ABSTRACT
Background: Project ECHO (Extension for Community Healthcare Outcomes) trains and mentors primary care providers (PCPs) in the care of patients with complex conditions. ECHO is a distance education model that connects specialists with numerous PCPs via simultaneous video link for the purpose of facilitating case-based learning. This article describes a teleECHO clinic based at the University of New Mexico Health Sciences Center that is focused on treatment of substance use disorders (SUDs) and behavioral health disorders. Methods: Since 2005, specialists in treatment of SUDs and behavioral health disorders at Project ECHO have offered a weekly 2-hour Integrated Addictions and Psychiatry (IAP) TeleECHO Clinic focused on supporting PCP evaluation and treatment of SUDs and behavioral health disorders. We tabulate the number of teleECHO clinic sessions, participants, and CME/CEU (continuing medical education/continuing education unit) credits provided annually. This teleECHO clinic has also been used to recruit physicians to participate in DATA-2000 buprenorphine waiver trainings. Using a database of the practice location of physicians who received the buprenorphine waiver since 2002, the number of waivered physicians per capita in US states was calculated. The increase in waivered physicians practicing in underserved areas in New Mexico was evaluated and compared with the rest of the United States. Results: Since 2008, approximately 950 patient cases have been presented during the teleECHO clinic, and more than 9000 hours of CME/CEU have been awarded. Opioids are the substances discussed most commonly (31%), followed by alcohol (21%) and cannabis (12%). New Mexico is near the top among US states in DATA-2000 buprenorphine-waivered physicians per capita, and it has had much more rapid growth in waivered physicians practicing in traditionally underserved areas compared with the rest of the United States since the initiation of the teleECHO clinic focused on SUDs in 2005. Conclusion: The ECHO model provides an opportunity to promote expansion of access to treatment for opioid use disorder and other SUDs, particularly in underserved areas.
KEYWORDS: Buprenorphine, distance, education, opioid-related disorders, substance-related disorders, vulnerable populations
Introduction
A model of health care education and mentoring in New Mexico (NM), known as Project ECHO (Extension for Community Healthcare Outcomes), is attempting to address the inadequate supply of culturally appropriate and accessible specialty care in rural and traditionally underserved areas. Established at the University of New Mexico Health Sciences Center (UNM-HSC), Project ECHO is designed to develop capacity for safe and effective treatment of chronic, common, and complex conditions, while monitoring outcomes to ensure quality of care.
Using multipoint video conferencing technology and clinical management tools, Project ECHO trains and supports primary care providers (PCPs) in the community in an attempt to help them to develop knowledge and self-efficacy in the care of a variety of complex health conditions that they might not typically have felt prepared to treat. 1,2 As a result, these providers receive support to help them to deliver best-practice care for such health conditions in federally qualified health centers (FQHCs) and other community-based clinics where this specialized care was previously unavailable.
The ECHO model is a distance education model in which specialists located at a “hub” (which is located in an academic medical center or more rarely in a public health department or FQHC) connect via simultaneous video link with numerous community-based PCPs (the “spokes”) for the purpose of facilitating case-based learning. The model has been proven safe and effective for teaching PCPs to treat hepatitis C, 3 and is being applied to many other conditions, both nationally and internationally. The ECHO model is based on the principle of demonopolizing medical knowledge, with specialists sharing their expertise and providing telementorship and guided practice to help PCPs to deliver high-quality specialized care to patients in their own communities. 4 Project ECHO serves as a model that other academic medical centers, departments of health, and primary care teams can build upon to provide complex specialized care to underserved populations. 5
We describe a teleECHO clinic, called the Integrated Addictions and Psychiatry (IAP) TeleECHO Clinic, that is focused on treatment of substance use disorders (SUDs) and behavioral health (BH) disorders and has been operating since 2005, in NM. The teleECHO clinic supports PCPs in treating SUDs, with a particular focus on opioid use disorders, which are highly prevalent in NM. Specific aims of the program include the use of case-based learning to teach NM primary care teams to address SUDs, and expansion of patient access to physicians who have the DATA-2000 waiver to prescribe buprenorphine for opioid use disorder. This article focuses on aspects of the teleECHO clinic that are related to SUDs.
The IAP TeleECHO Clinic has aims that are similar to the federally funded Physician Clinical Support System programs, in which individual PCPs are connected one to one with addiction specialists for mentorship. 6 Key differences include the small number of specialists who staff the teleECHO clinic and are able to offer guided practice and telementorship to numerous PCPs simultaneously. Also, the IAP ECHO program has thus far operated in NM and so has been implemented in one state rather than nationally.
