Summary
Objectives
The evidence linking socioeconomic status (SES) and adherence in cystic fibrosis (CF) is inconclusive and focused on medication uptake. We examined associations between SES, adherence to airway clearance therapy (ACT), and CF respiratory outcomes.
Study Design
Socioeconomic, clinical, and adherence data of CF patients (N = 110) at a single CF Center were evaluated in this cross-sectional observational study. SES was operationalized as maternal and paternal education and household income. Adherence to ACT was measured with utilization data from the high-frequency chest wall oscillation (HFCWO) device over 4–6 weeks. Statistical modeling was used to test three hypotheses: (H1) Higher SES is associated with higher ACT adherence; (H2) Higher SES is associated with better respiratory outcomes; and (H3) ACT adherence mediates the relationship between SES and respiratory outcomes.
Results
In multinomial logistic regression, maternal college education, annual income >$50,000, and more adults in the household were independently related to better adherence (P < 0.05). Paternal college education, income >$100,000, and lack of exposure to smoking were independently related to higher lung function (P < 0.05). Current adherence to ACT with HFCWO was not associated with lung function over 12 months.
Conclusions
SES is associated both with ACT adherence and respiratory outcomes in pediatric CF patients. However, the link between SES and respiratory outcomes in this study was not mediated by adherence to ACT with HFCWO. These data emphasize the importance of socioeconomic resources and household environment for CF health. Family socio-demographic profiles can help identify patients at increased risk for ACT nonadherence.
Keywords: adherence, airway clearance, cystic fibrosis, respiratory outcomes, socioeconomic status
INTRODUCTION
Cystic fibrosis (CF) is the second most common life-shortening genetic disorder in the United States. More than 75% of patients are diagnosed by age 2, and half of the CF patient population is under 18 years old.1 Daily airway clearance therapy (ACT), typically performed in conjunction with inhaled bronchodilators, mucolytics, steroids, and/or antibiotics, is a standard component of the increasingly complex therapeutic regimen. Adherence to the full therapeutic protocol is critical for slowing down the disease process and preventing early death.2,3
It has been reported that CF patients of lower socioeconomic status (SES) have worse growth and lung function and are more likely to die younger than those of higher SES.4–9 In the United States, these socioeconomic disparities are not driven by differential use of health services,4,10,11 likely because a network of accredited CF care centers and multidisciplinary case management help address issues with access and quality of care, at least for pediatric CF patients. Lower adherence may be a contributor to the poorer outcomes among CF children of low SES, but the supporting evidence is mixed. While a relationship between SES and adherence has been reported in other chronic diseases,12,13 it has not been clearly established in CF.14,15 In addition, the majority of evidence on adherence in CF has focused on medication uptake rather than ACT, which is the most time-consuming and hardest to measure component of the daily therapeutic regimen.16–19 The present study aims to determine the relationship between SES and ACT adherence in pediatric CF patients, and to examine the role of ACT adherence for respiratory outcomes in this population.
The study was informed by Cockerham’s health lifestyle theory, which explicates the social origins of health behavior.20 It argues that health behaviors are constrained by social structures rather than freely chosen. Such social limitations include the individual’s socioeconomic circumstances (income, education, occupation), living conditions, race/ethnicity, age, gender, and belief system. The socioeconomic circumstances exert a particularly powerful influence, with people of lower SES less likely to engage in health-benefiting behaviors. Based on this theoretical framework, we hypothesized that: (H1) Higher SES is associated with higher ACT adherence; (H2) Higher SES is associated with better respiratory outcomes; and (H3) Adherence mediates the relationship between SES and respiratory outcomes.
METHODS
Study Population
The study population was comprised of pediatric patients with CF treated at the University of Alabama at Birmingham (UAB)/Children’s of Alabama CF Center (N = 287). Patients who perform ACT with high-frequency chest wall oscillation (HFCWO) (n = 161) were eligible to participate. Eligibility was limited to these patients because the HFCWO device (vest) features a built-in chronometer that records cumulative device utilization time, thereby offering an accurate and objective adherence measure. HFCWO is the most common method for ACT in the United States, used by 86% of CF patients age 6–18.1 The study was approved by the UAB Institutional Review Board for Human Use (Protocol X140124004).
