To the Editor:
Each year, more than 1.5 million Americans are found to have a pulmonary nodule (1). As lung cancer screening becomes prevalent, still more nodules will be identified. Whether detected incidentally or through screening, guidelines recommend evaluating pulmonary nodules in a timely fashion to identify the subset that are malignant. Yet patients with pulmonary nodules often do not receive appropriate evaluation, seemingly “falling through the cracks” (2, 3). Systems-level structures and processes of care have been proposed to facilitate appropriate, efficient nodule evaluation (4–8), and indeed, clinicians have indicated that such system-level resources are essential to avoid loss to follow-up (9). However, the degree to which these structures and processes of care have been implemented nationally is unclear, and the American Thoracic Society (ATS) has called for more research in this area (10). We conducted a survey of ATS clinicians to characterize the availability of system-level resources to facilitate pulmonary nodule evaluation in the United States.
Methods
We surveyed clinician members of the ATS Respiratory Cell and Molecular Biology and Clinical Problems Assemblies (the parent assemblies of the Section of Thoracic Oncology at the time of survey administration). Eligible clinicians included physicians or midlevel providers who regularly saw patients in an outpatient clinic. ATS sent three e-mails in March and April 2014, inviting clinicians to participate in an anonymous online survey, with a $50 incentive for completion. The 32-item survey asked about demographics, practice setting, and practices regarding lung cancer screening and nodule evaluation. The Boston University Institutional Review Board approved this study.
Although this was an international survey, we restricted analysis to responses from U.S. clinicians, given differences in resource availability and practice patterns across countries. Proportions were compared using chi-squared tests, and medians with the Kruskal-Wallis test, with two-sided α < 0.05 as the threshold for statistical significance. All data were analyzed using Stata 10.1 (College Station, TX).
Results
Of 5,872 ATS members with a valid e-mail address, 1,444 opened the survey invitation and 428 eligible clinicians participated (response rate, 7% overall; 30% of those who opened the e-mail). Table 1 shows the characteristics and practice settings of the 320 U.S. respondents.
Table 1.
Respondent Characteristics
| Characteristics | % |
|---|---|
| Male | 74.3 |
| Physician | 99.1 |
| Clinical specialty | |
| Pulmonary/critical care/sleep | 90.5 |
| Primary care/internal medicine | 7.5 |
| Cardiothoracic surgery | 0.9 |
| Radiology | 0.6 |
| Outpatient versus inpatient effort | |
| Exclusively outpatient | 6.0 |
| Mostly outpatient | 49.2 |
| Mostly inpatient | 44.8 |
| Practice type | |
| Academic | 62.2 |
| Community/health maintenance organization/other | 30.0 |
| Department of Veteran Affairs | 7.8 |
| Practice setting | |
| Urban | 69.5 |
| Suburban | 24.8 |
| Rural | 5.7 |
| Practice location | |
| Northeast | 37.8 |
| South | 15.3 |
| Midwest | 27.8 |
| West | 19.1 |
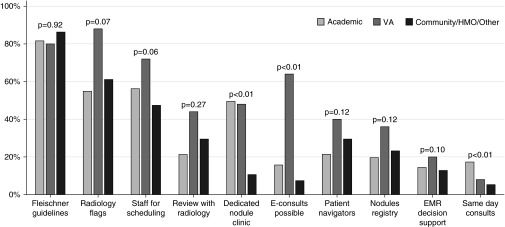
The most common structures and processes of care in place were inclusion of Fleischner Society guidelines in radiology reports (82.7%), flagged prompts to the ordering provider on radiology reports with new nodules (59.4%), and staff members to facilitate nodule evaluation (e.g., scheduling appointments, 55.2%) (Figure 1). Most respondents reported some (median, 3; interquartile range, 2–5) system-level resources to facilitate nodule evaluation. Veterans Affairs (VA) sites tended to have more resources in place, with 88.0% reporting at least three (vs. 69.8% at academic centers and 53.1% at community/health maintenance organization facilities; P < 0.001). There was a broad distribution of reported resources within all groups, however, with 11 respondents (3.5%) reporting no structures or processes of care to facilitate nodule evaluation and eight respondents (2.5%) reporting nine or more system-level resources in place.
Figure 1.
Systems-level resources in place to facilitate pulmonary nodule evaluation. E-consults = electronic consults; EMR = electronic medical record; HMO = health maintenance organization; VA = Veterans Affairs.
When comparing types of facilities, VA sites were significantly more likely to report electronic consults (64.0% VA, 15.7% academic, 7.4% community; P < 0.01; Figure 1). Clinicians in VA and academic settings were significantly more likely to report dedicated pulmonary nodule clinics than community/health maintenance organization physicians (48.0% VA, 49.5% academic, 10.6% community; P < 0.01). Academic settings were significantly more likely to report availability of same-day consults for pulmonary nodules (8.0% VA, 17.3% academic, 5.3% community; P < 0.01).
Discussion
This national survey identifies great variation in the availability of systems-level resources to facilitate pulmonary nodule evaluation across the United States. Although several structures and processes of care have been implemented to facilitate nodule evaluation, particularly in VA sites, only the use of templated reporting including guideline recommendations, radiology flags, and staff for scheduling have diffused to the majority of sites. Hence, at most sites, there is a missed opportunity to ensure patients with pulmonary nodules receive appropriate care. This raises questions about the preparedness of sites to implement comprehensive lung cancer screening programs, as professional societies recommend that screening programs have standardized structures and processes of care in place not only for screening but also for downstream evaluation and treatment of screen-detected nodules (7, 8).
