Abstract
Objective
Our objective was to examine the likelihood of vaginal birth after cesarean (VBAC) for women in Massachusetts.
Methods
We used birth certificate data among term, singleton, vertex presentation births by repeat cesarean or VBAC to conduct logistic regression models to examine the likelihood of VBAC for women categorized into standard classifications of race and ethnicity and into 31 detailed ethnicities. Data were analyzed for the entire study period (1996–2010, N = 119,752) and for the last 5 years (2006–2010, N = 46,081).
Results
The adjusted odds of VBAC were lowest for non-Hispanic Black mothers (0.91, CI [0.85, 0.98]) and highest for Asian/Pacific Islander mothers (1.41, CI [1.31, 1.53]) relative to non-Hispanic White women. VBAC rates ranged from 5.8 % among Brazilians to 29.3 % among Cambodians. The adjusted odds of VBAC were lower for 7 of the 30 ethnic groups (range of AORs 0.40–0.89) and higher for 8 of the 30 ethnic groups (range of AORs 1.18–2.11) relative to self-identified American mothers. For the last 5 years, Asian/Pacific Islander mothers had a higher adjusted VBAC rate (1.39, CI [1.21, 1.60]), as did 9 of the 30 ethnic groups (range of 1.25–1.84). Only Brazilian mothers had lower rates (0.37, CI [0.27, 0.50]), relative to self-identified American mothers.
Conclusions
Detailed maternal ethnicity explains the variation in VBAC rates more precisely than broad race/ethnicity categories. Improvements in our public health data infrastructure to capture detailed ethnicity are recommended to identify and address disparities and improve the quality of maternity care.
Keywords: Vaginal birth after cesarean, VBAC, Race/ethnicity, Disparity, Variation
Introduction
The current cesarean delivery rate is a result of both the rise in primary cesarean delivery and the decrease in vaginal birth after cesarean (VBAC) [1]. The overall VBAC rate in the United States (US) declined sharply from 24 % in 1996 to 8 % in 2010 [2], contrary to the Healthy People 2010 national target of 37 % (objective no. 16-9b) [3]. The probability of successful VBAC in population-based studies is estimated to be 60–80 % [4–7], yet success rates are reported to vary among different population groups based on maternal characteristics including race/ethnicity [8]. For example, a recent systematic review on factors influencing VBAC rates concluded that Black women and Hispanic women were less likely than their White counterparts to have a VBAC [9].
While maternal race/ethnicity is generally not considered a strong predictor of VBAC in individual women, it is a stable trait characteristic that is known at a women’s first prenatal visit. Grobman’s validated clinical prediction tool to determine a patient specific chance of successful VBAC after a trial of labor uses Black race and Hispanic ethnicity in its calculus of risk and weights these characteristics greater than maternal age [10]. At a population level, the variation in VBAC by race/ethnicity can be interpreted as a sign of poor quality healthcare and indicates either overuse or underuse of the procedure [11].
Minority women now account for 50 % of the over 4 million births in the US annually and persistent racial/ethnic disparities in perinatal outcomes are known to exist [12]. In order to track and monitor perinatal outcomes for all women and relevant groups, more detailed data reflective of our diverse composition are needed. However, existing studies use broad categories of race and a binary form of ethnicity that oversimplifies cultural diversity in the US [13]. Aggregating data, while analytically necessary at times, prevents examination of health outcomes for distinct racial and ethnic groups. Data pertaining to perinatal outcomes across heterogeneous ethnic groups in the US are limited despite the importance of better understanding healthcare disparities.
Therefore, we conducted this study using a large population-based data set that allowed examination of the likelihood of VBAC among thirty-one major ethnic groups. We compared our results to the standard Office of Management and Budget (OMB) classifications of race/ethnicity more commonly employed in epidemiological studies [14]. Massachusetts was an ideal setting because it is one of only a few US states to have collected detailed ethnicity data on the birth certificate for over 15 years.
Previously we found that detailed maternal ethnicity describes the variation in nulliparous, term, singleton, vertex presentation (NTSV) cesarean delivery rates more precisely than standard race/ethnicity categories that employ only one binary ethnic category (Hispanic/non-Hispanic). Use of standard categories can misclassify and therefore inaccurately make conclusions about disparities among minorities [15]. We therefore hypothesized that significant variation would exist in VBAC rates among ethnic groups not evident when examined by standard racial/ethnic classifications; furthermore, this variability would persist after adjustment for independent variables known to be associated with VBAC rates (maternal age, parity, maternal education, marital status, place of birth, prenatal care adequacy, infant birth weight, delivery source of payment, and hospital of birth).
Methods
Study Population
Data from the Massachusetts Registry of Vital Records and Statistics on all women who delivered a live birth over a fifteen-year period between January 1, 1996 and December 31, 2010were considered for inclusion. Among the 1,162,099 live births, there were 120,223 term (≥37 or<42 weeks of gestational age), singleton (one offspring), and vertex presentation (head down) deliveries by repeat cesarean or VBAC to women with a history of at least one cesarean delivery. We excluded 471 records with missing information on delivery mode and/or ethnicity as well as births that occurred out of the hospital, in unknown locations, at birth centers, or in hospitals with <15 births over the study period. The result was a final analytic sample of 119,752 births.
While limitations in birth certificate data exist, a population based validation study concluded that race and ethnicity by mode of delivery are reliable [16]. Birth certificate data were also found to be reliable for maternal race and mode of delivery when compared to the data available in a patient’s record [17]. The Standard Certificate of Live Birth (1989 Revision) is populated by data collected from both a Parent and Hospital Worksheet for Birth Certificates. Parent(s) are required to complete the legal portion of the Parent Worksheet, which contains both legal and socio-demographic information on the child’s mother and father. The Hospital Worksheet is completed by a designated hospital representative (e.g., nurse, midwife, or hospital birth registrar) and contains data on prenatal care, labor and delivery, neonatal, and discharge conditions and procedures.