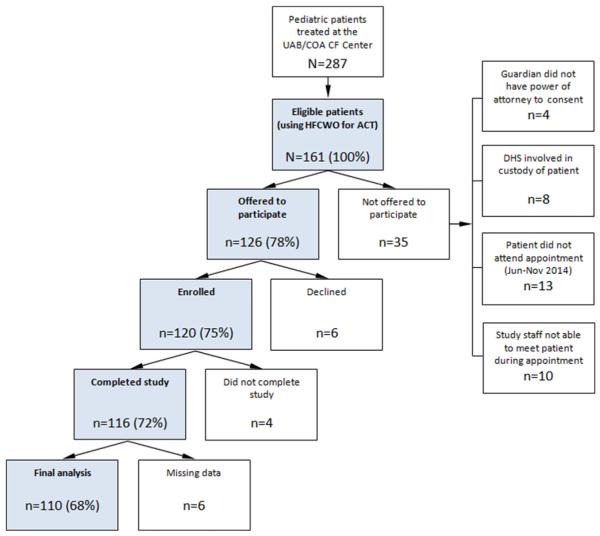
A flow chart of the study population is presented in Figure 1. Of all eligible patients (N = 161), 126 (78%) were offered to participate in the study. Participation was not offered when: (1) guardian(s) did not have a power of attorney to provide informed consent (n = 4, 3%); (2) the Department of Human Services was involved in the custody of a patient (n = 8, 5%); (3) a patient did not attend a routinely scheduled clinic appointment during the 6 months of study recruitment (Jun–Nov, 2014) (n = 13, 8%); or (4) study staff was not able to meet patient during appointment (n = 10; 6%). Of all patients who were offered to participate in the study (n = 126), 6 (5%) declined. Of those who enrolled (n = 120), 116 (97%) completed the study. Missing data resulted in the exclusion of 5% of observations (n = 6). The final analyses included 110 participants.
Fig. 1.
Study population.
Study Design
Data on the family’s demographic characteristics, SES indicators, and health behaviors were collected with a paper survey administered during a routine clinic visit. Patient clinical data were abstracted from the CF Patient Registry. Adherence data were obtained from the patient’s home HFCWO device (vest). HFCWO vests, regardless of model and manufacturer, are equipped with a built-in chronometer that records cumulative utilization time of the device (in hours and minutes). Two such readings were obtained from each patient’s HFCWO vest via telephone. The first reading was obtained within 2 days of study enrollment (or as soon as the family could be reached by telephone); the second reading was obtained 4 weeks after the baseline reading (or as soon after as the family could be reached). The difference between the two cumulative utilization readings, divided by the number of days between them, provided an average daily use of the HFCWO vest. In case of hospitalizations, the number of inpatient days was subtracted from the number of days between the two readings.
Measures
Adherence
Adherence rate was represented as a ratio (%) between the average daily use (see above) and the prescribed daily use of the HFCWO vest. Information on prescribed daily use was provided by the CF Center respiratory therapist. Adherence rates were coded in three categories: low (<35%), medium (36–79%), and high (≥80%).21
Socioeconomic Status
Mother’s and father’s education and annual household income were queried with the paper survey. Answers were grouped into three educational categories (≤ high school; some college experience but no degree; college degree) and three income categories (<$50,000; $50,000– $100,000; >$100,000).
Respiratory Status
Lung function was reported as percent of the predicted forced expiratory volume in 1 sec (FEV1%) recorded in the CF Patient Registry, in which FEV1% predicted values are estimated based on Wang equations22 for males ages 6–17 years and females ages 6–15 years, and with Hankinson equations23 for males ages 18 and older and females ages 16 and older. Mean value of FEV1% in the preceding 12 months was calculated for each patient. Mean FEV1% values were coded in three categories based on median lung function in patients age 6–17: below average (<85), average (85–99), and above average (≥100).1
Control Variables
Socio-demographic factors included race, gender, and marital status of the parent/caregiver, caregiver and patient age, number of adults in the household, and health insurance (private vs. public). Patient clinical characteristics included nutritional status (BMI percentiles calculated from the 2000 CDC growth charts; scores were coded as a binary variable (<50%, ≥50%) in concordance with the CF Foundation nutritional guidelines),24 hospitalizations in 12 months (0, 1, ≥2), genotype (coded as delta-F508 homozygous, delta-F508 heterozygous, and Other), P. aeruginosa status, CF-related diabetes, asthma, depression, and other comorbidities (0, 1, ≥2).
Statistical Analysis
Univariate statistics, including means, standard deviations, frequencies, and proportions, were obtained for all non-missing cases. Bivariate relationships were estimated between lung function and every SES measure (father’s education, mother’s education, household income), between adherence and every SES measure, and between adherence and lung function. Associations were estimated with analysis of variance (ANOVA), simple linear regression, or cross-tabulation using Pearson’s chi-square for cells with >5 observations and Fisher’s exact statistics for cells with ≥ observations. Strength of the association was assessed with Gamma or Cramer’s V test depending on the variable level.
To test the study hypotheses, multivariate statistical modeling was used. Separate multinomial logistic regression models were estimated for adherence and lung function. Each model included all SES indicators (mother’s education, father’s educations, household income) and controlled for all variables that were significant (P < 0.05) in the bivariate analyses: health insurance, number of adults in household, smoking in household, patient age, and patient depression. Statistical tests were two-sided and were conducted using a 5% significance level (α = 0.05). Analyses were performed with Stata software, version 12.
RESULTS
Socio-Demographic Characteristics
The socio-demographic characteristics of study participants are presented in Table 1. The racial/ethnic makeup of caregivers (92% white non-Latino) reflects the composition of the U.S. population with CF. Most caregivers (85%) were female, consistent with reports of gender imbalance among caregivers of children with chronic conditions, whereby mothers act as the default caregiver while fathers assume a supporting role.25–27 The majority of parents/caregivers were married/cohabiting (85%, n = 94). Mean parent/caregiver age was 41 years (range 26–72); mean patient age was 11 years (range 2–19). Mothers were better educated than fathers (P < 0.001), with 41% (n = 45) versus 34% (n = 37) having a college degree, and 21% (n = 23) versus 35% (n = 38) having high-school education or less. Forty-one percent of households (n = 45) had income <$50,000, and 25% (n = 27) included a smoker.
