Abstract
Objective:
Mental disorders are common in military organizations, and these frequently lead to functional impairments that can interfere with duties and lead to costly attrition. In Canada, the military mental health system has received heavy investment to improve occupational outcomes. We investigated military occupational outcomes of diagnosed mental disorders in a cohort of 30,513 personnel who deployed on the Afghanistan mission.
Methods:
Cohort members were military personnel who deployed on the Afghanistan mission from 2001 to 2008. Mental disorder diagnoses and their attribution to the Afghanistan mission were ascertained via medical records in a stratified random sample (n = 2014). Career-limiting medical conditions (that is, condition-associated restrictions that reliably lead to medically related attrition) were determined using administrative data. Outcomes were assessed from first Afghanistan-related deployment return.
Results:
At 5 years of follow-up, the Kaplan-Meier estimated cumulative fraction with career-limiting medical conditions was 40.9% (95% confidence interval [CI] 35.5 to 46.4) among individuals with Afghanistan service–related mental disorders (ARMD), 23.6% (CI 15.5 to 31.8) with other mental disorders, and 11.1% (CI 8.9 to 13.3) without mental disorders. The adjusted Cox regression hazard ratios for career-limiting medical condition risk were 4.89 (CI 3.85 to 6.23) among individuals with ARMD and 2.31 (CI 1.48 to 3.60) with other mental disorders, relative to those without mental disorders.
Conclusions:
Notwithstanding the Canadian military’s mental health system investments, mental disorders (particularly ARMD) still led to a high risk of adverse military occupational outcomes. Such investments have intrinsic value but may not translate into reduced medically related attrition without improvements in prevention and treatment effectiveness.
Keywords: military occupational fitness, service-related mental disorders, mental disorders
Abstract
Objectif:
Les troubles mentaux sont communs dans les organisations militaires, et ils mènent fréquemment à des déficiences fonctionnelles qui peuvent perturber les tâches et entraîner une attrition coûteuse. Au Canada, le système de santé mentale militaire a fait l’objet d’un investissement important afin d’améliorer les résultats professionnels. Nous avons investigué les résultats professionnels militaires des troubles mentaux diagnostiqués dans une cohorte de 30 513 membres du personnel qui ont été déployés pour la mission d’Afghanistan.
Méthodes:
Les membres de la cohorte faisaient partie du personnel militaire déployé pour la mission d’Afghanistan de 2001 à 2008. Les diagnostics de troubles mentaux et leur attribution à la mission d’Afghanistan ont été vérifiés par les dossiers médicaux d’un échantillon aléatoire stratifié (n = 2 014). Les affections médicales limitant la carrière (c.-à-d., des restrictions associées à une affection qui mènent assurément à une attrition médicale) ont été déterminées à l’aide des données administratives. Les résultats ont été évalués au premier retour de déploiement d’Afghanistan.
Résultats:
Au suivi de 5 ans, la fraction cumulative estimée par la méthode de Kaplan-Meier pour les affections médicales limitant la carrière était de 40,9% (intervalle de confiance (IC) à 95% 35,5 à 46,4) chez les personnes souffrant de troubles mentaux liés au service en Afghanistan (TMSA), de 23,6% (IC à 95% 15,5 à 31,8) pour les autres troubles mentaux, et de 11,1% (IC à 95% 8,9 à 13,3) sans troubles mentaux. Les ratios ajustés du modèle de régression de Cox pour le risque d’affection médicale limitant la carrière étaient de 4,89 (IC à 95% 3,85 à 6,23) chez les personnes souffrant de TMSA et de 2,31 (IC à 95% 1,48 à 3,60) pour les autres troubles mentaux, relativement à ceux sans troubles mentaux.
Conclusions:
Indépendamment des investissements dans le système de santé mentale militaire canadien, les troubles mentaux (particulièrement les TMSA) entraînaient toujours un risque élevé de résultats professionnels militaires indésirables. Ces investissements ont une valeur intrinsèque, mais ne se traduiront pas par une attrition médicale réduite sans améliorer l’efficacité de la prévention et du traitement.
Clinical Implications
Diagnosed mental disorders, particularly Afghanistan service–related ones, among Canadian Armed Forces personnel who deployed in support of the mission in Afghanistan were associated with the development of military occupation restrictions.
Improvements in prevention and treatment are needed to reduce the risk of medically related attrition among those with service-related mental disorders.
Limitations
Our results are rooted in the totality of the Canadian Armed Forces context and not directly generalizable to other organizations.
Medical problems other than mental disorders were not assessed, precluding a comparison of the relative contribution of mental disorder to health-related disability in the cohort.
Over the past decade, millions of military personnel have deployed to Southwest Asia. Psychiatric injury rates during this conflict have been high: in Canada, 13.5% of personnel deployed in support of the mission in Afghanistan were diagnosed with a service-related mental disorder within 4 years after their return.1 For those in high-threat locations, estimated rates approached 30% after 7 years.1
Military organizations have stringent fitness standards, reflecting the demanding and unpredictable nature of military work. When mental disorders or other medical conditions result in dysfunction that persistently restricts military duties, this can lead to a release from service for medical reasons. This medically related attrition results in loss of expertise and the potential need for veterans’ benefits and services.
