Abstract
Study objective
The Institute of Medicine has called on the US health care system to identify and reduce medical errors. Unfortunately, medication dosing errors remain commonplace and may result in potentially life-threatening outcomes, particularly for pediatric patients when dosing requires weight-based calculations. Novel medication delivery systems that may reduce dosing errors resonate with national health care priorities. Our goal was to evaluate novel, prefilled medication syringes labeled with color-coded volumes corresponding to the weight-based dosing of the Broselow Tape, compared with conventional medication administration, in simulated pediatric emergency department (ED) resuscitation scenarios.
Methods
We performed a prospective, block-randomized, crossover study in which 10 emergency physician and nurse teams managed 2 simulated pediatric arrest scenarios in situ, using either prefilled, color-coded syringes (intervention) or conventional drug administration methods (control). The ED resuscitation room and the intravenous medication port were video recorded during the simulations. Data were extracted from video review by blinded, independent reviewers.
Results
Median time to delivery of all doses for the conventional and color-coded delivery groups was 47 seconds (95% confidence interval [CI] 40 to 53 seconds) and 19 seconds (95% CI 18 to 20 seconds), respectively (difference=27 seconds; 95% CI 21 to 33 seconds). With the conventional method, 118 doses were administered, with 20 critical dosing errors (17%); with the color-coded method, 123 doses were administered, with 0 critical dosing errors (difference=17%; 95% CI 4% to 30%).
Conclusion
A novel color-coded, prefilled syringe decreased time to medication administration and significantly reduced critical dosing errors by emergency physician and nurse teams during simulated pediatric ED resuscitations.
Introduction
Medication errors are committed by health care providers in virtually all health care settings.1-8 Increased emphasis has been placed on reducing medical errors, particularly drug dosing errors.9 One of the highest risks for medication error exists during pediatric emergencies, with general emergency departments (EDs) being a particularly high-risk setting.8 Pediatric resuscitations are high-stress, high-stakes situations prone to medical errors.10 With limited information, clinicians must make rapid decisions on patient management. Multiple medications are often ordered and need to be delivered quickly and accurately to optimize a child's resuscitation.
The color-coded Broselow Pediatric Emergency Tape (Vital Signs, Inc., Totowa, NJ) was developed to standardize drug dosing according to a length-based estimate of a child's weight. It is one of the most reliable and commonly used tools for pediatric resuscitations.11-14 Unfortunately, this approach does not eliminate dosing errors because clinicians must still calculate the volumes of medications from ampoules to deliver the correct patient dose. Moreover, translation of medications from the Broselow Tape has been evaluated in a limited fashion.15 To our knowledge, until now no one has attempted to develop color-coded, prefilled syringes to be used in conjunction with the Broselow Tape for timely and accurate drug delivery.
The objective of this study was to compare novel, prefilled medication syringes labeled with color-coded volumes corresponding to the weight-based dosing of the Broselow Tape to conventional methods of drug administration in simulated pediatric ED resuscitation scenarios. We hypothesized that time of preparation to administration of drugs would be shorter and the proportion of dosing errors would be lower when color-coded syringes were used compared with conventional medication preparations.
Materials and Methods
Study Design
We performed a prospective, block-randomized, crossover study with data collected during 2 standardized, simulated, pediatric arrest scenarios on May 17, 2011, and repeated 4 to 16 weeks later (June 16, 2011, July 28, 2011, or September 14, 2011) (Figure E1, available online at http://www.annemergmed.com). Randomization was performed by one investigator (ADS) using a coin. On the first day, emergency physician and nurse participants were paired and randomized to begin with one of 2 simulation scenarios: an 8-year-old patient, using the conventional vial/syringe system for drug delivery; or an 8-month-old patient, using the color-coded, prefilled system for drug delivery. After completion of the first scenario, they completed the second scenario with the alternative methodology, performing the crossover on the same day. After an extended washout period of 4 to 16 weeks, teams completed the same scenarios, using both medication delivery methods but in the opposite order.
Study subjects were blinded to the purpose of the study during recruitment to minimize preparation bias; subjects were, however, unblinded to the study objectives during consent and when introduced to the color-coded syringe just before the simulations. The study was approved by the Colorado Multiple Institutional Review Board, and written informed consent was obtained from all participants before their involvement.
Setting
This study was performed at Denver Health Medical Center in Denver, CO. The center is an urban Level I adult and Level II pediatric trauma center with an annual pediatric ED census of approximately 28,000 visits, and is staffed by board-certified emergency physicians, pediatric emergency physicians, and pediatricians.