TABLE 1.
Characteristics of Study Participants (N=110)
| Variable | % | Mean (SD) |
|---|---|---|
| Socio-demographic | ||
| Caregiver: White | 91.82 | — |
| Caregiver: Female | 84.55 | — |
| Caregiver: Married/Cohabiting | 85.45 | — |
| Caregiver: Age (years) | — | 41.14 (8.01) |
| Patient: Age (years) | — | 11.19 (4.72) |
| Education: Father | ||
| ≤High school | 34.55 | — |
| Some college | 31.82 | — |
| Bachelor’s or higher | 33.64 | — |
| Education: Mother | ||
| ≤High school | 20.91 | — |
| Some college | 38.18 | — |
| Bachelor’s or higher | 40.91 | — |
| Household income | ||
| <$50,000 | 40.91 | — |
| $50,000–100,000 | 34.55 | — |
| >$100,000 | 24.55 | — |
| Adults in household | ||
| 1 | 10.91 | — |
| 2 | 70.91 | — |
| 3 | 13.64 | — |
| ≥4 | 4.55 | — |
| Smoking in household | 24.55 | — |
| Health insurance | ||
| Private | 64.55 | |
| Public | 35.45 | — |
| Clinical | ||
| FEV1% | ||
| <85 | 21.82 | — |
| 85–99 | 34.55 | — |
| ≥100 | 27.27 | — |
| N/A (age <6) | 16.36 | — |
| BMI | ||
| <50 | 38.18 | — |
| ≥50 | 61.82 | — |
| Hospitalizations | ||
| None | 51.82 | — |
| One | 21.82 | — |
| ≥Two | 26.36 | — |
| Genotype | ||
| ΔF508 homozygous | 52.73 | — |
| ΔF508 heterozygous | 38.18 | — |
| P. aeruginosa | 36.36 | — |
| Asthma | 75.45 | — |
| CF-Related diabetes | 14.55 | — |
| Depression | 12.73 | — |
| Other comorbidities | ||
| 0 | 30.00 | — |
| 1 | 33.64 | — |
| ≥2 | 36.36 | — |
| Adherence | ||
| Adherence rate | 60.56 (30.95) | |
| ≤35% | 28.18 | — |
| 36–79% | 37.27 | — |
| 80–100% | 34.55 | — |
Clinical Characteristics
The clinical characteristics of the sample (Table 1) were consistent with those reported nationally.1,28,29 Lung function was split fairly evenly across three groups: FEV1 85–99 (35%, n = 38), FEV1 <85 (22%, n = 24), FEV1 ≥100 (27%, n = 30). Lung function was not reported on patients younger than age 6 (16% of the sample).
Adherence to ACT
Based on utilization data from the patients’ HFCWO vests, the mean adherence rate was 61% (Table 1). One-third of all patients (35%, n = 38) were highly adherent (≥80%), and 28% (n = 31) were nonadherent (≤35%). Mean time between the two utilization readings was 37 days.
Bivariate Statistics
A series of significant associations were observed between SES measures, adherence, and CF respiratory outcomes. Specifically, adherence was positively associated with mother’s education (γ = 0.14, P < 0.01) and household income (γ = 0.22, P < 0.05), while lung function was positively associated with father’s education (γ = 0.03, P < 0.05) and household income (χ = 0.04, P < 0.01). Adherence, however, was not correlated with lung function. Smoking was negatively associated with both father’s education (γ = 0.45, P < 0.01) and mother’s education (γ = 0.47, P < 0.05).
Multivariate Models
ACT Adherence as a Function of SES
Table 2 shows results of the multinomial logistic regression model that tests Hypothesis 1: “Higher SES is associated with higher ACT adherence.” The results provide support for this hypothesis. Compared to patients whose mothers have high-school education or less, patients whose mothers have college experience or college degree are respectively 5 and 7 times more likely to have medium rather than low adherence (P < 0.05). Compared to household income <$50,000, incomes of $50,000–100,000 and >$100,000 are associated respectively with an 11- and 9-fold increase in the likelihood of having high rather than low adherence (P < 0.05). Each additional adult in the household doubles the likelihood of having medium rather than low adherence (P < 0.05).
TABLE 2.
