed rural-urban setting. Also, there were ethnic disparities in the prevalence of common chronic diseases. SES modified the effect of ethnicity on the prevalence of chronic diseases but such effect modification by SES depended on the nature of clinical disease (i.e., clinically overt diseases such as CHD versus clinically less overt diseases such as diabetes, hypertension, and mood disorder).
Despite the potential mitigating factors for health disparities (e.g., a relatively affluent community, a higher proportion of people working in the health care system, homogeneous distribution of people with different ethnicity in the community, and higher health insurance coverage), 16–19,30,40 there were still significant disparities in the prevalence of chronic disease among different ethnic groups in this community. Also, health disparities existed in our study’s majority, non-Hispanic White population with different SES in a dose-response manner across all chronic diseases examined. Furthermore, the ratios of prevalence of each chronic disease between the highest SES stratum (Q4) and the lowest (Q1) in our community (Q4/Q1) (i.e., 0.70 (CHD), 0.80 (asthma), 0.55 (diabetes)), 0.78 (hypertension), and 0.72 (mood disorder), were not drastically different from estimates by multiple studies at a national level [i.e., 0.4–0.66 (CHD), 0.94–1.04 (asthma), 0.38–0.47 (diabetes), 0.59–0.70 (hypertension), and 0.87 (mood disorder)].41–44 Since our study results were based on ICD-9 codes for chronic diseases and HOUSES for SES measure, it is unlikely to be due to report biases caused by self-report. Literature has shown that Non-Hispanic Whites have a reduced risk of multiple chronic diseases.45–49 As the Non-Hispanic White population has been often used as a reference group for analysis, the literature examining health disparities among Non-Hispanic White populations across different SES groups is relatively limited.3 Overall, our study results suggest that Non-Hispanic White populations do not seem to be exempt from health disparities across different SES.
Our study results reveal noteworthy findings. As shown in Figure 1 and eTable 1, overall, a higher prevalence of clinically less overt diseases (diabetes, hypertension, and mood disorder) was found in the minority groups with higher SES (above the median of HOUSES when stratified by HOUSES), compared to those with lower SES. Such patterns or trends were not observed in clinically overt disease such as CHD. In this respect, the higher prevalence of chronic diseases may reflect identification of diseases (diagnosis or detection) not necessarily representing only a risk of disease per se. For example, clinically less overt chronic diseases might be much more dependent upon access to health care and health literacy for identification of such diseases whereas those clinically more overt diseases such as CHD often require emergency care (as it can be a life-threatening condition), and thus are less dependent upon one’s ability to recognize the diseases and health care access. In this interpretation, we consider asthma as a disease with mixed features between clinically overt and less overt diseases and this is why asthma shows a different pattern from clinically overt disease and less overt diseases as shown in Figure 1. This suggests the extent to which SES modifies the effect of ethnicity on the risk of chronic diseases may depend on nature of disease. Therefore, one should bear in mind in interpreting our study results in terms of differentiating disease versus diagnosis as we used ICD-9 codes for defining chronic diseases. As Shippee et al pointed out, given the impact of SES on health care access and literacy, patients with lower SES may not seek timely care for appropriate diagnosis and treatment for clinically less overt disease until they develop clinically significant manifestations.50
Our study results have a few important implications on health care policy concerning health disparities. First, ethnic disparities in health outcomes should be interpreted in the context of SES and the nature of the disease examined as shown in our study results. The complex interaction among ethnicity, SES and the disease nature might not be captured if one examines health disparities across different ethnicity and SES separately, especially without considering the clinical nature of the disease. Second, true health disparities (i.e., disease risk) across different SES might be more underestimated in clinically less overt diseases such as diabetes or hypertension regardless of ascertainment methods (i.e., lower identification of such diseases in a lower SES group and greater detection in higher SES group). Therefore, while the health care system makes an effort to prevent these chronic diseases, to reduce health disparities in outcomes of clinically less overt diseases, identification of such diseases through improving health literacy and health care access should be a primary focus of intervention, especially among underserved populations including minorities or lower SES population. Finally, our study results highlight Non-Hispanic White populations with lower SES still represent underserved populations who are a target population for health promotion.
