Abstract
Hereditary cancer assessment at the end of life is a relatively unexplored area, but it could be critical for surviving family members. This study explored the prevalence of hereditary cancer among dying cancer patients and assessed patients’ perceived awareness of DNA testing and/or banking in a public access hospital. Palliative care patients with cancer from a single institution (or their medical-decision-making surrogates for patients unable to answer for themselves) completed structured interviews. Information was collected through medical records review and structured interviews for 43 dying cancer patients. Information for 9 patients was collected from surrogates. Nine patients (21%, 95% CI=8.8% to 33.1%) had strong genetic risk. Currently available genetic tests could have addressed this risk for several patients. None had previous genetic counseling, testing or DNA banking. Among strong-risk patients, about half of patients/surrogates had heard/read “almost nothing” about genetic testing (44%) and DNA banking (67%). Perceived genetic awareness was not associated with genetic risk, and neither were sociodemographic characteristics. The proportion of hereditary cancer may be at least as high in the palliative care population as in other clinical settings, but awareness and uptake among patients are low. These conditions are not being recognized upstream and families are losing valuable information.
Keywords: Hereditary, Neoplasm, Cancer, Genetic screening, DNA banking, End of life, Genetic testing, Genetic counseling
Introduction
Identifying patients’ risks and providing personalized prevention recommendations are key goals of cancer genetic counseling and testing (Berliner and Fay 2007). Yet, for dying cancer patients these outcomes are not medically indicated. Instead, it is the familial nature of genetics assessment that may be of value to this population. This attention to genetic legacy is an understudied phenomenon that might be of medical significance to surviving family members, and of personal psychological benefit to dying cancer patients (Lillie 2006; Quillin et al. 2008a; Skirton et al. 2006).
