Abstract
Objective
To evaluate a family- and church-based intervention for adolescents and caregivers in rural Kenya to improve family relationships, reduce HIV risk, and promote mental health.
Method
The intervention was developed using community-based participatory methods and focused on strengthening family communication. Modules addressed economic, relationship, and HIV-related topics using evidence-based behavioral strategies alongside culturally-grounded content. A stepped wedge cluster randomized trial was conducted with 124 families (237 adolescents ages 10 to 16; 203 caregivers) from four churches. Participants completed interviewer-administered surveys over 5 rounds. Primary outcomes included family communication, HIV risk knowledge, self-efficacy, and beliefs. Secondary outcomes included parenting, social support, mental health, and adolescent sexual behavior. We estimated intent-to-treat effects via ordinary least squares regression with clustered standard errors.
Results
Relative to controls, the intervention group reported better family communication across domains at 1- and 3-months post-intervention and higher self-efficacy for risk reduction skills and HIV-related knowledge at 1-month post-intervention. Sexually active youth in the intervention reported fewer high-risk behaviors at 1-month post-intervention, including unprotected sex or multiple partners. Male caregivers in the intervention reported higher parental involvement at both time points, and youth reported more social support from male caregivers at 3-months post-intervention. No effects on secondary outcomes of parenting, social support, and mental health were detected.
Conclusions
This intervention holds promise for strengthening positive family processes to protect against negative future outcomes for adolescents. Implementation with religious congregations may be a promising strategy for improving sustainability and scalability of interventions in low-resource settings.
Keywords: HIV prevention, Africa, adolescents, family intervention, mental health
Family environments and relationships can be a source of protection or risk for adolescents’ emotional and behavioral health, including engagement in high-risk sexual behavior (Dimbuene & Defo, 2011; Puffer et al., 2011; Wang, Hsu, Lin, Cheng, & Lee, 2010; Biddlecom, Awusabo-Asare, & Bankole, 2009; Pequegnat & Bell, 2012; Van Campen & Romero, 2012). Though family interactions are complex, positive caregiver-child communication, parental involvement, monitoring, and authoritative parenting—a balance of warmth and structure (Baumrind, 1966)—often emerge as protective factors. Conversely, distance and mistrust in relationships, harsh discipline, and permissiveness are often associated with risky behavior and mental health problems (Mejia, Calam, & Sanders, 2012; Kabiru, Beguy, Undie, Zulu, & Ezeh, 2010; Kincaid, Jones, Sterrett, & McKee, 2012; Boudreault-Bouchard et al., 2013). Thus, promoting protective interactions and preventing those that increase risk is an important approach for addressing both mental health and HIV risk among young people (Sandler, Schoenfelder, Wolchik, & MacKinnon, 2011; Betancourt et al., 2014; Betancourt & Khan, 2008).
Family-level interventions are particularly needed in low- and middle-income countries (LMICs) where rates of HIV and mental health problems remain high while resources for healthcare remain scarce (Kakuma et al., 2011; Kieling et al., 2011; World Health Organization, 2010). In Sub-Saharan Africa, an estimated 1 in 20 people are still living with HIV (WHO, n.d.), and mental health disorders account for the largest burden of non-fatal disease worldwide (Whiteford et al., 2013). A 2012 survey in a rural district in Kenya documented that 1 in 10 adults had a common mental disorder (Jenkins et al., 2012). In low-resource contexts, families living in poverty face multiple concurrent challenges: lack of basic needs, minimal access to healthcare and education, unemployment, effects of disease, and uncertainty about the future, all of which can lead to chronic stress and increased conflict, aggression, and disconnectedness in the family (Brook, Morojele, Zhang, & Brook, 2006; Mejia et al., 2012; Repetti, Taylor, & Seeman, 2002). Yet families can also be a source of great strength and resilience in the context of these economic and structural challenges.
Prevention interventions to promote protective factors against both mental health problems and HIV risk can be smart investments given the magnitude of both problems and the negative cycles that link the two. HIV is both a cause and consequence of mental health disorders; emotional and behavioral disorders are associated with increased risk behavior (Brown et al., 2010), and an HIV diagnosis is associated with the onset of mental health problems, including depression, anxiety, and traumatic stress (Collins et al., 2011). Thus prevention interventions can be a cost-effective means of reducing the incidence of mental health disorders and HIV by decreasing the need for treatment and promoting positive development outcomes (Catalano et al., 2012; Collins et al., 2011; Kieling et al., 2011; Engle et al., 2007; Betancourt & Khan, 2008).
Prevention interventions that focus on families and communities are particularly promising because they go beyond individual-level risk factors to target changes in the systems surrounding a child that influence development (Bronfenbrenner, 1979). Promoting change beyond the individual allows interventions to target social and cultural factors, which has emerged as a predictor of the efficacy of sexual risk reduction efforts (Barrera, Castro, Strycker, & Toobert, 2013; Scott-Sheldon, Huedo-Medina, Warren, Johnson, & Carey, 2011). Further, family and community environments can continue to affect a child or adolescent’s behavior and emotional wellbeing into early adulthood, increasing the chances of long-term benefits.
In the United States and other high-income countries, studies have documented positive effects of family-based and parenting interventions, including improved communication and parent-child relationships, decreased family conflict, and reductions of internalizing and externalizing symptoms, including risk behaviors (Sandler et al., 2011; Kumpfer & Alvarado, 2003). Most evidence-based programs for families focus on treating clinical populations and use behavioral approaches to build skills in domains such as parenting and communication. Prevention for non-clinical populations and community-based interventions are less common but often take these same behavioral approaches with a focus on building protective factors (Sandler et al., 2011; Weisz, Sandler, Durlak, & Anton, 2005; Cavaleri, Olin, Kim, Hoagwood, & Burns, 2011).
Family-based interventions specifically for HIV prevention have documented effects on reduced sexual risk behavior, improved parental decision-making, and increased family communication (Guilamo-Ramos et al., 2011; McKay et al., 2014; Miller et al., 2011). Progress has been made in expanding these programs to LMICs. Three examples are interventions developed in the United States and adapted for low-income countries. “Families Matter,” adapted from “Parents Matter!”, has been shown to increase caregiver-child communication about sex, sexual health knowledge, and positive parenting skills (Poulsen et al., 2010; Vandenhoudt et al., 2010). Research on the “Collaborative HIV Prevention and Adolescent Mental Health Program [CHAMP]” (Bell et al., 2008; McKay et al., 2014) has documented effects of increased parental comfort discussing sex and HIV, increased caregiver supervision, and improved social support (Bell et al., 2008; Bhana et al., 2004). The “Let’s Talk!” intervention, adapted for workplaces in South Africa from “Talking Parents, Healthy Teens,” improved aspects of parent-child communication specific to sex and HIV (Bogart et al., 2013).
In this study, we aim to build on this body of research by developing and evaluating a new family-based intervention to address a broader range of family-level risk factors associated with risk for future HIV infection and mental health problems. The intervention, entitled READY, targets family relationships, with emphasis on improving overall communication and communication related to economic, emotional, and HIV-related topics. Unlike many others, READY (a) is evidence-based but deeply culturally grounded and developed using a community-based participatory approach to improve relevance and targeting of context-specific needs (Puffer, Pian, Sikkema, Ogwang-Odhiambo, & Broverman; Fernando, 2012); (b) integrates direct skills training for HIV prevention, economic empowerment, and promotion of psychosocial well-being within one intervention and at the individual and family levels; (c) includes full participation of both caregivers and children to achieve outcomes through live practice; and (d) is delivered through local religious congregations, including components for leaders to improve long-term family support.
The community-based approach of delivering the intervention through churches—strong and established social structures—aims to increase the potential for feasibility and scalability, two essential characteristics of interventions developed for low-resource settings (Eaton et al., 2011). In settings where religiosity is high, as is the case in Kenya, religious congregations hold promise as a delivery setting that facilitates a wide reach (Garner, 2000; Taylor, 2006). Further, having a program that is universal and endorsed and sponsored by churches could decrease the stigma of participating in an intervention related to HIV prevention. Supporting these advantages are a few previous studies that have demonstrated progress in integrating HIV prevention activities in churches across diverse settings, including the United States and South Africa (Mash & Mash, 2012; Wingood, Simpson-Robinson, Braxton, & Raiford, 2011).
Beyond improving scalability, religiosity has been identified as a protective factor against sexual risk in some populations, including Kenyan adolescents (Haglund & Fehring, 2010; Kabiru & Orpinas, 2009), and local religious bodies are often trusted sources of social support and guidance on family relationships and sexual behavior (Smith, 2004; Agadjanian, 2005). However, although religious organizations have this influence, their involvement in HIV prevention can be complicated. In a study in South Africa documented ambivalence among church leaders about addressing HIV and inconsistent prevention messages, in part due to theology and resistance of some congregants (Eriksson, Lindmark, Axemo, Haddad, & Ahlberg, 2010). Another study conducted in three African countries suggested that churches were often silent on the issues, with some promoting traditional practices that could perpetuate the HIV epidemic (Marshall & Taylor, 2006). Thus, it is important to recognize the influence of religion and to engage by supporting faith communities to address issues of family relationships and sexual behavior in ways that reduce HIV risk and promote mental health (Marshall & Taylor, 2006).
Study Aims and Hypotheses
A stepped wedge cluster randomized trial design was used to evaluate the effects of READY in a rural community in Kenya. Our theory of change posited that the proximal impacts of the program would be improved family communication and HIV-related skills and beliefs. Improved communication would then enable better parenting and social support, all of which would improve long-term outcomes related to youths’ mental health and HIV risk behavior. Thus, primary hypotheses were that the intervention would improve family communication and reduced indicators of future HIV risk, including beliefs and self-efficacy for risk reduction behaviors. Secondary hypotheses were that we would then observe improvements in the more distal outcomes of parenting practices and social support, as well as improvement in adolescents’ current mental health and reductions in HIV risk behavior in the treatment group as compared with controls. Results have implications for intervention development and delivery in the fields of family psychology, HIV prevention, and global mental health.
