Abstract
Background
The efficacy and safety of hypnotic techniques in somatic medicine, known as medical hypnosis, have not been supported to date by adequate scientific evidence.
Methods
We systematically reviewed meta-analyses of randomized controlled trials (RCTs) of medical hypnosis. Relevant publications (January 2005 to June 2015) were sought in the Cochrane databases CDSR and DARE, and in PubMed. Meta-analyses involving at least 400 patients were included in the present analysis. Their methodological quality was assessed with AMSTAR (A Measurement Tool to Assess Systematic Reviews). An additional search was carried out in the CENTRAL and PubMed databases for RCTs of waking suggestion (therapeutic suggestion without formal trance induction) in somatic medicine.
Results
Out of the 391 publications retrieved, five were reports of meta-analyses that met our inclusion criteria. One of these meta-analyses was of high methodological quality; three were of moderate quality, and one was of poor quality. Hypnosis was superior to controls with respect to the reduction of pain and emotional stress during medical interventions (34 RCTs, 2597 patients) as well as the reduction of irritable bowel symptoms (8 RCTs, 464 patients). Two meta-analyses revealed no differences between hypnosis and control treatment with respect to the side effects and safety of treatment. The effect size of hypnosis on emotional stress during medical interventions was low in one meta-analysis, moderate in one, and high in one. The effect size on pain during medical interventions was low. Five RCTs indicated that waking suggestion is effective in medical procedures.
Conclusion
Medical hypnosis is a safe and effective complementary technique for use in medical procedures and in the treatment of irritable bowel syndrome. Waking suggestions can be a component of effective doctor–patient communication in routine clinical situations.
Hypnosis for purposes of medical treatment goes back a long way. The British Medical Association endorsed the use of hypnosis in somatic medicine in 1955, on the basis of case reports and series backed up by expert consensus, and the American Medical Association followed suit in 1958 (1, 2). Whether robust evidence exists for the efficacy and safety of hypnosis in somatic medicine in the era of evidence-based medicine (EBM) (3) remains to be clarified. Because systematic reviews with quantitative analysis (meta-analyses) of randomized controlled trials provide the highest level of evidence in EBM (3), we decided to carry out a systematic review of meta-analyses on medical hypnosis.
The aims of this article are as follows:
To define the various forms of hypnosis
To describe the requirements that have to be fulfilled before therapeutic hypnosis can be carried out
To provide a historical overview of the use of hypnosis in medicine and the assessment of its efficacy
To identify the indications for medical hypnosis supported by robust evidence
To present the evidence for use of positive suggestions as a component of effective doctor– patient communication.
Definitions
The term “hypnosis” is used to mean both an altered state of consciousness (synonym: hypnotic trance) and the procedure by which this state is induced (4). During a hypnotic trance physiological, cognitive, and affective processes as well as behavior can be modified. A hypnotic state and hypnotic phenomena can be induced by another person (therapist) or alone (self-hypnosis). The subjective experience of hypnosis is characterized by a high degree of authenticity (experienced as real) and involuntariness (“it happens by itself”) (4).
Hypnosis can be distinguished from other states of consciousness such as normal wakefulness, sleep, deep relaxation, or meditation by means of electroencephalography (EEG) and imaging modalities (4). A hypnotic trance is characterized by a number of physiological and mental reactions, e.g., altered perception of time, selective amnesia, regression to a younger age (retrieval of memories or experiences from an earlier developmental stage), a marked inward focus, and heightened suggestibility, i.e., a stronger reaction to suggestions (4). In clinical situations associated with high affective participation of the patient, such as emergencies, diagnostic and therapeutic interventions, or communication of a serious diagnosis, hypnotic phenomena may occur spontaneously (e1, e2).
Suggestions work via verbal and nonverbal signals that correspond to internal expectations and have a powerful effect on mental and involuntary somatic processes. For example, cutaneous perfusion or the flow of saliva is not amenable to influence by a deliberate intellectual action, but can be affected by a suggestion, e.g., a picture or a story. In general use the word “suggestion” tends to imply manipulation, but in hypnosis it should be understood as meaning a proposal, an offer of options (“I suggest”). In contrast to the widespread preconceptions, hypnosis is not authoritarian, passive, and centered around the therapist, but a resource- and solution-oriented method in which the focus is on the patient’s own potentials (4).
Applications of hypnosis
Depending on the goals, various applications of hypnotic techniques can be distinguished (4):
-
Medical hypnosis
Alleviation of somatic symptoms
Reduction of mental stress during medical treatment
Amelioration of disordered physiological/biochemical parameters
Facilitation of physiological/biochemical healing processes
-
Hypnotic communication
Waking suggestions (suggestions without trance induction)
Suggestions with the patient under general anesthesia
Use of findings from hypnotherapy for effective doctor–patient communication
-
Hypnotherapy (psychotherapy with the patient in a trance)
Improvement of problem management by giving the patient access to their own resources
Facilitation of changes in behavior
Restructuring (minimization, reinforcement, new conditioning) of cognitive–affective patterns
Restructuring of emotionally stressful events and sensations
Reintegration of non-accessible (dissociated) feelings
-
Experimental hypnosis
Basic research on somatic sensations (e.g., pain), emotions, and states of consciousness
-
Stage hypnosis
Demonstration of hypnotic phenomena to entertain an audience
The perception of hypnosis as an authoritarian, manipulative technique, nourished particularly by its use in stage shows, represents the greatest barrier to the (re)integration of hypnosis into medical treatment.
Phases of medical hypnosis
A session of medical hypnosis generally lasts between 20 and 50 min and can be divided into various phases (4):
- Verification of the indication; explanation (correction of inappropriate anxiety or false expectations); definition of goal(s)
Induction
Consolidation
Therapeutic suggestions
Reorientation, posthypnotic suggestions
Discussion
Integration into daily routine: use of an audio file at home; behavioral exercises (e.g., exposure training); possibly learning of self-hypnosis techniques.
A selection of broadcasts (mostly in German) publicly available on the internet can be found in eBox 1.
eBox 1. Selection of German-language videos and podcasts from public broadcasters on medical hypnosis.
-
3Sat 2015
Hypnosis in irritable bowel syndrome (gut-directed hypnosis): www.youtube.com/watch?v=AjBHaKq8B_g (6 min)
-
ZDF Abenteuer Wissen 2009
Medical hypnosis in the treatment of chronic pain and in surgery: www.youtube.com/watch?v=MdLQvrl84hU Plastic surgery, dental treatment (12 min)
-
ARD W wie Wissen 2014
The power of hypnosis: http://www.daserste.de/information/wissen-kultur/w-wie-wissen/videos/die-kraft-der-hypnose-100.html Dental treatment, brain MRI showing how hypnosis alleviates pain, brain surgery with the patient awake (7 min)
-
SWR Odysso 2014
Medicine: The healing power of the psyche: http://www.swr.de/odysso/medizin-die-heilkraft-der-psyche/-/id=1046894/did=14145774/nid=1046894/wrks2i/index.html Documentary on healing thoughts; the importance of waking suggestions and a positive attitude for the success of heart surgery (46 min)
-
SWR Odysso 2011
Hypnosis instead of general anesthesia: http://www.swr.de/odysso/hypnose-statt-vollnarkose/-/id=1046894/did=7345782/nid=1046894/3hlrni/index.html The anesthesia technique of hypnosedation, successfully used in over 8000 surgical patients in Belgium. This technique combines hypnosis with very light sedation and local anesthesia; the patient remains awake.