About 5% to 10% of cancers arise in individuals with autosomal dominant cancer susceptibility (Offit 1998; Garber and Offit 2005). Unfortunately, many of these families will not have identifiable genetic markers for their risks by currently available tests. For example, at most, half of families with hereditary breast cancer will test positive for a clinically useful mutation (Wooster and Weber 2003). Thus, without a known mutation in the family, a healthy woman with a strong family history of breast cancer cannot be fully reassured by negative genetic test results, and DNA banking could be more valuable.
Professional guidelines, such as those of the National Comprehensive Cancer Network (2008), can be helpful for identifying newly diagnosed patients for genetics risk assessment. While time of diagnosis represents an important opportunity for this triage, this does not always happen (Fowler et al. 2005; Grover et al. 2004; Shannon et al. 2002). The prevalence of unidentified hereditary cancer among dying cancer patients is unknown. Furthermore, whether these patients are aware of genetic testing for cancer risk or storing a blood sample for future family use (i.e., DNA banking), is unknown. This study aimed to fill these gaps.
The objectives of this study were to: 1) among end-of-life hospitalized oncology patients, estimate the proportion of patients with hereditary cancer risk appropriate for genetic services, and 2) assess perceived awareness of genetic testing and DNA banking among patients likely to have hereditary risk. We hypothesized the proportion of hereditary cancer risk in our sample would be similar to the proportion of hereditary cancer overall in the population (i.e., about 5% to 