Research has demonstrated that mental health problems have an impact on military occupational fitness.2–16 Large associations have been seen using different markers for mental health problems (e.g., questionnaires,4,10–12 outpatient care,2,3,6,8 fitness evaluations,5,7,9,14 hospitalization,13,15 and family history14) and a range of outcomes (e.g., attrition,2–4,6,8,10,12,13,15 medical release,5,7,9 and lack of occupational fitness11,14). Associations have been noted by studies from different military organizations (British Armed Forces,4,11,15 Australian Navy,10 and the US military2,3,5–9,12,13), among different service branches (Marines,2,3,5,6,8,12 Army,2,4,7–9,11–13,15 Navy,2,4,8,10,11 and Air Force2,4,8,11), in recruits,14 and after combat deployment.10,12,16,17
An important gap of past work in this area is that most studies emanate from the US military.2,3,5–9,12,13 Other military organizations may see different results because of differences in barriers to care, treatment, rehabilitation, and accommodation practices for those with disabilities.
In response to deficiencies identified in the 1990s, the Canadian Armed Forces (CAF) has invested heavily in their mental health system over the past 15 years. The number of mental health providers has increased. Seven multidisciplinary centers provide standardized assessment and treatment of service-related mental health problems. Lower levels of stigma and other barriers to care have been seen compared with other military organizations,18 perhaps a result of destigmatization efforts.19 Extensive resilience and mental health training is embedded throughout individuals’ careers and across the deployment cycle; in-depth postdeployment mental health screening is also required.20,21 Finally, the CAF has refined their approach to medical employment limitations (MELs), ensuring retention of individuals who respond to treatment and can safely deploy.
Past work exploring the impact of mental disorders on military occupational fitness has had some limitations, including the use of psychiatric hospitalizations as the index event,13,15 the use of administrative encounter data alone to establish mental disorder diagnoses,2,3,6,8 the use of brief follow-up periods,12,13 and the failure to use a time-to-event analysis approach to fully account for differential follow-up. Finally, no studies directly distinguished between the occupational impact of service-related and non–service-related mental disorders.
This study addresses the identified limitations and explores the long-term military occupational impact of service-related mental disorders among a large cohort of Canadian military personnel who deployed in support of its mission in Afghanistan.
Methods
Study Population and Sampling
This study used a weighted, stratified random sample of 2045 individuals from a retrospective cohort of CAF personnel (N = 30,513) who initiated a deployment outside of North America or Europe in support of the mission in Afghanistan from October 1, 2001, through December 31, 2008. The medical records of 2014 individuals in the sample were available for review. The sampling strata were defined by deployment location (6 categories) and apparent mental health services use (2 categories).1 The deployment locations (a proxy for deployment experiences) were Kandahar Province, Kabul or elsewhere in Afghanistan, the United Arab Emirates or elsewhere in the Middle East, the Arabian Gulf (on board ship), multiple locations, and an Afghanistan-related deployment of unspecified location. We determined individuals’ apparent use of mental health services using administrative data and preferentially weighted apparent users, those most likely to have had a mental disorder diagnosed.
Data Collection
As discussed in detail elsewhere,1 data on deployments were extracted from administrative databases; mental disorder diagnoses and any clinician-identified attribution to the Afghanistan or other missions were abstracted from the medical records over the period from June 22, 2010, to May 30, 2011. Although there is no standard CAF protocol for determining whether a diagnosed disorder is service related, it is standard practice for CAF clinicians to make such a judgment and to include it in their assessments. Data on military occupational fitness were extracted from administrative databases (data extract date: November 14, 2012). This was supplemented with data from systems that were enhanced in 2009 to capture primary and secondary diagnoses that contributed to individual’s MEL assessment (data extract date: January 15, 2013); this was not available for individuals assessed prior to 2009.
Military Occupational Fitness in the CAF
Military personnel in the CAF have an occupational fitness requirement, one that takes into consideration the potential duties required under the demanding and unpredictable conditions of operational deployments. This requirement is enshrined in the principle of “Universality of Service,” which the CAF enforces by requiring all personnel to be able to perform certain common military tasks and to be deployable to any environment with little medical support.22 Individuals who are persistently in violation of Universality of Service will be released from service.
When CAF personnel are diagnosed with a medical condition, their clinician determines whether the diagnosis or treatment may interfere with duties. This assessment is a sequential process; it begins with a thorough examination, followed by a comprehensive description of MELs. Clinicians assign a set of codes (“medical categories”) that summarize the MEL’s impact on duties. Persistent MELs and medical categories are validated by physicians in the Medical Standards Section of the CAF, ensuring a standardized application.
Whereas some persistent MELs will ultimately lead to a release from military service, others will be accommodated. Individuals whose validated MELs are likely to violate Universality of Service undergo an administrative review; those determined to be in violation will ultimately be released.
The medical category coding system captures the impact of MELs using 6 factors: visual acuity, colour vision, hearing, a geographical factor, an occupational factor, and an air factor for pilots.23 For mental disorders, the geographical and occupational factor codes drive retention decisions. The geographical factor captures an individual’s need for specialized medical care that might be unavailable at potential work locations (e.g., during deployment). The occupational factor captures an individual’s capacity to perform required job functions under the physical and mental stress associated with operational conditions. The codes for the geographical and occupational factors can range from 1 to 6; higher grades represent more severe limitations. Assigned medical categories may be temporary or persistent, reflecting clinicians’ judgment of prognosis in 18 to 24 months.
Outcome Definition
The primary outcome was defined as the development of a career-limiting medical condition, meaning MELs that reliably lead to a medical release from service. We chose this outcome instead of medical release because there is an unpredictable delay of up to several years between the recognition of a career-limiting medical condition and ultimate discharge. This delay is intended to foster a successful transition to civilian life, and its duration depends on administrative processes and service member preferences as opposed to the underlying illness or disability.
