Abstract
The Victorian Adolescent Health Cohort Study (VAHCS) is a long-term Australian cohort study that has documented cannabis use in young Australians from the mid-teens to the mid-30s. The study findings have described the natural history of early cannabis use, remission, and escalation and the social and mental health consequences of different patterns of use. The adverse consequences of cannabis use are most clear-cut in heavy early adolescent users. These consequences include educational failure, persisting mental health problems, and progression to other substance use. For later onset and occasional users, the risks are lower and appear to entail modest elevations in risk for other drug use compared with never users. With growing evidence of health consequences, there is a strong case for actions around early heavy adolescent users. Prevention of early use, identification and treatment of early heavy users, and harm reduction through diversion of early heavy users away from the custodial justice system into health care are all priority responses.
Keywords: cannabis, Victorian Adolescent Health Cohort Study, adolescence
Abstract
L’étude de cohorte sur la santé des adolescents dans l’État de Victoria (VAHCS) est une étude de cohorte australienne à long terme qui a documenté l’utilisation du cannabis chez les jeunes australiens de la mi-adolescence à la mi-trentaine. Les résultats de l’étude ont décrit l’histoire naturelle de l’utilisation précoce du cannabis, la rémission et l’escalade, et les conséquences sociales et sur la santé mentale des différents modes d’utilisation. Les conséquences indésirables de l’utilisation du cannabis sont les plus évidentes chez les adolescents précoces grands consommateurs. Ce sont notamment l’échec scolaire, des problèmes de santé mentale persistants, et la progression vers l’utilisation d’autres substances. Pour les utilisateurs qui commencent plus tard ou qui sont occasionnels, les risques sont plus faibles et semblent être liés surtout à de modestes hausses du risque d’utiliser d’autres drogues, comparativement à ceux qui n’ont jamais été utilisateurs. Étant donné les données probantes qui s’accumulent sur les conséquences pour la santé, tout plaide en faveur d’agir pour les adolescents précoces grands consommateurs. La prévention de l’utilisation précoce, l’identification et le traitement des grands consommateurs précoces et la réduction des méfaits en soumettant les grands consommateurs précoces aux soins de santé plutôt qu’au système de justice privatif sont toutes des réponses prioritaires.
In 1925, the Geneva Convention ratified international drug control and included Indian hemp despite a lack of conclusive evidence then of harmful consequences. Seventy years later, there was still little reliable evidence about the health and social consequences of early cannabis use. Debate remained polarised between those who argued that adolescent cannabis use was a benign, transient practice with few social and health consequences in most young people1,2 and those who viewed cannabis as having the potential to lead to escalating drug use and other problems in social adjustment.3,4 The debate included whether a cannabis dependence syndrome existed. Tolerance to prolonged cannabis use had long been documented, but evidence on withdrawal was equivocal. A widespread, popular view of cannabis as a “soft drug” led to minimal public health and treatment responses.
Various reasons contributed to the lack of evidence concerning the consequences of cannabis use. Cannabis research faced many impediments. Drug treatment services rarely dealt with cannabis, and so clinical studies were few. The illicit status of cannabis allowed little scope for human-subject studies, other than anecdotal reports, and researchers were unable to unequivocally guarantee confidentiality in the collection of survey data. The lack of research could also be attributed in part to vocal “soft drug” proponents who did not see the necessity for rigorous research, relying instead on anecdotal evidence.
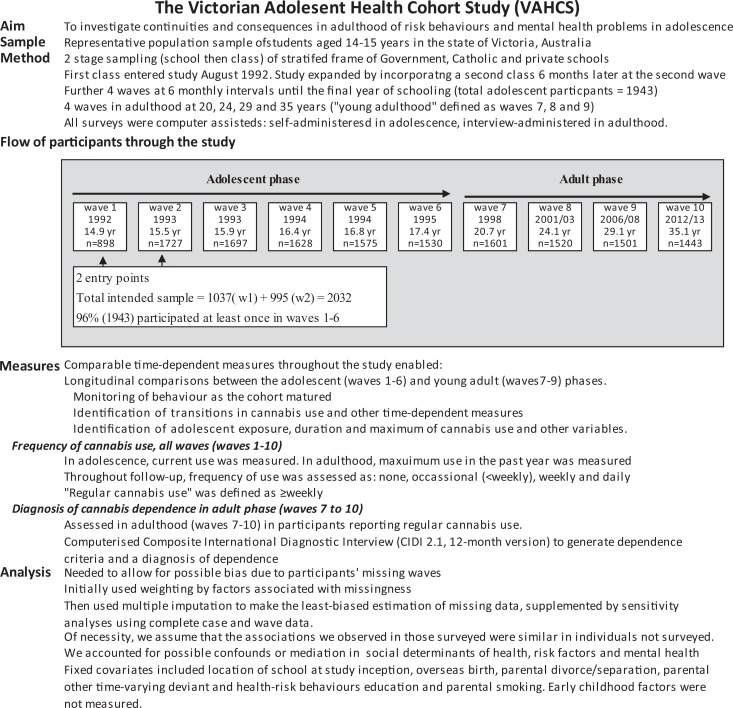
In this context, the Victorian Adolescent Health Cohort Study (VAHCS) was one of the first longitudinal studies to describe community patterns of cannabis use across adolescence and into adulthood. Previous observations had relied almost exclusively on cross-sectional and retrospective studies (e.g., Kandel in 19845). The methods of the VAHCS are described in Figure 1. The VAHCS was able to describe the following:
The natural history of cannabis use
Patterns and risks for escalation of cannabis use
Characterisation of the cannabis dependence syndrome
Consequences of adolescent cannabis use on other substance use, mental health, and social adjustment in young adulthood
Figure 1.