Methods
Setting and Recruitment
This study was conducted in a rural division of Migori County, Kenya from September 2010 to September 2011. This division is situated on the shores of Lake Victoria and shares a border with Tanzania. At the time this study was conducted, the adult HIV prevalence rate in Nyanza province—the former name for the larger area encompassing Migori County—was estimated to be 14.9 percent (NACC, 2009). This was more than twice the rate for Kenya overall, with Kenya ranking twelfth in the world for HIV prevalence (CIA, n.d.).
All 56 churches in the division were enumerated and mapped and represented multiple types of churches, including several Protestant denominations, churches based on indigenous beliefs, and a few Catholic congregations. Due to resource constraints, four churches were randomly selected to participate through lotteries conducted by community leaders; this resulted in the inclusion of three protestant churches and one indigenous. All families from these congregations with at least one adolescent living at home between the ages of 10 and 16 were eligible to participate. Youth living away from home the majority of the time (e.g., at boarding school) were not eligible to participate. As caregiving situations varied widely, caregivers were defined as any individual 18 years of age or older who stated that they were one of the primary people responsible for the adolescent(s). A total of 237 adolescents and 203 caregivers representing 124 families were enrolled. The Institutional Review Boards at Duke University and Kenya Medical Research Institute approved all study procedures. Prior to participation, informed consent and assent procedures were completed with caregivers and children, respectively.
Intervention
Congregations took part in READY at their church in the afternoons following weekly worship services. READY was developed in collaboration with a local Community Advisory Committee (CAC) using community-based participatory methods (Isreal et al., 2008). The process began with a formative study of psychosocial factors associated with HIV risk in this setting (Puffer et al., 2011; Puffer et al., 2012; Puffer, Watt, Sikkema, Ogwang-Odhiambo, & Broverman, 2012). Together, quantitative and qualitative results identified emotional and behavioral symptoms, sex-related self-efficacy, social support, mixed messages related to HIV, religious coping, and poverty as factors associated with sexual risk.
Joint interpretation of the data was followed by intervention development workshops in which the research team provided the overall framework based on evidence-based practices and the CAC provided the contextually-grounded examples and activities (for a more complete description of this process, see Puffer, Pian, Sikkema, Ogwang-Odhiambo, & Broverman, 2013). The resulting intervention was strongly influenced by ecological transactional theory, with content emphasizing the specific cultural and social context in which family interactions and adolescent behaviors occur (Henrich, Brookmeyer, Shrier, & Shahar, 2006; Lynch & Cicchetti, 1998). In this particular setting, examples of key contextual and cultural variables integrated into the intervention included: the fishing industry, associated with transactional “fish-for-sex” practices; the practice of polygamy; and mixed messages resulting from culturally-based, but often unspoken, expectations for early sexual debut alongside an explicit emphasis on abstinence based on tenets of the Christian faith.
The central objective of the 9-session READY intervention was to improve family relationships as a protective factor against risky sexual behavior and mental health symptoms. The intervention incorporated evidence-based strategies from behavioral family communication skills training, skills-based HIV prevention interventions, behavioral parent training, and cognitive behavioral therapies. The 2-hour sessions were divided into three modules: Economic Empowerment, Emotional Support, and HIV Education and Prevention (for an outline of sessions, see Table 1). Methods of teaching and activity components were influenced strongly by social cognitive theory, emphasizing modeling of new behaviors and in-session rehearsal (Bandura, 1998). All family members were invited to attend together, and family communication practice was a central component of each session.
Table 1.
Summary of the READY curriculum
| # | Title and Topic |
|---|---|
| Module 1: Economic Empowerment | |
| 1 |
Local Resources
|
| 2 |
Family Budgeting
|
| 3 |
Planning for the Future
|
|
| |
| Module 2: Emotional Support: “Building a…” | |
| 4 |
…Loving and Supportive Family
|
| 5 |
…Family that Can Cope with Stress Together
|
|
| |
| Module 3: Learning about HIV Together: “Building a Family That…” | |
| 6 |
…Learns about HIV Together
|
| 7 |
…Talks about HIV and Sexuality
|
| 8 |
…Learns About Safe and Healthy Sexuality Together
|
|
| |
| Conclusion | |
| 9 |
Getting READY to Continue Change!
|
Condom education and demonstrations were provided at the church leaders’ discretion; all decided to include this component.
READY was delivered in churches, as they are the most organized social structures in the community, trusted institutions where people seek support, and one of few places that all family members, of both genders, go together on a regular basis. This decision was made with the CAC and supported by formative data collected by the first author showing that over 90 percent of a representative sample self-identified as Christian and reported membership in a specific church.
The intervention content, teaching strategies, and curriculum materials were designed for lay providers with no prior formal training in mental health or HIV prevention. For this study, facilitators were drawn from members of the local CAC. Each church was assigned two primary facilitators, one male and one female, and two secondary facilitators who participated in skits and role-plays. Facilitators attended an initial 5-day training and then met each week (4 to 6 hours) to prepare for the upcoming sessions and contribute to the ongoing development and revision of the curriculum. Following implementation in the first church, meetings and practice decreased for the subsequent churches.
Sessions began with a 60-minute family session, which emphasized in-session communication practice. During these activities, families practiced concurrently while facilitators circulated to provide brief feedback focused on praising positive behaviors and to respond to questions. During this family component, a member of the local research team tracked completion of each activity and took notes related to facilitation quality and participant responses. Following this, youth met for another 60-minutes in gender-segregated groups for discussion and skills practice (e.g., for condom use). Concurrently, caregivers met together for 30 minutes to discuss applications of material to marital relationships and parenting before splitting into male and female discussion groups for the final 30 minutes. In addition, weekly discussion groups were held for church leaders that focused on identifying ways for church leaders to provide teaching and support to families related to the intervention topics both during and after READY. Leaders developed action plans to discuss with their congregation during the final intervention session. Participants were offered refreshments at each session.
Study Design and Procedures
A stepped wedge cluster randomized trial was conducted to estimate the impact of the intervention on youth- and family-level outcomes. Four churches were randomly assigned to receive the intervention first, second, third, or last. Survey data were collected from participants in five rounds (steps). The first round of data collection included participants from all four churches and occurred before any churches participated in the intervention. The second round took place 1-month after the first church completed the intervention but before the second church started. Each additional round of data collection took place 1-month after a church completed the 9-session intervention. Only the first and second churches participated in two post-intervention survey rounds at 1-month and 3-months post-intervention due to time and resource constraints. Hemming, Lilford, and Girling (2015) refers to this as an “incomplete” stepped wedge design. A participant flow diagram is displayed in Figure 1.
Figure 1.
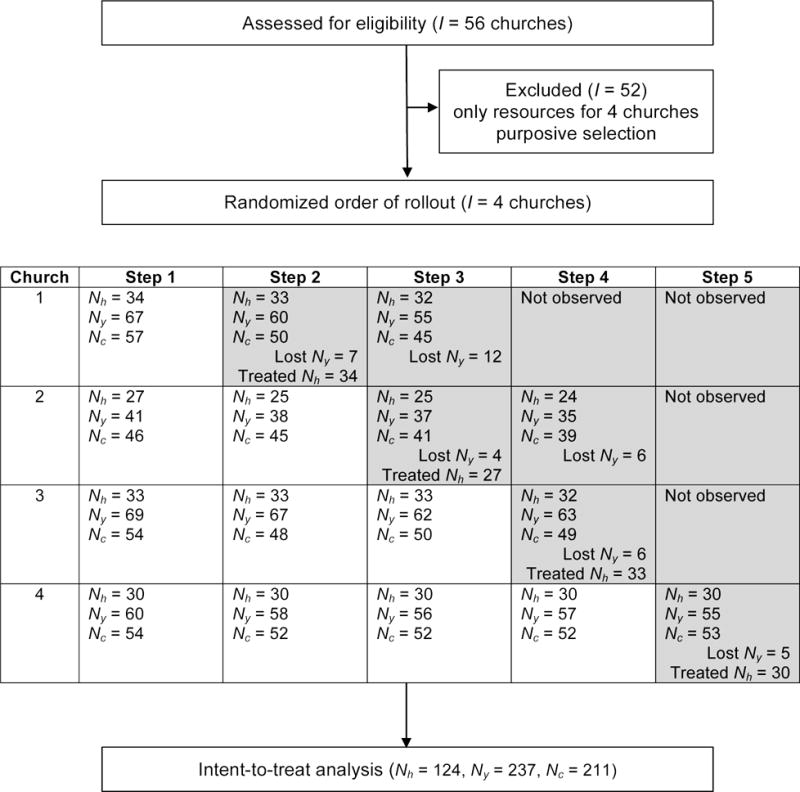
Study flow diagram. Shaded cells represent post-treatment observations. Nh=households. Ny=youth. Nc=caregivers.
A local team of Kenyan research assistants, trained by the lead researchers in data collection procedures and research ethics, administered surveys at families’ homes via handheld computers. Children and caregivers were administered the surveys separately, with some caregiver measures completed individually and others completed jointly in the two-caregiver households.
Measures
We used a combination of established measures and new assessment tools developed for this context based on formative qualitative data. Prior to conducting impact analyses, we used pre-intervention data from all participants to adapt and construct measures. This involved assessment of item-level descriptive statistics, internal consistency reliability, and results of confirmatory factor analyses. Scales with highly skewed items or evidence of a poor fit between the data and expected factor structures were revised through item screening and follow-up exploratory factor analysis (EFA). We relied on EFA results and prior theory to guide scale construction decisions; we preferred parsimonious and theoretically-meaningful factor structures containing items loading greater than 0.40 on one factor with no loadings of this magnitude or greater on other factors. Full details about each measure are presented in Appendix A. Estimates of internal consistency reliability for each scale for each round of data collection are presented in Table B1 in the Appendix. Estimates ranged from 0.49 to 0.93 across 34 scales and over 5 rounds of data collection.
