Abstract
Background
It is well documented that meeting the guideline levels (150 minutes per week) of moderate-to-vigorous physical activity (PA) is protective against chronic disease. Conversely, emerging evidence indicates the deleterious effects of prolonged sitting. Therefore, there is a need to change both behaviors. Self-monitoring of behavior is one of the most robust behavior-change techniques available. The growing number of technologies in the consumer electronics sector provides a unique opportunity for individuals to self-monitor their behavior.
Objective
The aim of this study is to review the characteristics and measurement properties of currently available self-monitoring devices for sedentary time and/or PA.
Methods
To identify technologies, four scientific databases were systematically searched using key terms related to behavior, measurement, and population. Articles published through October 2015 were identified. To identify technologies from the consumer electronic sector, systematic searches of three Internet search engines were also performed through to October 1, 2015.
Results
The initial database searches identified 46 devices and the Internet search engines identified 100 devices yielding a total of 146 technologies. Of these, 64 were further removed because they were currently unavailable for purchase or there was no evidence that they were designed for, had been used in, or could readily be modified for self-monitoring purposes. The remaining 82 technologies were included in this review (73 devices self-monitored PA, 9 devices self-monitored sedentary time). Of the 82 devices included, this review identified no published articles in which these devices were used for the purpose of self-monitoring PA and/or sedentary behavior; however, a number of technologies were found via Internet searches that matched the criteria for self-monitoring and provided immediate feedback on PA (ActiGraph Link, Microsoft Band, and Garmin Vivofit) and sedentary time (activPAL VT, the Lumo Back, and Darma).
Conclusions
There are a large number of devices that self-monitor PA; however, there is a greater need for the development of tools to self-monitor sedentary time. The novelty of these devices means they have yet to be used in behavior change interventions, although the growing field of wearable technology may facilitate this to change.
Keywords: sitting time, physical activity, measurement, feedback, activity monitor, scoping review
Introduction
Modern environments and technological advancements have radically altered the way we live our lives [1]. The need to undertake purposeful physical activity (PA) has all but disappeared and sedentary behavior, defined as “any waking behavior in a sitting or reclining posture with an energy expenditure ≤1.5 metabolic equivalent” [2] is the dominant behavior. Low levels of moderate-to-vigorous PA (MVPA) have been consistently associated with the risk of developing chronic diseases, such as type 2 diabetes, cardiovascular disease, and some cancers [3]. In addition, increasing the total level of daily movement, such as the number of steps taken, has been strongly inversely associated with the risk of developing chronic diseases [4,5]. There is also mounting evidence that the amount of time spent sedentary is an important determinant of health status independent of PA levels. For example, Wilmot and colleagues [6] found that when comparing those with the highest levels of sedentary behavior to those with the lowest levels, independent of PA levels, there was a 112%, 147%, 90%, and 49% increase in the relative risk of type 2 diabetes, cardiovascular disease, cardiovascular mortality, and all-cause mortality, respectively. Moreover, how sedentary time and PA are accumulated throughout the day may also be important, with frequent breaks in sedentary behavior associated with a healthier metabolic profile [7]. This has necessitated a paradigm shift that focuses on both the accumulation of MVPA (the traditional focus of lifestyle interventions) and the importance of postural allocation throughout the waking hours.
Over the last decade, there has been a plethora of tools developed to support PA and sedentary behavior change, of which the greatest growth has been seen in self-monitoring tools. Self-monitoring is defined as “a person closely and deliberately monitors their own behavior” [8,9] and “allowing the modification of their behaviors to achieve predetermined goals or outcomes” [10] and has a strong theoretical foundation for behavior change. Self-regulation theory posits that self-monitoring precedes self-evaluation of progress made toward one’s goal and as well as preceding self-reinforcement of behavior for progress to be made [9]. Furthermore, Control Theory proposes that self-monitoring of behavior, setting goals, receiving feedback, and reviewing relevant goals with feedback work synergistically and are central to self-management and behavioral control [11,12]. Self-monitoring, therefore, can increase an individual’s personal responsibility, promote independence, and individuals can create their own pathways toward goal achievement by taking an active rather than passive role [13]. When included in behavior change interventions, self-monitoring has proven to be an effective behavior change strategy across a variety of behaviors, including smoking, diet, and PA, and it is considered a foundation of lifestyle behavior change interventions [12,14].
Traditionally, self-monitoring of PA and sedentary time occurred via paper-based journal methods [14]; more recently, the pedometer became a popular method of self-monitoring for interventions designed to increase PA. Individuals who used pedometers increased their PA by 26.9% from baseline activity levels [15]. Subsequently, advances in technology have led to a proliferation in the number of bodily worn electronic devices becoming available that go beyond simply measuring and providing feedback on the number of steps per day (eg, Fitbit, Jawbone). Along with PA, electronic devices are also starting to measure sitting time, provide real-time feedback, as well as encouraging interruptions in prolonged sitting. It has been suggested that the use of these electronic approaches to self-monitor might lessen the burden of traditional methods and may improve adherence to self-monitoring resulting in greater achievement toward behavioral goals [16].
This increased availability of electronic self-monitoring devices provides an opportunity for researchers to utilize these novel technologies as an aid for behavior change in PA and sedentary behavior on a large scale. Furthermore, wearable technologies are increasingly integrating health care systems. Recent reports from the National Information Board in a review of the National Health Service in the United Kingdom indicate the need for “citizens” to start playing a more active role in their health care by accessing, entering, and uploading data into their own online medical record. Under these new plans, citizens will be able to access and download their detailed medical records as well as contribute to it with information from their personal wearable technology or biosensors [17,18]. In addition, as more health care providers in the United States move to a value-based care system (ie, “reward points” for positive lifestyle alterations that can be redeemed for discounts on a range of products and/or activities), mobile technologies that promote health and well-being by engaging in important health behaviors (eg, increased MVPA) will continue to grow and have the potential to be an integral piece of future health care systems. In light of this, a review of the current tools used to self-monitor PA and/or sedentary time has the potential to be a valuable resource to researchers, clinicians, health care providers, and the general public.
Therefore, it seems timely to review the characteristics and measurement properties (eg, wear location, integrated sensors, outcomes measured) of currently available self-monitoring devices, both those marketed to consumers and those used in research settings, that have been (or could be) utilized in, or developed for, real-time self-monitoring of sedentary behavior and/or PA.
Methods
Searches
The search strategy was built around three groups of keywords: behavior (ie, PA and sedentary behavior), measurement, and population. A detailed description of the keywords used and method of combination can be found in Multimedia Appendix 1. For the purposes of this study, tools were deemed to measure sedentary time if they could measure the wearer’s sitting and/or reclining posture.
Scopus, Medline, Web of Science, and the Institute of Electrical and Electronic Engineers (IEEE) databases were searched using these keywords from the inception of the databases to October 1, 2015. In addition, manual searches of personal files were conducted and reference lists of primary studies were screened.
