Abstract
Purpose:
Mobility disability is associated with poor lower body function among older adults. This study examines whether specific types of neighborhood characteristics moderate that association.
Design and Methods:
This study is based on a cross-sectional sample of 884 people aged ≥ 65 years identified through service organizations in Alameda County, CA; Cook County, IL; Allegheny County, PA; and Wake and Durham counties, NC. In-person interviews focus on neighborhood characteristics, physical and cognitive function, depression, and walking. Functional capacity is tested using objective measures of lower body strength, balance, and walking speed. Mobility disability, the main study outcome, is measured as self-reported level of difficulty in walking 2–3 neighborhood blocks. Estimates of main and interactive effects are derived from logistic regression models.
Results:
Among older adults with poor lower body function, those who report less proximity to goods and services and barriers to walking report more mobility disability than other older adults. In contrast, among older adults with good lower body function, there is a low prevalence of mobility disability and little association between perceptions of the neighborhood and mobility disability.
Implications:
In addition to more refined longitudinal studies, this research provides a foundation for innovative place-based rehabilitation and hospital discharge programs for older adults newly diagnosed and treated for chronic health conditions.
Level of difficulty in walking is an important measure of mobility disability among older adults (Lee & Buchner, 2008; Satariano et al., 2012). Those who report difficulty in walking two to three neighborhood blocks, a standard measure of mobility disability (Rosow & Breslau, 1966), are in poorer health and have lower levels of overall functioning than those who do not report such difficulty (Hardy, Kang, Studenski, & Degenholtz, 2010; Simonsick, Guralnik, Volpato, Balfour, & Fried, 2005). Disability is typically defined as physical or cognitive difficulty in performing social roles or other everyday activities (Pope & Tarlov, 1991). It represents a dynamic state in which functional capacities, such as balance and lower body strength, are insufficient to meet current and changing social expectations and environmental challenges (Verbrugge & Jette, 1994). Functional limitations, in turn, refer to either self-reported or directly measured reduced generic capacities, such as lifting, balance, walking speed, and lower body strength (Pope & Tarlov, 1991; Verbrugge & Jette, 1994).
Given the health and functional impact of walking, it is important to understand the reasons why some older adults report difficulty walking in their neighborhood (defined here as “mobility disability”), whereas others do not. Not only will this research contribute to a better understanding of the epidemiology of aging, health, and mobility, it will also serve as a foundation for the development of innovative interventions to promote walking and good health.
Reported difficulty in walking is associated with characteristics of both lower body functional capacity and environmental challenge (King, 2008; Lawton, 1986). For example, older adults with reduced functional capacity, such as poor lower body function, are more likely than those with good lower body function to be less mobile, experience greater disability, and suffer premature death (Guralnik, Ferrucci, Simonsick, Salive, & Wallace, 1995). There is also research indicating that older adults’ perceptions of their neighborhoods as well as the structural characteristics of the neighborhoods are associated with both frequency and level of difficulty in walking (Satariano, Ory, & Lee, 2012; Yen, Michael, & Perdue, 2009). Older adults who reside in neighborhoods that are single-use, have broken sidewalks, extended block lengths, or few walkable destinations tend to walk less than older residents living in more compact, mixed use (i.e., residences in close proximity to goods and services) neighborhoods with well-maintained sidewalks (Clarke, Ailshire, & Lantz, 2009; Li, Fisher, Brownson, & Bosworth, 2005; Satariano et al., 2010; Shumway-Cook et al., 2003). In addition, older adults who perceive their neighborhoods as unsafe with more impediments to walking are, in fact, less likely to walk and more likely to report difficulty walking there (Balfour & Kaplan, 2002; Clark et al., 2009; Wang & Lee, 2010).
There is a growing body of research indicating that the joint or interactive effects of characteristics of people and places may be especially important (Clarke, Ailshire, Bader, Morenoff, & House, 2008; Clarke & George, 2005; Gong, Gallacher, Palmer, & Fone, 2014). Indeed, the basic tenet of the environmental theory of aging, as first proposed by Lawton and colleagues, is that the effects of the environment on health and well-being become more salient as age-related functional limitations increase (Lawton & Nahemow, 1973; Lawton, 1986). This suggests, in turn, that elements of the environment, as measured by either self-reports or objective indicators, have a more significant effect on health and function both among older adults than among younger adults, and also among older adults with poor functional capacity than among older adults with good functional capacity. In other words, the characteristics of place may moderate the adverse effects of poor lower body functioning on ease of walking. Although the nature of the interaction involving the functional capacity of individuals and the characteristics of neighborhoods may vary by the type and measurement of mobility examined (e.g., reports of time spent walking in a typical week vs. reports of overall difficulty walking) and the type of analytic approach employed (Satariano et al., 2010), there is evidence to support Lawton and colleagues’ hypothesis. Compared with disabled older adults, those without disabilities travel greater distances, complete more errands, and are better able to circumvent environmental barriers, such as poor street conditions (Shumway-Cook et al., 2003; Shumway-Cook et al., 2002). From a policy perspective then, this research suggests that good neighborhood design and maintenance may reduce the extent and severity of difficulty walking among older people with reduced lower body capacity (Dumbaugh, 2008; Plouffe & Kalache, 2010). With the aging of the population and the prospects of an increase in the prevalence of lower body functional limitations, more detailed research in this area is needed.
Our purpose here is to examine whether elements of the neighborhood environment moderate the association between objectively measured lower body function and mobility disability, as measured by self-reported difficulty in walking two to three neighborhood blocks.
Methods
Sample
The data set used for this study is from the Healthy Aging Research Network (HAN) Walking Study, a cross-sectional study of the associations among functional capacity, the neighborhood environment, and walking in older residents in four locations across the United States, and funded by the Centers for Disease Control and Prevention (CDC). The sample consists of 884 people aged 65 and older identified through senior organizations in Alameda County, CA; Cook County, IL; Allegheny County, PA; and Wake and Durham Counties, NC. These counties, selected from among participating sites in the CDC HAN, reflect a range of weather and topographic patterns.
