Abstract
Objective
Cortisol reactivity to stress is associated with affective eating, an important behavioral risk factor for obesity and related metabolic diseases. Yoga practice is related to decreases in stress and cortisol levels, thus emerging as a potential targeted complementary intervention for affective eating. This randomized controlled trial examined the efficacy of a heated, hatha yoga intervention for reducing cortisol reactivity to stress and affective eating.
Method
Females (N = 52; ages 25–46; 75% White) at risk for obesity and related illnesses were randomly assigned to 8 weeks of Bikram Yoga practice or to waitlist control. Cortisol reactivity to and number of snacks consumed following a laboratory stress induction were measured at weeks 0 (pretreatment) and 9 (posttreatment). Self-reported binge eating frequency and coping motives for eating were assessed at weeks 0, 3, 6, and 9.
Results
Among participants with elevated cortisol reactivity at pre-treatment (“high-reactors”), those randomized to the yoga condition evidenced greater pre- to posttreatment reductions in cortisol reactivity (p = .042, d = .85), but there were not significant condition differences for the “low reactors” (p = .178, d = .53). Yoga participants reported greater decreases in binge eating frequency (p = .040, d = .62) and eating to cope with negative affect (p = .038, d = .54).
Conclusions
This study provides preliminary support for the efficacy of heated hatha yoga for treating physiological stress reactivity and affective eating among women at risk for obesity-related illnesses.
Keywords: Yoga, Eating, Stress, Cortisol, Obesity
Eating in response to stress or negative emotions is a risk factor for obesity and related illnesses (Epel et al., 2004). Women who intentionally restrict food intake to control weight (i.e., high in dietary restraint) constitute a particularly high-risk group because, relative to males also high in dietary restraint, they are more likely to engage in affective eating and to gain weight as a result (Drapeau et al., 2003; Wardle et al., 2000). Growing evidence suggests that dietary restraint results in affective eating in part due to cortisol hyperreactivity to stress (Adam & Epel, 2007; Epel et al., 2001; Newman et al., 2007; Roberts et al., 2014). Together, these findings support the development of specialized interventions that target cortisol hyperreactivity to stress.
In this manuscript, we report on the results of a randomized controlled trial that aimed to evaluate the efficacy of a heated hatha yoga intervention to reduce cortisol reactivity to stress and affective eating in women high in dietary restraint. We selected heated hatha yoga as an intervention to engage this treatment target because it specifically aims to teach individuals to regulate their emotional responding and to persist while being exposed to heat and new or uncomfortable bodily sensations (i.e., a stressor). Like aerobic exercise, yoga results in sympathetic activation through the practice of asana (i.e., physical postures) and certain types of pranayama (i.e., breathing exercises; Bidwell et al., 2012; Sarang & Telles, 2006; Telles et al., 2011) and may similarly function as repeated, prolonged exposure, thereby improving emotional responding in stressful situations. In addition, the meditative and relaxation aspects of yoga result in reduced sympathetic activity and increased vagal tone (Ross & Thomas, 2010; Sarang & Telles, 2006; Telles et al., 2013). Thus, the physiological mechanisms of hatha yoga may differ from more traditional aerobic exercise due to this alternation between sympathetic and parasympathetic activation. Consistent with this hypothesis are findings from West et al. (2004), who showed that, while hatha yoga and aerobic exercise (African dance) both resulted in reduced perceived stress, only yoga significantly reduced salivary cortisol. Support for using yoga as an intervention for women high in dietary restraint also comes from research showing that yoga can lead to significant decreases in salivary cortisol secretions and improvements in self-reported stress, anxiety, depression, emotional well-being, and disordered eating across samples of women (Banasiket et al., 2010; Carei et al., 2010; McIver et al., 2009; Michalsen et al., 2005).
The primary aim of this study was to examine the effects of an 8-week heated hatha yoga intervention on cortisol reactivity to stress. Secondly, we examined intervention effects on self-report measures of binge eating and affective eating. We expected that, relative to a waitlist control condition, at-risk women assigned to yoga would evidence greater improvements across all measures. In light of extant work demonstrating that the link between cortisol reactivity and affective eating is greater for high versus low “reactors,” we also expected that the effect of yoga on cortisol reactivity would be stronger for those who were initially high in cortisol reactivity.