Selection of Participants
Study participants were recruited from practicing attending emergency physicians and ED nurses in Denver, CO, and included both community-based and academic emergency physicians. All physicians and nurses were required to have completed formal pediatric resuscitation certification (eg, pediatric advanced life support or advanced pediatric life support) and to actively practice in a pediatric emergency care environment. An e-mail describing the general nature of the study but without specific details to ensure blinding was sent to emergency physicians from several acute-care hospitals in the Denver metropolitan region and to ED nursing staff at Denver Health Medical Center. a convenience sample was used, participation was completely voluntary, and subjects were compensated $100 for their participation.
We created a critical care environment by conducting simulations in situ or in actual pediatric resuscitation rooms in the Denver Emergency Center for Children, the pediatric ED at Denver Health Medical Center. Consistent with standard emergency medicine practice, we created clinical care teams consisting of an attending emergency physician, a registered nurse, and a health care technician. Physicians and nurses worked together to perform resuscitations, whereas health care technicians were available to assist with resuscitation by performing chest compressions and bag-valve-mask at the direction of the physician. In accordance with actual clinical practice, teams were not stipulated by study investigators and were not kept the same across scenarios.
Two pediatric critical care scenarios were developed to include advanced airway management and hemodynamic life support efforts, and face validity for each was assessed by a panel of experts in emergency medicine and pediatric emergency medicine and based on national American Heart Association guidelines. Each scenario was piloted and refined before implementation (Appendix E1, available online at http://www.annemergmed.com).
We used the BabySIM and PediaSIM simulation manikins and 2 digital audio and video recorders, one mounted directly above the manikin and focused on the intravenous port (215 PTZ with 12× optical, 4× digital zoom [Axis Communications, Lund, Sweden]) and another mounted in the resuscitation room's corner (212 PTZ with 3× zoom [Axis Communications]) to capture all activity of the scenario. We used METIVision (CAE Healthcare, Saint-Laurent, Quebec, Canada), a fully integrated, digital audio/visual management system to capture and store simulation data.
Before beginning the simulation, each group of participants was instructed to manage the scenario and treat with medication choices as they would in normal practice, using the Broselow Tape for determining drug dosages. Medications anticipated for use during resuscitation were developed as Broselow, color-coded syringes (Figure 1). Participants were instructed to verbalize their thought processes and medication orders during each scenario, and before each scenario, they received a 3-minute training (ie, prerecorded standardized video instruction and hands-on use) of the color-coded syringe method. Specific training was not performed before the conventional medication administration scenarios to simulate standard practice. After initial instructions, a scenario moderator read details of the case presentation to the study subjects before entering the resuscitation room.
Figure 1.

Color-coded, prefilled syringes.
Nurses were provided with a medication kit assembled by an ED pharmacist. Standard kits contained 10-mL vials of induction and paralytic agents, as well as multiple commercially available medications, including epinephrine and atropine. Intervention kits contained the same medications through preloaded color-coded syringes. On the first day, each team was randomly assigned by coin toss to a scenario involving a simulated patient aged 8 years, using a standard medication kit or a scenario involving a simulated patient aged 8 months, and using color-coded prefilled medication syringes in place of the standard ampoules. Each team then participated in the other scenario after a 10-minute intermission. During the simulation, scenario moderators made written notations of used medication vials and syringes where accessible and without interfering with the dynamics of the simulation.
At the completion of both scenarios, physicians and nurses individually completed a closed-response survey. The survey collected data on demographics, perceived difficulty of scenarios, and perceived ease and accuracy of use of the prefilled syringes compared with the conventional methods (Appendix E2, available online at http://www.annemergmed.com). Participants then returned between 4 and 16 weeks later and repeated the scenarios in reverse order, using the opposite medication delivery system for each scenario, and after participation completed an identical survey. Again, participants received the identical 3-minute training for the color-coded, prefilled syringe system before entering the scenario using that method.
Methods of Measurement
Video recordings were used to capture and verify medication choice, dose delivered, and elapsed time of medication preparation to delivery. Video review was conducted by 8 research assistants blinded to the purpose of the study. Research assistants were divided into 4, 2-person groups. Each pair was assigned a set of videos to independently evaluate and abstract either dose or timing data, for either the control system or the color-coded syringe system. Individuals in each group were trained by a study investigator to apply a standardized approach to reviewing the videos to maximize valid and reliable data collection. Groups were trained separately and blinded to the comparative medication delivery system being evaluated. a study investigator served to adjudicate all disagreements.
Outcome Measures
The outcomes were elapsed time (seconds) from initiation of medication preparation to completed administration and “dosing errors” and “critical dosing errors” based on doses published on the Broselow Tape (see definitions of errors below). To minimize the effect of differences in how scenarios were managed between subjects, pauses for assessments, spontaneous questions to the simulation moderator, or inactivity between rounds of medications was not included in elapsed times.
