Abstract
The objectives of osteoarthritis (OA) management are to reduce pain and inflammation, slow cartilage degradation, improve function and reduce disability. Current strategies for managing knee OA include nonpharmacological interventions, oral pharmacological treatments, localized intra-articular injections, and surgery. It has become evident that the inflammatory response is a key contributor to the development and progression of knee OA. Signaling pathways involving growth factors and cytokines are being investigated for the development of new therapies that target the underlying biological processes causing the disease. This concept of ‘molecular orthopedics’ enables more patient-centered diagnostic and treatment strategies. In contrast to other conservative therapies, which ultimately only address OA symptoms, intra-articular injections, in particular autologous conditioned serum (ACS), provide benefits that have the potential to outweigh those of established pharmacological treatments and surgery. Surgery has historically been considered the final solution for treatment of knee OA, both by treating physicians and by patients; however, there are increasing concerns regarding the lack of randomized clinical trials providing evidence to support this opinion. Intra-articular injection of ACS has demonstrated efficacy as a treatment for knee OA in a number of studies, with a very low rate of adverse events and side effects, compared with surgery. Treatment with ACS utilizes the release of anti-inflammatory cytokines and regenerative growth factors to support the natural healing processes in the knee, and has the potential to provide a valuable alternative to surgical intervention.
Keywords: autologous conditioned serum, intra-articular injections, knee, orthopedic surgery, osteoarthritis, pain management
Introduction
Osteoarthritis (OA) is the most prevailing form of joint disease, with symptoms affecting 10–15% of adults over the age of 60 worldwide [WHO, 2013]. Estimates are that 10% of men and 18% of women aged over 60 years have symptomatic OA, with 80% experiencing movement limitations, and 25% being unable to carry out normal daily activities [WHO, 2015]. The prevalence of OA is rising due to increasing life expectancy and certain risk factors, such as obesity [Hunter and Felson, 2006; WHO, 2013].
OA is characterized by articular cartilage damage, low-grade synovial inflammation and hypertrophic bone changes, leading to functional deterioration [Hunter and Felson, 2006; WHO, 2013]. The main OA symptom is pain, which is also the leading factor for patients making lifestyle changes and seeking medical intervention [Hrnack and Barber, 2014]. The combination of pain and impaired functionality places a substantial burden on individuals, communities, healthcare resources and social care systems [WHO, 2013].
The knee joint is the most frequently affected of all joints, and knee OA is one of the leading causes of global disability [Cross et al. 2014]. Radiographic evidence of knee OA is present in approximately 30% of men and women over the age of 65 [WHO, 2013], and in 2010, the global age-standardized prevalence of knee OA was 3.8% [Cross et al. 2014].
The objectives of OA management, according to the OA Research Society International (OARSI), are to reduce pain and inflammation, slow cartilage degradation, improve function and reduce disability [Hunter and Felson, 2006; WHO, 2013; Fibel et al. 2015]. Current strategies for managing knee OA include nonpharmacological and pharmacological therapy (including intra-articular treatments), stem cell therapy and surgery [Evans et al. 2014; Fibel et al. 2015]. However, there are an increasing number of concerns regarding the disconnect between trial evidence and orthopedic surgical practice [Lim et al. 2014], as well as the lack of studies evaluating conservative treatments and a perceived bias towards pharmaceutical interventions [Hunter and Felson, 2006; Aspenberg, 2014; Lohmander and Roos, 2015]. It has also been suggested that a publication bias exists against reports that question established surgical procedures [Miller and Kallmes, 2010; Prasad et al. 2012].
The aim of this review is to summarize ongoing discussions on the insufficient evidence supporting the high use of surgery for knee OA, and to consider the evidence base for surgery in this indication more fully. Conservative therapies will be reviewed to determine their place in the management of knee OA. As local delivery of therapeutics into the knee joint by intra-articular injection can provide treatment benefits, such as increased bioavailability, reduced systemic exposure, fewer adverse events and lower costs [Evans et al. 2014], we will focus particularly on this treatment strategy.
Hierarchy of treatment options for knee OA
The aims of knee OA management are to control and reduce pain and improve functionality; therefore, treatment strategies need to be evaluated and adjusted regularly on a patient-by-patient basis [Hunter and Felson, 2006; McAlindon et al. 2014]. The current hierarchy for knee OA treatment consists of nonpharmacological, pharmacological, intra-articular injections (including stem cell therapy) and surgery [Hunter and Felson, 2006; Crawford et al. 2013; WHO, 2013], depending on OA severity and individual patient needs [Menkes, 1991; McAlindon et al. 2014]. A recent update of Osteoarthritis Research Society International (OARSI) treatment guidelines recommends consideration of relevant comorbidities in order to optimize OA treatment strategies [McAlindon et al. 2014]. Since an extensive review of all treatment strategies in detail is outside the scope of this publication, we will focus on conservative therapies (i.e. nonsurgical OA treatments), in particular intra-articular injections, in comparison to surgery. An overview of knee OA treatment options is presented in Table 1.
Table 1.
Overview of treatment strategies for knee OA.
| Treatment options | Description | References |
|---|---|---|
| Nonpharmacological | ||
| Education, self-management, social support | Patients participate in self-management programs, such as those conducted by the Arthritis Foundation (USA) and Arthritis Care (UK), which provide resources for social support and instruction on coping skills | [Zhang et al. 2010; Du et al. 2011; De Rezende et al. 2013] |
| Joint-unloading therapies | ||
| Physiotherapy, exercise, weight loss | Physiotherapy (motion exercise, muscle strengthening/stretching, soft tissue mobilization) can facilitate improvement of symptoms and improve functional disability Exercise increases aerobic capacity, muscle strength, and endurance and facilitates weight loss, which in turn can promote reductions in pain and improvements in function Weight loss can reduce the risk of development of symptomatic knee OA and improve disability |
[Messier et al. 2004; Sowers et al. 2010; Christensen et al. 2015] |
| Biomechanical devices | Knee braces, knee sleeves, foot orthoses can provide effective means of decreasing pain, joint stiffness and use of pain medication | [Raja and Dewan, 2011; Moyer et al. 2015] |
| Transcutaneous electrical nerve stimulation (TENS) | TENS has been reported to relieve pain and improve function in patients with knee osteoarthritis | [Bjordal et al. 2007; Bennell et al. 2015] |
| Acupuncture, herbal remedies, dietary supplements | Acupuncture has been shown to provide some benefit in the relief of OA pain Evidence suggests that several herbal medicines and dietary supplements could potentially alleviate OA pain |
[Mobasheri, 2012; Chen et al. 2014; Bennell et al. 2015] |
| Pharmacological | ||
| Analgesics | Acetaminophen is the main oral analgesic used for mild–moderate OA pain Opioids can be a treatment option for severe pain, or if other analgesics are contraindicated |
[Da Costa et al. 2014; Prior et al. 2014; Bannuru et al. 2015; Gelber, 2015; Machado et al. 2015] |
| NSAIDs | Ibuprofen, diclofenac, arthrotec, celecoxib, naproxen, and rofecoxib (oral or topical) | [Da Costa et al. 2014; Machado et al. 2015] |
