Abstract
Many patients with fecal incontinence respond to conservative measures based upon a careful assessment and a multimodality approach that Is within the expertise of the practicing gastroenterologist. However, there Is a need for new and effective strategies when conservative therapy fails. This article reviews established therapies for fecal incontinence, such as biofeedback, as well as new therapies that have been approved by the US Food and Drug Administration (FDA), such as sacral neuromodulation and an injectable bulking agent. Also reviewed are some of the newer approaches that have not yet been approved by the FDA or that have uncertain efficacy.
Keywords: Fecal incontinence, sacral nerve stimulation, injectable bulking agent, neuromodulation
Fecal incontinence is one of the most emotionally devastating of all nonfatal conditions, resulting in considerable shame and anxiety to those who suffer from it. This condition affects 2% to 17% of adults living in the community1 and almost half of all nursing home residents.2 Many individuals with fecal incontinence are so embarrassed that they frequently do not voluntarily mention their condition to their physician and must be asked about it directly.3
The prevalence of fecal incontinence is comparable in both men and women, although the pathogenesis is often different between the sexes. Fecal incontinence is more prevalent in older age groups, those with poor health status or physical limitations,1 and individuals residing in nursing homes.2 Some recognized associations include complications with vaginal delivery, certain surgical procedures, coexistence of diarrheal disorders (including irritable bowel syndrome), and certain diseases (Table 1).
Table 1.
Select Diseases and Conditions Associated With Fecal Incontinence
|
|
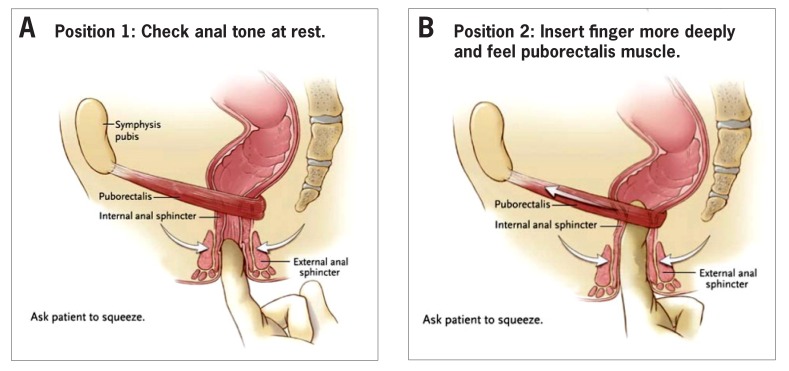
The specific causes of fecal incontinence include a number of broad categories that occur alone or in combination (Table 2).4 Many of these are suggested by a careful patient history (Table 3) and a directed physical examination that includes perianal inspection, a digital rectal examination (Figure 1), and a focused neurologic examination of the perineum and lower extremities. The performance of a rectal examination is heavily dependent upon the experience and skills of the examining physician. Unfortunately, the rectal examination is not taught well at any level of medical training, including gastroenterology fellowship programs.5 In select patients, especially when there is diagnostic uncertainty, tests to assess anorectal structure and function may be performed to assess pathogenetic mechanisms (Table 4).
Table 2.
Pathophysiology of Fecal Incontinence (Partial List)
| Overflow: fecal impaction |
| Impaired rectal/colonic storage function |
|
| Anal sphincter weakness |
|
|
| Rectal sensory impairment |
|
|
Table 3.
Topics to Discuss When Compiling a History of a Patient With Fecal Incontinence
| Topic | Rationale |
|---|---|
| Onset/risk factors | May suggest etiology |
| Natural history | May reveal reason for seeking medical attention |
| Bowel habits/type of incontinence | Incontinence for solid stool suggests greater sphincter weakness than incontinence for liquid stools only. Management is often based on the nature of bowel disturbance. |
| Warning before incontinence | Passive incontinence is often associated with internal anal sphincter weakness. Urge incontinence is often associated with external anal sphincter weakness. |
| Nocturnal incontinence | Most frequently seen in diabetes and scleroderma |
| Quality of life | Assesses severity and impact of incontinence |
| Urinary incontinence | A frequent comorbid condition that requires separate evaluation |
| Possible causes | See Tables 1 and 2. Inquire about obstetric history and medications or foods that may exacerbate incontinence. |
Figure 1.
Relevant anatomy of the anoreetum and digital examination of the anoreetum are shown in an adult with fecal incontinence. The rectum serves as both a storage area and a conduit from the colon to the anal canal. The anal canal is defined proximally by the levator ani muscles and includes the puborectalis muscle, which creates the anorectal angle. Two sphincters encircle the anal canal: the internal anal sphincter, which is a continuation of the circular smooth muscle of the rectum, and the external anal sphincter, which consists of striated muscle innervated by the pudendal nerves arising from sacral nerves S2, S3, and S4. Extrinsic innervation of the internal anal sphincter is by sympathetic and parasympathetic autonomic nerves. The initial examination assesses the resting tone of the anal canal, derived primarily from the internal anal sphincter (70%) with contributions from the external anal sphincter (30%; A). When the patient is asked to squeeze, the strength and duration of the contraction of the external anal sphincter may be assessed (curved arrows). To assess the puborectalis muscle, the examining finger is advanced and oriented posteriorly (B). When the patient is asked to squeeze, the contraction of the puborectalis muscle is felt as an anterior and upward tug as the muscle shortens (arrow). Simultaneously, the external anal sphincter contracts to increase the pressure in the anal canal.
Reprinted with permission from Wald A.4
Table 4.
Diagnostic Tests for Fecal Incontinence
| Information Obtained | |
|---|---|
| Helpful Tests | |
| Anorectal manometry | Anal canal pressures at rest and squeeze Rectal sensation |
| Anal sonography | Integrity of internal and external anal sphincters |
| Electromyography | Denervation of external anal sphincter or puborectalis muscle |
| Tests With Uncertain Benefit | |
| Pudendal nerve terminal motor latency test | Speed of pudendal nerve conduction |
| Barium proctography | Anorectal anatomy and function |
| Tests With Potential Benefit | |
| Pelvic magnetic resonance imaging | Dynamic anatomy and function of anorectum and nearby pelvic organs |
The major clinical point to emphasize is that fecal incontinence is a disorder that occurs via a number of different mechanisms. The corollary is that no single treatment approach is appropriate for all patients, and it is incumbent on clinical investigators who propose a new treatment to identify those patients most likely to benefit on the basis of carefully performed clinical studies.
