Abstract
Background:
Fetal malnutrition (FM) which describes the underweight/wasting seen in newborns is a significant contributor to perinatal morbidity and mortality and requires proper documentation. The objective of this study was to assess the nutritional status of term newborns at birth using Clinical Assessment of Nutritional (CAN) status score and four other anthropometric indices and to compare the efficiency of CAN score and the anthropometric indices in identifying FM in term newborns.
Materials and Methods:
The study was conducted on live singleton babies delivered ≥37–42 completed weeks of gestation at the inborn unit of Lagos University Teaching Hospital without major congenital abnormalities or severe perinatal illness. Birth weights and lengths were recorded at birth. Ponderal index (PI), body mass index (BMI), and mid-arm/head circumference (MAC/HC) ratio were calculated and the values were compared with standard curves. The CAN score consisted of inspection and estimation of loss of subcutaneous tissues and muscles. FM was defined as CAN score <25. Data were analyzed using the Statistical Package for Social Sciences statistics software version 17.0.
Results:
Two hundred and eighty-two newborns were analyzed. FM was identified in 14.5%, 10.3%, 13.1%, and 2.8% of newborns using CAN score, PI, BMI, and MAC/HC ratio, respectively. Out of the FM babies identified by CAN score, PI, MAC/HC, and BMI identified 19.5%, 12.3%, and 53.7% of them as FM also. BMI was the most sensitive anthropometric index for detecting FM.
Conclusion:
CAN score is a simple clinical tool for identifying FM and when used in conjunction with BMI will enhance FM detection.
Keywords: Clinical Assessment of Nutritional status score, fetal malnutrition, proportionality indices, term newborns
INTRODUCTION
Fetal malnutrition (FM) is a significant contributor to perinatal morbidity and mortality.1,2,3 It is a state of poor nutrition in-utero resulting from inadequate supply and/or utilization of nutrients1 leading to the fetus failing to acquire adequate amount of fat, subcutaneous tissues, and muscle mass during intrauterine growth.1 FM describes the underweight/wasting aspect of the clinical syndrome seen in malnourished newborns. This clinical state may be present at almost any birth weight.2 Globally, the incidence of FM is between 2% and 10% of total births with highest incidence in developing countries.2 A study conducted in Ile-Ife, Nigeria, reported an incidence of 18.8% for FM in term newborns.3
The assessment of the nutritional status of the fetus has been of considerable interest to clinicians because of its potential serious sequelae on multiple organ systems manifesting as perinatal problems and/or long-term central nervous system sequelae.3,4 Recent studies have also demonstrated the evidence that FM may have a far-reaching effect on adult life such as susceptibility to cardiovascular disease and non-insulin dependent diabetes mellitus.5,6,7
Various anthropometric indices have been used to identify babies that suffered suboptimal fetal growth (weight, length, mid-arm circumference (MAC) and head circumference (HC),8,9 proportionality indices (ponderal index [PI],8,9,10 MAC/HC ratio, body mass index [BMI]), and Clinical Assessment of Nutritional (CAN) status and its score.9,11,12
CAN score – which contains nine clinical signs, namely, hair, cheeks, neck, arms, chest, abdomen, back, buttocks, and legs, as developed by Metcoff11 to differentiate malnourished from appropriately nourished babies4 – has also been used widely by researchers to determine FM in the newborn period. There is a dearth of research in the combined use of CAN score, BMI, and the other anthropometric indices as a means of assessing FM in newborns in the West African subregion.
The aims of the present study are to assess the nutritional status of term newborns at birth using CAN score, BMI, PI, MAC/HC, and birth weight and to compare the relative efficiency of CAN score and the anthropometric indices in the identification of FM in term newborns. The findings from this study will provide renewed insight into the easier and better methods of determining FM in term newborns.
MATERIALS AND METHODS
The study was carried out on consecutive, singleton, live born babies of ≥37 completed weeks through 41 weeks of gestation at the inborn unit of LUTH between May 1, 2010, and November 30, 2010.
Exclusion criteria include any obvious major congenital abnormalities or severe perinatal illness. Ethical clearance was obtained from the Research and Ethics Committee of the Hospital. Informed parental consent was obtained for each newborn recruited.