Method
Design
Consistent with NIH guidelines for developing and standardizing behavioral therapies (Rounsaville et al., 2001), this trial examined the effects of a novel, community-based yoga intervention for stress reactivity and affective eating (i.e., Stage 1b trial) using a prospective, parallel research design with roughly equivalent allocation to each treatment arm. Before recruitment began, the first author generated a random allocation sequence using an online random number generator. The sequence was kept in a password-protected spreadsheet. At the end of each participant’s baseline assessment, a research assistant opened the spreadsheet and assigned the participant to the condition corresponding to the next number on the list.
Participants
We recruited a community sample of 52 females between April 2012 and May 2013. Recruitment materials presented the trial as a “study examining the effects of hot yoga on stress-relief and mental health.” Age was restricted to 25 to 45 years in light of age-related variations in estrogen levels that affect HPA reactivity in women (Seeman et al., 2001). Eligibility criteria also included: (1) elevated perceived stress (i.e., score ≥ 0.5 SD above the community mean on the Perceived Stress Questionnaire; Levenstein et al., 1993); (2) classification as a restrained eater (i.e., score of ≥ 15 on the Restraint Scale; Polivy et al., 1988); (3) elevated emotional eating (i.e., score of ≥ 2.06 on the Dutch Emotional Eating Scale; van Strien et al., 1986); (4) stable physical activity levels; and (5) written physician medical clearance. Exclusion criteria were: (1) regular practice of yoga; (2) presence of psychiatric or physical health conditions that would interfere with safety, and (3) concurrent mental health treatment of any kind.
Procedures
Baseline visit
Participants completed the baseline visit within the first 5 days of the follicular stage of their menstrual cycle and between 4:00 and 5:30 PM. The session lasted 3 hours and involved a baseline period, a series of laboratory stressors, and a recovery period. The stressors lasted approximately 30 minutes and included a modified Trier Social Stress Test (TSST; Kirschbaum et al., 1993), a breath-holding challenge, and a computerized mirror-tracing task. Salivary cortisol samples were collected seven times during the visit: twice during the half-hour baseline period (at −30″ and −15″), at onset of stressors (at 0″), during stressors (at +15″), at cessation of stressors (at +30″), and during recovery (at +60″ and +90″).
Intervention period
Yoga participants were instructed to attend at least two 90-minute yoga classes per week for 8 weeks. All yoga classes took place at a Bikram Yoga studio. Each class consisted of a standardized series of 26 hatha yoga postures, two breathing exercises, and two savasanas (i.e., a resting/relaxation posture) in a room heated to 104° F. Participants assigned to waitlist received an 8-week membership following the 8-week waitlist period. All participants completed online self-report measures at the end of each week.
Posttreatment visit
One week following the last yoga session, and within the first 5 days of the follicular stage, participants completed a posttreatment assessment that mirrored the Baseline Visit section, with the exception that the TSST speech topic was altered to provide a novel challenge. In order to blind participants, the study was presented as an examination of the effects of yoga practice on stress and mental health, without reference to eating behavior. Participants were debriefed at the end of the posttreatment assessment.
Assessment
Cortisol reactivity to stress
Cortisol samples were collected with synthetic salivettes (Sarstedt, Rommelsdorf, Germany) and assayed with an enzyme immunoassay in duplicate. The mean of the two values (expressed in ug/dL) was used for analyses. Examination of raw data suggested that cortisol levels peaked between 30 and 60 minutes following the onset of stressors (i.e., between samples +30″ and +60″). Meta-analysis has shown that cortisol typically peaks between 21 and 40 after stressor onset (Dickerson & Kemeny, 2004). Although overlapping with this established stressor onset-to-peak interval, cortisol levels in the current study may have peaked later and/or longer due to the acuteness and novelty of our third and final stressor task, mirror-tracing. Preliminary analyses revealed that cortisol increase in response to stress was best reflected in the 60-minute interval from the third sample (taken at 0″, i.e., stressor onset) to the sixth sample (taken at +60″, i.e., 60 min following stressor onset and approximately 30 min following stressor cessation). AUCI for cortisol reactivity for this study was thus calculated using the third (0″) through sixth (+60″) samples from each participant. Consistent with extant research (Fekedulegn’s et al., 2007; van Strien et al., 2013), we used area under the curve “with respect to increase” (AUCI) to represent cortisol reactivity. Cortisol reactivity values for each participant at both time points were scrutinized for outliers, defined as 3 SDs above or below the mean AUCI for each time point. Of the 89 AUCI values, there were two outliers above the mean and none below; these were replaced with the value 3 SD above the baseline AUCI mean.