Fecal incontinence can be separated into clinical subtypes: passive incontinence, which occurs without warning; urge incontinence, which occurs despite active efforts to retain stool; and mixed presentation. Potential contributing factors include structural or functional weakness of the anal sphincters and/or puborectalis muscle, impaired or hypersensitive rectal sensation, and reduced colonic and rectal storage capacity. Finally, the consistency and delivery of stool to the anorectum are important; for example, diarrhea or rapid stool propulsion may uncover subclinical weakness of continence mechanisms,6 whereas constipation may protect against incontinence in individuals with impaired continence mechanisms.
Basic Principles of Management
The management of fecal incontinence requires a multimodality approach, which is often within the expertise of the practicing gastroenterologist. Management should be based upon the following principles: (1) treatment approaches should be tailored to each patient, as there are many different causes of fecal incontinence; (2) optimal management is based upon an accurate assessment of pathogenesis and the capabilities of each patient to implement management strategies; (3) modifying bowel habits is often critical to effectively manage fecal incontinence without procedural interventions; (4) fecal incontinence is not an inevitable consequence of aging and should never be considered age-appropriate; and (5) many patients can be managed effectively without referral to tertiary care centers or the performance of diagnostic studies.
General Measures for the Practicing Gastroenterologist
General measures for the management of fecal incontinence are listed in Table 5. Incontinence pads provide skin protection and prevent soiling of clothing and linens; polymers conduct moisture away from the skin.7 Disposable products are superior to nondisposable products for providing skin protection.8 Barrier creams such as zinc oxide alone or with calamine may prevent skin irritation while perianal fungal infections may be treated with topical antifungal agents.7
Table 5.
Management Approaches to Fecal Incontinence in Adults
| Management | |
|---|---|
| General Management Measures | Skin care Pads Odor control Caregiver support |
| Overflow | Disimpaction Colon evacuation Periodic laxatives/enemas, if necessary |
| Decreased Storage Capacity | Low-fiber diet Loperamide Periodic defecation with or without laxatives |
| Isolated Internal Anal Sphincter Weakness | Loperamide as needed Anal cotton plug |
| Anal Sphincter Disruption | Loperamide Surgery |
| Peripheral Neuropathy | Sacral nerve stimulation |
| Behavioral Causes/Dementia | Prompted defecation or loperamide with regular laxatives, suppositories, or enemas twice weekly |
| Diarrhea/Urgency | Loperamide or another antidiarrheal agent |
Medical and Pharmacologic Treatments
In patients with overflow incontinence associated with fecal impaction, disimpaction and colon cleansing provide immediate relief of soiling.9 It is important to emphasize that impactions may not be located within reach of the examining finger. If fecal overload or a high impaction is suspected after a negative rectal examination, a simple abdominal radiograph may establish the diagnosis. It is also important to emphasize that such patients require an ongoing bowel management program because of a high frequency of recurrence without intervention. Such a program would involve regularly scheduled attempts to defecate with the assistance of osmotic laxatives, such as polyethylene glycol, or stimulant laxatives, such as senna or bisacodyl; glycerin or bisacodyl suppositories may be used as rescue therapy if there is no defecation for 3 days.4 Short-term success rates of 60% to 80% have been reported, but long-term recurrence rates are high, resulting in the need for ongoing vigilance.
When incontinence is associated with decreased colonic and rectal storage capacity or with chronic diarrhea, treatment is directed toward reversing the underlying cause (eg, inflammatory bowel disease) or, if this is not an option, modifying stool volume, consistency, and delivery.9 It is often beneficial in patients with decreased storage capacity to reduce dietary fiber intake while using antidiarrheal drugs, which slow colonic transit. The rationale is that reduced dietary fiber decreases the amount of stool to better accommodate reduced colonic capacity. On the other hand, patients with fecal incontinence who have normal storage capacity may benefit from fiber supplements, such as psyllium, with or without antidiarrheal agents.10 Of the antidiarrheal drugs available, loperamide is preferred, as it has no central nervous system effEcts and also may increase internal anal sphincter (IAS) tone.11-13 As adequate doses and timing are important, patients should be aware that the labels of these drugs are aimed at treating acute diarrhea. The optimal approach for treating fecal incontinence is to take 2 to 4 mg of loperamide 30 minutes before meals and prior to social occasions or traveling in order to avoid accidents outside of the home. In patients with diarrhea associated with irritable bowel syndrome, medications with anticholinergic effects, such as tricyclic agents14 and smooth muscle relaxants, may be effEctive. Alosetron is a 5-hydroxytryptamine-3 (5-HT3) antagonist that is approved for women with irritable bowel syndrome and diarrhea, but with certain restrictions.15 Because of cases of severe constipation and ischemic colitis in patients taking alosetron, US Food and Drug Administration (FDA) guidelines specify that the drug may be used in women with severe irritable bowel syndrome with diarrhea only when other agents are unsatisfactory. A recent study found that another 5-HT3 antagonist, ondansetron (4 mg), provided satisfactory relief of the most intensive symptoms of irritable bowel syndrome with diarrhea, namely loose stool, frequency, and urgency.16 Conservative treatment with an experienced therapeutic team has been shown to be effective in many patients with fecal incontinence without resorting to invasive or behavioral therapies.17
Many patients complain of small amounts of fecal or mucus seepage in the absence of urge or passive incontinence. This is the most common complaint of middle- aged or older men, but it may also occur in women. Some patients exhibit decreased anal canal tone due to an isolated weakness of the IAS associated with scleroderma or sphincterotomy for anal fissure, whereas other patients may have incomplete closure of the anal cushions (eg, after hemorrhoidectomy). Mucosal or hemorrhoidal prolapse is yet another cause. If tolerated, the use of an anal plug fashioned from an ordinary cotton ball is an inexpensive approach to restore the passive barrier function and also serves as an absorbent barrier.4
None of the above clinical scenarios require tertiary specialty referral or diagnostic tests other than a careful patient history, physical examination that includes a rectal examination, and/or a sigmoidoscopy. Thus, an automatic referral for diagnostic testing is unnecessary for many patients with fecal incontinence, and treatment falls within the capabilities of the practicing gastroenterologist. The treatments discussed in the subsequent sections require referral to a tertiary care center.
