Abstract
There is intense interest in developing novel methods for the sustained delivery of low levels of clinical therapeutics. MAX8 is a peptide-based beta-hairpin hydrogel that has unique shear thinning properties that allow for immediate rehealing after the removal of shear forces, making MAX8 an excellent candidate for injectable drug delivery at a localized injury site. The current studies examined the feasibility of using MAX8 as a delivery system for Nerve Growth Factor (NGF) and Brain-derived neurotrophic factor (BDNF), two neurotrophic growth factors currently used in experimental treatments of spinal cord injuries. Experiments determined that encapsulation of NGF and BDNF within MAX8 did not negatively impact gel formation or rehealing and that shear thinning did not result in immediate growth factor release. We found that increased NGF/BDNF dosages increased the amount and rate of growth factor release and that NGF/BDNF release was inversely related to the concentration of MAX8, indicating that growth factor release can be tuned by adjusting MAX8 concentrations. Encapsulation within MAX8 protected NGF and BDNF from in vitro degradation for up to 28 days. Released NGF resulted in the formation of neurite-like extensions in PC12 pheochromocytoma cells, demonstrating that NGF remains biologically active after release from encapsulation. Direct physical contact of PC12 cells with NGF-containing hydrogel did not inhibit neurite-like extension formation. On a molecular level, encapsulated growth factors activated the NGF/BDNF signaling pathways. Taken together, our data show MAX8 acts as a time-release gel, continually releasing low levels of growth factor over 21 days. MAX8 allows for greater dosage control and sustained therapeutic growth factor delivery, potentially alleviating side effects and improving the efficacy of current therapies.
Keywords: Hydrogel, Nerve growth factor, Brain-derived neurotrophic factor, MAX8
Introduction
Growth factor therapies, especially using nerve growth factor (NGF) and brain-derived neurotrophic factor (BDNF), are viewed as the most readily accessible clinical options for spinal cord injuries. Trophic factors have shown promise in regenerative strategies, and neurotrophins may enhance the implantation and differentiation rate of stem cell therapies used in regenerative medicine approaches to spinal cord injuries1. However, the high doses employed in such applications may lead to unwanted side effects and tend to dissipate very quickly, suggesting a need for a technological advance to deliver low doses of clinically relevant growth factors over an extended period of time. Adding growth factors to the site of injury is not enough to elicit functional recovery, as this approach results in a large bolus of growth factor with little sustained biological activity. For this reason, gel-based approaches to growth factor delivery have become an attractive approach2.
Broadly defined as a material made of a network of polymer chains that may be chemically or physically crosslinked with no flow behavior when in a steady state, hydrogels offer a solution to this problem. As a drug delivery vehicle, hydrogels provide an effective avenue for protein delivery and can improve therapeutic efficacy by providing a solubilizing environment in which proteins can be encapsulated and protected from degradation3, 4. The hydrogel network can be tailored to control the release rate and profile of the encapsulated macromolecule3, 5. Peptide-based hydrogels represent a further refinement and are customizable to allow for control over physical characteristics such as gelation time, desired fibrillar nanostructure, network stiffness, and ability to release macromolecules into the neighboring environment. Using peptides as building blocks for self-assembly allows one to make sequence specific modifications at the molecular level that ultimately influence the bulk properties of the self-assembled-hydrogel. Therefore, changes to the peptide sequence, which are accomplished easily by solid phase peptide synthesis or bacterial expression6, can be used to quickly fine tune material properties such as crosslink density, mesh size, hydrophilicity/electrostatics, and degradation rate7. Adjustments to solution conditions such as pH or salt concentrations also impact the final hydrogel properties such as stiffness, nanofibrillar structure and porosity allowing them to be assembled under physiological conditions conforming to their environment8–13. Because they are composed of amino acids, many peptide-based hydrogels can be assembled under physiological conditions. In contrast to methods that diffuse drugs/proteins into a preformed gel for delivery, resulting in difficulties in determining the ultimate concentration of encapsulated therapeutic, precise concentrations of therapeutics can be directly encapsulated into the gel network during the self-assembly process. As a class of biomaterials, peptides are extremely diverse due to the ability to change amino acid components to vary the size, chemical characteristics, and stiffness of the material being made. Peptide applications include tissue engineering, cell and structural scaffolds, drug delivery vehicles, 3D cell environments, and cell penetrating vehicles14–18.