All senior organizations (in most cases, senior centers) in these geographic areas were geocoded and categorized into quintiles of housing density levels as a general proxy for “walkability,” based on the 2000U.S. Census. In order to ensure that senior centers from different types of neighborhoods were selected, at least four senior organizations were randomly sampled from each of the five categories of housing density to ensure variability in walkability. This sampling was conducted in each of the four geographic areas. Fifteen participants per senior organization were targeted for enrollment. Ultimately, participants were recruited from 77 different senior organizations, which helped to ensure that the participants’ home residences were located in a wide variety of neighborhood types.
Prospective participants completed a brief questionnaire to determine eligibility: age ≥ 65 years, English-speaking, and residing at current address for 12 months or more with no plans to move during the next 3 months. Exclusion criteria included any chronic or serious condition that could limit participation in unsupervised light to moderate physical activity, outdoor walking restricted on doctor’s orders, self-reported inability to walk outdoors because of a medical condition, or signs of cognitive impairment sufficient to prevent completion of the interview and walking diary. These criteria restricted the sample to individuals who were physically capable of walking within their neighborhood. Enrollment was monitored to ensure recruitment of people with a range of self-reported overall health.
Eligible participants were interviewed at the senior organizations (78.7%); in the participant’s home (17.4%); or at some other location (3.9%). Informed consent was obtained prior to the interview, as provided by the Institutional Review Board at each of the participating universities: University of California, Berkeley; University of Illinois, Chicago; University of Pittsburgh; and University of North Carolina, Chapel Hill. The interviews were conducted between September 2005 and November 2007.
Baseline Interview
The interview included both a questionnaire and direct assessments of physical performance. The questionnaire included demographic and socioeconomic factors; history of chronic conditions and symptoms; history of falls and injuries; physical function and activities of everyday life (activities of daily living [ADLs], instrumental ADLs, Rosow-Breslau and Nagi items; Nagi, 1976; Rosow & Breslau, 1966; VanSwearingen & Brach, 2001); cognitive function (the Mental Alternation Test and a modified version of the Mini-Mental State Examination; Barnes, Yaffe, Satariano, & Tager, 2003; Billick, Siedenburg, Burgert, & Bruni-Solhkhah, 2001; Folstein, Folstein, & McHugh, 1975; Reitan, 1958); general feelings and a modified version of the Center for Epidemiologic Studies Depression Scale (Andresen, Malmgren, Carter, & Patrick, 1994); self-efficacy for walking; social networks and social support; extensive questions on assessments of neighborhood characteristics (Saelens, Sallis, Black, & Chen, 2003); and levels of walking and other forms of physical activity. Direct measures of performance were also included, based on measures of walking speed, balance, and lower body strength (Guralnik et al., 1995; Guralnik & Simonsick, 1993; Guralnik et al., 1994; Satariano et al., 2010).
Study Variables
Mobility Disability
Mobility disability, the main study outcome, is measured by self-reported walking difficulty, based on a modified set of standard questions from Rosow and Breslau (Rosow & Breslau, 1966; VanSwearingen & Brach, 2001). In this version, respondents were asked what level of difficulty they have had in the past month (a) getting up or down a flight of stairs and (b) walking two to three neighborhood blocks. If they had done the activity in the past month, respondents were asked to report their level of difficulty from the following options: “a lot,” “some,” “a little,” or “none.” If they had not done the activity in the past month, they were asked to report whether they did not do the activity because of doctor’s orders, are not able to, they never do, they do not know, or they refused to answer. Responses to the extent of difficulty were dichotomized as “no difficulty” (“none”) versus “any difficulty” (“a little”, “some”, or “a lot”). Those who reported that they did not do the activity because they were “not able to” were also included in the general summary category of “any difficulty.” Those reporting that they did not do the activity because of “doctor’s orders” (0%), because they “never do” (2.5%), “don’t know” (0%), or they “refused” to answer (0%) were dropped from the analysis. Given our focus on the outdoor environment and the inability to differentiate between indoor and outdoor stair climbing, we restricted the measurement of mobility disability to reported difficulty in walking two to three neighborhood blocks, which is consistent with other studies in this area (Clarke et al., 2008).
Lower Body Functional Capacity
A modified version of the Short Physical Performance Battery (SPPB) was used (Guralnik et al., 1995; Satariano et al., 2010). The standard version of SPPB, which is based on direct, objective measures of walking speed, balance, and lower body strength, was modified in several ways. First, to obtain a more sensitive measure of regular, sustained walking, walking speed (feet per second) was derived from a 60-s walk rather than a single 8-foot walk. Second, a one-legged stand was included to distinguish among those who could complete the full tandem stand (standing with the heel of one foot in front of and touching the toes of the other foot for 10 s), the final and most difficult standard SPPB assessment of balance. Seventy-six percent of the respondents could hold the full-tandem stand for 10 s, but 47.1% could not complete the more difficult one-legged test. More (49.1%) of the participants who completed the one-legged stand reported walking ≥ 150 minutes per week, the CDC recommended level of walking, compared with those who completed the full tandem stand only (30.6%). Finally, as in the standard SPPB, lower body strength was measured as the time to rise from a seated position to a standing position five times in sequence with arms folded across the chest. This modified SPPB, like the original version, was summarized in quartiles from poor to excellent lower body function (Satariano et al., 2010). The terms “lower body functional capacity,” “lower body function,” and “capacity” are used interchangeably in this article.
Neighborhood Environment: Self-report
Measurement of the neighborhood environment was based on questions from the Neighborhood Environment Walkability Scale (NEWS) (Saelens et al., 2003). This analysis was based on an abbreviated scoring scheme developed by Saelens and colleagues for each of the subscales (Cerin, Saelens, Salls, & Frank, 2006). Our interview included slightly fewer questions than the full abbreviated scoring scheme, but covered all the domains. Fourteen variables were created from the NEWS questions examining primary type of buildings, primary type of housing, walking time to destinations, land-use mix/access to services, street connectivity, walking facilities, aesthetics, pedestrian traffic safety, crime and safety, neighborhood satisfaction/social capital, parking, cul-de-sacs, hilliness, and barriers to walking (e.g., freeways, railway lines, and rivers) .