| Disease-modifying OA drugs | Glucosamine, chondroitin sulfate, diacerein, doxycycline, strontium ranelate | [Gibofsky et al. 2014; Lapane et al. 2015] |
| COX2 inhibitors | COX2 inhibitors may provide effective analgesic/anti-inflammatory actions without the common gastrointestinal complications of traditional NSAIDs. However, there are concerns over the cardiovascular safety of these therapies | [Bannuru et al. 2015; Fibel et al. 2015] |
| Intra-articular injections | ||
| Corticosteroids | Corticosteroid injections appear to be an effective way to decrease pain in the short-term and increase joint mobility | [Ayhan et al. 2014; Fibel et al. 2015] |
| Hyaluronic acid (visco supplementation) | Hyaluronic acid (sodium hyaluronate) is a natural component of synovial fluid and cartilage in the knee and functions as a shock absorber | [Ayhan et al. 2014; Legre-Boyer, 2015] |
| Platelet-rich plasma (PRP) | Platelets from patient blood are separated from other components by centrifugation of a blood sample, then injected back into the patient’s affected joints/tissue(s) | [Jayabalan et al. 2014; Laudy et al. 2014; Lai et al. 2015] |
| Autologous conditioned serum (ACS) | Cell-free serum, generated by incubation of patient blood with glass spheres, is injected into the patient’s affected joints/tissue(s). In contrast to PRP, ACS does not contain any cells, clotting factors or additives | [Wehling et al. 2007, 2009; Alvarez-Camino et al. 2013; Frisbie, 2015] |
| Stem cell therapy | ||
| Mesenchymal stem cell (MSC) injections | MSCs have been described to have immunomodulatory, reparative, and anti-inflammatory properties. Their potential clinical applications include tissue repair. MSC injections could be potentially efficacious for decreasing pain and may improve physical function in patients with knee OA | [Jo et al. 2014; Xia et al. 2015] |
| Surgical treatment | ||
| Arthroscopy | The most common orthopedic procedure | [Moseley et al. 2002; Felson, 2010; Barlow and Plant, 2015] |
| Osteotomy | Patients with unicompartmental knee OA may be treated with an osteotomy. The goal is to unload the affected knee compartment | [Bhandari et al. 2012; Fibel et al. 2015] |
| Total knee arthroplasty (TKA) | Replacing the weight-bearing surfaces of the knee joint to relieve pain and disability is recommended, if conservative therapies are unsuccessful. Revision TKA is frequently required and can be problematic | [Bhandari et al. 2012; Proffen et al. 2013] |
COX2, cyclooxygenase-2; NSAIDs, nonsteroidal anti-inflammatory drugs; OA, osteoarthritis.
Nonpharmacological treatments
Nonpharmacological treatment of knee OA includes patient education on self-management and focuses on joint-unloading therapies, which include weight loss, physiotherapy, exercise, biomechanical interventions and orthotic devices [Hunter and Felson, 2006; Fibel et al. 2015]. Despite conflicting evidence regarding their benefits, electrotherapeutic treatment, acupuncture, herbal remedies and dietary supplements are also increasingly considered as treatment options for symptomatic knee OA (Table 1).
Pharmacological treatments
If symptoms do not improve after an extended period of nonpharmacological therapy (generally 3–6 months), pharmacological add-on treatments (Table 1) are recommended, which can be combined where appropriate [Crawford et al. 2013; McAlindon et al. 2014]. Acetaminophen, oral or topical nonsteroidal anti-inflammatory drugs (NSAIDs), cyclooxygenase 2 (COX2) inhibitors, disease-modifying drugs and opioids are regularly prescribed for short-term management of OA pain; however, evidence regarding their efficacy is increasingly being questioned, due to their risk for serious adverse events [Bobacz, 2013; Bannuru et al. 2015; Fibel et al. 2015].
Intra-articular injections
Intra-articular injections [corticosteroids, hyaluronic acid (HA), blood-derived products, mesenchymal stem cells; Table 1] are considered the final option for conservative therapy, if pharmacological treatments are unsuccessful [Ayhan et al. 2014]. In contrast to systemic pharmaceutical interventions, which also affect healthy tissues and organs and are intended primarily to reduce symptomology, some newer intra-articular therapies exert their effect by more directly targeting the underlying pathophysiological processes of knee OA in combination with symptom improvement. The research and development of new therapies focusing on the actual causes of knee OA, that is, loss of cartilage in the joint and the associated biological processes, falls within the concept of ‘molecular orthopedics’ [Evans and Rosier, 2005].
Corticosteroids act as anti-inflammatory and immunosuppressive agents, which appear to be an effective way to decrease pain in the short-term and are used when signs of inflammation occur. HA is a natural component of synovial fluid and cartilage in the knee, and HA injection (viscosupplementation) aims to restore viscoelasticity of synovial fluid in knees affected by OA [Legre-Boyer, 2015].
Platelet-rich plasma (PRP) is obtained from patients’ blood drawn at the time of treatment, with addition of an anticoagulant that prevents platelet activation prior to its use. Single centrifugation of the whole blood achieves a 1.5–2-fold higher concentration of platelets per volume due to the removal of erythrocytes. More refined techniques, for example those involving a second centrifugation step, can increase volume over 10 fold. When PRP is then injected back into the patient, platelets are activated and release growth factors, contributors thought to be important for the structural repair in the joint. Autologous conditioned serum (ACS) is also a blood-based OA treatment, generated by incubation (conditioning) of whole blood with glass beads. The conditioned, cell-free serum is recovered by centrifugation and then injected into the patient at weekly intervals [Evans, 2005; Wehling et al. 2007].
Intra-articular injection of mesenchymal stem cells could be beneficial for improvement of knee function [Jo et al. 2014]; however, it must be acknowledged that more data from larger studies on methods of preparation, long-term efficacy and safety are required before more refined conclusions regarding the benefits of this therapy can be drawn [Fibel et al. 2015; Xia et al. 2015].
Surgery
Historically, surgery has been a common treatment for knee OA and is recommended if conservative therapies have been exhausted. Typical indications for surgery are debilitating pain and major functional limitation (walking and daily activities or impaired ability to sleep or work), as well as x-ray evidence of narrowing of the knee joint space. Total knee arthroplasty (TKA) is the standard of care procedure for end-stage multicompartment knee OA [Bhandari et al. 2012]. This procedure replaces the weight-bearing surfaces of the knee joint to relieve pain and disability. While good long-term outcomes from surgery can usually be expected, revision surgery for TKA is often required, substantially increasing the risk for subsequent complications, since much of the original joint structure is sacrificed during the first round of surgery [Bhandari et al. 2012; Proffen et al. 2013]. Arthroscopy is a prevalent orthopedic surgical procedure suggested for cases where symptoms derive from mechanically unstable joint tissues [Hunter and Felson, 2006; WHO, 2013], and unicompartmental knee arthroplasty and osteotomy provide alternatives for patients with OA confined to one joint compartment [Bhandari et al. 2012]. Osteotomy is indicated in patients where mechanical shifting of the load from the diseased to the healthy joint compartment can slow disease progression and delay the need for TKA [Bhandari et al. 2012]. As recovery from osteotomy is typically prolonged, and subsequent TKA is needed in approximately 20% of patients within 10 years, the procedure is more indicated for young and active patients with a life expectancy exceeding that of a knee prosthesis [Virolainen and Aro, 2004; Bhandari et al. 2012; Spahn et al. 2013].