Two hundred and eighty-two newborns were studied. Each infant was examined by the investigator within 48 h of birth. All the anthropometric measurements, except birth weight, were carried out by the investigator with trained assistance where needed, within 48 h of baby's birth. All the neonates were weighed completely nude at birth by the delivery room staff using the infant weighing scale (Weighmaster model®, USA) which records the weight to the nearest 10 g. Using the Olowe intrauterine growth chart,13 birth weights for gestational age below the 3rd percentile and above the 97th percentile on the chart were taken as small for gestational age (SGA) and large for gestational age (LGA), respectively. The infant's length was measured using an Infalength®. It was measured to the nearest 2 mm. The HC was measured using a flexible nonstretchable tape measure with due attention to the appropriate prominences.14 The measurement was to the nearest 0.1 cm. The MAC was measured using the same tape at the midpoint between the acromion and the olecranon process with the forearm flexed at 90° at the elbow.14 In the abducted arm with the elbow flexed (in almost all the term babies), a skin crease appears which corresponds approximately with the midpoint of the arm.14,15,16 The readings obtained were recorded to the nearest 0.1 cm.
PI was computed from the formula: PI = weight (g)/length3 (cm) × 100 and PI <2.2 was considered as malnutrition. The MAC/HC ratio was calculated for each infant and the value plotted on a standard curve designed for Nigerian newborn.16,17,18 BMI was calculated for each baby and the value was plotted on the BMI curve designed by Brock et al. for newborn babies.18
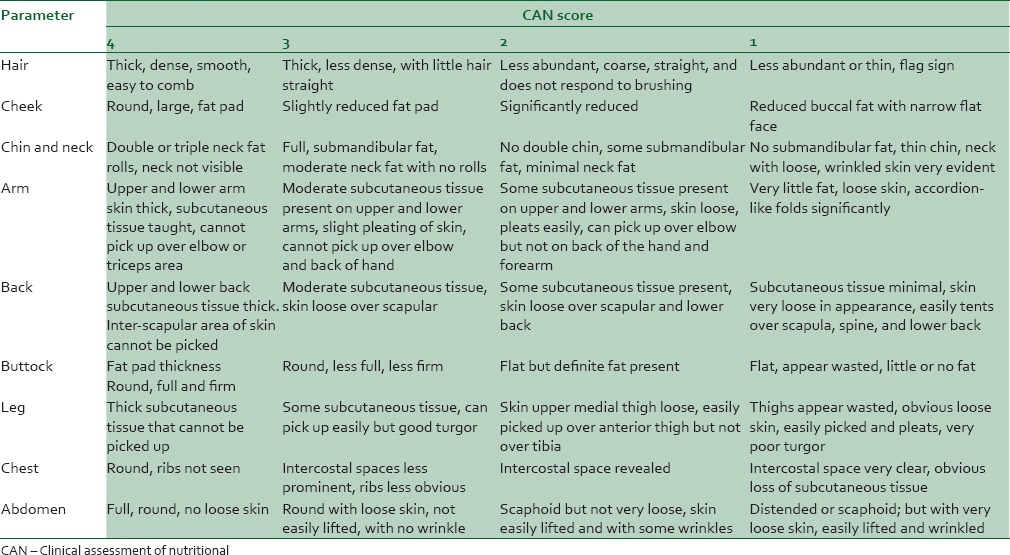
CAN status was done within 48 h of life on the basis of the superficial readily detectable signs of malnutrition in the newborn as described by Metcoff [Table 1].4 This consisted of inspection and estimation of loss of subcutaneous tissues and muscles in the designated areas. Hair, cheeks, neck and chin, arms, back, buttocks, legs, chest, and abdomen were examined and then scored. The range of scores for each varied between 1 and 4. A maximum score of 4 was awarded to each parameter with no evidence of malnutrition, and the lowest score of 1 was awarded to parameter with the worst evidence of malnutrition. The total rating of the 9 CAN score signs was the CAN score for the subject. FM was defined as CAN score <25.4,19,20
Table 1.
The nine signs for clinical assessment of nutritional status in the newborn
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS)for windows, version 17.0 (SPSS Inc®, Chicago released 2008, IBM Corp, New York). The variables were presented by frequency tables and cross-tabulations. Student's t-test was used to compare the mean anthropometry between males and females. Nonparametric data were analyzed using Mann–Whitney U-test. Chi-squared analysis was used to assess association between categorical variables. Fisher's exact test was used for variables <5. P < 0.05 was considered statistically significant at 95% confidence level.