Primary Outcomes
We measured multiple domains of family communication with five self-report measures. An 8-item Parent-Adolescent Communication Scale to assess overall quality of communication within adolescent and caregiver dyads (Barnes & Olson, 1985) and two 7-item scales measuring Frequency and Quality of Communication About Sex and HIV were administered. These were adapted from scales used in previous studies conducted in the United States and Kenya (Miller, Kotchick, Dorsey, Forehand, & Ham, 1998; Hutchinson, Jemmott III, Sweet Jemmott, Braverman, & Fong, 2003). From qualitative data, we developed an 8-item measure of whole family communication, as well as an 11-item measure of Economic Communication and Support related to caregiver-child communication about children’s needs and the family’s available resources; only youth reported on this, focusing on their perception of the adequacy of this support.
For proximal HIV risk indicators, we administered a 27-item HIV Knowledge Questionnaire with a focus on etiology and transmission (Carey & Schroder, 2002) including items similar to those administered in a study in South Africa (Kalichman & Simbayi, 2003); a Sex Self-Efficacy measure including three items drawn from the Self-Efficacy to Refuse Sexual Behavior Scale (Cecil & Pinkerton, 1998) and two developed for this study related to condom use; and an 8-item Sex Beliefs scale related to acceptance of risky behaviors and associated beliefs (e.g., “It is ok for men to have many sexual partners.”).
Secondary Outcomes
Secondary outcomes regarding caregiver behavior included parenting and social support. Parenting practices were assessed with a subset of items from the Alabama Parenting Questionnaire (APQ; Shelton, Frick, & Wootton, 1996). Confirmatory factor analysis revealed a poor fit of the data to the original 6-factor model. Results of an exploratory factor analysis suggested a 3-factor model reflecting parental involvement (7 items), positive parenting (6 items), and negative parenting (13 items); we report findings on these three domains. Youth also reported on each caregiver’s level of social support provided and the nature of their interactions with each caregiver using 30 items from the Network of Relationships Inventory (Furman & Buhrmester, 1985) resulting in two composite scores for Social Support and Negative Interactions.
Secondary outcomes also included youth-level outcomes, including self-esteem, symptoms of depression and anxiety, and HIV risk behaviors. Measures included the Rosenberg Self-Esteem Scale (Rosenberg, 1965) and items selected from the following measures based on confirmatory factor analyses: the Multi-Dimensional Anxiety Scale for Children 10-item short version (March, Parker, Sullivan, Stallings, & Conners, 1997); the Children’s Depression Inventory (Kovacs, 1992); and the Strengths and Difficulties Questionnaire (Goodman, 2001). Of these, the Strengths and Difficulties Questionnaire has been used most commonly across cultures, including in Kenya (Thurman, Kidman, Nice, & Ikamari, n.d.). We used two indicators of HIV risk behavior: (a) having ever had vaginal intercourse (asked to all youth), regardless of when it occurred or (b) having had high risk sex in the past three months defined by not using a condom during at least one sexual encounter and/or having more than one sexual partner in that time period (asked to sexually active youths). Brief qualitative interviews were conducted with a small subsample.
Empirical Strategy
We estimated intent-to-treat (ITT) effects via the following ordinary least squares (OLS) regression:
| (1) |
where Yijhk is an outcome of interest for person k in household h at time j (j in 1, …, T-1, where T=5) from church i (i in 1, …, C-1, where C=4); wij is an indicator of any post-intervention status for church i at time j (1=1-month and 3-months post-intervention; 0=control); θITT is the ITT treatment effect; Xij is an indicator of 3-month post-intervention status for church i at time j (1=3-months post-intervention; 0=control or 1-month post-intervention); θ3mo is the 3-month ITT treatment effect; βtime is a fixed effect of the time interval j; βchurch is a fixed effect of church i; and is a vector of household- and person-level controls measured at j=1. Thus, every church, family, and individual contributed treatment and control observations to the estimation of average treatment effects. Missing items (<5%) were mean imputed prior to scale construction.
The unit of randomization (intervention delivery order) was churches, but outcomes were measured for youth, caregivers, and families. Youth participants (siblings) were nested in households, and households were nested in churches. Across all outcomes, however, clustering at the church (cluster) level was negligible. The median intraclass correlation coefficient (ICC) for church was 0 and ranged from 0 to 0.06. Clustering at the household level was larger with a median ICC of 0.21. Therefore, standard errors were clustered at the household level. This study had 80 percent power to detect a standardized effect of 0.20 on youth-reported whole family communication (Hussey & Hughes, 2007). Analyses were conducted in R version 3.1.2 (R Core Team, 2014). This document was compiled directly from the raw data and analysis code using RStudio version 0.99.441 (RStudio, 2015) and LATEXMacTeX-2013 distribution (LaTeX3 Project, 2013).
Results
Participant Characteristics
Participant demographics are displayed in Table 2. A total of 237 youth and 203 caregivers from 124 households participated. Three out of five caregivers were female, and the mean caregiver age was 39.3 years, ranging from 18 to 91 years. As is typical in this setting, more male caregivers (62%) had completed primary school than their female counterparts (23%). The majority of caregivers reported current employment (often in the informal sector), and the average income was near USD $74 in the past 4 weeks.
Table 2.
Participant baseline (j=1) characteristics
| Participants | All | Church 1 | Church 2 | Church 3 | Church 4 |
|---|---|---|---|---|---|
| Families | |||||
| N | 124 | 34 | 27 | 33. | 30 |
| Mean income past 4 weeks (SD)† | 73.95 (72.62) | 85.99 (82.49) | 32.43 (18.79) | 93.5 (79.97) | 76.19 (70.99) |
| Mean household size (SD) | 6.6 (2.6) | 6.6 (3.0) | 5.7 (1.8) | 6.9 (2.5) | 7.1 (2.7) |
| Single parent household (%) | 8.9 | 5.7 | 6.7 | 3.8 | 5.9 |
|
| |||||
| Male Caregivers | |||||
| N | 82 | 20 | 18 | 20 | 24 |
| Mean age (SD) | 43.8 (14.1) | 40.5 (12.7) | 47.7 (17.8) | 46.6 (14.9) | 41.3 (10.9) |
| Luo tribe (%) | 20.7 | 40.0 | 27.8 | 10.0 | 8.3 |
| Completed primary (%) | 61.7 | 84.2 | 38.9 | 80.0 | 45.8 |
| Employed/Working (%) | 95.1 | 95.0 | 88.9 | 95.0 | 100.0 |
|
| |||||
| Female Caregivers | |||||
| N | 121 | 34 | 28 | 32 | 27 |
| Mean age (SD) | 36.2 (12.1) | 34.7 (12.5) | 38.4 (14.6) | 38.2 (11.9) | 33.6 (7.9) |
| Luo tribe (%) | 20.7 | 76.5 | 78.6 | 65.6 | 59.3 |
| Completed primary (%) | 61.7 | 26.5 | 14.3 | 37.5 | 11.1 |
| Employed/Working (%) | 95.1 | 76.5 | 57.1 | 84.4 | 85.2 |
|
| |||||
| Youth | |||||
| N | 237 | 67 | 41 | 69 | 60 |
| Mean age (SD) | 12.3 (2.0) | 12.2 (1.9) | 12.7 (2.3) | 12.2 (2.0) | 12.1 (2.0) |
| Female (%) | 51.9 | 59.7 | 43.9 | 49.3 | 51.7 |
| Luo tribe (%) | 60.3 | 77.6 | 73.2 | 40.6 | 55.0 |
| Single orphan (%) | 23.6 | 23.9 | 19.5 | 23.2 | 26.7 |
| Double orphan (%) | 12.7 | 17.9 | 12.2 | 15.9 | 3.3 |
| Attends school (%) | 98.7 | 100.0 | 95.1 | 98.6 | 100.0 |
Note.
An exchange rate of 80.5 Kenyan Shillings per $1 (September 1, 2010) was used to convert shillings to dollars. Self-reported income top-coded at the 99th percentile.
The average age of youth participants was 12.3 years, ranging from 10 to 16 years. More than a third of youth had lost one (23.6%) or both (12.7%) biological parents. Nearly all youth were attending school at the time of the first survey. There were 79 sets of siblings in the sample involving 81 percent of youth participants.
Treatment Attendance and Adherence
Every youth and caregiver enrolled in the study attended at least one session of the intervention, and no participants received the intervention before their church’s scheduled entry into the program. On average, female caregivers attended 61.8 percent of the 9-session intervention (see ). The average male caregiver attended 41.7 percent of sessions. Among 2-caregiver households, the average joint attendance rate was 28.7 percent. Youth participants attended most consistently (72.6%).
“Family treatment adherence” was defined as at least one caregiver and at least one youth from the household attending 5 or more sessions of the 9 session intervention. Overall, 75.2 percent of families were “adherent”, with adherence ranging from 67.6 to 83.3 percent across churches.
Survey Attrition
The youth survey attrition rate was 9.3 percent. This means that 22 youth did not participate in the survey round immediately after their church’s entry into the program. There are few statistically significant baseline differences between youth who were retained and those lost to follow up, none of which should have changed the interpretation of any findings. See Table B3 in the Appendix for the full list.
Treatment Effects
Family Communication
Program effects on family communication outcomes are reported in Table 3 and displayed graphically in Figure 2. Standardized effect sizes range from 0.21 to 0.86 1-month post-intervention and 0.36 to 0.89 3-months post-intervention. Based on caregiver report, READY produced an average increase in whole family communication of 0.53 standard deviations 1-month after the conclusion of the intervention. Results are more pronounced among youth: an increase in family communication of 0.54 standard deviations initially and an additional 0.18 standard deviations at the 3-month follow-up.
Table 3.