Data Collection and Processing and Primary Data Analysis
Data were manually collected by trained research assistants and entered into an electronic spreadsheet (Microsoft Excel 2010; Microsoft, Redmond, WA) by a study investigator. Data were then transferred into native SAS format (dfPower DBMS Copy; DataFlux Corporation, Cary, NC) and analyses were performed with SAS (SAS Enterprise Guide 4.3; version 9.3; SAS Institute, Inc., Cary, NC) or Stata (version 12; StataCorp, College Station, TX).
Medians with interquartile ranges (IQRs) were calculated for all continuous data and percentages with 95% confidence intervals (CIs) for all categorical data. Consistent with institutional policy and previously used standards, doses deviating more or less than 10% from the published Broselow Tape dose were considered dosing errors.8,16 Because the Broselow Tape dose is indicated for a range of weights within each color zone, a noncritical dosing error range was calculated by applying the milligram per kilogram dose (based on the median weight and the published medication dose for each Broselow Tape color zone) to the lightest and heaviest weights inclusive to that zone. For example, the published epinephrine dose for a child in the “red zone, 8 to 9 kg” is 0.085 mg, with the median weight of 8.5 kg producing a dose of 0.01 mg/kg. The weights inclusive of the red zone were considered to be 7.51 to 9.49 kg, thus indicating an acceptable range of doses to be from 0.0751 mg to 0.0949 mg (Appendix E3, available online at http://www.annemergmed.com). Applying a 10% deviation criterion to that range, doses administered at less than 90% of the minimum correct dose or greater than 110% of the maximum correct dose were designated as critical dosing errors. Alternatively, doses administered outside the correct dosing range but less than or equal to 10% were designated as simply dosing errors. For example, epinephrine doses less than 0.0676 mg (ie, <90% of 0.0751 mg) or greater than 0.104 mg (ie, >110% of 0.0949 mg) were designated critical dosing errors; alternatively, doses from 0.0676 to 0.0751 mg or 0.0949 to 0.104 mg were designated as dosing errors for a child in the red zone.
Nonparametric point estimates and 95% CIs were estimated with the centile and cendif functions in Stata for paired and independent comparisons, respectively. The calculation of median differences with these methods may differ slightly from the value obtained from simple subtraction of group medians. No adjustments were made for multiple comparisons, but variance estimates were adjusted for clustering at the level of the physician/nurse team. Unless stated otherwise, the unit of analysis was medication dose.
With medication dose as the unit of analysis, we used a 2-sided α of .05, accounted for clustering effects at the levels of the team and scenario, and incorporated an adjustment for non-normality for the distributions of data when determining the number of required participants. Ultimately, we estimated requiring 10 participants, 40 simulated scenarios, and approximately 120 medication doses administered to obtain a power of 95% to identify a mean difference of 15 seconds (SD 10 seconds) in administration time between standard and prefilled, color-coded syringe methods (PASS, version 11; NCSS, Kaysville, UT). Although no published data support a clinically meaningful minimum difference in administration of resuscitation medications, we believed a difference of 15 seconds would be clinically meaningful.
Results
Eleven physicians and 10 nurses participated in the study (Table 1). Because of scheduling conflicts among day 1 participants, 3 dates were needed to complete day 2 simulations and only 2 of the 10 nurses were able to be paired with the same emergency physician as on day 1. All physicians were board certified by the American Board of Emergency Medicine and all nurses were licensed and certified to practice in a pediatric ED; all participants had previously completed and had active pediatric advanced life support certification as part of the requirement of their employment.
Table 1.
Demographics of participants (N=21).
| Variable | N | % |
|---|---|---|
| Median age, IQR, y | 39 | 34–43 |
| Male sex | 12 | 57 |
| Number of years in medicine | ||
| 0–5 | 2 | 10 |
| 6–10 | 4 | 19 |
| 11–15 | 5 | 24 |
| 16–20 | 8 | 38 |
| >20 | 2 | 10 |
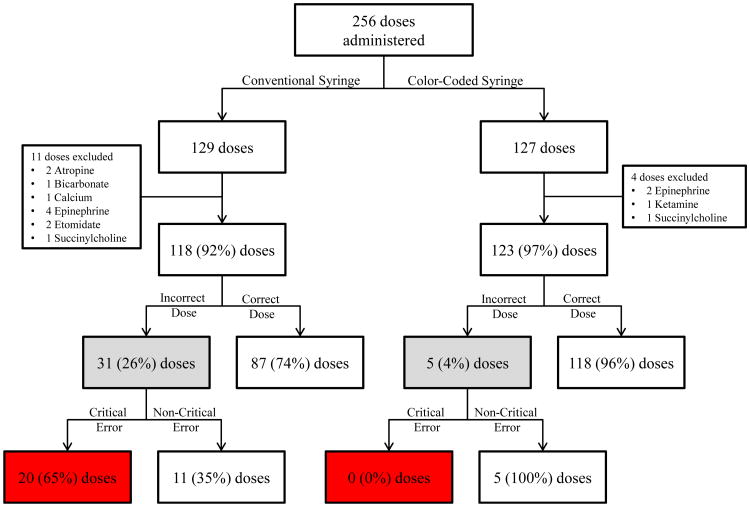
During the scenarios, 256 doses of medication were administered, 129 (50%) using the conventional delivery method and 127 (50%) using the color-coded delivery method. Fifteen total doses were excluded because they were either drawn up and never administered or did not have matching color-coded syringes (calcium and bicarbonate), or because the view of the intravenous port was obscured during review. As a result, 118 doses with the conventional delivery method and 123 doses with the color-coded delivery method were included in the analyses (Figure 2).
