Abstract
Purpose
We focused the attention on radiation therapy practices about the gynecological malignancies in Piedmont, Liguria, and Valle d'Aosta to know the current treatment practice and to improve the quality of care.
Material and methods
We proposed a cognitive survey to evaluate the standard practice patterns for gynecological cancer management, adopted from 2012 to 2014 by radiotherapy (RT) centers with a large amount of gynecological cancer cases. There were three topics: 1. Taking care and multidisciplinary approach, 2. Radiotherapy treatment and brachytherapy, 3. Follow-up.
Results
Nineteen centers treated gynecological malignancies and 12 of these had a multidisciplinary dedicated team. Radiotherapy option has been used in all clinical setting: definitive, adjuvant, and palliative. In general, 1978 patients were treated. There were 834 brachytherapy (BRT) treatments. The fusion between diagnostic imaging (magnetic resonance imaging – MRI, positron emission tomography – PET) and computed tomography (CT) simulation was used for contouring in all centers. Conformal RT and intensity modulated radiation therapy (IMRT) were the most frequent techniques. The image guided radiation therapy (IGRT) was used in 10/19 centers. There were 8 active BRT centers. Brachytherapy was performed both with radical intent and as boost, mostly by HDR (6/8 centers). The doses for exclusive BRT were between 20 to 30 Gy. The doses for BRT boost were between 10 and 20 Gy. Four centers used CT-MRI compatible applicators but only one used MRI for planning. The BRT plans on vaginal cuff were still performed on traditional radiographies in 2 centers. The plan sum was evaluated in only 1 center. Only 1 center performed in vivo dosimetry.
Conclusions
In the last three years, multidisciplinary approach, contouring, treatment techniques, doses, and control systems were similar in Liguria-Piedmont and Valle d'Aosta. However, the technology implementation didn't translate in a real treatment innovation so far.
Keywords: brachytherapy, gynecological cancer, multidisciplinary, radiotherapy
Purpose
Worldwide, cervical carcinoma is the fourth largest cause of death from cancer in women and overall gynecological cancer responsible for more than 14% of female cancer deaths. That is more than breast cancer or female lung cancer [1]. In Italy, the incidence of gynecological cancers is about 10% with about 16,600 cases occurring every year, of which 27% of cases are recorded in Northern Italy [2]. The collective population of Piedmont (4,500,000), Liguria (1,600,000), and Valle d'Aosta (128,000) is of about 6,200,000 inhabitants, which represents an important catchment area for radiotherapy (RT) centers in these regions. In several countries, the documentation of use of RT to treat gynecological malignancies has produced interesting researches [3, 4, 5, 6, 7, 8] (Table 1). However in Italy, the Oncology Network of Piedmont and Valle d'Aosta does not currently produce guidelines for gynecological tumors, and the two Italian documents of the AIRO (Italian Association of Radiation Oncology) brachytherapy group are outdated [9, 10].
Table 1.
Gynecological surveys of the last five years
| Authors | Years | Country | Type | Survey responders | Patients analyzed |
|---|---|---|---|---|---|
| Lee et al. [3] | 2015 | Korea | Endometrial cancer | 108/218 | – |
| Battista et al. [4] | 2015 | Germany | Endometrial cancer | 273/682 | – |
| Thompson et al. [5] | 2014 | Australia | Cervical cancer | 9 | 76 |
| Tomita et al. [6] | 2012 | Japan | Cervical cancer | – | 1200 |
| Viswanathan et al. [7] | 2012 | GCIG (intergroup) | Cervical cancer | 72/74 | – |
| Small et al. [8] | 2009 | GCIG (intergroup) | Endometrial cancer | 34/74 | – |
In 2015, at the tri-regional annual meeting of the AIRO, we focused our attention on RT practices adopted in these regions for the treatment of gynecological tumors. We designed a survey, which would investigate the standard practices for gynecological cancer management adopted in the last three years in order to obtain current data about RT treatment with modern techniques and technologies.