The main strength of our study is the population-based study design. Another strength is the prevalence of diseases was based on documented physician-diagnosis instead of self-report. In addition, we objectively measured SES based on real property data instead of self-reported conventional SES measures. Also, in this study, HOUSES index was available for nearly all eligible subjects (93%). Our findings need to be interpreted with caution. The main limitation of our study is the inability to verify ICD-9 codes.51,52 As we defined prevalence of each chronic condition with a single ICD-9 code as suggested by a previous study,35 Prevalence of some conditions might have been overestimated. For example, prevalence of CHD might have been changed after diagnostic procedures (10.9% in this study vs. 6.0% in the US and 4.9% in Minnesota).42 However, systematic differential misclassification of CHD across different SES or ethnicity is unlikely given the life-threatening nature of CHD. Also, given the availability of specific diagnostic tests or procedures for hypertension, diabetes, and asthma, our study results are unlikely to be due to systemic (differential) misclassification of diseases. The cross-sectional nature of the analysis (i.e., prevalence study) is also a limitation of this study. While we took into account traditional risk factors for certain diseases (CHD and diabetes), we did not have all pertinent risk factors for certain diseases examined to adjust the main results. For this study, we grouped the other/unknown category with the Non-Hispanic White category, as suggested by previous studies, but by presuming this may be inaccurate. Lastly, unavailability of insurance data for the REP population limited our further data analysis for impact of insurance type on the association of SES with prevalence of chronic conditions.
Conclusions
In a mixed rural-urban setting with predominant Non-Hispanic White population, health disparities in chronic diseases still exist across different SES. The degree to which SES modifies the effect of ethnicity on the risk of chronic diseases may depend on nature of disease.
Supplementary Material
Acknowledgments
Funding / Support: This work was supported by the National Institute of Allergy and Infectious Diseases (R21 AI101277) and the Scholarly Clinician Award from the Mayo Foundation. Also, this study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676.
Abbreviations
- SES
Socioeconomic status
- HOUSES
HOUsing-based SocioEconomic Status index
- CHD
Coronary Heart Disease
- ICD-9
The International Classification of Diseases, Ninth Revision
- REP
The Rochester Epidemiology Project
- RA
Rheumatoid Arthritis
- IQR
Interquartile Range
Footnotes
Conflict of Interest Disclosures: All authors will complete and submit the ICMJE Form for Disclosure of Potential Conflicts of Interest after the manuscript is submitted. No author has disclosures to be reported.
Role of Funder/Sponsor: The funding agency was not involved in the design and conduct of the study, in the collection, analysis, and interpretation of the data, and in the preparation, review, or approval of the manuscript.
Author Contributions: Dr. Juhn had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Wi, St. Sauver, Jacobson, Lahr, Ryu, Beebe, Sloan, Juhn
Acquisition, analysis, or interpretation of data: Wi, St. Sauver, Lahr, Ryu, Juhn
Drafting of the manuscript: Wi, Ryu, Juhn
Critical revision of the manuscript for important intellectual content: Wi, St. Sauver, Jacobson, Pendegraft, Lahr, Ryu, Beebe, Sloan, Rand-Weaver, Krusemark, Choi, Juhn
Statistical analysis: Wi, St. Sauver, Jacobson, Pendegraft, Lahr, Ryu, Juhn
Administrative, technical, or material support: Wi, Krusemark, Juhn
Study supervision: Juhn
Additional Contributions: We thank Mrs. Kelly Okeson for administrative assistance and support and appreciate Dr. Barbara Y. Yawn’s editorial review for the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1. [Accessed January 23th, 2015];Healthy People 2020. https://www.healthypeople.gov/