Consultations with physicians in the Medical Standards Section identified geographical and occupational factor coding that reliably leads to Universality of Service being violated in those with medical conditions. Individuals with a persistent grade 4 or worse in the geographical or occupational factors were considered to have career-limiting medical conditions. Those with a geographical grade of 3 or less (a need for specialist care no more frequent than every 6 months) and with occupational grades of 2 or less (no interference with duties) were considered occupationally fit.
Those with an acceptable geographical factor but an occupational factor grade of 3 may be determined unfit, depending on the specific nature of the underlying MELs. Such cases were judged fit or unfit based on the outcome of the administrative review of their MELs.
Covariate of Interest and Potential Confounders
The primary covariate of interest was the presence of a mental disorder diagnosis, which was categorized into disorders that were related to Afghanistan service, other mental disorders (including past disorders), or none. Individuals with diagnoses related to other CAF operations (n = 30, unweighted) were grouped for analytical purposes with individuals who had mental disorders that were not service related.
Mental disorder diagnoses that were captured included posttraumatic stress disorder (PTSD), other anxiety disorders, depressive disorders, bipolar disorder, other mood disorders, adjustment disorder, somatoform disorder, and substance-related disorders.
Sex, age, service (Army, Navy, or Air Forces), component (regular compared with reserve force), rank, as well as total deployment number and duration were considered potential confounders, based on conceptual considerations and other work.1–15 Age, rank, and component were determined with respect to the start date of individuals’ first Afghanistan-related deployment.
Data Analysis
The data were analyzed using SAS for Windows, version 9.3 (SAS Institute Inc., Cary, NC). The Taylor Series Linearization method24 was used with sample design weights to determine 95% confidence intervals (CIs) for the descriptive statistics and Cox regression. There were no missing values in the analyzed variables for the 2014 individuals whose medical charts were reviewed.
Weighted Kaplan-Meier curves25 were used to generate event probabilities. Zero-time was defined as the return date from the first Afghanistan-related deployment. Event-time was the date of the medical examination associated with the first persistent career-limiting medical condition. Individuals were censored at the earlier of military release date or database extraction date. Ninety-five percent CIs for Kaplan-Meier event-time estimates were generated using bootstrap methods.26
Weighted Cox regression assessed the association of a career-limiting medical condition with covariates. The mental disorder diagnosis variable was forced into a model that included potential confounders selected using Akaike’s Information Criterion with a forward selection process.25 Results are expressed as hazard ratios (HRs). Regression diagnostic plots were reviewed with respect to the proportional hazards assumption.25
Ethical Aspects
The research protocol was approved by Veritas Research Ethics Board (Dorval, Quebec, Canada).
Results
Study Cohort Characteristics
Table 1 summarizes the information for individuals whose charts were reviewed (n = 2014). The cohort was determined to consist largely of male, noncommissioned, Army personnel under the age of 40 years who were in the Regular Forces. The number of individuals with inaccessible medical charts was small (n = 31).
Table 1.
Estimated Mental Disorder Diagnosis and Demographic and Military Characteristics for the Study Cohort of Canadian Armed Forces Personnel Who Deployed in Support of the Afghanistan Mission During 2001 to 2008.
| Characteristic | Medical Charts Reviewed (n = 2014) | |||
|---|---|---|---|---|
| Sample No. | Weighted % | 95% CI | ||
| Mental disorder diagnosis | ||||
| ARMD | 415 | 13.5 | 12.1 to 14.8 | |
| Othera | 136 | 5.5 | 4.5 to 6.6 | |
| None identified | 1463 | 81.0 | 79.4 to 82.6 | |
| Sex | ||||
| Male | 1772 | 90.5 | 89.1 to 92.0 | |
| Female | 242 | 9.5 | 8.0 to 10.9 | |
| Age (years) | ||||
| <30 | 748 | 37.3 | 34.7 to 40.0 | |
| 30–39 | 803 | 39.4 | 36.7 to 42.0 | |
| ≥40 | 463 | 23.3 | 21.0 to 25.6 | |
| Component | ||||
| Regular Forces | 1870 | 91.2 | 89.7 to 92.7 | |
| Reserve Forces | 144 | 8.8 | 7.3 to 10.3 | |
| Service | ||||
| Army | 1419 | 63.2 | 61.2 to 65.2 | |
| Navy | 223 | 17.0 | 15.3 to 18.6 | |
| Air Force | 372 | 19.9 | 17.8 to 22.0 | |
| Rank | ||||
| Officer | 308 | 15.9 | 13.8 to 17.9 | |
| Senior NCM | 369 | 18.0 | 16.0 to 19.9 | |
| Junior NCM | 1337 | 66.2 | 63.7 to 68.7 | |
| Deployment location | ||||
| Kandahar Province | 865 | 41.8 | 41.6 to 42.1 | |
| Kabul or elsewhere in Afghanistan | 320 | 13.6 | 13.2 to 13.7 | |
| UAE or elsewhere in Middle East | 119 | 10.2 | 10.2 to 10.4 | |
| Arabian Gulf | 148 | 17.2 | 17.2 to 17.6 | |
| Multiple | 413 | 15.1 | 14.9 to 15.4 | |
| Unspecified | 149 | 1.9 | 1.8 to 1.9 | |
| Number of Afghanistan deployments | ||||
| 1 | 1523 | 79.6 | 78.1 to 81.2 | |
| 2 | 389 | 16.1 | 14.5 to 17.7 | |
| ≥3 | 102 | 4.3 | 3.4 to 5.1 | |
| Duration of first Afghanistan deployment | ||||
| <180 days | 1136 | 56.6 | 54.3 to 58.9 | |
| ≥180 days | 878 | 43.4 | 41.1 to 45.7 | |
| Total duration of Afghanistan deployments | ||||
| <180 days | 850 | 45.1 | 42.7 to 47.5 | |
| ≥180 days | 1164 | 54.9 | 52.5 to 57.3 | |
Abbreviations: ARMD, Afghanistan service-related mental disorders; CAF, Canadian Armed Forces; CI, confidence interval; NCM, noncommissioned members; UAE, United Arab Emirates.
a The “other” mental disorder diagnosis grouping includes individuals with mental disorder diagnoses related to CAF operations other than the mission in Afghanistan and individuals who had non–deployment-related mental disorder diagnoses.