Average treatment effects: Communication
| Outcome | Scale (>) (1) |
Obs (2) |
Control
|
1 month ATE
|
3 month ATE
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (3) |
SD (4) |
β (5) |
SE (6) |
Δ (7) |
Δ95% (8) |
β (9) |
SE (10) |
Δ (11) |
Δ95% (12) |
|||
| Caregiver report | ||||||||||||
| Whole family communication† | z (+) | 460 | 3.32 | 0.79 | 0.53 | 0.12*** | 0.67 | (0.37 to 0.97) | 0.70 | 0.13*** | 0.89 | (0.57 to 1.21) |
| Freq of communication about sex (FCG) | 0–3 (+) | 824 | 1.05 | 0.90 | 0.77 | 0.12*** | 0.86 | (0.61 to 1.11) | 0.71 | 0.14*** | 0.79 | (0.49 to 1.08) |
| Freq of communication about sex (MCG) | 0–3 (+) | 549 | 1.01 | 0.83 | 0.44 | 0.18* | 0.52 | (0.10 to 0.95) | 0.52 | 0.20** | 0.62 | (0.15 to 1.09) |
| Qual of communication about sex (FCG) | 1–4 (+) | 821 | 2.87 | 0.58 | 0.25 | 0.08** | 0.44 | (0.16 to 0.71) | 0.28 | 0.11* | 0.48 | (0.11 to 0.84) |
| Qual of communication about sex (MCG) | 1–4 (+) | 544 | 2.83 | 0.47 | 0.24 | 0.06*** | 0.51 | (0.25 to 0.77) | 0.17 | 0.10• | 0.36 | (−0.06 to 0.78) |
| Parent-adolescent communication (FCG) | 1–4 (+) | 822 | 3.03 | 0.43 | 0.31 | 0.07*** | 0.73 | (0.42 to 1.05) | 0.20 | 0.10* | 0.47 | (0.01 to 0.93) |
| Parent-adolescent communication (MCG) | 1–4 (+) | 548 | 3.01 | 0.38 | 0.32 | 0.07*** | 0.84 | (0.51 to 1.18) | 0.14 | 0.09 | 0.38 | (−0.09 to 0.85) |
|
| ||||||||||||
| Youth Report | ||||||||||||
| Whole family communication | z (+) | 877 | 2.70 | 0.85 | 0.54 | 0.10*** | 0.63 | (0.41 to 0.86) | 0.72 | 0.13*** | 0.85 | (0.56 to 1.14) |
| Freq of communication about sex | 0–3 (+) | 877 | 0.62 | 0.67 | 0.35 | 0.08*** | 0.53 | (0.28 to 0.77) | 0.53 | 0.12*** | 0.79 | (0.43 to 1.15) |
| Qual of communication about sex (FCG) | 1–4 (+) | 869 | 2.51 | 0.64 | 0.15 | 0.07* | 0.23 | (0.02 to 0.43) | 0.24 | 0.10* | 0.37 | (0.06 to 0.68) |
| Qual of communication about sex (MCG) | 1–4 (+) | 665 | 2.39 | 0.59 | 0.22 | 0.07** | 0.38 | (0.15 to 0.60) | 0.25 | 0.10** | 0.42 | (0.10 to 0.73) |
| Parent-adolescent communication (FCG) | 1–4 (+) | 863 | 3.13 | 0.45 | 0.10 | 0.06• | 0.23 | (−0.03 to 0.49) | 0.21 | 0.08** | 0.48 | (0.14 to 0.82) |
| Parent-adolescent communication (FCG) | 1–4 (+) | 654 | 2.88 | 0.54 | 0.11 | 0.07 | 0.21 | (−0.06 to 0.47) | 0.22 | 0.11* | 0.40 | (0.02 to 0.79) |
| Economic communication | 0–3 (+) | 877 | 1.69 | 0.56 | 0.14 | 0.06* | 0.26 | (0.04 to 0.48) | 0.25 | 0.09** | 0.44 | (0.11 to 0.77) |
p<0.1,
p<0.05,
p<0.01,
p<0.001
Caregivers’ “Whole Family Communication” scores were invariant at the household level, so this outcome is reported for the subset of unique households at each step (siblings in the sample make some households appear more than once per step).
Note. This table reports average treatment effects that are based on a comparison of treatment and control periods. Column 1 lists the scale of each outcome. The character in parentheses indicates the valence of higher values: good (+) or bad (−). Column 2 reports the number of observations across churches and time periods. Columns 3 and 4 report unadjusted means and standard deviations for outcomes at j=1 when all churches were in the control period. Columns 5 to 8 report the results from an OLS regression of each outcome on a combined indicator of 1- and 3-month post-treatment observations, time fixed effects (omitted), community fixed effects (omitted), and a vector of baseline covariates (omitted). Standard errors clustered at the household-level to account for siblings being nested in households. Columns 9 to 12 report the linear combination of the 1-month and marginal 3-month treatment effects. Columns 7 and 11 report Glass’s Δ, a standardized effect size (ATE/control group SD), and columns 8 and 12 report the 95% confidence interval around these effect size estimates. MCG and FCG indicate male and female caregivers, respectively.
Figure 2.
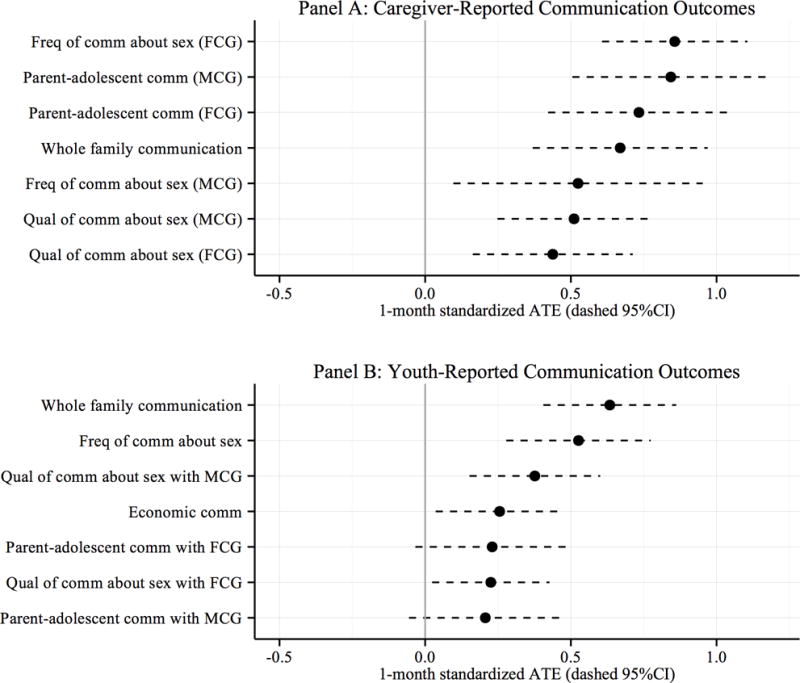
1-month average treatment effects on family communication (comm) as a percentage of control means from j=0. Black dots represent point estimates in the expected direction (grey if not in the expected direction). Dotted lines represent 95 percent confidence intervals. Abbreviations: MCG=Male caregiver; FCG=Female caregiver.
The program also had positive effects on the frequency and quality of communication about sex, communication about economic matters, and general communication patterns between caregiver and adolescent dyads. Effects on general and sex-related communication were seen across both caregiver- and youth-reported outcomes, though the magnitude of effects varied by reporter. The largest disparity was between general communication patterns between caregiver-youth dyads; the program effect on dyadic communication patterns was more than three times larger from the perspective of caregivers. This gap largely disappeared at 3 months. There was also a pattern of increasing magnitude of effect sizes over time. The only effects on communication to show a weakening at 3-months post-treatment were parent-adolescent communication as reported by caregivers and quality of communication about sex reported by male caregivers. It is particularly notable that the program got youths and caregivers talking about sex and HIV, with large effects across reporters and time.
Parenting and Social Support
Most of the observed effects on parenting behavior and social support were small and non-significant (see Table 4). However, male caregivers reported small, but non-significant, reductions in the use of negative parenting behaviors (reverse coded in Table 4) and modest, statistically significant (p<0.10) increases in parental involvement and positive parenting behaviors (standardized effect sizes of 0.33 and 0.39, respectively). The treatment effect on positive parenting was seen only at 1-month follow-up, but the effect on parental involvement remained, with the effect size doubling at the 3-month follow-up. Youth report of a significant increase in male caregiver social support at 3-months are consistent with these findings.
Table 4.