-
WDR Planet Wissen 2016
How negative thinking makes us ill: www1.wdr.de/mediathek/video/sendungen/planet-wissen-wdr/video-wie-uns-negative-gedanken-krank-machen-100.html Video about placebo and nocebo effects (58 min)
-
3sat 2012
Hypnosis instead of anesthesia: www.3sat.de/mediathek/?display=1&mode=play&obj=30167 Maxillary surgery on hypnosedated patients (5 min)
-
BBC exklusiv
www.youtube.com/watch?v=qJAnCLIBBus&feature=youtu.be Surgery with hypnosis instead of anesthesia; experimental pain; brain MRI showing how hypnosis alleviates pain (11 min)
-
HR alles wissen 2015
Hypnosis to counteract fear of the dentist: www.ardmediathek.de/tv/alles-wissen/Hypnose-gegen-Zahnarztphobie/hr-fernsehen/Video?documentId=29814680&bcastId=3416170 Dental treatment, brain MRI showing how hypnosis alleviates pain (6 min)
-
Radio: SWR 27.05.2015
Hypnotherapy: trance induction to combat anxiety and pain: www.ardmediathek.de/radio/SWR2-Wissen/Hypnotherapie-Trance-als-Mittel-gegen-%C3%84/SWR2/Audio-Podcast?documentId=28528316&bcastId=220656 (27 min)
Formal requirements
In Israel and Sweden, hypnosis may be carried out only by physicians and psychologists who have received appropriate training. In Germany, from the legal point of view, anyone can offer hypnosis for non-medical reasons. Treatment of illness by means of hypnosis requires a license to perform procedures for the purpose of healing (medical and psychological psychotherapists, child and adolescent psychotherapists, naturopaths) (e3). Medical hypnosis can be carried out by physicians of all patient-related specialties in the framework of basic psychosomatic care. An invoice for relaxation hypnosis according to the official German schedules for physicians’ fees (Uniform Value Scale, Einheitlicher Bewertungsmaßstab) can be submitted only by persons who possess a qualification in basic psychosomatic care and have successfully completed a course in hypnosis comprising two units of 16 hours each (e4). Most medical and psychological psychotherapists and child and adolescent psychotherapists learn the techniques of hypnotherapy as a supplementary qualification. As a rule hypnotherapists are also trained in other methods of psychotherapy.
Details of the history of hypnosis and assessment of its efficacy prior to the introduction of evidence-based medicine (EBM) are provided in eBox 2.
eBox 2. The history of hypnosis and assessment of its efficacy before the advent of evidence-based medicine (EBM).
Owing to their unconventional approach, hypnosis techniques attracted the attention of both orthodox physicians and the general public at an early stage. The scientific basis of hypnotic procedures was investigated as early as the 18th century.
The theory and techniques of “animal magnetism,” put forward by the Viennese physician Franz Anton Mesmer, are viewed as the precursor of modern hypnosis. Mesmer failed in his attempt to have animal magnetism accredited by the Académie des Sciences in Paris in 1784 (e5). The scientific committee appointed by King Louis XVI refuted the theory of magnetism and attributed Mesmer’s successful treatments to psychological mechanisms, namely the “arousal of powers of imagination and of imitation” (e6). The concept of magnetism persisted, however, and came to be adopted by a number of physicians. The English surgeon James Esdaile (1808–1859), working in India, carried out 345 major operations (amputations of arm, leg, breast, and penis, as well as excision of tumors) using the technique of “mesmerism” and recorded not only good analgesia but also low mortality (e7). The British physician John Elliotson (1791–1868) became professor at the University of London in 1831. Under pressure from the journal Lancet, which rejected his practice of animal magnetism, he resigned his post in 1838. From 1843 to 1856 he published a journal called The Zoist, dedicated exclusively to animal magnetism. However, this technique rapidly receded into the background with the introduction of ether and chloroform anesthesia in 1846/47 (e3).
The Scottish ophthalmologist Braid developed the theory of monoideism, whereby concentration on a single thought by means of optic fixation was held to lead to a neurologically conditioned state of sleep. This physiological explanation of hypnotic phenomena helped “hypnotism” attain recognition by physicians at a time when medicine was developing along scientific lines (e3). In 1891 the British Medical Association (BMA) commissioned a group of physicians to investigate hypnotism. After due appraisal the expert committee concluded that hypnotism was effective in the treatment of pain, sleep disorders, and functional symptoms. At its annual conference in 1892 the BMA unanimously recommended the therapeutic application of hypnosis (e8).
With the increasing importance of evidence-based medicine (EBM) in the 20th and 21st centuries, advocates and practitioners of clinical hypnosis came to see the necessity of controlled trials and synthesis of the findings in systematic reviews. The first German-language systematic review and meta-analysis of the efficacy of hypnosis was published in 2002 (e9). An expert report on evaluation of hypnotherapy as a psychotherapeutic technique according to the criteria of the German Scientific Advisory Committee on Psychotherapy (Wissenschaftlicher Beirat Psychotherapie) (§ 11, Psychotherapy Act) was produced in 2003 (e3). The Scientific Advisory Committee on Psychotherapy concluded that hypnotherapy can be considered a scientifically valid technique for the treatment, in adults, of mental and social factors in somatic diseases and of addiction and abuse (smoking cessation and methadone withdrawal) (ICD-10 F54, F10, F11) (e10).
Evidence for efficacy and safety
Methods
This review was conducted according to the recommendations of the Cochrane Collaboration for systematic reviews of previously published reviews and the recommendations of the Joanna Briggs Institute for umbrella reviews (6).
Systematic survey of the literature
The Cochrane databases CDSR and DARE and PubMed were searched for systematic reviews (SRs) published in the period January 2005 to June 2015. The following search terms were used: “review,” “meta-analysis,” and “hypnosis”. We searched PubMed with “((“hypnosis”[MeSH] OR “hypnosis, dental”[MeSH]) AND (“meta-Analysis” [Publication Type] OR “review” [Publication Type])) OR ((hypnosis OR hypnotherap*) AND (meta-analy* OR metaanaly*))”. Moreover, the reference lists of the SRs identified were inspected for further SRs. With regard to waking suggestions we searched the databases CENTRAL and PubMed for randomized controlled trials (RCTs) using the terms “suggestion” [MeSH] and “hypnotic suggestion”. Finally, for all topics we asked experts in medical hypnosis about SRs.
Inclusion criteria
The following conditions regarding study type, indications, setting, and study population had to be fulfilled:
Study type: We included SRs with meta-analysis of (quasi-)RCTs on hypnosis as intervention for somatic medical indications. In the event of serial publications by the same group of authors we used the most recent publication. We selected inclusion of at least 400 patients in quantitative analysis (meta-analysis) of the study results as a quantitative criterion of robust evidence (7).
Indications: The endpoints of the meta-analysis had to be somatic symptoms (e.g., pain or nausea) or physiological findings (e.g., bleeding time or airway resistance) and/or mental stress during medical treatments and/or cost-related data (e.g., operating time, legth of hospital stay, or drug consumption). We excluded meta-analyses of RCTs on psychiatric and psychotherapeutic indications (e.g., anxiety disorders, depressive disorders, addiction/abuse, or behavioral disorders) and meta-analyses of RCTs on various diseases (e.g., psychosomatic illnesses) in which no subgroup analyses were conducted for individual diseases.
Setting and study population: No restrictions were imposed with regard to setting, age, or country.
Methodological quality
The methodological quality of the meta-analyses was verified using AMSTAR (A Measurement Tool to Assess Systematic Reviews) (8). AMSTAR scores of 0–4 were classified as low, 5–8 as intermediate, and 9–11 as high methodological quality (9).
Data extraction
The following characteristics of the meta-analyses were extracted independently by two of the authors (WH, MH) and discrepancies were resolved by consensus:
The medical indication
The number of RCTs/patients included
The age and sex of the patients
The type and duration of hypnosis
The nature of the control group
The instrument for and results of measurement of methodological quality of the included RCTs
The databases searched and the period covered
The findings regarding efficacy, tolerance, and safety
The authors’ conclusions
The AMSTAR rating.
Given the heterogeneity of diseases and outcome variables, no quantitative data synthesis was planned from the outset.