Surgical versus conservative therapies
Surgical procedures
Prevalence
TKA is widely considered the most effective treatment for end-stage OA in those who have exhausted available conservative interventions. In 2006, the incidence for knee replacement was approximately 100 procedures per 100,000 people in Europe [WHO, 2013]. With 304 procedures per 100,000 population, the US had the highest rate of knee replacement of industrialized countries in 2011, followed by Austria, Germany and Switzerland (218, 206 and 205 per 100,000 population, respectively); the proportion of revision surgery in Germany rose from 7.2% to 9.5% between 2005 and 2011, and in the US increased from 7.4% to 8.4% [OECD, 2013; Wengler et al. 2014]. The demand for TKA is continuously rising due to the ageing population and increasing levels of obesity, and the number of replacement surgeries performed in the US is estimated to increase by 673% by 2030 [Kurtz et al. 2007; Bitton, 2009].
Evidence
Concerns about a disconnect between trial evidence and orthopedic surgical practice question the position of surgery as the final treatment option for knee OA. Reports comparing operative with nonoperative procedures have suggested a lack of quality randomized control trials (RCTs) to evaluate the indications for surgery, and it has been suggested that efficacy of the majority of orthopedic surgical interventions is not supported by solid RCT evidence [Aspenberg, 2014; Lim et al. 2014]. A recent systematic review found that half of the studies using placebo controls provided evidence against the continued use of the investigated surgical procedures [Wartolowska et al. 2014], and the superiority of surgical intervention over conservative therapies is questioned [Lohmander and Roos, 2015]. Similarly, a number of studies investigating the efficacy of orthopedic surgery provided evidence that it does not provide more benefits compared with conservative therapies or sham treatments [Husted et al. 2014; Khan et al. 2014; Wartolowska et al. 2014; Lohmander and Roos, 2015]. Others argue that common surgical and perioperative precautions cause cost and discomfort for no gain at all [Husted et al. 2014].
Arthroscopy in particular has been used for many years for the treatment of knee OA to address degenerative articular cartilage and meniscal tears in middle-aged and older patients. The benefits of this minimally invasive surgical procedure (less postoperative pain or swelling, reduced risk of infections, no requirement for lengthy hospital stay, fast recovery) have resulted in a rapid increase in the number of arthroscopic surgeries [Katz et al. 2014]. However, concerns are being raised about a lack of evidence-based assessment of the efficacy and cost effectiveness of arthroscopy, and results from large RCTs have demonstrated that arthroscopic surgery for knee OA does not provide additional benefit to optimized conservative therapies [Felson, 2010; Katz et al. 2014; Thorlund et al. 2015]. The benefits seen from these interventions have been deemed inconsequential and limited in time, and, like other surgical procedures, knee arthroscopy is associated with risks. Taken together, these findings do not support the practice of arthroscopic surgery as a treatment option for knee OA [Thorlund et al. 2015].
Safety
Whereas conservative treatments are administered in the patient’s home or the treating physician’s practice, surgical procedures may require lengthy stays in hospital. A recent report stated that 4.5% of patients under the age of 65 experience complications during hospitalization, and that the complication rate more than doubles for older adults [Greengard, 2015a]. As with any surgery, there are potential risks for the orthopedic patient, including reaction to anesthesia or analgesia, bleeding, infection, thromboembolism, nerve damage, lack of full range of motion, cardiac events, reinjury of the joint or soft tissue and death [Greengard, 2015a].
Death has been described as an uncommon event after orthopedic operations, with a rate of acute mortality after inpatient orthopedic surgery of approximately 1% for all patients in the US [Bhattacharyya et al. 2002]. Generally, post-TKA mortality rates within 6 months have declined [Lalmohamed et al. 2014]; however, the same frequency of adverse events has been defined as ‘common’ or ‘frequent’ by the Council of International Organizations of Medical Sciences (CIOMS) [CIOMS]. Additionally, comorbidities common for patients with knee OA, such as an age greater than 70 years, chronic renal failure, congestive heart failure and chronic obstructive pulmonary disease, present critical risk factors for complications (including death) during or after surgery [Bhattacharyya et al. 2002; Belmont et al. 2014].
Thrombotic complications are a major concern following orthopedic surgery, and advanced patient age contributes to an increased risk, as do other comorbidities, for example, diabetes, coronary artery disease and obesity [Oberweis et al. 2013; Yang et al. 2014]. Postoperative infections caused by drug-resistant strains are common and of particular concern, and the overall infection rate following orthopedic surgery has been estimated to be approximately 5%, including a 1-year incidence of peri-prosthetic joint infection of 0.7%; infection incidence increases with age and growing rates of diabetes and obesity [Yang et al. 2014; Hackett et al. 2015].
Other postoperative complications, such as loosening or lysis, peri-prosthetic fracture and postoperative pain are also common risks associated with TKA, which can culminate in the need for revision surgery [Bhandari et al. 2012].
Costs
Compared with conservative therapies, surgical treatments are associated with high costs. According to a recent report, the revenue generated by sales of products for joint reconstruction was $15,415 million worldwide in 2014, with knee implants being the main contributor ($7,526 million), and these sales are expected to increase over the coming years (Figure 1) [Orthoworld, 2015].
Figure 1.
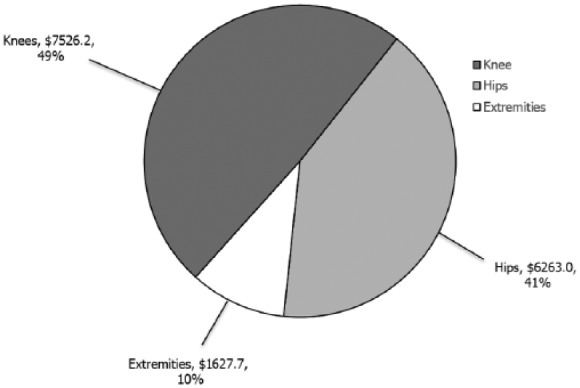
Sales by segment ($ millions) in 2014 in the joint reconstruction market. Adapted from the Orthopedic Industry Annual Report 2015, Orthoworld [Orthoworld, 2015].
Determining the cost of TKA per patient is challenging, with different reports stating a wide range of estimates which can vary substantially between countries, and even between hospitals, and depends on a variety of factors such as diagnosis, comorbidities, implant and surgical procedure cost [Bluecross]. One report found the average implant procedure cost per case to vary from $1,797 to $12,093 in the US [Robinson et al. 2012], whereas others stated that average TKA (including 5 years of follow-up care) costs £7,458 (approximately US $11,700) [Dakin et al. 2012]. Hospitalization comprises nearly half of the direct costs for OA; inpatient costs for primary TKA in the US were estimated to be $21,000 in 2009 ($25,000 for TKA revisions) [Bitton, 2009], however could be as high as $69,654 [Bluecross; Greengard, 2015b].
Revision TKAs significantly contribute to overall risks and costs of surgical treatment. Over 55,000 knee revision surgeries were performed in the US in 2010, and total costs associated with each revision TKA have been estimated to be over $49,000 [Bhandari et al. 2012], while other reports state average hospital costs of $19,000–31,000 [CALJRR, 2014], with the mean cost of a revision due to infection being more than three times that of an aseptic revision in the UK ($45,724 versus $14,709, respectively) [Kallala et al. 2015]. These costs exceed projections and, similarly to TKA, the number of revision surgery procedures is predicted to rise substantially by 2030, representing a major economic burden on healthcare systems [Iorio et al. 2005; Lavernia et al. 2006; Kurtz et al. 2007].