The Victorian Adolescent Cohort Study: design, measures and analytic strategies.
Natural History and Correlates of Adolescent Cannabis Use
It is well established that the initiation of cannabis use often occurs during adolescence, with heaviest use usually occurring during late adolescence and young adulthood.6 Two explanatory theories have been prominent. “Transition proneness” suggests that involvement in one problem behaviour increases the probability of involvement in others, including cannabis and other substance use, antisocial behaviours, and disregard for conventional norms such as school achievement and parental control.7 The “gateway theory” of substance use transition specifies that cigarette smoking and alcohol use by adolescents precede cannabis use, which then increases the risk of moving to other illicit substance use.8
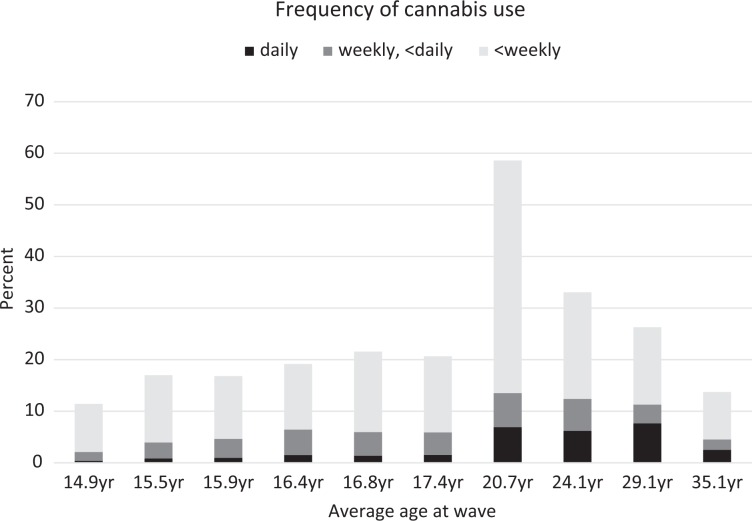
We found that cannabis use had become very common in youth living in Victoria. Sixty-two percent of VAHCS participants reported using cannabis at least once during follow-up from age 14 years to 35 years, with half commencing whilst of high school age and a further 38% by the time they were 20 years old (Figure 2). Use peaked at 20 years, with almost 60% of participants reporting some use in the past 12 months. Both initiation and prevalence then declined substantially, and by 29 years of age, only 26% reported using in the past year, declining to 14% at 35 years. The reduction in use in the 20s was largely due to decreases in those reporting only occasional use: 77% at 20 years, 62% at 24 years, 57% at 29 years, and 67% at 35 years, and there was a corresponding increase in the proportion of users who used at least weekly. The proportion of all participants at each wave reporting regular use remained fairly consistent across the 20s (14%, 10%, and 11% at 20, 24, and 29 years, respectively), but there was a marked reduction at 35 years to 5% of participants. Throughout follow-up, males consistently reported cannabis use more frequently than did females (adjusted for wave, average adjusted odds ratio [AOR] 1.7; 95% CI, 1.5 to 2.0).
Figure 2.
Cannabis use throughout follow-up in the Victorian Adolescent Health Cohort.
These observations differ from reports from the 1980s, when most cannabis users had ceased using by their late 20s.5 The current higher prevalence of use may contribute to this apparent change, reflecting a shift in mores reducing the social imperative to quit. The role of social transitions in young adulthood as a conduit to abstention may now be less potent or may have occurred when our cohort was older.
We separated the adolescent phase of follow-up into 2 sections: mid-school (average 14.9-15.9 years, waves 1-3) and late-school (average 16.4-17.4 years, waves 4-6). The frequency of adolescent cannabis use varied within individuals over time, but 82% of adolescents reporting mid-school use continued use into the late-school period.9 Antisocial behaviour, cigarette smoking, frequent and high-risk alcohol drinking, peer cannabis use, and the degree of school-level involvement in regular cannabis use were all associated with mid-school use. In mid-school nonusers, these same factors increased the likelihood of commencing cannabis use in late-school.9
Adolescent males both initiated use and escalated to higher levels of cannabis use more often than females: 13% of mid-school using males and 9% mid-school using females progressed to daily use in late-school. Escalation in boys was linked to perceived peer use, but this effect was not apparent in the girls, who were at risk of escalation if they reported high-risk alcohol use and antisocial behaviours. In general, perceived use by peers and a school environment in which regular cannabis use was reported more frequently provided a milieu in which initiation, continued use, and, for boys, escalation were more likely.10
Cannabis Dependence in Young Adults
Definitions of dependence were relaxed with the publication of the second edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-II) in 1968, allowing a diagnosis of a dependence syndrome without withdrawal symptoms if there was evidence of habitual use or a clear sense of need for the drug. This allowed cannabis to be classified as a drug of dependence, although it was only to receive cursory attention as such for another 35 years. No previous community study had described rates of cannabis dependence syndrome or the typical pattern of symptoms in the syndrome. We identified DSM-IV cannabis dependence criteria leading to a 12-month diagnosis of dependence in each adult wave (Table 1). Cannabis dependence, consistently more common in males, peaked at 20 years and thereafter declined in each subsequent wave. Overall, 12% (95% CI, 10% to 13%) of adults were assessed as cannabis dependent at least once from age 20 to 35 years.