How does the ECHO model work for SUDs? Recruitment of health care providers to participate in the addiction teleECHO clinic was initially accomplished primarily by providing grand rounds–type presentations in communities around NM at a community hospital or large clinic. These presentations provided information about the magnitude of the problem of SUDs in various regions of NM and educated participants about the potential benefits of participating in the IAP TeleECHO Clinic. In recent years, participants have primarily learned about the teleECHO program via word of mouth. Participation is free of charge, and upon contacting the IAP program, participants are provided with instructions for how to join the teleECHO clinic via video. The video software platform currently in use by ECHO is Zoom, and ECHO provides participants with access to a license that allows numerous simultaneous participants for extended video conferences. Participants download the Zoom software and are then able to join the teleECHO conference from their personal computer or mobile device. TeleECHO clinic sessions occur once per week for 2 hours. The hub that participants join by video is located at UNM-HSC at Project ECHO. The facilitators/specialists of the teleECHO clinic typically include an addiction specialist, a psychiatrist, a licensed clinical social worker with addiction expertise, a psychiatric nurse or psychiatric nurse specialist, and a community health worker. Participant learners include physicians (family medicine, internal medicine, pediatrics, preventive medicine, and psychiatry) and nonphysicians, including nurses, nurse practitioners, physician assistants, community health workers, counselors, social workers, pharmacists, public health officials, epidemiologists, and administrators.
A typical teleECHO clinic session starts with introductions of all participants (video, telephonic, and in-person) and announcements of events of interest, such as local training opportunities or the opening of new treatment programs. Then a brief didactic session is offered (30-minute presentation on an aspect of SUD or BH). This is followed by case presentations. Cases to be presented are typically submitted by participants in advance of the teleECHO clinic in a standard case template. The participant who submits the case gives an oral case presentation, in de-identified form. Clarifying questions are solicited from video and telephonic participants, and then from participants at the hub, including facilitator/specialists. Then the clinic facilitator invites recommendations and suggestions, and discussion ensues regarding teaching points raised by the presented case. Finally, recommendations are summarized and are later transmitted to the presenters electronically or via fax. Participants who are interested in obtaining no-cost continuing medical education (CME) or continuing education unit (CEU) credits must register online at the start of the clinic and then complete a brief electronic questionnaire at the end of the teleECHO clinic. Discussions vary in length, but complex cases may be discussed for 30 minutes or more.
Methods
New Mexico's IAP TeleECHO clinic
Starting in 2005, specialists in SUD and BH treatment at UNM-HSC have offered a weekly 2-hour teleECHO clinic for PCPs. PCPs from around NM have joined the virtual clinic, participated in brief didactic presentations, and presented de-identified cases from their own practices for feedback from the network in order to improve their ability to treat patients with SUDs and BH disorders. Participation is free of charge, and no-cost CME/CEU credits are offered to participants. To allow us to evaluate teleECHO clinics, we obtained approval from the UNM-HSC Human Research Protections Office (protocol 12–617).
We describe the number of teleECHO clinics offered each year, and the average number of annual participants, number of cases presented, and number of CME/CEU credits awarded. We report on the number of unique participants since the start of 2010, the average total number of teleECHO clinics attended, and the average duration of engagement in the teleECHO clinic. We studied cases that were presented during the first 4 weeks of each year between 2010 and 2015, and tabulated the frequency with which individual SUDs were presented and discussed. We report on the core SUD curriculum that is offered as part of the IAP didactic presentations each year.
Recruitment for buprenorphine training
This teleECHO clinic has also been used to recruit physicians to participate in the 8-hour DATA-2000 waiver training for prescribing buprenorphine for opioid use disorder. These trainings are offered by Project ECHO IAP program, with certification provided by the American Association of Addiction Psychiatry (AAAP) or American Osteopathic Association of Addiction Medicine (AOAAM). Supporting the availability of medication-assisted treatment (MAT) with buprenorphine has been a major focus of the teleECHO clinic.