Self-report measures
Binge eating frequency was assessed using item 8 of the Eating Disorder Diagnostic Scale (EDDS; Stice, Fisher, & Martinez, 2004). Coping motives for eating was assessed with the 18-item subscale of the Eating Expectancies Inventory (EEI; Hohlstein et al., 1998). Dietary restraint, examined as a covariate, was measured with the 10-item Dutch Restrained Eating Scale (DRES; van Strien et al., 1986).
Data Analytic Strategy
We used multilevel modeling (MLM) to analyze condition differences in outcomes and in slopes of change from pre- to posttreatment. MLM is an intent-to-treat approach that includes all subjects regardless of missing data. We used maximum-likelihood estimation and centered the Time variable at posttreatment so that the intercept and main effects would reflect scores at posttreatment. Level 1 of the model was composed of the intercept and time (pre/post), and treatment condition and baseline levels of the dependent variable (Raab et al., 2000) were included as level 2 predictors of the intercept and time. Because age varied by condition (see Table 1), dietary restraint is clinically prognostic of affective eating, and hormonal contraception use is related to cortisol levels, these three variables were examined as covariates in all analyses, but dropped from models if they were not significant (p > .10). The natural logs (Ln) of skewed continuous variables (cortisol reactivity) were used in all the models. Effect sizes for condition differences in change over time were estimated in accordance with Feingold (2013), and effect sizes for differences in posttreatment values were estimated using t to d transformation.
Table 1.
Baseline and Post-treatment Means (M) and Standard Deviations (SD), by Condition
| Yoga (n = 27)
|
Waitlist (n = 25)
|
|||
|---|---|---|---|---|
| Baseline | Post-treatment | Baseline | Post-treatment | |
| Body mass index (BMI) | n = 27 | n = 17 | n = 25 | n = 22 |
| M = 28.41 | M = 26.63 | M = 26.30 | M = 26.67 | |
| SD = 4.59 | SD = 2.94 | SD = 5.53 | SD = 5.65 | |
| Dietary restraint (DRES) | n = 27 | n = 20 | n = 24 | n = 22 |
| M = 2.83* | M = 2.87 | M = 3.17* | M = 2.91 | |
| SD = 0.55 | SD = 1.00 | SD = 0.55 | SD = 0.94 | |
| Cortisol reactivity (AUCI) | n = 27 | n = 18 | n = 24 | n = 20 |
| M = 3.52 | M = 0.67 | M = 2.35 | M = 1.31 | |
| SD = 4.94 | SD = 2.08 | SD = 3.95 | SD = 3.60 | |
| Perceived stress (PSQ) | n = 27 | n = 21 | n = 24 | n = 22 |
| M = 0.63 | M = 0.35* | M = 0.57 | M = 0.46* | |
| SD = 0.15 | SD = 0.16 | SD = 0.14 | SD = 0.16 | |
| Coping motives for eating (EEI scale 1) | n = 27 | n = 20 | n = 24 | n = 22 |
| M = 78.78 | M = 59.20 | M = 72.67 | M = 66.14 | |
| SD = 20.02 | SD = 22.14 | SD = 24.56 | SD = 25.44 | |
| Binge eating frequency (EDDS item 8) | n = 27 | n = 20 | n = 24 | n = 22 |
| M = 3.70 | M = 1.60 | M = 2.42 | M = 2.45 | |
| SD = 3.54 | SD = 1.05 | SD = 1.61 | SD = 3.11 | |
Note.