Table 1.
Prevalence of DSM-IV-defined dependence in adulthood (waves 7 to 10).
| Wave | Cannabis dependence | |||||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | |||||||
| No. | Average age, years | N | n | % | 95% CI | n | % | 95% CI |
| 7 | 20.7 | 1594 | 83 | 10.6 | 8.1 to 13.6 | 40 | 4.3 | 2.9 to 6.2 |
| 8 | 24.1 | 1517 | 72 | 8.7 | 6.5 to 11.6 | 30 | 3.3 | 2.1 to 5.0 |
| 9 | 29.1 | 1387 | 31 | 4.3 | 2.8 to 6.6 | 21 | 2.1 | 1.2 to 3.7 |
| 10 | 35.1 | 1345 | 22 | 2.5 | 1.4 to 4.3 | 10 | 1.6 | 0.9 to 3.0 |
| Any adult wave | 1755 | 136 | 16.5 | 14.1 to 19.2 | 69 | 7.4 | 5.9 to 9.3 | |
DSM-IV = Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition).
Stratifying by adolescent cannabis use, 27% (95% CI, 24% to 31%) of adolescent cannabis users were subsequently identified with dependence in at least 1 adult wave (20 to 35 years). Escalation to dependence was identified in 17% (95% CI, 14% to 22%) of adolescent occasional users and 45% (95% CI, 39% to 52%) of regular users. Only 4% (95% CI, 3% to 6%) of adolescent abstainers were later diagnosed with cannabis dependence. Regular cannabis use in adolescence was the clearest predictor of later problematic use, with use before 16 years of age carrying most of the burden of risk for dependence at 24 years.11–13 Table 2 shows the independent association between adolescent cannabis use and dependence at 24 years, underlining the risk of daily use, persistent use, and earlier adolescent use in escalation to dependence. However, escalation in use was not inevitable as about 40% of adolescent daily users were no longer using regularly by 24 years. Male sex, parental divorce or separation, and persistent (>1 wave) cigarette smoking in adolescence predicted later escalation of use. Compared with consistent regular users, occasional adolescent users and regular users who moderated their use in adolescence had less risk of dependent use at 24 years. Nonetheless, they were still at substantially elevated risk compared with nonusers.
Table 2.
Association between adolescent cannabis use (waves 1-6) and cannabis dependence in 1520 cohort participants at 24 years (wave 8), adjusted for background factorsa.
| Dependent cannabis use in wave 8 (n b = 103) | |||||
|---|---|---|---|---|---|
| Adolescent cannabis use (waves 1-6) | N b | n | %c | ORd | 95% CI |
| Maximal frequency of use | |||||
| None | 999 | 15 | 1 | 0.16 | 0.08 to 0.32 |
| Occasional | 331 | 33 | 10 | 1 | |
| Weekly | 124 | 28 | 22 | 2.8 | 1.5 to 5.1 |
| Daily | 66 | 27 | 41 | 5.8 | 2.7 to 12.3 |
| Number of waves of use | |||||
| None | 999 | 15 | 1 | 0.16 | 0.07 to 0.36 |
| 1 or 2 waves | 234 | 24 | 10 | 1 | |
| 3 to 6 waves | 287 | 64 | 22 | 2.3 | 1.2 to 4.5 |
| First wave of reported use | |||||
| None | 999 | 15 | 1 | 0.16 | 0.08 to 0.33 |
| Late (wave 4-6) | 171 | 17 | 10 | 1 | |
| Early (wave 1-3) | 350 | 71 | 20 | 2.7 | 1.5 to 4.8 |
aTable derived from Swift et al.12
bFrequencies obtained by averaging across 5 imputed datasets.
cThe percentage with dependence in wave 8 versus all participants in the given category (N).
dOdds ratio from multivariable logistic regression models, adjusted for sex, parental divorce/separation, and parental smoking. For each analysis, the reference exposure category was defined to be the lowest level of adolescent cannabis use.
Debate continues about the processes underpinning the development of dependence. As well as the effects of social mores and drug availability, the central mechanism of cannabis intoxication may be involved, with vulnerability arising from the impact of chronic cannabis exposure on the developing cannabinoid system in the brain of susceptible individuals14 and possibly genetic liability.15,16 (See also the article by Renard et al. in this issue.)
Cannabis and Other Substance Use
The gateway theory proposed that adolescents move from alcohol/cigarettes to cannabis to other illicit drugs.3 Kandel clarified that this sequence is not inevitable, but she asserted that few adolescents skip a stage and she did not consider the possibility of reciprocal relationship between substances.3 Given the shifts in attitudes about cigarette smoking and the rapid increase in cannabis use in recent decades, there is a real possibility that the sequencing of substance initiation might change.
Cannabis and Tobacco
Cigarette smoking contributes the highest risk for preventable death in high-income countries.17 There are plausible biological pathways by which cannabis smoking may increase the risk for lung cancer.18 Adolescent cigarette smoking was implicated as a risk for the initiation of cannabis use in adolescence9 and as a mediator of adverse outcomes in young adulthood.19 Conversely, cannabis use in non-cigarette-smokers predicted cigarette smoking initiation.20,21 Elevated risk for later initiation of cigarette smoking was identified both in adolescent non-cigarette-smokers (occasional cannabis users relative to nonusers: AOR 8.4; 95% CI, 1.9 to 37) and in 20-year-olds (daily users relative to occasional users, AOR 6.1; 95% CI, 2.7 to 13). Confounding factors, such as low socioeconomic status, might explain this observation.22 Similarly, the relationships may reflect a shared social environment for cannabis and tobacco use. This finding may also reflect a desensitisation to the route of administration or may arise from the common practice of smoking both substances on the same occasion.23 The influence on cigarette smoking initiation constitutes a potentially serious health consequence of regular cannabis use beyond that directly attributable to cannabis.