Results: survey and inclusion
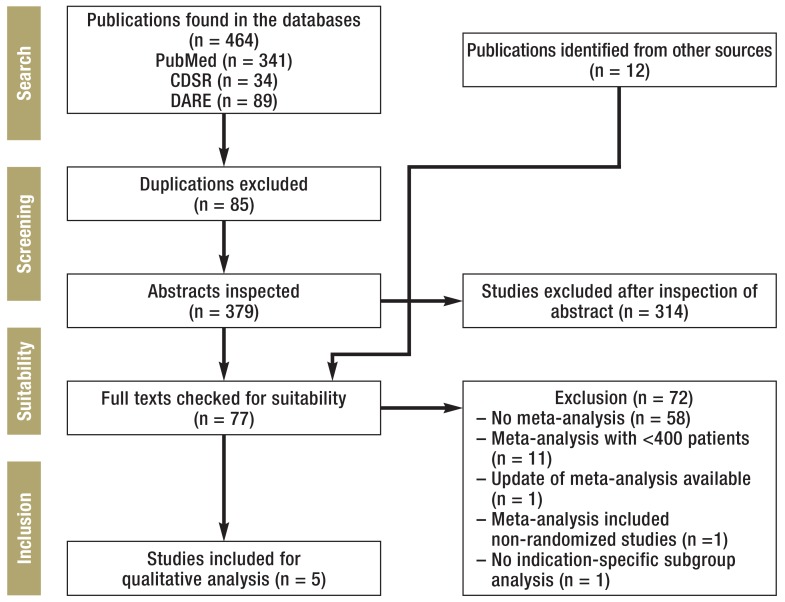
The database survey and the hand search identified 391 publications in total. Seventy-seven full texts were examined in detail (Figure). Fourteen meta-analyses (on topics such as chemotherapy-induced nausea and vomiting, fibromyalgia syndrome, and temporomandibular disorder) were excluded from analysis because they included fewer than 400 patients in their calculations (eTable 1) (e11– e24). Five meta-analyses were included in our qualitative review (10– 14). The methodological quality was high in one meta-analysis, intermediate in three, and low in one (eTable 2). The characteristics of the original articles investigated in these five meta-analyses are outlined in Table 1.
Figure.
Results of the literature survey
eTable 1. List of excluded systematic reviews with meta-analysis*.
| Reference | Medical indication (target group) | Number of RCTs/patients | Reason(s) for exclusion |
|---|---|---|---|
| Adachi et al. 2014 (e11) | Chronic pain (adults) | 6/237 (+ 6 controlled trials/432) | Non-randomized trials were included |
| Bernardy et al. 2011 (e12) | Fibromyalgia syndrome (adults) | 5/191 | N<400 |
| Birnie et al. 2014 (e13) | Pain and stress from injections (children and adolescents) | 7/222 | N<400 |
| Bowker et al. 2014 (e14) | Pain in physically disabling diseases (adults) | 6/237 (+4 non-randomized or only partly randomized trials) | N<400 |
| Enck et al. 2010 (e15) | Irritable bowel syndrome (adults) | 2/40 | N<400; meta-analysis with >400 patients available (12) |
| Flammer et al. 2007 (e16) | Psychosomatic diseases_(children and adults) | 18/916 | Not evaluated for each indication |
| Ford et al. 2014 (e17) | Irritable bowel syndrome (adults) | 5/278 | N<400; meta-analysis with >400 patients available (12) |
| Glazener et al. 2005 (e18) | Bed-wetting (children) | 2/98 | N<400; update of corresponding cochrane group available (e19) |
| Huang et al. 2011 (e19) | Bed-wetting (children) | 3/172 | N<400 |
| Köllner et al. 2012 (e20) | Fibromyalgia syndrome (adults) | 4/102 | N<400 |
| Lee et al. 2014 (e21) | Irritable bowel syndrome (adults) | 7/374 | N<400; meta-analysis with >400 patients available (12) |
| Richardson et al. 2007 (e22) | Nausea and vomiting in chemotherapy for cancer (children and adults) | 6/206 | N<400 |
| Smith et al. 2006 (e23) | Pain during labor and childbirth_(adolescents and adults) | 5/729 | Update of corresponding Cochrane group available (11) |
| Zhang et al. 2015 (e24) | Temporomandibular disorder _(adolescents and adults) | 3/159 | N<400 |
*In alphabetical order RCTs. randomized controlled trials
eTable 2. Assessment of the methodological quality of the meta-analyses of controlled trials of medical hypnosis by means of AMSTAR (8).
| Reference | Was an ’a priori’ design provided?* | Was there duplicate study selection and data extraction? | Was a comprehensive literature search performed? | Was the status of publication _(i.e. grey literature) used as an inclusion criterion? | Was a list of studies (included and excluded) provided? | Were the characteristics of the included studies provided? | Was the scientific quality of the included studies assessed and documented? | Was the scientific quality of the included studies used appropriately in formulating conclusions? | Were the methods used to combine the findings of studies appropriate? | Was the likelihood of publication bias assessed? | Was the conflict of interest included? | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Kekecs et al. 2014 (10) |
No | No | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No | 6 |
| Madden et al. 2012 (11) |
Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | 10 |
| Schäfert et al. 2014 (12) |
No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | No | 8 |
| Schnur et al. 2008 (13) |
No | Yes | No | No | No | Yes | No | No | Yes | Yes | No | 4 |
| Tefikow et al. 2013 (14) |
Yes | Yes | Yes | No | No | Yes | Yes | Yes | Yes | Yes | No | 8 |
*a priori design: protocol. internal review board approval. or research question previously published?
AMSTAR. A Measurement Tool to Assess Systematic Reviews
Table 1. Characteristics of the randomized controlled studies of medical hypnosis included in the meta-analyses*.
| Reference | Medical indication | Number of _studies/patients (sample size range) | Patients’ age and sex | Type and duration of hypnosis | Type of control groups | Methodological quality of the studies |
|---|---|---|---|---|---|---|
| Kekecs et al. 2014 (10) |
Minor (n=11). major (n=14) or unspecified (n=1) surgical interventions |
26/1890 (12–346) |
Children and adults. no further details | 13 studies with hypnosis. 11 studies with therapeutic suggestions. 2 studies with both; 13 studies with live hypnosis and 13 studies with ready-made audio files; no data on duration |
Standard treatment or attention control | Cochrane Risk of Bias Tool: relatively high risk of bias in the studies |
| Madden et al. 2012 (11) |
Pain during labor and childbirth |
7/1213 (38–520) | Adult women in six studies; minors in one study | 6 studies on prenatal classes (3 in groups and 3 in an individual setting) with at least 3 sessions; 1 study with 45 min (live) during contractions |
Standard treatment (i.e.. prenatal instruction) or attention control (supportive treatment) | Cochrane Risk of Bias Tool: 1 study with low and 6 studies with moderate to high risk of bias |
| Schaefert et al. 2014 (12) |
Irritable bowel_ | 8/464 _(24–91) | Adults; range of mean age 36.3–42 years (median 39.8); average proportion of women: 82% [79.3; 86.5] |
Median 8.5 (7–12) live hypnosis sessions over median 12 (5–12) weeks. median treatment duration 7 (2.5–12) h; 7 studies with individual sessions and 1 study with group sessions |
Standard treatment. waiting list or attention control (education. supportive treatment) | Cochrane Risk of Bias Tool: 6 studies with low and 2 studies with high risk of bias |
| Schnur et al. 2008 (13) | Medical interventions |
26/2342 (20–200) | 4.8–70.3 years; _no data on sex _distribution | 7 studies with therapeutic suggestions; 20 studies with live hypnosis. 6 studies with ready-made audio files; no data on frequency and duration of sessions | Standard treatment or attention control | No data |
| Tefikow et al. 2013 (14) |
Medical interventions |
34/2597 (16–347) | Adults; median age 40 years; median proportion of men 40% (experimental groups). 37% (control groups) |
21 studies with live hypnosis 9 studies with ready-made audio files. 4 studies with both; duration of intervention: 3–20 min: 9 studies 21–110 min: 17 studies 110–240 min: 8 studies |
Standard treatment or attention control | Cochrane Risk of Bias Tool: most studies with high or unclear risk of bias |
*The meta-analyses are listed in alphabetical order
Results: efficacy and safety
Hypnosis was superior to standard treatment or attention control (controls) in reduction of emotional stress, (10, 13, 14), pain (10, 14), duration of convalescence, and drug consumption (10) in interventional procedures and operations. The effect size on emotional stress varied: it was slight in one meta-analysis (10), intermediate in another (14), and high in a third (13). The effect size on pain reduction was low (10, 14). The effect sizes of hypnosis in medical interventions were dependent on the methodological quality of the original studies (10, 14).