Behavioral interventions
In patients who fail to respond to conservative measures, the use of manometric or electromyography-assisted biofeedback therapy may be very effective. In contrast to Kegel exercises, which are directed only toward strengthening the external anal sphincter (EAS) and puborectalis muscle, biofeedback uses a rectal balloon with anal manometry or a surface electromyography device. Treatment is directed toward contracting the EAS when balloon distension is perceived, using visual feedback from instrument tracings of anal pressure to guide the process. This process involves using progressively smaller volumes of distension in order to improve the threshold of rectal sensation and to shorten the response time between perception of distension and EAS contraction. Thus, higher squeeze pressures are not necessarily the endpoint; rather, enhanced perception and coordination with EAS contractions may be the most important outcome measures.18,19 A rigorous randomized controlled trial demonstrated that manometric biofeedback was superior to pelvic floor (Kegel) exercises alone (66% were completely continent vs 48%),20 although this has not been a universal finding.17 Such patients require referral to an experienced center as well as diagnostic anorectal manometry to maximize the chance of success.
Invasive interventions (Select List)
Many patients do not respond satisfactorily to conservative and behavioral measures,21 and there is a need for new and effective strategies when medical therapy fails. The need is particularly urgent because traditional surgical approaches, such as anal sphincter repairs, are of uncertain efficacy for functional fecal incontinence, even in patients who have documented anal sphincter defects. For example, in shortterm studies, up to 85% of patients with incontinence and sphincter defects improve after overlapping anal sphincteroplasty. However, long-term results have been disappointing, with failure rates of over 50% after 40 to 60 months and even more deterioration thereafter22,23; this is especially true in older patients. Other surgical procedures such as postanal repair may be performed in patients undergoing rectal prolapse repair with disabling incontinence. Gracilo- plasty is accompanied by significant morbidity (infections, device problems, leg pain) and often requires reoperation. Moreover, the hardware for graciloplasty is not approved in the United States.9
Sacral Nerve Stimulation
Sacral neuromodulation was first used to treat neurogenic bladder with urinary incontinence, and its use was subsequently extended to patients with fecal incontinence who had failed conservative therapy.24 The technique requires sophisticated skills to place a temporary stimulating electrode into a sacral foramen (most often S3). If there is a positive response during a 2-week period, a permanent electrode is connected to a subcutaneously embedded neurostimulator placed in the gluteal area. On the basis of a large North American multicenter industry-supported trial, the results of which were published in 2010,25 sacral nerve stimulation (SNS) was approved by the FDA in 2012 for fecal incontinence.
In the North American multicenter SNS study, 120 of 133 eligible patients with fecal incontinence responded to the test stimulation and proceeded to chronic stimulation. Patients were categorized as having passive incontinence (41%), urge incontinence (45%), or mixed. All patients underwent anorectal manometry and anal sonography, and completed the Fecal Incontinence Quality-of-Life (FIQOL) scale and Fecal Incontinence Severity Index. The primary outcome measure was at least 50% reduction in the number of incontinence episodes per week compared with baseline at 12 months postimplantation.
Improvement in weekly continent episodes was further stratified to 50% to 75%, more than 75% to less than 100%, and complete continence. At 12 months, 40% of patients had achieved complete continence, 28% of patients had improved their continence by more than 75% to less than 100%, and 14% of patients had improved their continence by 50% to 75%. Thus, using the original criterion of at least 50% reduction in the number of incontinent episodes, 83% of patients were improved at 12 months compared with baseline. All 4 subscales of the FIQOL scale significantly improved by 3 months and remained steady through 36 months. As expected, there were adverse effects with SNS, including 26 that were designated as serious. Removal of the device was necessary in 6 subjects because of chronic infection unresponsive to antibiotics. This was considered acceptable in view of the magnitude of efficacy. However, because there was no sham control group, there was no blinding of patients or investigators.
The rationale for the adoption of the placebo- or sham-controlled, randomized trial is an effort to control for selection and response biases by both subjects and investigators. For example, in the study by Heymen and colleagues on biofeedback, 41% of patients undergoing Kegel exercises reported significant relief and 21% achieved complete continence over 3 months.20 The investigators in the SNS trial addressed the absence of a sham group and concluded that it seemed unreasonable to attribute the magnitude of benefit (especially the 40% fully continent group) to a placebo effect; some objective observers would be inclined to agree. Nevertheless, all future studies of new treatments for fecal incontinence should include a placebo/sham arm, as the literature is filled with new treatments that were successful in uncontrolled studies but did not differ from, or even underperformed, sham/placebo arms.26 Another suggestion is that after such trials enroll patients with fecal incontinence, the patients first be given conservative therapy by specialized therapists and gastroenterologists before concluding that the patients have failed therapy. It is unclear in the SNS trials how rigorous the conservative therapy was before entry into the studies.
Rationale of Using the Procedure for Fecal Incontinence The initial and biologically plausible hypothesis underlying SNS was that it would alter anorectal physiology, perhaps by improving EAS and/or puborectalis functions, which are modulated by sacral motor pathways. However, this has not been convincingly demonstrated in subjects who improve with SNS and underscores the fact that clinical improvement of fecal incontinence may not correlate with anorectal measurements. An alternative explanation has been proposed by a recent study of SNS in li patients with urge incontinence.27 SNS resulted in a substantial increase in retrograde colonic propagating sequences, which did not occur with sham stimulation. This suggests that SNS may improve continence and urgency through alterations of colonic motility rather than having a direct effect on anorectal functions. This also reinforces the clinical importance of modulating stool delivery to the anorectum as being paramount in improving urge incontinence in some patients. This may also explain favorable reports of SNS treatment for fecal incontinence following low anterior resection for rectal cancer.28 If these results are confirmed, SNS could conceivably be indicated in patients who have fecal incontinence associated with decreased rectal storage capacity for different reasons, but this has not been convincingly demonstrated.29
Injections of Dextranomer in Stabilized Hyaluronic Acid
The concept of injecting a biomaterial to augment anal canal pressures to treat fecal incontinence was first proposed approximately 2 decades ago; since then, many different substances have been injected with varying results and often using suboptimal study designs.30 There has been renewed interest in injectable bulking agents since the publication of an industry-supported, randomized, sham- controlled study that reported the outcomes of injections of dextranomer in stabilized hyaluronic acid (NASHA Dx; Solesta, Salix) into the submucosa of the anal canal in 136 patients with fecal incontinence and sham injections in a control group of 70 patients.31 NASHA Dx had long been used as a bulking agent in urologic procedures with few side effects,32 and there seemed to be biologic plausibility for its use in select patients with fecal incontinence. Although the optimal group of patients would intuitively seem to be those with passive incontinence and low anal canal pressures, the pivotal study, which was performed with input from the FDA, studied mainly female patients who were not characterized as having either urge, passive, or mixed incontinence.31 The inclusion of patients with urge incontinence seems somewhat counterintuitive, as such patients often have weakness of the EAS as well as decreased rectal capacity and rectal hypersensitivity,33 none of which would be expected to be altered by an injectable bulking agent. Patients were assessed via the validated Cleveland Clinic Fecal Incontinence Severity (CCFIS) scale34 and the FIQOL scale35 before and after treatment. However, no studies of anorectal sensory or motor functions were performed at any time. This omission deprived the investigators of an opportunity to determine potential mechanisms for clinical improvement.