Neighborhood Environment: Geographic Information Systems
Three geographic information systems (GIS)-derived neighborhood variables were included in the analysis (number of selected types of businesses within 400 m of participant’s residence, median block length for census track of residence, and housing density for census track of residence).
Geocoding of participants’ residences was conducted in two rounds. The first round used ESRI Business Analyst 9.2. For the second round of geocoding, ArcInfo 9.3 was employed to take advantage of improvements to the base map. Manual geocoding was also used.
The GIS-derived neighborhood business density variable was based on geocoded environmental data within a 400-m buffer (radial distance) of each participant’s residential address (Nagel, Carlson, Bosworth, & Michael, 2008). This distance (a) has been used in other studies of older populations; (b) is comparable to the average distance traveled by older subjects, based on direct observations of neighborhood walking (~300 m) (Shumway-Cook et al., 2002); and (c) is consistent with a regular median walking distance traveled by members of the present study cohort (366 m), based on direct assessment of their walking speed (43 m/min) and reported time to reach common walking destinations. ESRI Business Analyst was used, which contains data from InfoUSA for businesses listed on January 1, 2006. Businesses that were possible walking destinations were categorized according to North American Industry Classification System codes and summed to create a count of the number of retail businesses within the 400 m buffer.
Street connectivity (e.g., median block length) and housing unit density were determined by the census tract of each participant’s residence. The U.S. Census 2000 data from the SF3 files was used to measure housing unit density. Median block length data from 2000 was used from the RAND Center for Population Health and Health Disparities (CPHHD) was used to measure street connectivity. In addition, the CPHHD median block length data for 2000 were supplemented with 1990 data when 2000 data were missing after validating that, when both 1990 and 2000 median block length data were available, they were usually identical.
Covariates
Data included a standard set of covariates: study site, age, gender, race, household income, education level, access to a car, and number of years at the current residential address.
Analytic Plan
General linear models (GLM) were used to fit models in R statistical software version 3.0.2 (R Development Core Team, 2013). We constructed a series of estimates of the interaction of lower body function with a series of neighborhood variables on the outcome of walking difficulty. We fit logistic regression models. All of the main effects were specified as dummy variables, including lower body function (four categories) and the neighborhood variables (two, three, or four categories). Each interaction term was specified as the continuous product of the ordered categories (lower body function times a neighborhood variable). To reduce the number of parameters in the models, we entered the ordered categorical variables for the interaction terms, not via dummy variables, but a simple integer scale (e.g., the barrier variable was parameterized in the interaction term as 4, 3, 2, and 1, with 4 = least barriers [most walkable] to 1 = most barriers [least walkable], whereas lower body function was parameterized in all the interaction term as 4, 3, 2, and 1, with 4 = best quartile of lower body function and 1 = worst quartile of lower body function). For the main effect variables, these same variables were coded as three dummy variables, that is, indicators of membership in groups 2–4. A separate model was derived for each of the 17 NEWS and GIS neighborhood variables and its interaction with lower body function, adjusting for a standard set of 8 previously identified potential confounders (study site, age, gender, race, education, income, access to a car, and number of years at the current address). For each model, we predicted the probability of difficulty walking two to three neighborhood blocks (mobility disability), setting the two variables of interest that make up the interaction at all relevant combinations, keeping the remaining variables at their observed value. Based on these adjusted marginal predictions, we constructed measures of additive interaction to calculate the excess risk associated with the extremes of perceived and GIS-based neighborhood characteristics for both the group with the highest functional capacity and the group with the lowest functional capacity. We then used the clustered nonparametric bootstrap (that is, randomly sampled clusters with replacement) (Efron, 1982) to derive robust standard errors, which account for correlation due to the clustering. Following convention, interaction terms with p < .20, rather than 0.05, were considered to be significant (Selvin, 1996). The Bonferroni correction was also calculated to adjust for multiple comparisons (Bland & Altman, 1995). Because there is some disagreement about the value of the Bonferroni correction in all instances, for example, unnecessary reduction of statistical power (Rothman, 1990), we present the results with and without the correction for the readers’ consideration.
Results
Sample Characteristics
Table 1 compares the distribution of key sociodemographic variables by study site between participants and the general population of residents aged ≥ 65 years in the corresponding county, based on Census 2000 data. These results are generally consistent with a 1984 national survey that found that women were over represented at senior centers (Krout, Cutler, & Coward, 1990). Census 2000 data on educational level, years living in neighborhood, and access to a car were categorized differently in the census data than in our interview data, so a comparison was not made.
Table 1.