Figure 2.
Medication doses administered, stratified by study arm and outcomes.
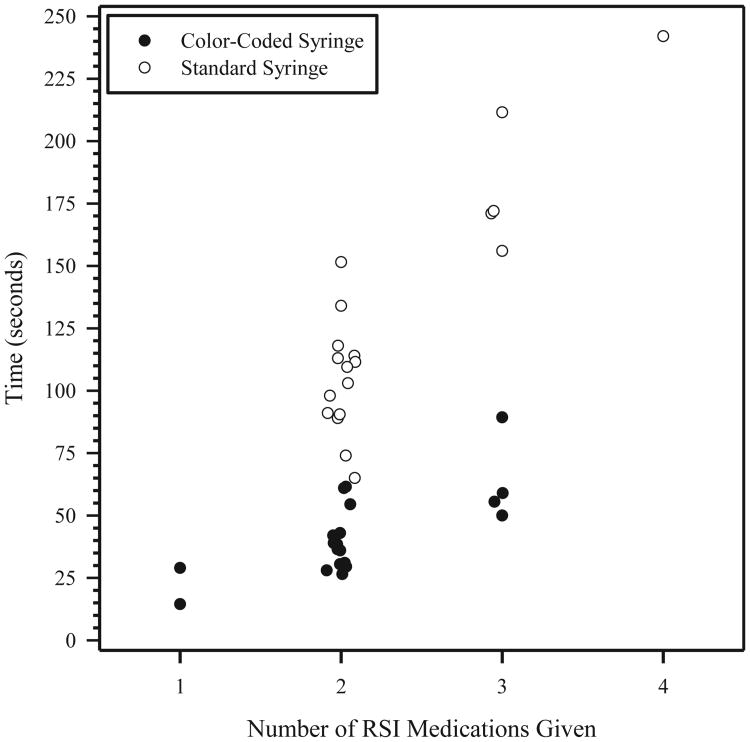
Time from preparation to delivery of all doses was significantly shorter with the color-coded delivery method. Time from preparation to delivery of the first dose of epinephrine or atropine was also significantly shorter with the color-coded delivery method. Finally, time from preparation to delivery of rapid sequence intubation medications was significantly shorter with the color-coded delivery method (Table 2 and Figure 3).
Table 2.
Time to medical delivery (seconds), conventional syringe versus color-coded syringe.
| Conventional Syringe | Color-Coded Syringe | Absolute Difference,* 95% CI | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Variable | Median | 95% CI | Median | 95% CI | ||
| All medications | 47 | 40–53 | 19 | 18–20 | 27 | 21–33 |
| First dose of atropine or epinephrine | 69 | 57–77 | 18 | 16–20 | 48 | 39–58 |
| Rapid sequence intubation medications, No. | ||||||
| 1 | — | 22 | 15–29 | |||
| 2 | 106 | 90–115 | 38 | 30–45 | 64 | 51–79 |
| 3 | 172 | 156–212 | 57 | 50–89 | 114 | 82–156 |
| 4 | 242 | Undefined | — | |||
—, No data.
Nonparametric point estimates and CIs were estimated with the centile and cendif functions of Stata for paired and independent comparisons, respectively. The calculation of median differences with these methods may differ slightly from the value obtained from simple subtraction of group medians.
Figure 3.
Time to preparation of rapid sequence intubation (RSI) medications, standard syringes versus color-coded syringes.