To enable injection, most current therapeutic hydrogels are primarily designed to exist as a low viscosity polymer solution ex vivo and are crosslinked to create a gel in vivo through stimuli such as ultraviolet radiation, temperature, or chemical reaction14. While these approaches allow for the local administration of therapeutic agents, ultraviolet radiation or high temperatures caused by covalent crosslinking chemical reactions can damage cells or drug payloads mixed within the network-forming molecules. Because crosslinking occurs in vivo, these approaches suffer from unavoidable dilution from body fluids before and during crosslinking, resulting in ill-defined material properties of the resultant network, premature drug release or an initial bolus similar to what is seen in traditional drug administration19, 20. MAX8, the hydrogel used in the current study, contains two arms of alternating lysines and valines surrounding a 4 residue sequence VDPPT. The sequence of MAX8 imparts the ability to undergo triggered hydrogelation in response to physiological pH, temperature, and salt concentrations (ph 7.4, 150 mM NaCl or 25 mM HEPES) to form mechanically rigid, viscoelastic gels21. In pH 7.4 aqueous solutions at low ionic strength, MAX8 is freely soluble and unfolded due to electrostatic repulsions between the positively charged lysine side chains. Physiological salt concentrations screen the electrostatic repulsions between the lysine side chains, and the peptide folds into a β-hairpin structure stabilized by intramolecular hydrogen bonds13, 22. As a well-characterized, self-assembling, and hydrogelating β-hairpin peptide, MAX8 has several properties that make it an excellent candidate for development as injectable, multi-functional vehicle for therapeutic drug delivery. Specifically, when an appropriate shear stress is applied, MAX8 fractures and flows due to the physical crosslinking between fibrils23. The flowing material effectively results in edge domains that experience shear forces and an inner region protected from shear forces24. The presence of these two regions allow for shear thinning, while simultaneously protecting whatever is encapsulated from shear; MAX8 is able to immediately recover into a solid hydrogel when shear stress ceases21, 23. These properties of MAX8 result in a low-viscosity gel that immediately recovers its mechanical rigidity after the application of shear has ceased. These shear-thinning and self healing properties are maintained under physiologically relevant conditions, making MAX8 especially useful for delivery of encapsulated therapeutic payloads via syringe25.
We present data examining the feasibility of using MAX8 as a delivery vehicle for NGF and BDNF. Encapsulation of either NGF or BDNF resulted in a low, steady release into cell culture media after hydrogel injection; increased dosages of encapsulated NGF or BDNF increased the amount and rate of growth factor release. NGF/BDNF release was inversely related to the concentration of MAX8, indicating that altering MAX8 concentration is a way to fine-tune growth factor delivery. Encapsulation of NGF within MAX8 did not disrupt gelation, alter the ability of MAX8 to shear-thin, or create barriers to rehealing. The rat adrenal phaeochromocytoma PC12 cell line (a validated neuronal cell line model) develop neurite-like extensions in response to NGF released from MAX8, indicating that NGF remains biologically active after encapsulation within MAX8. Direct physical contact of PC12 cells with NGF-containing hydrogel did not inhibit neurite formation. Long-term studies showed that NGF or BDNF encapsulated within MAX8 remain biologically active 7–8 times longer than their respective in vitro half-lives in aqueous solution. MAX8 does not inhibit normal growth factor signaling as released NGF resulted in fibroblast proliferation and encapsulated NGF/BDNF resulted in Erk phosphorylation in PC12 cells. Taken together, our data suggest that MAX8 can serve as an injectable, time-release gel to deliver low levels of therapeutic proteins and growth factors at precise locations.
Experimental (Materials and methods)
Peptide synthesis
MAX8 peptide was synthesized on Rink amide resins with an automated AAPPTEC peptide synthesizer, using standard Fmoc-based solid phase peptide synthesis and purified to homogeneity as described21.
Preparation of MAX8 hydrogels
For the preparation of 0.5 wt% MAX8 hydrogel (0.5 mg MAX8 in 100 ml of hydrogel), MAX8 peptide was first dissolved in deionized (DI) water. Self-assembly of the peptide was initiated with the addition of an equal volume of salt solution buffered to pH 7.4 or cell growth media (Ph 7.4). Buffer solutions used to trigger the self-assembly varied according to the nature of measurements. Buffers used were either DMEM cell culture media without fetal bovine serum (FBS) (ionic strength ~161 mM) or 25 mM HEPES (pH 7.4). The same protocol, with appropriate volume changes, was used to prepare 1 wt% and 1.5 wt% gels.