Outcome Measure
Mode of delivery was the primary outcome for the analysis. Each birth was indicated on the birth certificate as being delivered by one of two modes: VBAC or repeat cesarean, which was defined as a binary outcome. Repeat cesarean deliveries were those preceded by at least one cesarean delivery including those that were scheduled or occurred after a trial of labor.
Race/Ethnicity Measures
The primary independent variable was maternal ancestry or ethnic heritage (henceforth referred to as ethnicity). Ethnicity was derived from the following open-ended question on the Parent Worksheet for the birth certificate, “Please mark one category that best describes the mother’s ancestry or ethnic heritage”, of which 39 mutually exclusive options were self-reported. Single reporting of ethnicity occurred during the entire study period. Participants from 8 categories of 1800 mothers or less were included in the relevant “Other” categories (e.g., Other African, Other Central American). When visually displaying the data, this was the logical cut-off for groups due to small sample sizes across the study period. According to the Massachusetts Department of Public Health, mothers who reported their race as Black and ethnicity as American were recoded as African American ethnicity, which is consistent with the African American ethnicity option on the Parent Worksheet [18]. American mothers were defined as non-Black and non-Hispanic who considered their ethnicity to be American. As a result, 31 unique ethnicity categories were included in the analysis. American, the majority and historically advantaged ethnic group, was the category with which all other ethnic groups were compared.
The parent worksheet also asks “Please mark one category that best describes the mother’s race” and options include White, Black, Asian/Pacific Islander, American Indian, and Other. The maternal race and ethnicity questions were combined to construct the standard OMB categories. The five broad racial/ethnic categories used were: non-Hispanic White, non-Hispanic Black, Hispanic, Asian/Pacific Islander, and Other, which approximate standard OMB classifications for federal data collection in the US. Non-Hispanic White, the majority group, was the racial/ethnic category with which the other categories were compared.
Independent Variables
The following independent variables were included: maternal age (≤24, 25–29, 30–34, ≥35 years), parity (2 or ≥3), maternal education (less than high school, high school graduate, some college, college graduate and higher), marital status (married or not married), maternal place of birth (US or foreign born), prenatal care adequacy (adequate or inadequate), infant birth weight (low birth weight <2500 g, normal birth weight 2500–4000 g, and high birth weight >4000 g), delivery source of payment (private, public, other), and hospital of birth.
Women were considered to be foreign born if they listed their country of birth anywhere other than the 50 states that comprise the US and DC; thus, women from Puerto Rico were considered foreign born. The Adequacy of Prenatal Care Utilization (APNCU) Index was used to classify the level of prenatal care into adequate and inadequate [19]. Adequate prenatal care was defined as 80 % or greater on the APNCU Index (sum of the adequate and adequate plus categories) and the rest were considered inadequate. Missing values for maternal education were coded as missing to be included in the analysis. This research study was conducted in accord with prevailing ethical principles and reviewed by Boston College Institutional Review Board that considered it exempt.
Statistical Analyses
In descriptive analyses, the frequencies of VBAC by all study variables were examined. The odds of VBAC were examined by standard OMB race/ethnicity categories and then by detailed ethnicity categories. The first logistic regression model examined differences in VBAC between the five standard OMB racial/ethnicity categories relative to non-Hispanic White mothers. We adjusted for maternal age, to account for the higher rates of pregnancy risks with advancing age [20], and year of birth, to account for the nationwide decline in VBACs [2]. Maternal socio-demographic characteristics (parity, education, marital status, place of birth, delivery source of payment), birth characteristics (prenatal care adequacy, infant birth weight), and a hospital fixed effect, to control for the known hospital differences in cesarean delivery [21], were also included in the model. The regression model was then repeated for each of the 30 ethnic groups relative to self-identified American mothers. Data were analyzed for the entire study period (1996–2010) and, separately, for the last 5 years (2006–2010) to examine more recent patterns. All analyses were conducted using SPSS, V20.
Results
Across the entire study period there were 119,752 VBAC deliveries of which 46,081 occurred in the last 5 years between 2006 and 2010. The proportion of VBACs decreased from 36.1 % in 1996 to 4.3 % in 2010. The average VBAC rate for the entire study period was 17.6 %, and it was 9 % for last 5-year period.
A description of the study population and percent of VBAC deliveries by maternal and birth characteristics are shown in Table 1. Over the entire study period, the proportion of VBACs decreased with maternal age (p < 0.01) and increased with parity (p < 0.01). A higher proportion of VBACs occurred among US born than foreign-born women (p < 0.01) and among women who received less than adequate prenatal care (p < 0.01). Deliveries of high birth weight babies were less likely to occur as a VBAC than deliveries of normal or lower birth weight babies (p < 0.01). There were no differences by marital status. There were similar patterns in the last 5 years except no differences by age were observed and a higher proportion of VBACs occurred among foreign born than US born women (p < 0.01).
Table 1.