Adherence as a Function of SES
| RRR (SE) | [95%CI] | ||
|---|---|---|---|
| Medium Adherence (36–79%) vs. Low Adherence (≤35%) | |||
| SES variables | |||
| Father’s education1 | |||
| Some college | 0.28 (0.20) | 0.07 | 1.10 |
| College degree | 0.14* (0.11) | 0.03 | 0.67 |
| Mother’s education1 | |||
| Some college | 5.05* (3.98) | 1.08 | 23.70 |
| College degree | 6.81* (6.28) | 1.12 | 41.50 |
| Household income2 | |||
| $50,000–100,000 | 0.90 (0.71) | 0.19 | 4.21 |
| >$100,000 | 1.20 (1.09) | 0.20 | 7.15 |
| Control variables | |||
| Adults in household | 2.44* (1.14) | 0.99 | 6.08 |
| Smoking in household | 0.91 (0.63) | 0.23 | 3.57 |
| Health insurance | 0.82 (0.58) | 0.21 | 3.24 |
| Patient age | 0.89 (0.06) | 0.79 | 1.01 |
| Depression | 0.89 (0.72) | 0.19 | 4.31 |
| High Adherence (≥80%) vs. Low Adherence (≤35%) | |||
| SES variables | |||
| Father’s education1 | |||
| Some college | 0.24 (0.20) | 0.05 | 1.17 |
| College degree | 0.54 (0.45) | 0.11 | 2.74 |
| Mother’s education1 | |||
| Some college | 1.27 (1.04) | 0.25 | 6.35 |
| College degree | 1.73 (1.57) | 0.29 | 10.27 |
| Household income2 | |||
| $50,000–100,000 | 10.65* (9.51) | 1.85 | 61.32 |
| >$100,000 | 9.02* (8.74) | 1.35 | 60.20 |
| Control variables | |||
| Adults in household | 2.23 (1.10) | 0.85 | 5.88 |
| Smoking in household | 2.53 (1.79) | 0.63 | 10.12 |
| Health insurance | 2.81 (2.18) | 0.61 | 12.89 |
| Patient age | 0.93 (0.06) | 0.82 | 1.07 |
| Depression | 0.82 (0.70) | 0.15 | 4.32 |
Results of the multinomial logistic regression model (Adherence=SES+CVs+e) that tests Hypothesis 1: “Higher SES is associated with higher ACT adherence.”
N=110; RRR, Relative risk ratio; SE, Standard error; CI, Confidence interval.
P<0.05; Likelihood ratio chi2 (24)=38.19*.
Reference category is high school degree or less.
Reference category is <$50,000.
Lung Function as a Function of SES
Table 3 shows results of the multinomial logistic regression model that tests Hypothesis 2: “Higher SES is associated with better respiratory outcomes.” The results support this hypothesis. Patients whose fathers have college experience or college degree are respectively 7 and 8 times more likely to have medium rather than low lung function compared to patients whose fathers have high-school education or less (P < 0.05). Patients with household income >$100,000 are 13 times more likely to have high rather than low lung function compared to patients with household income <$50,000 (P < 0.05). Importantly, the presence of a smoker in the household decreases the likelihood of high lung function by 85% (P < 0.05).
TABLE 3.
Lung Function as a Function of SES
| RRR (SE) | [95%CI] | ||
|---|---|---|---|
| Medium Lung Function (FEV1 85-99) vs. Low Lung Function (FEV1 <85) | |||
| SES variables | |||
| Father’s education1 | |||
| Some college | 7.22* (6.03) | 1.40 | 37.10 |
| College degree | 8.12* (7.89) | 1.21 | 54.57 |
| Mother’s education1 | |||
| Some college | 0.81 (0.74) | 0.14 | 4.82 |
| College degree | 0.29 (0.32) | 0.03 | 2.51 |
| Household income2 | |||
| $50,000–100,000 | 0.96 (0.86) | 0.16 | 5.59 |
| >$100,000 | 4.63 (5.42) | 0.47 | 45.96 |
| Control variables | |||
| Adults in household | 0.88 (0.51) | 0.28 | 2.76 |
| Smoking in household | 0.51 (0.40) | 0.11 | 2.38 |
| Health insurance | 0.58 (0.48) | 0.11 | 2.98 |
| Patient age | 0.95 (0.09) | 0.80 | 1.14 |
| Depression | 0.54 (0.44) | 0.11 | 2.69 |
| High Lung Function (FEV1 ≥100) vs. Low Lung Function (FEV1 <85) | |||
| SES variables | |||
| Father’s education1 | |||
| Some college | 0.77 (0.76) | 0.11 | 5.34 |
| College degree | 0.60 (0.64) | 0.07 | 4.94 |
| Mother’s education1 | |||
| Some college | 0.54 (0.56) | 0.07 | 4.07 |
| College degree | 0.57 (0.67) | 0.06 | 5.72 |
| Household income2 | |||
| $50,000–100,000 | 2.18 (2.13) | 0.32 | 14.85 |
| >$100,000 | 13.09* (16.07) | 1.18 | 145.30 |
| Control variables | |||
| Adults in household | 2.48 (1.47) | 0.78 | 7.91 |
| Smoking in household | 0.15* (0.14) | 0.02 | 0.97 |
| Health insurance | 0.45 (0.41) | 0.07 | 2.70 |
| Patient age | 0.89 (0.09) | 0.73 | 1.09 |
| Depression | 0.00 (0.00) | 0.00 | |
Results of the multinomial logistic regression model (Lung Function=SES+CVs+e) that tests Hypothesis 2: “Higher SES is associated with better respiratory outcomes.”