10%). While it is unlikely that the prevalence of hereditary cancer risk differs in this population, these data are not documented elsewhere in the literature. Identifying the prevalence of hereditary cancer risk in this population, particularly if patients have not had prior genetics evaluation, is a critical step in light of the proposed need for genetic services in this population (e.g., Lillie 2006; Quillin et al. 2008a). Relatedly, we anticipated awareness would be low regarding genetic testing and especially regarding DNA banking. We also wanted to explore any differences in awareness by sociodemographic characteristics.
Methods
We conducted a cross-sectional exploratory study of hereditary cancer among advanced cancer patients, utilizing in-person structured interviews and medical records reviews.
Sample Population and Recruitment
Participant recruitment occurred for about seven months in the spring and summer of 2008 at Virginia Commonwealth University Health System (VCUHS) in downtown Richmond, Virginia. The VCUHS is an academic public-access health system and provides a significant proportion of indigent care for the state. The patient population reflects the Richmond metropolitan area, and about half of the patients are African-American. Eligible participants were adult, English-speaking patients at VCUHS in the palliative care and oncology units with advanced cancer diagnoses. For patients not able to answer questions themselves, their adult medical decision-making surrogates were eligible to participate.
Patient identification, consent, administration of structured interviews, and medical records reviews were conducted by a research assistant. The research assistant had a masters degree in clinical psychology and had previous research experience. Training specific to this project included hospital records review, patient confidentiality, and administration training required at our institution to gain access to hospital electronic medical records. She was further trained through review of a study manual about conducting valid structured research interviews. Concepts were reinforced in training sessions with the Principal Investigator along with interview practice sessions.