Cannabis and Alcohol
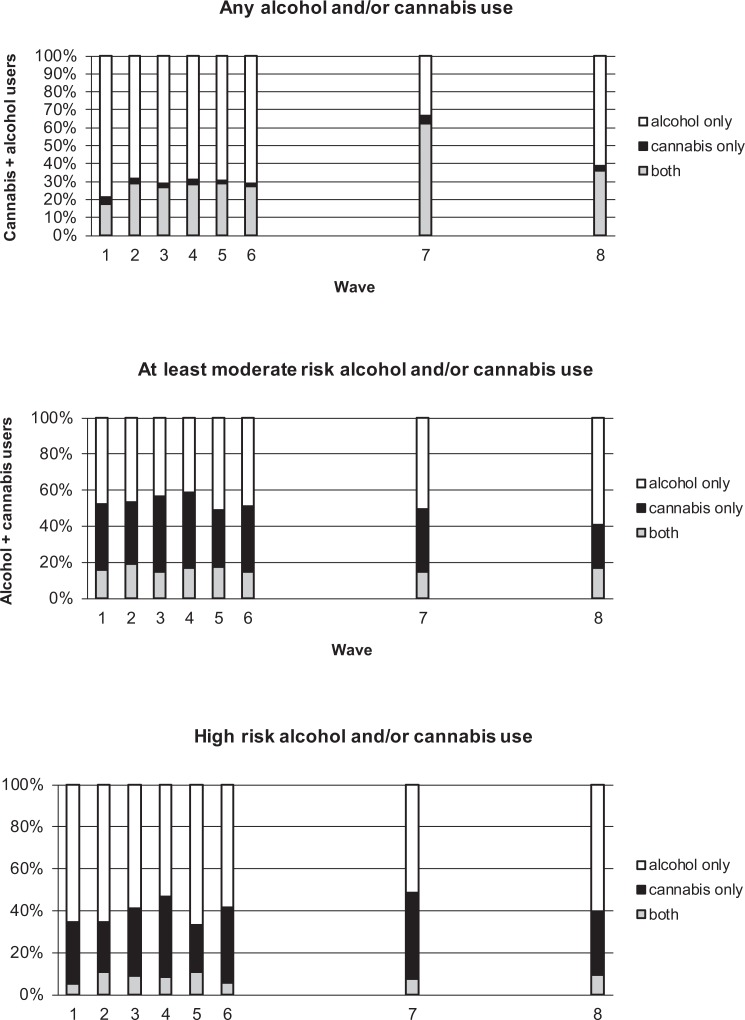
Consistent with the gateway theory, alcohol bingeing appeared to potentiate cannabis use9 but in later analyses became unimportant or even protective against an escalation in cannabis use. We hypothesised that there were identifiable disparate trajectories of problematic alcohol and cannabis use.24 In general, we found that adolescents heading toward substance abuse appeared to select either alcohol or cannabis, possibly as a result of availability and peer acceptability. We also reported that there were more extreme consequences of social and illicit substance use in the cannabis group than in the alcohol group at 24 years.24 The separation of substances at high levels of use is illustrated in Figure 3. Work on the Mid Atlantic Twin Registry suggested that drug selection was an environmental rather than a genetic phenomenon, whilst continuation may have a genetic component.25 It is therefore possible that public education initiatives aimed at reducing adolescent alcohol use in isolation may inadvertently increase cannabis uptake.
Figure 3.
Alcohol users only, cannabis users only, and both alcohol and cannabis users shown as a proportion of all users of any substance at each of waves 1 to 8, by 3 levels of use: any, moderate risk, and high risk. The x-axis scale reflects the relative timing of each survey. At least moderate use alcohol was defined as follows: in the week prior to survey, exceeded 28 standard drinks (SD) (1 SD = 10 g of alcohol) in males and 14 SDs in females. High-risk drinking was defined as follows: exceeded 43 SDs in males and 28 SDs in females. At least moderate risk cannabis use was defined as currently using at least weekly and high-risk use as currently using daily for both males and females. Figure from Patton et al.24
Cannabis and Other Illicit Substance Use
Adolescents using cannabis regularly are at high risk of escalation to other illicit substance use (e.g., Fergusson et al.26). An examination of the predictors and consequences of adolescent amphetamine use at 24 years brought the role of cannabis into stark focus. A clear dose-response relationship was noted between adolescent cannabis use and subsequent amphetamine initiation, independent of cigarette smoking, alcohol use, and antisocial behaviour.27 The links between adolescent amphetamine use and poor educational and substance use outcomes at 24 years were substantially confounded by adolescent cannabis use.27
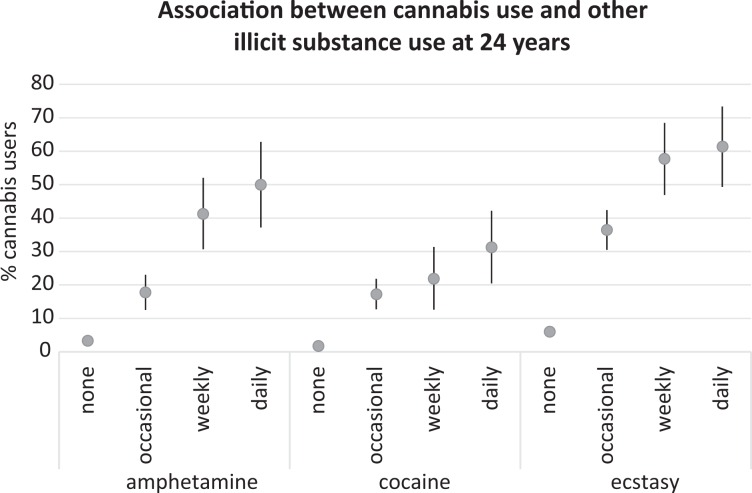
Some adolescents did not proceed beyond occasional adolescent cannabis use. For this group, 30% reported other illicit substance use at 24 years of age, so even occasional adolescent users were not completely protected from this outcome.13 We subsequently showed that cannabis and other illicit substance use co-occurred in each wave in young adulthood.21 This is illustrated for wave 8 in Figure 4. During young adulthood, both occasional and regular cannabis use predicted incident amphetamine, cocaine, and ecstasy use, with regular cannabis use providing the greatest risk. In contrast, quitting cannabis in young adulthood predicted lower illicit drug use.21
Figure 4.