The main purpose of the survey was to produce a snapshot of the current use of brachytherapy (BRT) and external beam radiotherapy (EBRT) in the treatment of gynecological tumors in the three regions concerned. The second goal was to produce guidelines, based on the latest evolution of BRT and EBRT in gynecology cancer treatment (image guided adaptive brachytherapy and radiotherapy – IGABT and IGRT). The third and most important objective was to improve the quality of care with the aim to offer the best treatment to all patients in this area and to optimize local resources.
Material and methods
A 30-questions survey was designed by the host of the tri-regional annual meeting of the AIRO, approved by the scientific council of the tri-regional AIRO and proposed to the centers with a large amount of gynecological cancer cases. The survey included questions about the organization of patient care, clinical choices, and types of treatments in the years 2012, 2013, and 2014. We know that 19 regional centers of radiotherapy (1 in Valle d'Aosta, 5 in Liguria, and 13 in Piedmont) deal with gynecological diseases: 14 general hospitals; 3 university hospitals (1 reserved to gynecological and pediatric cancers only); 1 cancer institute, and 1 private clinic. All these centers responded to the survey.
To cover the entire process of treatment management, the survey was divided into three sections. The first section concerned patient management and multidisciplinary approaches, which includes EBRT and BRT (the number of patients, computed tomography [CT]-simulation, contouring, dose prescription, planning, delivery, and treatment verification). The second group of questions regarded follow-up (assessment of outcome and toxicity), and the third area of inquiry was scientific productivity. The completed surveys were collected and the answers were processed by the reference center.
Results
Patient management and multidisciplinary approach
Twelve of the centers involved in the research program had a multidisciplinary team dedicated to gynecological tumors. In five cases, the same group was also involved in breast cancer with the constant presence of the surgeon, oncologist, and radiation oncologist. Other complementary specialists were present in some centers: a pathologist in nine, a radiologist in eight, a nuclear medicine specialist in seven, a pain therapist in four, a psychologist in two, and lastly a nurse and a specialist in palliative care only in one center. Only in 2 hospitals all the patients were taken care directly by a gynecological interdisciplinary care group (GIC). Radiotherapy approach is different according to the anatomical sites (endometrium, cervix, vagina, and vulva), except for ovarian cancer. In fact, for ovarian cancer, the use of RT has been traditionally limited in Italy with a stronger preference for surgical and oncological options. Table 2 shows the number of centers treating the different gynecological pathologies. Chemotherapy was performed in all centers by a medical oncologist, except in one center where chemotherapy was directly performed by a radiation oncologist.
Table 2.
Number of centers treating different pathologies
| Technique | Endometrium N (%) |
Cervix N (%) |
Vagina N (%) |