Gut-directed hypnosis was superior to the treatments used in the control groups with regard to the number of patients with an appropriate reduction of symptoms at the end of treatment (number needed to treat [NNT] 5) and at follow-up 6 months later (NNT 3) (12). Hypnosis was not more effective than standard treatment or attention control for pain during labor and childbirth (11).
Evaluation of the data on safety of hypnosis in two meta-analyses (pain during labor and childbirth, irritable bowel syndrome) (11, 12) revealed no signs of a higher rate of adverse effects than in controls (Table 2).
Table 2. Results of the meta-analyses of randomized controlled trials on medical hypnosis*.
| Reference | Datatabases and period covered by literature survey | Results for efficacy [95 % CI]; number of studies/patients (no data on number of studies/patients per outcome variable) |
Results for tolerability and safety [95% CI]; number of studies/patients |
|---|---|---|---|
| Kekecs et al. 2014 (10) |
PubMed. PsycINFO CINAHL. ProQuest from 1980 to February 2014 |
Postoperative anxiety: SMD 0.40 [0.13; 0.66]; 21/1479 Postoperative pain: SMD 0.25 [0.00; 0.50]; no p-value given; 15/1197 Postoperative consumption of painkillers: SMD 0.16 [−0.16; 0.47]. ns; 12/854 Postoperative nausea: SMD 0.38 [−0.06; 0.81). ns at α -level of p<0.01; 16/647 |
No data |
| Madden et al. 2012 (11) |
Cochrane Pregnancy and Childbirth Group’s Trials Register/Central. PubMed. Embase up to January 2012 | Drug treatment for pain: RR 0.63 [0.39; 1.01]. ns; 6/1032 Spontaneous vaginal delivery: RR1.35 [0.93; 1.96]. ns; 4/472 Satisfaction with pain reduction: RR1.06 [0.94; 1.20]. ns; 1/264 |
Resuscitation of newborns: RR: 0.67 [0.11;3.96]. ns; 1/520 Intensive care of newborns: RR: 0.58 [0.12; 2.89]. ns; 2/347 Intensive care of mothers: RR: 1.47 [0.25; 8.68]. ns; 1/305 Inpatient re-admission of newborns: RR: 1.39 [0.64; 3.02]. ns; 1/267 |
| Schaefert et al. 2014 (12) |
Allied und Complementary Medicine Database Central Register of Controlled Trials. CINAHL. PubMed. PsycINFO. Scopus up to June 2013 (restricted to studies published in journals) |
At end of treatment: Adequate reduction of symptoms: RR 1.69 [1.14; 2.51]; NNT 5 [3; 10]; 5/280 Reduction of global gastrointestinal symptoms: SMD 0.32; [0.08; 0.56]; 6/361 Follow-up (6 months): Adequate reduction of symptoms: RR 2.17 [1.22; 3.87]; NNT 3 [2; 10]; 1/90 Reduction of global gastrointestinal symptoms: SMD 0.57 [–0.26; 1.40]. ns; 2/171 |
Data from five studies: one patient reported dizziness. but continued treatment; one patient discontinued treatment due to a panic attack during hypnosis |
| Schnur et al. 2008 (13) |
PsycINFO and PubMed from beginning to February 2008 (restricted to English-language studies published in journals) | Emotional stress: SMD 0.88 [0.57; 1.19]; 26/2342 |
No data |
| Tefikow et al. 2013 (14) |
Central. PubMed. Web of Science. ProQuest up to September 2011 | Emotional stress: SMD 0.53 [0.37; 0.69) Pain: SMD 0.44; [0.26; 0.61] Drug consumption: SMD 0.38 [0.20; 0.56] Physiological parameters: SMD 0.10 [0.02; 0.18]; ns Duration of convalescence: SMD 0.25 [0.04; 0.46] Operation time: SMD 0.25 [0.12; 0.38]; ns |
No data |
*The meta-analyses are listed in alphabetical order CI. confidence interval; ns. not significant; p. probability; RR. relative risk; SMD. standardized mean difference; NNT. number needed to treat
Discussion of the results can be found in eBox 3.
eBox 3. Discussion of the findings concerning the evidence of the efficacy of medical hypnosis.
Three meta-analyses ((10, (13, (14) of the use of hypnosis in medical interventions fulfilled our criterion of including at least 400 patients. If these meta-analyses were to be based largely on the same original studies, the evidence could be overestimated. Indeed, inspection revealed the following overlapping of the randomized controlled trials (RCTs) included: Kekecs et al. (10) and Tefikow et al. (14): N = 12; Kekecs et al. (10) and Schnur et al. (13): N = 8; Schnur et al. (13) and Tefikow et al. (14): N = 10. At least 50% of the RCTs in each of the three meta-analyses were also included in one or both of the others (Kekecs et al.: 16 of 26; Tefikow et al.: 18 of 34; Schnur et al.: 13 of 26). Nevertheless, each of the three covered an appreciable number of original studies that were not featured in the others. This can be explained by the variation in focus: Kekecs et al. (10) and Tefikow et al. (14) restricted themselves to studies on adults, while Schnur et al. (13) also included children. Whereas Schnur et al. (13) confined themselves to “emotional stress” as endpoint, Kekecs et al. (10) and Tefikow et al. (14) each calculated several effect sizes for several outcome variables, with Kekecs et al. (10) concentrating solely on postoperative endpoints. Therefore, since differentiated conclusions can certainly be drawn, we chose to present the results of all three meta-analyses of medical hypnosis in diagnostic, interventional, and surgical procedures.
Recommendations on the use of medical hypnosis in medical procedures are limited, however, by the poor methodological quality of many original studies. Moreover, on statistical criteria the effect strengths were mostly low. Blinding of the therapists and the patients is usually not possible (intervention bias) in RCTs with hypnosis (and other psychological techniques). In fact, at least in some studies in which audio files were used for hypnosis the medical personnel or diagnosticians were blinded, which is associated with conservative effect sizes (10, 14). Therefore, using the Cochrane Risk of Bias Tool the danger of bias is higher in RCTs that use psychological techniques than in RCTs where medications are administered. Two of the three systematic reviews of hypnosis in medical procedures point to low or uncertain quality of the existing RCTs and recommend that further studies with high-quality methodology should be carried out (10, 14). Because the original studies reported only average data and no response rates (e.g., the proportion of patients with only slight postoperative pain or no postoperative nausea), the meta-analyses could not calculate the number needed to treat for an additional benefit (NNTB). The clinical benefit of medical hypnosis in interventions is therefore difficult to estimate.
The quality of the data is better for irritable bowel syndrome: the risk of bias was low in most of the studies included (12). Response rates with a clinically meaningful benefit (NNT 5 and 3 respectively) were computed for adequate symptom reduction at the end of treatment and at 6-month follow-up. With regard to these NNTs, it should be remembered that most of the RCTs included patients who had shown insufficient reduction of symptoms in response to an established regimen of medication (12).
Applications of hypnosis in daily clinical practice
Preparation and performance of interventions
Anesthesia and surgery: The use of hypnosis instead of local anesthesia in dental surgery (e25) and in place of anesthesia for more extensive surgery (cholecystectomy, aortocoronary bypass operation) has been described in case reports (e26). However, hypnosis is being routinely used as a complement rather than an alternative to modern, safe techniques of anesthesia, primarily to minimize anxiety and stress. Hypnosis has been shown to reduce pain, anxiety, and the consumption of analgesics and sedatives to a statistically significant extent in patients undergoing operations under local or regional anesthesia (e27, e28).