In spite of the associated high risks and costs, TKA is still considered to be a cost-effective treatment for knee OA [Daigle et al. 2012; Waimann et al. 2014]. However, due to the costs and use of advanced resources (for example, imaging procedures for diagnostic purposes) [Demehri et al. 2015], surgical treatments are often not readily available in many countries around the world [Hunter and Felson, 2006; WHO, 2013]. Given its invasive nature, the question arises if sufficient evidence exists to support the widespread use of surgery.
Physicians’ views and patient expectations
Although the number of orthopedic surgeries is increasing in industrialized countries, no standardized criteria exist to support evaluation of a patient’s suitability for these procedures. The fact that many orthopedic healthcare providers and, importantly, also patients see surgery as the ultimate treatment solution for knee OA is very likely an important reason why surgical intervention is still so prevalent.
The perceived superiority of orthopedic surgery is associated with established traditional opinions about its benefits, which, although often not evidence based [Moseley et al. 2002; Kirkley et al. 2008], are passed on to younger generations of orthopedic healthcare providers because ‘this is how it has always been done’ [Husted et al. 2014; Jarvinen et al. 2014; Barlow and Plant, 2015]. In addition, many surgeons feel under pressure from patients to offer a surgical procedure, believe that conservative treatments have been exhausted and that patients expect a different strategy [Barlow and Plant, 2015]. Physicians who believe in the value of the procedure that they recommend or administer may be more inclined to disregard scientific evidence that questions its suitability. However, this belief is often not based on clinical evidence. Therapeutic benefits are observed following the surgical intervention, but it cannot be determined if the intervention itself caused the benefits, if they are due to the patient’s placebo response or a result of natural disease progression [Miller and Kallmes, 2010]. Although the demand for TKAs is still rising, there is a notable trend to question the suitability of surgery on a case-by-case basis and to try and determine which patient might truly benefit from a surgical procedure [Dowsey et al. 2014].
Pain creates a significant burden, often resulting in lifestyle changes, and pain management is a paramount issue for symptomatic patients with OA. However, the origin of pain in knee OA is still not well understood, and no clear relation between radiographic OA damage and pain exists; patients can experience pain without radiographic evidence of OA, while others with radiographic OA have no symptoms related to these findings [Haviv et al. 2013].
Trying to understand the relationship between pathological pain and pain sensitivity could potentially offer insights into OA pain risk factors and management opportunities for the treating physician [Neogi et al. 2015]. However, patients with OA wish to receive an effective treatment that they feel will address their pain. Although they might be willing to consider self-management and conservative therapies, expectations of failure of these treatment modalities to manage pain are common [Smith et al. 2014], and surgery is still perceived as the ultimate strategy to achieve this goal, even though it cannot address the underlying cause of pain: inflammation. Similarly, patients are generally optimistic about the time required for functional recovery after surgery [De Achaval et al. 2015]. Together with the surgeons’ desire to meet their patients’ expectations and to help improve their quality of life, these factors can present a substantial barrier that prevents a change in the common perception of surgery being the final treatment option [Barlow and Plant, 2015].
Overall, these findings support the need for better quality RCTs to evaluate the indications for invasive orthopedic procedures, as well as in-depth evaluations in how established views of both orthopedic physicians and patients with OA can be challenged.
Conservative therapies, intra-articular injections and molecular orthopedics
Owing to the advances in molecular biology and continuous improvement of proteomic, pharmacogenetic and bioinformatic techniques, the range of therapeutic options available to orthopedic medicine is rapidly expanding. This concept of ‘molecular orthopedics’ is becoming increasingly relevant for the development and refinement of conservative therapies, allowing more patient-centered diagnostic and treatment strategies [Evans et al. 2005].
Although data on long-term efficacy are still limited, a key consideration for intra-articular injection as a treatment modality for knee OA is the superior safety profile: in comparison to surgery or pharmacological treatments, adverse events and side effects of intra-articular injections are rare and often due to reactions to the injection process itself (for example, swelling, redness), rather than the agent. Further advantages of intra-articular injections include ease of administration, which eliminates the need for hospitalization, increased bioavailability and reduced systemic exposure [Evans et al. 2014]. Ultimately, this could also contribute to a much lower cost of these therapeutic options compared with surgery [Arnold et al. 2007; Evans et al. 2014].
Data on costs and cost effectiveness for conservative therapies are limited. In 2012, OA disease-modifying drugs were priced at $1,000/year in the US, and it was suggested that their cost effectiveness depends on the treatment strategy they are part of and their ability to reduce the need for TKA [Losina et al. 2013]. A systematic review concluded that economic analyses investigating nonpharmacological OA treatments were seriously compromised due to most studies including comparators of unknown cost effectiveness [Pinto et al. 2012]. Costs are directly proportional to disease severity and, in 2013, the cost of conservative OA treatments was reported as $14.4 billion/year in the US, while their cost effectiveness was questioned due to lack of impact on disease progression [Crawford et al. 2013].
However, a growing number of physicians are starting to rely more on conservative therapies, and intra-articular injections in particular, for treatment of orthopedic indications, and are promoting research of their efficacy and safety [Evans, 2005]. Patient attitude towards conservative treatments remains an issue that requires further attention; uncertainty about long-term benefits and expectations of failure to manage pain and symptoms for conservative treatment are still common [Smith et al. 2014].
Autologous blood products
Autologous blood products (PRP and ACS) have demonstrated efficacy and safety as knee OA treatment in a number of studies, although further trials are required to fully evaluate their benefits.
Benefits of PRP injections as treatment for OA [Jayabalan et al. 2014; Laudy et al. 2014; Lai et al. 2015], in particular in younger patients with earlier stages of knee OA, have been demonstrated [Halpern et al. 2013; Patel et al. 2013]. Comparison of PRP with either placebo or HA injection provided evidence for PRP as the superior therapy [Filardo et al. 2015]. However, clinical results from PRP studies are inconsistent and provide insufficient evidence for the use of PRP in OA and other orthopedic indications [Ayhan et al. 2014; Moraes et al. 2014]. The main concern for this therapeutic option is that variations in PRP preparation, formulation and application could contribute to the observed differences in treatment outcomes. At least three different preparation methods for PRP have been described, which can yield products with varying compositions and characteristics. Upon injection into the joint, activated platelets release a host of soluble mediators, such as growth factors and cytokines, thereby inducing complex interactions that vary across tissues within the joint, introducing additional levels of complexity and potential for variable outcomes for this therapy. In addition, PRP also requires addition of calcium chloride and other additives (anticoagulant agents, thrombin). All these factors contribute to concerns regarding the lack of standardization and efficacy of this treatment modality [Ayhan et al. 2014; Moraes et al. 2014; Beitzel et al. 2015].