Vulva N (%) |
Ovary N (%) |
|---|---|---|---|---|---|
| Postoperative radiotherapy | 16 (84) | 15 (79) | 9 (47) | 15 (79) | 0 |
| Recurrence radiotherapy | 14 (74) | 14 (74) | 11 (58) | 13 (68) | 2 (18) |
| Radical radiotherapy | 12 (63) | 16 (84) | 14 (74) | 12 (63) | 1 (5) |
| Brachytherapy | 10 (53) | 10 (53) | 8 (42) | 6 (32) | 0 |
| Palliative radiotherapy | 16 (84) | 14 (74) | 14 (74) | 15 (79) | 11 (58) |
| Clinical protocols | 7 (37) | 7 (37) | 0 | 0 |
Radiotherapy
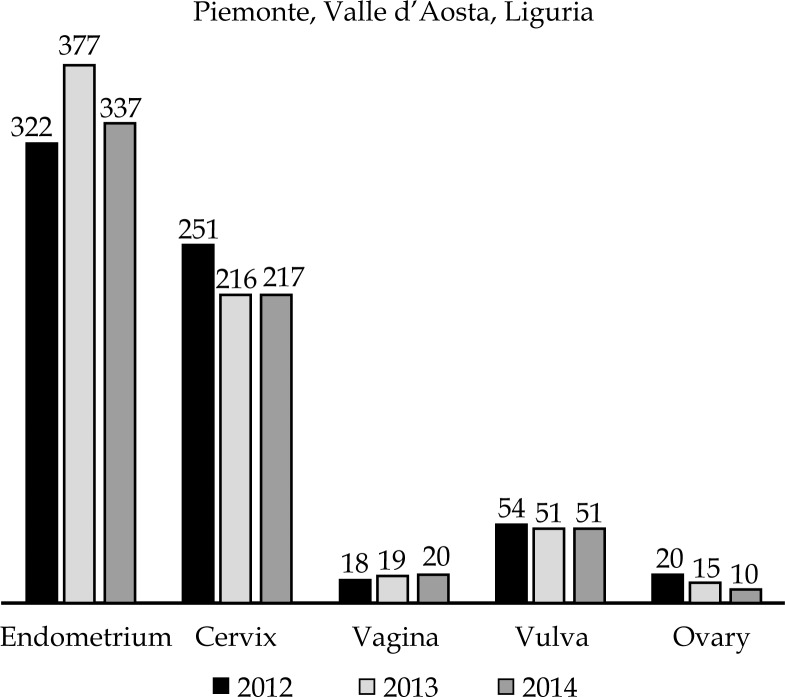
One thousand nine hundred seventy-eight patients affected by gynecological malignancies received RT in the last three years. The trend was quite stable: 665 cases treated in 2012, 678 in 2013, and 635 in 2014. Post-operative treatment was mainly used in endometrial (802 cases) and vulvar cancer (70 cases), while in cervical cancer the radiotherapy intent was equally distributed (279 cases, 259 radical cases), and the palliative intent was the preeminent indication in ovarian cancer (39 cases) (Table 3). Finally, the number of patients treated according to multicenter and/or international clinical protocols was less than 10% and is carried out in only six of nineteen centers. Figure 1 shows the trend of gynecological RT during the period 2012-2014.
Table 3.
Patients number according to tumor site and intent of treatment
| Intent | Endometrium | Cervix | Vagina | Vulva | Ovary |
|---|---|---|---|---|---|
| Postoperative radiotherapy | 802 | 279 | 12 | 78 | 1 |
| Recurrence radiotherapy | 79 | 38 | 9 | 17 | 8 |
| Radical radiotherapy | 27 | 259 | 27 | 18 | 0 |
| Palliative radiotherapy | 47 | 70 | 13 | 26 | 39 |
| Brachytherapy | 401 | 228 | 13 | 5 | 3 |
| Clinical protocols | 80 | 56 | 0 | 4 | 0 |
Fig. 1.
Trend of gynecological radiotherapy (during 2012-2014)
In eight centers, gross tumor volume (GTV) delineation was performed with diagnostic imaging (CT and/or magnetic resonance imaging [MRI] contrast agents and/or positron emission tomography [PET]-CT) in the treatment position fused with CT simulation without contrast enhancement (CE): rigid fusion in 5 cases, elastic in 3 cases. In eleven centers, contouring was performed with diagnostic imaging (CT and/or MRI contrast agents and/or PET-CT) but not in the treatment position, and fusion with CT simulation was rigid in 5 cases and elastic in 6 cases. Eleven centers also performed CE-CT simulation, and fusion with CE-MRI and/or PET-CT in the treatment position. Five centers used CT simulation alone. Regarding the use of the margins around the GTV to the clinical target volume (CTV) and from CTV to planning target volume (PTV), it was preferred in both cases to adopt margins between 5 and 10 mm. In six centers, the adoption of the internal target volume (ITV) minimized these margins under 5 mm.
The more frequent dose delivery techniques were conformal RT (3DCRT) and static IMRT by linear accelerator (LINAC) with a slight prevalence of the second. Six centers also used volumetric techniques (tomotherapy or VMAT). Conventional fractionation is the most used; only two centers employed hypofractionated schedule. The dose range of EBRT for most of the centers was between 50 Gy and 60 Gy (Table 4), using typically a boost with BRT.
Table 4.