Internet Search Engines
Because of the rapid release of technology in the consumer electronic area, a grey literature search of relevant websites was conducted for technologies that allow for the self-monitoring of PA and sedentary time but may not have made it into the published research to date. Keywords based on the same groups as the database searches were used to search the Internet engines Google, Bing, and Yahoo. Searches were extracted for later review using a specialized browser plug-in. The first 200 search results from each search engine were extracted for further review; this was a pragmatic approach because it was deemed that results after the first 200 were either not relevant or repetitive. This ensured that the results were unaffected by the changing algorithms of Web search engines. Searches were completed on October 1, 2015.
Study Inclusion and Exclusion Criteria
Two sets of inclusion criteria were developed for research articles and websites. For inclusion in the review, studies were required to (1) include adults aged 18 years or older, (2) be published in English, and (3) describe a device that objectively self-monitors PA, physical inactivity, and/or sedentary time/sitting and can, or has the potential to, provide feedback to the user. Traditionally, there would also be a criteria based around study type; however, in order to obtain the widest variety of devices, this was not included.
For inclusion in the review, only websites from manufacturers were included (ie, blogs or consumer reviews pertaining to technologies of interest were excluded) and devices that had the ability to self-monitor and were available for purchase at the time of the review were included.
Data Extraction
Potentially relevant articles were selected by screening titles, screening abstracts, and if abstracts were not available or did not provide sufficient data, the entire article was sought and screened to determine whether it met the inclusion criteria. Relevant websites were selected by screening webpage titles and screening devices on relevant webpages to determine whether it met the inclusion criteria. Data were extracted on standardized forms developed for this review.
Information on the devices was extracted from articles and cross-referenced with the device manufacturer’s information. Validity data on each device was not extracted; instead, articles with relevant validity data, where available [19-38], were referenced in the data table because the authors chose to focus this review on the characteristics of the devices to allow the reader to make a judgment about their efficacy as self-monitoring tools.
A 10% subsample of potentially relevant articles retrieved for full-paper screening were extracted by a second author (AL) to determine interrater agreement. Interrater agreement was high (Cohen’s kappa=.81). If any discrepancies arose, these were resolved by discussion between authors.
Self-Monitor Scoring
Each device was designated a self-monitoring code: (1) yes, self-monitors PA (YPA); (2) yes, self-monitors PA and physical inactivity, such as self-monitoring and feedback on lack of movement (YPI); and (3) yes, self-monitors sedentary time (YST).
The different attributes of the self-monitoring devices were based on Control Theory [11]; specifically, the ability to receive feedback (defined as the provision of informative and actionable insights on the performance of the behavior) and the ability to set goals (defined as agreeing on a goal/target defined in terms of the behavior to be achieved) [8]. Aspects included the different types of feedback (eg, vibratory, auditory, omnipresent in the form of colors or lights, or potentially via push notifications). Also included was the timing of the feedback (ie, immediate or delayed). Other features included the way in which the data were portrayed (eg, numeric data/graphical representation of the data). The platform pervasiveness was also included (ie, number of different devices/operating systems the data could be viewed on). Each of these was broken into the feedback attributes that were available on either the device or the backend platform (defined as the smart device/software that the technology connected to). Other attributes included were goal-setting capability of the device and whether the device or associated software could be customized by the end user via some method, usually an application programming interface or software development kit. Textbox 1 provides a detailed description of each self-monitoring attribute. Each attribute was split into whether the attribute was present on the device itself (denoted with “D”) or whether it was present on the backend platform (ie, mobile phone/tablet; denoted with “BP”).
Description of the self-monitoring attributes coded.
Auditory: feedback on behavior provided verbally from device (eg, via Sensoria voice-over feedback regarding ground contact from smartphone/smart MP3)
Vibratory: haptic feedback on predetermined behavioral thresholds provided using vibrations (eg, LumoBack)
Omnipresent: feedback that is visible all the time, usually in the form of a progression bar that changes with advancement toward predetermined goals (eg, Fitbit Flower)
Push notification: the delivery of information regarding behavioral goals from a software app to a computing device without a specific request from the user
Immediate: whether the data/feedback are immediate in its return to the user (eg, LumoBack)
Delayed: whether the data/feedback are delayed in its return to the user (eg, ActiGraph)
Numeric: data are returned in the form of numbers/figures or statistics
Graph: data are returned in the form of graphical representation
Written/textual feedback: data are returned in the form of textual feedback
‘Ometer (omnipresent meter): data are returned in the form of a growing or shrinking picture/image based on completion toward a predetermined goal (eg, UbiFit Garden)
Application: what operating system the mobile app can be accessed on for viewing the data/feedback
Software: the operating systems it can be accessed on if a piece of computing software is present for use at viewing the data
Website: can the data/feedback be viewed on a website?
Goal-setting capability: can predetermined goals be set by the user?
Customization: can the device or mobile app be customized by the end user (eg, via a software development kit)?
Each device was given a score between 1 and 6 for each attribute of behavior change. This score was used to describe two factors: (1) whether or not that device contained that behavior change attribute and (2) to what extent it did or did not contain the attribute. The self-monitoring scoring system that was used for each attribute was (1) yes; (2) yes, difficulties (eg, proximity to computer); (3) yes, lack of evidence to suggest this; (4) no, but present in future iterations; (5) no, but possible (with application programming interface or software development kit); and (6) not described/featured.
This scoring system was meant to be a descriptive tally of the behavior change attributes and not a judgment on the effectiveness of the various features.
Results
Review Statistics
Database searches identified 49,956 articles (Figure 1), of which 462 were deemed to be potentially relevant and were retrieved for full-text analysis. Articles were excluded for a number of reasons (n=337):
Figure 1.
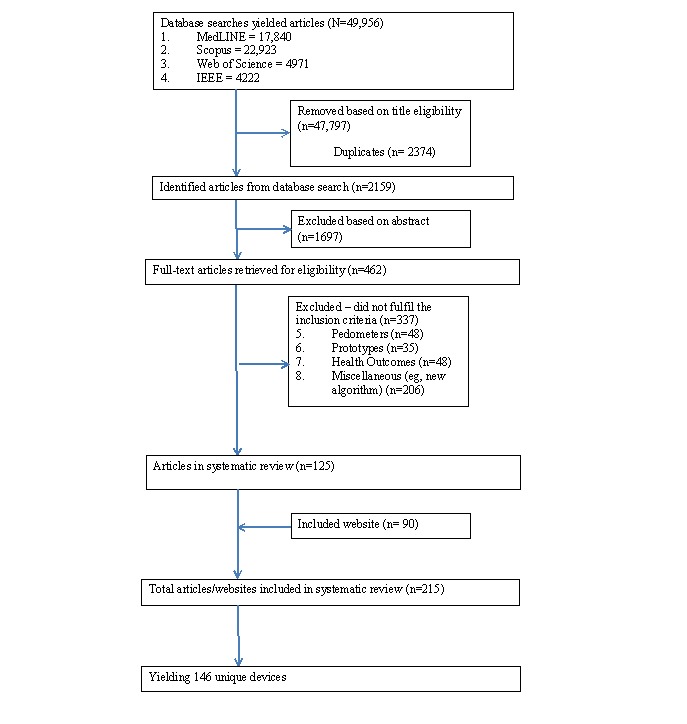
Study/website selection.