Preparation of growth factor loaded hydrogels
NGF or BDNF (Peprotech, Rocky Hill NJ) was suspended in deionized water to make a 1 μg/μl stock solution, 100× more concentrated than the final growth factor concentrations in the hydrogels. The volume of growth factor stock solutions in hydrogels was fixed to 1% (v:v) for all growth factor-containing hydrogels. Before the peptide hydrogel encapsulation process, NGF or BDNF stock solutions were added to DMEM cell culture media to yield 2% (v:v) growth factor:cell culture media. For example, 2 μl of 1 μg/μl growth factor stock solution was added to 48 μl of aqueous cell culture media. 50 μl of this growth factor:cell culture media mixture was added to an appropriate peptide solution (0.5 μg MAX8 in 50 μl DI water) to yield 100 μl of 0.5 wt% MAX8 hydrogel loaded with 1 μg growth factor.
NGF and BDNF immunoenzyme assays
BDNF and NGF were encapsulated within MAX8 in 0.4 μm pore-size polyester transwells (Corning Incorporated, Corning, NY) and transferred to 24-well plates containing 1 mL serum-free DMEM. Media was harvested and replaced with fresh serum-free DMEM at various time points and frozen at −80 °C. Once all samples were collected, the Emax ImmunoAssay kit (Promega) was used to determine the amount of growth factor in each sample, following the manufacturer’s protocol. Briefly, after an overnight coating of a 96-well plate, NGF and BDNF was detected using an antibody sandwich format and a horseradish peroxidase-conjugated secondary antibody and a single-component 3,3′,5,5′-tetramentylbenzidine (TMB) substrate for the final chromogenic detection of bound neurotrophic factor. To determine the in vitro kinetics of NGF and BDNF release we divided the total amount of growth factor released by the number of hours since the growth factor loaded MAX8 was placed in DMEM. Average release rate was calculated by dividing the amount of released growth factor by the amount of time that had passed.
Cells and cell culture
PC12 pheochromocytoma cells were cultured as described26 with modifications. Briefly, PC12 cells were grown in Dulbecco’s modified Eagle’s Medium (DMEM), supplemented with 6% calf serum (HyClone Laboratories, Logan, UT), 6% horse serum (HyClone), glutamine (Gibco) and penicillin/streptomycin (Gibco). Cells were maintained at 37 °C in a humidified incubator with 5% CO2. Cells were serum starved for at least 18 hours before the addition of NGF. Before cells were plated, culture dishes were either treated with 100 μg/ml polylysine for 2hr, then rinsed twice with sterile PBS or coated with 100 μL 0.5 wt% MAX8 dissolved in 25mM HEPES buffer. Cells were plated at 1–2 × l04 cells/mL. Cells were cultured in a fully humidified 37°C incubator with a 5% CO2 atmosphere. In parallel experiments, 3T3 cells were allowed to adhere for one hour before a transwell containing NGF-loaded 0.5 wt% MAX8 was placed in the well. 24 hours later cells were trypsinized and counted on a hemacytometer.
PC12 cells in contact with NGF/BDNF hydrogels
NGF/BDNF loaded hydrogels were prepared with DMEM without FBS or phenol red (100 μl,0.5 wt% MAX8 with 1μg NGF or 1μg BDNF) were injected into the bottom of 8-chambered glass coverslips and incubated for 2 hours with 500 μL serum-free DMEM at 37 °C and 95% humidity. The next day, scaffolds were washed with DMEM and cells were seeded at 1.0 × 104 cells/cm2 in complete cell growth medium covering the hydrogel (day 0). Cells were observed daily for 11 days; Differential interference contrast (DIC) images were obtained throughout this period using a Leica TCS SP5 confocal microscope.