Radiotherapy by centers according to dose and tumor sites
| Dose (Gy) | Endometrium N (%) |
Cervix N (%) |
Vagina N (%) |
Vulva N (%) |
Ovary N (%) |
Recurrence/persistence N (%) |
|---|---|---|---|---|---|---|
| 50 | 12 (63) | 11 (58) | 9 (47) | 7 (32) | 4 (21) | 7 (37) |
| > 50 – ≤ 60 | 10 (53) | 9 (47) | 8 (42) | 10 (53) | 1 (5) | 9 (47) |
| > 60 | 2 (11) | 4 (21) | 3 (16) | 5 (26) | 1 (5) | 3 (16) |
The treatment verification method most frequently used was 2D electronic portal imaging device (EPID) with MV beam (12/19), or KV beam (5/19). The volumetric methods of IGRT were common and were employed in ten of nineteen centers.
Brachytherapy
The cases treated with BRT were essentially stable over time: 200 in 2012, 222 in 2013, and 228 in 2014. There were eight active centers (the ninth was closed in 2013). Six of those were equipped with high-dose-rate (HDR) machines, one center with HDR, low-dose-rate (LDR), and pulsed-dose-rate (PDR) devices and one center with a PDR machine.
Four centers used CT-MRI compatible applicators. One center recently acquired the equipment to perform a combined intracavitary and interstitial gynecological BRT, to boost parametrial disease or to treat patients with unsatisfactory dose distribution with a standard applicator. Four centers fixed the cylinder applicators, three centers using plate, and one using bandages.
The BRT was performed both with radical intent and as a boost (Table 5) mostly by HDR. The exclusive BRT was performed prescribing doses between 20-30 Gy in 4-6 Gy/fraction. For unfit patients doses of 21 Gy in 3 fractions were used (Table 6). The BRT boost was administrated with doses between 10-20 Gy in 2-4 sessions.
Table 5.
Radiotherapy techniques according to tumor sites
| Radiotherapy technique | Endometrium N (%) |
Cervix N (%) |
Vagina N (%) |
Vulva N (%) |
Ovary N (%) |
Recurrence/persistence N (%) |
|---|---|---|---|---|---|---|
| 3DCRT | 10 (53) | 12 (63) | 9 (47) | 9 (47) | 5 (26) | 10 (53) |
| LINAC IMRT | 12 (63) | 12 (63) | 8 (42) | 10 (53) | 3 (16) | 8 (42) |
| Tomotherapy | 3 (16) | 3 (16) | 3 (16) | 3 (16) | 2 (11) | 3 (16) |
| VMAT | 3 (16) | 4 (21) | 3 (16) | 4 (21) | 2 (11) | 3 (16) |
| Conventional fractionation | 15 (79) | 15 (79) | 12 (63) | 13 (68) | 6 (32) | 12 (63) |
| Hypofractionation | 1 (5) | 1 (5) | 0 | 1 (5) | 3 (16) | 4 (21) |
| Concomitant boost | 8 (42) | 9 (47) | 7 (37) | 7 (37) | 1 (5) | 5 (26) |
| Sequential boost | 10 (53) | 11 (58) | 7 (37) | 9 (47) | 1 (5) | 6 (32) |
| HDR boost | 9 (47) | 7 (37) | 3 (16) | 2 (11) | 0 | 4 (21) |
| Definitive HDR | 6 (32) | 5 (26) | 3 (16) | 1 (5) | 0 | 4 (21) |
| PDR boost | 1 (5) | 1 (5) | 0 | 1 (5) | 0 | 0 |
| Definitive PDR | 0 | 0 | 1 (5) | 0 | 0 | 0 |
3DCRT – 3 dimensional radiation therapy, IMRT – intensity-modulated radiotherapy, VMAT – volumetric arc therapy, HDR – high-dose-rate, PDR – pulsed-dose-rate
Table 6.