In order to evaluate the possible impact of using the teleECHO network to recruit for the buprenorphine waiver courses that we have offered in NM, we obtained data from the Substance Abuse and Mental Health Services Administration (SAMHSA) on all DATA-2000 buprenorphine waivers that have been issued in the United States (US) since 2002, listing the practice ZIP code and the date of issue of the waiver. In order to examine the impact of states' efforts to increase the number of buprenorphine-waivered physicians, we ranked states by how many new buprenorphine waivers had been granted in their state during each calendar year from 2002 to 2014. We then grouped all waivered physicians by state and divided by the population of that state, arriving at a “total buprenorphine-waivered physicians per capita” number. Using this number, we ranked the states 1 through 50.
We obtained census demographic data at the ZIP code level (from Zipcodes.com) and used this to evaluate the availability of buprenorphine-certified physicians in ZIP codes that are poor, rural, and in which more than 50% of residents self-identify as American Indian or Alaska Native, Asian American, Black or African American, Hispanic or Latino, or Native Hawaiian/Other Pacific Islander. A priori, we defined high-poverty ZIP codes as those in which the average income per household was less than the US average. Rural ZIP codes were defined as those with less than 1000 residents per square mile. We used these criteria as a proxy for underserved areas. We calculated the number of physicians who received the DATA-2000 waiver and who listed their practice address in one of these underserved ZIP code in the years before and in the years following the initiation of the IAP TeleECHO Clinic. We compared the growth of the supply of waivered physicians in NM with those outside of NM in these target ZIP codes.
Results
Since 2008, more than 950 patient cases (both SUDs and BH disorders) have been presented during the IAP TeleECHO Clinic. More than 9000 hours of CME/CEU have been awarded for participation. An average of 147 participants join the teleECHO clinic each year. Since January 1, 2010, 654 unique participants attended at least 1 clinic (many of them national and international visitors to the ECHO Institute); 285 participants have attended more than 1 session. The maximum number of clinics that any individual attended was 101, with the average for those attending more than 1 clinic session being 12.4 clinics and the average length of time between first and last clinic being 16.3 months.
SUD cases that were presented during the first 4 teleECHO clinics of each calendar year (2010–2015) were tabulated. Opioids are the substances that have been presented and discussed most frequently (31% of total SUD cases), followed by alcohol (21%) and cannabis (12%). Other substances that were the focus of discussion in this sample of cases included, in descending order of frequency, cocaine, carisoprodol, benzodiazepines, tobacco, methamphetamine, and dextromethorphan.
For the brief didactic presentations, a set of core topics on treatment of SUDs is repeated annually (Table 1), along with presentations on BH disorders and other topics suggested by the particular cases that are presented.
Table 1.
Substance use disorder didactic curriculum from the integrated addictions and psychiatry (IAP) TeleECHO clinic
| Alcohol use disorder |
| Management of alcohol withdrawal |
| Opioid use disorder |
| Management of opioid withdrawal |
| Tobacco use disorder |
| Benzodiazepine use disorder |
| Cannabis use disorder |
| Synthetic drugs (“bath salts” and “spice”) |
| Identifying and treating dual-diagnosis patients |
| Challenging conversations in treatment of substance use disorders |
| Stigma and stigma-busting |
| Seeking safety (management of trauma and substance use disorders) |
| Relapse prevention |
| Community reinforcement approach (CRA) |
| Motivational interviewing update |
| Science of urine drug monitoring |
The ECHO model has allowed for rapid dissemination of new research findings and epidemiologic trends. Examples include rapid spread of information over the teleECHO network regarding purpura associated with cocaine that is adulterated with levamisole; real-time sharing of information about overdose deaths attributable to heroin adulterated with fentanyl; publicizing and encouraging the use of the NM Prescription Monitoring Program; and disseminating emerging data on the appropriate use of buprenorphine-metabolite testing.
Since 2006, when only 36 NM physicians were listed as buprenorphine-waivered in the federal database, more than 375 NM physicians have participated in DATA-2000 buprenorphine waiver trainings offered by Project ECHO IAP program (with certification provided by AAAP or AOAAM). In addition to the curriculum required by these organizations, the ECHO trainings include a patient panel, a provider panel, and training in harm reduction (educating patients about syringe exchange and reversal of overdose). Physicians were recruited for these trainings through the teleECHO network and came from all areas of the state.
New Mexico now has more buprenorphine-waivered physicians per capita than all but 3 other US states (Figure 1); the states of Vermont, Maine, Massachusetts, and New Mexico were the top-ranked states in number of waivers per capita as of 2014. Prior to the start of the ECHO IAP program in 2005, NM ranked 13th nationally in waivered physicians per capita (data not shown). In addition, the number of waivered physicians per capita who practice in underserved areas has increased more rapidly in NM than in the US overall since 2005 (Figure 2).