This study has limitations. First, our response rate was relatively low. Moreover, respondents from urban academic centers were disproportionately represented, whereas VA clinicians represented a small minority of respondents. Thus, our results may not be broadly generalizable. Second, this survey was anonymous: We do not know what centers are represented and whether some sites may be represented by more than one respondent. Finally, our survey does not evaluate the actual resources in place or their quality.
The ATS has identified a need for research to establish which structures and processes most effectively improve outcomes of patients with pulmonary nodules so that facilities know how best to invest limited resources (10). As lung cancer screening is implemented, these studies are all the more urgently needed to assure appropriate resources are in place to facilitate pulmonary nodule evaluation. This study provides the first national data on availability of systems-level processes of care to facilitate pulmonary nodule evaluation, which is critical data to inform readiness for widespread implementation of lung cancer screening.
Footnotes
This study was funded by the National Cancer Institute (K07 CA138772) and supported with resources from the Edith Nourse Rogers Memorial Veterans Affairs Hospital and the Veterans Affairs Portland Health Care System. C.G.S. was sponsored by a Veterans Affairs Health Services Research and Development Career Development Award (CDA 09-025 and CDP 11-227).
The views expressed in this manuscript do not necessarily represent the views of the Department of Veterans Affairs or the U.S. Government.
Author Contributions: R.S.W. had full access to the data and takes responsibility for the data integrity and the accuracy of the data analysis. Study concept and design, M.K.G., C.G.S., and R.S.W. Acquisition, analysis, or interpretation of data, J.S. and R.S.W. Drafting of the manuscript, J.S. and R.S.W. Critical revision of the manuscript for important intellectual content, all authors. Statistical analysis, J.S. and R.S.W. Obtaining funding, R.S.W. Study supervision, R.S.W.
Author disclosures are available with the text of this letter at www.atsjournals.org.
References
- 1.Gould MK, Tang T, Liu IL, Lee J, Zheng C, Danforth KN, Kosco AE, Di Fiore JL, Suh DE. Recent trends in the identification of incidental pulmonary nodules. Am J Respir Crit Care Med. 2015;192:1208–1214. doi: 10.1164/rccm.201505-0990OC. [DOI] [PubMed] [Google Scholar]
- 2.Wiener RS, Gould MK, Slatore CG, Fincke BG, Schwartz LM, Woloshin S. Resource use and guideline concordance in evaluation of pulmonary nodules for cancer: too much and too little care. JAMA Intern Med. 2014;174:871–880. doi: 10.1001/jamainternmed.2014.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tanner NT, Aggarwal J, Gould MK, Kearney P, Diette G, Vachani A, Fang KC, Silvestri GA. Management of pulmonary nodules by community pulmonologists: a multicenter observational study. Chest. 2015;148:1405–1414. doi: 10.1378/chest.15-0630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Woloshin S, Schwartz LM, Dann E, Black WC. Using radiology reports to encourage evidence-based practice in the evaluation of small, incidentally detected pulmonary nodules: a preliminary study. Ann Am Thorac Soc. 2014;11:211–214. doi: 10.1513/AnnalsATS.201307-242BC. [DOI] [PubMed] [Google Scholar]
- 5.Hunnibell LS, Slatore CG, Ballard EA. Foundations for lung nodule management for nurse navigators. Clin J Oncol Nurs. 2013;17:525–531. doi: 10.1188/13.CJON.525-531. [DOI] [PubMed] [Google Scholar]
- 6.Alsamarai S, Yao X, Cain HC, Chang BW, Chao HH, Connery DM, Deng Y, Garla VN, Hunnibell LS, Kim AW, et al. The effect of a lung cancer care coordination program on timeliness of care. Clin Lung Cancer. 2013;14:527–534. doi: 10.1016/j.cllc.2013.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Mazzone P, Powell CA, Arenberg D, Bach P, Detterbeck F, Gould MK, Jaklitsch MT, Jett J, Naidich D, Vachani A, et al. Components necessary for high-quality lung cancer screening: American College of Chest Physicians and American Thoracic Society Policy Statement. Chest. 2015;147:295–303. doi: 10.1378/chest.14-2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wiener RS, Gould MK, Arenberg DA, Au DH, Fennig K, Lamb CR, Mazzone PJ, Midthun DE, Napoli M, Ost DE, et al. ATS/ACCP Committee on Low-Dose CT Lung Cancer Screening in Clinical Practice. An official American Thoracic Society/American College of Chest Physicians policy statement: implementation of low-dose computed tomography lung cancer screening programs in clinical practice. Am J Respir Crit Care Med. 2015;192:881–891. doi: 10.1164/rccm.201508-1671ST. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Golden SE, Wiener RS, Sullivan D, Ganzini L, Slatore CG. Primary care providers and a system problem: a qualitative study of clinicians caring for patients with incidental pulmonary nodules. Chest. 2015;148:1422–1429. doi: 10.1378/chest.14-2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Slatore CG, Horeweg N, Jett JR, Midthun DE, Powell CA, Wiener RS, Wisnivesky JP, Gould MK ATS Ad Hoc Committee on Setting a Research Framework for Pulmonary Nodule Evaluation. An Official American Thoracic Society research statement: a research framework for pulmonary nodule evaluation and management. Am J Respir Crit Care Med. 2015;192:500–514. doi: 10.1164/rccm.201506-1082ST. [DOI] [PMC free article] [PubMed] [Google Scholar]