RESULTS
Two hundred and eighty-two term newborns were studied. One hundred and thirty-seven were male while 145 were female, with a male: female ratio of 1:1.07. Eight babies (2.8%) were of low birth weight and SGA while 15 (5.3%) were LGA. The anthropometric characteristics of the study population showed that the mean birth weight was 3260 ± 460 g and mean length of 49.37 ± 2.26 cm while the MAC and HC were 34.63 ± 1.19 cm and 10.83 ± 1.01, respectively.
Selected maternal characteristics of the study population
The mean age of the mothers was 30.4 ± 4.6 years. Sixty-two percent of the mothers had tertiary level of education. Only 4.2% had primary level of education or below. About 53.2% of the babies were born to multiparous mothers and 39% of the mothers had various illnesses during pregnancy (high blood pressure [30%], malaria [15.9%], and retroviral disease [37.8%]).
The nutritional assessments
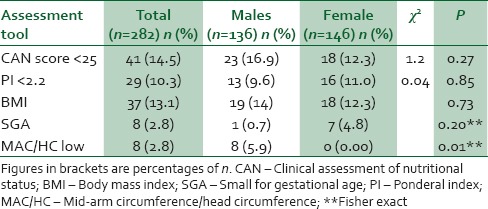
The prevalence of FM as detected by CAN score was 14.5% while BMI detected 13.1% of the study participants as malnourished. PI and MAC/HC detected FM in 10.3% and 2.8% of the study population, respectively. The relationship between sex and FM is as shown in Table 2. The incidence of FM is slightly more in male babies, but it was not statistically significant except with MAC/HC ratio which detected no female newborn with FM.
Table 2.
Relationship between sex and fetal malnutrition
Two hundred and fifty-nine babies (91.8%) were appropriate for gestational age (AGA), 15 (5.3%) were LGA, and 8 (2.8%) were classified as SGA using Olowe's intrauterine growth chart. CAN score identified 15.4% of the AGA babies as FM and only one of the SGA babies as FM. None of the LGA was malnourished by CAN score.
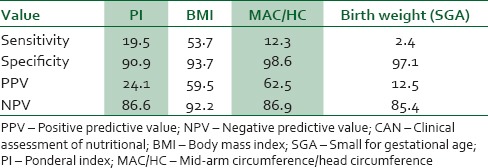
Tables 3 and 4 show the comparison of CAN score with anthropometry in detection of FM. BMI showed the highest sensitivity (53.7%) in detecting FM. It detected 22 out of the 41 babies that CAN score classified as malnourished. BMI also showed a high specificity of 93.7%. PI, MAC/HC, and birth weight showed very low sensitivity of 19.5%, 12.3%, and 2.4%, respectively, in detecting FM; however, all showed very high specificity (90.9%, 98.6%, and 97.1%, respectively) in detecting FM.
Table 3.
Comparison between clinical assessment of nutritional score and anthropometric indices in detection of fetal malnutrition in term newborns
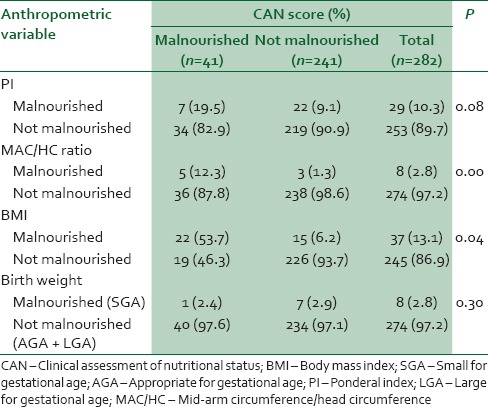
Table 4.
The sensitivity, specificity and predictive value of anthropometric indices in determining fetal malnutrition
DISCUSSION
FM is prevalent in the developing countries.3,21 Studies have documented that the nutritional status of the newborn is important for identifying perinatal risks4,22,23 as any deviation from the normal is associated with an increased risk of morbidity and mortality.24
In the present study, we evaluated 282 babies for FM. The mean birth weight of the babies was 3260 ± 460 g which was higher than 3067 g recorded in Ile-Ife5 and 3080 g in Jos,24 both in Nigeria, and 2600 g reported in India.25 It was however comparable with the 3290 g documented by Metcofff4 in the USA.