Prevalence of substance use at 24 years (wave 8), stratified by concurrent cannabis use frequency. Percentages are shown with 95% CIs.
Whether cannabis use is actually causal in the escalation to other drugs of dependence28 or arises as a result of drug availability or the adoption of peer attitudes remains uncertain. Regardless of the mechanism, cannabis use places adolescents at risk of later use of other illicit drugs.
Social and Educational Outcomes
The links between cannabis use and educational attainment and participation in adult roles have been well-established (e.g., Kandel et al.,3 Fergusson and Horwood29). We, too, found that unemployment and welfare dependence were associated with regular cannabis use.19,30 School dropout was an important mediator in those using cannabis daily before year 11 (the penultimate year of schooling). The negative relationship between adolescent cannabis use and higher education was consistent across 3 Australasian cohorts.31
Adolescents at risk of initiating cannabis use also had high rates of antisocial behaviour, cigarette smoking, and high-risk alcohol use, all likely to heighten failure in making transitions to adulthood. It nevertheless remains possible that disengagement with school, accompanied by a history of failure, may have occurred before initiation and escalation of cannabis use or even may have contributed to it causally, due to association with like-minded peers who commenced cannabis use in a concerted effort not to conform to adult expectations.32
Mental Health
A consistent association was noted between depression and cannabis use in adolescence and young adulthood, but the relationship weakened as adolescents matured into young adults.33 A question remained about the directionality of the association between depression and cannabis use. Females, but not males, using daily in adolescence or at 20 years were shown to be more likely to report anxiety and depression symptoms at 20 years than were nonusers (females: AOR 1.9; 95% CI, 1.1 to 3.3; males: AOR 0.47; 95% CI, 0.17 to 1.3).34 By 29 years, adolescent daily cannabis users were demonstrably at increased risk of DSM-IV-defined anxiety disorder, whether or not they had abstained in the meantime35 (Table 3). This association was independent of background factors including other illicit substance use and earlier symptoms of anxiety and depression.
Table 3.
Associations of maximum adolescent use and late-onset cannabis use with anxiety disorder identified in 1756 cohort participants (mean age 29 years)a.
| Continuity in cannabis use from adolescence to 29 years | Anxiety disorder at 29 years (wave 9) (n = 199) | |||||||
|---|---|---|---|---|---|---|---|---|
| Maximum adolescent use (waves 2-6) | Use at 29 years (wave 9) | N b | Adjusted for background factors | Further adjusted for concurrent alcohol and other illicit substance use at 29 years | Further adjusted for any adolescent anxiety/depression (CIS-R>11) | |||
| ORc | 95% CI | ORd | 95% CI | ORe | 95% CI | |||
| None, <weekly | None | 1173 | 1 | 1 | 1 | |||
| Weekly+ | None | 97 | 2.0 | 1.1 to 3.7 | 2.2 | 1.1 to 4.2 | 1.8 | 0.96 to 3.5 |
| None, <weekly | Occasional-weekly | 288 | 1.8 | 1.2 to 2.8 | 2.1 | 1.3 to 3.3 | 2.0 | 1.2 to 3.3 |
| Weekly+ | Occasional-weekly | 79 | 1.4 | 0.60 to 3.5 | 1.7 | 0.67 to 4.2 | 1.5 | 0.58 to 3.7 |
| None, <weekly | Daily | 85 | 2.2 | 0.91 to 5.2 | 2.4 | 0.98 to 5.8 | 2.5 | 1.0 to 6.1 |
| Weekly+ | Daily | 35 | 3.1 | 1.2 to 8.3 | 3.8 | 1.3 to 11 | 3.2 | 1.1 to 9.2 |
aTable derived from Degenhardt et al.35
bAll estimates obtained by averaging across the imputed datasets.
cOdds ratios from multivariable logistic regression models adjusted for background factors: sex, nonmetropolitan school location, low parental education, parental divorce/separation by wave 6.
dOdds ratios from multivariable logistic regression models adjusted for background factors and, at 29 years, substance use: high-risk alcohol use in the past week and other illicit substance use (any of amphetamine, cocaine, or ecstasy use in the past year).
eOdds ratios from multivariable logistic regression models adjusted for background factors, other concurrent substance use, and any adolescent anxiety and depression symptoms measured using the revised Clinical Interview Schedule (CIS-R) (waves 2 to 6).