p < .05
Results
Preliminary Analyses
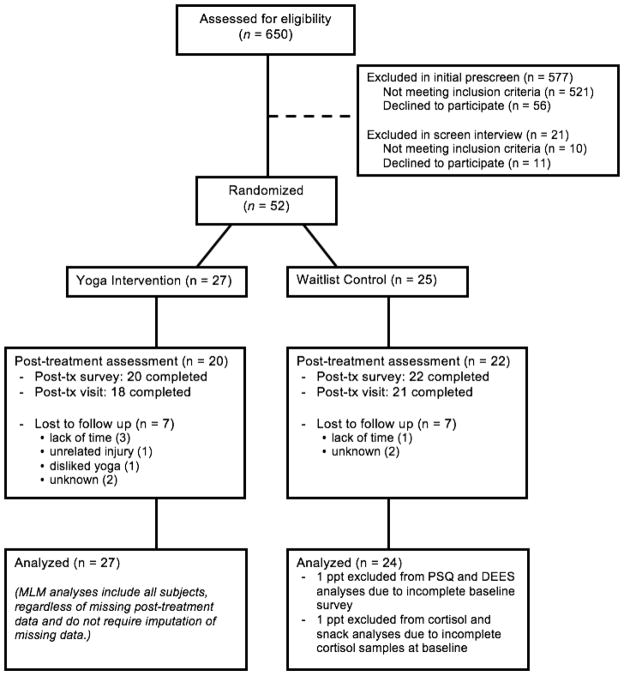
Figure 1 shows participant flow. The sample (N = 52; M age = 33.5, SD = 6.4) was predominantly middle to upper-middle class, with 40 participants (77%) reporting at least a college degree and 58.7% reporting an annual household over $50K. The majority identified as Caucasian (n = 39, 75.0%), 11 as African American/Black (21.2%), 2 as Asian (3.8%), and 10 as Hispanic/Latina (19.2%). Baseline and posttreatment means and standard deviations for the primary study variables are shown in Table 1. No between-group differences were evident for any demographic variables or baseline clinical variables, except that participants assigned to yoga were younger (31.5 vs. 35.7 years old; F(1,50) = 5.96, p = .018) and reported less restrained eating (F(1,49) = 4.87, p = .032). Average weekly yoga class attendance ranged from 0.13 to 3.25 sessions per week (M = 1.56, SD = 0.82).
Figure 1.
CONSORT Flow Diagram.
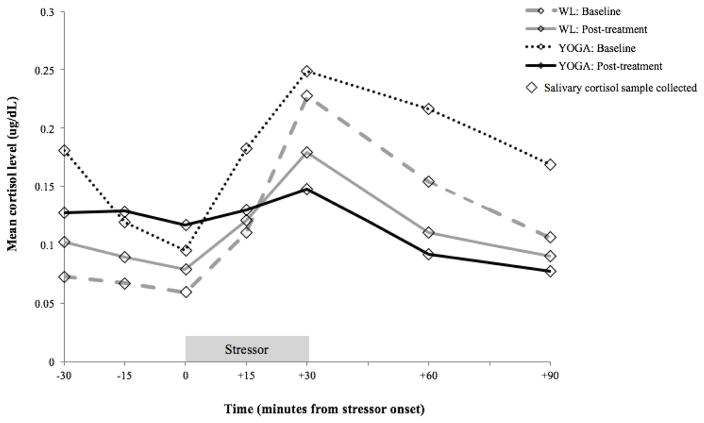
Effects of Yoga on Cortisol Reactivity to Stress
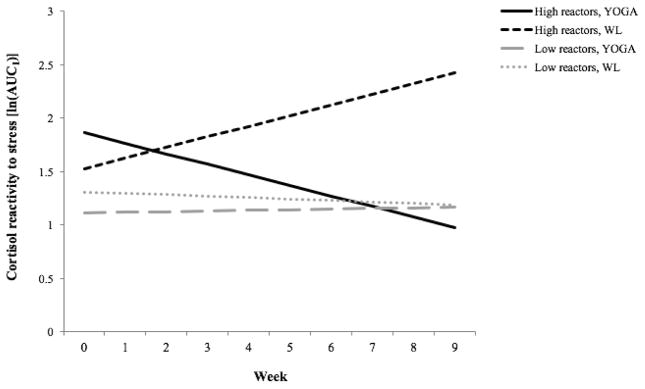
As predicted, the three-way interaction of Time, Condition, and Initial Reactivity was significant (b = −0.46, t(89) = −2.07, p = .041). The interaction was probed by re-running the model with initial cortisol reactivity centered at 1.5 SD above and below the mean (see Figures 2 and 3). Among the “high reactors,” those randomized to yoga had greater decreases in cortisol reactivity over time (b = −0.52, t(89) = −2.06, p = .042, d = 0.85) and lower reactivity levels at posttreatment (b = −0.49, t(89) = −2.54, p = .013, d = 0.54). Among the “low reactors,” there were no condition differences in cortisol reactivity changes over time (b = 0.32, t(89) = 1.36, p = .178, d = 0.53) or in posttreatment cortisol reactivity values (b = 0.34, t(89) = 1.99, p = .055, d = 0.42).