Demographics, Lower Body Function, and Mobility Disability of Sample by Site Compared With County Census Data
| Demographic variables | Alameda County, CA | Allegheny County, PA | Cook County, IL | Wake and Durham Counties, NC | Total | p valueb | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Study | Countya | Study | County | Study | County | Study | County | Study | ||
| (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | (%) | ||
| Age (n = 884) | ||||||||||
| 65–74 years | 49.2 | 51.6 | 46.3 | 49.3 | 52.2 | 52.4 | 56.0 | 55.0 | 51.0 | .92 |
| 75+ years | 50.8 | 48.4 | 53.7 | 50.7 | 47.8 | 47.6 | 44.0 | 45.0 | 49.0 | |
| Sex (n =884) | ||||||||||
| Female | 77.4 | 59.3 | 78.6 | 61.0 | 71.4 | 60.5 | 78.4 | 60.7 | 76.6 | <.0001 |
| Male | 22.6 | 40.7 | 21.4 | 39.0 | 28.6 | 39.5 | 21.6 | 39.3 | 23.4 | |
| Race (n = 866) | ||||||||||
| Other race | 5.0 | 3.2 | 0.0 | 0.2 | 1.0 | 2.3 | 0.0 | 0.4 | 1.6 | <.0001 |
| Two or more races | 4.2 | 2.5 | 0.0 | 0.4 | 2.5 | 1.3 | 0.4 | 0.6 | 1.8 | |
| African-American | 15.8 | 14.2 | 22.5 | 7.8 | 21.0 | 20.3 | 35.7 | 20.5 | 23.8 | |
| Asian | 13.8 | 17.7 | 1.5 | 0.3 | 0.5 | 3.0 | 7.5 | 1.3 | 6.2 | |
| White | 61.3 | 62.4 | 76.0 | 91.3 | 75.0 | 73.2 | 56.4 | 77.2 | 66.6 | |
| Latino or Hispanic (n = 871) | ||||||||||
| Yes | 5.8 | 8.6 | 0.5 | 0.4 | 3.0 | 5.8 | 1.7 | 0.8 | 2.9 | .10 |
| No | 94.2 | 91.4 | 99.5 | 99.6 | 97.0 | 94.2 | 98.3 | 99.2 | 97.1 | |
| Years of schooling (n = 872) | ||||||||||
| 0–11 years | 7.9 | NA | 18.9 | NA | 5.5 | NA | 15.7 | NA | 11.9 | |
| 12 years | 19.2 | NA | 51.2 | NA | 32.8 | NA | 30.0 | NA | 32.6 | |
| Over 12 years | 72.9 | NA | 29.9 | NA | 61.7 | NA | 54.3 | NA | 55.5 | |
| Income (n = 680) | ||||||||||
| Less than $15,000 | 20.9 | 23.0 | 36.1 | 28.1 | 15.1 | 25.3 | 30.8 | 22.8 | 26.0 | <.0001 |
| $15,000–$24,999 | 19.4 | 16.4 | 33.5 | 23.3 | 23.8 | 18.6 | 21.1 | 15.9 | 24.0 | |
| $25,000–$49,999 | 32.7 | 27.3 | 23.4 | 28.9 | 38.9 | 28.5 | 25.9 | 28.9 | 29.9 | |
| $50,000 or more | 27.0 | 33.3 | 7.0 | 19.7 | 22.2 | 27.6 | 22.2 | 32.4 | 20.1 | |
| Currently drive or access to driver (n = 876) | ||||||||||
| No | 13.2 | NA | 23.4 | NA | 14.9 | NA | 17.7 | NA | 17.1 | |
| Yes | 86.8 | NA | 76.6 | NA | 85.1 | NA | 82.3 | NA | 82.9 | |
| Years living in neighborhood | ||||||||||
| <10 years | 28.2 | NA | 29.4 | NA | 25.6 | NA | 53.0 | NA | 34.4 | |
| 10–19 years | 14.9 | NA | 12.4 | NA | 13.8 | NA | 16.4 | NA | 14.5 | |
| 20–29 years | 13.3 | NA | 12.4 | NA | 13.8 | NA | 10.3 | NA | 12.4 | |
| 30–39 years | 19.8 | NA | 14.4 | NA | 24.6 | NA | 9.1 | NA | 16.9 | |
| 40–49 years | 16.1 | NA | 17.4 | NA | 12.8 | NA | 7.8 | NA | 13.5 | |
| 50–59 years | 6.5 | NA | 9.5 | NA | 7.4 | NA | 2.6 | NA | 6.3 | |
| >60 years | 1.2 | NA | 4.5 | NA | 2.0 | NA | 0.9 | NA | 2.0 | |
| Lower body function | ||||||||||
| Excellent | 20.7 | NA | 18.4 | NA | 20.4 | NA | 16.1 | NA | 18.1 | |
| Good | 24.4 | NA | 25 | NA | 27.4 | NA | 25.9 | NA | 25.6 | |
| Fair | 19.5 | NA | 23.5 | NA | 23.7 | NA | 26.8 | NA | 23.2 | |
| Poor | 35.2 | NA | 33.2 | NA | 28.5 | NA | 31.3 | NA | 32.3 | |
| Difficulty walking 2–3 blocks | ||||||||||
| Any difficulty | 23.8 | NA | 31.1 | NA | 32 | NA | 20.2 | NA | 26.4 | |
Notes: aU.S. Census 2000 data for adults 65+.
bOverall p value for the chi-square statistic comparing study populations to county populations as measured by the 2000 Census across the four geographic sites.
NA = Not available; census data categorized in the same way restricted to adults age 65+.
Lower Body Function, Neighborhoods, and Walking Difficulty
Overall, 26.4% of the respondents report difficulty in walking 2–3 neighborhood blocks (mobility disability). Here, difficulty is categorized as reports of any difficulty versus no difficulty. Table 2 shows the modeled percentage of people who have difficulty in the lowest and highest quartiles of objectively measured lower body function.
Table 2.