In contrast to PRP, ACS is a cell-free serum preparation that contains no additives. ACS is used as a local treatment to control the pain and impaired function in knee and hip OA, lower back pain, sport and meniscal injuries and tendinopathies [Wehling et al. 2007; Evans et al. 2014]. Processing of ACS includes incubation of whole blood, releasing anti-inflammatory cytokines (e.g. interleukin 1Ra) and regenerative growth factors (e.g. transforming growth factor ß), and the injected cell-free ACS supports the natural healing processes in the knee [Wehling et al. 2009; Fox and Stephens, 2010; Evans et al. 2014]. Utilization of an ACS-processing device ensures a standardized procedure for the generation of every single ACS injection. Preparation and injection of ACS are uncomplicated and less invasive than surgery, and clinical studies have demonstrated that treatment with ACS is highly effective for improving pain and function, as well as being well tolerated, with a low incidence of adverse events [Wehling et al. 2007, 2009; Auw Yang et al. 2008; Baltzer et al. 2009; Astolfi et al. 2014; Rutgers et al. 2015]. Clinical data indicate a more robust clinical response to ACS than has been shown for PRP. The clinical superiority of ACS over intra-articular placebo and HA has been demonstrated in a randomized trial [Baltzer et al. 2009], and evidence of the efficacy of ACS combined with physiotherapy regarding pain and global OA outcomes has been recently established [Baselga and Hernandez, 2015].
Due to its autologous nature and mode of administration, not requiring patient hospitalization, ACS treatment is associated with fewer risks and lower costs (ACS treatment, comprising six injections, costs approximately US$2,500–3,000 per patient, depending on country) than other pharmacological therapies or surgery [Wehling et al. 2009]. The concerns regarding variability in PRP composition and treatment outcomes do not apply to ACS due to its cell-free nature. The standardized preparation methodology (including aliquoting and storage by freezing after a single withdrawal of patient’s blood) ensures that ACS composition is consistent, whereas blood for the generation of PRP has to be withdrawn for each injection and cannot be stored or frozen. The apparent symptom- and possibly disease-modifying effects of ACS are based on its mechanism of action, which targets the underlying molecular, rather than the mechanical causes of OA [Wehling et al. 2009].
Conclusion
Multiple therapy options, aside from surgery, are available for the treatment of OA. It is important to recognize that the pathophysiology of the OA disease process is complex and requires a flexible treatment approach to improve pain and function [Fibel et al. 2015]. There is substantial evidence that conservative therapies, in particular intra-articular injections, have the potential to provide benefits potentially outweighing those of established pharmacological treatments, for example, concerns about bioavailability, dosing or drug interactions [Evans et al. 2014], and surgery.
The common perception of surgery as a ‘go-to-solution’, both of physicians as well as patients, should be questioned and awareness raised about the benefits of conservative therapies [Barlow and Plant, 2015; De Achaval et al. 2015]. The traditional hierarchy of treatment options for knee OA is becoming less rigid, especially as patients’ individual needs and preferences, as well as their molecular profile, are being considered in the context of a personalized care strategy [Evans and Rosier, 2005; McAlindon et al. 2014]. Furthermore, the need for evidence supporting the use of surgical procedures, transparency of conduct and reporting of surgical research is recognized [McCulloch et al. 2009; Miller and Kallmes, 2010; Wartolowska et al. 2014; Lohmander and Roos, 2015]. In addition, a possible publication bias, which might hinder or favor the publication of results that contradict or question the superiority of surgery, has caused substantial controversy [Miller and Kallmes, 2010; Lubowitz et al. 2014; Rossi et al. 2014; Lohmander and Roos, 2015]; however, a detailed review of the ongoing discussions regarding the publication policies is outside the scope of this publication.
Another controversy is presented when considering mortality rates: death post surgery (acute mortality rates: approximately 1%) [Bhattacharyya et al. 2002] has been deemed an uncommon event, diverging from the CIOMS drug safety evaluation criteria. Similarly, as the ageing population contributes to the increasing number of joint replacement procedures in industrialized countries, it may be questioned if this type of elective surgery should be considered a mere routine treatment, rather than as a last option, in particular when examining its cost effectiveness.
In order to provide alternatives to surgery that are recognized and valued by healthcare providers and patients, more data are required on the efficacy, safety and cost effectiveness of conservative therapies, so that their integration into treatment strategies for knee OA can be further optimized. Focus is shifting towards research and development of treatments targeting the underlying molecular mechanisms of knee OA to slow or even prevent disease progression, rather than just providing symptomatic pain relief, as well as identification of patients who may benefit most from a particular treatment strategy. Reduction of pain and inflammation, as well as promotion of reparative processes, leads to clinical improvements, resulting in better functionality and mobility, and therefore enabling patients to regain better quality of life.
ACS as therapy for knee OA is a prime example for an efficacious therapy based on the concept of molecular orthopedics. Rather than just being part of the hierarchy leading towards it, this treatment strategy has the potential to provide a valuable alternative to surgery, by targeting multiple pathways involved in tissue repair.
Acknowledgments
The authors thank Dr Tanju Kaptan (Medical Director, Orthogen AG) for publication management. The authors acknowledge Julia Bárdos, PhD and Helen Croxall, PhD from Costello Medical Consulting, UK for writing assistance and administrative support.
Footnotes
Funding: All costs associated with development of this publication were funded by Orthogen AG.
Conflict of interest statement: PW is the CEO of Orthogen AG. CM has provided consultancy for Orthogen AG. WM has provided consultancy for Orthogen AG. Orthogen AG currently holds patents for ACS and for the ACS processing device.
Contributor Information
Peter Wehling, Center of Molecular Orthopaedics and Regenerative Medicine, Stadttor 1, 40219 Düsseldorf, Germany.
Carsten Moser, Grönemeyer Institute for Microtherapy, University Witten/Herdecke, Bochum, Germany.
William Maixner, Center for Translational Pain Medicine, Duke University School of Medicine, Durham, North Carolina, USA.