The links with poor mental health despite later abstinence suggest a possibility of partially irreversible neurotoxicity with heavy, early adolescent use. The Dunedin cohort study in New Zealand reported a demonstrable neuropsychological decline at 38 years in subjects who had used cannabis daily in adolescence.36 As in our study, this was identified despite subsequent abstinence.
Summary of the Main Findings
Analyses from the Victorian Adolescent Health Cohort Study provide unequivocal evidence of harms following heavy cannabis use in early adolescence. These include the following:
Academic failure and school dropout
Persisting mental health problems
Heightened risk for dependence on cannabis
Further substance abuse of other drugs
Occasional adolescent users have far fewer adverse consequences than heavy users, but even in occasional adolescent users, risks for other later substance use and abuse are higher than for nonusers.
We confirmed that in adolescence, other risk behaviours such as cigarette smoking and antisocial behaviour are often associated with the initiation, continuation, and escalation of cannabis use.
Public Health Intervention and Legislation
The health and social policy implications of these findings have yet to be fully recognised and implemented in any jurisdiction. The findings have a particular salience at a time when legislative frameworks around cannabis use are changing rapidly.37 The increasing decriminalisation and legalisation of cannabis possession for personal use in many countries, including some U.S. states and Canada, have the potential to increase the availability of cannabis to adolescents even where purchasing the drug remains illegal before the age of 18 (e.g., the Netherlands) or 21 (e.g., Washington State).
Responses are likely to be needed at 3 levels. First, there is a need for stronger preventive interventions, particularly in settings where cannabis use in adults is legal. Measures that have been effective in reducing tobacco use, including taxation and control of marketing, are essential elements of an effective preventive response, with a particular emphasis on limiting sales to minors. Given that neurodevelopment continues well into the 20s, there would be a strong argument for making sales to those younger than 21 illegal. For this to occur, politicians will need the knowledge and fortitude to carry the general public toward a more effective legislative structure, alongside the provision of clear evidence-based information, easily accessible by the lay public, that is designed to dispel myths, inform about potential harms, and encourage responsible use is essential.38
Demands are increasing for rigorously evaluated strategies to treat cannabis use disorders,39,40 and given the high rates of cannabis dependence found in the VAHCS, there is a specific pressing need for more and better evaluation of promising interventions in adolescents. For adolescents who have become heavy users, health services need to respond early and effectively in family and community settings. There is currently limited evidence, mostly in adults, of effectiveness of psychotherapeutic interventions for cannabis dependence. Pharmacological treatments have not yet been shown to be effective,41 although this modality is awaiting more thorough evaluation.42 A large European, multiple-centre, randomised controlled trial of multidimensional family therapy versus individual therapy with self-referred or coerced teenagers (13 to 18 years) with cannabis abuse or dependence has reported promising results, with about 60% of participants showing symptomatic improvement at 12-month follow-up, albeit without a requirement for abstention.43
Treatment-seeking by symptomatic Australian cannabis users at a rate of about 1 in 3 is still unacceptably low,44 and it is likely to be substantially lower in younger adolescents, who are those at most risk of adverse consequences from heavy cannabis use. Social marketing has the potential to increase service use. So too, the development of online strategies may have the potential to reach a group who otherwise are unlikely to have any clinical intervention. A randomised trial of web-based psychotherapeutic treatment for uncomplicated cannabis use disorder in treatment-seeking adults has shown short-term, modest improvement in cannabis use and related harms compared with an educational program.41 In common with other web-based treatment interventions, attrition was a problem and the authors suggested combining this modality with a face-to-face component. In a meta-analysis of web-based interventions of varying intensity targeting both teenagers and adult cannabis users, attrition was least when mother-daughter dyads were enrolled.45 Short duration of follow-up appears to be a limiting factor in the evaluation of most interventions.