Pedometer studies: these were excluded if no evidence could be found that the pedometer in question provided temporally stamped data.
Prototypes: if the device was not commercially available or if no data currently existed for the prototype and only proof of concept information was available were excluded.
Health outcome: articles were excluded if they examined the relationship between behavior (eg, sedentary behavior and/or PA) and a particular health outcome (eg, blood pressure, lipid profile) and the measurement tool of choice was not the main focus of the article.
Miscellaneous: articles were excluded if the purpose of the study was to examine a new algorithm or data processing procedure for device analysis.
The remaining 125 studies (on 46 devices) and 90 websites yielded 146 devices (see Multimedia Appendix 2) that were selected for detailed scrutiny. Of these, 64 were further removed because there was no evidence that they were designed for, had been used in, or could readily be modified for real-time self-monitoring purposes or that they were not currently available for purchase.
The remaining 82 [39-119] technologies were included in this review. Of these, 73 [39-110] technologies measured / self-monitored PA, of which 16 [43,45,55,56,58,62-66,81,86,90,91,94,103,107-109] provided some measure of physical inactivity (see Multimedia Appendix 3). In all, 9 [111-119] technologies measured self-monitored sedentary time (Multimedia Appendix 4), 8 [111,112,114-119] of which measured both PA and sedentary time.
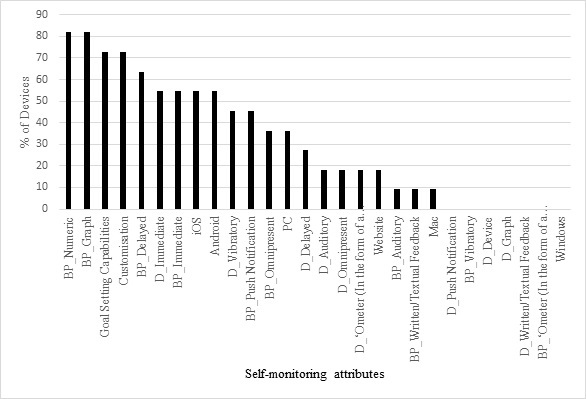
Physical Activity Self-Monitoring Technologies
Figure 2 displays the number of self-monitoring attributes apparent in each of the devices found to measure/self-monitor PA. The device with the highest number of feedback attributes was the Microsoft Band [77] with 18 of 28 feedback possibilities that were coded. The most common feedback attribute used in the devices found was joint numeric and graphical data feedback on the associated backend platform, with 94% of the devices that self-monitored PA displaying these attributes. The least common form of feedback attribute was auditory feedback from the device (D_Auditory). This particular type of feedback was only present in 2% of cases (Figure 3).
Figure 2.
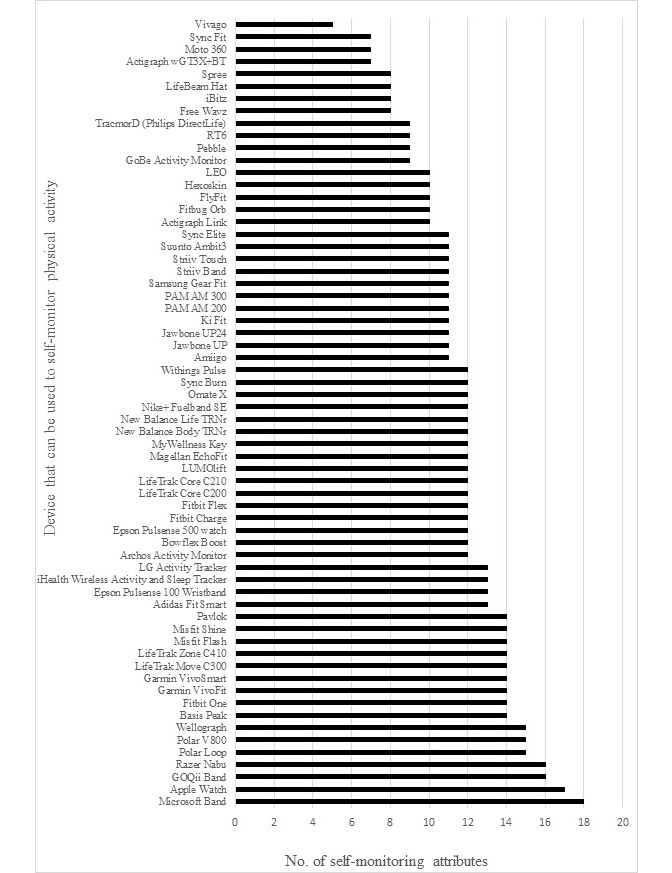
Technologies found that can be used to self-monitor and provide feedback on PA ordered by number of self-monitoring attributes that were found to be present in the technologies.
Figure 3.
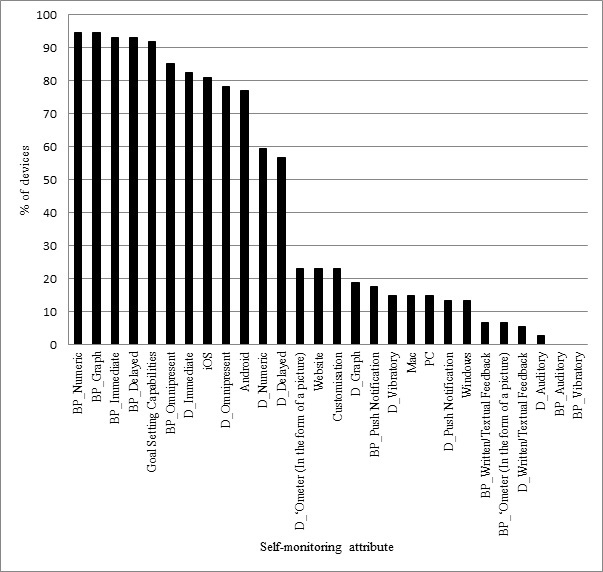
The proportion of devices that could be used to self-monitor and provided feedback on physical activity with specific self-monitoring attributes.
Sedentary Time Self-Monitoring Technologies
Figure 4 displays the number of self-monitoring attributes apparent in each of the devices found to measure/self-monitor sedentary time. Figure 5 documents the popularity of the self-monitoring attributes with sedentary time self-monitoring devices. The device with the highest number of feedback attributes was the Lumo Back posture sensor and feedback coach [17] with 13 of 28 feedback possibilities that were coded. The most common feedback attribute used in the devices found was joint numeric and graphical data feedback on the associated backend platform, with 81% of the devices that self-monitor sedentary time displaying these attributes. The least common form of feedback attribute was push notification of feedback from the device of sedentary time on the device. This particular type of feedback was not present in any of the devices found.
Figure 4.