References
- Alvarez-Camino J., Vazquez-Delgado E., Gay-Escoda C. (2013) Use of autologous conditioned serum (Orthokine) for the treatment of the degenerative osteoarthritis of the temporomandibular joint. Review of the literature. Med Oral Patol Oral Cir Bucal 18: e433–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold W., Fullerton D., Holder S., May C. (2007) Viscosupplementation: managed care issues for osteoarthritis of the knee. J Manag Care Pharm 13: S3–19; quiz S20–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aspenberg P. (2014) Mythbusting in orthopedics challenges our desire for meaning. Acta Orthop 85: 547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Astolfi M., McGuire K., Kaminski T. (2014) The effectiveness of autologous conditioned serum in the treatment of knee osteoarthritis. J Sport Rehabil 23: 365–369. [DOI] [PubMed] [Google Scholar]
- Auw Yang K., Raijmakers N., Van Arkel E., Caron J., Rijk P., Willems W., et al. (2008) Autologous interleukin-1 receptor antagonist improves function and symptoms in osteoarthritis when compared to placebo in a prospective randomized controlled trial. Osteoarthritis Cartilage 16: 498–505. [DOI] [PubMed] [Google Scholar]
- Ayhan E., Kesmezacar H., Akgun I. (2014) Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J Orthop 5: 351–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baltzer A., Moser C., Jansen S., Krauspe R. (2009) Autologous conditioned serum (Orthokine) is an effective treatment for knee osteoarthritis. Osteoarthritis Cartilage 17: 152–160. [DOI] [PubMed] [Google Scholar]
- Bannuru R., Schmid C., Kent D., Vaysbrot E., Wong J., McAlindon T. (2015) Comparative effectiveness of pharmacologic interventions for knee osteoarthritis: a systematic review and network meta-analysis. Ann Intern Med 162: 46–54. [DOI] [PubMed] [Google Scholar]
- Barlow T., Plant C. (2015) Why we still perform arthroscopy in knee osteoarthritis: a multi-methods study. BMC Musculoskelet Disord 16: 85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baselga J., Hernandez P. (2015) Treatment of osteoarthritis of the knee with a combination of autologous conditioned serum and physiotherapy: a two-year observational study. PLoS One 10: e0145551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beitzel K., Allen D., Apostolakos J., Russell R., McCarthy M., Gallo G., et al. (2015) US definitions, current use, and FDA stance on use of platelet-rich plasma in sports medicine. J Knee Surg 28: 29–34. [DOI] [PubMed] [Google Scholar]
- Belmont P., Jr, Goodman G., Waterman B., Bader J., Schoenfeld A. (2014) Thirty-day postoperative complications and mortality following total knee arthroplasty: incidence and risk factors among a national sample of 15,321 patients. J Bone Joint Surg Am 96: 20–26. [DOI] [PubMed] [Google Scholar]
- Bennell K., Buchbinder R., Hinman R. (2015) Physical therapies in the management of osteoarthritis: current state of the evidence. Curr Opin Rheumatol 27: 304–311. [DOI] [PubMed] [Google Scholar]
- Bhandari M., Smith J., Miller L., Block J. (2012) Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord 5: 89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhattacharyya T., Iorio R., Healy W. (2002) Rate of and risk factors for acute inpatient mortality after orthopaedic surgery. J Bone Joint Surg Am 84-A: 562–572. [DOI] [PubMed] [Google Scholar]
- Bitton R. (2009) The economic burden of osteoarthritis. Am J Manag Care 15: S230–S235. [PubMed] [Google Scholar]
- Bjordal J., Johnson M., Lopes-Martins R., Bogen B., Chow R., Ljunggren A. (2007) Short-term efficacy of physical interventions in osteoarthritic knee pain. a systematic review and meta-analysis of randomised placebo-controlled trials. BMC Musculoskelet Disord 8: 51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluecross. (2015) A study of cost variations for knee and hip replacement surgeries in the U.S. Available at: http://www.bcbs.com/healthcare-news/bcbsa/bcbsa-study-reveals-extreme-cost-variations-for-knee-and-hip-replacement-surgeries.html (accessed April 2016).
- Bobacz K. (2013) Pharmacologic treatment of hand-, knee- and hip-osteoarthritis. Wien Med Wochenschr 163: 236–242. [DOI] [PubMed] [Google Scholar]
- CALJRR (2014) The California Joint Replacement Registry: progress update. Available at http://caljrr.org/attachments/cjrr2014progressupdate.pdf (accessed November 2015).
- Chen X., Spaeth R., Retzepi K., Ott D., Kong J. (2014) Acupuncture modulates cortical thickness and functional connectivity in knee osteoarthritis patients. Sci Rep 4: 6482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christensen R., Henriksen M., Leeds A., Gudbergsen H., Christensen P., Sorensen T., et al. (2015) Effect of weight maintenance on symptoms of knee osteoarthritis in obese patients: a twelve-month randomized controlled trial. Arthritis Care Res (Hoboken) 67: 640–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CIOMS. (2001) Guidelines for preparing core clinical-safety information on drugs, including new proposals for investigators brochures. Report of CIOMS Working Groups III and V. Geneva: CIOMS. [Google Scholar]
- Crawford D., Miller L., Block J. (2013) Conservative management of symptomatic knee osteoarthritis: a flawed strategy? Orthop Rev (Pavia) 5: e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cross M., Smith E., Hoy D., Nolte S., Ackerman I., Fransen M., et al. (2014) The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 Study. Ann Rheum Dis 73: 1323–1330. [DOI] [PubMed] [Google Scholar]
- Da Costa B., Nuesch E., Kasteler R., Husni E., Welch V., Rutjes A., et al. (2014) Oral or transdermal opioids for osteoarthritis of the knee or hip. Cochrane Database Syst Rev 9: CD003115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daigle M., Weinstein A., Katz J., Losina E. (2012) The cost-effectiveness of total joint arthroplasty: a systematic review of published literature. Best Pract Res Clin Rheumatol 26: 649–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dakin H., Gray A., Fitzpatrick R., Maclennan G., Murray D. (2012) Rationing of total knee replacement: a cost-effectiveness analysis on a large trial data set. BMJ Open 2: e000332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Achaval S., Kallen M., Amick B., Landon G., Siff S., Edelstein D., et al. (2016) Patients’ expectations about total knee arthroplasty outcomes. Health Expect 19: 299–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Demehri S., Hafezi-Nejad N., Carrino J. (2015) Conventional and novel imaging modalities in osteoarthritis: current state of the evidence. Curr Opin Rheumatol 27: 295–303. [DOI] [PubMed] [Google Scholar]
- De Rezende M, De Campos G., Pailo A. (2013) Current concepts in osteoarthritis. Acta Ortop Bras 21: 120–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dowsey M., Gunn J., Choong P. (2014) Selecting those to refer for joint replacement: who will likely benefit and who will not? Best Pract Res Clin Rheumatol 28: 157–171. [DOI] [PubMed] [Google Scholar]
- Du S., Yuan C., Xiao X., Chu J., Qiu Y., Qian H. (2011) Self-management programs for chronic musculoskeletal pain conditions: a systematic review and meta-analysis. Patient Educ Couns 85: e299–e310. [DOI] [PubMed] [Google Scholar]
- Evans C. (2005) Novel biological approaches to the intra-articular treatment of osteoarthritis. BioDrugs 19: 355–362. [DOI] [PubMed] [Google Scholar]
- Evans C., Kraus V., Setton L. (2014) Progress in intra-articular therapy. Nat Rev Rheumatol 10: 11–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans C., Rosier R. (2005) Molecular biology in orthopaedics: the advent of molecular orthopaedics. J Bone Joint Surg Am 87: 2550–2564. [DOI] [PubMed] [Google Scholar]
- Felson D. (2010) Arthroscopy as a treatment for knee osteoarthritis. Best Pract Res Clin Rheumatol 24: 47–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fibel K., Hillstrom H., Halpern B. (2015) State-of-the-art management of knee osteoarthritis. World J Clin Cases 3: 89–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filardo G., Di Matteo B., Di Martino A., Merli M., Cenacchi A., Fornasari P., et al. (2015) Platelet-rich plasma intra-articular knee injections show no superiority versus viscosupplementation: a randomized controlled trial. Am J Sports Med 43: 1575–1582. [DOI] [PubMed] [Google Scholar]
- Fox B., Stephens M. (2010) Treatment of knee osteoarthritis with orthokine-derived autologous conditioned serum. Expert Rev Clin Immunol 6: 335–345. [DOI] [PubMed] [Google Scholar]
- Frisbie D. (2015) Autologous-conditioned serum: evidence for use in the knee. J Knee Surg 28: 63–66. [DOI] [PubMed] [Google Scholar]
- Gelber A. (2015) Conventional medical therapy for osteoarthritis: current state of the evidence. Curr Opin Rheumatol 27: 312–317. [DOI] [PubMed] [Google Scholar]
- Gibofsky A., Hochberg M., Jaros M., Young C. (2014) Efficacy and safety of low-dose submicron diclofenac for the treatment of osteoarthritis pain: a 12 week, phase 3 study. Curr Med Res Opin 30: 1883–1893. [DOI] [PubMed] [Google Scholar]
- Greengard S. (2015a) Risks and complications of total knee replacement surgery. Available at: http://www.healthline.com/health/total-knee-replacement-surgery/risks-complications#1 (accessed 20 August 2015).