N=110; RRR, Relative risk ratio; SE, Standard error; CI, Confidence interval.
P<0.05; Likelihood ratio chi2 (36)=150.46***.
Reference category is high-school degree or less.
Reference category is <$50,000.
Lung Function as a Function of Adherence
An association between current adherence to HFCWO and lung function over 12 months was not observed in the study (Table 4). In the absence of a relationship between adherence and lung function, we find no support for Hypothesis 3: “Adherence mediates the relationship between SES and respiratory outcomes.” Among the control variables, each additional adult in the household increases the likelihood of high rather than low lung function nearly 4 times (P < 0.05). Exposure to smoking decreases the likelihood of high lung function by 85% (P < 0.05).
TABLE 4.
Lung Function as a Function of Adherence
| RRR (SE) | [95%CI] | ||
|---|---|---|---|
| Medium lung function (FEV1 85–99) vs. low lung function (FEV1 <85) | |||
| Adherence1 | |||
| Medium (36–79) | 0.26 (0.19) | 0.06 | 1.11 |
| High (≥80) | 0.48 (0.36) | 0.11 | 2.09 |
| Control variables | |||
| Adults in household | 1.59 (0.84) | 0.57 | 4.48 |
| Smoking in household | 0.39 (0.27) | 0.10 | 1.51 |
| Health insurance | 0.35 (0.22) | 0.11 | 1.17 |
| Patient age | 0.91 (0.08) | 0.77 | 1.08 |
| Depression | 0.48 (0.36) | 0.11 | 2.08 |
| High Lung Function (FEV1 ≥100) vs. Low Lung Function (FEV1 <85) | |||
| Adherence 1 | |||
| Medium (36–79) | 0.66 (0.58) | 0.12 | 3.69 |
| High (≥80) | 1.17 (1.05) | 0.20 | 6.83 |
| Control variables | |||
| Adults in household | 3.81* (2.32) | 1.15 | 12.60 |
| Smoking in household | 0.15* (0.13) | 0.03 | 0.83 |
| Health insurance | 0.37 (0.26) | 0.09 | 1.45 |
| Patient age | 0.88 (0.09) | 0.73 | 1.07 |
| Depression | 0.00 (0.00) | 0.00 | |
Results of the multinomial logistic regression model (Lung Function=Adherence+CVs+e) that tests the association between adherence and lung function. No such association is found. Hypothesis 3: “Adherence mediates the relationship between SES and respiratory outcomes” cannot be supported.
N=110; RRR, Relative risk ratio; SE, Standard error; CI, Confidence interval.
P<0.05; Likelihood ratio chi2 (24)=134.14***.
Reference category is low adherence (≤35).
DISCUSSION
Informed by the health lifestyle theory, which maintains that health behaviors are shaped by socioeconomic conditions,20 this study sought to answer the questions: (1) Does SES influence ACT adherence? (2) Does SES influence CF respiratory outcomes, and (3) Does ACT adherence mediate the relationship between SES and CF respiratory outcomes?
The statistical models present evidence for a link between SES and adherence to ACT. Specifically, both maternal college education and high household income are associated with better utilization of HFCWO vests. While maternal college education is linked to medium adherence, high income is associated with high adherence. This finding is an important contribution to the adherence literature in CF, which so far has provided limited or inconclusive evidence for a socioeconomic basis of the adherence behavior. Our data suggest that the SES–adherence association observed in other chronic diseases30–33 exists in CF, specifically for ACT with HFCWO vest.
The study concurred with previous reports of association between SES and pulmonary health.5,9,34,35 It showed that both paternal college education and high household income are associated with better respiratory outcomes. While paternal college education is significantly associated with medium lung function, household income >$100,000 is significantly associated with high lung function. It is possible that the mother, a default caregiver, drives the health behaviors in relation to CF, while the father, a default income provider, drives the CF respiratory outcomes, likely through his earning potential. This interpretation needs to be tested in future work.
The parallels in the respective effects of education and income on adherence and respiratory outcomes are noteworthy. Our analyses show that college education is associated with medium adherence and medium lung function, while high income is associated with high adherence and high lung function.
Adherence and lung function were linked not only to education and income, but also to the number of adults in the household. Every additional adult beyond the first one doubled the likelihood of medium adherence and quadrupled the likelihood of high lung function. These results provide further evidence for the importance of family structure in the management of a pediatric chronic condition.36,37 Since the responsibility for daily treatments remains with the adults in the household, supportive family structure (more adult caregivers) is associated with higher adherence. This finding is not surprising considering the high treatment burden in CF.19 Our data therefore indicate that one-adult families are at increased risk for suboptimal adherence.