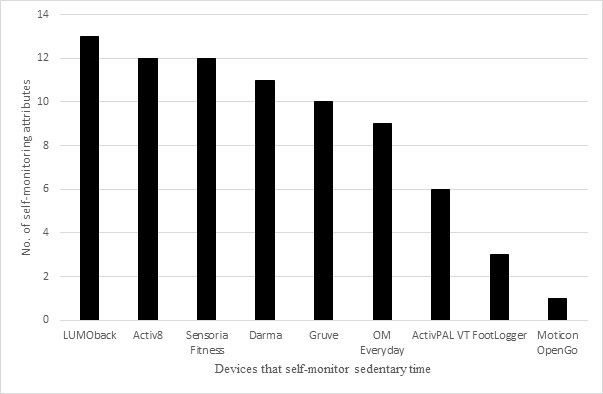
Technologies found that could be used to self-monitor and provided feedback on sedentary time ordered by number of feedback elements in the technologies.
Figure 5.
The proportion of devices that could be used to self-monitor and provided feedback on sedentary time with specific self-monitoring attributes.
Discussion
The present systematic review sought to identify current measurement technologies available that could be used for real-time self-monitoring of sedentary time and/or PA. The review identified 125 articles on 46 device and 90 websites, for a combined total of 146 technologies that monitor sedentary time and/or PA. Of these, 82 devices were considered capable of self-monitoring sedentary time and/or PA. These devices can be used by researchers, clinicians, and the general public.
Technologies that self-monitor PA mainly come from the consumer health and fitness market. In general, these devices consist of an accelerometer for activity measurement (steps, calories burned, distance traveled) with varying secondary sensors, including gyroscope, inclinometer, lux sensors, skin sweat sensors, and other sensors that provide additional pieces of information. However, these devices will provide feedback only on PA and increases in PA do not automatically lead to decreases in sedentary time [120]. Additionally, more and more of these devices are providing feedback on not only the amount of PA, but also the length of time spent inactive.
There are devices from both the commercial and research sectors that self-monitor sedentary behavior. These devices tend to measure sedentary time in two different ways. Firstly, posture sensors measure sedentary time either through an accelerometer in conjunction with gravitational components and proprietary algorithms (eg, activPAL) or through the alignment of the area of the body surrounding the pelvic area (ie, pelvic alignment is different depending on standing, sitting, and lying). The other way technologies tend to measure sedentary time is via pressure sensors. These pressure sensors are either located in a sock, shoe, or chair. When placed in a sock or shoe, the pressure can determine standing when there is pressure on the sensor and when there is less pressure the wearer is sitting or lying. Located on a chair, there is a simple binary outcome: when the pressure sensor is active the user is sitting and when it is inactive there is no sitting behavior at that site.
Both these types of devices usually provide feedback either via vibratory feedback (eg, Jawbone UP) or via an omnipresent display on the device (eg, Garmin Vivofit). These devices tend to, but not exclusively, connect to a mobile app for feedback on the PA and sedentary time. For PA, this usually takes the form of energy expenditure or proprietary company points (eg, Nike Fuel). For sedentary time, this usually takes the form of time spent sitting (eg, LumoBack) These mobile apps allow the wearer to receive real-time continuous feedback along with goal-setting capabilities and customization of type and timing of feedback; this is an aspect not traditionally offered by research devices.
With the plethora of devices now available (see Figure 6 for an example of popular devices), with differing attributes and cost, it is unsurprising that these devices are growing in popularity. However, and perhaps paradoxically, there are a small number of devices specifically designed to measure sitting time. Furthermore, the small number of devices that do provide feedback on sitting were not either originally designed for its measurement (eg, LumoBack) or are still primarily research tools to be used in scientific study (eg, ActivPAL VT).
Figure 6.
Example of devices discussed in this review. Clockwise from top left: Fitbit Charge HR, Garmin Vivofit, Jawbone Up, Nike Fuelband SE, Lumo Back Posture Sensor, and a mobile app.
Self-monitoring technologies need to provide real-time feedback on aspects of PA and sitting that are personalized and relevant to the individual (ie, the attributes of real-time feedback must resonate with the individual and not be simply information that has been presupposed for them). Additionally, the immediate feedback should be of a low cognitive load so that it can resonate immediately with the end user [121,122]. For example, the Fitbit one has a growing flower as a feedback indication of progression toward a user-defined goal. Using a pictorial representation of this nature will resonate easier with the user [123,124]. However, more detailed information on the temporal patterning of the behavior, for example, should be accessible from a mobile app, website, or software. Furthermore, the likelihood of the feedback being acted upon could be increased if it is provided in a manner that is context aware. In other words, the feedback must be given at a time when it can be acted upon by the user. For example, to reduce sitting, it should provide feedback while watching television rather than sitting in an exam or during a prolonged dental procedure. If these attributes could be integrated into a single device, it would help facilitate its use by differing populations regardless of technological ability. These devices need to have a substantial battery life and memory capacity at a reasonable cost. For this to occur, there is a need for cooperative work across different research disciplines and commercial fields to develop these context-aware, personalized feedback devices.
Not every user will have the same needs and the presentation of actionable information will need to be tailored to fit individual needs. In addition, simply providing more medical data to patients not only fails to guarantee improved outcomes, but also could potentially lead to negative consequences [125]. Activity trackers have poor evidence of prolonged use, with a conservatively estimated one-third discontinuing use by 6 months after initiation [126]. A recent study of several tools to encourage medication adherence in older adults, a major area of focus of mHealth developers, found that the most common descriptors participants used to describe their experience with the devices were “frustrating” and “challenging” [127]. In another study of the usage of a dietary app to promote healthy eating, investigators found that fewer than 3% used the app for at least 1 week and fewer than 10% of these individuals made positive changes in their diet [128]. Users require consumer-friendly devices and apps that are self-reinforcing and enjoyable to use. These goals might be accomplished with the use of incentives, gamification, and social networks to promote managed competition/cooperation among peers or family members.
In order for the promise of wearable technology to be fully realized, consumers, providers, and health care systems must be able to trust the reliability, privacy, and security of their data as well as the devices that collect and share it. Although regulatory oversight is often considered to be an impediment to the rapid propagation of innovative technologies, the existence of potential scams that could harm the end user dictates the need for some level of oversight. Globally, there is a great deal of uncertainty around wearable technology regulation; there are numerous countries that have no regulatory framework, whereas the other countries that do have a framework are still in their infancy and being actively refined [129,130].
Wearable technology users are also concerned about the privacy and ownership of their health data. In the era of big data, it is critical that the terms of ownership of personal data, most especially medical data, be unmistakably stated—not buried in the commonly unread and then accepted terms of use agreements—with users required to explicitly consent whenever their data are sold or transmitted to others [131].
One of the benefits of mHealth is easier accessibility to pertinent health care data, but this increased availability to both consumers and providers creates the potential for substantial security risks. Because of the small size of the device, it becomes easier to inadvertently lose or easier to steal, which may mean that the information stored on the device becomes accessible to others.
As consumer demand for wearable sensor increases, health care providers will face the possibility of being inundated by a flood of patient data. This will create a number of difficult challenges, including the potential requirement for 24/7 oversight, the need to summarize multiparameter, continuously collected data into a usable and clinically meaningful format [132].