Average treatment effects: Parenting and social support
| Outcome | Scale (>) (1) |
Obs (2) |
Control
|
1 month ATE
|
3 month ATE
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (3) |
SD (4) |
β (5) |
SE (6) |
Δ (7) |
Δ95% (8) |
β (9) |
SE (10) |
Δ (11) |
Δ95% (12) |
|||
| Parenting | ||||||||||||
| Female caregiver report | ||||||||||||
| Negative parenting | 1–5 (−) | 823 | 1.48 | 0.37 | 0.07 | 0.05 | 0.20 | (−0.08 to 0.49) | −0.05 | 0.07 | 0.14 | (−0.52 to 0.25) |
| Parental involvement | 1–5 (+) | 823 | 3.34 | 0.68 | 0.04 | 0.10 | 0.06 | (−0.24 to 0.36) | 0.06 | 0.13 | 0.08 | (−0.28 to 0.45) |
| Positive parenting | 1–5 (+) | 823 | 3.66 | 0.65 | 0.10 | 0.09 | 0.16 | (−0.12 to 0.44) | 0.08 | 0.12 | 0.12 | (−0.25 to 0.50) |
| Male caregiver report | ||||||||||||
| Negative parenting | 1–5 (−) | 546 | 1.61 | 0.43 | −0.07 | 0.07 | 0.15 | (−0.46 to 0.16) | −0.04 | 0.13 | 0.10 | (−0.70 to 0.51) |
| Parental involvement | 1–5 (+) | 546 | 3.37 | 0.68 | 0.23 | 0.11* | 0.33 | (0.01 to 0.66) | 0.42 | 0.16** | 0.62 | (0.17 to 1.06) |
| Positive parenting | 1–5 (+) | 546 | 3.62 | 0.62 | 0.24 | 0.13 | 0.39 | (−0.02 to 0.81) | 0.19 | 0.16 | 0.30 | (−0.19 to 0.80) |
| Youth report | ||||||||||||
| Negative parenting | 1–5 (−) | 877 | 1.75 | 0.46 | −0.04 | 0.05 | 0.09 | (−0.30 to 0.12) | −0.05 | 0.06 | 0.10 | (−0.35 to 0.15) |
| Positive parenting | 1–5 (+) | 877 | 3.29 | 0.60 | 0.02 | 0.08 | 0.03 | (−0.22 to 0.29) | 0.19 | 0.11 | 0.31 | (−0.06 to 0.69) |
| Parental involvement, female caregiver | 1–5 (+) | 867 | 2.79 | 0.72 | −0.05 | 0.10 | 0.07 | (−0.35 to 0.22) | 0.18 | 0.14 | 0.26 | (−0.13 to 0.64) |
| Parental involvement, male caregiver | 1–5 (+) | 664 | 2.53 | 0.80 | 0.07 | 0.12 | 0.09 | (−0.22 to 0.39) | 0.14 | 0.16 | 0.18 | (−0.21 to 0.57) |
|
| ||||||||||||
| Social Support | ||||||||||||
| Youth report about female caregiver | ||||||||||||
| Social support, female caregiver | 1–5 (+) | 871 | 3.59 | 0.76 | 0.06 | 0.09 | 0.08 | (−0.15 to 0.31) | 0.16 | 0.11 | 0.22 | (−0.07 to 0.50) |
| Negative interaction, female caregiver | 1–5 (+) | 871 | 4.46 | 0.52 | 0.07 | 0.05 | 0.14 | (−0.06 to 0.34) | 0.07 | 0.07 | 0.14 | (−0.12 to 0.39) |
| Youth report about male caregiver | ||||||||||||
| Social support, male caregiver | 1–5 (+) | 673 | 2.96 | 0.92 | 0.06 | 0.13 | 0.07 | (−0.20 to 0.34) | 0.31 | 0.15* | 0.34 | (0.02 to 0.66) |
| Negative interaction, male caregiver | 1–5 (+) | 668 | 4.55 | 0.48 | −0.02 | 0.05 | 0.04 | (−0.26 to 0.18) | −0.02 | 0.08 | 0.04 | (−0.36 to 0.28) |
p<0.1,
p<0.05,
p<0.01,
p<0.001
Note. This table reports average treatment effects that are based on a comparison of treatment and control periods. Column 1 lists the scale of each outcome. The character in parentheses indicates the valence of higher values: good (+) or bad (−). Column 2 reports the number of observations across churches and time periods. Columns 3 and 4 report unadjusted means and standard deviations for outcomes at j=1 when all churches were in the control period. Columns 5 to 8 report the results from an OLS regression of each outcome on a combined indicator of 1- and 3-month post-treatment observations, time fixed effects (omitted), community fixed effects (omitted), and a vector of baseline covariates (omitted). Standard errors clustered at the household-level to account for siblings being nested in households. Columns 9 to 12 report the linear combination of the 1-month and marginal 3-month treatment effects. Columns 7 and 11 report Glass’s Δ, a standardized effect size (ATE/control group SD), and columns 8 and 12 report the 95% confidence interval around these effect size estimates. MCG and FCG indicate male and female caregivers, respectively. Youth-reported negative interactions with caregivers have been reverse coded so that higher scores represent less negative interactions.
Youth Outcomes
Youth outcomes are presented in Table 5. For youth, READY had positive effects on HIV knowledge (small) and sex self-efficacy (modest) at the 1-month endline, though at 3-months, these statistically significant effects were smaller and non-significant. There were no measurable effects of the program on youth mental health outcomes. In the baseline round when all churches were in the control period, 25% of youth (N=59) reported having had sex, with a median age of sexual debut of 12 years. Of these sexually active adolescents, 84% (N=50) reported having engaged in high risk sex behaviors. No intervention effect was found on sexual debut (i.e., ever having had vaginal sex), but there was a 24.8 percent reduction in youth-reported high-risk sex (unprotected sex or multiple partners) among sexually active youth at the 1-month follow-up only.
Table 5.
Average treatment effects: HIV and mental health outcomes
| Outcome | Scale (>) (1) |
Obs (2) |
Control | 1 month ATE | 3 month ATE | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (3) |
SD (4) |
β (5) |
SE (6) |
Δ (7) |
Δ95% (8) |
β (9) |
SE (10) |
Δ (11) |
Δ95% (12) |
|||
| HIV-related outcomes | ||||||||||||
| HIV knowledge | 0–1 (+) | 876 | 0.67 | 0.18 | 0.03 | 0.01* | 0.16 | (0.01 to 0.31) | 0.03 | 0.02 | 0.16 | (−0.06 to 0.38) |
| Sex self-efficacy | 1–5 (+) | 877 | 2.96 | 1.01 | 0.41 | 0.12*** | 0.41 | (0.18 to 0.64) | 0.18 | 0.17 | 0.18 | (−0.16 to 0.51) |
| Sex beliefs | 1–4 (−) | 877 | 1.71 | 0.44 | −0.04 | 0.06 | 0.10 | (−0.36 to 0.16) | −0.04 | 0.08 | 0.10 | (−0.44 to 0.24) |
| Ever vaginal sex | 0–1 (−) | 878 | 0.25 | 0.43 | −0.05 | 0.03 | 0.11 | (−0.25 to 0.02) | −0.01 | 0.05 | 0.03 | (−0.26 to 0.21) |
| High risk sex | 0–1 (−) | 144 | 0.84 | 0.37 | −0.25 | 0.12* | 0.67 | (−1.31 to −0.02) | −0.08 | 0.15 | 0.23 | (−1.02 to 0.56) |
|
| ||||||||||||
| Mental health outcomes | ||||||||||||
| Rosen self-esteem | 0–3 (+) | 878 | 2.15 | 0.40 | 0.02 | 0.06 | 0.06 | (−0.22 to 0.34) | 0.10 | 0.08 | 0.24 | (−0.14 to 0.63) |
| SDQ difficulties | 0–2 (−) | 878 | 0.53 | 0.32 | −0.03 | 0.03 | 0.08 | (−0.27 to 0.10) | −0.00 | 0.04 | 0.01 | (−0.28 to 0.27) |
| CDI depression | 0–2 (−) | 876 | 0.27 | 0.19 | −0.01 | 0.02 | 0.05 | (−0.23 to 0.12) | −0.01 | 0.02 | 0.05 | (−0.29 to 0.18) |
p<0.1,
p<0.05,
p<0.01,
p<0.001
Note. This table reports average treatment effects that are based on a comparison of treatment and control periods. Column 1 lists the scale of each outcome. The character in parentheses indicates the valence of higher values: good (+) or bad (−). Column 2 reports the number of observations across churches and time periods. Columns 3 and 4 report unadjusted means and standard deviations for outcomes at j=1 when all churches were in the control period. Columns 5 to 8 report the results from an OLS regression of each outcome on a combined indicator of 1- and 3-month post-treatment observations, time fixed effects (omitted), community fixed effects (omitted), and a vector of baseline covariates (omitted). Standard errors clustered at the household-level to account for siblings being nested in households. Columns 9 to 12 report the linear combination of the 1-month and marginal 3-month treatment effects. Columns 7 and 11 report Glass’s Δ, a standardized effect size (ATE/control group SD), and columns 8 and 12 report the 95% confidence interval around these effect size estimates. MCG and FCG indicate male and female caregivers, respectively.
Discussion
In this study, we evaluated the potential of a church- and family-based prevention intervention to improve family communication, HIV risk, and adolescent well-being using a stepped wedge cluster randomized design. The READY intervention was developed through community-based participatory methods, which allowed for a blending of established evidence-based practices with contextually relevant strategies and delivery methods. To our knowledge, this is the first study in a low-income country to evaluate a family strengthening program delivered through religious congregations, which are often strong social structures in impoverished communities with few resources for health and social services. READY was designed to be scalable and sustainable across diverse low-resource settings to promote positive change within individuals, families and communities.
Results indicate that READY improved multiple aspects of family communication, a well-documented protective factor against HIV risk behavior and mental health disorders (Bastien, Kajula, & Muhwezi, 2011; Biddlecom et al., 2009; Kaminski, Valle, Filene, & Boyle, 2008; Greenberg, Domitrovich, & Bumbarger, 2001). Effects were statistically significant based on both caregiver and youth reports, strengthening our confidence in these results, as effects reported by youth themselves have been less consistent than caregiver-reported effects in previous evaluations of family-based programs (Bell et al., 2008; Bogart et al., 2013).
Within the effects on communication, we find two particularly interesting. First, the impact on communication within the entire family is notable in that it suggests a change in overall family dynamics, which we expected could be more difficult to shift than dyadic relationships. This was a central goal of READY because while female caregivers often have primary parenting responsibilities, males typically have more decision-making power that could either undermine or greatly strengthen changes in the family overall. Thus changes in the overall dynamics could potentially lead to longer-term and larger changes. Seeing this effect was particularly encouraging given that it occurred despite relatively low male caregiver attendance.
A second interesting finding is the impact on economic support communication. Results suggest benefits of including “economic empowerment” as a topic, which is unique amongst HIV prevention and mental health interventions. Addressing financial difficulties within families explicitly was strongly recommended by the CAC, even without any monetary or material support provided, because financial needs are the most common and serious stressors and sources of conflict. Indeed, during the intervention, many examples of the quality of relationships related to whether or not male caregivers provided for the family and whether both caregivers provided for the children; for example, many children described feeling “loved” if parents paid their school fees. Since READY increased youths’ perceived support from their parents regardless of whether they had the means to meet needs immediately, it follows that building skills related to discussing and problem-solving around resources may be helpful in future interventions. A potential topic of future research may be how economic assistance combined with READY may affect treatment effects, if at all.