Description of study population and percent VBAC deliveries, Massachusetts
| 1996–2010 (N = 119, 752)a
|
2006–2010 (N = 46, 081)b
|
|||
|---|---|---|---|---|
| n (%) | % VBAC | n (%) | % VBAC | |
| Maternal age (years) | ||||
| <24 | 11,580 (9.7) | 20.9 | 4581 (9.9) | 8.8 |
| 25–29 | 23,493 (19.6) | 19.0 | 9219 (20.0) | 9.1 |
| 30–34 | 44,239 (36.9) | 17.9 | 16,048 (34.8) | 9.3 |
| 35+ | 40,440 (33.8) | 15.4 | 16,233 (35.2) | 8.7 |
| Parity | ||||
| 2 | 76,871 (64.2) | 15.3 | 30,594 (66.4) | 7.5 |
| 3+ | 42,881 (35.8) | 21.7 | 15,487 (33.6) | 12.0 |
| Maternal education | ||||
| Less than high school | 10,096 (8.4) | 19.1 | 4008 (8.7) | 9.6 |
| High school graduate | 30,990 (25.9) | 17.3 | 11,258 (24.4) | 8.1 |
| Some college | 29,245 (24.4) | 17.1 | 10,005 (21.7) | 7.6 |
| College graduate and higher | 49,209 (41.1) | 17.7 | 20,735 (45.0) | 10.0 |
| Missing | 212 (0.2) | 24.1 | 75 (0.2) | 17.3 |
| Marital status | ||||
| Married | 94,480 (78.9) | 17.6 | 34,846 (75.6) | 9.0 |
| Not married | 25,272 (21.1) | 17.5 | 11,235 (24.4) | 9.0 |
| Maternal place of birth | ||||
| US born | 87,673 (73.3) | 18.0 | 31,723 (68.9) | 8.6 |
| Foreign born | 32,014 (26.7) | 16.5 | 14,350 (31.1) | 9.9 |
| Delivery payment | ||||
| Private | 84,788 (70.8) | 17.8 | 30,708 (66.7) | 9.1 |
| Public | 33,779 (28.2) | 16.7 | 15,094 (32.8) | 8.7 |
| Other | 1162 (1) | 29.9 | 271 (0.6) | 14.4 |
| Prenatal care | ||||
| Adequate | 101,450 (84.7) | 17.2 | 38,769 (84.1) | 8.8 |
| Less than adequate | 18,302 (15.3) | 19.5 | 7312 (15.9) | 9.9 |
| Birth weight | ||||
| Low birth weight | 2013 (1.7) | 16.3 | 797 (1.7) | 9.2 |
| Normal birth weight | 100,841 (84.3) | 18.1 | 39,585 (86.0) | 9.3 |
| High birth weight | 16,822 (14.1) | 14.5 | 5665 (12.3) | 6.8 |
Missing values: maternal place of birth (65), delivery payment (23), birth weight (76)
Missing values: maternal place of birth (8), delivery payment (8), birth weight (34)
Standard OMB Race/Ethnic Categories
Over the entire study period, the mean VBAC rate was 17.5 % for non-Hispanic White women, 17.1 % for non-Hispanic Black women, 18.1 % for Hispanic women, 19.6 % for Asian/Pacific Islander and 17.4 % for “Other” category women. Temporal trends in the mean VBAC rate for standard racial and ethnic categories are depicted in Fig. 1. The Healthy People 2010 VBAC target was never achieved between 2000 and 2010 by any racial/ethnic group.
Fig. 1.
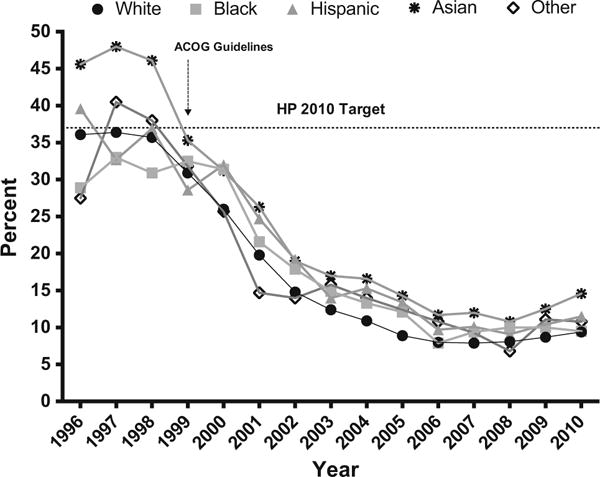
Percent (unadjusted) VBAC deliveries by standard race/ethnic categories, Massachusetts Births 1996–2010 (N = 119,752)
In the regression model using standard OMB racial and ethnic categories (Table 2), adjusting for year of birth, maternal socio-demographic and birth characteristics, and a hospital fixed effect, the odds of VBAC relative to non-Hispanic White mothers was lower for non-Hispanic Black mothers (adjusted odds ratio (AOR) 0.91, 95 % CI [0.85, 0.98]) and higher for Asian/Pacific Islander mothers (AOR 1.41, 95 % CI [1.31, 1.53]). No other racial/ethnic group was significantly different from non-Hispanic White women. Employing data from the last 5 years, the odds of VBAC remained higher for Asian/Pacific Islander women (AOR 1.39, 95 % CI [1.21, 1.60]) and were higher for Hispanic women (AOR 1.11, 95 % CI [1.00, 1.27]) relative to non-Hispanic White women. There were no other significant differences.
Table 2.