The strengths of this review are the systematic approach taken and the comprehensive range of technologies found. However, there are some limitations. Due to the nature of articles included, it was not possible to present data on the validity and reliability of the devices in their ability to measure sedentary time. Similarly, due to the fact that self-monitoring using objective measurement tools is in its infancy, there are gaps in the literature as to whether these devices truly work as self-monitors; consequently, we cannot comment on how useful or valid they are in these settings. However, validity data are important. Users of self-monitoring technologies must be able to trust in the feedback that is being returned to them otherwise they may become disenfranchised with the tool and the behavior change tool. Therefore, incorporating important valid data with the feedback tools means additional value can be added to the consumers and potentially more potent behavior change.
In conclusion, the authors believe that this review is the first of its kind to systematically describe the wide breadth of devices that self-monitor and provide feedback on PA and sedentary behavior. There has been an explosion in the number of devices that measure PA and there is a greater need for the development of tools that specifically measure sitting time. Cooperative work between engineers, computer scientists, and academics in relevant fields is needed to develop these technologies that provide real-time, personalized, context-aware feedback to aid in the reduction in sitting time and its detrimental effect on cardiometabolic health independent of PA. This could potentially lead to the use of these devices in a health care setting as part of the increasing value-based care systems that are starting to arise in the United States or as a diagnostic tool, which is beginning to be implemented in the National Health Service in the United Kingdom.
This scoping review provides a record of a plethora of devices with information on their capabilities both in terms of their ability to measure behavior and to provide feedback to the user, providing a foundation for clinical, research, and public health use. Future studies are needed to further investigate the validity of these devices and their feasibility in increasing PA and/or decreasing sedentary time and the public health impact this may produce.
Acknowledgments
TY and CLE acknowledge support from the National Institute for Health Research Collaboration for Leadership in Applied Health Research and Care-East Midlands (NIHR CLAHRC-EM) and the Leicester Clinical Trials Unit, as well as the NIHR Leicester-Loughborough Diet, Lifestyle and Physical Activity Biomedical Research Unit, which is a partnership between University Hospitals of Leicester NHS Trust, Loughborough University, and the University of Leicester. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health.
This work was supported in part by a Medical Research Council grant in LLHW Promoting Physical Activity in Older Age 2012 (MRC Reference: MR/K025090/1). This work was additionally supported by an EPSRC Small Equipment Grant titled: Upgrading the Small Equipment base for Early Career Researchers in the Engineering and Physical Sciences (EP/K03118X/1).
Abbreviations
- PA
physical activity
- MVPA
moderate-to-vigorous physical activity
Search Strategy.
Supplementary Table 1 - All Devices.
Supplementary Table 2 - Devices that self monitor physical activity.
Supplementary Table 3 - Devices that Self-monitor Sedentary behaviour.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Katzmarzyk PT, Mason C. The physical activity transition. J Phys Act Health. 2009 May;6(3):269–280. doi: 10.1123/jpah.6.3.269. [DOI] [PubMed] [Google Scholar]
- 2.Sedentary Behaviour Research Network Letter to the editor: standardized use of the terms "sedentary" and "sedentary behaviours". Appl Physiol Nutr Metab. 2012 Jun;37(3):540–542. doi: 10.1139/h2012-024. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization . Global Recommendations on Physical Activity for Health. Geneva: World Health Organization; 2010. [PubMed] [Google Scholar]
- 4.Ogilvie D, Foster CE, Rothnie H, Cavill N, Hamilton V, Fitzsimons CF, Mutrie N, Scottish Physical Activity Research Collaboration Interventions to promote walking: systematic review. BMJ. 2007 Jun 9;334(7605):1204. doi: 10.1136/bmj.39198.722720.BE. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=17540909 .bmj.39198.722720.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Morris JN, Hardman AE. Walking to health. Sports Med. 1997 May;23(5):306–332. doi: 10.2165/00007256-199723050-00004. [DOI] [PubMed] [Google Scholar]
- 6.Wilmot EG, Edwardson CL, Achana FA, Davies MJ, Gorely T, Gray LJ, Khunti K, Yates T, Biddle SJ. Sedentary time in adults and the association with diabetes, cardiovascular disease and death: systematic review and meta-analysis. Diabetologia. 2012 Nov;55(11):2895–2905. doi: 10.1007/s00125-012-2677-z. [DOI] [PubMed] [Google Scholar]
- 7.Healy GN, Dunstan DW, Salmon J, Cerin E, Shaw JE, Zimmet PZ, Owen N. Breaks in sedentary time: beneficial associations with metabolic risk. Diabetes Care. 2008 Apr;31(4):661–666. doi: 10.2337/dc07-2046.dc07-2046 [DOI] [PubMed] [Google Scholar]
- 8.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, Eccles MP, Cane J, Wood CE. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013 Aug;46(1):81–95. doi: 10.1007/s12160-013-9486-6. [DOI] [PubMed] [Google Scholar]
- 9.Kanfer F, Gaelick-Buys L. Help People Change: A Textbook of Methods. 4th ed. Elmsford, NY: Pergamon Press; 1991. Self-management methods; pp. 309–355. [Google Scholar]
- 10.Fogg B. Persuasive Technology: Using Computers to Change What We Think and Do. San Francisco, CA: Morgan Kaufmann; 2003. [Google Scholar]
- 11.Carver CS, Scheier MF. Control theory: a useful conceptual framework for personality-social, clinical, and health psychology. Psychol Bull. 1982 Jul;92(1):111–135. [PubMed] [Google Scholar]
- 12.Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009 Nov;28(6):690–701. doi: 10.1037/a0016136.2009-20990-006 [DOI] [PubMed] [Google Scholar]
- 13.Schachter SC. Quality of life for patients with epilepsy is determined by more than seizure control: the role of psychosocial factors. Expert Rev Neurother. 2006 Jan;6(1):111–118. doi: 10.1586/14737175.6.1.111. [DOI] [PubMed] [Google Scholar]
- 14.Burke LE, Wang J, Sevick MA. Self-monitoring in weight loss: a systematic review of the literature. J Am Diet Assoc. 2011 Jan;111(1):92–102. doi: 10.1016/j.jada.2010.10.008. http://europepmc.org/abstract/MED/21185970 .S0002-8223(10)01644-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bravata DM, Smith-Spangler C, Sundaram V, Gienger AL, Lin N, Lewis R, Stave CD, Olkin I, Sirard JR. Using pedometers to increase physical activity and improve health: a systematic review. JAMA. 2007 Nov 21;298(19):2296–2304. doi: 10.1001/jama.298.19.2296.298/19/2296 [DOI] [PubMed] [Google Scholar]
- 16.Turner-McGrievy GM, Beets MW, Moore JB, Kaczynski AT, Barr-Anderson DJ, Tate DF. Comparison of traditional versus mobile app self-monitoring of physical activity and dietary intake among overweight adults participating in an mHealth weight loss program. J Am Med Inform Assoc. 2013 May 1;20(3):513–518. doi: 10.1136/amiajnl-2012-001510. http://jamia.oxfordjournals.org/cgi/pmidlookup?view=long&pmid=23429637 .amiajnl-2012-001510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Information Board Personalised Health and Care 2020: Using Data and Technlogy to Transform Outcomes for Patients and Citizens - A Framework for Action. 2014. [2016-04-04]. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/384650/NIB_Report.pdf .