Impacts on frequency and quality of communication about sex are also important given that they are perhaps most directly associated with future HIV risk. In terms of individual-level sexual risk prevention, READY led to higher HIV knowledge and self-efficacy for safer sexual behaviors at 1-month but not 3-month follow-up. The effect on self-efficacy is encouraging, as this is associated consistently with positive changes in health behaviors in general (Bandura, 1998) and specifically with reduced risky sexual behavior (Basen-Engquist & Parcel, 1992; Sheeran, Abraham, & Orbell, 1999). However, the fact that the effect was not maintained calls into question whether the confidence in skills decreased quickly. There was no treatment effect on beliefs related to sexual risk, perhaps because endorsement of “risky” beliefs was low at baseline in both groups. For sexual risk behaviors, READY did not affect whether or not youth had had sex but had a positive effect at 1-month follow-up on risk behaviors (i.e., sex without a condom, multiple partners) among those who were already sexually active. Since this effect also was no longer significant at 3-month follow-up, and the majority of the adolescents were not yet sexually active, longer follow-up would be valuable to better understand the longer-term effects on risk behavior trajectory, assess effects of the treatment on sexual debut, and examine relationships between the changes in self-efficacy and behavior in the entire sample.
Among parenting outcomes, we observed two treatment effects, both related to male caregivers’ behaviors. Male caregivers in the treatment group reported more involvement in their child’s life at both 1- and 3-months post-intervention, and youth reported more social support from male caregivers at the 3-month follow-up. Again, this was somewhat surprising given the lower attendance of male caregivers. Possible contributors were mentioned during qualitative follow-up. Some men reportedly asked their wives and children about sessions and reviewed handouts out of curiosity or desire to monitor their family’s learning, while others were exposed to some of the material during “special talk time” (“budho makende” in Luo), an ongoing assignment for families to spend five minutes together per day. Some observational learning also was described, especially in terms of watching female caregivers discipline and talk with children more gently and openly. These findings, though tentative, are important given the dearth of research on fathering in low-resource settings. There is reason to believe that there are gender differences in caregiving that could be addressed in engagement and intervention strategies to maximize effects of family-based interventions for caregivers of both genders (Panter-Brick et al., 2014; Cowan, Cowan, Pruett, Pruett, & Wong, 2009). Further research on fathering practices can inform strategies for promoting specific father-child interactions that are protective.
The absence of other effects on parenting practices could be due to short follow-up periods coupled with less emphasis in the intervention on practicing specific behavioral parenting skills, such as discipline strategies, and more emphasis on behavioral communication skills and relationship building. This is important to consider in future delivery of the intervention for clinical populations of adolescents (e.g., those with existing behavioral symptoms) in which stronger emphasis on behavior management may be warranted (Dretzke et al., 2009). Results also showed no treatment effect on adolescent mental health in the time frame of our study. This was likely due in part to the low endorsement of symptoms at baseline, as recruitment did not specifically target adolescents with current mental health concerns. Also, for adolescents with very high levels of symptoms, it is possible that this universal prevention intervention alone would be insufficient; for these individuals, more intensive treatment approaches are likely needed. Though our follow-up period did not allow for exploration of longer term effects, a treatment effect could emerge over time as the adolescents grow older and continue to face new stressors; our hypothesis for prevention posits that improvements in the family environment could protect against future incidence of mental health problems throughout adolescence and adulthood even among adolescents not experiencing any emotional or behavioral problems at the time of the study (Repetti et al., 2002; Weisz et al., 2005).
Developing prevention and intervention approaches that are scalable and cost-effective for very low-resource settings is a priority for increasing access to care (Catalano et al., 2012; Eaton et al., 2011; Hecht et al., 2010; Jordans, Tol, Ndayisaba, & Komproe, 2013). Thus a main focus in this study was to deliver the intervention with lay facilitators and through existing and trusted social structures that have the potential to sustain the intervention with minimal external support. Churches are one natural choice as one of the very few places where families go together regularly in a rural African setting where most social gatherings are gender- or age-specific. We designed this study to test this delivery method alongside the intervention content in the same study to maximize external validity of results.
Attendance results were interesting and suggest challenges that need to be addressed, especially among male caregivers. One potential barrier to consistent attendance is that afternoon church activities tend to be less formal, are often geared towards youth, and are sometimes meetings where families typically send only one representative. Orientation to READY may not have been clear enough to differentiate it as a structured, time-limited family commitment. The focus on communication practice during sessions also could have led to some resistance, which is important to explore to determine how to best frame and begin those in-session experiences. Our methodology also sacrificed attendance for external validity in that (a) our enrollment was conducted in homes rather than at the church in order to include family members who were not regular church-goers and (b) we included all family members in the intervention and analysis rather than one target caregiver and child. As noted above, however, effects that suggested changes in all family members were observed despite inconsistent attendance, perhaps due to the ways in which the central skills are repeated and built upon throughout. In future implementation, barriers to attendance should be explored prior to and throughout intervention delivery to improve engagement and retention strategies.
Acceptability data documented interest in participation from the vast majority of churches within the study location and acceptance of condom demonstrations by leaders of all participating churches. Though this was a small number of churches, the openness to condom use education raises questions about the assumptions about religious organizations’ views on prevention methods that have deterred some in the HIV prevention community from seeking out these partnerships. Future studies are needed to evaluate this approach across a wider range of types of religious groups and to test the approach of scaling up prevention interventions through religious institutions. Results of this study suggest that this may be a promising but overlooked implementation strategy.
Limitations of this study raise several questions for future research. First, we were not able to implement the program in a large number of clusters (i.e., churches), which reduced our power to detect effects on secondary outcomes. All clusters also were relatively close geographically, potentially allowing for contamination and related attenuation of treatment effects. Further, although 1-month follow-up analyses included data from all clusters, only two were included for the 3-month analyses due to resource constraints; having all churches included would have improved precision of the 3-month estimates. The lack of longer-term follow up also precluded our ability to evaluate the future preventive effects of the program, particularly on mental health symptoms that are less likely to change immediately in a non-clinical population. Lastly, some measures showed only moderate reliability in this sample. Though psychometric analyses led to item reduction that improved performance of the measures, further work needs to be done to validate measures that show both high reliability and validity in this and other diverse populations.
Results suggest that READY holds promise as an approach to strengthen protective family processes that may prevent future negative outcomes for adolescents living in low-resource contexts. Implementation through religious congregations was feasible in this study and could be an effective and scalable delivery strategy for family-based and HIV prevention interventions. Larger studies with longitudinal designs could test preventive effects of specific outcomes, including mental health disorders and HIV infection, as well as the mechanisms of change underlying treatment impact.
Acknowledgments
Community Advisory Board, intervention facilitators, research assistants, the Women’s Institute for Secondary Education and Research, and the Africa Mental Health Foundation.
Funding: the NIH Fogerty International Center, Johnson & Johnson, the Duke Global Health Institute, and the Duke Center for AIDS Research.
Footnotes
Public Health Significance Statement. This study highlights the benefits of a culturally-grounded, behavioral family-based intervention to improve family communication in low-resource settings. Results further suggest that religious organizations hold potential as community-based settings for interventions targeting family well-being and HIV prevention.
Contributor Information
Eve S. Puffer, Department of Psychology & Neuroscience, Duke University and Duke Global Health Institute (DGHI), Duke University
Eric P. Green, DGHI, Duke University, Duke University
Kathleen J. Sikkema, Department of Psychology & Neuroscience, Duke University and DGHI, Duke University
Sherryl A. Broverman, Department of Biology, Duke University and DGHI, Duke University
Rose A. Ogwang-Odhiambo, Institute of Women, Gender & Development Studies, Egerton University, Egerton University
Jessica Pian, DGHI, Duke University, Duke University.