An example of the efficacy of hypnotic communication—even without formal trance induction—is its application in waking craniotomies, as performed for instance for removal of a brain tumor close to the speech area or for deep brain stimulation. In these procedures the patient receives regional anesthesia of the head and remains awake for the whole duration of the brain surgery for purposes of neurological testing, with no need for sedation and additional analgesia. Dissociation to an inner place of tranquility away from the operating room plays an important part, as does the reinterpretation of sensory perceptions (e29).
Some German hospitals offer live or audio file–aided hypnosis as a complement to general and regional anesthesia.
Gastroenterology: With the aid of hypnosis—e.g., self-hypnosis or hypnosis by means of audio files— diagnostic esophagogastroduodenoscopy procedures can be carried out without sedation (e30). The use of audio files is also efficacious in irritable bowel syndrome (e31). These files can be given to patients with irritable bowel syndrome by their primary care physician or internist, and the progress with regard to symptom control can be discussed with the patients in the framework of basic psychosomatic care (e32). This aproach can greatly facilitate the clinical application of hypnosis. Gastroenterology departments in Great Britain (e33), Austria (e34), and the USA (e35) have integrated psychosocial services that offer live and audio file–aided hypnosis to patients with functional gastrointestinal disorders who do not respond well to conventional medicinal treatment (see eBox 1 for more on gut-directed hypnosis). Some office-based gastroenterologists in Germany offer hypnosis as an alternative to sedation in esophagogastroduodenoscopy.
Dentistry: The German Dental Hypnosis Society (Deutsche Gesellschaft für Zahnärztliche Hypnose) has trained around 3000 dentists in hypnosis. The society’s website lists over 600 dentists who offer this service to their patients. The indications for which hypnosis is available are pronounced fear of dental treatment, gag reflex, intolerance of local anesthetics, and craniomandibular dysfunction. Hypnosis in the following forms is offered (e25):
The use of CDs developed specially for dental treatment (e.g. “Beim Zahnarzt ohne Spritze [Dental surgery without injection]”). At the beginning of the treatment session track 1 is played repeatedly over headphones, and at the end of treatment the patient is woken by track 2.
Delegation of the hypnosis to a trained member of staff (hypnosis assistant). In this case the dentist must also be trained in hypnosis, because he/she is responsible for the patient’s welfare and must be able to deal with the rare cases of adverse reaction to hypnosis.
Induction of hypnosis by the dentist him-/herself. This takes 2 to 5 min for relaxation prior to an injection, about 10 min for treatment without local anesthesia.
It is advantageous to combine nitrous oxide and hypnosis, because the gas has an anxiolytic effect and increases suggestibility.
Some dentists who concentrate on treatment of patients with anxiety or craniomandibular dysfunction draw on the services of an external hypnotist.
Live hypnosis versus audio file–aided hypnosis
A meta-analysis of hypnosis in medical interventions demonstrated no significant differences in efficacy between live hypnosis and suggestion by means of audio files (14). Another meta-analysis by a different group of authors concluded that only live hypnosis, which is more apt to provide the context of a personal relationship, significantly reduced postoperative anxiety and pain. Both live and audio file–aided hypnosis significantly decreased postoperative nausea and consumption of analgesics (10).
Waking suggestions in doctor–patient communication
The German Medical Assembly 2015 spoke out in favor of strengthening physicians’ communicative competence (15). In our opinion, together with authentic and empathetic interaction (16), effective doctor–patient communication has to include avoidance of negative suggestions (16– 19) and targeted use of positive waking suggestions (18). In this context, communication could be improved by applying basic principles of hypnotherapy such as employment of indirect suggestions and the establishment of a trusting doctor–patient relationship (rapport). Three RCTs on invasive radiological procedures found that positive suggestions and empathy, with and without techniques of self-hypnosis, were superior to the standard treatment in reducing pain and anxiety and in decreasing consumption of analgesics (20– 22). In two RCTs, neutral or positive instructions before blood sampling (“I’m going to start taking the blood sample now”) or induction of local anesthesia led to lower levels of pain than (unintended) negative suggestions (“this may hurt a bit”) (23, 24). A RCT in a hospital emergency room found that the pain-relieving effect of intramuscular diclofenac was not reinforced by a waking suggestion (“this is a powerful painkiller”) in patients with acute headache (25) (eTable 3). Therapeutic waking suggestions can be used by all physicians in a medical context (see Table 3 for examples).
eTable 3. Overview of randomized controlled trials on the effect of waking suggestions in medical treatment procedures*.
| Reference | Type of medical treatment | Type of suggestion Number of patients | Control intervention Number of patients | Result |
|---|---|---|---|---|
| Lang et al. 2000 (20) |
Percutaneous vascular intervention | Structured attention control―; N=80 Structured attention control plus self-relaxation and self-hypnosis; N = 82 |
Standard treatment; N=79 | Increase in pain: significantly greater for standard treatment (mean 0.09 pain score/15 min) and attention control (mean 0.04/15 min) than for hypnosis (no increase) |
| Drug consumption: significantly higher increase in standard treatment group (mean 1.9 units) than in attention control group (mean 0.07) and hypnosis group (mean 0.11) | ||||
| Reduction of anxiety: no significant difference between attention control (mean –0.07) und hypnosis (mean –0.11); significantly lower with standard treatment (mean 0.04) | ||||
| Hemodynamic instability: significantly lower for hypnosis (1.2%) than for attention control (12.5%) and standard treatment (15.2%) | ||||
| Duration of intervention: significantly shorter for hypnosis (mean 61 min) and attention control (mean 67 min) than for standard treatment (mean 78 min) | ||||
| Lang et al. 2006 (21) |
Breast biopsy | Structured attention control**; N=82 Structured attention control plus self-relaxation and self-hypnosis; N = 78 |
Standard treatment; N=76 | Increase in pain: significantly greater for standard treatment (mean 0.53) than for attention control (mean 0.37) and hypnosis (mean 0.34) |
| Drug consumption: significantly higher increase in standard treatment group (mean 0.18) than in attention control group (mean −0.04) and hypnosis group (mean –0.27) | ||||
| Reduction of anxiety: significantly less reduction in standard treatment group (mean 0.18) than in attention control group (mean –0.04) and hypnosis group (mean –0.27) | ||||
| Complications: no significant differences among standard treatment (8.9%). attention control (13.8%). and hypnosis (3.7%) | ||||
| Duration of intervention: no significant differences among hypnosis (mean 39 min). attention control (mean 43 min). and standard treatment (mean 46 min) | ||||
| Lang et al. 2008 (22) |
Radiofrequency ablation or embolization of carcinomas | Structured attention control**; N=65 Structured attention control plus self-relaxation and self-hypnosis; N = 66 |
Standard treatment; N=70 | Increase in pain: significantly greater for standard treatment (median 2.5 units) and attention control (median 2.5 units) than for hypnosis (median 0 units) |
| Reduction of anxiety: no significant differences among standard treatment group (median 2 units). attention control group (median 2 units). and hypnosis group (median 1 unit) | ||||
| Complications: significantly higher rates in attention control group (48%) compared to hypnosis group (12%) and standard treatment group (26%) | ||||
| Duration of intervention: no significant differences among hypnosis (median 110 min). attention control (median 120 min). and standard treatment (median 110 min) | ||||
| Ott et al. 2012 (23) |
Sampling of venous blood | “I’m going to start taking the blood sample now” N=50 | “This will hurt a bit” N=50 | Mean pain intensity. as measured on an 11-point (0–10) numeric rating scale (NRS) was 2.7 in the “This will hurt” group compared with 1.6 in the “I’m going to” group (p = 0.001). 58 % of the probands in the “This will hurt” group but only two probands (4.2 %) in the “I’m going to” group rated the pain intensity of the injection at ≥ 1 on the NRS. the threshold value for mild to moderate pain (p<0.001). |
| Oktay et al. 2014 (25) |
Acute headache | “This drug is a powerful pain killer for your headache. Its analgesic effect peaks at about 20 to 30 minutes. We are expecting that your headache will resolve in 45 minutes” N=50 (group 1) | “A nurse is going to administer you a pain killer called … by intramuscular injection” N=50 (group 2) “If your headache does not resolve in 45 minutes. we can administer you a more potent pain killer” N=53 (group 3) | Pain reduction on a 0–100 visual analog scale 45 min after injection (p=0.49): group 1: 43 ± 30 group 2: 39 ± 29 group 3: 36 ± 24 |
| Varelmann et al. 2010 (24) |
Local anesthesia before creation of access for peridural or spinal anesthesia in pregnant women before delivery | “We are now going to give you a local anesthetic so that it’s comfortable for you when we perform the epidural spinal anesthesia” N=33 | “You will now feel a prick and a burning sensation in your back as though you have been stung by a bee; that’s the worst part of the whole procedure” N=32 | Pain was rated significantly stronger by patients who received the second instruction (median pain intensity 5 versus 3 on an 11-point scale). |
*Trials listed in alphabetical order
**Agreement with the patient’s verbal and non-verbal communication patterns; attentive listening; reinforcement of feeling of autonomy (“Let us know at any time what we can do for you”); swift action in response to the patient’s wishes; avoidance of negative suggestions (“How bad is your pain? “You will now feel a prick and a burning sensation“); positive suggestions (focus on sensations of fullness. coolness. warmth during painful stimuli) Significant. p<0.05
Table 3. Examples of positive waking suggestions at premedication and before induction of anesthesia (modified from [18. 19]).