Range of doses of brachytherapy according to technique and tumor sites
| Technique | Endometrium [Gy] | Cervix [Gy] | Vagina [Gy] | Vulva [Gy] | Ovary [Gy] | Recurrence/persistence [Gy] |
|---|---|---|---|---|---|---|
| HDR boost | 10-20 | 10-20 | 10 | 15 | 0 | 0 |
| Definitive HDR | 15-30 | 20-30 | 15-27 | 0 | 0 | 15-20 |
| PDR boost | 10-15 | 15-20 | 15-20 | 0 | 0 | 0 |
| Definitive PDR | 15-20 | 20-25 | 15-20 | 0 | 0 | 0 |
HDR – high-dose-rate, PDR – pulsed-dose-rate
Brachytherapy boost was usually administered in two sessions a week, not concurrent with EBRT, except in one center. The interval between EBRT and BRT was 6.6 days on average (range 3-10). A single RT department employed a two daily hyperfractionated treatments for endometrial cancers unfit for surgery. All BRT plans with tandem applicator were calculated on CT scan, except one that used MRI. Two centers still used the traditional planning by radiographs for BRT on vaginal cuff; no center used MRI for BRT planning with cylinder. In all centers were used rectum preparation and bladder filling to control organ and/or tumor motion in EBRT. In BRT, rectum preparation was used in 4 centers. In all centers, patients were contoured and planned with the Oncentra® Brachy Treatment Planning System. The treatments were performed with microSelectron v2 afterloader system (Elekta A.B. Stockholm, Sweden) in 5 centers or v3 Digital (Elekta A.B. Stockholm, Sweden) in 3 centers. Only one center performed in vivo dosimetry by means of rectal tandem diodes. For radical treatments, 4 centers used a control imaging each BRT session and 2 centers performed a re-planning. For adjuvant BRT, 2 centers used the same control and only one performed a re-planning.
Follow-up
A program of follow-up treatment was offered to assess the treatment response and possible side effects, evaluated according to RTOG (Radiation Therapy Oncology Group)/EORTC (European Organization for Research and Treatment of Cancer) scale. The follow-up was widely shared with gynecologists and clinical oncologists (in 10 centers): only in three centers follow-up was performed by a radiation oncologist with a frequency, for the majority of cases, of about four months for a duration of one year in one center, five years in eight centers, and ten years or more in the six remaining centers.
The last topic to be evaluated was the scientific productivity of the different centers. One center published in medical journals in the last three years [11, 12, 13, 14, 15] and nine centers produced abstracts for various events. Finally, five centers were involved in clinical trials regarding gynecologic oncology.
Discussion
Multidisciplinarity is a hot topic due to the proliferation of highly specialized structures that involve different specialists as surgeons, clinicians, and radiation oncologists. This synergy has resulted in excellent therapeutic strategies [16, 17, 18, 19]. However, the possibility to perform formal multidisciplinary meeting with different specialists is a difficult challenge due to a lack of staff time. The incidence of treated patients was shown to be stable over time (Figure 1) and RT was an established option for all different intents of care. However, the low number of patients treated in clinical trials does not allow a comparison among different centers limiting offered treatments. Gynecological radiotherapy is only now beginning to take advantage of the technological innovations available [20, 21, 22]. The use of new morphological and functional diagnostic imaging (multiparametric MRI, 18-FDG PET) allowed not only to optimize the disease staging and to contour with precision the target volumes, integrating multimodality imaging information by rigid or elastic co-registration algorithms. For target delineation, all centers used the fusion between diagnostic imaging and CT simulation in different ways. An uncommon method was contouring directly on PET-CT or MRI. However, these methods did not allow the adoption of reduced margins, which is one of the goals for a better target definition. Technological development also introduced the use of new irradiation techniques such as IMRT, which allows, thanks to the possibility of a better dose conformation, to deliver high doses preserving healthy tissue close to the target. Therefore, the new control system of the images (IGRT) allowed for safe delivery high hypofractionated doses [23, 24, 25].
The results showed that LINAC-IMRT was almost used as 3DCRT, and the adoption of volumetric techniques (tomotherapy and VMAT) also increased (Table 5). Despite the fact that IMRT appeared to be a well-established technique for the complex volumes irradiation, such as the pelvic and/or lumbar-aortic volume, different verification modalities (traditional portal verification and modern image guidance) coexisted. It could be due to the equipment modernization with the coexistence (double control) of both modalities, or to the use of different imaging modalities for different treatments. Therefore, the implementation of these new techniques did not modify the use of conventional fractionation (Table 5) or the dose range (Table 4 and 6).