- 18.National Information Board GOV.UK. 2015. [2016-04-04]. Delivering the five year forward view: personalised health and care 2020 https://www.gov.uk/government/publications/implementing-personalised-health-and-care-2020/delivering-the-five-year-forward-view .
- 19.Dannecker K, Petro S, Melanson EL, Browning RC. Accuracy of Fitbit activity monitor to predict energy expenditure with and without classification of activities. Med Sci Sport Exer. 2011;43(Suppl 1):62. doi: 10.1249/01.MSS.0000402857.55729.ab. [DOI] [Google Scholar]
- 20.Dannecker KL, Sazonova NA, Melanson EL, Sazonov ES, Browning RC. A comparison of energy expenditure estimation of several physical activity monitors. Med Sci Sports Exerc. 2013 Nov;45(11):2105–2112. doi: 10.1249/MSS.0b013e318299d2eb. http://europepmc.org/abstract/MED/23669877 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bonomi AG, Plasqui G, Goris AH, Westerterp KR. Estimation of free-living energy expenditure using a novel activity monitor designed to minimize obtrusiveness. Obesity (Silver Spring) 2010 Sep;18(9):1845–1851. doi: 10.1038/oby.2010.34.oby201034 [DOI] [PubMed] [Google Scholar]
- 22.Plasqui G, Bonomi AG, Westerterp KR. Daily physical activity assessment with accelerometers: new insights and validation studies. Obes Rev. 2013 Jun;14(6):451–462. doi: 10.1111/obr.12021. [DOI] [PubMed] [Google Scholar]
- 23.Bergamin M, Ermolao A, Sieverdes JC, Zaccaria M, Zanuso S. Validation of the mywellness key in walking and running speeds. J Sports Sci Med. 2012;11(1):57–63. http://europepmc.org/abstract/MED/24149122 . [PMC free article] [PubMed] [Google Scholar]
- 24.Sieverdes JC, Wickel EE, Hand GA, Bergamin M, Moran RR, Blair SN. Reliability and validity of the Mywellness Key physical activity monitor. Clin Epidemiol. 2013;5:13–20. doi: 10.2147/CLEP.S38370. doi: 10.2147/CLEP.S38370.clep-5-013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Herrmann SD, Hart TL, Lee CD, Ainsworth BE. Evaluation of the MyWellness Key accelerometer. Br J Sports Med. 2011 Feb;45(2):109–113. doi: 10.1136/bjsm.2009.062182.bjsm.2009.062182 [DOI] [PubMed] [Google Scholar]
- 26.Ryan CG, Grant PM, Tigbe WW, Granat MH. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med. 2006 Sep;40(9):779–784. doi: 10.1136/bjsm.2006.027276. http://europepmc.org/abstract/MED/16825270 .bjsm.2006.027276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grant PM, Ryan CG, Tigbe WW, Granat MH. The validation of a novel activity monitor in the measurement of posture and motion during everyday activities. Br J Sports Med. 2006 Dec;40(12):992–997. doi: 10.1136/bjsm.2006.030262. http://europepmc.org/abstract/MED/16980531 .bjsm.2006.030262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kozey-Keadle S, Libertine A, Lyden K, Staudenmayer J, Freedson PS. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011 Aug;43(8):1561–1567. doi: 10.1249/MSS.0b013e31820ce174. [DOI] [PubMed] [Google Scholar]
- 29.Chastin SF, Granat MH. Methods for objective measure, quantification and analysis of sedentary behaviour and inactivity. Gait Posture. 2010 Jan;31(1):82–86. doi: 10.1016/j.gaitpost.2009.09.002.S0966-6362(09)00602-X [DOI] [PubMed] [Google Scholar]
- 30.Vanhelst J, Hurdiel R, Mikulovic J, Bui-Xuân G, Fardy P, Theunynck D, Béghin L. Validation of the Vivago wrist-worn accelerometer in the assessment of physical activity. BMC Public Health. 2012;12:690. doi: 10.1186/1471-2458-12-690. http://www.biomedcentral.com/1471-2458/12/690 .1471-2458-12-690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Takacs J, Pollock CL, Guenther JR, Bahar M, Napier C, Hunt MA. Validation of the Fitbit One activity monitor device during treadmill walking. J Sci Med Sport. 2014 Sep;17(5):496–500. doi: 10.1016/j.jsams.2013.10.241.S1440-2440(13)00472-6 [DOI] [PubMed] [Google Scholar]
- 32.Lee J, Kim Y, Welk GJ. Validity of consumer-based physical activity monitors. Med Sci Sports Exerc. 2014 Sep;46(9):1840–1848. doi: 10.1249/MSS.0000000000000287. [DOI] [PubMed] [Google Scholar]
- 33.Harrington DM, Welk GJ, Donnelly AE. Validation of MET estimates and step measurement using the ActivPAL physical activity logger. J Sports Sci. 2011 Mar;29(6):627–633. doi: 10.1080/02640414.2010.549499.934038486 [DOI] [PubMed] [Google Scholar]
- 34.Rosenberger ME, Buman MP, Haskell WL, Mcconnell MV, Carstensen LL. Twenty-four hours of sleep, sedentary behavior, and physical activity with nine wearable devices. Med Sci Sport Exer. 2016;48(3):457–465. doi: 10.1249/MSS.0000000000000778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ferguson T, Rowlands AV, Olds T, Maher C. The validity of consumer-level, activity monitors in healthy adults worn in free-living conditions: a cross-sectional study. Int J Behav Nutr Phys Act. 2015;12:42. doi: 10.1186/s12966-015-0201-9. http://www.ijbnpa.org/content/12//42 .10.1186/s12966-015-0201-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tucker WJ, Bhammar DM, Sawyer BJ, Buman MP, Gaesser GA. Validity and reliability of Nike + Fuelband for estimating physical activity energy expenditure. BMC Sports Sci Med Rehabil. 2015;7:14. doi: 10.1186/s13102-015-0008-7. http://bmcsportsscimedrehabil.biomedcentral.com/articles/10.1186/s13102-015-0008-7 .8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kooiman TJ, Dontje ML, Sprenger SR, Krijnen WP, van der Schans CP, de Groot M. Reliability and validity of ten consumer activity trackers. BMC Sports Sci Med Rehabil. 2015;7:24. doi: 10.1186/s13102-015-0018-5. http://europepmc.org/abstract/MED/26464801 .18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bai Y, Welk GJ, Nam YH, Lee JA, Lee J, Kim Y, Meier NF, Dixon PM. Comparison of consumer and research monitors under semistructured settings. Med Sci Sports Exerc. 2015 Jul 6;:151–158. doi: 10.1249/MSS.0000000000000727. [DOI] [PubMed] [Google Scholar]
- 39.ActiGraph LLC. 2015. [2015-10-26]. ActiGraph Link http://www.actigraphcorp.com/
- 40.ActiGraph LLC. 2013. [2015-10-26]. ActiGraph wGT3X-BT Monitor http://www.actigraphcorp.com/
- 41.Adidas International Trading BV. 2014. [2015-10-27]. Adidas MiCoach - Fit Smart http://micoach.adidas.com/fitsmart/
- 42.Amiigo. 2014. [2015-10-27]. Amiigo Wristband https://amiigo.com/
- 43.Apple Inc. 2014. [2015-10-27]. Apple Watch http://www.apple.com/watch/
- 44.ARCHOS. 2014. [2015-10-27]. ARCHOS Activity Tracker http://www.archos.com/gb/products/objects/cself/aat/index.html .