| Positive statements instead of negations | “Everything will be fine” “We’ll do this together” rather than “You don’t need to worry.” |
| Use of positive suggestions (safety. support. well-being) | “We’ll keep a close eye on you until you’ve completely recovered from the operation.” |
| Combine explanations with positive suggestions | “We’re attaching a blood pressure cuff and ECG leads so we can take good care of you.” |
| Combine information about procedures with positive suggestions | “After the operation you can stay in the recovery room until you wake up naturally. and when you feel well enough we’ll take you back to your room.” |
| Combine references to the patient’s autonomy with positive suggestions | “You can help us to increase the safety of the anesthesia by not eating anything for 12 hours before the operation.” |
| Combine information about possible complications with positive suggestions | “Please tell us straightaway if you get a headache after the spinal anesthesia. We have good medication for treating this kind of headache.” |
Psychosomatic medicine
Examples of the application of medical hypnosis by psychotherapists in somatic medicine are given in the Box.
Box. Potential applications of medical hypnosis in daily clinical practice (case reports and/or case series).
-
All patient-related areas: waking suggestions
-
Anesthesia
-
Gastroenterology
-
Dentistry
-
Psychosomatic medicine
Psychotherapy for pain management: chronic non-cancer and cancer pain (e42, e43)
Component of psychotherapeutic measures in hospital consultation and advisory services, e.g., in gynecology (e44), palliative medicine (e45), and transplant surgery (e46)
Dentistry: fear of the dentist, strong gag reflex, fear of dental materials and injections, allergy to local anesthetics, intolerance of implants, parafunctions, temporomandibular dysfunction) (e40, e47)
Conclusion
Hypnosis techniques have long been used—and their efficacy assessed—in somatic medicine. The modern evidence-based indications (emotional stress associated with medical interventions, functional disorders such as irritable bowel syndrome) correspond with the applications of mesmerism in medicine in the middle of the 19th century (e5). Learning techniques of self-hypnosis empowers patients to participate in their own treatment and grants them independence. Hypnosis techniques such as the building of a trusting relationship with the patient and therapeutic waking suggestions can considerably reinforce the communicative competence of physicians (15).
Key Messages.
Medical hypnosis comprises the use of hypnotic techniques, with or without induction of a trance.
Robust evidence (from meta-analysis of randomized controlled trials including at least 400 patients) of the efficacy of medical hypnosis exists for reduction of pain and emotional stress, duration of interventions, drug consumption during medical interventions, and reduction of irritable bowel symptoms.
The preparation and conduct of medical interventions can be facilitated by hypnosis.
Waking suggestions, taking advantage of patients’ heightened suggestibility, have a pain-reducing effect in diagnostic and therapeutic interventions.
Hypnotic techniques such as the creation of a trusting relationship with the patient and therapeutic waking suggestions can be used in daily clinical practice by all physicians and dentists and can form an effective component of overall doctor–patient communication.
Acknowledgments
Translated from the original German by David Roseveare
Footnotes
Conflict of interest statement
Dr. Häuser receives royalties from the sale of CDs on medical hypnosis in irritable bowel syndrome and fibromyalgia syndrome from Hypnos Verlag. He is an instructor for hypnosis of the German Society for Medical Hypnosis and Autogenous Training (Deutsche Gesellschaft für Ärztliche Hypnose und Autogenes Training).
Dr. phil. Dipl.-Psych. Hagl has received honoraria for authorship or co-authorship of yearly reviews of hypnosis research from the Milton H. Erickson Society for Clinical Hypnosis (Milton H. Erickson Gesellschaft für Klinische Hypnose).
Dr. Schmierer has received an honorarium for authorship or co-authorship from Quintessenzverlag (dental hypnosis).
Prof. Hansen is a member of the scientific advisory board of the Milton H. Erickson Society for Clinical Hypnosis (Milton H. Erickson Gesellschaft für klinische Hypnose).
References
- 1.British Medical Association. Medical use of hypnotism: report of a subcommittee appointed by the Psychological Medicine Group Committee of the British Medical Association. BMJ Suppl. 1955;23:190–193. [Google Scholar]
- 2.Council on Mental Health. Medical use of hypnosis. JAMA. 1958;168:186–189. [Google Scholar]
- 3.Baethge C. Evidenzbasierte Medizin. In der Versorgung angekommen, aber noch nicht heimisch. Dtsch Arztebl. 2014;111:1630–1640. doi: 10.1016/j.zefq.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 4.Peter B. Hypnosis. In: Wright DE, editor. International encyclopedia of the social and behavioral sciences. 2nd edition. Volume 11. Oxford: Elsevier; 2015. pp. 458–464. [Google Scholar]
- 5.Higgins JPT, Green S, editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] The Cochrane Collaboration. 2011. www.cochrane-handbook.org (last accessed on 1 August 2015)
- 6.Aromataris E, Fernandez R, Godfrey C, et al. Methodology for jbi umbrella reviews. The Joanna Briggs Institute Reviewers Manual. 2014 http://arrow.monash.edu.au/hdl/1959.1/1131560 (last accessed on 1 June 2015) [Google Scholar]
- 7.Andrew Moore R, Eccleston C, Derry S, et al. ACTINPAIN Writing Group of the IASP Special Interest Group on Systematic Reviews in Pain Relief; Cochrane Pain, Palliative and Supportive Care Systematic Review Group Editors: „Evidence“ in chronic pain-establishing best practice in the reporting of systematic reviews. Pain. 2010;15:386–389. doi: 10.1016/j.pain.2010.05.011. [DOI] [PubMed] [Google Scholar]
- 8.Shea BJ, Hamel C, Wells GA, et al. AMSTAR is a reliable and valid measurement tool to assess the methodological quality of systematic reviews. J Clin Epidemiol. 2009;62:1013–1020. doi: 10.1016/j.jclinepi.2008.10.009. [DOI] [PubMed] [Google Scholar]
- 9.Seo HJ, Kim KU. Quality assessment of systematic reviews or meta-analyses of nursing interventions conducted by Korean reviewers. BMC Med Res Methodol. 2012;12 doi: 10.1186/1471-2288-12-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kekecs Z, Nagy T, Varga K. The effectiveness of suggestive techniques in reducing postoperative side effects: a meta-analysis of randomized controlled trials. Anesth Analg. 2014;119:1407–1419. doi: 10.1213/ANE.0000000000000466. [DOI] [PubMed] [Google Scholar]