Adjusted model of VBAC deliveries by broad racial/ethnic categories
| 1996–2010 (N = 119, 593)a
|
2006–2010 (N = 46, 034)b
|
|||||
|---|---|---|---|---|---|---|
| n | % VBAC | AOR 95 % CIc | n | % VBAC | AOR 95 % CIc | |
| Non-Hispanic White | 88,780 | 17.4 | 1.00 [Reference] | 32,489 | 8.4 | 1.00 [Reference] |
| Non-Hispanic Black | 9649 | 17.0 | 0.91 [0.85, 0.98] | 4115 | 9.4 | 0.94 [0.83, 1.07] |
| Hispanic | 12,748 | 18.1 | 1.04 [0.98, 1.11] | 5504 | 10.1 | 1.11 [1.00, 1.27] |
| Asian/Pacific Islander | 6295 | 19.6 | 1.41 [1.31, 1.53] | 3046 | 12.3 | 1.39 [1.21, 1.60] |
| Other | 2262 | 17.6 | 1.01 [0.90, 1.14] | 922 | 9.7 | 1.02 [0.80, 1.29] |
Missing values: race/ethnicity (18)
Missing values: race/ethnicity (5)
Model adjusted for maternal age, year of birth, parity, maternal education, marital status, maternal place of birth, delivery source of payment, prenatal care, birth weight, and hospital of birth
Detailed Ethnic Categories
Average VBAC rates by detailed ethnicity varied more than the standard OMB categories (Table 3). Over the entire study period, the average VBAC rate ranged from 5.8 % among Brazilians to 29.3 % among Cambodians, 12.4 percentage points lower and 11.1 percentage points higher, respectively, than the average rate for self-identified American women (18.2 %) (Fig. 2). In the last 5-year period, the mean VBAC rate ranged from 3.0 % among Brazilians to 16.9 % among Japanese, 5.3 percentage points lower and 8.6 percentage points higher, respectively, than the average rate for self-identified Americans (8.3 %).
Table 3.
Percent VBAC delivery by maternal ethnicity, Massachusetts 1996–2010 and 2006–2010
| Ethnicity | 1996–2010 (N = 119, 752)
|
2006–2010 (N = 46, 081)
|
||
|---|---|---|---|---|
| n (%) | % VBAC | n (%) | % VBAC | |
| American | 55,432 (46.3) | 18.2 | 18,875 (41.0) | 8.3 |
| African-American | 3796 (3.2) | 19.8 | 1553 (3.4) | 10.8 |
| Native American | 380 (0.3) | 16.3 | 141 (0.3) | 5.7 |
| Puerto Rican | 6581 (5.5) | 19.0 | 2665 (5.8) | 9.3 |
| Dominican | 3478 (2.9) | 13.8 | 1531 (3.3) | 7.6 |
| Mexican | 719 (0.6) | 18.1 | 346 (0.8) | 12.7 |
| Columbian | 528 (0.4) | 17.4 | 193 (0.4) | 7.8 |
| Salvadoran | 1036 (0.9) | 16.7 | 553 (1.2) | 11.6 |
| Other Central American | 1271 (1.1) | 21.2 | 611 (1.3) | 16.0 |
| Other Hispanic | 273 (0.2) | 23.1 | 91 (0.2) | 9.9 |
| Haitian | 2032 (1.7) | 13.6 | 861 (1.9) | 6.6 |
| Jamaican | 382 (0.3) | 18.6 | 147 (0.3) | 10.9 |
| Other West Indian/Caribbean | 563 (0.5) | 19.5 | 192 (0.4) | 7.8 |
| Cape Verdean | 1151 (1.0) | 17.9 | 524 (1.1) | 9.4 |
| Brazilian | 3568 (3.0) | 5.8 | 1959 (4.3) | 3.0 |
| Other Portuguese | 2003 (1.7) | 12.3 | 694 (1.5) | 3.6 |
| European | 23,324 (19.5) | 17.3 | 9311 (20.2) | 9.8 |
| Lebanese | 447 (0.4) | 16.8 | 172 (0.4) | 6.4 |
| Other Middle Eastern | 833 (0.7) | 18.5 | 383 (0.8) | 13.6 |
| Nigerian | 437 (0.4) | 18.3 | 162 (0.4) | 7.4 |
| Other African | 1670 (1.4) | 14.6 | 974 (2.1) | 11.1 |
| Asian Indian | 1726 (1.4) | 13.8 | 964 (2.1) | 8.6 |
| Chinese | 1681 (1.4) | 21.3 | 736 (1.6) | 14.5 |
| Vietnamese | 856 (0.7) | 22.2 | 380 (0.8) | 13.7 |
| Cambodian | 443 (0.4) | 29.3 | 204 (0.4) | 14.2 |
| Korean | 443 (0.4) | 19.0 | 219 (0.5) | 12.8 |
| Filipino | 382 (0.3) | 18.1 | 177 (0.4) | 11.9 |
| Japanese | 169 (0.1) | 24.9 | 71 (0.2) | 16.9 |
| Other Asian/Pacific Islander | 726 (0.6) | 21.1 | 350 (0.8) | 14.3 |
| Other | 2578 (2.2) | 22.8 | 697 (1.5) | 11.0 |
| Total | 119,752 (100) | 17.6 | 46,081 (100) | 9.0 |
Fig. 2.