References
- Agadjanian V. Gender, religious involvement, and HIV/AIDS prevention in mozambique. Social Science & Medicine. 2005;61(7):1529–1539. doi: 10.1016/j.socscimed.2005.03.012. [DOI] [PubMed] [Google Scholar]
- Bandura A. Health promotion from the perspective of social cognitive theory. Psychology and Health. 1998;13(4):623–649. [Google Scholar]
- Barnes HL, Olson DH. Parent-adolescent communication and the circumplex model. Child Development. 1985:438–447. [Google Scholar]
- Barrera M, Castro FG, Strycker LA, Toobert DJ. Cultural adaptations of behavioral health interventions: A progress report. Journal of Consulting and Clinical Psychology. 2013;81(2):196. doi: 10.1037/a0027085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basen-Engquist K, Parcel GS. Attitudes, norms, and self-efficacy: A model of adolescents’ hiv-related sexual risk behavior. Health Education & Behavior. 1992;19(2):263–277. doi: 10.1177/109019819201900209. [DOI] [PubMed] [Google Scholar]
- Bastien S, Kajula LJ, Muhwezi WW. A review of studies of parent-child communication about sexuality and hiv/aids in sub-saharan africa. Reproductive Health. 2011;8(25) doi: 10.1186/1742-4755-8-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumrind D. Prototypical descriptions of 3 parenting styles. Psychology. 1966;37 [Google Scholar]
- Bell CC, Bhana A, Petersen I, McKay MM, Gibbons R, Bannon W, Amatya A. Building protective factors to offset sexually risky behaviors among black youths: a randomized control trial. Journal of the National Medical Association. 2008;100(8):936. doi: 10.1016/s0027-9684(15)31408-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Khan KT. The mental health of children affected by armed conflict: protective processes and pathways to resilience. International Review of Psychiatry. 2008;20(3):317–328. doi: 10.1080/09540260802090363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Betancourt TS, Ng LC, Kirk CM, Munyanah M, Mushashi C, Ingabire C, Sezibera V. Family-based prevention of mental health problems in children affected by hiv and aids: an open trial. AIDS. 2014 Jul;28:S359–S368. doi: 10.1097/QAD.0000000000000336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhana A, Petersen I, Mason A, Mahintsho Z, Bell C, McKay M. Children and youth at risk: adaptation and pilot study of the champ (amaqhawe) programme in south africa. African Journal of AIDS Research. 2004;3(1):33–41. doi: 10.2989/16085900409490316. [DOI] [PubMed] [Google Scholar]
- Biddlecom A, Awusabo-Asare K, Bankole A. Role of parents in adolescent sexualactivity and contraceptive use in four african countries. International Perspectives on Sexual and Reproductive Health. 2009:72–81. doi: 10.1363/ipsrh.35.072.09. [DOI] [PubMed] [Google Scholar]
- Bogart LM, Skinner D, Thurston IB, Toefy Y, Klein DJ, Hu CH, Schuster MA. Let’s talk!, a south african worksite-based hiv prevention parenting program. Journal of Adolescent Health. 2013;53(5):602–608. doi: 10.1016/j.jadohealth.2013.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boudreault-Bouchard AM, Dion J, Hains J, Vandermeerschen J, Laberge L, Perron M. Impact of parental emotional support and coercive control on adolescents’ self-esteem and psychological distress: Results of a four-year longitudinal study. Journal of Adolescence. 2013 Aug;36(4):695–704. doi: 10.1016/j.adolescence.2013.05.002. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U. The ecology of human development. Cambridge, MA: Harvard University Press; 1979. [Google Scholar]
- Brook DW, Morojele NK, Zhang CS, Brook JS. South african adolescents: pathways to risky sexual behavior. Aids Education and Prevention. 2006 Jun;18(3):259–272. doi: 10.1521/aeap.2006.18.3.259. [DOI] [PubMed] [Google Scholar]
- Brown LK, Hadley W, Stewart A, Lescano C, Whiteley L, Donenberg G, DiClemente R. Psychiatric disorders and sexual risk among adolescents in mental health treatment. Journal of Consulting and Clinical Psychology. 2010 Aug;78(4):590–597. doi: 10.1037/a0019632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey MP, Schroder KE. Development and psychometric evaluation of the brief hiv knowledge questionnaire. AIDS Education and Prevention. 2002;14(2):172. doi: 10.1521/aeap.14.2.172.23902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catalano RF, Fagan AA, Gavin LE, Greenberg MT, Irwin CE, Jr, Ross DA, Shek DT. Worldwide application of prevention science in adolescent health. The Lancet. 2012 May;379(9826):1653–1664. doi: 10.1016/S0140-6736(12)60238-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cavaleri MA, Olin SS, Kim A, Hoagwood KE, Burns BJ. Family support in prevention programs for children at risk for emotional/behavioral problems. Clinical Child and Family Psychology Review. 2011 Dec;14(4):399–412. doi: 10.1007/s10567-011-0100-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cecil H, Pinkerton SD. Reliability and validity of a self-efficacy instrument for protective sexual behaviors. Journal of American College Health. 1998;47(3):113–121. doi: 10.1080/07448489809595631. [DOI] [PubMed] [Google Scholar]
- CIA. The world factbook. n.d. Retrieved from https://www.cia.gov/library/publications/resources/the-world-factbook/
- Collins PY, Patel V, Joestl SS, March D, Insel TR, Daar AS, Fairburn C. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi: 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowan PA, Cowan C, Pruett M, Pruett K, Wong J. Promoting fathers’ engagement with children: Preventive interventions for low-income families. Journal of Marriage and Family. 2009;3(71):663–679. [Google Scholar]
- Dimbuene ZT, Defo BK. Risky sexual behaviour among unmarried young people in cameroon: another look at family environment. Journal of Biosocial Science. 2011;43(2):129–153. doi: 10.1017/S0021932010000635. [DOI] [PubMed] [Google Scholar]
- Dretzke J, Davenport C, Frew E, Barlow J, Stewart-Brown S, Bayliss S, Hyde C. The clinical effectiveness of different parenting programmes for children with conduct problems: a systematic review of randomised controlled trials. Child and Adolescent Psychiatry and Mental Health. 2009;3(1):7. doi: 10.1186/1753-2000-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton J, McCay L, Semrau M, Chatterjee S, Baingana F, Araya R, Saxena S. Scale up of services for mental health in low-income and middle-income countries. The Lancet. 2011 Oct;378(9802):1592–603. doi: 10.1016/S0140-6736(11)60891-X. [DOI] [PubMed] [Google Scholar]
- Engle PL, Black MM, Behrman JR, Cabral de Mello M, Gertler PJ, Kapiriri L, International Child Development Steering, G Strategies to avoid the loss of developmental potential in more than 200 million children in the developing world. The Lancet. 2007 Jan;369(9557):229–42. doi: 10.1016/S0140-6736(07)60112-3. [DOI] [PubMed] [Google Scholar]
- Eriksson E, Lindmark G, Axemo P, Haddad B, Ahlberg BM. Ambivalence, silence and gender differences in church leaders’ HIV-prevention messages to young people in KwaZulu-natal, south africa: SHORT REPORT. Culture, Health & Sexuality. 2010;12(1):103–114. doi: 10.1080/13691050903141192. [DOI] [PubMed] [Google Scholar]
- Fernando GA. The roads less traveled: mapping some pathways on the global mental health research roadmap. Transcultural Psychiatry. 2012 Jul;49(3–4):396–417. doi: 10.1177/1363461512447137. [DOI] [PubMed] [Google Scholar]
- Furman W, Buhrmester D. Children’s perceptions of the personal relationships in their social networks. Developmental Psychology. 1985;21(6):1016. [Google Scholar]
- Garner RC. Safe sects? dynamic religion and AIDS in south africa. The Journal of Modern African Studies. 2000;38(01):41–69. doi: 10.1017/s0022278x99003249. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Greenberg MT, Domitrovich C, Bumbarger B. The prevention of mental disorders in school-aged children: Current state of the field. Prevention & Treatment. 2001;4(1) [Google Scholar]
- Guilamo-Ramos V, Bouris A, Jaccard J, Gonzalez B, McCoy W, Aranda D. A parent-based intervention to reduce sexual risk behavior in early adolescence: building alliances between physicians, social workers, and parents. The Journal of Adolescent Health. 2011 Feb;48(2):159–163. doi: 10.1016/j.jadohealth.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haglund KA, Fehring RJ. The association of religiosity, sexual education, and parental factors with risky sexual behaviors among adolescents and young adults. Journal of Religion and Health. 2010;49(4):460–472. doi: 10.1007/s10943-009-9267-5. [DOI] [PubMed] [Google Scholar]
- Hecht R, Stover J, Bollinger L, Muhib F, Case K, de Ferranti D. Financing of hiv/aids programme scale-up in low-income and middle-income countries, 2009–31. The Lancet. 2010;376(9748):1254–1260. doi: 10.1016/S0140-6736(10)61255-X. [DOI] [PubMed] [Google Scholar]
- Hemming K, Lilford R, Girling AJ. Stepped-wedge cluster randomised controlled trials: a generic framework including parallel and multiple-level designs. Statistics in Medicine. 2015 Jan;34(2):181–196. doi: 10.1002/sim.6325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henrich CC, Brookmeyer KA, Shrier LA, Shahar G. Supportive relationships and sexual risk behavior in adolescence: An ecological–transactional approach. Journal of Pediatric Psychology. 2006;31(3):286–297. doi: 10.1093/jpepsy/jsj024. [DOI] [PubMed] [Google Scholar]
- Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemporary Clinical Trials. 2007;28(2):182–191. doi: 10.1016/j.cct.2006.05.007. [DOI] [PubMed] [Google Scholar]
- Hutchinson MK, Jemmott JB, III, Sweet Jemmott L, Braverman P, Fong GT. The role of mother–daughter sexual risk communication in reducing sexual risk behaviors among urban adolescent females: a prospective study. Journal of Adolescent Health. 2003;33(2):98–107. doi: 10.1016/s1054-139x(03)00183-6. [DOI] [PubMed] [Google Scholar]
- Isreal BA, Schulz AJ, Parker EA, Becker AB, Allen AJ, Guzman JR. Critical issues in developing and following cbpr principles Community-Based Participatory Research for Health: From Process to Outcomes. San Francisco. CA: Jossey-Bass; 2008. pp. 47–66. [Google Scholar]
- Jenkins R, Njenga F, Okonji M, Kigamwa P, Baraza M, Ayuyo J, Kiima D. Prevalence of common mental disorders in a rural district of kenya, and socio-demographic risk factors. International journal of environmental research and public health. 2012;9(5):1810–1819. doi: 10.3390/ijerph9051810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordans MJ, Tol WA, Ndayisaba A, Komproe IH. A controlled evaluation of a brief parenting psychoeducation intervention in burundi. Social Psychiatry and Psychiatric Epidemiology. 2013;48(11):1851–1859. doi: 10.1007/s00127-012-0630-6. [DOI] [PubMed] [Google Scholar]