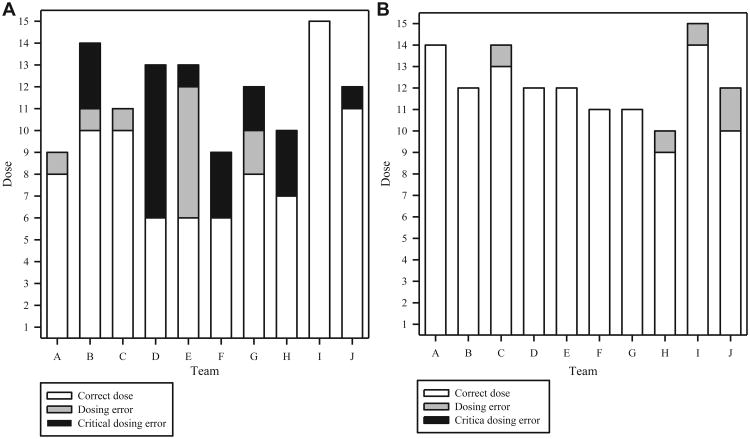
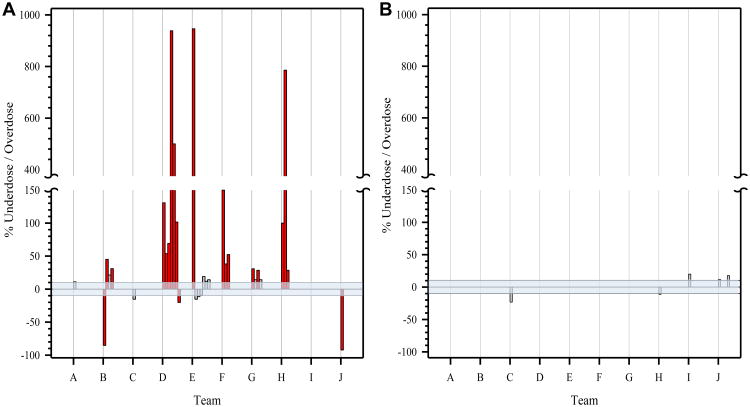
Using the conventional delivery method, 9 of the 10 teams (90%) made at least 1 dosing error and 7 (70%) made 1 or more critical dosing errors. Of the 118 doses administered, 31 (26%; 95% CI 19% to 35%) were dosing errors, with 20 (17%; 95% CI 7% to 16%) classified as critical dosing errors (17 critical overdoses and 3 critical underdoses) (Table 3 and Figures 4A and 5A).
Table 3.
Frequency of errors, conventional syringe versus color-coded syringe.
| Conventional Syringe | Color-Coded Syringe | Absolute Difference, 95% CI | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Variable | N | % | N | % | ||
| Total number of doses administered | 118 | 123 | ||||
| Number of dosing errors* | 31 | 26 | 5 | 4 | 22 | 5–40 |
| Number of doses outside of the Broselow range | 26 | 22 | 4 | 3 | 19 | 3–34 |
| Number of critical dosing errors† | 20 | 17 | 0 | 0 | 17 | 4–30 |
An incorrect dose is defined by a dose that was greater than or equal to 10% or less than or equal to 10% of the published Broselow dose.
Critical dose error defined as a dose administered at less than 90% of the minimum correct Broselow dose or greater than 110% of the maximum correct Broselow dose.
Figure 4.
A, Dosing errors by team, using conventional syringes (N=118 total doses). B, Dosing errors by team, using color-coded, prefilled syringes (N=123 total doses).
Figure 5.
A, Percentage error of incorrect doses (N=31) by team, using the conventional syringe method. The horizontal shaded area represents correct dose range. B, Percentage error of incorrect doses (N=5) by team, using the color-coded syringe method. The horizontal shaded area represents correct dose range.
Using the color-coded method, 4 of the 10 teams (40%) made at least 1 dosing error and 0 made a critical dosing error. Of the 123 doses administered, 5 (4%; 95% CI 1% to 9%) were classified as dosing errors and 0 (95% CI 0% to 3%) as critical dosing errors (Table 3 and Figures 4B and 5B).
Participants rated the difficulty of each scenario similarly. On a 5-point Likert scale in which 1 defined “very difficult” and 5 defined “very easy,” the median values for the 8-year-old patient scenario were 4 (IQR 4 to 4) for color-coded and 3 (IQR 2 to 4) for conventional syringe methods. For the 8-month-old patient scenario, the median values were 3 (IQR 2 to 4) for the color-coded and 4 (IQR 4 to 5) for the conventional syringe methods. Median estimates of training adequacy of the Broselow Tape system was 3 (IQR 3 to 3), color-coded syringe was 3.5 (IQR 3 to 4), and standard syringe was 4 (IQR 3.5 to 4), where 1 represented “poor, I need more training” and 4 represented “confident, I understand it completely.” Comparing ease of use between the color-coded and standard syringe systems resulted in median ratings of 5 (IQR 5 to 5) and 4 (IQR 2 to 3) (P<.001), respectively. Of the 21 participants, 20 (95%) indicated that the prefilled, color-coded syringe would increase their confidence in accurately choosing a dose for a pediatric patient and would be a safer alternative to dose calculation compared with standard syringe methods.