- 11.Madden K, Middleton P, Cyna AM, Matthewson M, Jones L. Hypnosis for pain management during labour and childbirth. Cochrane Database Syst Rev. 2012;11 doi: 10.1002/14651858.CD009356.pub2. CD009356. [DOI] [PubMed] [Google Scholar]
- 12.Schaefert R, Klose P, Moser G, Häuser W. Efficacy, tolerability, and safety of hypnosis in adult irritable bowel syndrome: systematic review and meta-analysis. Psychosom Med. 2014;76:389–398. doi: 10.1097/PSY.0000000000000039. [DOI] [PubMed] [Google Scholar]
- 13.Schnur JB, Kafer I, Marcus C, Montgomery GH. Hypnosis to manage distress related to medical procedures: a meta-analysis. Contemp Hypn. 2008;25:114–128. doi: 10.1002/ch.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tefikow S, Barth J, Maichrowitz S, Beelmann A, Strauss B, Rosendahl J. Efficacy of hypnosis in adults undergoing surgery or medical procedures: a meta-analysis of randomized controlled trials. Clin Psychol Rev. 2013;33:623–636. doi: 10.1016/j.cpr.2013.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Klinkhammer G. Förderung der ärztlichen Kommunikationskompetenz gefordert. Dtsch Arztebl. 2015 www.aerzteblatt.de/nachrichten/62808/Aerztetag-Foerderung- der-aerztlichen-Kommunikationskompetenz-gefordert (last accessed on 1 July 2015) [Google Scholar]
- 16.Bingel U Placebo Competence Team. Avoiding nocebo effects to optimize treatment outcome. JAMA. 2014;312:693–4. doi: 10.1001/jama.2014.8342. [DOI] [PubMed] [Google Scholar]
- 17.Häuser W, Hansen E, Enck P. Nocebo phenomena in medicine: their relevance in everyday clinical practice. Dtsch Arztebl Int. 2012;109:459–465. doi: 10.3238/arztebl.2012.0459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hansen E, Bejenke C. [Negative and positive suggestions in anaesthesia: Improved communication with anxious surgical patients] Anaesthesist. 2010;59:199–202. doi: 10.1007/s00101-010-1679-9. 204-6, 208-9. [DOI] [PubMed] [Google Scholar]
- 19.Seemann M, Zech N, Graf BM, Hansen E. [The premedication visit—suggestions for a patient-friendly design] Anasthesiol Intensivmed Notfallmed Schmerzther. 2015;50:142–146. doi: 10.1055/s-0040-100082. [DOI] [PubMed] [Google Scholar]
- 20.Lang EV, Benotsch EG, Fick LJ, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures: a randomised trial. Lancet. 2000;355:1486–1490. doi: 10.1016/S0140-6736(00)02162-0. [DOI] [PubMed] [Google Scholar]
- 21.Lang EV, Berbaum KS, Faintuch S, et al. Adjunctive self-hypnotic relaxation for outpatient medical procedures: a prospective randomized trial with women undergoing large core breast biopsy. Pain. 2006;126:155–164. doi: 10.1016/j.pain.2006.06.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lang EV, Berbaum KS, Pauker SG, et al. Beneficial effects of hypnosis and adverse effects of empathic attention during percutaneous tumor treatment: when being nice does not suffice. J Vasc Interv Radiol. 2008;19:897–905. doi: 10.1016/j.jvir.2008.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ott J, Aust S, Nouri K, Promberger R. An everyday phrase may harm your patients. Clin J Pain. 2012;28:324–328. doi: 10.1097/AJP.0b013e3182321cc3. [DOI] [PubMed] [Google Scholar]
- 24.Varelmann D, Pancaro C, Cappiello EC, Camann WR. Nocebo-induced hyperalgesia during local anesthetic injection. Anesth Analg. 2010;110:868–870. doi: 10.1213/ANE.0b013e3181cc5727. [DOI] [PubMed] [Google Scholar]
- 25.Oktay C, Eken C, Goksu E, Dora B. Contribution of verbal suggestion to the therapeutic efficacy of an analgesic agent for acute primary headache. Cephalalgia. 2015;35:579–584. doi: 10.1177/0333102414553821. [DOI] [PubMed] [Google Scholar]
- e1.Barabasz AF. Whither spontaneous hypnosis: a critical issue for practitioners and researchers. Am J Clin Hypn. 2005;48:91–97. doi: 10.1080/00029157.2005.10401501. [DOI] [PubMed] [Google Scholar]
- e2.Cheek DB. Importance of recognizing that surgical patients behave as though hypnotized. Am J Clin Hypn. 1962;4:227–231. doi: 10.1080/00029157.1962.10401905. [DOI] [PubMed] [Google Scholar]
- e3.Revenstorf D. Expertise zur Beurteilung der wissenschaftlichen Evidenz des Psychotherapieverfahrens Hypnotherapie entsprechend den Kriterien des Wissenschaftlichen Beirats Psychotherapie. Hypnose-ZHH. 2006 1:7–164. [Google Scholar]
- e4.Fritzsche K, Geigges W, Richter H, Wirsching M, editors. 1st edition. Heidelberg: Springer; 2003. Psychosomatische Grundversorgung. [Google Scholar]
- e5.Peter B. Zur Geschichte der Hypnose in Deutschland. Hypnose und Kognition. 2000;17:47–106. [Google Scholar]
- e6.Bailly JS. Exposé zu den Erfahrungen, die zur Untersuchung des animalischen Magnetismus gesammelt worden sind. HyKog. 1784/2000;17:107–14. [Google Scholar]
- e7.Esdaile J. London: Longman, Borwon, Green and Longmans; 1846. Mesmerism in India, and its practical application in surgery and medicine. [Google Scholar]
- e8.Robertson D. BMA Report on Hypnosis. www.rebhp.org/articles1892.pdf. (last accessed on 1 July 2015) [Google Scholar]
- e9.Bongartz W, Flammer E, Schwonke R. Die Effektivität der Hypnose. Eine meta-analytische Studie. Psychotherapeut. 2002;47:67–76. [Google Scholar]
- e10.Wissenschaftliche Beirat Psychotherapie. Gutachten zur wissenschaftlichen Anerkennung der Hypnotherapie. Wissenschaftlicher Beirat Psychotherapie. www.wbpsychotherapie.de/page.asp?his=0.113.122.123. 2006. (last accessed on 1 July 2015)
- e11.Adachi T, Fujino H, Nakae A, Mashimo T, Sasaki J. A meta-analysis of hypnosis for chronic pain problems: a comparison between hypnosis, standard care, and other psychological interventions. Int J Clin Exp Hypn. 2014;62:1–28. doi: 10.1080/00207144.2013.841471. [DOI] [PubMed] [Google Scholar]
- e12.Bernardy K, Füber N, Klose P, Häuser W. Efficacy of hypnosis/guided imagery in fibromyalgia syndrome-a systematic review and meta-analysis of controlled trials. BMC Musculoskelet Disord. 2011;12 doi: 10.1186/1471-2474-12-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e13.Birnie KA, Noel M, Parker JA, et al. Systematic review and meta-analysis of distraction and hypnosis for needle-related pain and distress in children and adolescents. J Pediatr Psychol. 2014;39:783–808. doi: 10.1093/jpepsy/jsu029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e14.Bowker E, Dorstyn D. Hypnotherapy for disability-related pain: A meta-analysis. J Health Psychol. 2014 doi: 10.1177/1359105314530452. epub ahead of print. [DOI] [PubMed] [Google Scholar]
- e15.Enck P, Junne F, Klosterhalfen S, Zipfel S, Martens U. Therapy options in irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2010;22:1402–1411. doi: 10.1097/MEG.0b013e3283405a17. [DOI] [PubMed] [Google Scholar]
- e16.Flammer E, Alladin A. The efficacy of hypnotherapy in the treatment of psychosomatic disorders: meta-analytical evidence. Int J Clin Exp Hypn. 2007;55:251–274. doi: 10.1080/00207140701338696. [DOI] [PubMed] [Google Scholar]