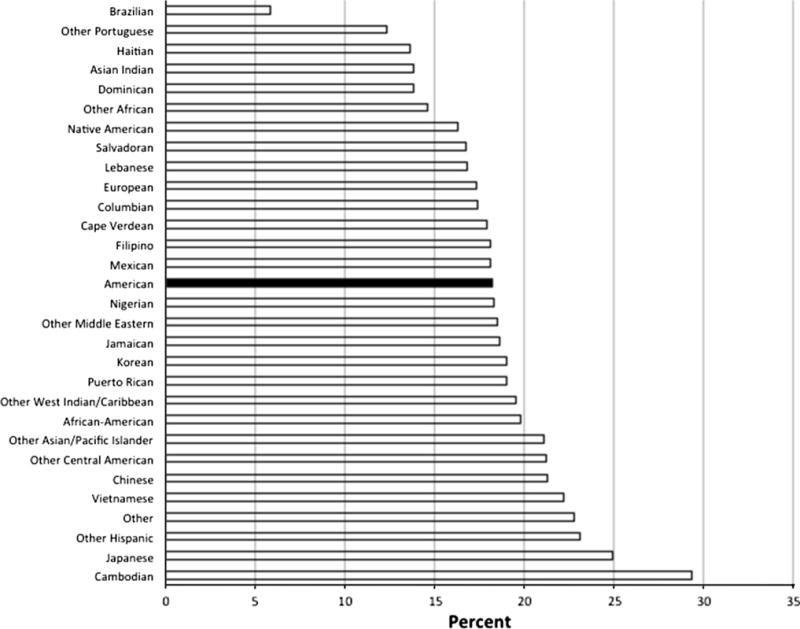
Percent VBAC deliveries by ethnicity, Massachusetts births 1996–2010 (N = 119,752)
The odds of VBAC relative to self-identified American mothers were lower for 7 of the 30 ethnic groups (range of AORs 0.40–0.89) and higher for 8 of the 30 ethnic groups (range of AORs 1.18–2.11) in the adjusted model using detailed ethnicity (Table 4). The odds of a VBAC were lowest for Brazilian women (AOR 0.40, 95 % CI [0.34–0.47] and highest among Cambodian women (AOR 2.11, 95 % CI [1.67–2.68]. There were no significant differences in VBACs for the remaining 15 groups. Employing data from the last 5 years, the odds of VBAC was lower for only Brazilian mothers (AOR 0.37, 95 % CI [0.27, 0.50]) and higher for 9 of the 30 ethnic groups (range of AORs 1.25–1.84), six of which were consistently higher across the entire study period and in the last 5 years. Other Central American (AOR 1.84, 95 % CI [1.40, 2.41]) and Cambodian women (AOR 1.83, 95 % CI [1.18, 2.85]) had the highest odds of VBAC in the last 5-year period, relative to self-identified American mothers.
Table 4.
Adjusted model of VBAC deliveries by detailed maternal ethnicity Massachusetts births
| Ethnicity | 1996–2010 AORa [95 % CI] |
2006–2010 AORa [95 % CI] |
|---|---|---|
| American | 1.00 [Reference] | 1.00 [Reference] |
| African American | 0.89 [0.81, 0.98] | 0.95 [0.78, 1.15] |
| Native American | 0.80 [0.60, 1.07] | 0.77 [0.37, 1.61] |
| Puerto Rican | 0.87 [0.80, 0.95] | 0.85 [0.71, 1.01] |
| Dominican | 0.79 [0.70, 0.90] | 0.88 [0.70, 1.12] |
| Mexican | 1.19 [0.96, 1.47] | 1.43 [1.01, 2.02] |
| Columbian | 1.05 [0.82, 1.34] | 0.87 [0.50, 1.51] |
| Salvadoran | 1.18 [0.97, 1.43] | 1.34 [1.01, 1.91] |
| Other Central American | 1.41 [1.20, 1.66] | 1.84 [1.40, 2.41] |
| Other South American | 0.84 [0.84, 0.68] | 1.20 [0.82, 1.76] |
| Other Hispanic | 0.95 [0.70, 1.29] | 0.82 [0.40, 1.67] |
| Haitian | 0.79 [0.68, 0.92] | 0.79 [0.58, 1.08] |
| Jamaican | 0.91 [0.69, 1.20] | 0.99 [0.58, 1.72] |
| Other West Indian/Caribbean | 0.97 [0.77, 1.22] | 0.82 [0.47, 1.42] |
| Cape Verdean | 1.12 [0.95, 1.33] | 1.42 [1.02, 2.00] |
| Brazilian | 0.40 [0.34, 0.47] | 0.37 [0.27, 0.50] |
| Other Portuguese | 0.83 [0.71, 0.97] | 0.95 [0.62, 1.45] |
| European | 1.07 [1.03, 1.12] | 1.25 [1.13, 1.37] |
| Lebanese | 0.87 [0.66, 1.14] | 0.72 [0.38, 1.36] |
| Other Middle Eastern | 0.96 [0.79, 1.16] | 1.23 [0.89, 1.71] |
| Nigerian | 0.92 [0.70, 1.21] | 0.73 [0.39, 1.35] |
| Other African | 0.96 [0.82, 1.12] | 1.03 [0.81, 1.31] |
| Asian Indian | 0.94 [0.80, 1.10] | 0.98 [0.75, 1.27] |
| Chinese | 1.44 [1.25, 1.66] | 1.75 [1.38, 2.23] |
| Vietnamese | 1.65 [1.34, 1.98] | 1.72 [1.23, 2.39] |
| Cambodian | 2.11 [1.67, 2.68] | 1.83 [1.18, 2.85] |
| Korean | 1.21 [0.93, 1.56] | 1.23 [0.80, 1.88] |
| Filipino | 1.18 [0.89, 1.56] | 1.47 [0.91, 2.37] |
| Japanese | 1.60 [1.10, 2.33] | 1.77[0.93, 3.37] |
| Other Asian/Pacific Islander | 1.22 [1.00, 1.49] | 1.35 [0.97, 1.88] |
| Other | 1.18 [1.06, 1.30] | 1.40 [1.09, 1.81] |
Model adjusted for maternal age, parity, year of birth, maternal education, marital status, maternal place of birth, delivery source of payment, prenatal care, birth weight, and hospital of birth
Discussion
We found significant racial and ethnic variation in VBAC rates in Massachusetts between 1996 and 2010 and the likelihood of VBAC relative to “American” women varied depending on whether women were grouped into the standard OMB categories or by the detailed ethnicity categories. The overall decline in VBAC, after the 1996 peak, was consistent with national trends associated with practice guidelines from the American Congress of Obstetricians and Gynecologists (ACOG), issued in 1999, that stipulated that a trial of labor after previous cesarean delivery should occur only in facilities with “immediately available” surgeons and anesthesiologists [22]. As hypothesized, a more nuanced picture of VBAC variation emerges when data are analyzed by detailed ethnicity categories after adjustment for independent variables known to be associated with VBAC rates.