Modeled Percent of People in Best and Worse Functional Capacity Categories Having Difficulty Walking Two to Three Blocks by Neighborhood Characteristics
| Poor capacity (%) | Good capacity (%) | p value (%) | |
|---|---|---|---|
| Primary type of buildings in neighborhood (n = 883) | |||
| Commercial/mixed | 32.7 | 5.1 | |
| Residential | 46.3 | 6.0 | |
| Excess risk (95% CI) | 13.6 (0.6, 23.7) | 0.8 (−5.6, 7.4) | .075 |
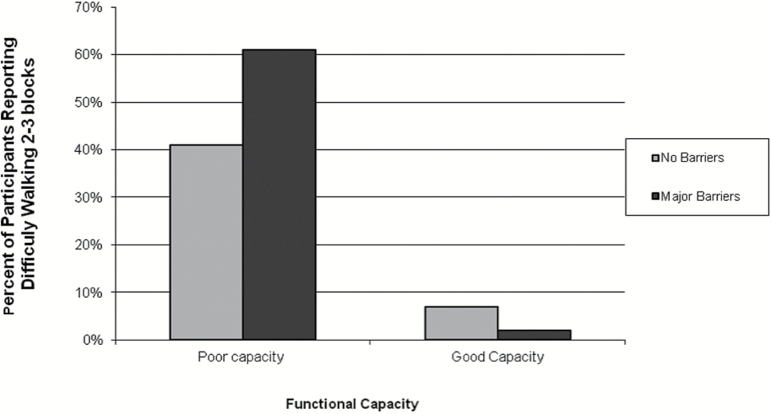
| Major barriers to walking (n = 874) | |||
| No barriers | 40.6 | 6.8 | |
| Major barriers | 61.2 | 2.2 | |
| Excess risk (95% CI) | 20.5 (1.4, 37.7) | −4.6 (−11.3, 2.1) | <.01* |
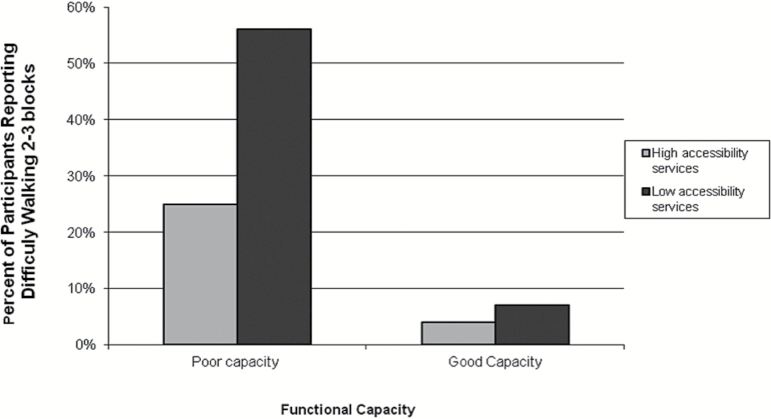
| Land-use mix/access to services scale (n = 878) | |||
| High accessibility services | 24.7 | 3.8 | |
| Low accessibility services | 55.9 | 7.4 | |
| Excess risk (95% CI) | 31.2 (15.9, 46.2) | 3.6 (−1.8, 14.9) | <.01* |
| Walking times to specific destinations (n = 884) | |||
| Short walking time to destinations | 24.9 | 4.4 | |
| Long walking time to destinations | 56.9 | 7.2 | |
| Excess risk (95% CI) | 32.0 (15.7, 45.9) | 2.8 (−3.8, 13.9) | <.01* |
*p value remains significant at <.20 level after Bonferroni adjustment.
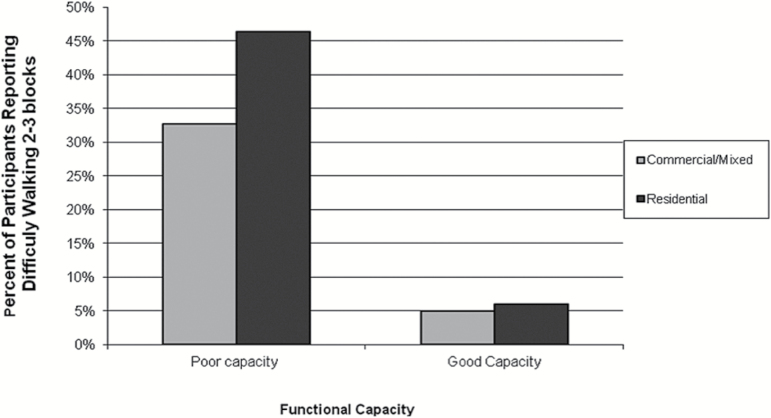
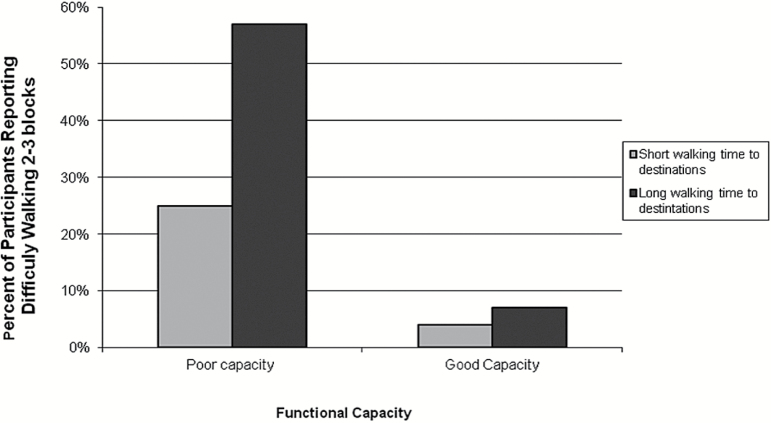
Estimates of interaction were obtained from lower body function and each of the NEWS and GIS neighborhood variables. Separate models were derived for each of the 17 environmental variables and their interaction with lower body function, adjusting for the covariates. Of the 17 neighborhood models, significant interactions (p < .20) were found for four self-report NEWS variables: Type of neighborhood buildings (commercial/mixed vs. residential), major barriers to walking (no barriers vs. major barriers), land use mix/access to services (high accessibility to services vs. low accessibility to services), and walking time to specific destinations (short walking time to destinations vs. long walking time to destinations). There were no significant interactions found for lower body function and any of the GIS variables. (Table 2; Figures 1–4)
Figure 1.
Percentage of participants reporting difficulty walking two to three blocks by functional capacity by primary type of building in neighborhood.
Figure 4.
Percentage of participants reporting difficulty walking two to three blocks by functional capacity by walking times to various destinations.
Figure 2.
Percentage of participants reporting difficulty walking two to three blocks by functional capacity by barriers to walking.
Figure 3.
Percentage of participants reporting difficulty walking two to three blocks by functional capacity by land-use mix.