- e17.Ford AC, Quigley EM, Lacy BE, et al. Effect of antidepressants and psychological therapies, including hypnotherapy, in irritable bowel syndrome: systematic review and meta-analysis. Am J Gastroenterol. 2014;109:1350–1365. doi: 10.1038/ajg.2014.148. [DOI] [PubMed] [Google Scholar]
- e18.Glazener CM, Evans JH, Cheuk DK. Complementary and miscellaneous interventions for nocturnal enuresis in children. Cochrane Database Syst Rev. 2005;18 doi: 10.1002/14651858.CD005230. CD005230. [DOI] [PubMed] [Google Scholar]
- e19.Huang T, Shu X, Huang YS, Cheuk DK. Complementary and miscellaneous interventions for nocturnal enuresis in children. Cochrane Database Syst Rev. 2011;12 doi: 10.1002/14651858.CD005230.pub2. CD005230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e20.Köllner V, Häuser W, Klimczyk K, et al. Arbeitsgemeinschaft der Wissenschaftlichen Medizinischen Fachgesellschaften: [Psychotherapy for patients with fibromyalgia syndrome. Systematic review, meta-analysis and guideline]. Schmerz. 2012;26:291–296. doi: 10.1007/s00482-012-1179-8. [DOI] [PubMed] [Google Scholar]
- e21.Lee HH, Choi YY, Choi MG. The efficacy of hypnotherapy in the treatment of irritable bowel syndrome: A systematic review and meta-analysis. J Neurogastroenterol Motil. 2014;20:152–162. doi: 10.5056/jnm.2014.20.2.152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e22.Richardson J, Smith JE, McCall G, Richardson A, Pilkington K, Kirsch I. Hypnosis for nausea and vomiting in cancer chemotherapy: a systematic review of the research evidence. Eur J Cancer Care. 2007;16:402–412. doi: 10.1111/j.1365-2354.2006.00736.x. [DOI] [PubMed] [Google Scholar]
- e23.Smith CA, Collins CT, Cyna AM, Crowther CA. Complementary and alternative therapies for pain management in labour. Cochrane Database Syst Rev. 2006;18 doi: 10.1002/14651858.CD003521.pub2. CD003521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e24.Zhang Y, Montoya L, Ebrahim S, et al. Hypnosis/relaxation therapy for temporomandibular disorders: a systematic review and meta-analysis of randomized controlled trials. J Oral Facial Pain Headache. 2015;29:115–125. doi: 10.11607/ofph.1330. [DOI] [PubMed] [Google Scholar]
- e25.Schmierer A. Hypnose in der Zahnheilkunde: Geschichte, Organisation, Methoden, Praxis. Hypnose-ZHH. 2010;5:69–94. [Google Scholar]
- e26.Faymonville ME. Hypnose in der Anästhesie. Hypnose-ZHH. 2010;5:111–120. [Google Scholar]
- e27.Faymonville ME, Mambourg PH, Joris J, et al. Psychological approaches during conscious sedation. Hypnosis versus stress reducing strategies: a prospective randomized study. Pain. 1997;7:361–367. doi: 10.1016/S0304-3959(97)00122-X. [DOI] [PubMed] [Google Scholar]
- e28.Faymonville ME, Fissette J, Mambourg PH, Roediger L, Joris J, Lamy M. Hypnosis as adjunct therapy in conscious sedation for plastic surgery. Reg Anesth. 1995;20:145–151. [PubMed] [Google Scholar]
- e29.Hansen E, Seemann M, Zech N, Doenitz C, Luerding R, Brawanski A. Awake craniotomies without any sedation: the awake-awake-awake technique. Acta Neurochir (Wien) 2013;155:1417–1424. doi: 10.1007/s00701-013-1801-2. [DOI] [PubMed] [Google Scholar]
- e30.Häuser W. Hypnose in der Gastroenterologie. Hypnose und Kognition. 1997;14:25–32. [Google Scholar]
- e31.Rutten JM, Vlieger AM, Frankenhuis C, et al. Gut-directed hypnotherapy in children with irritable bowel syndrome or functional abdominal pain (syndrome): a randomized controlled trial on self exercises at home using CD versus individual therapy by qualified therapists. BMC Pediatr. 2014;14 doi: 10.1186/1471-2431-14-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e32.Häuser W. Hypnose in der Therapie des Reizdarmsyndroms. Psychomed. 2002;14:227–232. [Google Scholar]
- e33.Gonsalkorale WM, Houghton LA, Whorwell PJ. Hypnotherapy in irritable bowel syndrome: a large-scale audit of a clinical service with examination of factors influencing responsiveness. Am J Gastroenterol. 2002;97:954–961. doi: 10.1111/j.1572-0241.2002.05615.x. [DOI] [PubMed] [Google Scholar]
- e34.Moser G, Trägner S, Gajowniczek EE, et al. Long-term success of GUT-directed group hypnosis for patients with refractory irritable bowel syndrome: a randomized controlled trial. Am J Gastroenterol. 2013;108:602–609. doi: 10.1038/ajg.2013.19. [DOI] [PubMed] [Google Scholar]
- e35.Kinsinger SW, Ballou S, Keefer L. Snapshot of an integrated psychosocial gastroenterology service. World J Gastroenterol. 2015;21:1893–1899. doi: 10.3748/wjg.v21.i6.1893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e36.Colloca L, Finniss D. Nocebo effects, patient-clinician communication, and therapeutic outcomes. JAMA. 2012;307:567–568. doi: 10.1001/jama.2012.115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- e37.Iserson KV. An hypnotic suggestion: review of hypnosis for clinical emergency care. J Emerg Med. 2014;46:588–596. doi: 10.1016/j.jemermed.2013.09.024. [DOI] [PubMed] [Google Scholar]
- e38.Zech N, Seemann M, Signer-Fischer S, Hansen E. [Communication with children: practical hints and tools for the anesthesiology routine] Anaesthesist. 2015;64:197–207. doi: 10.1007/s00101-015-0001-2. [DOI] [PubMed] [Google Scholar]
- e39.Seemann M, Zech N, Graf B, Hansen E. [Anesthesiological management of awake craniotomy: Asleep-awake-asleep technique or without sedation] Anaesthesist. 2015;64:128–136. doi: 10.1007/s00101-014-2396-6. [DOI] [PubMed] [Google Scholar]
- e40.Eitner S, Sokol B, Wichmann M, Bauer J, Engels D. Clinical use of a novel audio pillow with recorded hypnotherapy instructions and music for anxiolysis during dental implant surgery: a prospective study. Int J Clin Exp Hypn. 2011;59:180–197. doi: 10.1080/00207144.2011.546196. [DOI] [PubMed] [Google Scholar]
- e41.Hermes D, Truebger D, Hakim SG, Sieg P. Tape recorded hypnosis in oral and maxillofacial surgery-basics and first clinical experience. J Craniomaxillofac Surg. 2005;33:123–129. doi: 10.1016/j.jcms.2004.06.009. [DOI] [PubMed] [Google Scholar]
- e42.Ebell H, Beyer A. Stuttgart, New York: Thieme; 2001. Die Schmerzbehandlung von Tumorpatienten. [Google Scholar]
- e43.Ebell H. Hypnose und Selbsthypnose in der Behandlung von Patienten, die an chronischen Schmerzen leiden. Hypnose und Kognition. 2002;19:27–38. [Google Scholar]
- e44.Tschugguel W, Tschuguell S. Hypnose bei Patientinnen mit gynäkologischen Symptomen. Hypnose-ZHH. 2010;5:121–144. [Google Scholar]
- e45.Schulze W. Hypnose in der Palliativmedizin. Hypnose-ZHH. 2010;5:145–161. [Google Scholar]
- e46.Tigges-Limmer K, Gummert J. Hypnotherapeutische Interventionen in der Herztransplantation. Hypnose-ZHH. 2010;5:179–197. [Google Scholar]
- e47.Schmierer A, Schmierer G. Hypnose in der Zahnarztpraxis - eine sichere und schnelle Möglichkeit zum Angstabbau. DZzH. 2004;3:31–51. [Google Scholar]