Figure 2.
Baseline and posttreatment curves for cortisol reactivity (ug/dL) in response to the laboratory stress induction, by treatment condition.
Figure 3.
Condition differences in cortisol reactivity [ln(AUCI)] changes from baseline (week 0) to postintervention (week 9), by initial cortisol reactivity levels.
Effects of Yoga on Self-Reported Eating Behavior
Consistent with hypothesis, participants assigned to yoga reported significantly greater decreases in binge eating frequency over time (b = −0.59, t(179) = −2.07, p = .040, d = 0.62) and at posttreatment (b = −1.87, t(179) = −3.21, p = .001, d = 0.48) relative to participants assigned to waitlist. Similarly, participants assigned to yoga evidenced significantly greater reductions in coping-oriented motives for eating (b = −3.97, t(179) = −2.09, p = .038, d = 0.54) and lower levels at posttreatment (b = −12.13, t(179) = −3.26, p = .001, d = 0.49) relative to waitlist participants.
Discussion
This study aimed to test the efficacy of an 8-week heated yoga intervention for reducing cortisol reactivity to stress and affective eating among an at-risk group of women high in dietary restraint. Our findings showed a significant advantage of yoga over waitlist for reducing self-reported binge eating frequency and coping-oriented motives for eating, as well as for reducing cortisol reactivity to stress, although statistical significance of the effects on the latter treatment target only emerged among women who evidenced elevated cortisol reactivity to stress at the baseline visit prior to the intervention.
Follow-up research must build upon these findings by including repeated measures of both the putative treatment mechanism (i.e., cortisol reactivity) and outcome (affective eating) and conducting formal mediation analysis (testing for causality). This research may consider testing stress chronicity as a moderator of the relation between physiological reactivity to acute stress and affective eating. Indeed, recent research has suggested that over time, affective eaters experience a down-regulation of their HPA-axis stress responses, as a result of chronic stress, affective eating, and obesity (Tomiyama et al., 2011). Because our findings relating heated yoga practice to reduced HPA-axis reactivity suggest that this intervention may have effects beyond reducing affective eating (Chrousos & Gold, 1998), it would be worthwhile to test its efficacy on other relevant psychiatric and health outcomes in this at-risk group.
This study has a number of limitations. First, our use of a waitlist control group limits conclusions about intervention specificity. Using contact control and active interventions as a basis of comparison will be important for future studies. Here, it may be particularly useful to include both exercise and mindfulness-based non-physical activity control conditions, as such comparators would help dismantle the efficacy of the yoga intervention. Second, the effect sizes and statistical significance (and lack thereof) of our findings cannot be generalized to other forms of yoga. Bikram yoga is a heated style of yoga, and less intense or more meditative types of yoga may have different effects on both physiology and behavior. Similarly, these findings should not be generalized to all women. Women in this sample were 25–46 years of age and were selected for their elevated levels of stress, dietary restraint, and affective eating. Third, despite careful randomization, women randomized to yoga tended to be younger and less restrained in their eating. However, we controlled for age and dietary restraint in analyses in which they were associated with the outcome variable at the p < .10 level. Fourth, although 60% of participants completed the 8-week yoga intervention, only 37% of the participants assigned to yoga condition met the prescribed two classes per week. Such findings call for research examining predictors of yoga adherence as well as studies that examine dose-response relations by manipulating dose.
In conclusion, this study provides initial evidence for the efficacy of Bikram yoga for reducing cortisol reactivity to stress and self-reported binge eating and coping motives for eating. Keeping in mind the rise in popularity of complementary and integrative approaches, this research, if replicated and extended, may aid the goal to develop more effective interventions that can reach more people in need.
Public Health Significance.
By targeting key behavioral and physiological mechanisms, yoga interventions may help address the obesity epidemic. This study provides initial support for the use of heated hatha yoga for improving cortisol reactivity and affective eating among women at risk for weight gain and obesity-related illnesses.