Limitations
Prefilled syringes have been shown to decrease dosing error and time to medication administration.17 To our knowledge, prefilled, color-coded Broselow Tape syringes specific for individual medications are not yet commercially manufactured and prepared in standardized pediatric volumes and have not been evaluated in actual pediatric resuscitations. Results of this simulation study may therefore not translate to actual clinical practice, and although we believe the results are compelling, future pragmatic comparative effectiveness trials may be warranted. Additionally, we assumed that the doses of the medications studied were valid, and such dosing errors, as described, may in fact not negatively affect patient outcomes, although this was not a goal of our study.
Our prefilled syringes were created from the same commercially available syringe sizes used in the standard method, but with Broselow color-coded volumes calibrated and applied by the investigators. The syringe volume per unit length was not optimal for small divisions in the purple and red color zones. The markings differed only by 1/8 to 3/32 inch, and thus delineations may have been difficult to use in a high-stress environment. Although errors were rare with the color-coded syringe, future manufacturing of longer, narrower lumen syringes in 3- and 5-mL volumes with perfected color shadings would provide improved visually distinctive differences.
The study cohort included actively practicing and experienced emergency physicians and nurses, using the same general conventional medication delivery system used in their clinical practices. Thus, satisfactory training and familiarity with the conventional method was presumed. Because only a brief training on the color-coded syringe system was provided just before a scenario was begun, it is possible the proximity of the training to its use within the scenario biased timing results toward improved performance with use of the color-coded syringe system. It was necessary to provide subjects with a minimum level of familiarity with the color-coded syringe system so that they could use it properly. However, the training was considered minimal (total length of the video training was approximately 3 minutes) and would approximate the level of familiarity needed to use the conventional medication delivery system.
This study was performed in 1 setting but with physicians from several EDs and therefore may not generalize to other settings, physicians, or practices. We believe, however, that standardization of medication syringes will inherently reduce time to medication administration and dosing errors regardless of the setting. Misclassification bias may have been introduced during data extraction from video clips; to minimize such bias, research assistants were trained and worked independently, and a study investigator served to adjudicate any discrepancies or disagreements at data entry.
Discussion
This study, conducted in an ED setting, showed that use of a novel, prefilled, color-coded medication delivery system reduced time required to prepare and administer medications, reduced overall dosing errors, and eliminated critical dosing errors during simulated pediatric resuscitations. The prefilled, color-coded syringe system improves the medication delivery process by eliminating calculation as part of the complex cognitive process while using preparations that contain pediatric-specific volumes and color designations for identifying correct medication volumes. To our knowledge, this is the first study to demonstrate the effectiveness of this type of medication administration system by emergency physician and nurse teams, and the results are consistent with those from previous studies demonstrating relatively high dosing errors with conventional drug administration systems4-6 and a study in which paramedics reduced time to administration and dosing errors by using the same color-coded delivery system.18 This provides further evidence for the development of a comparable Broselow Tape–based syringe system for use by emergency care personnel during pediatric resuscitations.
Several factors contribute to dosing errors during resuscitation, including simultaneous actions and multiple sequential cognitive steps beginning from the time of deciding to administer a medication to its actual administration.19 These steps include accurate estimation of weight, calculation of weight-based doses, and conversion of the doses in milligrams to milliliters before actual administration. Although the former 2 steps may be facilitated by use of a Broselow Tape,10,20 significant dosing error may still occur during the latter step, in which manual cognitive actions are currently required.21 Furthermore, clinicians occasionally have to choose from more than 1 concentration of the same medication (eg, epinephrine, dextrose), further complicating the process. As such, use of standardized, prefilled syringes may significantly mitigate dosing errors during resuscitations.
Medication dosing errors are also more likely to occur during the care of the acutely ill or injured patient.8,22 Resuscitations in pediatrics are uncommon, and despite pediatric-specific guidelines, pediatric cardiac arrests have poor outcomes.23 It is thought that during pediatric resuscitations, there is increased “cognitive load” or increased intellectual burden on providers running the resuscitation.24 Activities can be divided into nonautomatic actions and automatic actions. Automatic actions are those that are performed without conscious thought, whereas nonautomatic actions require conscious intellectual input, including performing drug dosing calculations. These nonautomatic activities can lead to delay in implementation time and increase the potential for error.21 Park25 noted that there was a 3% error rate in calculations done by individuals. When those calculations were reviewed by a second person, the error rate increased to 10%. In situations of stress, the error rate increased to approximately 25%.