- Greengard S. (2015b) Understanding knee replacement costs: what’s on the bill? Available at: http://www.healthline.com/health/total-knee-replacement-surgery/understanding-costs#1 (accessed 20 August 2015).
- Hackett D., Rothenberg A., Chen A., Gutowski C., Jaekel D., Tomek I., et al. (2015) The economic significance of orthopaedic infections. J Am Acad Orthop Surg 23(Suppl.): S1–S7. [DOI] [PubMed] [Google Scholar]
- Halpern B., Chaudhury S., Rodeo S., Hayter C., Bogner E., Potter H., et al. (2013) Clinical and MRI outcomes after platelet-rich plasma treatment for knee osteoarthritis. Clin J Sport Med 23: 238–239. [DOI] [PubMed] [Google Scholar]
- Haviv B., Bronak S., Thein R. (2013) The complexity of pain around the knee in patients with osteoarthritis. Isr Med Assoc J 15: 178–181. [PubMed] [Google Scholar]
- Hrnack S., Barber F. (2014) Managing the pain of knee osteoarthritis. Phys Sportsmed 42: 63–70. [DOI] [PubMed] [Google Scholar]
- Hunter D., Felson D. (2006) Osteoarthritis. BMJ 332: 639–642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Husted H., Gromov K., Malchau H., Freiberg A., Gebuhr P., Troelsen A. (2014) Traditions and myths in hip and knee arthroplasty. Acta Orthop 85: 548–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iorio R., Healy W., Ayers M. (2005) Economics of revision total knee arthroplasty: increasing prevalence, decreasing reimbursement. In: Bono J., Scott R. (eds), Revision Total Knee Arthroplasty. Berlin: Springer. [Google Scholar]
- Jarvinen T., Sihvonen R., Englund M. (2014) Arthroscopy for degenerative knee – a difficult habit to break? Acta Orthop 85: 215–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayabalan P., Hagerty S., Cortazzo M. (2014) The use of platelet-rich plasma for the treatment of osteoarthritis. Phys Sportsmed 42: 53–62. [DOI] [PubMed] [Google Scholar]
- Jo C., Lee Y., Shin W., Kim H., Chai J., Jeong E., et al. (2014) Intra-articular injection of mesenchymal stem cells for the treatment of osteoarthritis of the knee: a proof-of-concept clinical trial. Stem Cells 32: 1254–1266. [DOI] [PubMed] [Google Scholar]
- Kallala R., Vanhegan I., Ibrahim M., Sarmah S., Haddad F. (2015) Financial analysis of revision knee surgery based on NHS tariffs and hospital costs: does it pay to provide a revision service? Bone Joint J 97-b: 197–201. [DOI] [PubMed] [Google Scholar]
- Katz J., Brownlee S., Jones M. (2014) The role of arthroscopy in the management of knee osteoarthritis. Best Pract Res Clin Rheumatol 28: 143–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan M., Evaniew N., Bedi A., Ayeni O., Bhandari M. (2014) Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ 186: 1057–1064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkley A., Birmingham T., Litchfield R., Giffin J., Willits K., Wong C., et al. (2008) A randomized trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 359: 1097–1107. [DOI] [PubMed] [Google Scholar]
- Kurtz S., Ong K., Lau E., Mowat F., Halpern M. (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89: 780–785. [DOI] [PubMed] [Google Scholar]
- Lai L., Stitik T., Foye P., Georgy J., Patibanda V., Chen B. (2015) Use of platelet rich plasma in intra-articular knee injections for osteoarthritis: a systematic review. PM R 7: 637–638. [DOI] [PubMed] [Google Scholar]
- Lalmohamed A., Vestergaard P., De Boer A., Leufkens H., Van Staa T., De Vries F. (2014) Changes in mortality patterns following total hip or knee arthroplasty over the past two decades: a nationwide cohort study. Arthritis Rheumatol 66: 311–318. [DOI] [PubMed] [Google Scholar]
- Lapane K., Yang S., Driban J., Liu S., Dube C., Mcalindon T., et al. (2015) Effects of prescription nonsteroidal antiinflammatory drugs on symptoms and disease progression among patients with knee osteoarthritis. Arthritis Rheumatol 67: 724–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudy A., Bakker E., Rekers M., Moen M. (2015) Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br J Sports Med 49: 657–672. [DOI] [PubMed] [Google Scholar]
- Lavernia C., Lee D., Hernandez V. (2006) The increasing financial burden of knee revision surgery in the United States. Clin Orthop Relat Res 446: 221–226. [DOI] [PubMed] [Google Scholar]
- Legre-Boyer V. (2015) Viscosupplementation: techniques, indications, results. Orthop Traumatol Surg Res 101: S101–S108. [DOI] [PubMed] [Google Scholar]
- Lim H., Adie S., Naylor J., Harris I. (2014) Randomised trial support for orthopaedic surgical procedures. PLoS One 9: e96745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lohmander L., Roos E. (2015) The evidence base for orthopaedics and sports medicine. BMJ 350: g7835. [DOI] [PubMed] [Google Scholar]
- Losina E., Daigle M., Suter L., Hunter D., Solomon D., Walensky R., et al. (2013) Disease-modifying drugs for knee osteoarthritis: can they be cost-effective? Osteoarthritis Cartilage 21: 655–667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lubowitz J., Provencher M., Rossi M. (2014) Could the New England Journal of Medicine be biased against arthroscopic knee surgery? Part 2. Arthroscopy 30: 654–655. [DOI] [PubMed] [Google Scholar]
- Machado G., Maher C., Ferreira P., Pinheiro M., Lin C., Day R., et al. (2015) Efficacy and safety of paracetamol for spinal pain and osteoarthritis: systematic review and meta-analysis of randomised placebo controlled trials. BMJ 350: h1225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAlindon T., Bannuru R., Sullivan M., Arden N., Berenbaum F., Bierma-Zeinstra S., et al. (2014) OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis Cartilage 22: 363–388. [DOI] [PubMed] [Google Scholar]
- McCulloch P., Altman D., Campbell W., Flum D., Glasziou P., Marshall J., et al. (2009) No surgical innovation without evaluation: the IDEAL recommendations. Lancet 374: 1105–1112. [DOI] [PubMed] [Google Scholar]
- Menkes C. (1991) Radiographic criteria for classification of osteoarthritis. J Rheumatol Suppl 27: 13–15. [PubMed] [Google Scholar]
- Messier S., Loeser R., Miller G., Morgan T., Rejeski W., Sevick M., et al. (2004) Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the Arthritis, Diet, and Activity Promotion Trial. Arthritis Rheum 50: 1501–1510. [DOI] [PubMed] [Google Scholar]
- Miller F., Kallmes D. (2010) The case of vertebroplasty trials: promoting a culture of evidence-based procedural medicine. Spine (Phila Pa 1976) 35: 2023–2026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mobasheri A. (2012) Intersection of inflammation and herbal medicine in the treatment of osteoarthritis. Curr Rheumatol Rep 14: 604–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moraes V., Lenza M., Tamaoki M., Faloppa F., Belloti J. (2014) Platelet-rich therapies for musculoskeletal soft tissue injuries. Cochrane Database Syst Rev 4: CD010071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moseley J., O’Malley K., Petersen N., Menke T., Brody B., Kuykendall D., et al. (2002) A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med 347: 81–88. [DOI] [PubMed] [Google Scholar]
- Moyer R., Birmingham T., Bryant D., Giffin J., Marriott K., Leitch K. (2015) Biomechanical effects of valgus knee bracing: a systematic review and meta-analysis. Osteoarthritis Cartilage 23: 178–188. [DOI] [PubMed] [Google Scholar]
- Neogi T., Frey-Law L., Scholz J., Niu J., Arendt-Nielsen L., Woolf C., et al. (2015) Sensitivity and sensitisation in relation to pain severity in knee osteoarthritis: trait or state? Ann Rheum Dis 74: 682–688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oberweis B., Nukala S., Rosenberg A., Guo Y., Stuchin S., Radford M., et al. (2013) Thrombotic and bleeding complications after orthopedic surgery. Am Heart J 165: 427–433 e421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OECD (2013) Health at a glance 2013: OECD indicators. Available at: http://wwwoecdorg/els/health-systems/Health-at-a-Glance-2013pdf (accessed April 2015):
- Orthoworld (2015) The orthopedic industry annual report. Available at: https://www.orthoworld.com/index.php/products/oiar (accessed 18 March 2016).