Overall, 29.6% (95% CI 27.7 to 31.6) of the study population ever initiated an encounter with CAF specialty mental health services as of the chart review date. An estimated 19.0% (95% CI 17.4 to 20.6) of the cohort had a mental disorder diagnosis over a median follow-up period of almost 4 years (1364 days); 13.5% (95% CI 12.1 to 14.8) had an Afghanistan service–related mental disorder (ARMD). PTSD was the most common ARMD, diagnosed in 8.0% (95% CI 7.0 to 9.0) of the population; 5.5% (95% CI 4.5 to 6.5) had other ARMD. An additional 1.2% (95% CI 0.7 to 1.7) had a mental disorder diagnosis related to other CAF operations. Finally, 4.3% (95% CI 3.4 to 5.3) were diagnosed with a mental disorder unrelated to any operation.
Career-Limiting Medical Conditions
As shown in Table 2, 18.6% (95% CI 16.6 to 20.5) of the study population developed a career-limiting medical condition over a median postdeployment follow-up of 1833 days (mean 1956 days; range 4 to 4048 days). CAF personnel with ARMD and those with other mental disorders were more likely to develop a career-limiting medical condition than were personnel without mental disorders; Kaplan-Meier estimates indicated that at 5 years of follow-up, the cumulative fractions with a career-limiting medical condition were 40.9% (95% CI 35.5 to 46.4) and 23.6% (95% CI 15.5 to 31.8), respectively, relative to 11.1% (95% CI 8.9 to 13.3) among those without mental disorders.
Table 2.
Estimated Percentage With Career-Limiting Medical Conditions, by Mental Disorder Diagnosis Category, Demographic and Military Characteristics in the Study Cohort of CAF Personnel Who Deployed in Support of the Afghanistan Mission During 2001 to 2008.
| Characteristic | Career-Limiting Medical Conditions | |||
|---|---|---|---|---|
| Sample No. | Weighted % | 95% CI | ||
| Mental disorder diagnosis | ||||
| ARMD | 211 | 47.7 | 42.3 to 53.1 | |
| Othera | 53 | 33.3 | 24.1 to 42.6 | |
| None identified | 220 | 12.7 | 10.6 to 14.8 | |
| Total | 484 | 18.6 | 16.6 to 20.5 | |
| Sex | ||||
| Male | 409 | 17.7 | 15.7 to 19.7 | |
| Female | 75 | 26.7 | 19.9 to 33.5 | |
| Age | ||||
| <30 | 135 | 12.8 | 10.4 to 15.3 | |
| 30–39 | 217 | 20.6 | 17.3 to 23.8 | |
| ≥40 | 132 | 24.4 | 19.6 to 29.2 | |
| Component | ||||
| Regular Forces | 468 | 19.4 | 17.4 to 21.5 | |
| Reserve Forces | 16 | 9.4 | 4.5 to 14.4 | |
| Service | ||||
| Army | 355 | 18.4 | 16.4 to 20.5 | |
| Navy | 56 | 20.8 | 14.6 to 27.0 | |
| Air Force | 73 | 17.1 | 12.2 to 21.9 | |
| Rank | ||||
| Officer | 43 | 12.4 | 7.6 to 17.3 | |
| Senior NCM | 99 | 21.0 | 16.6 to 25.3 | |
| Junior NCM | 342 | 19.4 | 16.9 to 21.8 | |
| Deployment location | ||||
| Kandahar Province | 169 | 15.2 | 12.8 to 17.5 | |
| Kabul or Elsewhere in Afghanistan | 109 | 27.2 | 22.2 to 32.2 | |
| UAE or Elsewhere in Middle East | 19 | 15.5 | 8.0 to 23.0 | |
| Arabian Gulf | 35 | 20.3 | 13.5 to 27.0 | |
| Multiple | 106 | 19.4 | 15.9 to 22.9 | |
| Unspecified | 46 | 25.6 | 18.8 to 32.4 | |
| Number of Afghanistan deployments | ||||
| 1 | 369 | 19.0 | 16.8 to 21.3 | |
| 2 | 97 | 17.9 | 14.1 to 21.7 | |
| ≥3 | 18 | 12.3 | 6.3 to 18.3 | |
| Duration of first Afghanistan deployment | ||||
| <180 days | 308 | 20.8 | 18.0 to 23.7 | |
| ≥180 days | 176 | 15.6 | 13.1 to 18.1 | |
| Total duration of Afghanistan deployments | ||||
| <180 days | 239 | 21.9 | 18.5 to 25.4 | |
| ≥180 days | 245 | 15.8 | 13.6 to 17.9 | |
Abbreviations: ARMD, Afghanistan service-related mental disorders; CAF, Canadian Armed Forces; CI, confidence interval; NCM, noncommissioned members; UAE, United Arab Emirates.
a The “other” mental disorder diagnosis grouping includes individuals with mental disorder diagnoses related to CAF operations other than the mission in Afghanistan and individuals who had non–deployment-related mental disorder diagnoses.