Because calculations increase cognitive load and can lead to delay in care and errors, diminishing the need for calculations during resuscitations could have an effect on the care of the pediatric patient. By reducing the need for calculations, the color-coded syringe correlated to the Broselow Tape reduced time to delivery of medication and medication dosing errors. By removing calculations from the duties performed, we have reduced cognitive load and allowed the nurse and physician to divert their attention to other aspects of the resuscitation. Though it is unclear whether decreasing time to medication delivery will ultimately affect resuscitation outcomes, we assume that quicker and more accurate dosing will optimize outcomes.26
In summary, novel color-coded prefilled syringes decrease time to medication administration and significantly reduce critical dosing errors by emergency physician and nurse teams during simulated pediatric ED resuscitations. Implementing systems that eliminate calculations during ED management of pediatric emergencies may reduce potentially harmful mistakes, therefore contributing to improved patient outcomes.
Supplementary Material
Figure E1. Study design schematic.
Acknowledgments
The authors acknowledge Christine Black, MD, Mark Brownson, MD, Claire Chappell, MS, Amy Dear-Ruel, BS, Melissa O'Meara, BA, Ramya Mishra, MD, Adam Plate, MD, and Ashley Phipps, MD, for their participation as research assistants; Kevin Kaucher, PharmD, for development of study materials, including medication vials; Comilla Sasson, MD, PhD, for her suggestions related to the article; and the emergency physicians and nurses who participated as study subjects.
Funding and support: By Annals policy, all authors are required to disclose any and all commercial, financial, and other relationships in any way related to the subject of this article as per ICMJE conflict of interest guidelines (see www.icmje.org). This study was funded by an unrestricted grant from the COPIC Medical Foundation, Denver, CO. Dr. Haukoos was supported, in part, by an Independent Scientist Award (K02HS017526) from the Agency for Healthcare Research and Quality and an Investigator-Initiated Grant (R01AI106057) from the National Institutes of Health. Dr. Hernandez holds a pending patent for the color-coded, prefilled syringes used in this study but has not marketed or received payment for them.
Footnotes
Author contributions: ADS and JSH had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analyses. CH was responsible for color-coded syringe design and obtaining funding. CH and JSH were responsible for the study concept. MEM, CH, ADS, SJ, MS, JRB, EH, KB, and JSH were responsible for the study design. CH, ADS, SJ, MS, and JRB were responsible for acquisition of data. ADS, EH, and JSH were responsible for statistical analyses. MEM, CH, ADS, EH, and JSH were responsible for interpretation of results. MEM, ADS, and JSH were responsible for drafting the article. All authors were responsible for critical revision of the article for important intellectual content. ADS, SJ, JRB, EH, and JSH were responsible for administrative, technical, and material support. JSH was responsible for study supervision. JSH takes responsibility for the paper as a whole.
The COPIC Medical Foundation had no role in the design, conduct, or reporting of this study.
Presented at the American Heart Association Resuscitation Science Symposium, November 2012, Los Angeles, CA.
References
- 1.Barker KN, Flynn EA, Pepper GA, et al. Medication errors observed in 36 health care facilities. Arch Intern Med. 2002;162:1897–1903. doi: 10.1001/archinte.162.16.1897. [DOI] [PubMed] [Google Scholar]
- 2.Doherty C, McDonnell C. Tenfold medication errors: 5 years' experience at a university-affiliated pediatric hospital. Pediatrics. 2012;129:916–924. doi: 10.1542/peds.2011-2526. [DOI] [PubMed] [Google Scholar]
- 3.Folli HL, Poole RL, Benitz WE, et al. Medication error prevention by clinical pharmacists in two children's hospitals. Pediatrics. 1987;79:718–722. [PubMed] [Google Scholar]
- 4.Ghaleb MA, Barber N, Franklin BD, et al. The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Child. 2010;95:113–118. doi: 10.1136/adc.2009.158485. [DOI] [PubMed] [Google Scholar]
- 5.Hoyle JD, Davis AT, Putman KK, et al. Medication dosing errors in pediatric patients treated by emergency medical services. Prehosp Emerg Care. 2012;16:59–66. doi: 10.3109/10903127.2011.614043. [DOI] [PubMed] [Google Scholar]
- 6.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA. 2001;285:2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- 7.Maidment ID, Lelliott P, Paton C. Medication errors in mental healthcare: a systematic review. Qual Saf Health Care. 2006;15:409–413. doi: 10.1136/qshc.2006.018267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marcin JP, Dharmar M, Cho M, et al. Medication errors among acutely ill and injured children treated in rural emergency departments. Ann Emerg Med. 2007;50:361–367. doi: 10.1016/j.annemergmed.2007.01.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Institute of Medicine. To err is human: building a safer health system. [Accessed December 1, 2014];1999 Available at: http://www.iom.edu/w/media/Files/Report%20Files/1999/To-Err-is-Human/To%20Err%20is%20Human%201999%20%20report%20brief.pdf.