When adjusting for multiple comparisons, using the conservative Bonferroni correction, there is still a significant interaction for three of the four interactions (lower body function interacting with major barriers, land use mix/access to services, and walking time to specific destinations). However, with this correction, there is no significant interaction at p < .20 for lower body function and the perceived primary neighborhood building type (mixed commercial vs. residential). The symbol (*) is used in Table 2 to designate those tests of interaction that are still statistically significant (at p < .20) following the Bonferroni correction. In each of the four models, people in the lowest quartile of lower body function were more likely than those in the highest quartile to report difficulty walking two to three neighborhood blocks, suggesting a main effect for capacity. Furthermore, the environment mattered more to those in the lowest quartile of lower body function. Put differently, the additive impact of perceived elements of the neighborhood is greatest among those with the poorest level of lower body functioning. In contrast, less than 10% of those with the best lower body functioning reported difficulty walking two to three neighborhood blocks.
Discussion
The association between reduced lower body function and reported mobility disability among older adults is moderated by neighborhood factors, consistent with other studies in this area (Clarke et al., 2008; Clarke et al., 2009). Among older adults with poor lower body function, those perceiving their neighborhood as “walkable”, based on the number of walking destinations, time to destinations, and barriers to walking, were less likely to report mobility disability, as measured by difficulty in walking two to three neighborhood blocks. To recall, the interaction between lower body function and perceived primary building type (residential vs. mixed commercial) is not statistically significant at the p < .020, based the Bonferroni correction for multiple comparisons. Overall, the results suggest that there is less of a mobility disadvantage experienced by older adults with poor lower body function if they reside in a neighborhood perceived by them to be more “walkable.” Among older adults with good lower body function, however, their perceptions of the walkability of their neighborhood, as measured by the same set of factors, did not affect their reports of walking disability. Those demonstrating good lower body function were unlikely to report difficulty walking two to three neighborhood blocks, regardless of their place of residence. It is clear from Figures 1–4 that lower body function is more strongly associated with reported walking difficulty than are perceived neighborhood characteristics. Second, perceived neighborhood characteristics are most meaningful as a modifier of the relatively strong association between lower body function and reports of walking difficulty.
One study limitation is related to the subject population of community-dwelling older adults who were enrolled from senior-serving organizations. Accordingly, the study is not population-based, which may create bias toward the type of older adult common at such sites, including the possibility that they are healthier than older adults who are not affiliated with such sites. We attempted to offset this by ensuring that our recruitment sample targeted the variety of older adults at each senior center, including people who did not rate their health as good or excellent (22% of the sample rated their health as poor or fair). Our results, therefore, may not be generalizable to the entire older adult population in the United States, specifically a population that also includes more frail institutionalized older adults.
While the results of this study are also limited by a cross-sectional design, which precludes any consideration of causality, selection bias (in this case, selection of residential neighborhood based on level of walking), or even the temporal nature of the associations, there are a number of strengths, which should be noted. First, this examination was not limited to older adults living in a single community. The sample of older adults is derived from people residing in four different locations in the United States. Each area reflects a distinctive geographic and climatic area. Second, lower body function is based on direct measures of performance, that is, measures of balance, lower body strength, and walking speed. Third, measures of neighborhood characteristics are based on both GIS and self-report. In this study, only self-reported assessments of neighborhood elements, based on NEWS items, are associated with reports of difficulty walking two to three neighborhood blocks. It is possible that the three objective GIS measures used here were too crude to measure the elements of the objective environment most important to older adults. Street-level, objective measures, such as those used for neighborhood audits may be more appropriate in this regard (Kealey et al., 2005).
Future research should consider longitudinal examinations of the extent to which neighborhood factors moderate the association between lower body function and measures of walking. This should include a more detailed examination of the similarities and differences between self-reported and objective assessment of neighborhood factors. Objective measures, for example, as measured by GIS, may be too general and may not provide the detailed information provided by self-reports, which better reflect the residents’ current and past familiarity with neighborhood factors and the extent to which those factors are perceived by them as either facilitating or impeding walking. This research also should be conducted among diverse populations of older adults residing in different locations in the United States and elsewhere. Since most studies in the United States, including this study, are restricted to English-speaking respondents, it would be important to ensure wider coverage in future studies by including older adults who speak only languages other than English. Future studies should also include older adults recently diagnosed and treated for different types of chronic conditions as well as surveys of older adults from the general population. Studies of older adults with specific, newly diagnosed and treated conditions, such as cancer, will help to establish whether place of residence affects the timing, extent, and nature of recovery (Gomez et al., 2011). That research may lead to the development and evaluation of more place-based rehabilitation programs and hospital discharge planning protocols. There is also a need to clarify the reasons, that is, the biological, behavioral, and social mechanisms, for why specific neighborhood factors may serve to moderate the disabling effects of lower body limitations. As noted previously, this will require more detailed examinations of the relative significance of self-reported and objective measures of the neighborhood environment, including systematic assessments of whether the interaction between these neighborhood factors and lower body function varies by the type of mobility outcome as well as the neighborhood factors themselves. It is also necessary to begin to look beyond individual types of mobility, for example, walking, and begin to investigate the ease with which older adults use combinations of different types of mobility, for example, walking and driving, as part of their daily activities (Satariano et al., 2012). In the end, research of this kind will require a more precise assessment and conceptual understanding of the health effects of neighborhood residence over the life course.
Conclusion
If the results are confirmed in other, more sophisticated, longitudinal studies, there are important implications for public health promotion in aging populations. Environmental interventions may serve to moderate impairments, limitations, disabilities, and perhaps health care costs associated with a growing and increasingly diverse aging population. This may suggest new strategies (a) to better design neighborhoods, for example, through more informed building codes, and (b) to more effectively introduce older adults to the best features of their neighborhoods, for example, knowledge of and access to safe walking routes and other modes of mobility (Satariano et al., 2012). Finally, the results underscore the importance of the association between directly measured lower body function and self-reported difficulty in walking, and thus the need to continue to improve strategies to enhance the functional capacity of individuals, perhaps leading to innovative multilevel interventions that focus on both people and places (Satariano & McAuley, 2003).