The prevalence of SGA in term babies in the present study is low (2.8%) compared to the prevalence reported by Adebami et al.3 in Ile-Ife (12.1%) and Mehta et al.25 in India (25%) while Metcoff4 documented SGA prevalence of 11% in term newborns in Oklahoma, USA. The low prevalence of SGA in the present study may be due to the different intrauterine growth curves used. The Olowe intrauterine growth chart13 used in this study classified babies <2 standard deviations below the mean or below the 3rd percentile as SGA, whereas the Brenner intrauterine growth chart which uses the 10th percentile as the cutoff for SGA was used in the study by Metcoff4 and Adebami et al.3 A similar study in India by Sankhyan et al.9 had also reported a lower prevalence of SGA when local Indian intrauterine growth chart was used (9.1%) compared to when international growth charts which had higher cutoff weights at each gestational age was used (45.4%) resulting in higher sensitivity but low specificity.
The prevalence of FM in the present study using CAN score (14.5%) is slightly lower than 18.8% documented in Ile-Ife by Adebami et al.3 and is 2–3-fold lower than that documented in India by Sankhyan et al.9 and Mehta et al.25 The reason for the lower prevalence in our study may be related to the demographics and socioeconomic status of the population studied. A well-nourished and healthy mother is more likely to deliver a healthy and well-nourished baby. The prevalence of FM using CAN score and anthropometry in various gestational age groups of infants had been reported by different researchers. It has been demonstrated that birth weight alone may not reflect the fetal state of nutrition of a newborn adequately. Previous researchers had demonstrated that not all SGA babies had FM and that some AGA babies may have features of FM. In the study by Metcoff,4 the prevalence of FM was reported to be 5.5% in AGA infants and 54.0% in SGA infants. Sankhyan et al.9 documented features of FM in 57.1% of SGA and 3.8% of AGA newborns. Adebami et al.3 detected FM in 11.5% of term AGA babies using CAN score. In the present study, CAN score identified FM in 15.4% of term AGA babies indicating that these babies suffered from FM in spite of having normal birth weight. Among SGA babies, only one baby (2.4%) was malnourished using CAN score; thus, the term FM and SGA are not synonymous. This finding is also similar to that of other researchers such as Metcoff that not all SGA babies were FM.
The anthropometric parameters are important to reflect intrauterine growth and to define a baseline to follow-up the nutritional progress of the infant. Many authors have proposed that the assessment of body proportions may be more useful than single measurements for age alone for assessing newborn nutrition.8,9,26,27 BMI provides a high estimate of body fat mass as it has a positive correlation with skinfold thickness and other methods of estimating the percentage of body fat,15 and it takes advantage of the physiologic principle regarding sparing length at the expense of weight during mild to moderate malnutrition.28 In our study, BMI detected FM in 13.1% of the babies and on comparing with CAN score, it was noted that the sensitivity of BMI in detecting FM was the highest among anthropometric parameters, suggesting BMI may be a sensitive indicator of FM. Soundarya et al.29 also found BMI to be a sensitive indicator of FM in their study and proposed a combination of BMI and PI in the screening of babies for FM.
PI has been used by various authors to classify intrauterine growth and FM infants. The present study recorded FM prevalence of 10.3% in term babies using PI. This is lower than the prevalence recorded by Mehta et al.25 (29.19%) and Kayshap et al.27 (27.8%) in India. It is, however, comparable with the lower prevalence of 8.1% documented by Adebami et al.3 Both Mehta et al.25 and Kashyap et al.27 combined the late gestational preterm babies of ≥ 35 weeks to the analysis of their results and thus may have contributed to their higher prevalence. Some babies with normal PI were found to be malnourished using CAN score in the present study. CAN score identified 34 (13.4%) of the babies with normal PI as malnourished. This underscores the limitations of PI in identifying FM.
The prevalence of FM in the present study using MAC/HC ratio was very low (2.8%). This is lower than the 49.76% recorded in term babies in India by Mehta et al.25 although both studies used different cutoff values in determining FM.25,27,30
It is interesting to note that not all babies classified as malnourished by anthropometry were found malnourished by CAN score and vice versa. The present study, like others in the literature, had also shown that CAN score identified more babies with FM compared to anthropometry making it a reliable tool in the detection of FM.