Oscillatory Rheology
Rheology measurements were obtained on an AR G2 rheometer from TA instruments with either a 20 mm or 8 mm diameter stainless steel parallel plate geometry. Samples were prepared as described previously25 with DMEM. After mixing the peptide solution with the buffer solution to trigger intramolecular folding and consequent self-assembly into a hydrogel, the samples were loaded immediately onto the temperature control peltier plate; 80 μl of MAX8 was used for the 8 mm plate and 170 μl of MAX8 was used for the 20 mm plate. The geometry was then quickly lowered to the gelling solution using a gap of 500 μm, mineral oil was added around the circumference of the geometry to prevent dehydration of the hydrogel, and data collection was initiated. Dynamic time sweep experiments (DTS) were performed to monitor the storage (G′) and loss (G″) modulus as a function of time (6 rad/s frequency, 0.2% strain) for 60 min. For shear-thinning experiments, the samples were subjected to 500 s−1 steady-state shear for 60 s after which oscillatory measurement was immediately performed at 6 rad/s frequency, 0.2% strain. Subsequently, recovery of the storage (G′) and loss (G″) modulus as a function of time was monitored for 30 min. Dynamic frequency (0.1–100 rad/s frequency, 1.0% strain) sweep experiments were performed to establish the frequency response of the samples. All measurements were held at 37°C and made in triplicate.
Microscopy
Cells grown on 8-chambered glass coverslips were incubated with NGF as indicated. DIC images were acquired with a Leica TCS SP5 laser-scanning confocal microscope using 20× and 40× objectives and LSM software (Leica Microsystems, Mannheim, Germany). At least 1000 cells were used for each condition during the quantification of biological responses to NGF.
Growth factor degradation experiments
100 ng of NGF or 100 ng of BDNF was added to 1 mL of serum-free DMEM and collected at various timepoints. In parallel experiments, 1 μg NGF or 1 μg BDNF was encapsulated within 0.5 wt% MAX8 in a transwell and moved to a well containing 1 mL serum-free DMEM. The media was collected and replaced with 1 mL of fresh serum-free DMEM at various timepoints and ELISA analyses determined the amount of growth factor remaining in the culture media. The amount of NGF and BDNF at these various timepoints was used to calculate the half-life of each growth factor.
Western blot analysis
For total cell lysates, cell pellets were lysed by boiling in 2x sodium dodecyl sulphate (SDS) sample buffer without Coomassie Blue containing 1 mM phenylmethylsulfonyl fluoride and 5 mg/ml of antipapain, leupeptin and pepstatin27, 28, 29. Lysate proteins (20 μg) were separated by SDS-polyacrylamide gel electrophoresis (SDS-PAGE) and transferred to nitrocellulose30. Membranes were blocked in 5% BSA in Tris-buffered saline with 0.1% Tween 20 (TBST), incubated overnight with primary antibody diluted in 5% bovine serum albumin (BSA)/TBST. Antibodies used in these experiments included phospho-ERK, total ERK, and β-actin (Cell Signaling, Beverly, MA). After incubation with HRP-conjugated secondary antibodies (Cell Signaling) in blocking solution, protein bands were visualized by Enhanced Chemiluminescence Plus (GE Healthcare, Piscataway, NJ).
Statistics
Mean values are shown with error bars indicating the SEM, unless indicated otherwise. Statistical analysis was performed by Student’s t test, where P < 0.05 denotes statistical significance.
Results and Discussion
Encapsulated NGF and BDNF are continuously released from MAX8
Previously, small molecules25 and macromolecules31, 32 have been encapsulated within MAX8, resulting in a slow, steady release of encapsulated components33. This current study tested if MAX8 could similarly deliver NGF and BDNF, two neurologic trophic growth factors critical to neurological regeneration34. To accomplish this, increasing concentrations of either NGF or BDNF were encapsulated within 100μL of 1.0 wt% MAX8 in a transwell. The transwells containing MAX8, MAX8 plus NGF, or MAX8 plus BDNF were then placed into a 24-well dish containing serum-free DMEM, and the supernatant was collected to determine the amount of NGF or BDNF present via enzyme-linked immunosorbent assay (ELISA). During these measurements, increased loading of either NGF (Figure 1A) or BDNF (Figure 1C) resulted in increased total amounts of growth factor released into the media. The initial rate of release of either growth factor also increased as greater amounts of either NGF (Figure 1B) or BDNF (Figure 1D) were encapsulated within 1.0 wt% MAX8. These data indicate that NGF or BDNF encapsulated within MAX8 was continuously released for at least 15 days, suggesting that MAX8 could potentially serve as a time-release gel for the in vivo delivery of NGF and BDNF.
Figure 1. Encapsulated NGF and BDNF is continuously released from MAX8.