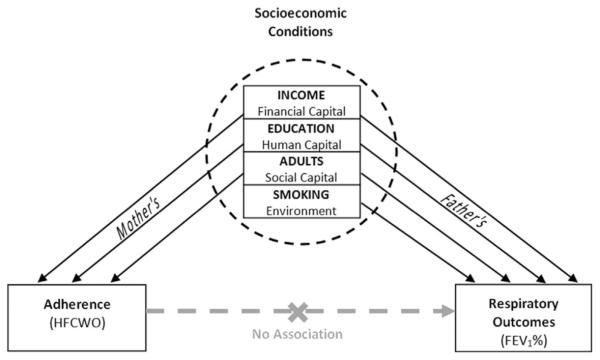
The study is among few in CF research to assess SES by more than one indicator and to measure access to a variety of resources: human capital (education), financial capital (household income), and social capital (family structure and number of caregivers).7 As demonstrated by the results, these SES indicators are differently associated with ACT adherence and respiratory outcomes. Access to human capital (college education) is protective against low ACT adherence and poor lung health. Access to financial capital (high household income) promotes high ACT adherence and optimal lung health. Access to social capital (family structure and number of caregivers) protects against low ACT adherence and further improves lung health. Smoking, a covariate of low SES, decreases the likelihood of high lung function by 85%. These findings, summarized in Figure 2, suggest that SES is a multidimensional construct: while its components are correlated, they are not interchangeable and contribute independently to respiratory outcomes in CF. While this conclusion is well-established in the sociological and general medical literature,38,39 it has not been sufficiently explored in CF research.
Fig. 2.
Framework of study findings.
A relationship between current adherence to ACT with HFCWO and pulmonary function over the preceding 12 months was not observed in the study. We interpret this finding as affirming the importance of socioeconomic resources and household environment over and beyond adherence to therapy. However, several study limitations may have contributed to the reported lack of association between ACT adherence and lung function. First, ACT adherence data were collected prospectively, while pulmonary data were collected retrospectively; it is possible that current ACT adherence is not indicative of past ACT adherence. Additionally, an indication bias, or confounding by severity of disease, may have resulted in patients with less severe disease to be less adherent to ACT. Conclusions regarding the long-term efficacy of ACT with HFCWO40 are beyond the scope of this study. Rather, our results should be construed to highlight the role of socioeconomic factors and household environment, both for adherence to ACT and pulmonary health.
The study is limited in that it includes about half of the pediatric CF patients (or about 70% of those who use a HFCWO vest) in a single CF center. The study population may not be representative of all pediatric CF patients, both in this and other CF centers. A multi-center study is necessary to establish a link between SES and ACT in a nationally representative sample. Additionally, the small study size may have resulted in over-modeling, as suggested by several wide confidence intervals (Tables 2 and 3). Finally, utilization data from the HFCWO device were collected by phone, as HFCWO vests are not equipped for direct data transmission. Participants were not informed when study staff will call to record a reading, either baseline or follow-up; on many occasions, the follow-up reading was provided by a different individual (parent/caregiver or patient) than the one providing the baseline reading. Despite these measures to rule out information bias, it is possible, though unlikely, that more educated parents/caregivers have inflated the follow-up reading to over-report usage. Future studies may consider direct data collection from the HFCWO device instead of parent/caregiver report of such data.
As a form of health behavior, adherence is practiced in socioeconomic, cultural, and family contexts that determine what behavioral options are both available and appropriate. Access to financial (income), human (education), and social (family structure and networks) resources exerts powerful influence on a parent/caregiver’s ability to perform complex and time-consuming daily therapies. Without regards to these underlying factors that generate and reproduce the behavior, adherence-promoting interventions may have limited success.
CONCLUSIONS
SES is associated both with ACT adherence and respiratory outcomes in pediatric CF patients. While low maternal education, low household income, and one-adult family structure are risk factors for low ACT adherence in this population, low paternal education, low household income, and second-hand smoke are risk factors for low respiratory outcomes. These findings emphasize the importance of socioeconomic resources and household environment for CF health. Clinicians can use the results to identify CF patients at increased risk for ACT nonadherence based on the family’s socio-demographic profile.
ACKNOWLEDGMENTS
This study was supported by the UAB Gregory Fleming James Cystic Fibrosis Research Center. Special thanks are offered to its then-director, Dr. Eric Sorscher. Thanks to LaCrecia Britton, RN, MSN, for facilitating this study.
ABBREVIATIONS
- ACT
airway clearance therapy
- BMI
p mass index
- CF
cystic fibrosis
- FEV1
forced expiratory volume in 1 second
- HFCWO
high frequency chest wall oscillation
- SES
socioeconomic status
Footnotes
Conflict of interest: None.