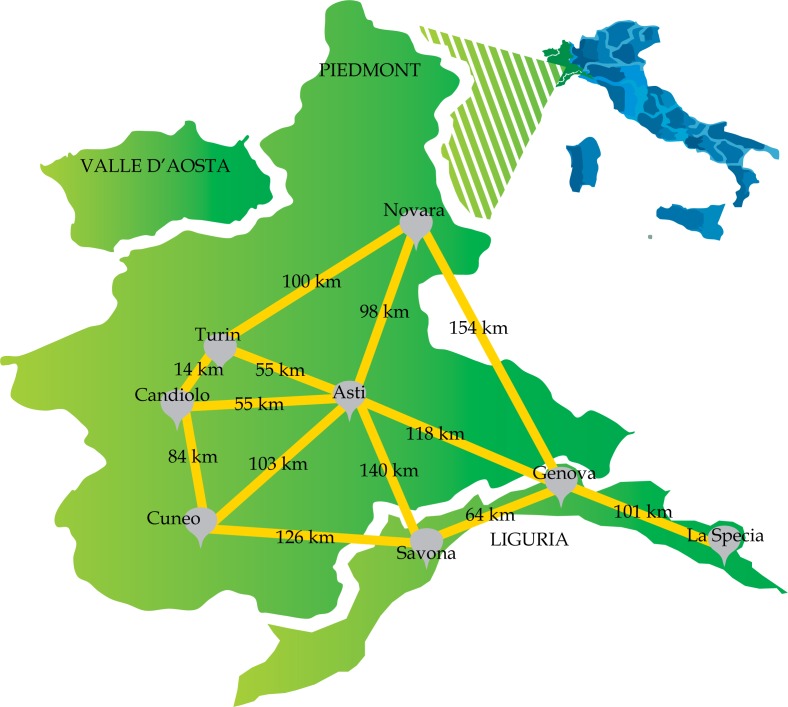
Even if in Italy BRT is a technique which is gradually falling out of use due to the lack of dedicated radiation oncologists, in the North-West Italian regions BRT is still widely used and the treated cases were essentially stable as displayed in Figure 1. In most gynecological cancers, BRT remains a powerful weapon even in comparison to the sophisticated techniques of EBRT. Intensity modulated radiation therapy with IGRT can hardly compete with an optimal BRT implant in terms of organ motion management and dose distribution. Historically, our BRT centers were located far from each other (the mean distance between each center is more than 90 km), rather than concentrated in a few specialized institutions (Figure 2). Recent studies evaluated the effect of distance on the possibility of access to RT care [26] but there are no papers dedicated to BRT. A future goal would be to assess how many patients do not receive BRT due to the distances and the center distribution within the catchment area.
Fig. 2.
Distribution of brachytherapy centers on the territory
The HDR technique was the most commonly used, because it is fast, cheap, acceptable to patients, and does not require hospitalization. Furthermore, only two centers had care protected rooms, in which LDR and PDR were performed. Over half of the centers used MRI compatible applicators but contouring and planning were performed on CT in most cases, since it was very difficult to have the availability of MRI equipment. In few cases where a dedicated CT was not present, adjuvant BRT planning was performed using orthogonal radiographs.
In order to understand the current practice in our regions, the questions proposed were basic while the topics were extensive. For this reason, the study shows several limitations due to the lack of more detailed analysis for each topic: EBRT, BRT, contouring, planning and diagnostic pathway, and other related therapies. New surveys will be proposed in order to complete the information gaps. The final results will allow us to create a treatment guideline, which will be proposed to the oncology network for our regions.
Conclusions
This survey, following the example of other countries [3, 4, 5, 6, 7, 8], is the first to asses practice patterns for RT treatments in Liguria-Piedmont-Valle d'Aosta. It shows that in the last three years, the RT practice shifted towards multidisciplinary cares with a uniformity of performance as regards techniques, doses, and treatment volumes. The use of IMRT is almost comparable to the more traditional 3D practices, and the more modern simulation approaches and volumes identification seem to result, in many cases, in traditional control treatment systems, fractionation schedules, and doses.