Figure 1.
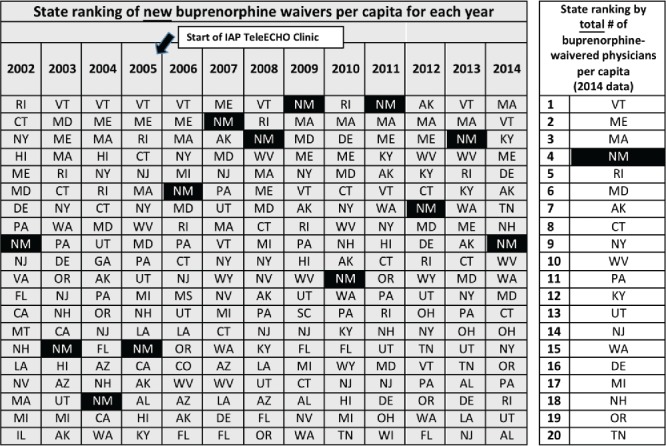
States ranked by number of new buprenorphine-waivered physicians per capita in each state per year, before and after the start of the Integrated Addictions and Psychiatry (IAP) TeleECHO Clinic in 10/2005; and states ranked by total number of buprenorphine-waivered physicians per capita (2014).
Figure 2.
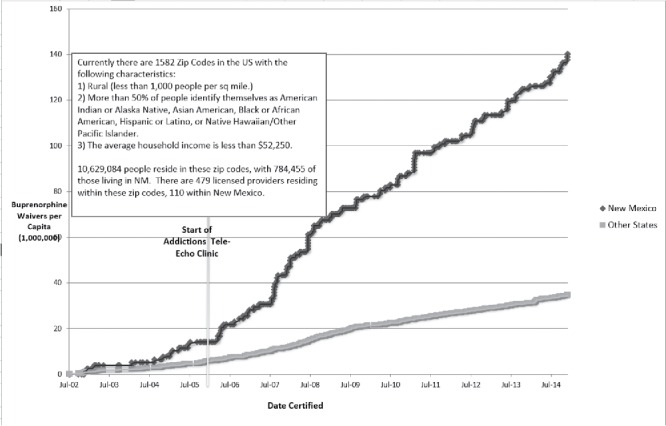
Cumulative number of buprenophine-waivered physicians per million population in traditionally underserved ZIP codes in New Mexico versus the United States.
Discussion
The ECHO model has provided a platform to reach hundreds of NM PCPs over the past decade and to engage them in case-based learning about the diagnosis and treatment of SUDs.
The applied, case-based nature of the teaching in the teleECHO clinic is designed to promote rapid incorporation of new information into clinical practice. It also provides a mechanism to disseminate information that has time-sensitive safety implications, such as an increase in overdose risk caused by new availability of a more potent street-drug formulation.
Participants in ECHO cite the opportunity to learn up-to-date information and diminished professional isolation as important motivators for participation in teleECHO clinics. 2,5 Potential barriers to participation include lack of reimbursement for participation in teleECHO clinics, decreased clinical productivity caused by time allocated to teleECHO participation (which may in turn have implications for PCP income), and, in the case of the IAP TeleECHO Clinic, hesitation on the part of PCPs or administrators to engage in treatment of addiction due to stigma or practical barriers.
Access to buprenorphine treatment for opioid use disorder in the US remains limited, particularly outside of urban areas. 7 Recent studies suggest that almost all US states have an inadequate supply of buprenorphine treatment providers to meet their populations' need for this type of treatment. 8
Efforts are occurring nationally to improve access to buprenorphine treatment. Use of the IAP TeleECHO Clinic to recruit physicians to obtain the DATA-2000 waiver to prescribe buprenorphine has coincided with marked increases in the numbers of waivered physicians who practice in traditionally underserved areas in NM, and also with NM achieving one of the highest per capita numbers of waivered physicians in the US. It is impossible to disentangle the effects of the addiction teleECHO program from the influence of national or other state efforts. However, these increases are notable in light of the fact that NM ranks below the US average in spending on treatment for BH and SUDs, unlike the other states that exceed NM in waivered physicians per capita (Figure 1). In 2005 NM spent an average of $316 per person on BH and SUD treatment, compared with Vermont (VT) $741, Maine (ME) $673, Massachusettts (MA) $652, and US average $423. 9 New Mexico also has higher proportions of adults who reported use of illicit drugs in the year prior to being surveyed (2009–2013) than do these other states (NM 3.5%, VT 3.4%, MA 3.3%, and ME 2.2%). 10-13
The teleECHO clinic's focus on opioid use disorder and buprenorphine training, certification, and support has coincided with enhancement of the capacity to treat opioid use disorder in NM. Because the teleECHO network reaches PCPs in remote areas and appeals to physicians who work with traditionally underserved populations, it may provide an effective way to reach and recruit these physicians. Use of a teleECHO clinic to recruit and train PCPs in treatment of SUDs may be a cost-effective way to create a more highly trained workforce to address SUDs in traditionally underserved areas.