REFERENCES
- 1.Cystic Fibrosis Foundation Patient Registry: 2013 Annual Data Report to Center Directors . Cystic Fibrosis Foundation; Bethesda, Maryland: 2014. [Google Scholar]
- 2.Eakin MN, Bilderback A, Boyle MP, Mogayzel PJ, Riekert KA. Longitudinal association between medication adherence and lung health in people with cystic fibrosis. J Cystic Fibrosis. 2011;10:258–264. doi: 10.1016/j.jcf.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Schechter MS, Shelton BJ, Margolis PA, Fitzsimmons SC. The association of socioeconomic status with outcomes in cystic fibrosis patients in the United States. Am J Respir Crit Care Med. 2001;163:1331–1337. doi: 10.1164/ajrccm.163.6.9912100. [DOI] [PubMed] [Google Scholar]
- 5.Barr HL, Britton J, Smyth AR, Fogarty AW. Association between socioeconomic status, sex, and age at death from cystic fibrosis in England and Wales (1959 to 2008): cross sectional study. BMJ. 2011;343:d4662. doi: 10.1136/bmj.d4662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.O’Connor GT, Quinton HB, Kneeland T, Kahn R, Lever T, Maddock J, Robichaud P, Detzer M, Swartz DR. Median household income and mortality rate in cystic fibrosis. Pediatrics. 2003;111:e333–e339. doi: 10.1542/peds.111.4.e333. [DOI] [PubMed] [Google Scholar]
- 7.Balmer DF, Schall JI, Stallings VA. Social disadvantage predicts growth outcomes in preadolescent children with cystic fibrosis. J Cyst Fibros. 2008;7:543–550. doi: 10.1016/j.jcf.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Taylor-Robinson D, Whitehead M, Diggle P, Smyth R. The effect of social deprivation on weight in the UK cystic fibrosis population. J Epidemiol Community Health. 2011;65:A389–A389. [Google Scholar]
- 9.Taylor-Robinson DC, Smyth RL, Diggle PJ, Whitehead M. The effect of social deprivation on clinical outcomes and the use of treatments in the UK cystic fibrosis population: a longitudinal study. Lancet Respir Med. 2013;1:121–128. doi: 10.1016/S2213-2600(13)70002-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schechter MS, McColley SA, Silva S, Haselkorn T, Konstan MW, Wagener JS. Investigators, coordinators of the epidemiologic study of cystic F, North American Scientific Advisory Group for E. Association of socioeconomic status with the use of chronic therapies and healthcare utilization in children with cystic fibrosis. J Pediatr. 2009;155:634–639. doi: 10.1016/j.jpeds.2009.04.059. e1–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schechter MS, McColley SA, Regelmann W, Millar SJ, Pasta DJ, Wagener JS, Konstan MW, Morgan WJ. Investigators, coordinators of the epidemiologic study of Cystic F. Socioeconomic status and the likelihood of antibiotic treatment for signs and symptoms of pulmonary exacerbation in children with cystic fibrosis. J Pediatr. 2011;159:819–824. doi: 10.1016/j.jpeds.2011.05.005. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Apter AJ, Reisine ST, Affleck G, Barrows E, ZuWallack RL. Adherence with twice-daily dosing of inhaled steroids. Socioeconomic and health-belief differences. Am J Respir Crit Care Med. 1998;157:1810–1817. doi: 10.1164/ajrccm.157.6.9712007. [DOI] [PubMed] [Google Scholar]
- 13.Rapoff MA, Belmont JM, Lindsley CB, Olson NY. Electronically monitored adherence to medications by newly diagnosed patients with juvenile rheumatoid arthritis. Arthritis Rheum. 2005;53:905–910. doi: 10.1002/art.21603. [DOI] [PubMed] [Google Scholar]
- 14.Pendleton DA, David TJ. The compliance conundrum in cystic fibrosis. J R Soc Med. 2000;93:9–13. [PMC free article] [PubMed] [Google Scholar]
- 15.Schechter MS. Non-genetic influences on cystic fibrosis lung disease: the role of sociodemographic characteristics, environmental exposures, and healthcare interventions. Semin Respir Crit Care Med. 2003;24:639–652. doi: 10.1055/s-2004-815660. [DOI] [PubMed] [Google Scholar]
- 16.Llorente RPA, Garcia CB, Martin JJD. Treatment compliance in children and adults with Cystic Fibrosis. J Cyst Fibros. 2008;7:359–367. doi: 10.1016/j.jcf.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 17.Myers LB, Horn SA. Adherence to chest physiotherapy in adults with cystic fibrosis. J Health Psychol. 2006;11:915–926. doi: 10.1177/1359105306069093. [DOI] [PubMed] [Google Scholar]
- 18.Quittner AL, Espelage DL, Ievers-Landis C, Drotar D. Measuring adherence to medical treatments in childhood chronic illness: considering multiple methods and sources of information. J Clin Psychol Med S. 2000;7:41–54. [Google Scholar]
- 19.Sawicki GS, Sellers DE, Robinson WM. High treatment burden in adults with cystic fibrosis: challenges to disease self-management. J Cyst Fibros. 2009;8:91–96. doi: 10.1016/j.jcf.2008.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cockerham WC. Health lifestyle theory and the convergence of agency and structure. J Health Soc Behav. 2005;46:51–67. doi: 10.1177/002214650504600105. [DOI] [PubMed] [Google Scholar]