- 2.Healthy People 2020 Leading Health Indicators: Progress Update. U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2014. [Google Scholar]
- 3.Braveman PA, Cubbin C, Egerter S, Williams DR, Pamuk E. Socioeconomic disparities in health in the United States: what the patterns tell us. Am J Public Health (N Y) 2010 Apr 1;100(Suppl 1):S186–196. doi: 10.2105/AJPH.2009.166082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Karlamangla AS, Merkin SS, Crimmins EM, Seeman TE. Socioeconomic and ethnic disparities in cardiovascular risk in the United States, 2001–2006. Ann Epidemiol. 2010 Aug;20(8):617–628. doi: 10.1016/j.annepidem.2010.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Banks J, Marmot M, Oldfield Z, Smith JP. Disease and disadvantage in the United States and in England. Jama. 2006 May 3;295(17):2037–2045. doi: 10.1001/jama.295.17.2037. [DOI] [PubMed] [Google Scholar]
- 6.Signorello LB, Cohen SS, Williams DR, Munro HM, Hargreaves MK, Blot WJ. Socioeconomic status, race, and mortality: a prospective cohort study. Am J Public Health (N Y) 2014 Dec;104(12):e98– e107. doi: 10.2105/AJPH.2014.302156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Farmer MM, Ferraro KF. Are racial disparities in health conditional on socioeconomic status? Soc Sci Med. 2005 Jan;60(1):191–204. doi: 10.1016/j.socscimed.2004.04.026. [DOI] [PubMed] [Google Scholar]
- 8.Mackenbach JP, Stirbu I, Roskam AJ, et al. Socioeconomic inequalities in health in 22 European countries. N Engl J Med. 2008 Jun 5;358(23):2468–2481. doi: 10.1056/NEJMsa0707519. [DOI] [PubMed] [Google Scholar]
- 9.MW . Inequalities in Health: The Black Report and Health Divide. 1992. [Google Scholar]
- 10.Smedley BD, Stith AY, Nelson AR, editors. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): 2003. [PubMed] [Google Scholar]
- 11.National Healthcare Disparities Report. U.S. Department of Health and Human Services, Agency for Healthcare Research and Quality (AHRQ); 2013. [Accessed February 13, 2015]. http://www.ahrq.gov/research/findings/nhqrdr/nhdr13/2013nhdr.pdf. [Google Scholar]
- 12.Kamangar F, Dores GM, Anderson WF. Patterns of cancer incidence, mortality, and prevalence across five continents: defining priorities to reduce cancer disparities in different geographic regions of the world. J Clin Oncol. 2006 May 10;24(14):2137–2150. doi: 10.1200/JCO.2005.05.2308. [DOI] [PubMed] [Google Scholar]
- 13.America’s Health Rankings. Annual Report. United Health Foundation; 2014. [Accessed February 13, 2015]. http://www.americashealthrankings.org/reports/annual. [Google Scholar]
- 14.McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of medicare coverage. Ann Intern Med. 2009 Apr 21;150(8):505–515. doi: 10.7326/0003-4819-150-8-200904210-00005. [DOI] [PubMed] [Google Scholar]
- 15.Ayanian JZ, Landon BE, Newhouse JP, Zaslavsky AM. Racial and ethnic disparities among enrollees in Medicare Advantage plans. N Engl J Med. 2014 Dec 11;371(24):2288–2297. doi: 10.1056/NEJMsa1407273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. [Accessed February 13, 2015];United States Census. 2010 http://www.census.gov/2010census/popmap/ipmtext.php?fl=27.
- 17.State of the Air. American Lung Association; 2014. [Accessed February, 2015]. http://www.stateoftheair.org/2014/assets/ALA-SOTA-2014-Full.pdf. [Google Scholar]
- 18.Occupational Employment Statistics. Metropolitan and Nonmetropolitan Area Occupational Employment and Wage Estimates. Rochester, MN: US Bureau of Labor Statistics; May, 2013. [Accessed February 28, 2015]. website. http://www.bls.gov/oes/current/oes_40340.htm#otherlinks. Page 21 of 30_Wi. [Google Scholar]
- 19.National Occupational Employment and Wage Estimates by ownership; cross-industry, private ownership only. US Bureau of Labor Statitstics; May, 2013. [Accessed February 28, 2015]. website. http://www.bls.gov/oes/current/000001.htm. [Google Scholar]
- 20.US. [Accessed Jun 29th, 2015];Discover America in a New Century, Resident Segregation. 2010 http://www.s4.brown.edu/us2010/segregation2010/Default.aspx?msa=10180.