Following successful training, the research assistant reviewed hospital admission notes for the palliative care and oncology units daily and selected patients who were either on the palliative care unit because of advanced disease, or because they had been admitted to the oncology service with terminal cancer. The research assistant obtained informed consent from all participants, and the study was approved by the Virginia Commonwealth University Institutional Review Board. If patients were not able, or preferred not, to answer questions for themselves due to their medical condition, their medical decision-making surrogate was invited to participate. Although patients and surrogates likely differ in terms of family history knowledge and attitudes toward genetic testing, for the purposes of this study surrogates’ responses were considered critical, since they are the ones reporting family history and deciding about genetic testing for the patient.
Instrumentation
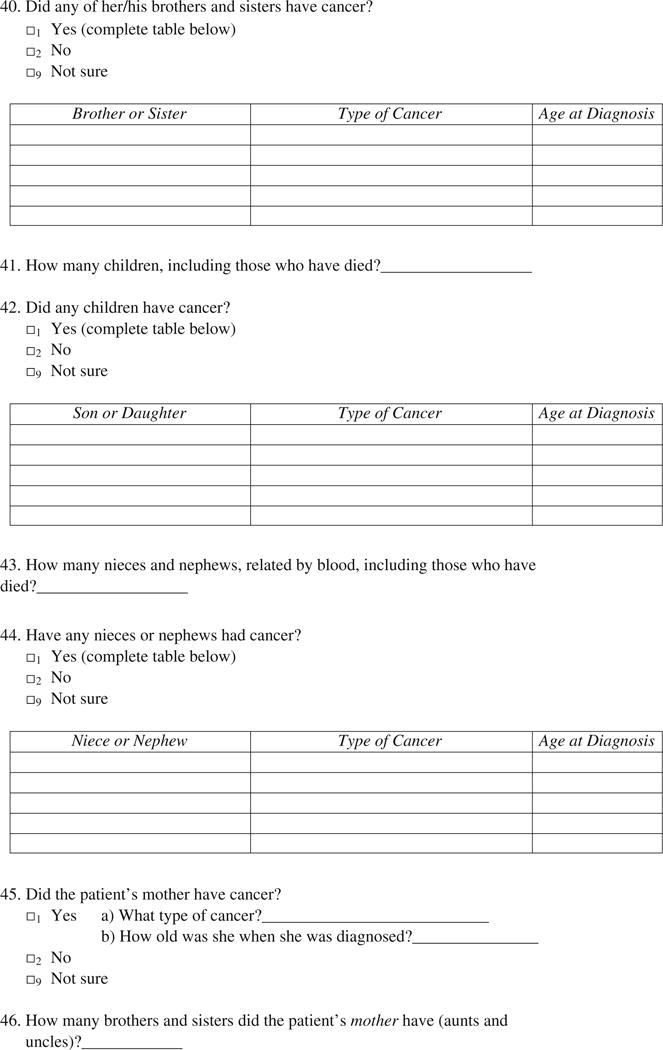
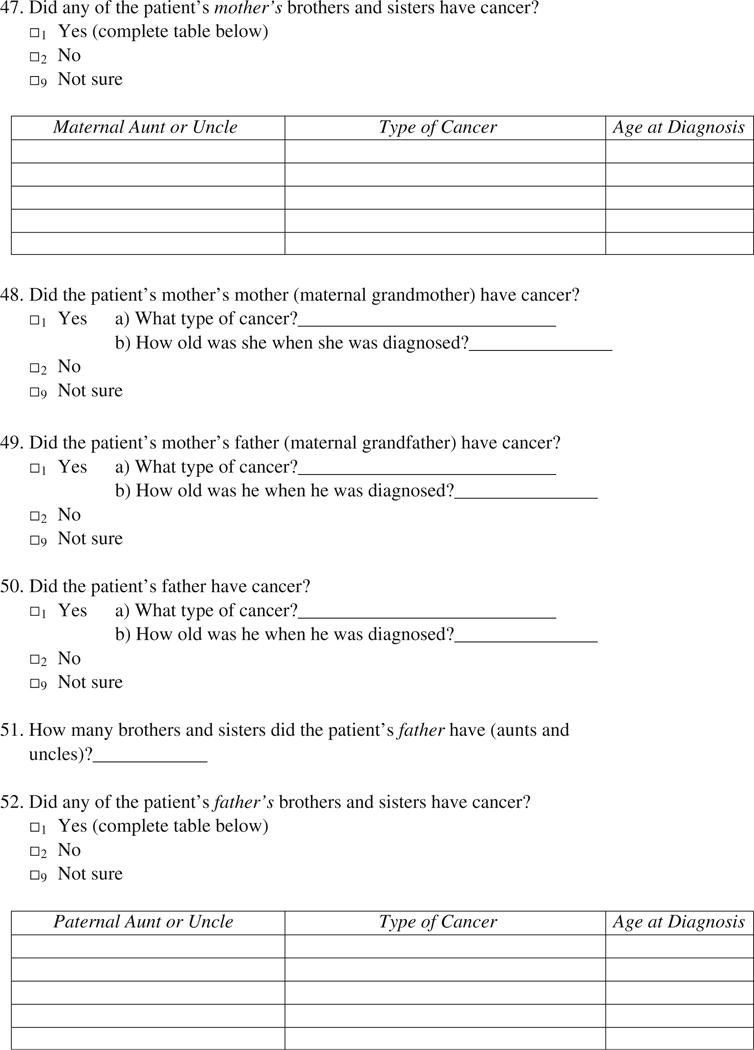
Medical Records
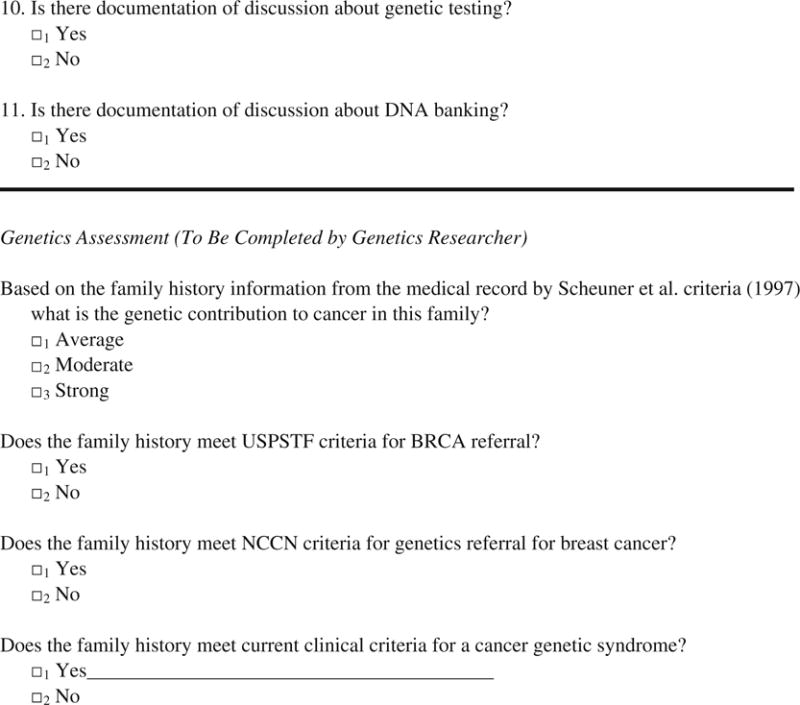
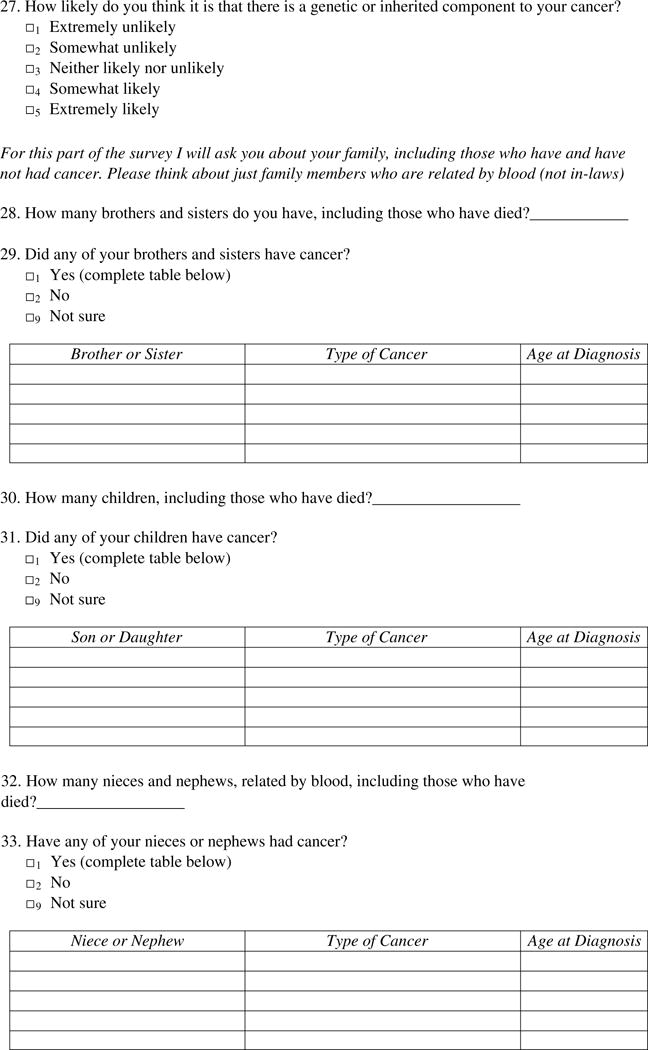
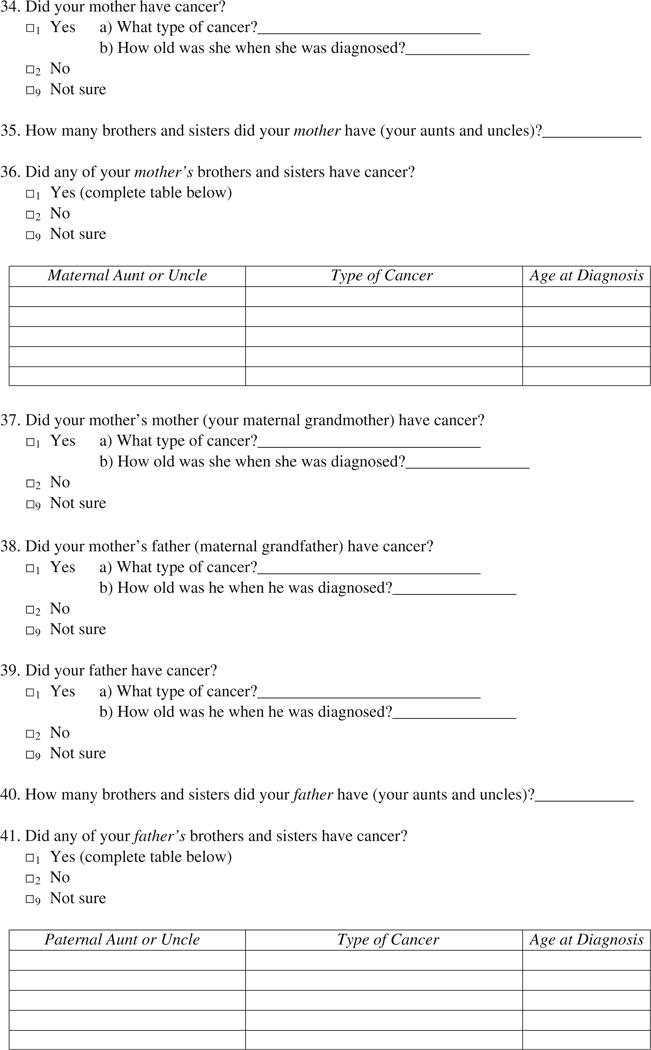
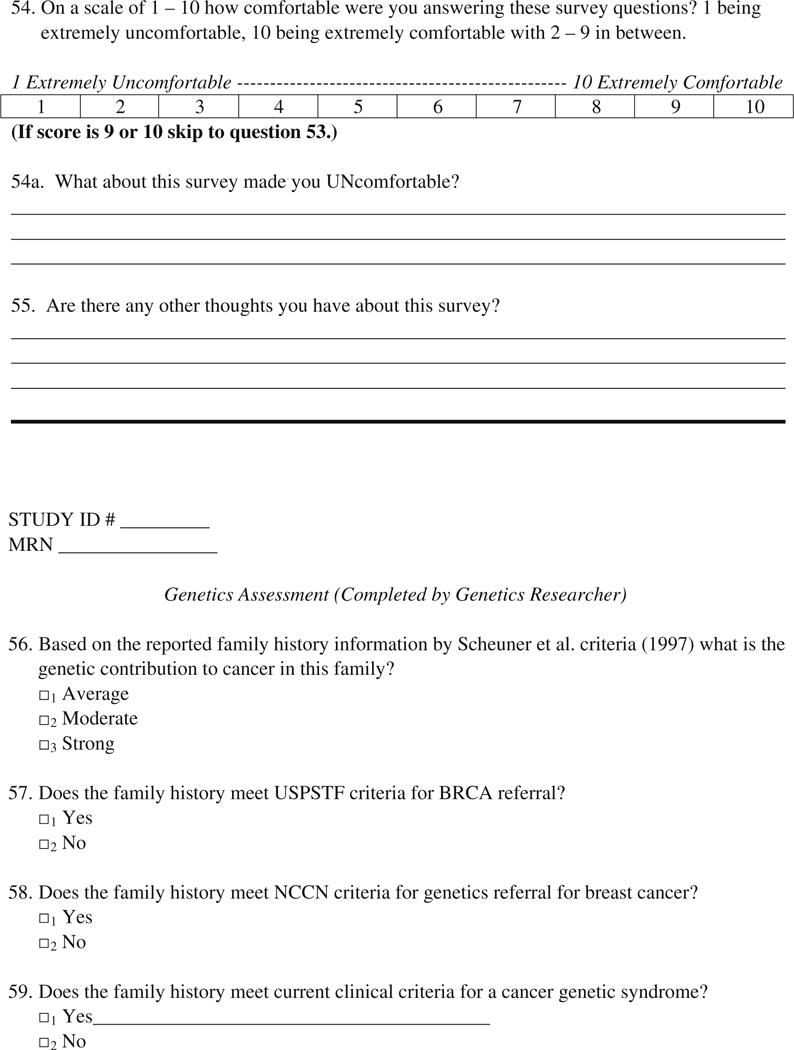
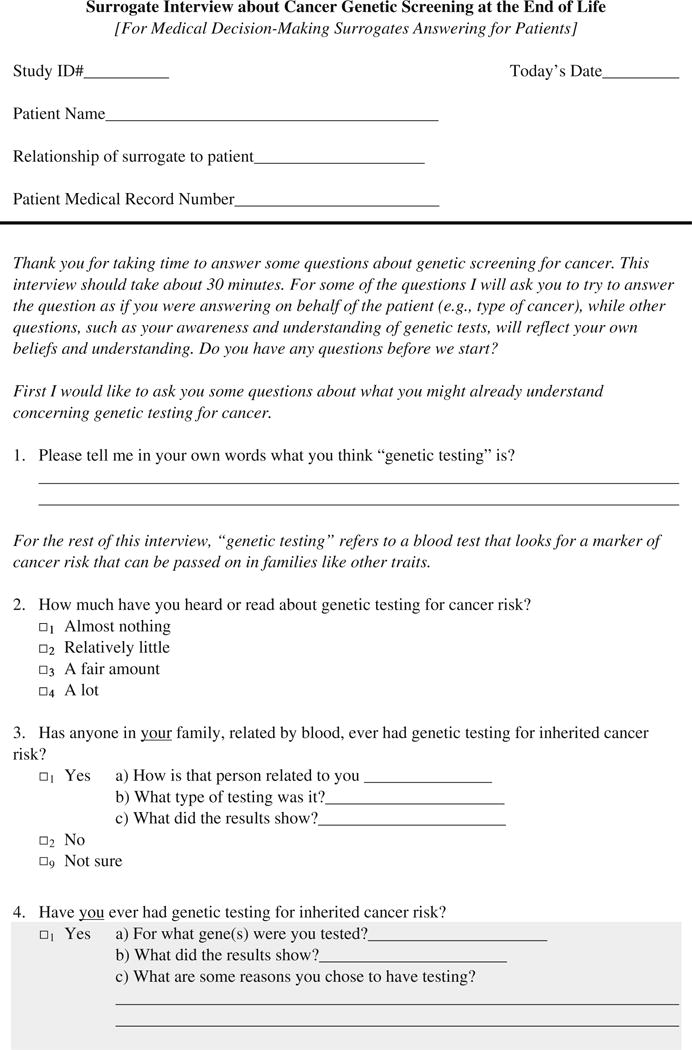
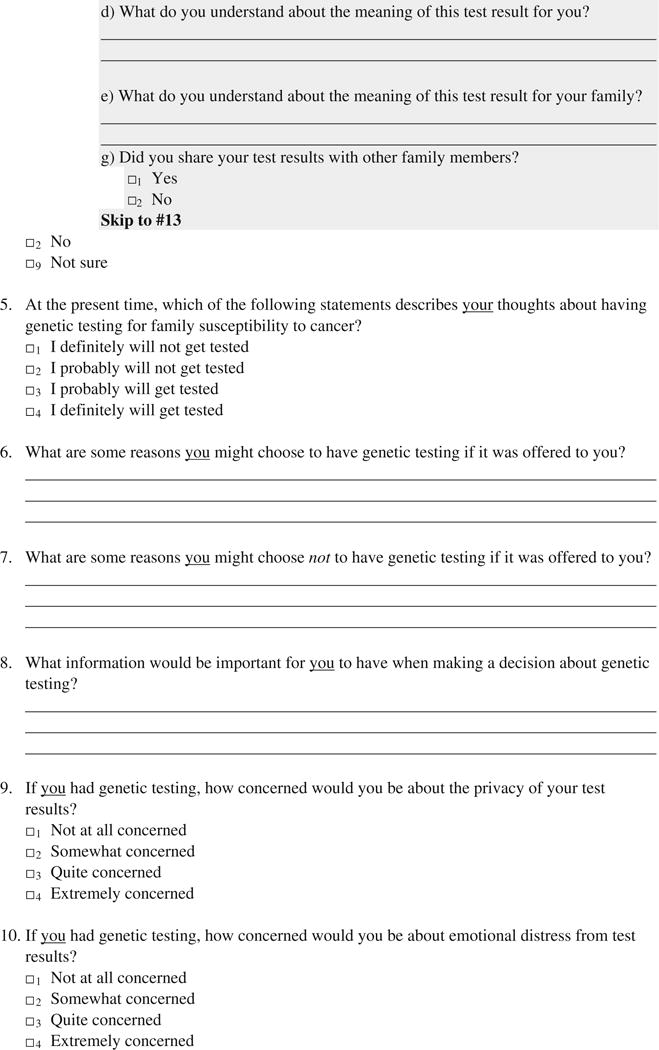
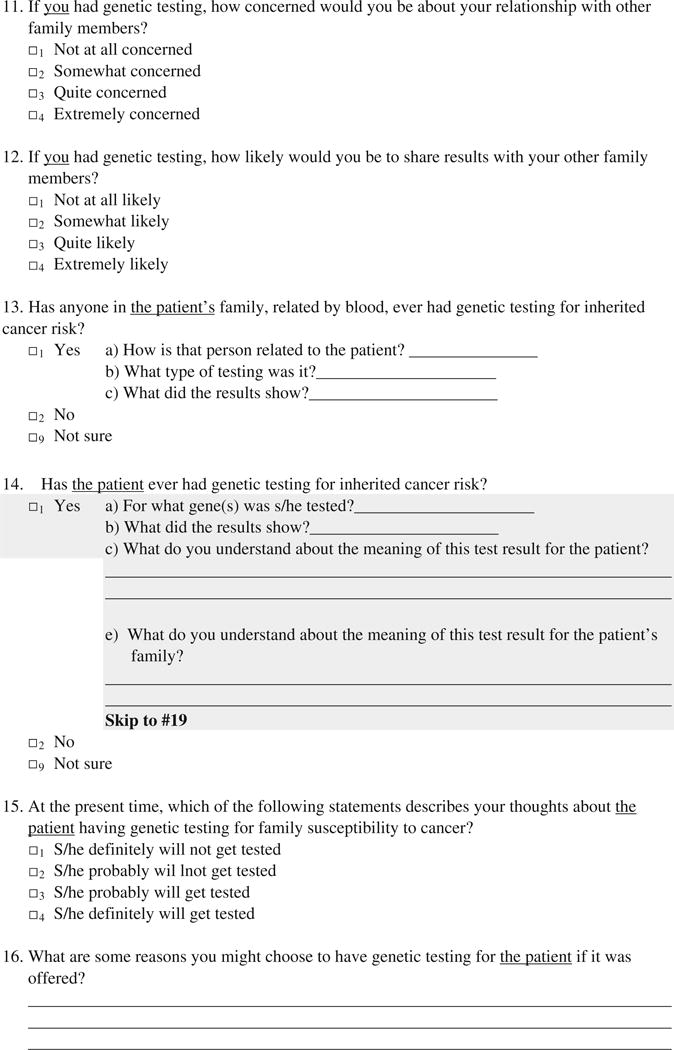
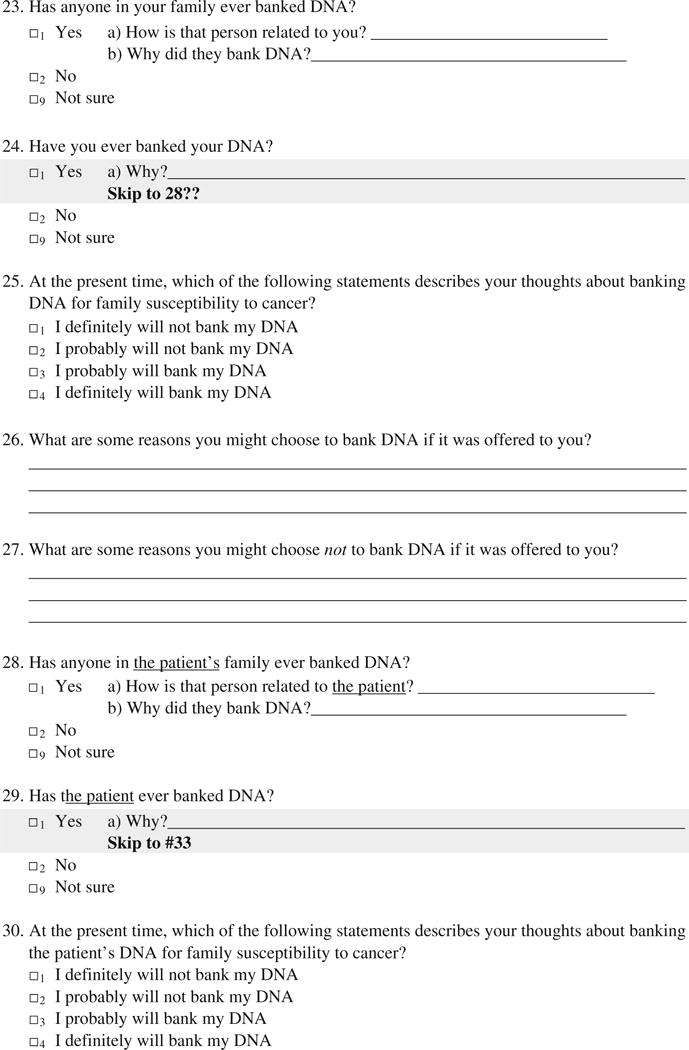
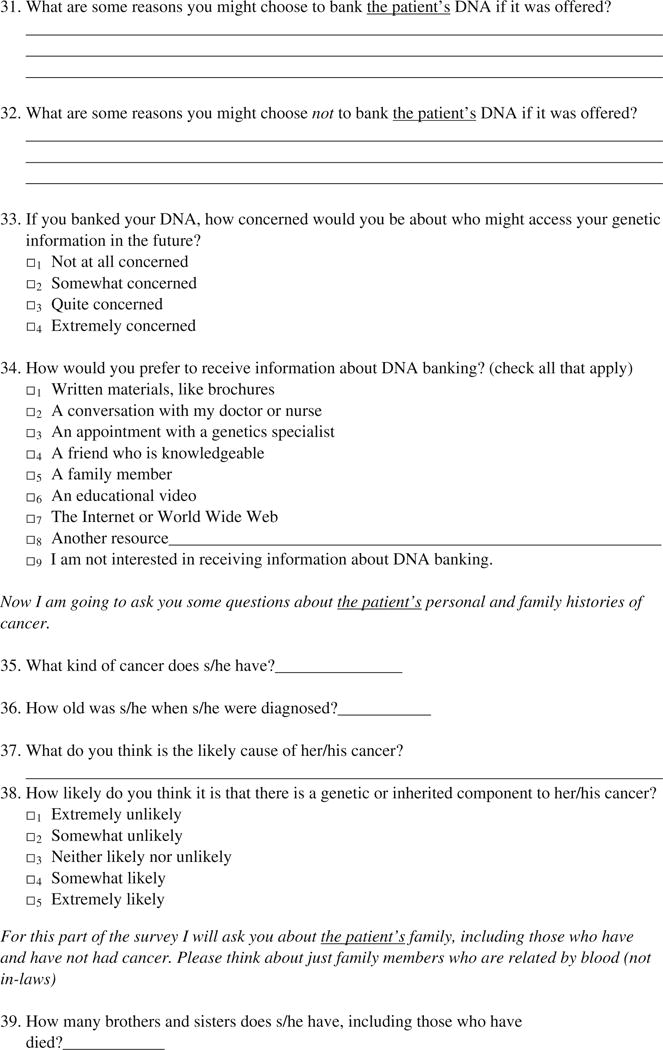
Patient medical records were reviewed by the research assistant using a study-specific data abstraction form (Appendix) to confirm cancer diagnoses and to assess for any previous interaction with genetics services.
