Abstract
Background:
Intertrochanteric femur fractures are elderly is very common and can be treated by different fixation methods such as internal fixation and arthroplasty. In our study, we investigated the correlation between the hemiarthroplasty treatment method and functional results.
Materials and Methods:
The study consists of 121 patients with intertrochanteric fractures and these patients are divided into three groups. Eighty-five were male and 36 were female. Group I was uncemented bipolar hemiarthroplasty patients, Group II was cemented bipolar hemiarthroplasty and Group III was cemented calcar preserving bipolar hemiarthroplasty. Mean follow-up period was 16 months. Harris hip score was used to evaluate functional outcome of the patients.
Results:
There were no significant differences between three groups when comparing the mortality rate in the 1st month and 1st year but all time mortality was proportionally lower in Group I comparing to the two other groups. There were no significant differences between three groups when comparing the functional results in 1st month and 1st year.
Conclusion:
In our study, uncemented bipolar hemiarthroplasty is a preferable treatment over the two other arthroplasty treatment model (cemented bipolar and calcar preserving) regarding to the mortality rate since there is no significant difference between. This conclusion needs further studies with greater number of patients.
Keywords: Bone cement, complications, hemiarthroplasty, unstable intertrchanteric fracture
INTRODUCTION
In geriatric population, fall is the leading cause of injuries and hospital admission.1 Forty-five percent of all hip fractures are intertrochanteric fractures, and 35–40% of these fractures are unstable three or four part fractures and associated with high rates of morbidity and mortality.2,3
Due to difficulty in obtaining anatomical reduction, treatment of the unstable intertrochanteric fractures in elderly patients is challenging and controversial.4,5
Osteoporosis and instability are the most important factors preventing early weight bearing and leading to unsatisfactory results in these cases.5,6,7 Over the years, osteosynthesis has been indicated as the preferable treatment for stable intertrochanteric fractures and has shown promising results, but high rate of mortality render this option impractical in unstable intertrochanteric fracture cases.8 As a result, primary cemented bipolar hemiarthroplasty has emerged as a valid choice for treatment of unstable intertrochanteric fractures and has shown promising results with fewer complications.
In addition, early mobilization in elderly is crucial because of additional problems.
With this background, in this study, the results of intertrochanteric fractures including uncemented bipolar hemiarthroplasty, cemented bipolar hemiarthroplasty, and calcar preserving cemented bipolar hemiarthroplasty were compared.
MATERIALS AND METHODS
Local ethical committee approval is obtained for the study. The list of the patients with unstable intertrochanteric femur fractures treated by bipolar hemiarthroplasty between March 2010 and November 2014 is obtained from the local data system. AO/OTA type 31-A1 and A2 fractures are included. Unipolar hemiarthroplasties and total hip replacements were excluded. Age, gender, time of death, Harris hip scores,9 and postoperative follow-up periods were the parameters of the study. Patients were divided into three groups: Uncemented bipolar hemiarthroplasty (Group I), cemented bipolar hemiarthroplasty (Group II) and cemented calcar preserving bipolar hemiarthroplasty (Group III) [Figure 1].
Figure 1.