The primary endpoint chosen was a decrease of at least 50% in the number of incontinence episodes and a corresponding increase in days free of incontinence episodes, as assessed over a 2-week period at various predetermined time intervals after treatment. A second injection was permitted in patients who had no improvement within 1 month; indeed, 80% of patients in the active treatment group required a second injection. Based on these criteria, 53% of patients receiving NASHA Dx vs 32% of patients receiving sham injection were classified as responders at 6 months. Surprisingly, no significant differences in responses were noted at 3 months. In contrast to the SNS study, no significant improvements were noted between active and sham patients in 3 of the 4 parts of the FIQOL scale (lifestyle, depression and self-perception, embarrassment), and only a small improvement was noted in coping and behavior. As previously mentioned, there was no sham group in the SNS study with which to compare differences in quality-of-life scores. Only 6% of treated patients were fully continent at 6 months. (To my knowledge, no data have been reported for sham-treated patients.) Subsequent reports indicate that 11% of the NASHA Dx—treated patients were fully continent at 12 months. Using the 6-month data, a doctor would have to treat 17 patients (with up to 2 injections) to produce 1 fully continent individual (or 9 patients using the 1-year results). These calculations assume that no patient in the sham group became fully continent at those time intervals. NASHA Dx was approved in 2011 by the FDA as safe and effective for the treatment of fecal incontinence and is now marketed as an office-based treatment that can be administered by health care providers who have received appropriate technical training.
Candidates for the Procedure It would be plausible to assume that patients with passive incontinence are candidates for NASKA Dx. Although there are several possible causes of passive fecal incontinence, a predominant cause has been weakness of the IAS, which is responsible for approximately 70% of resting anal canal pressure.4 This occurs due to fibrosis of the IAS in systemic sclerosis, damage to the myenteric nerves following radiation therapy, or structural damage from sphincterotomy for chronic anal fissure, fistula surgery, hemorrhoidectomy, or trauma during childbirth. Although anorectal manometry can provide objective measurements of resting anal canal pressure, the normal range of anal pressure is broad and there is often little correlation between measured resting pressures and passive incontinence. Nevertheless, it would appear biologically plausible that enhancing resting anal canal pressures with an injectable bulking agent might be effective in this group.
Unfortunately, patients in the NASHA Dx report were not categorized clinically or manometrically. Whether NASHA Dx injections increase anal canal pressures is uncertain, as another study of patients with fecal incontinence who received up to 2 injections of NASHA Dx had no increase in resting or squeeze anal canal pressures when studied 6 months after treatment.36 Moreover, outcomes in this latter study were no better than those from a comparator group that received biofeedback. The signal for efficacy in the NASHA Dx study may also have been diluted by the inclusion of patients with urge incontinence or weakness of other continence mechanisms, which would not be addressed by the injection of a bulking agent. Therefore, offering this therapy to patients with urge or mixed incontinence would likely increase the failure rate and engender pessimism among health care providers about offering this treatment. This might deprive the patients who are most likely to benefit from such therapy from being offered it.37
Criteria for Efficacy for Fecal Incontinence A primary variable in any treatment study is the definition of efficacy. In a nonfatal condition such as fecal incontinence, this should include patient satisfaction and enhanced quality of life related to incontinence. The latter was the reason for the development and validation of the symptom-specific FIQOL scale,35 which has become the standard for studies of treatments related to fecal incontinence. This instrument consists of 4 domains: lifestyle (ΙΟ questions), coping/behavior (9 questions), depression (7 questions), and embarrassment (3 questions). Clinical investigators need such instruments to determine whether treatment has made a difference (positive or negative) to their patients and, if so, how much. Although a clinician’s orientation is necessary for conducting trials, the patient’s perspective of improvement is essential.38
In the NASHA Dx study, more patients treated with NASHA Dx met the primary endpoint than with sham (P=.0089). However, the median decrease in the number of incontinence episodes at 3 and 6 months was not significantly different from the sham group, nor did the mean change in the CCFIS scale differ between the 2 groups at 6 months. In addition, the mean CCFIS was 1Ο.9 (on a scale of Ο-2Ο) after treatment with NASHA Dx, which was above the minimum CCFIS required for entry into the trial. Finally, no differences in lifestyle, depression, and self-perception or embarrassment were noted between the treatment and sham groups on the FIQOL scale.
This is not to deny that NASHA Dx was effective for some patients with fecal incontinence. However, because of the inclusion criteria and failure to characterize patients into those with passive or urge incontinence, the results are difficult to interpret. There were some patients who did achieve complete continence, but it is not known who they are. There is clearly a need for a well-designed study of NASHA Dx to be performed in patients with fecal incontinence who are well-characterized clinically (passive vs urge incontinence), with anorectal measurements and meaningful clinical endpoints.
Radiofrequency Energy Delivery to the Anal Canal
This intervention was approved by the FDA in 2ΟΟ2 for treating fecal incontinence that has failed conservative treatments. The device delivers temperature-controlled radiofrequency energy to the anal sphincter complex and is based upon the biologic rationale that the procedure results in collagen deposition and tissue remodeling. The positive results reported by small industry studies39 have not been confirmed by other small studies in Europe and Asia,40,41 nor did any of the studies demonstrate changes in anorectal manometric measures. Moreover, fecal incontinence often persisted at levels that would be clinically unsatisfactory. At present, this technique cannot be recommended until larger studies of appropriate design are performed.9
Colostomy
Colostomy is considered to be a last resort for patients with intractable fecal incontinence, and it can be performed with low morbidity. Although many patients are initially resistant to the idea, it should be emphasized that this intervention is generally associated with improved quality of life and allows greater freedom of activity because of the removal of fear of incontinence episodes.42 This approach should be mentioned early in the discussion about therapeutic choices for fecal incontinence, even if other options are chosen. A visit with a stomal therapist for information gathering is also helpful, and it should be emphasized that such a consultation is not a commitment to undergo the procedure.