Structured Interviews
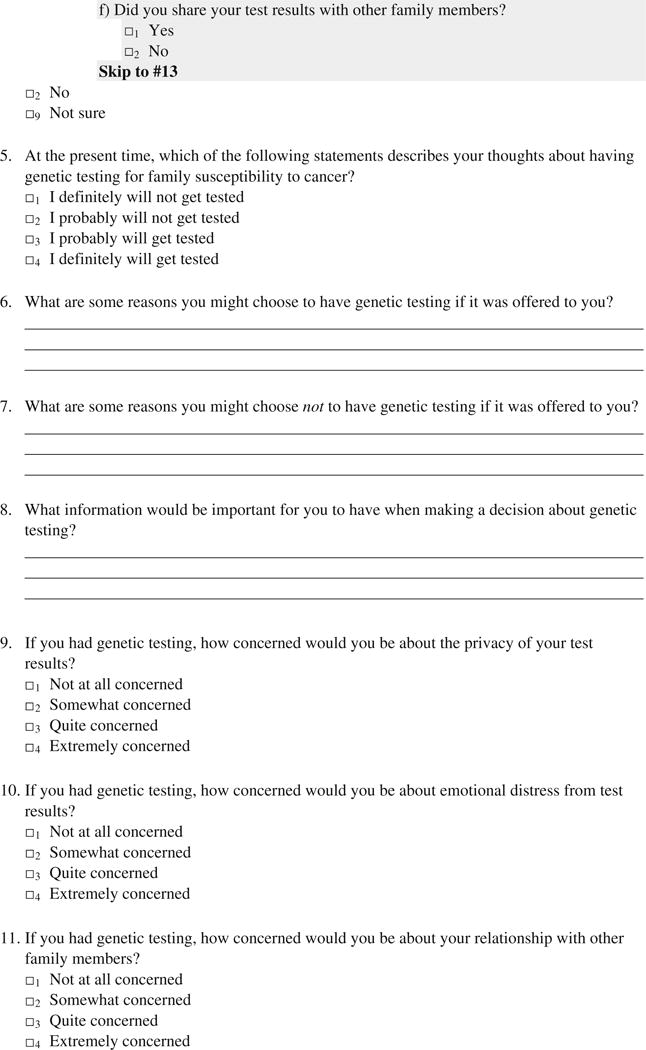
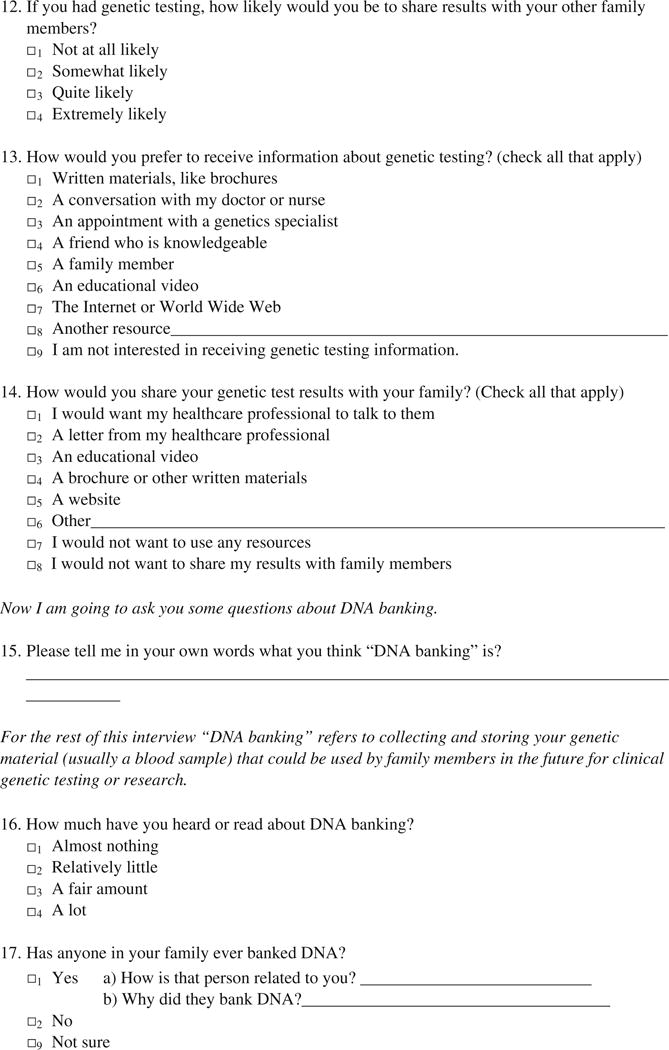
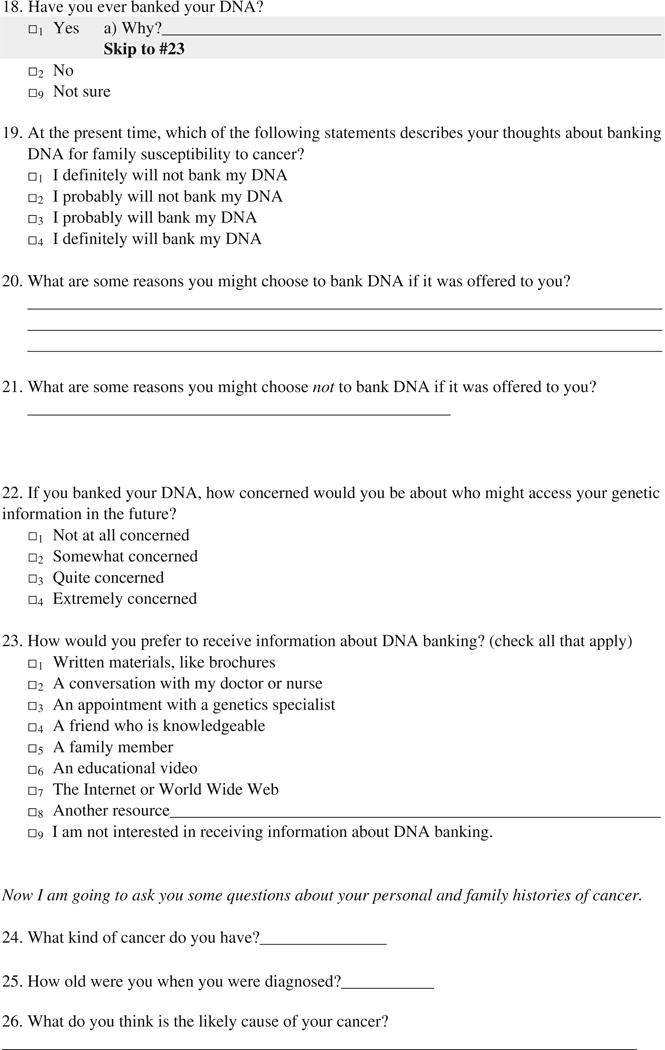
The research assistant verbally administered structured interviews to patients or to the patients’ medical decision-making surrogates. The interview schedules are included in the Appendix. Interviews were anticipated to take 15 to 30 min to complete.