CONCLUSION
We concluded that the newborn baby with FM is a high-risk newborn and his postnatal survival greatly depends on careful observation and documentation of the evidence of his adverse intrauterine life and a proactive management of his anticipated complications. A simple and easy way of identifying FM at birth is ideal and will make for judicious use of scarce resources in developing countries. The different anthropometric indices measure different aspects of the well-being of a newborn while CAN score measures the visible wasting observed in malnourished newborn. All the parameters, in one-way or the other, reflect the adverse intrauterine nutrition these newborns suffered. Therefore, the use of multiple methods of determining FM will increase the likelihood of identification of most babies with FM. The combination of CAN score and BMI to the routine assessment of newborns at birth may further improve newborn care and buttress the need to look out for these high-risk babies for anticipatory care and follow-up.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Scott KE, Usher R. Fetal malnutrition: Its incidence, causes, and effects. Am J Obstet Gynecol. 1966;94:951–63. doi: 10.1016/0002-9378(66)90033-0. [DOI] [PubMed] [Google Scholar]
- 2.Crosby WM. Studies in fetal malnutrition. Am J Dis Child. 1991;145:871–6. doi: 10.1001/archpedi.1991.02160080047019. [DOI] [PubMed] [Google Scholar]
- 3.Adebami OJ, Owa JA, Oyedeji GA, Oyelami OA. Prevalence and problems of foetal malnutrition in term babies at Wesley Guild Hospital, South Western Nigeria. West Afr J Med. 2007;26:278–82. doi: 10.4314/wajm.v26i4.28327. [DOI] [PubMed] [Google Scholar]
- 4.Metcoff J. Clinical assessment of nutritional status at birth. Fetal malnutrition and SGA are not synonymous. Pediatr Clin North Am. 1994;41:875–91. doi: 10.1016/s0031-3955(16)38836-8. [DOI] [PubMed] [Google Scholar]
- 5.Barker DJ, Gluckman PD, Godfrey KM, Harding JE, Owens JA, Robinson JS. Fetal nutrition and cardiovascular disease in adult life. Lancet. 1993;341:938–41. doi: 10.1016/0140-6736(93)91224-a. [DOI] [PubMed] [Google Scholar]
- 6.Barker DJ. Fetal origins of coronary heart disease. Br Heart J. 1993;69:195–6. doi: 10.1136/hrt.69.3.195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Latha N, Nair MK, Chacko DS. Markers of fetal onset adult diseases. Review article. Indian Pediatr. 2009;46:548–54. [PubMed] [Google Scholar]
- 8.Adebami OJ, Owa JA. Comparison between CANSCORE and other anthropometric indicators in fetal malnutrition. Indian J Pediatr. 2008;75:439–42. doi: 10.1007/s12098-008-0069-7. [DOI] [PubMed] [Google Scholar]
- 9.Sankhyan N, Sharma VK, Singh S. Detection of fetal malnutrition using “CAN score”. Indian J Pediatr. 2009;76:903–6. doi: 10.1007/s12098-009-0196-9. [DOI] [PubMed] [Google Scholar]
- 10.Roje D, Banovic I, Tadin I, Vucinovic M, Capkun V, Barisic A, et al. Gestational age – The most important factor of neonatal ponderal index. Yonsei Med J. 2004;45:273–80. doi: 10.3349/ymj.2004.45.2.273. [DOI] [PubMed] [Google Scholar]
- 11.Sasanow SR, Georgieff MK, Pereira GR. Mid-arm circumference and mid-arm/head circumference ratios: Standard curves for anthropometric assessment of neonatal nutritional status. J Pediatr. 1986;109:311–5. doi: 10.1016/s0022-3476(86)80393-6. [DOI] [PubMed] [Google Scholar]
- 12.Eregie CO. Arm/head ratio in the nutritional evaluation of newborn infants: A report of an African population. Ann Trop Paediatr. 1992;12:195–202. doi: 10.1080/02724936.1992.11747568. [DOI] [PubMed] [Google Scholar]