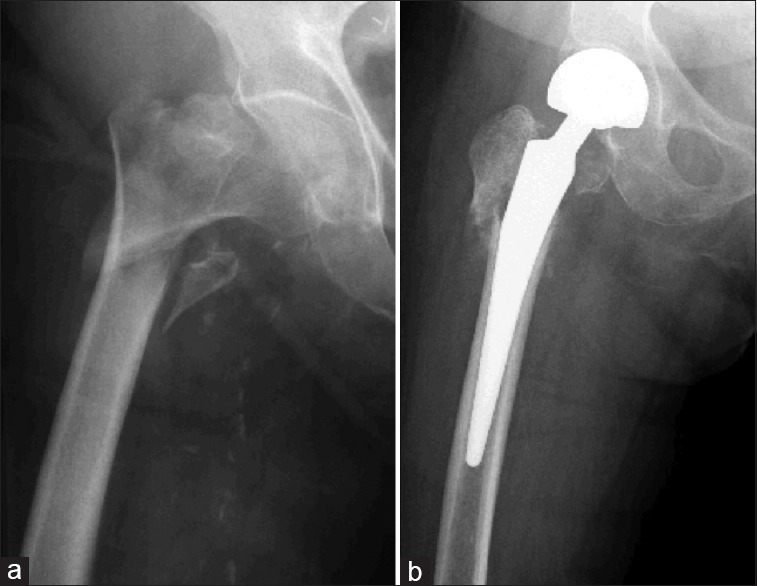
78-year-old female patient, unstable intertrochanteric femur fracture due to fall (a) → the figure on the left, treated by uncemented hemiarthroplasty (b) → the figure on the right
The study consists of 121 patients. Eighty-five were female, and 36 were male. Ninety-seven of patients were operated under spinal anesthesia, and 24 of patients were operated under general anesthesia. All of the patients were operated in lateral decubitus position with modified Gibson approach.10 Extra fixation of the neck and trochanter minor was discarded (such as trochanteric grip and cable). Standard reaming of the femoral stem was done in coherence with prosthesis brand. On the second postoperative day, all drains were removed, and ambulation with full weight bearing with the aid of a walker was started.
Mean follow-up period was 16 months (13–38) in Group I, 22 months (12–48) in Group II and 24 months (12–48) in Group III. Five patients had an infection around the surgical area (two in Group II, three in Group III). Two of the infected patients has been treated by debridement and lavage, and the three others had two-stage revision. Figure 2 two patients in Group III had one-step revision due to aseptic loosening. Two hip dislocations were observed in Group III, none in others.
Figure 2.
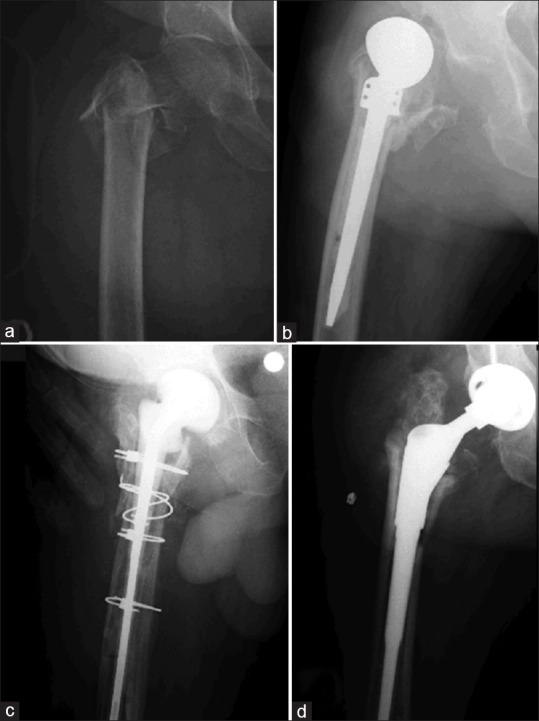
81-year-old male patient, treated by cemented hemiarthroplasty (a), 9 months later, he is infected, and the hip is dislocated (b) thus, the prosthesis is removed, and antibiotic covered spacer is placed into the femur (c). Finally, he is treated with total hip arthroplasty with long femoral stem (d)
Postoperative mortality was classified as in a 1st month and 1st year.
Statistical analysis
The data were analyzed via The statistical software package SPSS version 21 (IBM Corp. Released 2014. IBM SPSS Statistics for Windows, USA). The normality test of the data was analyzed via Shapiro–Wilk. The independent sample test, one-way variance analysis were used in the comparison of the parameters which are normally distributed. Mann–Whitney U-test was used in the comparison of the data that are not normally distributed. Two ratio tests were used in the comparison of the ratios. The results were presented as arithmetic mean, standard deviation, median (minimum–maximum). The significance level was P < 0.05.