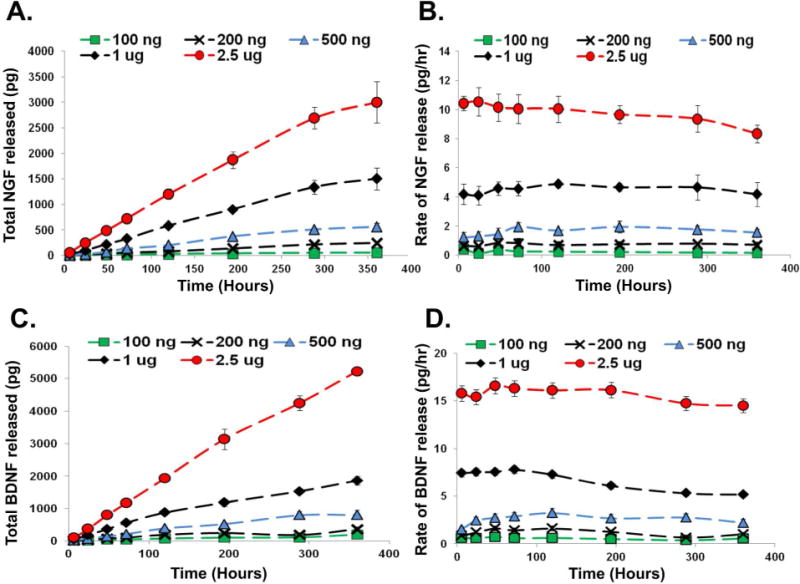
Various concentrations of either NGF (A, B) or BDNF (C, D) were encapsulated in 1.0 wt% MAX8. Media was sampled at the given intervals and the amount of growth factor released was measured by ELISA. Shown is the total amount (A, C) and rate (B, D) of growth factor release (n=3). Error bars represent the SEM for all experiments in this figure.
Growth factor release is tunable and dependent upon the concentration of MAX8
Increasing the concentration of MAX8 increases nanofibril concentration and leads to increased fibril crosslinking due to increased fibril branching and entanglement within the gel network35. Increase in peptide concentration also results in gels with smaller mesh sizes25. Thus, the adjustment of MAX8 concentration provides the ability to fine-tune the amount and rate of release of materials encapsulated within gel. Therefore, we next investigated how changes in MAX8 concentration changed both the total amount and rate of growth factor release. Either 1 μg of NGF or 1 μg of BDNF was encapsulated within 100 μL of 0.5, 1.0, or 1.5 wt% MAX8. We then placed the transwells into a 12-well dish containing serum-free DMEM and harvested the media to determine the amount of NGF or BDNF present via ELISA. Not surprisingly, the total amount of NGF released from MAX8 gels over the course of 15 days was dependant on the weight percent (w/v) MAX8, with 1.5-fold more NGF being released from a 0.5 wt% gel than 1.5 wt% MAX8 (Figure 2A). The 0.5 wt% gel released 1.3-fold more NGF than 1.0 wt% MAX8 1.0 (n=4; p<0.05). There was a similar inverse relationship between the rate of NGF released and the percent MAX8. Encapsulation of 1 μg NGF within 0.5 wt% MAX8 resulted in a steady NGF release rate of approximately 5 pg/hour (n=4; p<0.05), while encapsulation within 1.0 wt% MAX8 resulted in an average NGF release rate of 4.2 pg/hour; encapsulation within 1.5 wt% MAX8 resulted in an average NGF release rate of 2.9 pg/hour (Figure 2B; n=4, p<0.05). The total amount of BDNF released over the course of 15 days also varied with the concentration of MAX8, with 0.5 wt% MAX8 releasing 1.4 times as much BDNF than 1.0 wt% MAX8 and 2.1 times as much BDNF as 1.5 wt% MAX8 on day 15 (Figure 2C). The rate of BDNF release followed the same trend, with encapsulation of 1 μg BDNF within 0.5 wt% MAX8 resulting in an average of 9.5 pg/hour of BDNF released; 1.0 wt% MAX8 resulted in an average of 7.5 pg/hour of BDNF released and 1.5 wt% MAX8 resulted in 5.3 pg/hour of BDNF released (Figure 2D). These data indicate that the release of NGF or BDNF can be tuned by adjusting the concentration of MAX8 the growth factors are encapsulated within.
Figure 2. Encapsulated NGF and BDNF release is dependent upon the concentration of MAX8.