- 45.BASIS Science Inc. 2014. [2015-10-27]. Basis Peak http://www.mybasis.com/
- 46.Nautilus Inc. 2013. [2015-10-27]. Bowflex Boost http://www.bowflexboost.com/bowflex-boost-us/homepage.jsp .
- 47.Epson America Inc. 2014. [2015-10-27]. Epson Pulsense - Fitness Watch & Band http://www.epson.com/cgi-bin/Store/jsp/Landing/pulsense-fitness-sensing-watches.do?ref=van_pulsense .
- 48.Fitbit Inc. 2014. [2015-10-27]. Fitbit Charge https://www.fitbit.com/uk .
- 49.Fitbit Inc. 2014. [2015-10-27]. Fitbit Flex https://www.fitbit.com/uk .
- 50.Fitbit Inc. 2012. [2015-10-27]. Fitbit One https://www.fitbit.com/uk .
- 51.Fitbit Inc. 2014. [2015-10-28]. Fitbit Surge http://www.fitbit.com/uk/home .
- 52.Fitbug Ltd. 2014. [2015-10-27]. Fitbug Orb https://www.fitbug.com/g/orb?lng=en_UK .
- 53.FlyFit. 2014. [2015-10-27]. FlyFit http://www.myflyfit.com/
- 54.Free Wavz. 2014. [2015-10-27]. Free Wavz -wire free smart earphones http://www.freewavz.com/
- 55.Garmin Ltd. 2014. [2015-10-27]. Garmin VivoFit https://buy.garmin.com/en-GB/GB/watches-wearable-technology/wearables/vivofit-/prod143405.html .
- 56.Garmin Ltd. 2014. [2015-10-27]. Garmin VivoSmart https://buy.garmin.com/en-GB/GB/watches-wearable-technology/wearables/vivosmart-/prod154886.html .
- 57.HealBe Corporation. 2014. [2015-10-27]. HealBe GoBe Activity Monitor http://healbe.com/us/
- 58.GOQii Inc. 2014. [2015-10-27]. GOQii Life http://goqii.com/
- 59.Hexoskin. 2013. [2015-10-27]. Hexoskin - wearable body metrics http://www.hexoskin.com/
- 60.GeoPalz LLC. 2014. [2015-10-27]. iBitz http://ibitz.com/
- 61.iHealth Lab Inc. 2014. [2015-10-27]. iHealth Wireless Activity and Sleep Tracker http://www.ihealthlabs.com/fitness-devices/wireless-activity-and-sleep-tracker/
- 62.Jawbone. 2014. [2015-10-27]. Jawbone UP https://jawbone.com/
- 63.Jawbone. 2014. [2015-10-28]. Jawbone UP2 https://jawbone.com/
- 64.Jawbone. 2014. [2015-10-27]. Jawbone UP24 https://jawbone.com/
- 65.Jawbone. 2014. [2015-10-28]. Jawbone UP3 https://jawbone.com/
- 66.Jawbone. 2015. [2015-10-28]. Jawbone UP4 https://jawbone.com/
- 67.Ki Performance. 2014. [2015-10-27]. Ki Fit http://www.kiperformance.co.uk/
- 68.Gesture Logic. 2014. [2016-04-04]. LEO http://leohelps.com/
- 69.LG Electronics. 2014. [2015-10-27]. LG Lifeband Touch Activity Tracker http://www.lg.com/us/mobile-accessories/lg-FB84-BL-activity-tracker .
- 70.LifeBeam Technologies Ltd. 2014. [2015-10-27]. LifeBeam Hat http://life-beam.com/shop/smart-hat/
- 71.Salutron Inc. 2014. [2015-10-27]. LifeTrak Move C200 http://lifetrakusa.com/product/core-c200/
- 72.Salutron Inc. 2014. [2015-10-27]. LifeTrak Core C210 https://lifetrakusa.com/product/move-c300/
- 73.Salutron Inc. 2014. [2015-10-27]. LifeTrak Move C300 https://lifetrakusa.com/product/move-c300/
- 74.Salutron Inc. 2014. [2015-10-27]. LifeTrak Zone C410 http://lifetrakusa.com/product/zone-c410/
- 75.LumoBodyTech Inc. 2014. [2015-10-27]. LumoLift http://www.lumobodytech.com/
- 76.MiTAC International Corporation. 2014. [2015-10-27]. Magellan EchoFit Series http://www.magellangps.com/lp/echofit/index.html .
- 77.Microsoft. 2014. [2015-10-27]. Microsoft Band http://www.microsoft.com/microsoft-band/en-gb .
- 78.Misfit Wearables. 2014. [2015-10-27]. Misfit Flash Fitness + Sleep Monitor http://misfit.com/
- 79.Misfit Wearables. 2014. [2015-10-27]. Misfit Shine Fitness + Sleep Tracker http://misfit.com/
- 80.Motorola Mobility. 2014. [2015-10-27]. Moto 360 http://www.motorola.co.uk/Moto-360/moto-360-gb.html .
- 81.Technogym. 2011. [2015-10-27]. MyWellness Key http://www.technogym.com/gb/products.html .
- 82.New Balance. 2014. [2015-10-27]. New Balance Life TRNr http://www.nike.com/gb/en_gb/c/nikeplus-fuel .
- 83.New Balance. 2014. [2015-10-27]. New Balance Body TRNr http://www.newbalance.com/pd/body-trnr/52569.html .
- 84.Nike Inc. 2013. [2016-04-04]. Nike+ Fuelband SE http://www.nike.com/gb/en_gb/c/nikeplus-fuelband .
- 85.Omate. 2014. [2015-10-27]. Omate X http://www.omate.com/index.html .
- 86.PAM bv. 2008. [2015-10-27]. PAM AM200 http://www.pam.com/index.php?pid=1 .
- 87.PAM bv. 2009. [2015-10-27]. PAM AM300 http://www.pam.com/index.php?pid=1 .
- 88.Behavioral Technology Group. 2014. [2015-10-27]. Pavlok http://pavlok.com/
- 89.Pebble. 2012. [2016-04-04]. Pebble Smart Watch https://getpebble.com/
- 90.Polar Electro. 2014. [2015-10-28]. Polar Loop http://www.polar.com/en/products/fitness_crosstraining/loop2 .
- 91.Polar Electro. 2014. [2015-04-01]. Polar V800 Sports Watch http://www.polar.com/en/products/maximize_performance/running_multisport/V800 .
- 92.Razer Inc. 2014. [2016-04-04]. Razer Nabu http://www.razerzone.com/gb-en/nabu .
- 93.Razer Inc. 2015. [2016-04-04]. Razr Nabu X http://www.razerzone.com/nabu-x .