- 10.Kaji AH, Gausche-Hill M, Conrad H, et al. Emergency medical services system changes reduce pediatric epinephrine dosing errors in the prehospital setting. Pediatrics. 2006;118:1493–1500. doi: 10.1542/peds.2006-0854. [DOI] [PubMed] [Google Scholar]
- 11.Krieser D, Nguyen K, Kerr D, et al. Parental weight estimation of their child's weight is more accurate than other weight estimation methods for determining children's weight in an emergency department. Emerg Med J. 2007;24:756–759. doi: 10.1136/emj.2007.047993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lubitz DS, Seidel JS, Chameides L, et al. A rapid method for estimating weight and resuscitation drug dosages from length in the pediatric age group. Ann Emerg Med. 1988;17:576–581. doi: 10.1016/s0196-0644(88)80396-2. [DOI] [PubMed] [Google Scholar]
- 13.Luten RC, Zaritsky A, Wears R, et al. The use of the Broselow tape in pediatric resuscitation. Acad Emerg Med. 2007;14:500–501. doi: 10.1197/j.aem.2007.02.015. [DOI] [PubMed] [Google Scholar]
- 14.So TY, Farrington E, Absher RK. Evaluation of the accuracy of different methods used to estimate weights in the pediatric population. Pediatrics. 2009;123:e1045–e1051. doi: 10.1542/peds.2008-1968. [DOI] [PubMed] [Google Scholar]
- 15.Barata IA, Benjamin LS, Mace SE, et al. Pediatric patient safety in the prehospital/emergency department setting. Pediatr Emerg Care. 2007;23:412–418. doi: 10.1097/01.pec.0000278393.32752.9f. [DOI] [PubMed] [Google Scholar]
- 16.McPhillips HA, Stille CJ, Smith D, et al. Potential medication dosing errors in outpatient pediatrics. J Pediatr. 2005;147:761–767. doi: 10.1016/j.jpeds.2005.07.043. [DOI] [PubMed] [Google Scholar]
- 17.Adapa RM, Mani V, Murray LJ, et al. Errors during the preparation of drug infusions: a randomized controlled trial. Br J Anaesth. 2012;109:729–734. doi: 10.1093/bja/aes257. [DOI] [PubMed] [Google Scholar]
- 18.Moreira ME, Stevens AD, Hernandez CS, et al. Novel, color-coded prefilled syringe significantly decreases time to medication administration, preparation for endotracheal intubation, and eliminates critical dosing errors in simulated pediatric resuscitations. Circulation. 2012;126:2798. abstract. [Google Scholar]
- 19.Glover ML, Sussmane JB. Assessing pediatrics residents' mathematical skills for prescribing medication: a need for improved training. Acad Med. 2002;77:1007–1010. doi: 10.1097/00001888-200210000-00013. [DOI] [PubMed] [Google Scholar]
- 20.Feleke R, Kalynych CJ, Lundblom B, et al. Color coded medication safety system reduces community pediatric emergency nursing medication errors. J Patient Saf. 2009;5:79–85. doi: 10.1097/PTS.0b013e3181a647ab. [DOI] [PubMed] [Google Scholar]
- 21.Luten R. Error and time delay in pediatric trauma resuscitation: addressing the problem with color-coded resuscitation aids. Surg Clin North Am. 2002;82:303–314. doi: 10.1016/s0039-6109(02)00007-5. [DOI] [PubMed] [Google Scholar]
- 22.Oakley PA. Inaccuracy and delay in decision making in paediatric resuscitation, and a proposed reference chart to reduce error. BMJ. 1988;297:817–819. doi: 10.1136/bmj.297.6652.817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Donoghue AJ, Nadkarni V, Berg RA, et al. Out-of-hospital pediatric cardiac arrest: an epidemiologic review and assessment of current knowledge. Ann Emerg Med. 2005;46:512–522. doi: 10.1016/j.annemergmed.2005.05.028. [DOI] [PubMed] [Google Scholar]
- 24.Luten R, Wears RL, Broselow J, et al. Managing the unique size-related issues of pediatric resuscitation: reducing cognitive load with resuscitation aids. Acad Emerg Med. 2002;9:840–847. doi: 10.1111/j.1553-2712.2002.tb02175.x. [DOI] [PubMed] [Google Scholar]
- 25.Park K. Human Error. New York, NY: Wiley; 1997. pp. 150–173. [Google Scholar]
- 26.Kozer E, Seto W, Verjee Z, et al. Prospective observational study on the incidence of medication errors during simulated resuscitation in a paediatric emergency department. BMJ. 2004;329:1321. doi: 10.1136/bmj.38244.607083.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure E1. Study design schematic.