Acknowledgments
Funding: Research reported in this manuscript was in part supported by grants R01 DA027533, K01 DA035930, and F31 DA036919 awarded by the National Institute on Drug Addiction. Cortisol assays for this study were funded by a grant from Pure Action, Inc., Austin, TX, USA, a 501c3 nonprofit organization.
Footnotes
Trial Registration: ClinicalTrials.gov, NCT01652807, https://clinicaltrials.gov/ct2/show/NCT01652807
Declarations of Interest: Dr. Smits receives royalties from Oxford University Press for books on exercise as a treatment for mood and anxiety disorders. Drs. Hopkins, Rosenfield, Powers, Ms. Medina, and Ms. Baird report no financial relationships with commercial interests.
References
- Adam TC, Epel ES. Stress, eating, and the reward system. Physiology & Behavior. 2007;91:449–458. doi: 10.1016/j.physbeh.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Banasik J, Williams H, Haberman M, Blank SE, Bendel R. Effect of lyengar yoga practice on fatigue and diurnal salivary cortisol concentration in breast cancer survivors. Journal of the American Academy of Nurse Practitioners. 2010;23:135–142. doi: 10.1111/j.1745-7599.2010.00573.x. [DOI] [PubMed] [Google Scholar]
- Bidwell A, Yazel B, Davin D, Fairchild TJ, Kanaley JA. Yoga training improves quality of life in women with asthma. The Journal of Complementary and Alternative Medicine. 2012;18:755. doi: 10.1089/acm.2011.0079. [DOI] [PubMed] [Google Scholar]
- Carei TR, Fyfe-Johnson AL, Breuner CC, Brown MA. Randomized controlled clinical trial of yoga in the treatment of eating disorders. Journal of Adolescent Health. 2010;46:346–351. doi: 10.1016/j.jadohealth.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chrousos GP, Gold PW. Editorial: A healthy body in a healthy mind – and vice versa – the damaging power of uncontrollable stress. Journal of Clinical Endocrinology. 1998;83:1842–1845. doi: 10.1210/jcem.83.6.4908. [DOI] [PubMed] [Google Scholar]
- Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: A theoretical integration and synthesis of laboratory research. Psychological Bulletin. 2004;130:355–391. doi: 10.1037/0033-2909.130.3.355. [DOI] [PubMed] [Google Scholar]
- Drapeau V, Provencher V, Lemieux S, Després J, Bouchard C, Tremblay A. Do 6-y changes in eating behaviors predict changes in body weight? Results from the Québec Family Study. International Journal of Obesity. 2003;27:808–814. doi: 10.1038/sj.ijo.0802303. [DOI] [PubMed] [Google Scholar]
- Epel E, Jimenez S, Brownell K, Stroud L, Toney C, Niaura R. Are stress eaters at risk for the metabolic syndrome? Annals of the New York Academy of Sciences. 2004;1032:208–210. doi: 10.1196/annals.1314.022. [DOI] [PubMed] [Google Scholar]
- Epel E, Lapidus R, McEwen B, Brownell K. Stress may add bite to appetite in women: a laboratory study of stress-induced cortisol and eating behavior. Psychoneuroendocrinology. 2001;26:37–49. doi: 10.1016/s0306-4530(00)00035-4. [DOI] [PubMed] [Google Scholar]
- Feingold A. A regression framework for effect size assessments in longitudinal modeling of group differences. Review of General Psychology. 2013;17:111–121. doi: 10.1037/a0030048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fekedulegn DB, Andrew ME, Burchfiel CM, Violanti JM, Hartley TA, Charles LE, Miller DB. Area under the curve and other summary indicators of repeated waking cortisol measurements. Psychosomatic Medicine. 2007;69(7):651–659. doi: 10.1097/PSY.0b013e31814c405c. [DOI] [PubMed] [Google Scholar]
- Hohlstein LA, Smith GT, Atlas JG. An application of expectancy theory to eating disorders: Development and validation of measures of eating and dieting expectancies. Psychological Assessment. 1998;10:49–58. [Google Scholar]
- Kirschbaum C, Pirke K, Hellhammer D. The “Trier Social Stress Test”- a toll for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993;28:76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Levenstein S, Prantera C, Varvo V, Sribano ML, Berto E, Luzi C, Andreoli A. Development of the Perceived Stress Questionnaire: A new tool for psychosomatic research. Journal of Psychosomatic Research. 1993;37:19–32. doi: 10.1016/0022-3999(93)90120-5. [DOI] [PubMed] [Google Scholar]