- 94.Stayhealthy Research. 2013. [2015-10-27]. RT6 http://www.rt6tracker.com/
- 95.SAMSUNG. 2014. [2015-10-27]. SAMSUNG Gear Fit http://www.samsung.com/us/mobile/wearable-tech/SM-R3500ZKAXAR .
- 96.Spree Wearables. 2014. [2015-10-27]. Spree http://spreewearables.com/
- 97.Stayhealthy Research. 2014. [2015-10-28]. SAM http://www.rt6tracker.com/
- 98.Striiv Inc. 2014. [2016-04-04]. Striiv Band http://www.striiv.com/striivband/
- 99.Striiv Inc. 2015. [2015-10-28]. Striiv Fusion https://jawbone.com/
- 100.Striiv Inc. 2015. [2015-10-28]. Striiv Fusion Bio https://jawbone.com/
- 101.Striiv Inc. 2015. [2015-10-28]. Striiv Fusion Lite https://jawbone.com/
- 102.Striiv Inc. 2014. [2016-04-04]. Striiv Touch http://www.striiv.com/striivtouch/
- 103.Amer Sports Brand. 2014. [2015-10-27]. Suunto Ambit3 http://www.suunto.com/en-GB/Products/sports-watches/Suunto-Ambit3-Sport/Suunto-Ambit3-Sport-Blue/
- 104.SYNC. 2014. [2015-10-27]. SYNC Burn http://syncactive.com/products/activity-trackers/
- 105.SYNC. 2014. [2015-10-27]. SYNC Elite http://syncactive.com/products/fitness/
- 106.SYNC. 2014. [2015-10-27]. SYNC Fit http://syncactive.com/products/fitness/
- 107.Philips. 2009. [2015-04-01]. Direct Life http://www.directlife.philips.com/
- 108.Vivago SAS. 2012. [2015-10-27]. Vivago http://www.vivagowellness.fr/
- 109.Wellograph Company Ltd. 2013. [2015-10-27]. Wellograph https://wellograph.com/
- 110.Withings. 2012. [2015-04-01]. Withings Pulse http://www.withings.com/uk/en/store/details/pulse-O2 .
- 111.VitaMove. 2013. [2015-10-27]. Activ8 http://www.vitamove.nl/products/activ8/
- 112.PAL technologies. 2014. [2015-10-27]. ActivPAL VT http://www.paltechnologies.com/products/
- 113.Darma Inc. 2014. [2015-10-27]. Darma http://darma.co/
- 114.3L Labs. 2014. [2015-10-27]. Footlogger http://www.footlogger.com/
- 115.Gruve Technologies. 2012. [2015-10-27]. Gruve http://www.gruvetechnologies.com/
- 116.LumoBodyTech Inc. 2012. [2015-10-27]. Lumo Back http://www.lumobodytech.com/lumo-back/
- 117.Moticon. 2013. [2015-10-27]. Moticon OpenGo http://www.moticon.de/products/science-research .
- 118.OM Everyday. 2013. [2015-10-27]. OM Signal http://www.omsignal.com/
- 119.Heapsylon. 2013. [2015-10-27]. Sensoria Fitness Socks http://www.sensoriafitness.com/
- 120.Prince SA, Saunders TJ, Gresty K, Reid RD. A comparison of the effectiveness of physical activity and sedentary behaviour interventions in reducing sedentary time in adults: a systematic review and meta-analysis of controlled trials. Obes Rev. 2014 Nov;15(11):905–919. doi: 10.1111/obr.12215. doi: 10.1111/obr.12215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Glendon A, Cernecca L. Young drivers’ responses to anti-speeding and anti-drink-driving messages. Transp Res Part F Traffic Psychol Behav. 2003 Sep 24;6(3):197–216. doi: 10.1016/S1369-8478(03)00026-3. [DOI] [Google Scholar]
- 122.Glendon AI, Walker BL. Can anti-speeding messages based on protection motivation theory influence reported speeding intentions? Accid Anal Prev. 2013 Aug;57:67–79. doi: 10.1016/j.aap.2013.04.004.S0001-4575(13)00139-5 [DOI] [PubMed] [Google Scholar]
- 123.Sweller J. Cognitive load during problem solving: effects on learning. Cogn Sci. 1988;12(2):257–285. doi: 10.1207/s15516709cog1202_4. [DOI] [Google Scholar]
- 124.Varshney U. A model for improving quality of decisions in mobile health. Decis Support Syst. 2014 Jun;62:66–77. doi: 10.1016/j.dss.2014.03.005. [DOI] [Google Scholar]
- 125.O'Kane MJ, Bunting B, Copeland M, Coates VE. Efficacy of self monitoring of blood glucose in patients with newly diagnosed type 2 diabetes (ESMON study): randomised controlled trial. BMJ. 2008 May 24;336(7654):1174–1177. doi: 10.1136/bmj.39534.571644.BE. http://www.bmj.com/cgi/pmidlookup?view=long&pmid=18420662 .bmj.39534.571644.BE [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Ledger D, McCaffrey D. Inside Wearables: How the Science of Human Behavior Change Offers the Secret to Long-Term Engagement Internet. Cambridge, MA: Endeavour Partners; 2014. [2015-12-20]. http://endeavourpartners.net/assets/Endeavour-Partners-Wearables-White-Paper-20141.pdf . [Google Scholar]
- 127.Grindrod KA, Li M, Gates A. Evaluating user perceptions of mobile medication management applications with older adults: a usability study. JMIR Mhealth Uhealth. 2014;2(1):e11. doi: 10.2196/mhealth.3048. http://mhealth.jmir.org/2014/1/e11/ v2i1e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Helander E, Kaipainen K, Korhonen I, Wansink B. Factors related to sustained use of a free mobile app for dietary self-monitoring with photography and peer feedback: retrospective cohort study. J Med Internet Res. 2014;16(4):e109. doi: 10.2196/jmir.3084. http://www.jmir.org/2014/4/e109/ v16i4e109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.GOV.UK Medicine & Healthcare products Regulatory Agency. 2014. Aug 08, [2015-12-20]. Medical device stand-alone software including apps https://www.gov.uk/government/publications/medical-devices-software-applications-apps/medical-device-stand-alone-software-including-apps .
- 130.US Food and Drug Administration. 2014. Mobile medical applications http://www.fda.gov/medicaldevices/digitalhealth/mobilemedicalapplications/default.htm#f .
- 131.Steinhubl SR, Muse ED, Topol EJ. The emerging field of mobile health. Sci Transl Med. 2015 Apr 15;7(283):283rv3. doi: 10.1126/scitranslmed.aaa3487. http://europepmc.org/abstract/MED/25877894 .7/283/283rv3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Yang YT, Silverman RD. Mobile health applications: the patchwork of legal and liability issues suggests strategies to improve oversight. Health Aff (Millwood) 2014 Feb;33(2):222–227. doi: 10.1377/hlthaff.2013.0958.33/2/222 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search Strategy.
Supplementary Table 1 - All Devices.
Supplementary Table 2 - Devices that self monitor physical activity.
Supplementary Table 3 - Devices that Self-monitor Sedentary behaviour.