For the subset of the sample whose career-limiting medical condition assessment was in 2009 or later and thus had an available diagnostic attribution (n = 211 of 484 with a career-limiting medical condition, unweighted), the primary contributing medical diagnoses were predominantly either a mental disorder (48%) or a musculoskeletal problem (33%). Mental disorders contributed especially heavily to career-limiting medical conditions in those with ARMD, for whom the primary and secondary contributor was a mental disorder in 77% and 7%, respectively.
Referring to all individuals identified with a career-limiting medical condition, it was estimated that almost one-half (45%) of all such designations in the cohort occurred in the minority of the population with an ARMD (35%) or other mental disorder diagnoses (10%). This is an overrepresentation as only 19% of individuals in the cohort had a diagnosed mental disorder.
Kaplan-Meier curves (Figure 1) demonstrated that those with ARMDs had the highest probability and those without mental disorders the lowest probability of developing a career-limiting medical condition. The probability for individuals with other mental disorders was intermediate. After a decade of follow-up, the predicted probability of a career-limiting medical condition was 68.8% (95% CI 59.9 to 77.8) among those with an ARMD, and there was no indication of the cumulative incidence curve leveling off after 10 years of follow-up.
Figure 1.
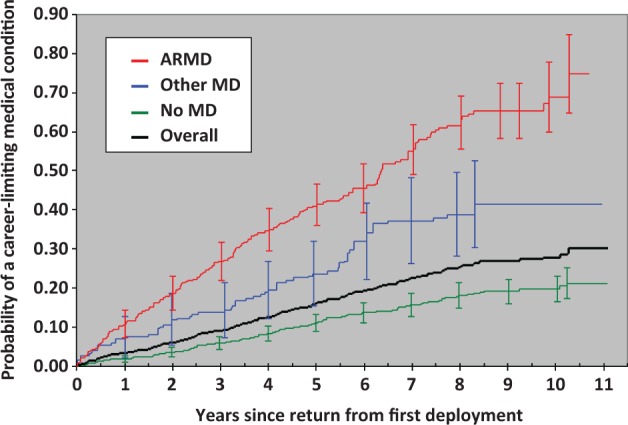
Kaplan-Meier estimates of the probability of a career-limiting medical condition by mental disorder diagnosis category in the study cohort of Canadian Armed Forces (CAF) personnel who deployed in support the Afghanistan mission during 2001 to 2008. Error bars represent 95% confidence intervals for representative points on the curve. The other mental disorder diagnosis grouping includes individuals with mental disorder diagnoses related to CAF operations other than the mission in Afghanistan, who had non–deployment-related mental disorders, or who had a prior mental disorder diagnosis. ARMD, Afghanistan-related mental disorders.
Cox Proportional Hazards Regression
Cox regression (Table 3) showed that individuals with an ARMD were associated with a markedly increased risk of a career-limiting medical condition (HR 4.89; 95% CI 3.85 to 6.23) relative to those without a mental disorder diagnosis; those with other mental disorders also had an elevated risk (HR 2.31; 95% CI 1.48 to 3.60). Groups at higher risk for a career-limiting medical condition included junior noncommissioned members, women, older individuals, individuals with fewer Afghanistan deployments, and individuals with Afghanistan deployments of less than 180 days’ duration.
Table 3.
Association of Mental Disorder Diagnosis Category and Demographic and Military Characteristics With Adverse Occupational Outcome (i.e., Career-Limiting Medical Condition) in the Study Cohort of CAF Personnel Who Deployed in Support of the Afghanistan Mission During 2001 to 2008.
| Characteristic | Unadjusted HR | 95% CI | Adjusted HR from selected model | 95% CI | |
|---|---|---|---|---|---|
| Mental disorder diagnosis | |||||
| ARMD | 4.81 | 3.77 to 6.13 | 4.89 | 3.85 to 6.23 | |
| Othera | 2.47 | 1.64 to 3.72 | 2.31 | 1.48 to 3.60 | |
| None identified | 1.00 | Referent | 1.00 | Referent | |
| Sex | |||||
| Male | 1.00 | Referent | 1.00 | Referent | |
| Female | 1.59 | 1.14 to 2.22 | 1.46 | 1.04 to 2.07 | |
| Age | |||||
| <30 | 1.00 | Referent | 1.00 | Referent | |
| 30–39 | 1.39 | 1.05 to 1.85 | 1.50 | 1.11 to 2.04 | |
| ≥40 | 2.21 | 1.61 to 3.04 | 2.92 | 1.97 to 4.34 | |
| Component | |||||
| Regular Forces | 1.00 | Referent | 1.00 | Referent | |
| Reserve Forces | 0.62 | 0.35 to 1.12 | 0.63 | 0.36 to 1.10 | |
| Service | |||||
| Army | 1.00 | Referent | — | — | |
| Navy | 0.85 | 0.59 to 1.23 | — | — | |
| Air Force | 0.84 | 0.59 to 1.19 | — | — | |
| Rank | |||||
| Officer | 1.00 | Referent | 1.00 | Referent | |
| Senior NCM | 1.89 | 1.16 to 3.08 | 1.49 | 0.92 to 2.41 | |
| Junior NCM | 1.56 | 0.99 to 2.44 | 1.95 | 1.19 to 3.21 | |
| Deployment location | |||||
| Kandahar Province | 1.00 | Referent | 1.00 | Referent | |
| Kabul or Elsewhere in Afghanistan | 1.26 | 0.94 to 1.69 | 1.12 | 0.83 to 1.53 | |
| UAE or Elsewhere in Middle East | 0.78 | 0.44 to 1.39 | 0.80 | 0.44 to 1.43 | |
| Arabian Gulf | 0.83 | 0.53 to 1.30 | 0.67 | 0.42 to 1.10 | |
| Multiple | 0.76 | 0.57 to 1.01 | 1.36 | 0.81 to 2.28 | |
| Unspecified | 1.44 | 0.99 to 2.10 | 1.16 | 0.77 to 1.74 | |
| Number of Afghanistan deployments | |||||
| 1 | 1.00 | Referent | 1.00 | Referent | |
| 2 | 0.65 | 0.49 to 0.87 | 0.56 | 0.33 to 0.96 | |
| ≥3 | 0.39 | 0.22 to 0.68 | 0.35 | 0.18 to 0.69 | |
| Duration of first Afghanistan deployment | |||||
| <180 days | 1.00 | Referent | — | — | |
| ≥180 days | 0.91 | 0.71 to 1.16 | — | — | |
| Total duration of Afghanistan deployments | |||||
| <180 days | 1.00 | Referent | 1.00 | Referent | |
| ≥180 days | 0.70 | 0.55 to 0.89 | 0.73 | 0.56 to 0.95 | |
Abbreviations: ARMD, Afghanistan service-related mental disorders; CAF, Canadian Armed Forces; CI, confidence interval; HR, hazard ratio; NCM, noncommissioned members; UAE, United Arab Emirates.