Categorizing women into the standard OMB Hispanic category shows that Hispanic women are no more or less likely to have a VBAC than their non-Hispanic White counterparts. However, detailed ethnic patterns reveal that groups commonly aggregated into the standard Hispanic category—Puerto Rican, Dominican, and Other South American women—were significantly less likely to have a VBAC than non-Hispanic White women, consistent with the generally accepted finding that Hispanic women have lower VBAC rates [9]. The same general observation is seen among Asian/Pacific Islander women, who were more likely to have a VBAC than any other standard racial group. However, this finding masks the heterogeneity within the broad Asian/Pacific Islander category. No differences in VBACs were observed for Asian Indian, Korean, and Filipino women compared to self-identified American women in the adjusted model.
Our data partially supports the observation that Black women have lower rates of VBAC. For the entire study period non-Hispanic Black women had lower adjusted rates of VBAC than non-Hispanic White women and the adjusted rate for African Americans compared to self-identified Americans was slightly lower. However, no significant difference was observed in the last 5 years for either non-Hispanic Black or African American women. Recent changes in the composition of women in the non-Hispanic Black category in Massachusetts [27] could account the inconsistency of our data from the last 5 years, relative to the generally accepted and historic finding that Black or African American women have lower rates of VBACs than White women [9]. For example, Massachusetts has experienced rising Black immigration, from countries like from Cape Verde and higher rates of VBAC are observed among Cape Verdean women.
Comparisons with previous studies are complicated by differences in data sources and methods including classifications of race and ethnicity with no known studies examining VBAC variation using detailed ethnicity. Consistent with findings from our previous study on primary cesarean rates [15], Brazilian and Cambodian women had the lowest and highest VBAC rates, respectively, of all detailed ethnic groups.
Several limitations need consideration. Data on clinical risks for a repeat cesarean were not available in our dataset. Yet, the indication for most repeat cesareans is a previous cesarean and VBAC rates have dropped faster than changes in clinical risks for cesarean delivery can explain [23]. We also did not have data on trial of labor attempts. However, a study based on New York birth certificate data demonstrated little change in the proportions of women achieving a VBAC once trial of labor was undertaken [24]. Further, race/ethnicity misclassification due to multiple ethnic identities, the intersection of race and ethnicity, and cultural heterogeneity can produce inaccurate results [25]. Our data are derived from self-reported race/ethnicity, which is considered the “gold standard” endorsed by the Institute of Medicine [25].
It is unclear whether higher or lower rates of VBACs during the study period represent better or worse quality of care. Practice guidelines from ACOG, issued in 1999, stipulated that a trial of labor after previous cesarean delivery should occur only in facilities with “immediately available” surgeons and anesthesiologists, and are considered an important factor in the rate of VBAC decline [22]. The guidelines were based on data that showed an increased risk of uterine rupture for VBACs [26]. Unable to comply, some hospitals and obstetricians removed VBAC as an option, thereby limiting access. Accepting these guidelines as the standard of care, the essential observation is that during the study period, lower rates of VBAC represent a higher quality of care. Yet, based on our results, which controlled for hospital of birth or differential access to VBAC, it would be difficult to argue, that ethnic groups with lower VBAC rates in Massachusetts had less access and received lower quality maternity care than ethnic groups with higher VBAC rates. Nonetheless, with the overall VBAC rate increasing in Massachusetts from 9.4 % in 2011 to 11.2 % in 2012 [27], and the ACOG 2010 guidelines that are less restrictive of VBACs [28], it will be important to continue to monitor for equitable uptake of the procedure.
The debate on the role of race and ethnicity in variation in maternity care practice centers on whether the association is the result of biological differences or whether ethnicity is acting as a proxy for underlying socio-cultural attributes that might impact counseling, labor management, and/or maternal preferences. While there is insufficient evidence to support the biological argument [29, 30], the influence of socio-cultural attitudes toward childbirth has been demonstrated [31–35] in areas such as mode of delivery preferences [36], fear of birth [37], and communication patterns with delivery care providers [38–40]. Socio-cultural factors likely play a role in the decision to have a repeat cesarean or VBAC as such decisions are subject to clinical discretion and sensitive to women’s preferences. Further investigation into the socio-cultural specificities that shape women’s preferences and interactions with health care providers about mode of delivery decisions may help target public health initiatives that prevent repeat cesareans.
Conclusions
Our data provide baseline information about racial/ethnic patterns in a large population based cohort with significant racial and ethnic diversity that can be compared to future cohorts. This study demonstrated wide variability in VBAC rates by maternal ethnicity and that detailed maternal ethnicity explains the variation in VBAC rates more precisely than broad race/ethnicity categories. Describing patterns of VBAC utilization by detailed ethnicity allows for analysis that recognizes within-group heterogeneity. From a public health standpoint we recommend improvements in the capacity of our state and national measurement infrastructure to allow for detailed ethnic identification. Given the large number of repeat cesareans performed each year and the growing number of minority births in the US, the disparity in VBACs observed could have an important impact on health care quality and equity in maternal outcomes at a population level.