Use of the ECHO model to focus on SUD diagnosis and treatment can be replicated nationally and internationally by academic medical centers and departments of health that seek to expand SUD treatment capacity in their region. Implementation of an ECHO program is facilitated by no-cost training and technical support offered by the ECHO Institute (echo.unm.edu).
Acknowledgments
We thank especially Leena Imam, Melissa Meier, and Bonnie Kraybill, RN, for supporting the operations of the IAP TeleECHO Clinic; and Andrea Bradford, MSc, for editorial assistance.
Author contributions
Miriam Komaromy conceived of the study design, participated in data collection and analysis/interpretation, and drafted and revised the manuscript. Dan Duhigg and Tom Burke participated in data analysis and interpretation of results, and provided manuscript revisions. Adam Metcalf, Cristina Carlson, and Karla Thornton participated in interpretation of results and provided manuscript revisions. Summers Kalishman, Leslie Hayes, and Sanjeev Arora participated in analysis and interpretation and revised the manuscript.
Funding
Funding for the IAP TeleECHO Clinic was generously provided by the NM State Legislature and grants from Robert Wood Johnson Foundation, GE Foundation, and the Agency for Healthcare Research and Quality (AHRQ; 1R24HS016510-01A1). The funders provided financial support only for the project. The authors declare that they have no conflicts of interest.
References
- Masi C, Hamlish T, Davis A. Using an established telehealth model to train urban primary care providers on hypertension management. J Clin Hypertens. 2012;14:45. doi: 10.1111/j.1751-7176.2011.00559.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora S, Kalishman S, Thornton K. Expanding access to hepatitis C virus treatment—Extension for Community Healthcare Outcomes (ECHO) Project: disruptive innovation in specialty care. Hepatology. 2010;52:1124. doi: 10.1002/hep.23802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora S, Thornton K, Murata G. Outcomes of treatment for hepatitis C virus infection by primary care providers. N Engl J Med. 2011;364:2199–2207. doi: 10.1056/NEJMoa1009370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arora S, Thornton K, Komaromy M. Demonopolizing medical knowledge. Acad Med. 2014;89:30–32. doi: 10.1097/ACM.0000000000000051. [DOI] [PubMed] [Google Scholar]
- Arora S, Kalishman S, Dion D. Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care. Health Aff (Millwood) 2011;30:1176–1184. doi: 10.1377/hlthaff.2011.0278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egan JE, Casadonte P, Gartenmann T. The physician clinical support system-buprenorphine (PCSS-B): a novel project to expand/improve buprenorphine treatment. J Gen Intern Med. 2010;25:936–941. doi: 10.1007/s11606-010-1377-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt RA, Andrilla CH, Catlin M. Geographic and specialty distribution of US physicians trained to treat opioid use disorder. Ann Fam Med. 2015;13:23–26. doi: 10.1370/afm.1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones CM, Campopiano M, Baldwin G. National and state treatment need and capacity for opioid agonist medication-assisted treatment. Am J Public Health. doi: 10.2105/AJPH.2015.302664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . State-Level Spending on Mental Health Services and Substance Abuse Treatment, 1997–2005. Rockville, MD: Center for Mental Health Services and Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; 2012. pp. 12–4672. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Behavioral Health Barometer. New Mexico: Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Behavioral Health Barometer: Massachusetts, 2014. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Behavioral Health Barometer: Vermont, 2014. 380 Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]
- Substance Abuse and Mental Health Services Administration . Behavioral Health Barometer: Maine, 2014. 380 Rockville, MD: Substance Abuse and Mental Health Services Administration; 2015. [Google Scholar]