- 21.Modi AC, Cassedy AE, Quittner AL, Accurso F, Sontag M, Koenig JM, Ittenbach RF. Trajectories of adherence to airway clearance therapy for patients with cystic fibrosis. J Pediatr Psychol. 2010;35:1028–1037. doi: 10.1093/jpepsy/jsq015. [DOI] [PubMed] [Google Scholar]
- 22.Wang XB, Dockery DW, Wypij D, Fay ME, Ferris BG. Pulmonary-Function between 6 and 18 Years of Age. Pediatric Pulmonology. 1993;15:75–88. doi: 10.1002/ppul.1950150204. [DOI] [PubMed] [Google Scholar]
- 23.Hankinson JL, Odencrantz JR, Fedan KB. Spirometric reference values from a sample of the general U.S. population. Am J Respir Crit Care Med. 1999;159:179–187. doi: 10.1164/ajrccm.159.1.9712108. [DOI] [PubMed] [Google Scholar]
- 24.Stallings VA, Stark LJ, Robinson KA, Feranchak AP, Quinton H. Clinical Practice Guidelines on G, Nutrition S, Ad Hoc Working G. Evidence-based practice recommendations for nutrition-related management of children and adults with cystic fibrosis and pancreatic insufficiency: results of a systematic review. J Am Diet Assoc. 2008;108:832–839. doi: 10.1016/j.jada.2008.02.020. [DOI] [PubMed] [Google Scholar]
- 25.Williams B, Mukhopadhyay S, Dowell J, Coyle J. From child to adult: an exploration of shifting family roles and responsibilities in managing physiotherapy for cystic fibrosis. Soc Sci Med. 2007;65:2135–2146. doi: 10.1016/j.socscimed.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 26.Sullivan-Bolyai S, Rosenberg R, Bayard M. Fathers’ reflections on parenting young children with type 1 diabetes. Am J Maternal Child Nursing. 2006;31:24–31. doi: 10.1097/00005721-200601000-00007. [DOI] [PubMed] [Google Scholar]
- 27.Ojmyr-Joelsson M, Nisell M, Frenckner B, Rydelius PA, Christensson K. A gender perspective on the extent to which mothers and fathers each take responsibility for care of a child with high and intermediate imperforate anus. J Pediatr Nursing. 2009;24:207–215. doi: 10.1016/j.pedn.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 28.Rosenfeld M, Ramsey BW, Gibson RL. Pseudomonas acquisition in young patients with cystic fibrosis: pathophysiology, diagnosis, and management. Curr Opin Pulm Med. 2003;9:492–497. doi: 10.1097/00063198-200311000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Moran A, Dunitz J, Nathan B, Saeed A, Holme B, Thomas W. Cystic fibrosis-related diabetes: current trends in prevalence, incidence, and mortality. Diabetes Care. 2009;32:1626–1631. doi: 10.2337/dc09-0586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kalkan K, Bacciogly K, Kalpakliogly AF. Allergic rhinitis: can we identify nonadherence to therapy and its predictors easily in daily practice? J Investig Allergol Clin Immunol. 2013;23:315–322. [PubMed] [Google Scholar]
- 31.Rust G, Zhang S, Reynolds J. Inhaled corticosteroid adherence and emergency department utilization among Medicaid-enrolled children with asthma. J Asthma. 2013;50:769–775. doi: 10.3109/02770903.2013.799687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lemstra M, Blackburn D, Crawley A, Fung R. Proportion and risk indicators of nonadherence to statin therapy: a meta-analysis. Can J Cardiol. 2012;28:574–580. doi: 10.1016/j.cjca.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 33.DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 34.Schechter MS. Nongenetic influences on cystic fibrosis outcomes. Curr Opin Pulm Med. 2011;17:448–454. doi: 10.1097/MCP.0b013e32834ba899. [DOI] [PubMed] [Google Scholar]
- 35.Schechter MS. Wealth as a disease modifier in cystic fibrosis. Lancet Respir Med. 2013;1:93–95. doi: 10.1016/S2213-2600(13)70014-6. [DOI] [PubMed] [Google Scholar]
- 36.Rand CS, Nides M, Cowles MK, Wise RA, Connett J. Long-term metered-dose inhaler adherence in a clinical trial. The Lung Health Study Research Group. Am J Respir Crit Care Med. 1995;152:580–588. doi: 10.1164/ajrccm.152.2.7633711. [DOI] [PubMed] [Google Scholar]
- 37.Trivedi RB, Bryson CL, Udris E, Au DH. The influence of informal caregivers on adherence in COPD patients. Ann Behav Med. 2012;44:66–72. doi: 10.1007/s12160-012-9355-8. [DOI] [PubMed] [Google Scholar]
- 38.Braveman PA, Cubbin C, Egerter S, Chideya S, Marchi KS, Metzler M, Posner S. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 39.Adler NE, Rehkopf DH. U.S. disparities in health: descriptions, causes, and mechanisms. Annu Rev Public Health. 2008;29:235–252. doi: 10.1146/annurev.publhealth.29.020907.090852. [DOI] [PubMed] [Google Scholar]
- 40.Warnock L, Gates A, van der Schans CP. Chest physiotherapy compared to no chest physiotherapy for cystic fibrosis. Cochrane Database Syst Rev. 2013;9:CD001401. doi: 10.1002/14651858.CD001401.pub2. [DOI] [PubMed] [Google Scholar]