a The “other” mental disorder diagnosis grouping includes individuals with mental disorder diagnoses related to CAF operations other than the mission in Afghanistan and individuals who had non–deployment-related mental disorder diagnoses.
Discussion
Key Findings
ARMDs were associated with a high career-limiting medical condition designation risk. A decade after deployment, almost 70% of cohort members with ARMD are expected to have such career limitations, and the Kaplan-Meier estimates suggests no leveling off of risk over at least 10 years of follow-up. Those with ARMD had a 5-fold higher independent risk of a career-limiting medical condition relative to those without mental disorders.
Comparison With Other Findings
Our finding that mental health problems contribute strongly to adverse military occupational outcomes is consistent with other work in this field. For example, 29% of medical retirements in US Army personnel were attributed to mental disorders, largely PTSD.16 We noted that almost half (45%) of career-limiting medical conditions in our data occurred in the minority with mental disorder diagnoses. Attrition among US military personnel reporting postdeployment mental health concerns was as high as 23% only 1 year after deployment.12 Among US Army personnel with hospitalizations, the 6-month attrition rate was 45% for mental disorder hospitalizations compared with 11% for hospitalizations due to other illnesses.13 Self-reported concerns and mental disorder hospitalizations represent more inclusive and exclusive populations, respectively, relative to diagnoses in our cohort. Multiple methodological differences unfortunately preclude any direct comparison of our findings with those of others; however, we, and others, have demonstrated a significant impact of mental disorders on military occupational fitness.
We are not familiar with any comparable work looking directly at the impact of service-related versus other mental disorders on military occupational fitness. However, others have noted indirect evidence of this,10,12,16,17 consistent with our more direct finding.
Our findings on other risk factors for impaired military occupational fitness largely mirror those from other studies. For example, others have noted a higher risk of adverse military occupational outcomes in female personnel5,6,9,27 and in noncommissioned personnel.4,9,11,27,28 Most others have noted a higher risk in younger personnel,4,9,11,27 whereas we found a higher risk in older individuals. In contrast to others,4,11,28 we did not find that Army service was an independent risk factor. We could not locate other work touching directly on the influence of deployment-related factors (such as number of deployments and duration). Further work is needed to investigate the mechanisms that lead to these additional independent associations with occupational fitness.
Limitations
The study’s primary limitation is that its findings are largely rooted in the totality of the CAF context (i.e., their deployment experiences, mental health system, and medical standards). Hence, it is difficult to generalize these findings directly to other organizations.
In addition, it is possible that some individuals received a mental disorder diagnosis after the medical chart review period and before outcome data were extracted, an 18-month window, whereas others may have had an undiagnosed mental disorder, possibly less severe, that resolved prior to their later health assessment when MELs were assessed; these individuals would be misclassified as having no diagnoses. Although the number of such cases is expected to be small, these misclassifications likely operate in opposite directions: the former adding individuals with a greater probability of having the outcome and the latter adding individuals with a lower probability of having the outcome in the no mental disorder category.
Errors in clinician attribution of the disorder to military service are possible, as there is no validation of the CAF’s approach.
We did not assess other medical problems, so we cannot place the impact of mental disorders within the larger context of health-related disability. Nevertheless, most career-limiting medical conditions in the ARMD group were attributed to a mental disorder, and nearly half of all career-limiting designations were in the minority of the population with a mental disorder diagnosis. This reinforces the important role of mental disorders as a driver of military occupational fitness problems in the CAF.
Implications
ARMD have had a significant impact on military occupational fitness among CAF personnel who deployed in support of that mission. The absolute magnitude of the impact could place pressure on readiness and force sustainability, a reality that needs to be reflected in casualty estimates, human resource planning, and medical services resourcing. The often lengthy period from deployment return to career-limiting designation suggests that the impact will be felt for years after the mission ends.
The military occupational outcome that results after a mental disorder diagnosis depends on many factors, including the natural history of the underlying condition, the efficacy of available care, the effectiveness with which care is applied, and the stringency of occupational standards. Our findings reflect the net effect of these factors.