Significance.
What is already known on the subject?
Vaginal birth after cesarean (VBAC) rates vary among population groups based on standard racial/ethnic classifications. However, the applicability of these findings is limited by the use of broad racial/ethnic categories, which can mask considerable within-group heterogeneity.
What this study adds?
Detailed maternal ethnicity more precisely describes the variation in VBAC rates than standard race/ethnicity categories after adjustment for independent variables known to be associated with VBAC rates. Detailed maternal ethnicity might be a proxy for socio-cultural attributes that impact VBAC decisions.
Acknowledgments
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number R00HD068506 to SSH. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funder did not have any role in the study design; in the collection analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Footnotes
Conflict of interest The authors declare that they have no conflict of interest.
References
- 1.Macdorman MF, Menacker F, Declercq E. Cesarean birth in the United States: Epidemiology, trends, and outcomes. Clinics in Perinatology. 2008;35(2):293–307. doi: 10.1016/j.clp.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 2.MacDorman M, Declercq E, Menacker F. Recent trends and patterns in cesarean and vaginal birth after cesarean (VBAC) deliveries in the United States. Delivery After Previous Cesarean. 2011;38(2):179–192. doi: 10.1016/j.clp.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 3.United States Department of Health and Human Services. Healthy People 2020. 2010 http://www.healthypeople.gov/2020/about/new2020.aspx. Accessed 21 April 2011.
- 4.Lavin JP, Stephens RJ, Miodovnik M, et al. Vaginal delivery in patients with a prior cesarean section. Obstetrics and Gynecology. 1982;59(2):135–148. [PubMed] [Google Scholar]
- 5.Flamm B, Newman LA, Thomas SJ, et al. Vaginal birth after cesaeran delivery: Results of a 5 year multicenter collaborative study. Obstetrics and Gynecology. 1990;76:750–754. doi: 10.1097/00006250-199011000-00004. [DOI] [PubMed] [Google Scholar]
- 6.Miller DA, Diaz FG, Paul RH. Vaginal birth after cesarean: A 10-year experience. Obstetrics and Gynecology. 1994;84(2):255–258. [PubMed] [Google Scholar]
- 7.Knight H, Gurol-Urganci I, van der Meulen J, et al. Vaginal birth after cesarean section: A cohort study investigating factors associated with its uptake and success. BJOG. 2014;121:183–193. doi: 10.1111/1471-0528.12508. [DOI] [PubMed] [Google Scholar]
- 8.Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Process. 1991;50:179–211. [Google Scholar]
- 9.Guise JM, Eden KB, Emeis C, et al. Vaginal birth after cesarean: New insights. Rockville, MD: Agency for Healthcare Research and Quality; 2010. (Evidence Report/Technology Assessment No. 191). [Google Scholar]
- 10.Grobman WA. Rates and prediction of successful vaginal birth after cesarean. Seminars in Perinatology. 2010;34(4):244–248. doi: 10.1053/j.semperi.2010.03.003. [DOI] [PubMed] [Google Scholar]
- 11.Agency for Healthcare Research and Quality. Vaginal birth after cesarean (VBAC) delivery rate, uncomplicated [version 4.4] Rockville, MD: 2012. Inpatient quality indicators #22: technical specifications; p. 2. [Google Scholar]
- 12.Bryant AS, Worjoloh A, Caughey AB, et al. Racial/ethnic disparities in obstetric outcomes and care: Prevalence and determinants. American Journal of Obstetrics and Gynecology. 2010;202(4):335–343. doi: 10.1016/j.ajog.2009.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hawkins SS, Torres B, May GS, et al. Setting the standards for collecting ethnicity data in the Commonwealth of Massachusetts. Journal of Public Health Management and Practice. 2011;17(6):550–553. doi: 10.1097/PHH.0b013e318215a4c7. [DOI] [PubMed] [Google Scholar]
- 14.Comstock R, Castillo E, Lidsay S. Four-year review of the use of race and ethnicity in epidemiologic and public health research. American Journal Epidemiology. 2004;159(6):611–619. doi: 10.1093/aje/kwh084. [DOI] [PubMed] [Google Scholar]
- 15.Edmonds JK, Hawkins SS, Cohen BB. The influence of detailed maternal ethnicity on cesarean delivery: Findings from the US birth certificate in the State of Massachusetts. Birth. 2014;41(3):290–298. doi: 10.1111/birt.12108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Roberts CL, Bell JS, Ford JB, et al. Monitoring the quality of maternity care: How well are labour and delivery events reported in population health data? Paediatric and Perinatal Epidemiology. 2008;23(2):144–152. doi: 10.1111/j.1365-3016.2008.00980.x. [DOI] [PubMed] [Google Scholar]
- 17.DiGiuseppe DL, Aron DC, Ranbom L, et al. Reliability of birth certificate data: A multi-hospital comparison to medical records information. Maternal and Child Health Journal. 2002;6(3):169–179. doi: 10.1023/a:1019726112597. [DOI] [PubMed] [Google Scholar]
- 18.Massachusetts Department of Public Health. Massachusetts Births 2010. Boston, MA: Division of Research and Epidemiology Bureau of Health Information, Statistics, Research, and Evaluation; 2012. [Google Scholar]