Variables
To estimate the proportion of cancers that appear to have a hereditary component, the primary data were cancer diagnoses (types and ages of onset) for patients and their first- and second-degree relatives, as reported by the participant. Based on this information, patients were classified as having “strong,” or “moderate/average” genetic risk by the principal investigator who is a genetic counselor, certified by the American Board of Genetic Counseling. Consensus clinical criteria for referral for hereditary cancer syndromes were used whenever available. For patients with breast, ovarian, endometrial, colon, or prostate cancer, the risk classification scheme developed by Scheuner et al. (1997) was used. Patients with family histories of breast and/or ovarian cancer were assessed to see if they met criteria for BRCA1 and BRCA2 genetic testing referral, according to relevant guidelines of the National Comprehensive Cancer Network (NCCN) (2008) and the United States Preventive Services Task Force (USPSTF) (2005). If family history was unknown or data were otherwise missing, family history was assumed to be negative for cancer.
Perceived awareness of genetic testing and DNA banking was assessed with the question, “How much have you heard or read about genetic testing [DNA banking] for cancer risk?” (Durfy et al. 1999; Quillin et al. 2008b) Participants responded on a 4-point scale with answers ranging from “Almost nothing” to “A lot.” Race/ethnicity, educational background, and household annual income of participants (patients or surrogates) were also elicited through the interviews. Ages of patients were calculated from dates of birth abstracted from medical records. We did not collect data about ages of medical decision-making surrogates.
Sample Size
The initial target enrollment for this study was 150 participants. This sample size was originally chosen based on expectations of perceived genetic awareness among participants. Based on a previous study, about 10% of research participants were expected to have high awareness (i.e., to report having heard or read “a lot” about genetic testing (Quillin et al. 2008b)). A sample size of 150 would have allowed us to estimate this proportion with a 95% confidence interval that is +/−5%. The recruitment rate was lower than expected, and the recruitment period was not extended due to limited funding.
Data Analyses
All analyses were conducted using SAS v.9.1.3. Reported family histories and data from medical records were reviewed by a genetic counselor who was certified by the American Board of Genetic Counseling. The proportion of families meeting hereditary cancer criteria or having “strong” genetic risk was assessed, and a 95% confidence interval for the proportion was obtained, using the BINOMIAL option in SAS. The proportion of participants having various levels of awareness was also estimated for genetic testing and DNA banking. Chi-square analyses were conducted to look for differences in awareness of genetic testing and DNA banking by genetic risk. We also looked for differences in the prevalence of hereditary cancer risk by sociodemographic characteristics (race, income, and educational background) with Chi-square analyses. For association analyses involving small proportions, Fisher’s exact test was used. Alpha levels of p<.05 were considered statistically significant.
Although the participant pool included a mix of patients answering for themselves (n=34) and medical decision-making surrogates (n=9), for data analyses we did not distinguish these types of participants. In clinical practice, when a patient cannot communicate with her or his care providers, communicating family health history and deciding about genetic testing are responsibilities of a decision-making surrogate when one is available. Thus, for the goal of identifying hereditary cancer in clinical palliative care practice, this exploratory study utilized relevant clinical information just as it would come to a provider—either from the patient or from a medical decision-making surrogate.
Results
From January to July, 2008, 88 patients were screened eligible, and we recruited 43 for a recruitment rate of 49%. Fifty-eight of the 88 patients were actually approached and invited to the study, so the acceptance rate was 74%. Thirty-four participants were patients answering for themselves, and nine participants were medical decision-making surrogates. Attempts to recruit many patients failed because it was an inconvenient time (e.g., patient sleeping, had visitors, patient getting a procedure). This occurred for at least 36% of patients who were not recruited. Other reasons for patients declining study participation included imminent death (i.e., death expected within 24 h) or discharge from the hospital, the patient or others conveying to the research assistant that it was not a good time for discussion (e.g., family visiting), lack of availability of a surrogate decision maker, participants feeling overwhelmed because of concurrent involvement in another research study, and general lack of interest in participating in research. No one who declined expressed discomfort with the study topic. Some data were missing for five participants because they were not able to complete the interview in the hospital and were lost to follow up, despite several attempts to reach them by phone.
About half of the participants (20/39) reporting race were African-American. Mean age of patients in the study was 55 years (Median 54, Range: 19 to 87). About 20% of study participants had a college education or more, and the annual income for 27% of participants was less than $15,000.
Overall, nine (21%, 95% CI=8.8% to 33.1%) of the 43 patients had family histories suggestive of hereditary risk (Table 1). This included eight families that met criteria by Scheuner et al. (1997), five that met NCCN (2008) criteria for breast/ovarian cancer, and two that met USPSTF (2005) criteria for breast/ovarian cancer. One family met criteria for familial lung cancer (Bailey-Wilson et al. 2004).
Table 1.
Family Characteristics for Those with Strong Genetic Risk for Cancer
| Patient Diagnosis(es) | Reported Family History of Cancer | Criteria Meta |
|---|---|---|
| Squamous cell anal cancer, 44 years old, not HIV-related | Maternal aunt with breast cancer at age 40 years Maternal grandmother with bone cancer at age 64 years |
Scheuner et al. (1997) NCCN |
| Colorectal cancer, 50 years old | None | Scheuner et al. (1997) |
| Leukemia, 27 years old | Maternal aunt/uncle with colorectal cancer, 28 years old Paternal aunt/uncle with breast cancer, 43 years old Paternal aunt/uncle with throat or lung cancer, 58 years old Paternal grandmother with breast cancer, age unknown |
Scheuner et al. (1997) NCCN |
| Colorectal cancer, 49 years old | Maternal aunt/uncle with breast cancer, 40 years old Maternal aunt/uncle with colorectal cancer, 85 years old Maternal aunt/uncle with colorectal cancer, 75 years old Maternal aunt/uncle with lung cancer, 75 years old Maternal grandmother with ovarian cancer, 75 years old Paternal aunt with breast cancer, 68 years old Paternal aunt with breast cancer, 68 years old Paternal grandmother with ovarian cancer, 75 years old |
Scheuner et al. (1997) NCCN USPSTF |
| Colorectal cancer, 47 years old | Maternal aunt/uncle with lung cancer, 58 years old Father with cancer of unknown type, 40 years old |
Scheuner et al. (1997) |
| Lung cancer, 78 years old | Child with colorectal cancer, 49 years old Son with prostate cancer, 55 years old Father with cancer of unknown type, unknown age |
Scheuner et al. (1997) |
| Breast cancer, 60 years old | Sister with breast cancer, 65 years old Mother with ovarian cancer and leukemia, 70 years old Father with bladder cancer, 82 years old Paternal uncle with esophageal cancer, 77 years old |
Scheuner et al. (1997) NCCN USPSTF |
| Colorectal cancer, 43 years old | Mother with breast cancer, 39 years old Paternal aunt/uncle with colon cancer, unknown age Paternal grandparent with breast cancer, unknown age |
Scheuner et al. (1997) NCCN |
| Pancreatic cancer, 54 years old | Three sisters with lung cancer at a young age, one at 36 and the other two diagnosed at unknown ages, but likely early-onset (before menopause) | Bailey-Wilson et al. (2004) |
Among all participants, more than half reported they had heard or read “almost nothing” about genetic testing (52%) and DNA banking (67%). The proportion of participants with this low perceived awareness of genetic services was similar between those with and without hereditary cancer by family history (p>.05). Similarly, presence of hereditary cancer risk was not associated with educational background, income, race, or age (Table 2).
Table 2.