- Kabiru CW, Beguy D, Undie C-C, Zulu EM, Ezeh AC. Transition into first sex among adolescents in slum and non-slum communities in nairobi, kenya. Journal of Youth Studies. 2010;13(4):453–471. doi: 10.1080/13676261003801754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabiru CW, Orpinas P. Factors associated with sexual activity among high-school students in nairobi, kenya. Journal of Adolescence. 2009;3.x(4):1023–1039. doi: 10.1016/j.adolescence.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Kakuma R, Minas H, van Ginneken N, Dal Poz MR, Desiraju K, Morris JE, Scheffler RM. Human resources for mental health care: current situation and strategies for action. The Lancet. 2011 Nov;378(9803):1654–63. doi: 10.1016/S0140-6736(11)61093-3. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC. Hiv testing attitudes, aids stigma, and voluntary hiv counselling and testing in a black township in cape town, south africa. Sexually Transmitted Infections. 2003;79(6):442–447. doi: 10.1136/sti.79.6.442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaminski JW, Valle LA, Filene JH, Boyle CL. A meta-analytic review of components associated with parent training program effectiveness. Journal of Abnormal Child Psychology. 2008 Jan;36(4):567–589. doi: 10.1007/s10802-007-9201-9. [DOI] [PubMed] [Google Scholar]
- Kieling C, Baker-Henningham H, Belfer M, Conti G, Ertem I, Omigbodun O, Rahman A. Child and adolescent mental health worldwide: evidence for action. Lancet. 2011 Oct;378(9801):1515–25. doi: 10.1016/S0140-6736(11)60827-1. [DOI] [PubMed] [Google Scholar]
- Kincaid C, Jones DJ, Sterrett E, McKee L. A review of parenting and adolescent sexual behavior: the moderating role of gender. Clinical Psychology Review. 2012;3.x(3):177–188. doi: 10.1016/j.cpr.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kovacs M. Children’s depression inventory: manual [Computer software manual] Multi-Health Systems 1992 [Google Scholar]
- Kumpfer KL, Alvarado R. Family-strengthening approaches for the prevention of youth problem behaviors. American Psychologist. 2003;58(6–7):457. doi: 10.1037/0003-066X.58.6-7.457. [DOI] [PubMed] [Google Scholar]
- LaTeX3 Project. Latex: A document preparation system 2013 [Google Scholar]
- Lynch M, Cicchetti D. An ecological-transactional analysis of children and contexts: The longitudinal interplay among child maltreatment, community violence, and children’s symptomatology. Development and Psychopathology. 1998;10(02):235–257. doi: 10.1017/s095457949800159x. [DOI] [PubMed] [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The multidimensional anxiety scale for children (masc): factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(4):554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Marshall M, Taylor N. Tackling HIV and AIDS with faith-based communities: learning from attitudes on gender relations and sexual rights within local evangelical churches in burkina faso, zimbabwe, and south africa. Gender & Development. 2006;14(3):363–374. [Google Scholar]
- Mash R, Mash RJ. A quasi-experimental evaluation of an HIV prevention programme by peer education in the anglican church of the western cape, south africa. BMJ Open. 2012;2(2):e000638. doi: 10.1136/bmjopen-2011-000638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay MM, Alicea S, Elwyn L, McClain ZRB, Parker G, Small LA, Mellins CA. The development and implementation of theory-driven programs capable of addressing poverty-impacted children’s health, mental health, and prevention needs: Champ and champ+, evidence-informed, family-based interventions to address hiv risk and care. Journal of Clinical Child Adolescent Psychology. 2014 May;43(3):428–441. doi: 10.1080/15374416.2014.893519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mejia A, Calam R, Sanders MR. A review of parenting programs in developing countries: opportunities and challenges for preventing emotional and behavioral difficulties in children. Clinical Child and Family Psychology Review. 2012 Jun;15(2):163–75. doi: 10.1007/s10567-012-0116-9. [DOI] [PubMed] [Google Scholar]
- Miller KS, Kotchick BA, Dorsey S, Forehand R, Ham AY. Family communication about sex: what are parents saying and are their adolescents listening? Family Planning Perspectives. 1998;30(5) [PubMed] [Google Scholar]
- Miller KS, Lin CY, Poulsen MN, Fasula A, Wyckoff SC, Forehand R, Armistead L. Enhancing hiv communication between parents and children: efficacy of the parents matter! program. AIDS Education and Prevention. 2011;23(6):550–563. doi: 10.1521/aeap.2011.23.6.550. [DOI] [PubMed] [Google Scholar]
- NACC. Kenya aids indicator survey 2007. National AIDS Control Council; 2009. [Google Scholar]
- Panter-Brick C, Burgess A, Eggerman M, McAllister F, Pruett K, Leckman JF. Practitioner review: Engaging fathers -recommendations for a game change in parenting interventions based on a systematic review of the global evidence. Journal of Child Psychology and Psychiatry. 2014 Jun; doi: 10.1111/jcpp.12280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pequegnat W, Bell CC. Family and hiv/aids. New York, New York: Springer; 2012. Future directions for family-based prevention and treatment research: challenges and emerging issues; pp. 331–339. [Google Scholar]
- Poulsen MN, Vandenhoudt H, Wyckoff SC, Obong’o CO, Ochura J, Njika G, Miller KS. Cultural adaptation of a us evidence-based parenting intervention for rural western kenya: from parents matter! to families matter! AIDS Education and Prevention. 2010;22(4):273–285. doi: 10.1521/aeap.2010.22.4.273. [DOI] [PubMed] [Google Scholar]
- Puffer ES, Drabkin AS, Stashko AL, Broverman SA, Ogwang-Odhiambo RA, Sikkema KJ. Orphan status, HIV risk behavior, and mental health among adolescents in rural Kenya. Journal of pediatric psychology. 2012;37(8):868–878. doi: 10.1093/jpepsy/jss077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puffer ES, Meade CS, Drabkin AS, Broverman SA, Ogwang-Odhiambo RA, Sikkema KJ. Individual- and family-level psychosocial correlates of hiv risk behavior among youth in rural kenya. Journal of Pediatric Psychology. 2011;15(6):1264–1274. doi: 10.1007/s10461-010-9823-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puffer ES, Pian J, Sikkema KJ, Ogwang-Odhiambo RA, Broverman SA. Developing a Family-Based Hiv Prevention Intervention in Rural Kenya: Challenges in Conducting Community-Based Participatory Research. Journal of Empirical Research on Human Research Ethics. 2013;8(2):119–128. doi: 10.1525/jer.2013.8.2.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puffer ES, Watt MH, Sikkema KJ, Ogwang-Odhiambo RA, Broverman SA. The Protective Role of Religious Coping in Adolescents’ Responses to Poverty and Sexual Decision-Making in Rural Kenya. Journal of Research on Adolescence. 2012;22(1):1–7. doi: 10.1111/j.1532-7795.2011.00760.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing; Vienna, Austria: 2013. URL http://www.R-project.org/ [Google Scholar]
- Repetti RL, Taylor SE, Seeman TE. Risky families: family social environments and the mental and physical health of offspring. Psychological Bulletin. 2002;128(2):330–366. [PubMed] [Google Scholar]
- Rosenberg M. Society and the adolescent self-image 1965 [Google Scholar]
- RStudio. Rstudio: Integrated development environment for r. Boston, MA: 2015. [Google Scholar]
- Rosenberg M. Society and the adolescent self-image. Princeton, NJ: Princeton University Press; 1965. [Google Scholar]
- Sandler I, Schoenfelder E, Wolchik S, MacKinnon D. Long-term impact of prevention programs to promote effective parenting: lasting effects but uncertain processes. Annual Review of Psychology. 2011;62:299–329. doi: 10.1146/annurev.psych.121208.131619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Huedo-Medina TB, Warren MR, Johnson BT, Carey MP. Efficacy of behavioral interventions to increase condom use and reduce sexually transmitted infections: a meta-analysis, 1991 to 2010. Journal of Acquired Immune Deficiency Syndromes. 2011 Dec;58(5):489–498. doi: 10.1097/QAI.0b013e31823554d7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheeran P, Abraham C, Orbell S. Psychosocial correlates of heterosexual condom use: a meta-analysis. Psychological Bulletin. 1999;125(1):90. doi: 10.1037/0033-2909.125.1.90. [DOI] [PubMed] [Google Scholar]
- Shelton KK, Frick PJ, Wootton J. Assessment of parenting practices in families of elementary school-age children. Journal of Clinical Child Psychology. 1996;25(3):317–329. [Google Scholar]
- Smith DJ. Youth, sin and sex in nigeria: Christianity and HIV/AIDS-related beliefs and behaviour among rural-urban migrants. Culture, Health & Sexuality. 2004;6(5):425–437. [Google Scholar]
- Taylor N. Working together?: Challenges and opportunities for international development agencies and the church in the response to AIDS in africa (Tech Rep) Middlesex, UK: Tearfund; 2006. [Google Scholar]
- Thurman TR, Kidman R, Nice J, Ikamari L. Family functioning and child behavioral problems in households affected by HIV and AIDS in Kenya. AIDS and Behavior. 2015;19(8):1408–1414. doi: 10.1007/s10461-014-0897-6. [DOI] [PubMed] [Google Scholar]
- Van Campen KS, Romero AJ. How are self-efficacy and family involvement associated with less sexual risk taking among ethnic minority adolescents? Family Relations. 2012 Oct;61(4):548–558. [Google Scholar]
- Vandenhoudt H, Miller KS, Ochura J, Wyckoff SC, Obong’o CO, Otwoma NJ, Buvé A. Evaluation of a us evidence-based parenting intervention in rural western kenya: from parents matter! to families matter! AIDS Education and Prevention. 2010;22(4):328–343. doi: 10.1521/aeap.2010.22.4.328. [DOI] [PubMed] [Google Scholar]
- Wang R-H, Hsu H-Y, Lin S-Y, Cheng C-P, Lee S-L. Risk behaviours among early adolescents: risk and protective factors. Journal of Advanced Nursing. 2010;66(2):313–323. doi: 10.1111/j.1365-2648.2009.05159.x. [DOI] [PubMed] [Google Scholar]
- Weisz JR, Sandler IN, Durlak JA, Anton BS. Promoting and protecting youth mental health through evidence-based prevention and treatment. American Psychologist. 2005;60(6):628–648. doi: 10.1037/0003-066X.60.6.628. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Burstein R. Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. The Lancet. 2013;382(9904):1575–1586. doi: 10.1016/S0140-6736(13)61611-6. [DOI] [PubMed] [Google Scholar]
- WHO. Global health observatory (GHO) data: HIV/AIDS. n.d. Retrieved from http://www.who.int/gho/hiv/en/
- Wingood GM, Simpson-Robinson L, Braxton ND, Raiford JL. Design of a faith-based HIV intervention: successful collaboration between a university and a church. Health Promotion Practice. 2011;12(6):823–831. doi: 10.1177/1524839910372039. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Towards universal access: scaling up priority hiv/aids interventions in the health section: progress report 2010. Geneva: World Health Organization; 2010. [Google Scholar]