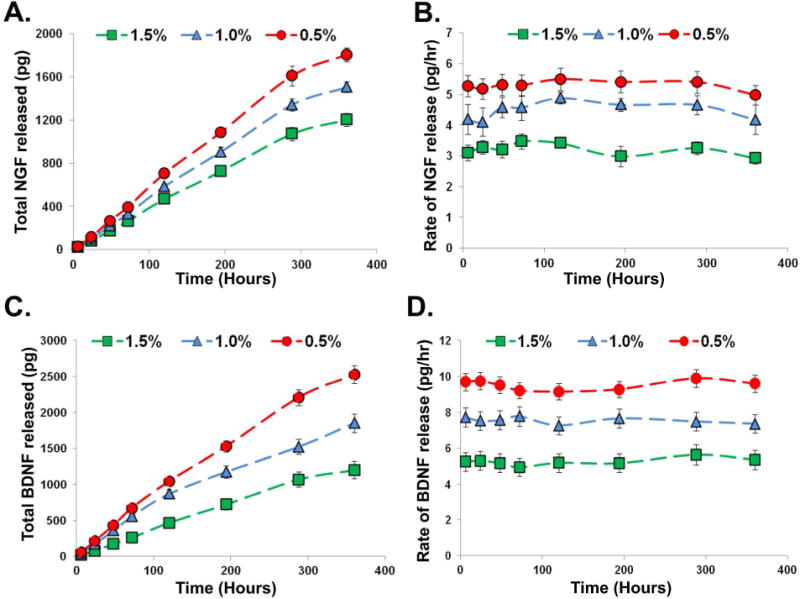
1 μg of either NGF (A, B) or BDNF (C, D) was encapsulated in 0.5 wt%, 1.0 wt%, or 1.5 wt% MAX8. Media was sampled at the given intervals and the amount of growth factor released was measured by ELISA. Shown is the total amount (A, C) and rate (B, D) of growth factor release (n=3–4). Error bars represent the SEM for all experiments in this figure.
Physical properties of MAX8 do not change after NGF encapsulation
To examine if the sheer forces present within a syringe during injection would affect growth factor release, 1 μg NGF or 1 μg BDNF was encapsulated within 0.5 wt% MAX8. After gelation, MAX8 or MAX8 containing encapsulated NGF or BDNF was delivered using a 20-gauge needle to the bottom of an Eppendorf tube containing 1mL serum-free DMEM. The supernatant was collected and the quantity of growth factor released was quantified via ELISA analysis. Less than 3 percent of encapsulated NGF or BDNF was released immediately into the surrounding media. Therefore, injection through a needle did not significantly increase these levels from previously studied gels formed directly in transwells (Figures 3A, B). To verify that growth factor encapsulation did not alter the physical properties of MAX8, we performed oscillatory rheology experiments comparing 0.5 wt% MAX8 to 0.5 wt% MAX8 containing 1 μg of NGF. An initial time sweep was performed in which the MAX8 is set with or without NGF, respectively. The presence of growth factor does not significantly influence the ability of MAX8 to gel (Figures 4A, B). After 60 minutes, the gels were disrupted using shear and a second time sweep was done to monitor rehealing. As determined during a time sweep, NGF encapsulation did not alter the ability of MAX8 to shear thin or reheal (Figure 4A, B). Frequency sweeps were also performed and showed that 0.5 wt% MAX8 containing 1 μg NGF had similar gel-like properties to control MAX8 (Figures 4C, D).
Figure 3. Shear thinning does not result in release of encapsulated NGF.
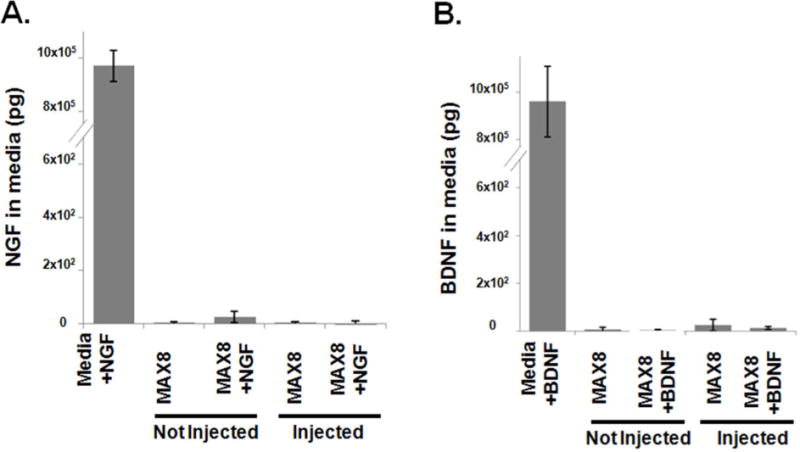
1 μg of either NGF (A) or BDNF (B) was added directly to media or encapsulated within 0.5 wt%MAX8. MAX8 or MAX8 containing NGF/BDNF was allowed to gel before media was added or MAX8 or MAX8 containing NGF/BDNF was delivered via syringe into a well containing media; media was harvested after 5 minutes and growth factor release was quantified by ELISA. Error bars represent the SEM for all experiments in this figure.