RESULTS
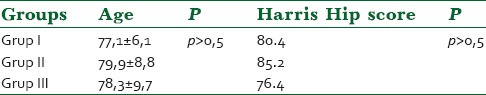
There was no significant difference between mean age of patients with intertrochanteric fracture treated by hemiarthroplasty in all three groups [Table 1].
Table 1.
Median age of the groups and Harris hip score
Aseptic loosening and infection were not observed in Group I. One patient in Group II and two patients in Group III had one stage revision surgery due to aseptic loosening. One patient in Group II and one patient in Group III had a two-stage revision due to infection. Two dislocations were seen in Group III.
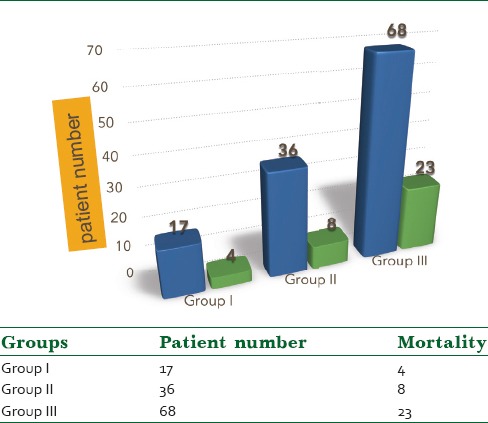
There was no statistically significant difference on groups mortality rate; however, postoperative mortality rate in Group I was lower. All time mortality was proportionally lower in Group I comparing to the other two groups [Table 2].
Table 2.
All time mortality of groups comparison
Harris hip score was 80.4, 85.2, 76.4, respectively in Group I, II, III. There was no significant difference between three groups in term of functional results.
DISCUSSION
There is still no consensus on the best treatment method for unstable intertrochanteric fractures and fixation materials.11 Although the internal fixation of the unstable intertrochanteric femur fractures was the first choice of treatment for years, the improvements in prosthesis design makes hemiarthroplasty treatment a considerable method in elderly. There are several internal fixation methods such as dynamic hip screw and proximal femoral nail for the treatment of unstable intertrochanteric fractures.12,13 In addition, early mobilization is of particular importance for these patients as it might decrease the risk of mortality and morbidity. Younger age, the absence of co-morbidities and presence of patient's cooperation are good prognostic factors.
In the past, Haentjens et al. investigated the clinical outcomes of internal fixation compared with bipolar hemiarthroplasty and reported 75% satisfactory results and fewer postoperative complications in the arthroplasty group.14 They insisted that early weight bearing was the major factor responsible for decreasing postoperative complications. Delay in surgery has a correlation with mortality rate.
Due to the risk of fixation failure or nonunion in elderly and the subsequent need to revise to cemented hemiarthroplasty and the risk of cement-related fatal cardiovascular complications; uncemented hemiarthroplasty is a preferable treatment. They require shorter operation times and are associated with less intraoperative blood loss and also the cement-related complications are avoided.15
The lower mortality rate in Group I in the 1st month can be explained by the uncemented stems since the absence of cement causes no fatal complication.
Hemiarthroplasty is also a preferable treatment modality for other types of proximal femur fractures (such as neck) in elderly patients above 60 years.16
Andress et al., showed adequate osteointegration of the implant, supporting the conclusion that an uncemented prosthesis can be used successfully to treat complex, unstable intertrochanteric fractures.17
Regarding to the current literature, there are studies, which suggest the uncemented endoprosthesis as a better treatment comparing to the cemented hemiarthroplasty. Up to the study of Ng and Krishna cementless hemiarthroplasty is preferred over cemented hemiarthroplasty because of reduced operating time and intraoperative blood loss.18
Uncemented hemiarthroplasty has higher overall survival compared to cemented endoprostheses. Survival to aseptic loosening is superior in uncemented hemiarthroplasty patient group than the cemented hemiarthroplasty group.19 Stem fixation is the only significant variable for survival according to the study of Pala et al.20
No infection or aseptic loosening was observed in Group I while five patients in Group II and III had a revision surgery due to aseptic loosening or infection. Thus, uncemented stems are preferable in this regard. Infection or aseptic loosening are most likely seen in cemented stems.