There are an appropriate numbers of BRT centers that are well distributed in the territory. Computed tomography planning is almost a standard, and the introduction of MRI is starting, but up to now is limited by the availability of resources. High-dose-rate brachytherapy is the most common technique because it is easy and does not require hospitalization. The efforts in implementation of technology made by different centers, in this hardship time, still do not translate effectively into a scientific production, which could help us to evaluate the effectiveness of gynecological tumor treatment in our region. Human resources, shared data, and time dedicated to research may allow a more complete analysis. The purpose of this survey is to inform all radiation oncologists of the results achieved in order to define goals for the future in the context of multidisciplinary cooperation, and the creation of a set of common guidelines. In this way, we aim to improve the treatment offered to all patients of the three regions.
Acknowledgements
The research was supported by 5 x Mille 2008 Ministero della Salute – FPRC Onlus and 5 x Mille 2009 Ministero della Salute – FPRC Onlus.
Meeting presentations
This manuscript is based on data presented at the tri-regional annual meeting of the Italian Association of Radiation Oncologist (AIRO) in Candiolo, May 23, 2015.
Disclosure
Authors report no conflict of interest.
References
- 1.Ferlay J, Shin HR, Bray F, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127:2893–2917. doi: 10.1002/ijc.25516. [DOI] [PubMed] [Google Scholar]
- 2.AIOM-CCM-AIRTUM. Intermedia Editore; I numeri del cancro in Italia 2014. [Google Scholar]
- 3.Lee JY, Kim K, Lee TS, et al. Controversies in the management of endometrial cancer: a survey of the Korean Gynecologic Oncology Group. J Gynecol Oncol. 2015;26:277–283. doi: 10.3802/jgo.2015.26.4.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Battista MJ, Schmidt M, Rieks N, et al. Adjuvant treatment decisions for patients with endometrial cancer in Germany: results of the nationwide AGO pattern of care studies from the years 2013, 2009, and 2006. J Cancer Res Clin Oncol. 2015;141:555–562. doi: 10.1007/s00432-014-1834-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Thompson SR, Delaney GP, Gabriel GS, et al. Patterns of care study of brachytherapy in New South Wales: cervical cancer treatment quality depends on caseload. J Contemp Brachytherapy. 2014;6:28–32. doi: 10.5114/jcb.2014.42022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tomita N, Toita T, Kodaira T, et al. Patterns of radiotherapy practice for patients with cervical cancer in Japan, 2003-2005: changing trends in the pattern of care process. Int J Radiat Oncol Biol Phys. 2012;83:1506–1513. doi: 10.1016/j.ijrobp.2011.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Viswanathan AN, Creutzberg CL, Craighead P, et al. International brachytherapy practice patterns: a survey of the Gynecologic Cancer Intergroup (GCIG) Int J Radiat Oncol Biol Phys. 2012;82:250–255. doi: 10.1016/j.ijrobp.2010.10.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Small W, Jr, Du Bois A, Bhatnagar S, et al. Gynecologic Cancer Intergroup (GCIG) Practice patterns of radiotherapy in endometrial cancer among member groups of the gynecologic cancer intergroup. Int J Gynecol Cancer. 2009;19:395–399. doi: 10.1111/igc.0b013e3181a1cee8. [DOI] [PubMed] [Google Scholar]
- 9.Gruppo di studio Brachiterapia. AIRO; 1998. Standard di riferimento in brachiterapia del carcinoma dell'endometrio. [Google Scholar]
- 10.Gruppo di studio Brachiterapia. AIRO; 2002. La Radioterapia dei tumori ginecologici. Indicazioni e criteri di guida. [Google Scholar]
- 11.Gadducci A, Cosio S, Landoni F, et al. Adjuvant treatment and analysis of failures in patients with high-risk FIGO Stage Ib-II endometrial cancer: an Italian multicenter retrospective study (CTF study) Gynecol Oncol. 2014;134:29–35. doi: 10.1016/j.ygyno.2014.04.008. [DOI] [PubMed] [Google Scholar]