Association Between Patient Characteristics and Hereditary Cancer Risk
| Category | na | Average/Moderate Genetic Risk (n=34) (%) | Strong Genetic Risk (n=9) (%) | p-Valueb |
|---|---|---|---|---|
| Awareness of Genetic Testing | ||||
| Almost nothing | 22 | 54.6 | 44.4 | 0.714 |
| At least some | 20 | 45.4 | 55.6 | |
| Awareness of DNA Banking | ||||
| Almost nothing | 26 | 66.7 | 66.7 | 1.000 |
| At least some | 13 | 33.3 | 33.3 | |
| Educational Background | ||||
| Up to college | 30 | 60.0 | 66.7 | 1.000 |
| At least college | 9 | 40.0 | 33.3 | |
| Annual Income | ||||
| <$15,000 | 10 | 21.4 | 44.4 | 0.127 |
| $15,000–$34,999 | 10 | 35.7 | 0.00 | |
| $35,000–$74,999 | 11 | 25.0 | 44.4 | |
| $75,000+ | 6 | 17.9 | 11.1 | |
| Race/Ethnicityc | ||||
| African American | 20 | 48.3 | 66.7 | 0.454 |
| Caucasian | 18 | 51.7 | 33.3 | |
| Patient Age (mean) | 54.6 years | 55.1 years | 52.9 years | 0.717d |
Total within categories may be less than 43 because of missing data
Fisher’s exact test
One participant who reported “Other” race was excluded from this analysis
T-test
Discussion
The aims of this study were to assess the proportion of hereditary cancer among dying cancer patients, their awareness of genetic testing and DNA banking, and to look for associations of hereditary risk with genetic awareness and sociodemograpic variables. In this sample, about one in five patients met criteria for genetics referral. This was higher than anticipated, though the 95% confidence interval of this proportion overlapped with the typical estimated 5% to 10% of cancer patients expected to have hereditary risk. It would be unrealistic to expect any one set of criteria to have both perfect sensitivity and specificity, and, for purposes of genetics referral, it is likely appropriate to have higher sensitivity at the cost of some specificity (i.e., higher toleration for false screen positives). For example, the USPSTF (2005) estimated 2% of the general population (having no personal history of cancer) would meet their criteria for BRCA1 and BRCA2 referral, compared to a population BRCA1 and BRCA2 carrier rate of much lower than 1%. A subsequent study (Palomaki et al. 2006) found an actual screen positive rate of 7.5%. Using a checklist approach, Bellcross et al. (2009) found a similar proportion (6.2%) of women in a mammography clinic had at least a 10% chance of having a BRCA1 or BRCA2 mutation, and thus might be appropriate for referral. Subsequent studies showed a positive screen rate closer to 2% when multiple criteria agree (McClain et al. 2008). Among women with breast or ovarian cancer, one study found 20.6% screened positive using a 10% mutation probability threshold by the Myriad model (Dominguez et al. 2005), whereas a study among Japanese patients found 7.5% screened positive using the same criterion (Komata et al. 2009). Hampel et al. (2004) tested a comprehensive set of criteria for use among healthy individuals and cancer patients and found that 14.9% were considered to be high risk. The findings from the current study are within the range found in the literature.
While the purpose of this study was not to test various methods for identification of hereditary risk, it is notable that the criteria used [Scheuner et al. (1997) classification, NCCN (2008), USPSTF (2005), and expert genetic counseling review] did not identify, on face value, any inappropriate referrals. Genetic testing was not a part of the study, so it is unknown what proportion of patients had identifiable mutations. However, given the limited clinical sensitivity of currently available genetic tests, the missed opportunities for hereditary risk counseling and DNA banking in these families is notable.
Relatedly, about half of all patients, including those with hereditary risk had heard/read almost nothing about genetic testing and DNA banking. This low awareness is similar to levels found in other studies (Durfy et al. 1999; Quillin et al. 2008a, b). These findings reinforce that providers cannot assume that patients with family histories will know about the availability of genetic services. None of the patients was seen by our institution’s genetics clinic, and none reported having previous clinical genetic testing for cancer risk or banking DNA (data not shown). Risk for genetic disease cut across all levels of sociodemographic characteristics, suggesting the implications of our findings may apply broadly, at least for the characteristics identified in this study (e.g., race, income).
Study Limitations
This study has limitations. First, we recruited fewer participants than we had planned. Funding and time limitations contributed to this lower sample size. Still, the participant characteristics, in terms of cancer diagnoses and sociodemographics, were typical of patients at our institution. There is no obvious bias in our sample that would suggest results are not generalizable to other clinical settings such as the one in our study. Still, a larger sample size would help support the applicability of our findings to the larger patient population. The study was also limited by patient report of family history. We also note that awareness was assessed through a single-item measure that only captured perceived, self-reported exposure to genetic information. Although this measure has literature precedence, the use of a single measure could compromise precision, and we note that it may not capture actual knowledge of genetics effectively. Finally, although we were able to confirm patients’ diagnoses, we did not attempt to confirm reported family history. These limitations notwithstanding, in clinical practice patient report will likely be the main source of family history data.
Practice Implications
If confirmed, the implications of this study are important for the practice of genetic counseling. Prevalence of unidentified hereditary cancer is likely at least as high among dying cancer patients in this study as the hypothesized 5% to 10%. Yet, at least at one institution that has expert and readily available genetic consultation services, and likely elsewhere, it does not appear that this risk is being addressed. The opportunities for involvement of genetic counselors may be lost when the patient dies, often within hours or days of the belated recognition of genetic risk. Surviving relatives may be losing opportunities to know if their family has detectable genetic markers for cancer risk, with lost opportunities for genetic counseling, prevention, screening, and early treatment.
Research Recommendations
Though exploratory, findings from this study support a related research agenda. First, given the small sample size, confirmatory studies at other institutions would be helpful. If the underutilization of genetic services is confirmed, future studies would be warranted to identify patient, surrogate, and provider facilitators and barriers relevant for genetic services. Ultimately, intervention research to test models for genetic services delivery at the end of life could help to address this unmet need. The high prevalence of low awareness suggests that stage-of-change interventions, such as the Precaution Adoption Process Model (Weinstein 1988) and the Transtheoretical Model (Prochaska and DiClemente 2005) might be particularly effective. Once awareness is raised, additional studies could investigate barriers and facilitators of genetic testing and banking relevant for decision-making and counseling. Although testing and banking intentions were investigated in our study, the low prevalence of genetic awareness limit the usefulness of those data, even among the small proportion of patients suspected of having hereditary cancer. It should also be noted that end-of-life research should continue in tandem with efforts to identify hereditary cancer upstream—sooner after diagnosis or, ideally, before diagnosis based on family health history.
In addition, further work is needed to address the potential practical and ethical challenges and alternatives for integrating genetic testing and DNA banking in palliative care. DNA banking is typically not covered by insurance and can cost hundreds of dollars. While this is certainly less than the cost of most clinical genetic tests, this financial barrier could be significant for many patients. Furthermore, future genetic testing of the banked sample might not be covered by insurance. Insurance coverage for clinical genetic testing is often based on “medical necessity”, typically referring to the necessity for the patient herself, rather than the patient’s family. Thus, while a patient might meet family history criteria for testing, it might be difficult for ordering providers to justify medical necessity for dying cancer patients.
Alternatively, identification of hereditary cancer may still be of benefit to patients’ families even without DNA banking or testing. The family history interview might identify other living affected relatives who are appropriate for testing. Or, the death of a patient from cancer could serve as a “teachable moment” for surviving family members that could prompt them to adopt cancer prevention or screening practices (Humpel et al. 2007). Future research studies are needed to address these potentially impactful questions.
Acknowledgments
Funding for this study was from the Massey Cancer Center at Virginia Commonwealth University. We would like to thank Ms. Funmi Obiri for recruitment and administrative assistance.
Appendix








Contributor Information
John Martin Quillin, Email: jquillin@mcvh-vcu.edu, Massey Cancer Center, Human & Molecular Genetics, Virginia Commonwealth University, 1101 E. Marshall St., Richmond, VA 23298-0033, USA.