Noninvasive Approaches of interest
There are several ongoing investigations into novel treatment strategies for fecal incontinence, both invasive and noninvasive. Among these are minimally invasive neurostimulation techniques, such as percutaneous posterior tibial nerve stimulation (PTNS), a removable transvaginal device for women with severe and intractable fecal incontinence, and a removable anal insertion device. None of these devices are approved by the FDA.
Posterior Tibial Nerve Stimulation
The concept of indirectly providing sacral stimulation by stimulating the posterior tibial nerve represents a logical, if unproven, iteration of SNS. The posterior tibial nerve contains sensory, motor, and autonomic fibers that emerge from L4 and Li as well as SI to S3. Both transcutaneous and percutaneous stimulation have been attempted. A well- designed, randomized, sham-controlled trial found that transcutaneous PTNS was no more effective than sham treatment for fecal incontinence.43 Although several studies have suggested that percutaneous PTNS might be efficacious, a recent sham-controlled trial encompassing 228 patients with fecal incontinence demonstrated no significant clinical benefit over sham.44 Although PTNS is easier, simpler, less expensive, and less invasive than SNS, its precise role in treating fecal incontinence remains unproven.45
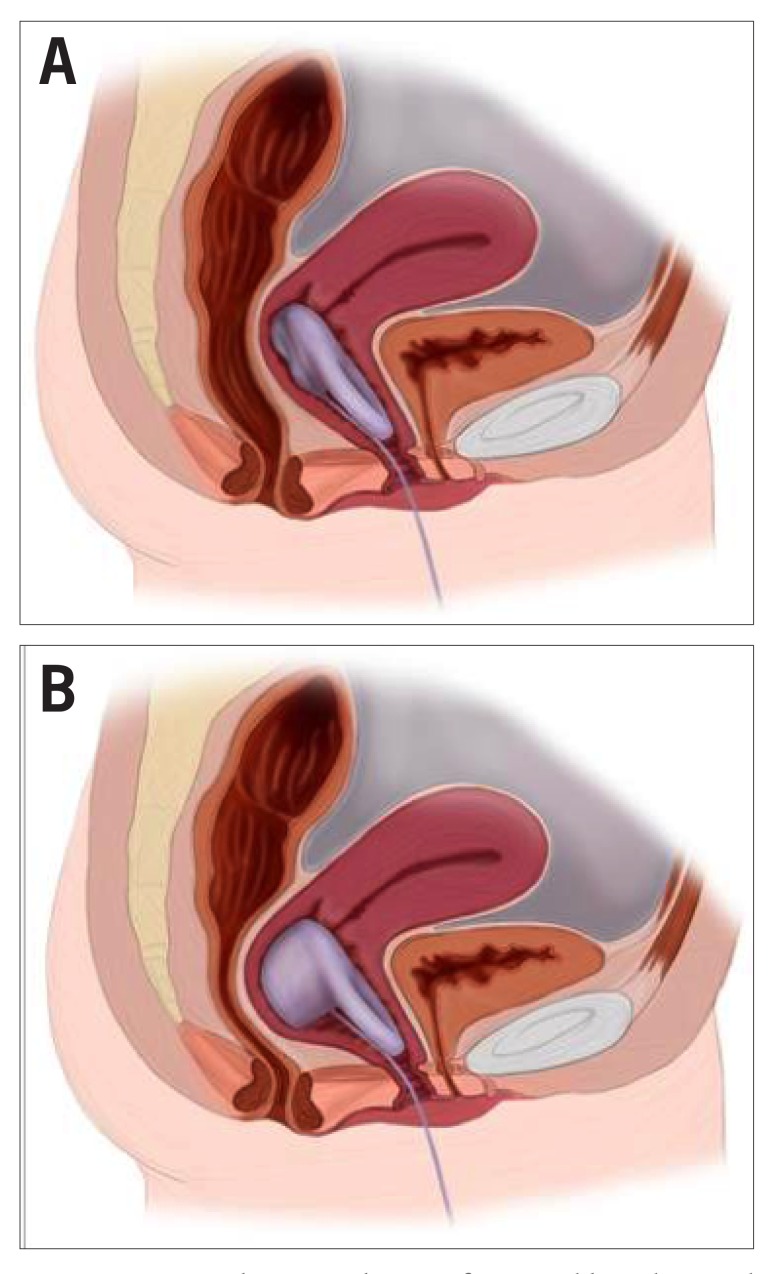
Vaginal Bowel Control Device
In a small, proof-of-concept, multicenter study, 61 women with fecal incontinence were successfully fit for a vaginal inflatable balloon and pump system (Figure 2). At 1 month, approximately 40% were continent and 79% were improved, defined as over 50% reduction in episodes of fecal incontinence46 with no serious adverse events. The advantage of such a device is that it can be removed and replaced at will. A randomized sham-controlled study will be necessary to establish this technique as effective for some women with fecal incontinence.
Figure 2.
Images depicting the use of a vaginal bowel control device. A shows the uninflated device, which allows bowel movements. B shows the inflated device, which prevents stool leakage.
Images courtesy of Heidi Brown, MD, University of Wisconsin School of Medicine and Public Health, Madison, Wisconsin.