Harm reduction strategies will remain important. Public education in a parent- and teen-appropriate manner focussing on the harms associated with cannabis use is an important facet of prevention. Our findings lead to further questions about policies to regulate cannabis use as well as the scope for prevention and treatment. Further curtailment of legal penalties for possession and small-scale production could take place while penalties for commercial production and dealing are retained. This has the potential to reduce the damaging consequences of obtaining a criminal record through noncompliance with reduced penalties and enables diversion from the court system and custodial sentences into health and rehabilitative interventions. Other strategies that will be important include the development and enforcement of legislation restricting access to minors, regulation of tetrahydrocannabinol (THC) content, and taxation to raise the price of cannabis. Given its ease of cultivation, the latter may prove difficult. So too, improved training of health and education providers might lead to better recognition and timely and effective treatment. Given the current limited evidence base for action, innovation in preventive and treatment approaches are essential. To build our evidence base for future action, these will need the highest possible level of evaluation.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Shedler J, Block J. Adolescent drug use and psychological health: a longitudinal inquiry. Am Psychol. 1990;45(5):612–630. [DOI] [PubMed] [Google Scholar]
- 2. Robins L. The natural history of substance use as a guide to setting drug policy. Am J Public Health. 1995;85(1):12–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kandel DB, Davies M, Karus D, et al. The consequences in young adulthood of adolescent drug involvement: an overview. Arch Gen Psychiatry. 1986;43(8):746–754. [DOI] [PubMed] [Google Scholar]
- 4. Fergusson DM, Lynskey MT, Horwood LJ. The short-term consequences of early onset cannabis use. J Abnorm Child Psychol. 1996;4:499–512. [DOI] [PubMed] [Google Scholar]
- 5. Kandel DB. Marijuana users in young adulthood. Arch Gen Psychiatry. 1984;41(2):200–209. PubMed PMID: 6607718. [DOI] [PubMed] [Google Scholar]
- 6. Chen K, Kandel DB. The natural history of drug use from adolescence to the mid-thirties in a general population sample. Am J Public Health. 1995;85(1):41–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jessor R. Predicting time of onset of marijuana use: a developmental study of high school youth. J Consult Clin Psychol. 1976;44(1):124–134. [DOI] [PubMed] [Google Scholar]
- 8. Kandel DB. Stages in adolescent involvement in drug use. Science. 1975;4217:912–914. [DOI] [PubMed] [Google Scholar]
- 9. Coffey C, Lynskey M, Wolfe R, et al. Initiation and progression of cannabis use in a population-based Australian adolescent longitudinal study. Addiction. 2000;95(11):1679–1690. PubMed PMID: 11219371. [DOI] [PubMed] [Google Scholar]
- 10. Hawkins JD, Catalano RF, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: implications for substance abuse prevention. Psychol Bull. 1992;112(1):64–105. PubMed PMID: 1529040. [DOI] [PubMed] [Google Scholar]
- 11. Coffey C, Carlin JB, Lynskey M, et al. Adolescent precursors of cannabis dependence: findings from the Victorian Adolescent Health Cohort Study. Br J Psychiatry. 2003;182:330–336. doi: 10.1192/bjp.182.4.330. PubMed PMID: WOS:000182140100014. [DOI] [PubMed] [Google Scholar]
- 12. Swift W, Coffey C, Carlin JB, et al. Adolescent cannabis users at 24 years: trajectories to regular weekly use and dependence in young adulthood. Addiction. 2008;103(8):1361–1370. doi: 10.1111/j.1360-0443.2008.02246.x. PubMed PMID: WOS:000257692800018. [DOI] [PubMed] [Google Scholar]
- 13. Swift W, Coffey C, Carlin JB, et al. Are adolescents who moderate their cannabis use at lower risk of later regular and dependent cannabis use? Addiction. 2009;104(5):806–814. doi: 10.1111/j.1360-0443.2009.02534.x. PubMed PMID: WOS:000265008400024. [DOI] [PubMed] [Google Scholar]
- 14. Schneider M. Puberty as a highly vulnerable developmental period for the consequences of cannabis exposure. Addict Biol. 2008;13(2):253–63. doi: 10.1111/j.1369-1600.2008.00110.x. [DOI] [PubMed] [Google Scholar]
- 15. Gillespie NA, Kendler KS, Neale MC. Psychometric modeling of cannabis initiation and use and the symptoms of cannabis abuse, dependence and withdrawal in a sample of male and female twins. Drug Alcohol Depend. 2011;118(2-3):166–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Renard J, Rushlow WJ, Laviolette SR. What can rats tell us about adolescent cannabis exposure? Insights from pre-clinical research. Can J Psychiatry. 2016;61(6):328–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. WHO. Global health risks [Internet]. Geneva (Switzerland): World Health Organisation; 2004. [cited 2012 June 30]. Available at: http://www.who.int/topics/risk_factors/en/ [Google Scholar]
- 18. Tashkin DP. Does cannabis use predispose to chronic airflow obstruction? Eur Respir J. 2010;35(1):3–5. [DOI] [PubMed] [Google Scholar]
- 19. Degenhardt L, Dierker L, Chiu WT, et al. Evaluating the drug use “gateway” theory using cross-national data: consistency and associations of the order of initiation of drug use among participants in the WHO World Mental Health Surveys. Drug Alcohol Depend. 2010;108(1-2):84–97. PubMed PMID: 20060657; PubMed Central PMCID: PMC2835832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patton GC, Coffey C, Carlin JB, et al. Reverse gateways? Frequent cannabis use as a predictor of tobacco initiation and nicotine dependence. Addiction. 2005;100(10):1518–1525. doi: 10.1111/j.1630-0443.2005.01220.x. PubMed PMID: WOS:000232102600017. [DOI] [PubMed] [Google Scholar]
- 21. Swift W, Coffey C, Degenhardt L, et al. Cannabis and progression to other substance use in young adults: findings from a 13-year prospective population-based study. J Epidemiol Community Health. 2012;66(7):e26 PubMed PMID: 21771817. [DOI] [PubMed] [Google Scholar]
- 22. Creemers HE, Korhonen T, Kaprio J, et al. The role of temperament in the relationship between early onset of tobacco and cannabis use: the TRAILS study. Drug Alcohol Depend. 2009;104(1-2):113–118. PubMed PMID: 19482444. [DOI] [PubMed] [Google Scholar]