On a conceptual basis, stringent occupational standards are an important driver of our findings: application of the CAF’s Universality of Service concept means that some individuals who are in complete remission may be deemed unfit if there is a significant risk of serious relapse with reexposure to occupational trauma. Intrinsic technical limitations of existing care must also contribute substantially: even under the optimal circumstances of clinical trials, the risk difference between the most widely used evidence-based psychotherapies and inactive controls for loss of a PTSD diagnosis varies from 0.44 for cognitive processing therapy to 0.66 for prolonged exposure.29 Data on outcomes in real-world settings are sparse but ultimately discouraging: in the US Army, for example, only 20% of those diagnosed with PTSD achieve remission in treatment.30 Although the CAF has a comprehensive, well-resourced mental health system, research elsewhere has consistently demonstrated significant opportunities for quality improvement in mental health care.31 However, verification of treatment effectiveness and quality of care was beyond the scope of the present study.
Options for seeing lesser impacts are constrained. Getting individuals into care sooner will improve their quality of life, but the effect on military occupational outcomes is uncertain; better treatments for traumatic stress disorders are clearly needed. Relaxing military medical fitness standards is possible but could have deleterious effects on readiness, operational effectiveness, and health outcomes.
This leaves only 1 realistic opportunity to see better military occupational outcomes among those with mental disorders over the near term: ensure that the best available treatments are optimally applied. Hence, systematic assessment of the process and outcomes of care in the CAF and other military organizations is a priority. However, at present, military and veteran organizations can only foster a process to promote a successful transition to civilian life.
The results of this study may be misconstrued in ways that could negatively influence care-seeking behaviors, possibly effecting a barrier among those with service-related mental disorders given that concerns about the career impact of care seeking are prevalent. Thoughts of a military career ending due to a medical condition could be catastrophized, compounding care avoidance.32–34 In addition, some may conclude that care is ineffective and avoid it.32,35,36
The above considerations highlight research priorities for service-related mental disorders. Research on prevention and better treatments are clearly needed, given that once disorders occur, complete recovery without military career impacts cannot be guaranteed. An assessment of the congruence of care delivery against best practices is a critical initial step in quality improvement, as is the assessment of outcomes. The assessment of how those with a career-limiting medical condition are functioning when and after they transition to civilian life could lead to interventions that promote improved transition outcomes. Finally, it is essential to enhance interventions to reduce barriers to care.32
Conclusion
The substantial impact of service-related mental disorders on military occupational fitness in the CAF reflects the reality of what happens when serious, unpreventable illnesses with imperfect treatments collide with stringent occupational fitness standards. In the face of these constraints, a well-resourced mental health system in a forward-thinking organization can go only so far. Investment in a stronger military mental health system37 has intrinsic value, but this, in isolation, may not translate into dramatically lower rates of medically related attrition without advancing our understanding of the illness and developing more effective prevention and treatments. In the meantime, efforts to ensure that existing treatments are optimally applied are a priority.
Acknowledgements
We thank Julie Lanouette and Suzanne Giroux for their assistance with the data collection from patient medical records.
Authors’ Note: Both authors are employees of the Canadian Department of National Defence, and funding for this research came via this department. No other disclosures reported.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by funding from the Canadian Armed Forces Surgeon General’s Medical Research Program.
References
- 1. Boulos D, Zamorski MA. Deployment-related mental disorders among Canadian Forces personnel deployed in support of the mission in Afghanistan, 2001-2008. CMAJ. 2013;185:E545–E552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ireland RR, Kress AM, Frost LZ. Association between mental health conditions diagnosed during initial eligibility for military health care benefits and subsequent deployment, attrition, and death by suicide among active duty service members. Mil Med. 2012;177:1149–1156. [DOI] [PubMed] [Google Scholar]
- 3. Schmied EA, Highfill-McRoy RM, Larson GE. Mental health and turnover following an initial term of military service. Mil Med. 2012;177:766–772. [DOI] [PubMed] [Google Scholar]
- 4. Buckman JE, Forbes HJ, Clayton T, et al. Early service leavers: a study of the factors associated with premature separation from the UK Armed Forces and the mental health of those that leave early. Eur J Public Health. 2013;23:410–415. [DOI] [PubMed] [Google Scholar]
- 5. Sikorski C, Emerson MA, Cowan DN, et al. Risk factors for medical disability in U.S. enlisted Marines: fiscal years 2001 to 2009. Mil Med. 2012;177:128–134. [DOI] [PubMed] [Google Scholar]
- 6. Crain JA, Larson GE, Highfill-McRoy RM, et al. Postcombat outcomes among Marines with preexisting mental diagnoses. J Trauma Stress. 2011;24:671–679. [DOI] [PubMed] [Google Scholar]
- 7. Niebuhr DW, Krampf RL, Mayo JA, et al. Risk factors for disability retirement among healthy adults joining the U.S. Army. Mil Med. 2011;176:170–175. [DOI] [PubMed] [Google Scholar]