Funding
This work was supported by a grant from the Robert Wood Johnson Foundation, Active Living Research Program (grant # 052515). The CDC Healthy Aging Research Network is a Prevention Research Centers program funded by the CDC Healthy Aging Program. We also used data from the RAND Center for Population Health and Health Disparities (CPHHD), which is funded by Grant 1-P50-ES012383 from the National Institute of Environmental Health Sciences.
Acknowledgments
It represents a collaboration of the CDC Healthy Aging Research Network. Efforts were supported in part by cooperative agreements from CDC’s Prevention Research Centers Program: U48-DP-000033, 001908, 000059, 001944, 000048, and 000025. The contents of this manuscript are solely the responsibility of the authors and do not necessarily represent the official views of the CDC.
References
- Andresen E. M. Malmgren J. A. Carter W. B., & Patrick D. L. (1994). Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). American Journal of Preventive Medicine, 10, 77–84. doi:10.1037/t10141-000 [PubMed] [Google Scholar]
- Balfour J. L., & Kaplan G. A. (2002). Neighborhood environment and loss of physical function in older adults: evidence from the Alameda County Study. American Journal of Epidemiology, 155, 507–515. doi:10.1093/aje/155.6.507 [DOI] [PubMed] [Google Scholar]
- Barnes D. Yaffe K. Satariano W., & Tager I (2003). A longitudinal study of cardiorespiratory fitness and cognitive function in healthy older adults. Geriatrics, 51, 459–465. doi:10.1046/j.1532-5415.2003.51153.x [DOI] [PubMed] [Google Scholar]
- Billick S. B. Siedenburg E. Burgert W. 3rd, & Bruni-Solhkhah S. M. (2001). Validation of the Mental Alternation Test with the Mini-Mental State Examination in geriatric psychiatric inpatients and normal controls. Comprehensive Psychiatry, 42, 202–205. doi:10.1053/comp.2001.23146 [DOI] [PubMed] [Google Scholar]
- Bland J. M., & Altman D. G (1995). Multiple significance tests: the Bonferroni method. BMJ, 310, 170 doi:10.1136/bmj.310.6973.170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerin E., Saelins B. E., Sallis J. F., Frank L. D. (2006). Neighborhood environment walkability scale: Validity and development of a short form. Medicine & Science in Sports & Medicine, 38, 1682–1691. doi:10.1249/01.mss.0000227639.83607.4d [DOI] [PubMed] [Google Scholar]
- Clark C. R. Kawachi I. Ryan L. Ertel K. Fay M. E., & Berkman L. F (2009). Perceived neighborhood safety and incident mobility disability among elders: the hazards of poverty. BMC Public Health, 9, 162 doi:10.1186/1471-2458-9-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P. Ailshire J. A. Bader M. Morenoff J. D., & House J. S (2008). Mobility disability and the urban built environment. American Journal of Epidemiology, 168, 506–513. doi:10.1093/aje/kwn185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P. Ailshire J. A., & Lantz P (2009). Urban built environments and trajectories of mobility disability: findings from a national sample of community-dwelling American adults (1986-2001). Social science & medicine (1982), 69, 964–970. doi:10.1016/j.socscimed.2009.06.041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke P., & George L. K (2005). The role of the built environment in the disablement process. American Journal of Public Health, 95, 1933–1939. doi:10.2105/AJPH.2004.054494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumbaugh E. (2008). Designing communities to enhance the safety and mobility of older adults a universal approach. Journal of Planning Literature, 23, 17–36. doi:10.1177/0885412208318559 [Google Scholar]
- Efron B. (1982). The jackknife, the bootstrap and other resampling plans. Philadelphia, PA: Society for Industrial and Applied Mathematics. [Google Scholar]
- Folstein M. F. Folstein S. E., & McHugh P. R (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. doi:10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- Gomez S. L., Glaser S. L., McClure L. A., Shema S. J., Kealey M., Keegan T. H., et al. (2011). The California Neighborhoods Data System: a new resource for examining the impact of neighborhood characteristics on cancer incidence and outcomes in populations. Cancer Causes & Control: CCC, 22, 631–647. doi:10.1007/s10552-011-9736-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong Y. Gallacher J. Palmer S., & Fone D (2014). Neighbourhood green space, physical function and participation in physical activities among elderly men: the Caerphilly Prospective study. The International Journal of Behavioral Nutrition and Physical Activity, 11, 40 doi:10.1186/1479-5868-11-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik J. M. Ferrucci L. Simonsick E. M. Salive M. E., & Wallace R. B (1995). Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. The New England Journal of Medicine, 332, 556–561. doi:10.1056/NEJM199503023320902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guralnik J. M., & Simonsick E. M (1993). Physical disability in older Americans. Journal of Gerontology, 48 Spec No, 3–10. doi:10.1093/geronj/48.Special_Issue.3 [DOI] [PubMed] [Google Scholar]
- Guralnik J. M., Simonsick E. M., Ferrucci L., Glynn R. J., Berkman L. F., Blazer D. G., et al. (1994). A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49, M85–M94. doi:10.1093/geronj/49.2.M85 [DOI] [PubMed] [Google Scholar]
- Hardy S. Kang Y. Studenski S., & Degenholtz H (2010). Ability to walk 1/4 mile predicts subsequent disability, mortality, and health care costs. Journal of General Internal Medicine, 26, 130–135. doi:10.1007/s11606-010-1543-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kealey M. Kruger J. Hunter R. Ivey S. Satariano W. Bayles C., …Williams K (2005). Engaging older adults to be more active where they live: Audit tool development. Preventing Chronic Disease: Public Health Research, Practice, and Policy, 2, 1–2. [Google Scholar]