- 23. Agrawal A, Budney AJ, Lynskey MT. The co-occurring use and misuse of cannabis and tobacco: a review. Addiction. 2012;107(7):1221–1233. PubMed PMID: 22300456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Patton GC, Coffey C, Lynskey MT, et al. Trajectories of adolescent alcohol and cannabis use into young adulthood. Addiction. 2007;102(4):607–615. doi: 10.1111/j.1360-0443.2006.01728.x. PubMed PMID: 17286642. [DOI] [PubMed] [Google Scholar]
- 25. Kendler KS, Schmitt E, Aggen SH, et al. Genetic and environmental influences on alcohol, caffeine, cannabis, and nicotine use from early adolescence to middle adulthood. Arch Gen Psychiatry. 2008;65(6):674–682. doi: 10.1001/archpsyc.65.6.674. PubMed PMID: 18519825; PubMed Central PMCID: PMCPMC2844891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Fergusson DM, Horwood LJ, Swain-Campbell N. Cannabis use and psychosocial adjustment in adolescence and young adulthood. Addiction. 2002;97(9):1123–1135. PubMed PMID: 12199828. [DOI] [PubMed] [Google Scholar]
- 27. Degenhardt L, Coffey C, Moran P, et al. The predictors and consequences of adolescent amphetamine use: findings from the Victoria Adolescent Health Cohort Study. Addiction. 2007;102(7):1076–1084. doi: 10.1111/j.1360-0443.2007.01839.x. PubMed PMID: 17567396. [DOI] [PubMed] [Google Scholar]
- 28. Strang J, Witton J, Hall W. Improving the quality of the cannabis debate: defining the different domains. BMJ. 2000;320(7227):108–110. PubMed PMID: 10625271; PubMed Central PMCID: PMCPMC1117366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fergusson DM, Horwood LJ. Early onset cannabis use and psychosocial adjustment in young adults. Addiction. 1997;92(3):279–296. PubMed PMID: 9219390. [PubMed] [Google Scholar]
- 30. Lynskey MT, Coffey C, Degenhardt L, et al. A longitudinal study of the effects of adolescent cannabis use on high school completion. Addiction. 2003;98(5):685–692. doi: 356 [pii]. PubMed PMID: 12751986. [DOI] [PubMed] [Google Scholar]
- 31. Horwood LJ, Fergusson DM, Hayatbakhsh MR, et al. Cannabis use and educational achievement: findings from three Australasian cohort studies. Drug Alcohol Depend. 2010;110(3):247–253. PubMed PMID: 20456872. [DOI] [PubMed] [Google Scholar]
- 32. Rogeberg O. Correlations between cannabis use and IQ change in the Dunedin cohort are consistent with confounding from socioeconomic status. Proc Natl Acad Sci U S A. 2013. PubMed PMID: 23319626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Horwood LJ, Fergusson DM, Coffey C, et al. Cannabis and depression: an integrative data analysis of four Australasian cohorts. Drug Alcohol Depend. 2012;126(3):369–378. doi: 10.1016/j.drugalcdep.2012.06.002. PubMed PMID: 22749560. [DOI] [PubMed] [Google Scholar]
- 34. Patton GC, Coffey C, Carlin JB, et al. Cannabis use and mental health in young people: cohort study. BMJ. 2002;325(7374):1195–1198. PubMed PMID: 12446533; PubMed Central PMCID: PMC135489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Degenhardt L, Coffey C, Romaniuk H, et al. The persistence of the association between adolescent cannabis use and common mental disorders into young adulthood. Addiction. 2012. doi: 10.1111/j.1360-0443.2012.04015.x. PubMed PMID: 22775447. [DOI] [PubMed] [Google Scholar]
- 36. Meier MH, Caspi A, Ambler A, et al. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc Natl Acad Sci U S A. 2012;109(40):E2657–E2664. PubMed PMID: 22927402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Cressey D. The cannabis experiment. Nature. 2015;524(7565):280–283. PubMed PMID: 26295084. [DOI] [PubMed] [Google Scholar]
- 38. Murray RM, Morrison PD, Henquet C, et al. Cannabis, the mind and society: the hash realities. Nat Rev Neurosci. 2007;8(11):885–895. doi: 10.1038/nrn2253. PubMed PMID: 17925811. [DOI] [PubMed] [Google Scholar]
- 39. Copeland J, Swift W. Cannabis use disorder: epidemiology and management. Int Rev Psychiatry. 2009;21(2):96–103. doi: 10.1080/09540260902782745. PubMed PMID: 19367503. [DOI] [PubMed] [Google Scholar]
- 40. Hall W, Fischer B. Harm reduction policies for cannabis In: Rhodes T, Hedrich D, editors. Harm reduction: evidence, impacts and challenges. Luxembourg: Publications Office of the European Union; 2010. p. 235–252. [Google Scholar]
- 41. Rooke S, Copeland J, Norberg M, et al. Effectiveness of a self-guided web-based cannabis treatment program: randomized controlled trial. J Med Internet Res. 2013;15(2):e26 doi: 10.2196/jmir.2256. PubMed PMID: 23470329; PubMed Central PMCID: PMCPMC3636012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Vandrey R, Haney M. Pharmacotherapy for cannabis dependence: how close are we? CNS Drugs. 2009;23(7):543–553. doi: 10.2165/00023210-200923070-00001. PubMed PMID: 19552483; PubMed Central PMCID: PMCPMC2729499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Rigter H, Henderson CE, Pelc I, et al. Multidimensional family therapy lowers the rate of cannabis dependence in adolescents: a randomised controlled trial in Western European outpatient settings. Drug Alcohol Depend. 2013;130(1-3):85–93. [DOI] [PubMed] [Google Scholar]
- 44. Teesson M, Slade T, Swift W, et al. Prevalence, correlates and comorbidity of DSM-IV cannabis use and cannabis use disorders in Australia. Aust N Z J Psychiatry. 2012;46(12):1182–1192. [DOI] [PubMed] [Google Scholar]
- 45. Tait RJ, Spijkerman R, Riper H. Internet and computer based interventions for cannabis use: a meta-analysis. Drug Alcohol Depend. 2013;133(2):295–304. doi: 10.1016/j.drugalcdep.2013.05.012. PubMed PMID: 23747236. [DOI] [PubMed] [Google Scholar]