Joann N. Bodurtha, Massey Cancer Center, Human & Molecular Genetics, Virginia Commonwealth University, 1101 E. Marshall St., Richmond, VA 23298-0033, USA
Laura A. Siminoff, Email: lasiminoff@vcu.edu, Massey Cancer Center, Social & Behavioral Health, Virginia Commonwealth University, 1112 E. Clay St., Richmond, VA 23298-0149, USA.
Thomas J. Smith, Email: tsmith5@mcvh-vcu.edu, Massey Cancer Center, Internal Medicine, Virginia Commonwealth University, P.O. Box 980230, Richmond, VA 23298-0230, USA.
References
- Bailey-Wilson JE, Amos CI, Pinney SM, Petersen GM, de Andrade M, Wiest JS, et al. A major lung cancer susceptibility locus maps to chromosome 6q23–25. American Journal of Human Genetics. 2004;3:460–474. doi: 10.1086/423857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bellcross CA, Lemke AA, Pape LS, Tess AL, Meisner LT. Evaluation of a breast/ovarian cancer genetics referral screening tool in a mammography population. Genetics in Medicine. 2009;11:783–9. doi: 10.1097/GIM.0b013e3181b9b04a. [DOI] [PubMed] [Google Scholar]
- Berliner JL, Fay AM. Risk assessment and genetic counseling for hereditary breast and ovarian cancer: recommendations of the national society of genetic counselors. Journal of Genetic Counseling. 2007;16(3):241–260. doi: 10.1007/s10897-007-9090-7. [DOI] [PubMed] [Google Scholar]
- Dominguez FJ, Jones JL, Zabicki K, Smith BL, Gadd MA, et al. Prevalence of hereditary breast/ovarian carcinoma risk in patients with a personal history of breast or ovarian carcinoma in a mammography population. Cancer. 2005;104:1849–53. doi: 10.1002/cncr.21393. [DOI] [PubMed] [Google Scholar]
- Durfy SJ, Bowen DJ, McTiernan A, Sporleder J, Burke W. Attitudes and interest in genetic testing for breast and ovarian cancer susceptibility in diverse groups of women in western Washington. Cancer Epidemiology, Biomarkers & Prevention. 1999;4(Pt 2):369–375. [PubMed] [Google Scholar]
- Fowler ES, Neese ER, Schwartzberg LS. Cancer genetic counseling: trends in patient referrals and genetic testing in a community-based program. Community Oncology. 2005;3:253–260. [Google Scholar]
- Garber JE, Offit K. Hereditary cancer predisposition syndromes. Journal of Clinical Oncology. 2005;23:276–92. doi: 10.1200/JCO.2005.10.042. [DOI] [PubMed] [Google Scholar]
- Grover S, Stoffel EM, Bussone L, Tschoegl E, Syngal S. Physician assessment of family cancer history and referral for genetic evaluation in colorectal cancer patients. Clinical Gastroenterology and Hepatology. 2004;9:813–819. doi: 10.1016/s1542-3565(04)00352-0. [DOI] [PubMed] [Google Scholar]
- Hampel H, Sweet K, Westman JA, Offit K, Eng C. Referral for cancer genetics consultation: a review and compilation of risk assessment criteria. Journal of Medical Genetics. 2004;41:81–91. doi: 10.1136/jmg.2003.010918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humpel N, Magee C, Jones SC. The impact of a cancer diagnosis on the health behaviors of cancer survivors and their family and friends. Supportive Care in Cancer. 2007;15:621–30. doi: 10.1007/s00520-006-0207-6. [DOI] [PubMed] [Google Scholar]
- Komata D, Yahata T, Kodama S, Koyama Y, Takeda N, et al. The prevalence of hereditary breast/ovarian cancer risk in patients with a history of breast or ovarian cancer in Japanese subjects. The Journal of Obstetrics and Gynaecology Research. 2009;35:912–7. doi: 10.1111/j.1447-0756.2009.01090.x. [DOI] [PubMed] [Google Scholar]
- Lillie AK. Exploring cancer genetics and care of the family: an evolving challenge for palliative care. International Journal of Palliative Nursing. 2006;12:70–4. doi: 10.12968/ijpn.2006.12.2.20533. [DOI] [PubMed] [Google Scholar]
- McClain MR, Palomaki GE, Hampel HH, Westman JA, Haddow JE. Screen positive rates among six family history screening protocols for breast/ovarian cancer in four cohorts of women. Familial Cancer. 2008;7:341–5. doi: 10.1007/s10689-008-9188-6. [DOI] [PubMed] [Google Scholar]
- National Comprehensive Cancer Network. Practice Guidelines in Oncology. Genetic/Familial High Risk Assessment: Breast and Ovarian Cancer. 2008 V.1.2008. [Google Scholar]
- Offit K. Clinical cancer genetics. New York: Wiley-Liss, Inc; 1998. [Google Scholar]
- Palomaki GE, McClain MR, Steinort K, Sifri R, LoPresti L, Haddow JE. Screen-positive rates and agreement among six family history screening protocols for breast/ovarian cancer in a population-based cohort of 21- to 55-year-old women. Genetics in Medicine. 2006;8:161–8. doi: 10.1097/01.gim.0000204458.84988.f2. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. The transtheoretical approach. In: Norcross JC, Goldfried MR, editors. Handbook of psychotherapy integration. 2nd. New York: Oxford University Press; 2005. pp. 147–171. [Google Scholar]
- Quillin JM, Bodurtha JN, Smith TJ. Genetics assessment at the end of life: suggestions for implementation in clinic and future research. Journal of Palliative Medicine. 2008a;11:451–8. doi: 10.1089/jpm.2007.0150. [DOI] [PubMed] [Google Scholar]
- Quillin JM, Silberg J, Jones RM, Wilson DB, Maes H, Bowen D, et al. Tolerance for ambiguity could influence awareness of breast cancer genetic testing and inform health education. Cancer Causes & Control. 2008b;19(10):1227–1232. doi: 10.1007/s10552-008-9193-y. [DOI] [PubMed] [Google Scholar]
- Scheuner MT, Wang SJ, Raffel LJ, Larabell SK, Rotter JI. Family history: a comprehensive genetic risk assessment method for the chronic conditions of adulthood. American Journal of Medical Genetics. 1997;3:315–324. doi: 10.1002/(sici)1096-8628(19970822)71:3<315::aid-ajmg12>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- Shannon KM, Lubratovich ML, Finkelstein DM, Smith BL, Powell SN, Seiden MV. Model-based predictions of BRCA1/2 mutation status in breast carcinoma patients treated at an academic medical center. Cancer. 2002;2:305–313. doi: 10.1002/cncr.10223. [DOI] [PubMed] [Google Scholar]
- Skirton H, Frazier LQ, Calvin AO, Cohen MZ. A legacy for the children–attitudes of older adults in the United Kingdom to genetic testing. Journal of Clinical Nursing. 2006;5:565–573. doi: 10.1111/j.1365-2702.2006.01372.x. [DOI] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force. Genetic risk assessment and BRCA mutation testing for breast and ovarian cancer susceptibility: recommendation statement. Annals of Internal Medicine. 2005;5:355–361. doi: 10.7326/0003-4819-143-5-200509060-00011. [DOI] [PubMed] [Google Scholar]
- Weinstein ND. The precaution adoption process. Health Psychology. 1988;7:355–386. doi: 10.1037//0278-6133.7.4.355. [DOI] [PubMed] [Google Scholar]
- Wooster R, Weber BL. Breast and ovarian cancer. The New England Journal of Medicine. 2003;23:2339–2347. doi: 10.1056/NEJMra012284. [DOI] [PubMed] [Google Scholar]