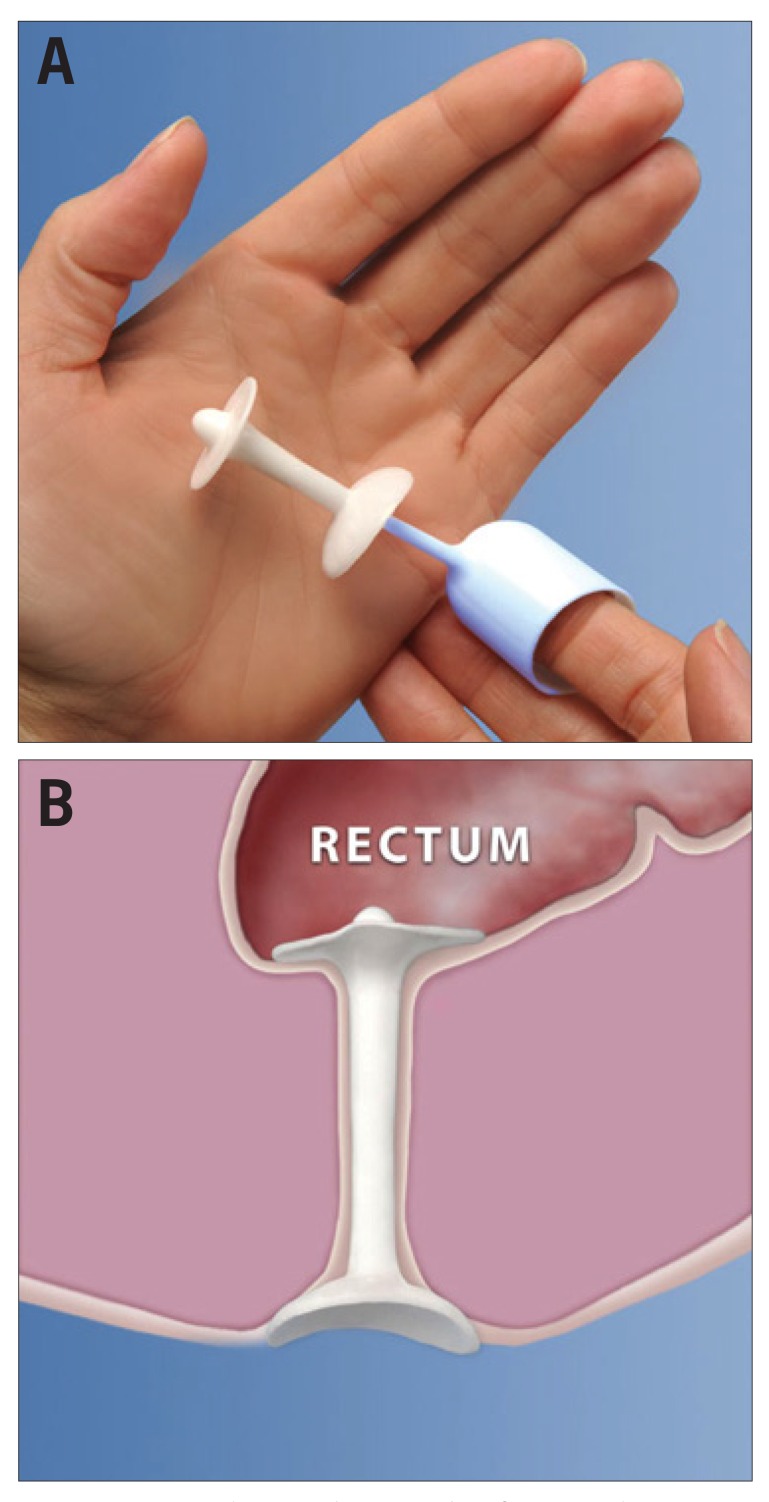
Anal Insertion Device
The available data concerning the use of anal plugs to treat fecal incontinence are very limited, and plugs may be difficult to tolerate.47 The latest device to be developed in this category consists of a soft silicone anal insert that can be placed with the use of a fingertip applicator (Renew Medical; Figure 3). Using intention-to-treat analysis in a multicenter, prospective, open-label study with a single-arm cohort, 62% of 91 subjects achieved a reduction of over Soya in incontinence frequency over a 12-week period48 with few moderately adverse effects related to device use. The most likely group to benefit might be patients with passive incontinence associated with weak anal canal tone or structural impairment of anal cushions. Another anal insertion device currently available is the Procon II device (Incontinent Control Devices, Inc), which was first introduced in 2002. Future studies are needed to better characterize which patients with fecal incontinence may benefit and should include larger numbers of men, longer durations of assessment, and validated quality-of-life and fecal incontinence severity instruments.
Figure 3.
An anal insert device with a finger applicator (A). The device in place (B).
Reprinted with permission from Deutekom M, Dobben AC.47
Summary
Fecal incontinence is not uncommon at all ages and remains underdiagnosed because of patient reluctance to volunteer this complaint and physician failure to inquire directly about it. Therefore, it is important that health care providers screen for fecal incontinence in a proactive fashion. The causes of fecal incontinence are many and varied but often may be identified by a careful patient history and a directed physical examination. Well over half of patients with this condition will respond completely or partially to conservative measures, which are well within the capacity of the practicing gastroenterologist, using a multimodality approach.
There are a number of behavioral and invasive treatments that can be effective in select patients with fecal incontinence. These include biofeedback, SMS, and, possibly, injections of bulking agents into the anorectal submucosa. New techniques of interest (but as of yet unproven) include PTNS, a vaginal bowel control device, and a silicone anal insertion device. However, there is insufficient evidence to support the clinical use of these new techniques until larger, well-designed studies demonstrate clinical efficacy.
Footnotes
The author has no relevant conflicts of interest to disclose.