- 21.Juhn YJ, Beebe TJ, Finnie DM, et al. Development and initial testing of a new socioeconomic status measure based on housing data. J Urban Health. 2011 Oct;88(5):933–944. doi: 10.1007/s11524-011-9572-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Johnson MD, Urm SH, Jung JA, et al. Housing data-based socioeconomic index and risk of invasive pneumococcal disease: an exploratory study. Epidemiol Infect. 2013 Apr;141(4):880–887. doi: 10.1017/S0950268812001252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bang DW, Manemann SM, Gerber Y, et al. A Novel Socioeconomic Measure Using Individual Housing Data in Cardiovascular Outcome Research. Int J Env Res Pub He. 2014 Nov;11(11):11597–11615. doi: 10.3390/ijerph111111597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Juhn Y, Krusemark E, Rand-Weaver J, et al. A novel measure of socioeconomic status using individual housing data in health disparities research for asthma in adults. Allergy. 2014 Sep;69:327–327. [Google Scholar]
- 25.Harris MN, Lundien MC, Finnie DM, et al. Application of a novel socioeconomic measure using individual housing data in asthma research: an exploratory study. Npj Prim Care Resp M. 2014 Jun 26;24 doi: 10.1038/npjpcrm.2014.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ghawi H, Crowson CS, Rand-Weaver J, Krusemark E, Gabriel SE, Juhn YJ. A novel measure of socioeconomic status using individual housing data to assess the association of SES with rheumatoid arthritis and its mortality: a population-based case-control study. BMJ Open. 2015;5(4):e006469. doi: 10.1136/bmjopen-2014-006469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. [Accessed June 5, 2015];Census Urban and Rural Classification and Urban Area Criteria. 2010 https://www.census.gov/geo/reference/ua/urban-rural-2010.html.
- 28.United States Census Bureau. [Accessed February 28, 2015];State & County QuickFacts. http://quickfacts.census.gov/qfd/states/00000.html.
- 29.Health Resources and Services Administration, U.S. Department of Health and Human Services. [Accessed 10/15/2014]; http://muafind.hrsa.gov/index.aspx.
- 30.Olmsted County, Minnesota Community Health Needs Assessment. [Accessed 10/15/2014];2013 http://www.co.olmsted.mn.us/OCPHS/reports/Documents/Community%20Health%20Needs%20Assessment%202013.pdf.
- 31.St Sauver JL, Grossardt BR, Leibson CL, Yawn BP, Melton LJ, 3rd, Rocca WA. Generalizability of epidemiological findings and public health decisions: an illustration from the Rochester Epidemiology Project. Mayo Clin Proc. 2012 Feb;87(2):151–160. doi: 10.1016/j.mayocp.2011.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.St Sauver JL, Grossardt BR, Yawn BP, Melton LJ, Rocca WA. Use of a Medical Records Linkage System to Enumerate a Dynamic Population Over Time: The Rochester Epidemiology Project. Am J Epidemiol. 2011 May 1;173(9):1059–1068. doi: 10.1093/aje/kwq482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rocca WA, Yawn BP, St Sauver JL, Grossardt BR, Melton LJ., 3rd History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012 Dec;87(12):1202–1213. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.The High Concentration of US Health Care Expenditures. [Accessed May 19, 2012];Agency for Health Care Research and Quality, US Department of Health and Human Services. 2006 at http://www.ahrq.gov/research/ria19/expendria.htm.
- 35.St Sauver JL, Warner DO, Yawn BP, et al. Why patients visit their doctors: assessing the most prevalent conditions in a defined American population. Mayo Clin Proc. 2013 Jan;88(1):56–67. doi: 10.1016/j.mayocp.2012.08.020. Page 22 of 30_Wi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Quality AfHRa. [Accessed November 18, 2014];Medical Expenditure Panel Survey HC-120, Appendix 3: Clinical Classification Code to ICD-9-CM Code Crosswalk. http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h120/h120_icd9codes.shtml.