Figure 4. Physical properties of MAX8 do not change after NGF encapsulation.
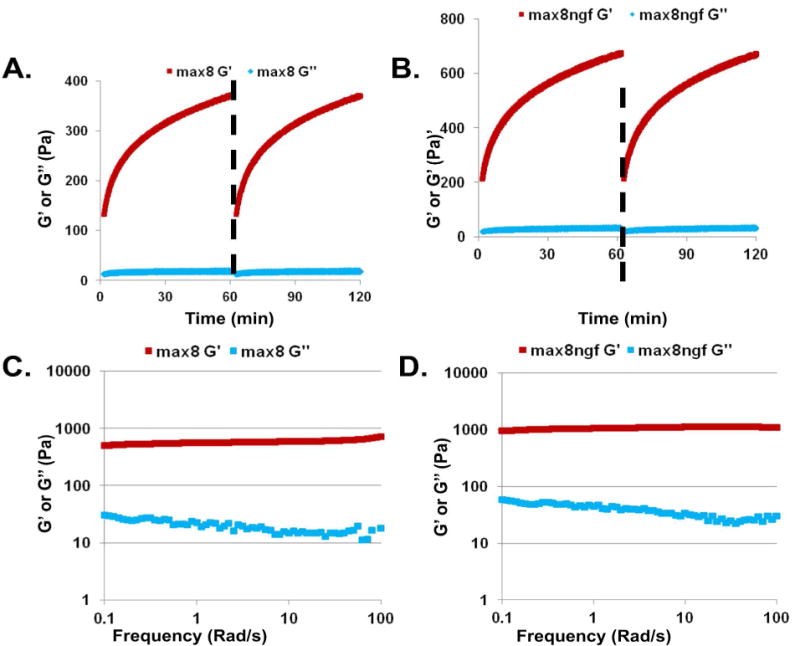
Time sweep using oscillatory rheology to monitor the effects of NGF encapsulation (1μg) on gel formation (G′ and G″) of 1 wt% MAX8 before (A) and after (B) shear was applied. A dashed line represents when shear was applied. G′ after 180 seconds was 293 ± 68 for MAX8 and 479 ± 63 for MAX containing NGF for initially assembled gels; G′ 180 seconds after shearing was 350 ± 66 for MAX8 and 572 ± 48 for MAX8 containing NGF. Frequency sweep of 1.0 wt% MAX8 encapsulated without (C) or with (D) 1μg NGF using oscillatory rheology. At 1 rad/s, G′ was 805±186 for MAX8 and 1334±143 for MAX8 containing NGF.
PC12 cells extend neurite-like extensions in response to NGF encapsulated within MAX8
We next investigated if released NGF and BDNF could elicit in vitro biological responses using the PC12 cell line, a clonal cell line derived from a rat pheochromocytoma36. In this experiment, NGF was delivered from a MAX8 gel contained in a transwell insert and cells were not in contact with the gel. PC12 cells project long, neurite-like extensions in response to 50–100 ng/mL NGF in as little as one day, and maximal neurite projections occur after 7–9 days in culture37. As shown in Figure 5A, PC12 cells cultured in the absence of NGF had a rounded morphology. Although some adherent cells appeared to extend pseudopodia, none were as long as the length of a PC12 cell body (Figure 5A). Therefore, in subsequent quantification experiments, cells were only deemed positive for neurite-like extensions if the extensions were longer than the size of the cell body (Figure 5B). Typical cell culture experiments use 50–100 ng NGF every 3 days to culture. Because encapsulation within MAX8 releases a very low level of NGF (Figure 1), we chose to encapsulate 1μg NGF in these experiments. PC12 cells developed an extensive network of neurite-like extensions after being cultured for 7 days in the presence of 1 μg NGF encapsulated within 0.5 wt% MAX8, similar to what occurred when 100 ng/ml NGF was added to PC12 cell media (Figures 5A, 5B). This data confirms that encapsulated NGF remains biologically active. Although NGF was added every 2–4 days in control experiments (NGF in basal media lacking MAX8), the media was never changed in samples containing encapsulated NGF, suggesting that encapsulation within MAX8 resulted in a continuous release of biologically active NGF. Collectively, these data suggest that encapsulation within 0.5 wt% MAX8 does not change the ability of NGF to differentiate PC12 cells and that the NGF is protected for up to 7 days when encapsulated within 0.5 wt% MAX8.