- Patel S., Dhillon M., Aggarwal S., Marwaha N., Jain A. (2013) Treatment with platelet-rich plasma is more effective than placebo for knee osteoarthritis: a prospective, double-blind, randomized trial. Am J Sports Med 41: 356–364. [DOI] [PubMed] [Google Scholar]
- Pinto D., Robertson M., Hansen P., Abbott J. (2012) Cost-effectiveness of nonpharmacologic, nonsurgical interventions for hip and/or knee osteoarthritis: systematic review. Value Health 15: 1–12. [DOI] [PubMed] [Google Scholar]
- Prasad V., Cifu A., Ioannidis J. (2012) Reversals of established medical practices: evidence to abandon ship. JAMA 307: 37–38. [DOI] [PubMed] [Google Scholar]
- Prior M., Harrison D., Frustaci M. (2014) A randomized, double-blind, placebo-controlled 12 week trial of acetaminophen extended release for the treatment of signs and symptoms of osteoarthritis. Curr Med Res Opin 30: 2377–2387. [DOI] [PubMed] [Google Scholar]
- Proffen B., Vavken P., Dorotka R. (2013) Surgical management of osteoarthritis. Wien Med Wochenschr 163: 243–250. [DOI] [PubMed] [Google Scholar]
- Raja K., Dewan N. (2011) Efficacy of knee braces and foot orthoses in conservative management of knee osteoarthritis: a systematic review. Am J Phys Med Rehabil 90: 247–262. [DOI] [PubMed] [Google Scholar]
- Robinson J., Pozen A., Tseng S., Bozic K. (2012) Variability in costs associated with total hip and knee replacement implants. J Bone Joint Surg Am 94: 1693–1698. [DOI] [PubMed] [Google Scholar]
- Rossi M., D’Agostino R., Jr, Provencher M., Lubowitz J. (2014) Could the New England Journal of Medicine be biased against arthroscopic knee surgery? Arthroscopy 30: 536–537. [DOI] [PubMed] [Google Scholar]
- Rutgers M., Creemers L., Auw Yang K., Raijmakers N., Dhert W., Saris D. (2015) Osteoarthritis treatment using autologous conditioned serum after placebo. Acta Orthop 86: 114–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T., Purdy R., Lister S., Salter C., Fleetcroft R., Conaghan P. (2014) Attitudes of people with osteoarthritis towards their conservative management: a systematic review and meta-ethnography. Rheumatol Int 34: 299–313. [DOI] [PubMed] [Google Scholar]
- Sowers M., Karvonen-Gutierrez C. (2010) The evolving role of obesity in knee osteoarthritis. Curr Opin Rheumatol 22: 533–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spahn G., Hofmann G., Von Engelhardt L., Li M., Neubauer H., Klinger H. (2013) The impact of a high tibial valgus osteotomy and unicondylar medial arthroplasty on the treatment for knee osteoarthritis: a meta-analysis. Knee Surg Sports Traumatol Arthrosc 21: 96–112. [DOI] [PubMed] [Google Scholar]
- Thorlund J., Juhl C., Roos E., Lohmander L. (2015) Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. BMJ 350: h2747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Virolainen P., Aro H. (2004) High tibial osteotomy for the treatment of osteoarthritis of the knee: a review of the literature and a meta-analysis of follow-up studies. Arch Orthop Trauma Surg 124: 258–261. [DOI] [PubMed] [Google Scholar]
- Waimann C., Fernandez-Mazarambroz R., Cantor S., Lopez-Olivo M., Zhang H., Landon G., et al. (2014) Cost-effectiveness of total knee replacement: a prospective cohort study. Arthritis Care Res (Hoboken) 66: 592–599. [DOI] [PubMed] [Google Scholar]
- Wartolowska K., Judge A., Hopewell S., Collins G., Dean B., Rombach I., et al. (2014) Use of placebo controls in the evaluation of surgery: systematic review. BMJ 348: g3253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehling P., Moser C., Frisbie D., McIlwraith C., Kawcak C., Krauspe R., et al. (2007) Autologous conditioned serum in the treatment of orthopedic diseases: the Orthokine therapy. BioDrugs 21: 323–332. [DOI] [PubMed] [Google Scholar]
- Wehling P., Moser C., Reinecke J. (2009) Use of autologous conditioned cell-free serum (Orthokine®) in treating osteoarthritis and sciatic back pain. Eur Musculoskel Rev 4: 8–11. [Google Scholar]
- Wengler A., Nimptsch U., Mansky T. (2014) Hip and knee replacement in Germany and the USA: analysis of individual inpatient data from German and US hospitals for the years 2005 to 2011. Dtsch Arztebl Int 111: 407–416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) (2013) Osteoarthritis. Update on background paper 6.12. Available at: http://appswhoint/medicinedocs/en/m/abstract/Js20259en/ (accessed April 2015).
- World Health Organization (WHO) (2015) Chronic rheumatic conditions. Available at: http://wwwwhoint/chp/topics/rheumatic/en/ (accessed April 2015).
- Xia P., Wang X., Lin Q., Li X. (2015) Efficacy of mesenchymal stem cells injection for the management of knee osteoarthritis: a systematic review and meta-analysis. Int Orthop 39: 2363–2372. [DOI] [PubMed] [Google Scholar]
- Yang Z., Liu H., Xie X., Tan Z., Qin T., Kang P. (2014) The influence of diabetes mellitus on the post-operative outcome of elective primary total knee replacement: a systematic review and meta-analysis. Bone Joint J 96-B: 1637–1643. [DOI] [PubMed] [Google Scholar]
- Zhang W., Nuki G., Moskowitz R., Abramson S., Altman R., Arden N., et al. (2010) OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthritis Cartilage 18: 476–499. [DOI] [PubMed] [Google Scholar]