Many studies have reported that postfracture mortality is increased during the 1st year and then decreases gradually over time.21
Retaining of lesser trochanter and reconstruction of femoral calcar are important for improving periprosthetic biomechanics and reducing local complications.22 In the long-term, union in calcar region and osteointegration of the prosthesis increases the survival term of the prosthesis. Moreover, the torque of the iliopsoas muscles which inserts to lesser trochanter allows the continuity of the muscle function around the hip.11 However, calcar replacement is a technically demanding procedure.2 Stable fixation of the posteromedial fragment is also necessary to avoid the femoral stem subsidence. Patients with intertrochanteric fracture, which were fixated by plate and screws were excluded from the study.
There are few published studies in treatment of unstable intertrochanteric fractures with total hip arthroplasty. Comparing bipolar hemiarthroplasty to total hip replacement, the authors reported the superiority of total hip replacement in terms of control of pain, however, they also highlighted certain drawbacks of total hip replacement arthroplasty in elderly patients such as instability, impaired reflexes, cognitive impairment, and higher dislocation rates.23 In our daily practice, total hip replacement in active elderly patients is a good choice of treatment, otherwise bipolar hemiarthroplasty is the leading treatment when low survival rate is expected. The dislocation rate also is lower in bipolar hemiarthroplasty group comparing to total hip replacement. Even though total hip replacement is superior comparing to hemiarthroplasty in term of acetabular erosion, dislocation rate is lower in hemiarthroplasty patients.23
There were only two dislocations in our study that can be explained by this mechanism.
The retrospective design, number of patients and the short follow-up period can be considered as the limitations of our study.
CONCLUSION
Although the internal fixation is a good treatment method in younger active patients, early weight bearing in elderly patients highlights arthroplasty as a good method of treatment.
With improvements on the implant design, uncemented stems may be preferred by the surgeon after the intraoperative assessment. Thus, cement related complications will be avoided.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82:1020–3. doi: 10.2105/ajph.82.7.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grimsrud C, Monzon RJ, Richman J, Ries MD. Cemented hip arthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fractures. J Arthroplasty. 2005;20:337–43. doi: 10.1016/j.arth.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 3.Sidhu AS, Singh AP, Singh AP, Singh S. Total hip replacement as primary treatment of unstable intertrochanteric fractures in elderly patients. Int Orthop. 2010;34:789–92. doi: 10.1007/s00264-009-0826-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, et al. Fracture and dislocation classification compendium – 2007: Orthopaedic trauma association classification, database and outcomes committee. J Orthop Trauma. 2007;21(10 Suppl):S1–133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 5.Sancheti KH, Sancheti P, Shyam A, Patil S, Dhariwal Q, Joshi R. Primary hemiarthroplasty for unstable osteoporotic intertrochanteric fractures in the elderly: A retrospective case series. Indian J Orthop. 2010;44:428–34. doi: 10.4103/0019-5413.67122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim WY, Han CH, Park JI, Kim JY. Failure of intertrochanteric fracture fixation with a dynamic hip screw in relation to pre-operative fracture stability and osteoporosis. Int Orthop. 2001;25:360–2. doi: 10.1007/s002640100287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Geiger F, Zimmermann-Stenzel M, Heisel C, Lehner B, Daecke W. Trochanteric fractures in the elderly: The influence of primary hip arthroplasty on 1-year mortality. Arch Orthop Trauma Surg. 2007;127:959–66. doi: 10.1007/s00402-007-0423-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh S, Shrivastava C, Kumar S. Hemi replacement arthroplasty for unstable inter-trochanteric fractures of femur. J Clin Diagn Res. 2014;8:LC01–4. doi: 10.7860/JCDR/2014/10171.4972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–55. [PubMed] [Google Scholar]