- 37.Quality AfHRa. [Accessed November 18, 2014];Healthcare Cost and Utilization Project: Clinical Classification Software (CCS) for ICD-9-CM. http://www.hcup-us.ahrq.gov/toolssoftware/ccs/ccs.jsp.
- 38.United States Census Bureau. [Accessed Sep 8, 2014];2010 http://factfinder2.census.gov/faces/tableservices/jsf/pages/productview.xhtml?src=bkmk.
- 39.(NIH) NIoH, editor Racial and Ethnic Categories and Definitions for NIH Diversity Programs and for Other Reporting Purposes - See more at: http://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-089.html#sthash.OD1zPDgj.dpuf.
- 40. [Accessed November 18, 2014];Segregation: Dissimilarity Indices. http://www.censusscope.org/us/rank_dissimilarity_white_black.html.
- 41.Health, United States. [Accessed November 18, 2014];2012 National Center for Health Statistics (CDC), 2007–2010. 2012 http://www.cdc.gov/nchs/data/hus/2012/064.pdf.
- 42.Prevalence of coronary heart disease--United States, 2006–2010. MMWR Morb Mortal Wkly Rep. 2011 Oct 14;60(40):1377–1381. [PubMed] [Google Scholar]
- 43.Schiller JS, Lucas JW, Peregoy JA. Summary health statistics for u.s. Adults: national health interview survey, 2011. Vital Health Stat. 2012 Dec;10(256):1–218. [PubMed] [Google Scholar]
- 44.Horwath E, Johnson J, Klerman GL, Weissman MM. Depressive symptoms as relative and attributable risk factors for first-onset major depression. Arch Gen Psychiatry. 1992 Oct;49(10):817–823. doi: 10.1001/archpsyc.1992.01820100061011. [DOI] [PubMed] [Google Scholar]
- 45.Jones DW, Chambless LE, Folsom AR, et al. Risk factors for coronary heart disease in African Americans: the atherosclerosis risk in communities study, 1987–1997. Arch Intern Med. 2002 Dec 9–23;162(22):2565–2571. doi: 10.1001/archinte.162.22.2565. [DOI] [PubMed] [Google Scholar]
- 46.Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime risk and persistence of psychiatric disorders across ethnic groups in the United States. Psychol Med. 2005 Mar;35(3):317–327. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.McDaniel M, Paxson C, Waldfogel J. Racial disparities in childhood asthma in the United States: Evidence from the National Health Interview Survey, 1997 to 2003. Pediatrics. 2006 May;117(5):E868–E877. doi: 10.1542/peds.2005-1721. [DOI] [PubMed] [Google Scholar]
- 48.Heisler M, Smith DM, Hayward RA, Krein SL, Kerr EA. Racial disparities in diabetes care processes, outcomes, and treatment intensity. Med Care. 2003 Nov;41(11):1221–1232. doi: 10.1097/01.MLR.0000093421.64618.9C. [DOI] [PubMed] [Google Scholar]
- 49.Hertz RP, Unger AN, Cornell JA, Saunders E. Racial disparities in hypertension prevalence, awareness, and management. Arch Intern Med. 2005 Oct 10;165(18):2098–2104. doi: 10.1001/archinte.165.18.2098. [DOI] [PubMed] [Google Scholar]
- 50.Shippee ND, Shah ND, May CR, Mair FS, Montori VM. Cumulative complexity: a functional, patient-centered model of patient complexity can improve research and practice. J Clin Epidemiol. 2012 Oct;65(10):1041–1051. doi: 10.1016/j.jclinepi.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 51.Yawn BP, Wollan P, St Sauver J. Comparing shingles incidence and complication rates from medical record review and administrative database estimates: how close are they? Am J Epidemiol. 2011 Nov 1;174(9):1054–1061. doi: 10.1093/aje/kwr206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Roger VL, Killian J, Henkel M, et al. Coronary disease surveillance in Olmsted County objectives and methodology. J Clin Epidemiol. 2002 Jun;55(6):593–601. doi: 10.1016/s0895-4356(02)00390-6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.