References
- 1.Ditah I, Devaki P, Luma HN, et al. Prevalence, trends, and risk factors for fecal incontinence in United States adults, 2005-2010. Clin Gastroenterol Hepatol. 2014;12(4):636–643.e2. doi: 10.1016/j.cgh.2013.07.020. [DOI] [PubMed] [Google Scholar]
- 2.Bharucha AE, Dunivan G, Goode PS, et al. Epidemiology, pathophysiology and classification of FI: state of the science summary for the NIDDK workshop. Am J Gastroenterol. 2015;110(1):127–136. doi: 10.1038/ajg.2014.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leigh RJ, Turnberg LA. Faecal incontinence: the unvoiced symptom. Lancet. 1982;1(8285):1349–1351. doi: 10.1016/s0140-6736(82)92413-8. [DOI] [PubMed] [Google Scholar]
- 4.Wald A. Clinical practice. Fecal incontinence in adults. N Engl J Med. 2007;356(16):1648–1655. doi: 10.1056/NEJMcp067041. [DOI] [PubMed] [Google Scholar]
- 5.Wong RK, Drossman DA, Bharucha AE, et al. The digital rectal exam: a multicenter survey of physician and students’ perceptions and practice. Am J Gastroenterol. 2012;11:947–957. doi: 10.1038/ajg.2012.23. [DOI] [PubMed] [Google Scholar]
- 6.Bharucha AE, Zinsmeister AR, Schleck CD, Melton LJ III. Bowel disturbances are the most important risk factors for late onset fecal incontinence: a population- based case-control study in women. Gastroenterology. 2010;139(5):1559–1566. doi: 10.1053/j.gastro.2010.07.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rao SS. American College of Gastroenterology Practice Parameters Committee. Diagnosis and management of fecal incontinence. Am J Gastroenterol. 2004;99(8):1585–1604. doi: 10.1111/j.1572-0241.2004.40105.x. [DOI] [PubMed] [Google Scholar]
- 8.Shirran E, Brazzelli M. Absorbent products for the containment of urinary and/or faecal incontinence in adults [update in Cochrane Database Syst Rev. 2007;(2):CD001406] Cochrane Database Syst Rev. 2000;(2):CD001406. doi: 10.1002/14651858.CD001406. [DOI] [PubMed] [Google Scholar]
- 9.Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109(8):1141–1157. doi: 10.1038/ajg.2014.190. quiz 1058. [DOI] [PubMed] [Google Scholar]
- 10.Markland AD, Burgio KL, Whitehead WE, et al. Loperamide versus psyllium fiber for treatment of fecal incontinence: the Fecal Incontinence Prescription (Rx) Management (FIRM) randomized clinical trial. Dis Colon Rectum. 2015;58(10):983–993. doi: 10.1097/DCR.0000000000000442. [DOI] [PubMed] [Google Scholar]
- 11.Palmer KR, Corbett CL, Holdsworth CD. Double-blind cross-over study comparing loperamide, codeine and diphenoxylate in the treatment of chronic diarrhea. Gastroenterology. 1980;79(6):1272–1275. [PubMed] [Google Scholar]
- 12.Read M, Read NW, Barber DC, Duthie HL. Effects of loperamide on anal sphincter function in patients complaining of chronic diarrhea with fecal incontinence and urgency. Dig Dis Sci. 1982;27(9):807–814. doi: 10.1007/BF01391374. [DOI] [PubMed] [Google Scholar]
- 13.Sun WM, Read NW, Verlinden M. Effects of loperamide oxide on gastrointestinal transit time and anorectal function in patients with chronic diarrhoea and faecal incontinence. Scand J Gastroenterol. 1997;32(1):34–38. doi: 10.3109/00365529709025060. [DOI] [PubMed] [Google Scholar]
- 14.Santoro GA, Eitan BZ, Pryde A, Bartolo DC. Open study of low-dose amitriptyline in the treatment of patients with idiopathic fecal incontinence. Dis Colon Rectum. 2000;43(12):1676–1681. doi: 10.1007/BF02236848. [DOI] [PubMed] [Google Scholar]
- 15.Garsed K, Chernova J, Hastings M, et al. A randomised trial of ondansetron for the treatment of irritable bowel syndrome with diarrhoea. Gut. 2014;63(10):1617–1625. doi: 10.1136/gutjnl-2013-305989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Norton C, Chelvanayagam S, Wilson-Barnett J, Redfern S, Kamm MA. Randomized controlled trial of biofeedback for fecal incontinence. Gastroenterology. 2003;125(5):1320–1329. doi: 10.1016/j.gastro.2003.09.039. [DOI] [PubMed] [Google Scholar]
- 18.Wald A, Tunuguntla AK. Anorectal sensorimotor dysfunction in fecal incontinence and diabetes mellitus. Modification with biofeedback therapy. N Engl J Med. 1984;310(20):1282–1287. doi: 10.1056/NEJM198405173102003. [DOI] [PubMed] [Google Scholar]
- 19.Chiarioni G, Bassotti G, Stanganini S, Vantini I, Whitehead WE. Sensory retraining is key to biofeedback therapy for formed stool fecal incontinence. Am J Gastroenterol. 2002;97(1):109–117. doi: 10.1111/j.1572-0241.2002.05429.x. [DOI] [PubMed] [Google Scholar]
- 20.Heymen S, Scarlett Y, Jones K, Ringel Y, Drossman D, Whitehead WE. Randomized controlled trial shows biofeedback to be superior to pelvic floor exercises for fecal incontinence. Dis Colon Rectum. 2009;52(10):1730–1737. doi: 10.1007/DCR.0b013e3181b55455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Whitehead WE, Rao SS, Lowry A, et al. Treatment of fecal incontinence: state of the science summary for the NIDDK workshop. Am J Gastroenterol. 2015;110(1):138–146. doi: 10.1038/ajg.2014.303. [DOI] [PubMed] [Google Scholar]
- 22.Bravo Gutierrez A, Madoff RD, Lowry AC, Parker SC, Buie WO, Baxter NN. Long-term results of anterior sphincteroplasty. Dís Colon Rectum. 2004;47(5):727–731. doi: 10.1007/s10350-003-0114-6. [DOI] [PubMed] [Google Scholar]
- 23.Halverson AL, Hull TL. Long-term outcome of overlapping anal sphincter repair. Dís Colon Rectum. 2002;45(3):345–348. doi: 10.1007/s10350-004-6180-6. [DOI] [PubMed] [Google Scholar]
- 24.Leroi AM, Michot F, Grise P, Denis P. Effect of sacral nerve stimulation in patients with fecal and urinary incontinence. Dís Colon Rectum. 2001;44(6):779–789. doi: 10.1007/BF02234695. [DOI] [PubMed] [Google Scholar]
- 25.Wexner SD, Coller JA, Devroede G, et al. Sacral nerve stimulation for fecal incontinence: results of a 120-patient prospective multicenter study. Ann Surg. 2010;251(3):441–449. doi: 10.1097/SLA.0b013e3181cf8ed0. [DOI] [PubMed] [Google Scholar]