- McIver S, O’Halloran P, McGartland M. Yoga as a treatment for binge eating disorder: A preliminary study. Complementary Therapies in Medicine. 2009;17:196–202. doi: 10.1016/j.ctim.2009.05.002. [DOI] [PubMed] [Google Scholar]
- Michalsen A, Grossman P, Acil A, Langhorst J, Lüdtike R, Esch T, … Dobos GJ. Rapid stress reduction and anxiolysis among distressed women as a consequence of a three-month intensive yoga program. Medical Science Monitor: International Medical Journal of Experimental And Clinical Research. 2005;11:555–561. [PubMed] [Google Scholar]
- Newman E, O’Connor DB, Conner M. Daily hassles and eating behaviour: The role of cortisol reactivity status. Psychoneuroendocrinology. 2007;32:125–132. doi: 10.1016/j.psyneuen.2006.11.006. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman C, Howard K. The Restraint Scale: Assessment of dieting. In: Hersen M, Bellack AS, editors. Dictionary of behavioral assessment techniques. 1988. pp. 337–380. [Google Scholar]
- Roberts CJ, Campbell IC, Troop N. Increases in weight during chronic stress are partially associated with a switch in food choice towards increased carbohydrate and saturated fat intake. European Eating Disorders Review. 2014;22:77–82. doi: 10.1002/erv.2264. [DOI] [PubMed] [Google Scholar]
- Ross A, Thomas S. The health benefits of yoga and exercise: A review of comparison studies. Journal of Alternative and Complementary Medicine. 2010;16:3–12. doi: 10.1089/acm.2009.0044. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: Getting started and moving on from stage I. Clinical Psychology: Science and Practice. 2001;8:133–142. [Google Scholar]
- Sarang P, Telles S. Effects of two yoga based relaxation techniques on heart rate variability (HRV) International Journal of Stress Management. 2006;13:460–475. [Google Scholar]
- Seeman TE, Singer B, Wilkinson CW, McEwen B. Gender differences in age-related changes in HPA axis reactivity. Psychoneuroendocrinology. 2001;26:225–240. doi: 10.1016/s0306-4530(00)00043-3. [DOI] [PubMed] [Google Scholar]
- Stice E, Fisher M, Martinez E. Eating Disorder Diagnostic Scale: Additional Evidence of Reliability and Validity. Psychological Assessment. 2004;16:60–71. doi: 10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- Telles S, Raghavendra BR, Naveen KV, Manjunath NK, Kumar S, Subramanya P. Changes in autonomic variables following two meditative states described in yoga texts. The Journal of Complementary and Alternative Medicine. 2013;19:35–42. doi: 10.1089/acm.2011.0282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Telles S, Singh N, Balkrishna A. Heart rate variability changes during high frequency yoga breathing and breath awareness. Biopsychosocial Medicine. 2011;5(4):1–6. doi: 10.1186/1751-0759-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomiyama AJ, Dallman MF, Epel ES. Comfort food is comforting to those most stressed: Evidence of the chronic stress response network in high stress women. Psychoneuroendocrinology. 2011;36:1513–1519. doi: 10.1016/j.psyneuen.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Strien T, Frijters JER, Bergers GPA, Defares PB. The Dutch Eating Behavior Questionnaire (DEBQ) for assessment of restrained, emotional, and external eating behavior. International Journal of Eating Disorders. 1986;5:295–315. [Google Scholar]
- van Strien T, Roelofs K, de Weerth C. Cortisol reactivity and distress-induced emotional eating. Psychoneuroendocrinology. 2013;38:677–684. doi: 10.1016/j.psyneuen.2012.08.008. [DOI] [PubMed] [Google Scholar]
- Wardle J, Steptoe A, Oliver G, Lipsey Z. Stress, dietary restraint and food intake. Journal of Psychosomatic Research. 2000;48:195–202. doi: 10.1016/s0022-3999(00)00076-3. [DOI] [PubMed] [Google Scholar]
- West J, Otte C, Geher K, Johnson J, Mohr DC. Effects of hatha yoga and African dance on perceived stress, affect, and salivary cortisol. Annals of Behavioral Medicine. 2004;28:114–118. doi: 10.1207/s15324796abm2802_6. [DOI] [PubMed] [Google Scholar]