- King D. (2008). Neighborhood and individual factors in activity in older adults: results from the neighborhood and senior health study. Journal of Aging and Physical Activity, 16, 144–170. [DOI] [PubMed] [Google Scholar]
- Krout J. A., Cutler S. J., Coward R. T. (1990). Correlates of senior center participation: a national analysis. The Gerontologist, 30, 72–79. doi:10.1093/geront/30.1.72 [DOI] [PubMed] [Google Scholar]
- Lawton M., & Nahemow L (1973). Ecology and the aging process. In Eisdorfer C., Lawton M. (Eds.), The psychology of adult development and aging (pp. 619–674). Washington, DC: American Psychological Association. [Google Scholar]
- Lawton M. P. (1986). Environment and aging (2nd ed). Albany, NY: Center for the Study of Aging. [Google Scholar]
- Lee I. M., & Buchner D. M (2008). The importance of walking to public health. Medicine and Science in Sports and Exercise, 40(7 Suppl), S512–S518. doi:10.1249/MSS.0b013e31817c65d0 [DOI] [PubMed] [Google Scholar]
- Li F. Fisher K. J. Brownson R. C., & Bosworth M (2005). Multilevel modelling of built environment characteristics related to neighbourhood walking activity in older adults. Journal of Epidemiology and Community Health, 59, 558–564. doi:10.1136/jech.2004.028399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagel C. L., Carlson N. E., Bosworth M., Michael Y. L. (2008). The relation between neighborhood built environment and walking activity among older adults. American Journal of Epidemiology, 168, 461–468. doi:10.1093/aje/kwn158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagi S. Z. (1976). An epidemiology of disability among adults in the United States. The Milbank Memorial Fund quarterly. Health and society, 54, 439–467. doi:10.2307/3349677 [PubMed] [Google Scholar]
- Plouffe L., Kalache A. (2010). Towards global age-friendly cities: determining urban features that promote active aging. Journal of Urban Health: bulletin of the New York Academy of Medicine, 87, 733–739. doi:10.1007/s11524-010-9466-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pope A. M., & Tarlov A. R (1991). Disability in America: toward a national agenda for prevention. Washington, DC: National Academies Press. [Google Scholar]
- R Development Core Team. (2013). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. Retrieved from http://www.R-project.org/ [Google Scholar]
- Reitan R. (1958). Validity of the Trail Making Test as an indicator of organic brain damage. Perceptual and Motor Skills, 8, 76 doi:10.2466/PMS.8.7.271-276 [Google Scholar]
- Rosow I., Breslau N. (1966). A Guttman health scale for the aged. Journal of Gerontology, 21, 556–559. doi:10.1093/geronj/21.4. 556 [DOI] [PubMed] [Google Scholar]
- Rothman K. J. (1990). No adjustments are needed for multiple comparisons. Epidemiology, 1, 43–46. doi:10.1097/00001648- 199001000-00010 [PubMed] [Google Scholar]
- Saelens B. E., Sallis J. F., Black J. B., Chen D. (2003). Neighborhood-based differences in physical activity: an environment scale evaluation. American Journal of Public Health, 93, 1552–1558. doi:10.1016/j.socscimed.2009.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satariano W. A., Guralnik J. M., Jackson R. J., Marottoli R. A., Phelan E. A., Prohaska T. R. (2012). Mobility and aging: new directions for public health action. American Journal of Public Health, 102, 1508–1515. doi:10.2105/AJPH.2011.300631 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satariano W. A., Ivey S. L., Kurtovich E., Kealey M., Hubbard A. E., Bayles C. M., et al. (2010). Lower-body function, neighborhoods, and walking in an older population. American Journal of Preventive Medicine, 38, 419–428. doi:10.1016/j.amepre.2009.12.031 [DOI] [PubMed] [Google Scholar]
- Satariano W. A., & McAuley E (2003). Promoting physical activity among older adults: From ecology to the individual. American Journal of Preventive Medicine, 25(3 Suppl. 2), 184–192. doi: 10.1016/S0749-3797(03)00183-1 [DOI] [PubMed] [Google Scholar]
- Satariano W. A., Ory M. G., Lee C. (2012). Planned and built environments in public health. In Prohaska T. R., Anderson L. A., Binstock R. H. (Eds.), Public health for an aging society (pp. 327). [Google Scholar]
- Selvin S. (1996). Statistical analysis of epidemiological data (2nd ed, Vol. 25). New York: Oxford University Press. [Google Scholar]
- Shumway-Cook A., Patla A., Stewart A., Ferrucci L., Ciol M. A., Guralnik J. M. (2003). Environmental components of mobility disability in community-living older persons. Journal of the American Geriatrics Society, 51, 393–398. doi:10.1046/j.1532-5415.2003.51114.x [DOI] [PubMed] [Google Scholar]
- Shumway-Cook A., Patla A. E., Stewart A., Ferrucci L., Ciol M. A., Guralnik J. M. (2002). Environmental demands associated with community mobility in older adults with and without mobility disabilities. Physical Therapy, 82, 670–681. [PubMed] [Google Scholar]
- Simonsick E. M. Guralnik J. M. Volpato S. Balfour J., & Fried L. P (2005). Just get out the door! Importance of walking outside the home for maintaining mobility: findings from the women’s health and aging study. Journal of the American Geriatrics Society, 53, 198–203. doi:10.1111/j.1532-5415.2005.53103.x [DOI] [PubMed] [Google Scholar]
- VanSwearingen J. M., & Brach J. S (2001). Making geriatric assessment work: selecting useful measures. Physical Therapy, 81, 1233–1252. [PubMed] [Google Scholar]
- Verbrugge L. M., & Jette A. M (1994). The disablement process. Social science & medicine (1982), 38, 1–14. doi:10.1016/0277- 9536(94)90294-1 [DOI] [PubMed] [Google Scholar]
- Wang Z., & Lee C (2010). Site and neighborhood environments for walking among older adults. Health & Place, 16, 1268–1279. doi:10.1016/j.healthplace.2010.08.015 [DOI] [PubMed] [Google Scholar]
- Yen I. H. Michael Y. L., & Perdue L (2009). Neighborhood environment in studies of health of older adults: a systematic review. American Journal of Preventive Medicine, 37, 455–463. doi:10.1016/j.amepre.2009.06.022 [DOI] [PMC free article] [PubMed] [Google Scholar]