- 26.Wald A. Clonidine and botulinum toxin: a tale of two treatments. Clin Gastroenterol Hepatol. 2014;12(5):852–853. doi: 10.1016/j.cgh.2013.08.022. [DOI] [PubMed] [Google Scholar]
- 27.Patton V, Wiklendt L, Arkwright JW, Lubowski DZ, Dinning PG. The effect of sacral nerve stimulation on distal colonic motility in patients with faecal incontinence. BrJ Surg. 2013;100(7):959–968. doi: 10.1002/bjs.9114. [DOI] [PubMed] [Google Scholar]
- 28.de Miguel M, Oteiza F, Ciga MA, Armendáriz P, Marzo J, Ortiz H. Sacral nerve stimulation for the treatment of faecal incontinence following low anterior resection for rectal cancer. Colorectal Dís. 2011;13(1):72–77. doi: 10.1111/j.1463-1318.2009.02066.x. [DOI] [PubMed] [Google Scholar]
- 29.Thomas GP, Bradshaw E, Vaizey CJ. A review of sacral nerve stimulation for faecal incontinence following rectal surgery and radiotherapy. Colorectal Dís. 2015;17(11):939–942. doi: 10.1111/codi.13069. [DOI] [PubMed] [Google Scholar]
- 30.Maeda Y, Laurberg S, Norton C. Perianal injectable bulking agents as treatment for faecal incontinence in adults. Cochrane Database SystRev. 2013;(2):CD007959. doi: 10.1002/14651858.CD007959.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Graf W, Mellgren A, Matzel KE, Hull T, Johansson C, Bernstein M. NASHA Dx Study Group. Efficacy of dextranomer in stabilised hyaluronic acid for treatment of faecal incontinence: a randomised, sham-controlled trial. Lancet. 2011;377(9770):997–1003. doi: 10.1016/S0140-6736(10)62297-0. [DOI] [PubMed] [Google Scholar]
- 32.Molitierno JA, Scherz HC, Kirsch AJ. Endoscopic treatment of vesicoureteral reflux using dextranomer hyaluronic acid copolymer. J Pediatr Urol. 2008;4(3):221–228. doi: 10.1016/j.jpurol.2007.11.015. [DOI] [PubMed] [Google Scholar]
- 33.Bharucha AE, Fletcher JG, Harper CM, et al. Relationship between symptoms and disordered continence mechanisms in women with idiopathic faecal incontinence. Gut. 2005;54(4):546–555. doi: 10.1136/gut.2004.047696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Jorge JMN, Wexner SD. Etiology and management of fecal incontinence. Dís Colon Rectum. 1993;36(1):77–97. doi: 10.1007/BF02050307. [DOI] [PubMed] [Google Scholar]
- 35.Rockwood TH, Church JM, Fleshman JW, et al. Fecal Incontinence Quality of Life Scale: quality of life instrument for patients with fecal incontinence. Dís Colon Rectum. 2000;43(1):9–16. doi: 10.1007/BF02237236. [DOI] [PubMed] [Google Scholar]
- 36.Dehli T, Stordahl A, Vatten LJ, et al. Sphincter training or anal injections of dextranomer for treatment of anal incontinence: a randomized trial. Scand J Gastroenterol. 2013;48(3):302–310. doi: 10.3109/00365521.2012.758770. [DOI] [PubMed] [Google Scholar]
- 37.Wald A. New treatments for fecal incontinence: update for the gastroenterologist. Clin Gastroenterol Hepatol. 2014;12(11):1783–1788. doi: 10.1016/j.cgh.2014.02.013. [DOI] [PubMed] [Google Scholar]
- 38.Whitehead WE, Corazziari E, Prizont R, Senior JR, Thompson WG, Veldhuyzen Van Zanten SJ. Definition of a responder in clinical trials for functional gastrointestinal disorders: report on a symposium. Gut. 1999;45(suppl 2):II78–II79. doi: 10.1136/gut.45.2008.ii78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Efron JE, Corman ML, Fleshman J, et al. Safety and effectiveness of temperature- controlled radio-frequency energy delivery to the anal canal (Secca procedure) for the treatment of fecal incontinence. Dís Colon Rectum. 2003;46(12):1606–1616. doi: 10.1007/BF02660763. [DOI] [PubMed] [Google Scholar]
- 40.Lefebure B, Tuech JJ, Bridoux V, et al. Temperature-controlled radio frequency energy delivery (Secca procedure) for the treatment of fecal incontinence: results of a prospective study. Int J Colorectal Dís. 2008;23(10):993–997. doi: 10.1007/s00384-008-0514-0. [DOI] [PubMed] [Google Scholar]
- 41.Kim DW, Yoon HM, Park JS, Kim YH, Kang SB. Radiofrequency energy delivery to the anal canal: is it a promising new approach to the treatment of fecal incontinence? Am J Surg. 2009;197(1):14–18. doi: 10.1016/j.amjsurg.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 42.Norton C, Burch J, Kamm MA. Patients’ views of a colostomy for fecal incontinence. Dís Colon Rectum. 2005;48(5):1062–1069. doi: 10.1007/s10350-004-0868-5. [DOI] [PubMed] [Google Scholar]
- 43.Leroi AM, Siproudhis L, Etienney I, et al. Transcutaneous electrical tibial nerve stimulation in the treatment of fecal incontinence: a randomized trial (CONSORT la) Am J Gastroenterol. 2012;107(12):1888–1896. doi: 10.1038/ajg.2012.330. [DOI] [PubMed] [Google Scholar]
- 44.Knowles CH, Horrocks EJ, Bremner SA, et al. CONFIDeNT study group. Percutaneous tibial nerve stimulation versus sham electrical stimulation for the treatment of faecal incontinence in adults (CONFIDeNT): a double-blind, multicentre, pragmatic, parallel-group, randomised controlled trial. Lancet. 2015;386(10004):1640–1648. doi: 10.1016/S0140-6736(15)60314-2. [DOI] [PubMed] [Google Scholar]
- 45.Thaha MA, Abukar AA, Thin NN, Ramsanahie A, Knowles CH. Sacral nerve stimulation for faecal incontinence and constipation in adults. Cochrane Database Syst Rev. 2015;(8):CD004464. doi: 10.1002/14651858.CD004464.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Richter HE, Matthews CA, Muir T, et al. A vaginal bowel-control system for the treatment of fecal incontinence. Obstet Gynecol. 2015;125(3):540–547. doi: 10.1097/AOG.0000000000000639. [DOI] [PubMed] [Google Scholar]
- 47.Deutekom M, Dobben AC. Plugs for containing faecal incontinence. Cochrane Database Syst Rev. 2015;(7):CD005086. doi: 10.1002/14651858.CD005086.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lukacz ES, Segall MM, Wexner SD. Evaluation of an anal insert device for the conservative management of fecal incontinence. Dís Colon Rectum. 2015;58(9):892–898. doi: 10.1097/DCR.0000000000000427. [DOI] [PubMed] [Google Scholar]