- 10.Moed BR. The modified gibson posterior surgical approach to the acetabulum. J Orthop Trauma. 2010;24:315–22. doi: 10.1097/BOT.0b013e3181c4aef8. [DOI] [PubMed] [Google Scholar]
- 11.Celiktas M, Togrul E, Kose O. Calcar preservation arthroplasty for unstable intertrochanteric femoral fractures in elderly. Clin Orthop Surg. 2015;7:436–42. doi: 10.4055/cios.2015.7.4.436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdulkareem IH. A review of tip apex distance in dynamic hip screw fixation of osteoporotic hip fractures. Niger Med J. 2012;53:184–91. doi: 10.4103/0300-1652.107550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Uzer G, Elmadag NM, Yildiz F, Bilsel K, Erden T, Toprak H. Comparison of two types of proximal femoral hails in the treatment of intertrochanteric femur fractures. Ulus Travma Acil Cerrahi Derg. 2015;21:385–91. doi: 10.5505/tjtes.2015.72173. [DOI] [PubMed] [Google Scholar]
- 14.Haentjens P, Casteleyn PP, De Boeck H, Handelberg F, Opdecam P. Treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Primary bipolar arthroplasty compared with internal fixation. J Bone Joint Surg Am. 1989;71:1214–25. [PubMed] [Google Scholar]
- 15.Yli-Kyyny T, Ojanperä J, Venesmaa P, Kettunen J, Miettinen H, Salo J, et al. Perioperative complications after cemented or uncemented hemiarthroplasty in hip fracture patients. Scand J Surg. 2013;102:124–8. doi: 10.1177/1457496913482249. [DOI] [PubMed] [Google Scholar]
- 16.Daniel M, Mohammed S, Francis A, William Y, Joseph K, Cornilius E. Early result of hemiarthroplasty in elderly patients with fracture neck of femur. Niger Med J. 2015;56:64–8. doi: 10.4103/0300-1652.149174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Andress HJ, von Rückmann B, Zwönitzer R, Kahl S, Ringling M, Lob G. Changes in bone density of the femur after cement-free implantation of a modular hip prosthesis with a long shaft. Unfallchirurg. 2001;104:622–8. doi: 10.1007/s001130170093. [DOI] [PubMed] [Google Scholar]
- 18.Ng ZD, Krishna L. Cemented versus cementless hemiarthroplasty for femoral neck fractures in the elderly. J Orthop Surg (Hong Kong) 2014;22:186–9. doi: 10.1177/230949901402200214. [DOI] [PubMed] [Google Scholar]
- 19.Wechter J, Comfort TK, Tatman P, Mehle S, Gioe TJ. Improved survival of uncemented versus cemented femoral stems in patients aged <70 years in a community total joint registry. Clin Orthop Relat Res. 2013;471:3588–95. doi: 10.1007/s11999-013-3182-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pala E, Mavrogenis AF, Angelini A, Henderson ER, Douglas Letson G, Ruggieri P. Cemented versus cementless endoprostheses for lower limb salvage surgery. J BUON. 2013;18:496–503. [PubMed] [Google Scholar]
- 21.Vestergaard P, Rejnmark L, Mosekilde L. Has mortality after a hip fracture increased? J Am Geriatr Soc. 2007;55:1720–6. doi: 10.1111/j.1532-5415.2007.01420.x. [DOI] [PubMed] [Google Scholar]
- 22.Bao NR, Zhao JN, Zhou LW, Zeng XF, Guo T. Complications of bipolar hemiarthroplasty for the treatment of unstable intertrochanteric fractures in the elderly. Zhongguo Gu Shang. 2010;23:329–31. [PubMed] [Google Scholar]
- 23.Fan L, Dang X, Wang K. Comparison between bipolar hemiarthroplasty and total hip arthroplasty for unstable intertrochanteric fractures in elderly osteoporotic patients. PLoS One. 2012;7:e39531. doi: 10.1371/journal.pone.0039531. [DOI] [PMC free article] [PubMed] [Google Scholar]