- 19.Kotelchuck M. The adequacy of prenatal care utilization index: Its US distribution and association with low birthweight. American Journal of Public Health. 1994;84(9):1486–1489. doi: 10.2105/ajph.84.9.1486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Srinivas SK, Stamilio DM, Sammel MD, et al. Vaginal birth after caesarean delivery: Does maternal age affect safety and success? Paediatric and Perinatal Epidemiology. 2007;21(2):114–120. doi: 10.1111/j.1365-3016.2007.00794.x. [DOI] [PubMed] [Google Scholar]
- 21.Caceres IA, Arcaya M, Decleraq E, et al. Hospital differences in cesarean deliveries in Massachusettes (US) 2004–2006: The case against case-mix artifact. PLoS One. 2013;8(3):e57817. doi: 10.1371/journal.pone.0057817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.American College of Obstetrics and Gynecology. ACOG practice bulletin. Vaginal birth after previous cesarean delivery. Number 5, July 1999. International Journal Gynaecology and Obstetrics. 1999;66(2):197–204. [PubMed] [Google Scholar]
- 23.Grobman WA, Lai Y, Landon MB, et al. The change in the VBAC rate: An epidemiologic analysis. Paediatric and Perinatal Epidemiology. 2011;25(1):37–43. doi: 10.1111/j.1365-3016.2010.01169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yeh J, Wactawski-Wende J, Shelton JA, et al. Temporal trends in the rates of trial of labor in low-risk pregnancies and their impact on the rates and success of vaginal birth after cesarean delivery. American Journal of Obstetrics & Gynecology. 2006;194(1):144. doi: 10.1016/j.ajog.2005.06.079. [DOI] [PubMed] [Google Scholar]
- 25.Lin SS, Kelsey JL. Use of race and ethnicity in epidemiologic research: Concepts, methodological issues, and suggestions for research. Epidemiological Review. 2000;22(2):187–202. doi: 10.1093/oxfordjournals.epirev.a018032. [DOI] [PubMed] [Google Scholar]
- 26.McMahon M, Luther E, Bowes W, et al. Comparison of a trial of labor with an elective second Cesarean section. New England Journal of Medicine. 1996;335:689–695. doi: 10.1056/NEJM199609053351001. [DOI] [PubMed] [Google Scholar]
- 27.Massachusetts Department of Public Health. Massachusetts Births 2011 and 2012. Boston, MA: Office of Data Management and Outcomes Assessment; 2014. [Google Scholar]
- 28.American College of Obstetrics and Gynecology. ACOG Practice bulletin no. 115: Vaginal birth after previous cesarean delivery. Obstetrics and Gynecology. 2010;116(2 Pt 1):450. doi: 10.1097/AOG.0b013e3181eeb251. [DOI] [PubMed] [Google Scholar]
- 29.Hunt LM, Megyesi MS. The ambiguous meanings of the racial/ethnic categories routinely used in human genetics research. Social Science and Medicine. 2008;66(2):349–361. doi: 10.1016/j.socscimed.2007.08.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Owen CM, Goldstein EH, Clayton JA, et al. Racial and ethnic health disparities in reproductive medicine: An evidence-based overview. Seminars in Reproductive Medicine. 2013;31(5):317–324. doi: 10.1055/s-0033-1348889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lewallen LP. The importance of culture in childrearing. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2011;40(1):4–8. doi: 10.1111/j.1552-6909.2010.01209.x. [DOI] [PubMed] [Google Scholar]
- 32.Helsel D, Petitti DB, Kunstadter P. Pregnancy among the Hmong: Birthweight, age, and parity. American Journal of Public Health. 1992;82:1361–1364. doi: 10.2105/ajph.82.10.1361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Leeman L, Leeman R. A Native American community with a 7 % cesarean delivery rate: Does case mix, ethnicity, or labor management explain the low rate? The Annals of Family Medicine. 2003;1(1):36–43. doi: 10.1370/afm.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Walker R, Turnbull D, Wilkinson C. Increasing cesarean section rates: Exploring the role of culture in an Australian community. Birth. 2004;31(2):117–124. doi: 10.1111/j.0730-7659.2004.00289.x. [DOI] [PubMed] [Google Scholar]
- 35.Zlot A, Jackson D, Korenbrot C. Association of acculturation with cesarean section among Latinos. Maternal and Child Health Journal. 2005;9(1):11–20. doi: 10.1007/s10995-005-2447-3. [DOI] [PubMed] [Google Scholar]
- 36.Gamble J, Creedy DK, McCourt C, et al. A critique of the literature on women’s request for cesarean section. Birth-Issues in Perinatal Care. 2007;34(4):331–340. doi: 10.1111/j.1523-536X.2007.00193.x. [DOI] [PubMed] [Google Scholar]
- 37.Callister LC, Khalaf I, Semenic S, et al. The pain of childbirth: Perceptions of culturally diverse women. Pain Management Nursing. 2003;4(4):145–154. doi: 10.1016/s1524-9042(03)00028-6. [DOI] [PubMed] [Google Scholar]
- 38.Eden KB, Hashima JN, Osterweil P, et al. Childbirth preferences after cesarean birth: A review of the evidence. Birth. 2004;31(1):49–60. doi: 10.1111/j.0730-7659.2004.0274.x. [DOI] [PubMed] [Google Scholar]
- 39.Essén B, Binder P, Johnsdotter S. An anthropological analysis of the perspectives of Somali women in the West and their obstetric care providers on caesarean birth. Journal of Psychosomatic Obstetrics & Gynecology. 2011;32(1):10–18. doi: 10.3109/0167482X.2010.547966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Guo S, Munshi D, Cockburn-Wootten C, et al. Cultural dilemmas of choice: Deconstructing consumer choice in health communication between maternity-care providers and ethnic Chinese mothers in New Zealand. Health Communication. 2014;29(10):1020–1028. doi: 10.1080/10410236.2013.831515. [DOI] [PubMed] [Google Scholar]