- 8. Garvey Wilson AL, Messer SC, Hoge CW. U.S. military mental health care utilization and attrition prior to the wars in Iraq and Afghanistan. Soc Psychiatry Psychiatr Epidemiol. 2009;44:473–481. [DOI] [PubMed] [Google Scholar]
- 9. Bell NS, Schwartz CE, Harford TC, et al. Temporal changes in the nature of disability: U.S. Army soldiers discharged with disability, 1981-2005. Disabil Health J. 2008;1:163–171. [DOI] [PubMed] [Google Scholar]
- 10. Creamer M, Carboon I, Forbes AB, et al. Psychiatric disorder and separation from military service: a 10-year retrospective study. Am J Psychiatry. 2006;163:733–734. [DOI] [PubMed] [Google Scholar]
- 11. Rona RJ, Hooper R, Greenberg N, et al. Medical downgrading, self-perception of health, and psychological symptoms in the British Armed Forces. Occup Environ Med. 2006;63:250–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hoge CW, Auchterlonie JL, Milliken CS. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295:1023–1032. [DOI] [PubMed] [Google Scholar]
- 13. Hoge CW, Toboni HE, Messer SC, et al. The occupational burden of mental disorders in the U.S. military: psychiatric hospitalizations, involuntary separations, and disability. Am J Psychiatry. 2005;162:585–591. [DOI] [PubMed] [Google Scholar]
- 14. Cigrang JA, Carbone EG, Todd S, et al. Mental health attrition from Air Force basic military training. Mil Med. 1998;163:834–838. [PubMed] [Google Scholar]
- 15. Jones N, Fear NT, Greenberg N, et al. Occupational outcomes in soldiers hospitalized with mental health problems. Occup Med (Lond). 2009;59:459–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Patzkowski JC, Rivera JC, Ficke JR, et al. The changing face of disability in the US Army: the Operation Enduring Freedom and Operation Iraqi Freedom effect. J Am Acad Orthop Surg. 2012;20(Suppl 1):S23–S30. [DOI] [PubMed] [Google Scholar]
- 17. Bell NS, Hunt PR, Harford TC, et al. Deployment to a combat zone and other risk factors for mental health-related disability discharge from the U.S. Army: 1994-2007. J Trauma Stress. 2011;24:34–43. [DOI] [PubMed] [Google Scholar]
- 18. Gould M, Adler A, Zamorski M, et al. Do stigma and other perceived barriers to mental health care differ across Armed Forces? J R Soc Med. 2010;103:148–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Department of National Defence. Operational stress injury social support program website [cited 13 Jan 2015]. Available from: http://www.osiss.ca.
- 20. Canadian Armed Forces. Road to Mental Readiness (R2MR) program [cited 12 Sep 2014]. Available from: http://www.forces.gc.ca/en/caf-community-health-services-r2mr/indexpage.
- 21. Garber BG, Zamorski MA. Evaluation of a third-location decompression program for Canadian Forces members returning from Afghanistan. Mil Med. 2012;177:397–403. [DOI] [PubMed] [Google Scholar]
- 22. Department of National Defence. Fit to serve: universality of service and related support programs [cited 5 Dec 2013]. Available from: http://adpna.com/files/DND_universsality_of_service.pdf.
- 23. Department of National Defence. Medical standards for military occupations [cited 12 Dec 2014]. Available from: http://www.forces.gc.ca/en/about-policies-standards-medical-occupations/indexpage.
- 24. Wolter KM. Introduction to variance estimation. New York (NY): Springer-Verlag; 1985. [Google Scholar]
- 25. Klein JP, Moeschberger ML. Survival analysis: Techniques for censored and truncated data. New York (NY: ): Springer-Verlag; 1997. [Google Scholar]
- 26. Efron B. Censored data and the bootstrap. J Am Stat Assoc. 1981;76:312–319. [Google Scholar]
- 27. Bell NS, Schwartz CE, Harford T, et al. The changing profile of disability in the U.S. Army: 1981-2005. Disabil Health J. 2008;1:14–24. [DOI] [PubMed] [Google Scholar]
- 28. Iversen A, Nikolaou V, Greenberg N, et al. What happens to British veterans when they leave the armed forces? Eur J Public Health. 2005;15:175–184. [DOI] [PubMed] [Google Scholar]
- 29. Jonas DE, Cusack K, Forneris CA, et al. Psychological and pharmacological treatments for adults with posttraumatic stress disorder (PTSD) Comparative Effectiveness Reviews Number 92 [cited 17 Dec 2013]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK137702/pdf/TOC.pdf. [PubMed]
- 30. U.S.Department of Defense. 2012 MHS Stakeholders Report. Available at: http://www.health.mil/Reference-Center/Reports/2012/12/31/2012-MHS-Stakeholders-Report Accessed 20 December 2013.
- 31. Institute of Medicine, Committee on Crossing the Quality Chasm. Adaptation to mental health and addictive disorders Improving the quality of health care for mental and substance-use conditions. Washington (DC): National Academy Press; 2006. [Google Scholar]
- 32. Sudom KA, Zamorski MA, Garber BG. Stigma and barriers to mental health care in deployed Canadian forces personnel. Mil Psychol. 2012;24:414–431. [Google Scholar]
- 33. Rona RJ, Jones M, French C, et al. Screening for physical and psychological illness in the British Armed Forces: I: the acceptability of the programme. J Med Screen. 2004;11:148–152. [DOI] [PubMed] [Google Scholar]
- 34. Sareen J, Cox BJ, Afifi TO, et al. Combat and peacekeeping operations in relation to prevalence of mental disorders and perceived need for mental health care: findings from a large representative sample of military personnel. Arch Gen Psychiatry. 2007;64:843–852. [DOI] [PubMed] [Google Scholar]
- 35. Hoge C, Castro C, Messer S, et al. Combat duty in Iraq and Afghanistan, mental health problems, and barriers to care. N Engl J Med. 2004;351:13–22. [DOI] [PubMed] [Google Scholar]
- 36. Iversen AC, van Staden L, Hughes JH, et al. The stigma of mental health problems and other barriers to care in the UK Armed Forces. BMC Health Serv Res. 2011;11:31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Interagency Task Force on Military and Veterans Mental Health. 2013. Interim report of the Interagency Task Force on Military and Veterans Mental Health [cited 21 Sep 2013]. Available from: http://www.whitehouse.gov/sites/default/files/uploads/2013_interim_report_of_the_interagency_task_force_on_military_and_veterans_mental_health.pdf.