- 12.Piovano E, Fuso L, Poma CB, et al. Complications after the treatment of endometrial cancer: a prospective study using the French-Italian glossary. Int J Gynecol Cancer. 2014;24:418–426. doi: 10.1097/IGC.0000000000000094. [DOI] [PubMed] [Google Scholar]
- 13.Carrara L, Gadducci A, Landoni F, et al. Could different follow-up modalities play a role in the diagnosis of asymptomatic endometrial cancer relapses?: an Italian multicentric retrospective analysis. Int J Gynecol Cancer. 2012;22:1013–1019. doi: 10.1097/IGC.0b013e31825ad3ee. [DOI] [PubMed] [Google Scholar]
- 14.Landoni F, Sartori E, Maggino T, et al. Is there a role for postoperative treatment in patients with stage Ib2-IIb cervical cancer treated with neo-adjuvant chemotherapy and radical surgery? An Italian multicenter retrospective study. Gynecol Oncol. 2014;132:611–617. doi: 10.1016/j.ygyno.2013.12.010. [DOI] [PubMed] [Google Scholar]
- 15.Katsaros D, Gribaudo S. The proper use of multimodality treatment in locally advanced cervical cancer. Gynecol Oncol. 2011;121:422–423. doi: 10.1016/j.ygyno.2010.12.346. author reply 422. [DOI] [PubMed] [Google Scholar]
- 16.Patel A, Franko ER, Jr, Fleshman JW. Utilizing the multidisciplinary team for planning and monitoring care and quality improvement. Clin Colon Rectal Surg. 2015;28:12–20. doi: 10.1055/s-0035-1545065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rao K, Manya K, Azad A, et al. Uro-oncology multidisciplinary meetings at an Australian tertiary referral centre – impact on clinical decision-making and implications for patient inclusion. BJU Int. 2014;114(Suppl 1):50–54. doi: 10.1111/bju.12764. [DOI] [PubMed] [Google Scholar]
- 18.Ottevanger N, Hilbink M, Weenk M, et al. Oncologic multidisciplinary team meetings: evaluation of quality criteria. Eval Clin Pract. 2013;19:1035–1043. doi: 10.1111/jep.12022. [DOI] [PubMed] [Google Scholar]
- 19.Gabriele P. Quality standards in multidisciplinary setting. ESTRO course Praha 2013, November 9-12 and Turin 2015, February 1-4. [Google Scholar]
- 20.Portelance L, Chao KS, Grigsby PW, et al. Intensity-modulated radiation therapy (IMRT) reduces small bowel, rectum, and bladder doses in patients with cervical cancer receiving pelvic and para-aortic irradiation. Int J Radiat Oncol Biol Phys. 2001;51:261–266. doi: 10.1016/s0360-3016(01)01664-9. [DOI] [PubMed] [Google Scholar]
- 21.Fernandez-Ots A, Crook J. The role of intensity modulated radiotherapy in gynecological radiotherapy: Present and future. Rep Pract Oncol Radiother. 2013;18:363–370. doi: 10.1016/j.rpor.2013.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hymel R, Jones GC, Simone CB., 2nd Whole pelvic intensity-modulated radiotherapy for gynecological malignancies: A review of the literature. Crit Rev Oncol Hematol. 2015;94:371–379. doi: 10.1016/j.critrevonc.2014.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gill BS, Lin JF, Krivak TC, et al. National Cancer Data Base analysis of radiation therapy consolidation modality for cervical cancer: the impact of new technological advancements. Int J Radiat Oncol Biol Phys. 2014;90:1083–1090. doi: 10.1016/j.ijrobp.2014.07.017. [DOI] [PubMed] [Google Scholar]
- 24.Townamchai K, Poorvu PD, Damato AL, et al. Radiation dose escalation using intensity modulated radiation therapy for gross unresected node-positive endometrial cancer. Pract Radiat Oncol. 2014;4:90–98. doi: 10.1016/j.prro.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 25.Rijkmans EC, Nout RA, Rutten IH, et al. Improved survival of patients with cervical cancer treated with image-guided brachytherapy compared with conventional brachytherapy. Gynecol Oncol. 2014;135:231–238. doi: 10.1016/j.ygyno.2014.08.027. [DOI] [PubMed] [Google Scholar]
- 26.Gabriel G, Barton M, Delaney GP. The effect of travel distance on radiotherapy utilization in NSW and ACT. Radiother Oncol. 2015;117:386–389. doi: 10.1016/j.radonc.2015.07.031. [DOI] [PubMed] [Google Scholar]