- 13.Olowe SA. Standards of intrauterine growth for an African population at sea level. J Pediatr. 1981;99:489–95. doi: 10.1016/s0022-3476(81)80358-7. [DOI] [PubMed] [Google Scholar]
- 14.Fang S. Management of preterm infants with intrauterine growth restriction. Early Hum Dev. 2005;81:889–900. doi: 10.1016/j.earlhumdev.2005.09.004. [DOI] [PubMed] [Google Scholar]
- 15.Carrera JM, Devesa R, Salvador J. Aetiology and pathogenesis of intrauterine growth restriction. In: Kurjak A, editor. Textbook of Perinatal Medicine. London: Parthenon Publishing; 1998. pp. 1171–91. [Google Scholar]
- 16.World Health Organization. The newborn infant. WHO Physical Status: The Use and Interpretation of Anthropometry. Report of a WHO Expert Committee. WHO Technical Report Series. 1995;854:121–58. [PubMed] [Google Scholar]
- 17.10th Revision. Geneva: World Health Organization; 1992. World Health Organization. International Statistical Classification of Diseases and Related Health Problems. [Google Scholar]
- 18.Brock RS, Falcão MC, Leone C. Body mass index values for newborns according to gestational age. Nutr Hosp. 2008;23:487–92. [PubMed] [Google Scholar]
- 19.Ashworth A. Effects of intrauterine growth retardation on mortality and morbidity in infants and young children. Eur J Clin Nutr. 1998;52(Suppl 1):S34–41. [PubMed] [Google Scholar]
- 20.Adebami OJ, Owa JA, Oyedeji GA, Oyelami OA, Omoniyi-Esan GO. Associations between placental and cord blood malaria infection and fetal malnutrition in an area of malaria holoendemicity. Am J Trop Med Hyg. 2007;77:209–13. [PubMed] [Google Scholar]
- 21.Crosby WM. Studies in fetal malnutrition. Am J Dis Child. 1991;145:871–6. doi: 10.1001/archpedi.1991.02160080047019. [DOI] [PubMed] [Google Scholar]
- 22.Anderson MS, Hay WW., Jr . Intrauterine growth restriction and the small for gestational age infant. In: Avery GB, Fletcher MS, MacDonald MG, editors. Neonatology. 6th ed. Philadelphia, PA: Lippincott Williams and Wilkins; 2006. [Google Scholar]
- 23.Hussain K, Aynsley-Green A. The effect of prematurity and intrauterine growth restriction on glucose metabolism in the newborn. Neoreviews. 2004;5:e365–8. [Google Scholar]
- 24.Yilgwan CS, Abok II, Yinnang WD, Vajime BA. Prevalence and Risk Factors of Low Birth Weight in Jos. [Last accessed on 2015 Aug 29]. Available from: http://www.ajol.info/indexhp/um/articleviewfile/55095/43568 .
- 25.Mehta S, Tandon A, Dua T, Kumari S, Singh SK. Clinical assessment of nutritional status at birth. Indian Pediatr. 1998;35:423–8. [PubMed] [Google Scholar]
- 26.Korkmaz A, Teksam O, Yurdakök M, Yigit S, Tekinalp G. Fetal malnutrition and its impacts on neonatal outcome in preterm infants. Turk J Pediatr. 2011;53:261–8. [PubMed] [Google Scholar]
- 27.Kashyap L, Dwivedi R. Detection of fetal malnutrition by CAN score at birth and its comparison with other methods of determining intrauterine growth. Pediatr Oncall. 2006;1:3–5. [Google Scholar]
- 28.Owa JA, Adebami JO. Looking for the best indicator of fetal malnutrition: An overview. Internet J Nutr Wellness. 2007;3:12–6. [Google Scholar]
- 29.Soundarya M, Basavaprabhu A, Raghuveera K, Baliga B, Shivanagaraja B. Comparative assessment of fetal malnutrition by anthropometry and CAN score. Iran J Pediatr. 2012;22:70–6. [PMC free article] [PubMed] [Google Scholar]
- 30.Eregie CO. Mid-arm Circumference/Head Circumference Ratio: An Intrauterine Growth Standard for the Assessment of Nutritional Status in Nigerian Newborn Infants. A Dissertation Submitted to the National Postgraduate Medical College of Nigeria in Partial Fulfilment of the Requirement for the Fellowship of the College. 1988 Nov [Google Scholar]