Figure 5. PC12 cells develop neurite-like extensions in response to NGF released from MAX8.
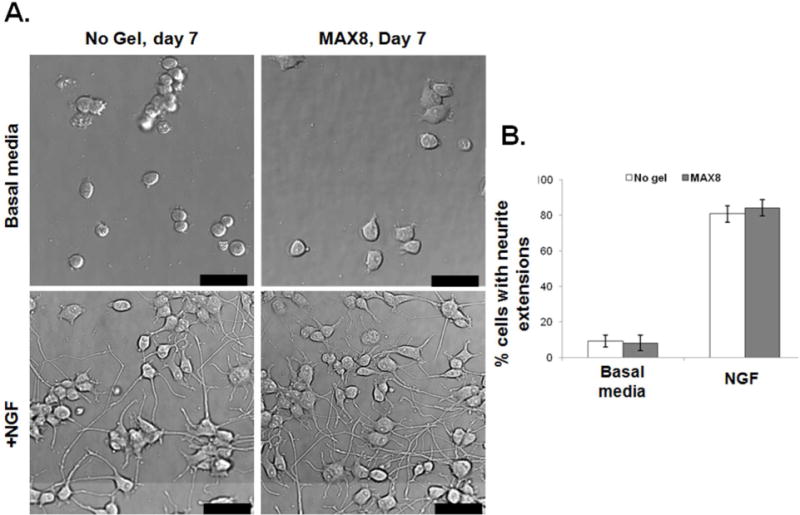
(A) Transwells containing 0.5% MAX8 with and without 1 μg encapsulated NGF were added to PC12 cells. Media was not replaced during this experiment and cells were imaged after 7 days. Shown are representative images; bars represent 50 μm. (B) Images from three separate experiments were analyzed and the number of cells with neurite-like extensions were recorded. Error bars represent the SEM for all experiments in this figure.
PC12 cells extend neurite-like extensions while in direct contact with MAX8
The properties of supporting substrates, including surface biochemistry, topography (type, size, organization, and geometry of nanostructures), and mechanical properties provide extracellular cues that influence cellular phenotypes including cellular adhesion and differentiation state of neuronal and hematopoietic progenitor cells38, 39. With this in mind, we examined if physical contact with MAX8 changes the biological response of PC12 cells to encapsulated NGF. In these experiments, we coated the bottom of an 8-chambered Nunc chamber with 100 μL of 0.5 wt% MAX8 containing either 1μg NGF or DI water (vehicle control). PC12 cells were then allowed to adhere on top of the MAX8 and were visualized by differential interference contrast (DIC) microscopy at the indicated timepoints. We found that contact with MAX8 alone did not extend processes longer than their cell body (Figure 6A), while PC12 cells in contact with 0.5 wt% MAX8 containing 1μg NGF began forming what appeared to neurite-like extensions as early as 1 day later although none of these extensions were longer than the cell body (data not shown). While PC12 cells did not form neurite-like extensions without the addition of NGF regardless of the presence or absence of MAX8, after 3 days 67 percent of PC12 cells growing on top of MAX8 containing encapsulated NGF had formed neurite-like extensions in response to NGF treatment (Figures 6A, B). After 7 days in culture, 76 percent of cells cultured on top of 0.5 wt% MAX8 containing 1 μg encapsulated NGF formed neurite-like extensions, indicating that direct contact with MAX8 did not perturb the formation of NGF-induced neurite extensions (Figure 6C). There were no statistical differences between PC12 cells cultured on top of NGF-containing MAX8 and control experiments where NGF was supplemented directly into the media (p = 0.333 after 3 and p = 0.627 after 7 days in culture). These data support the hypothesis that direct contact with MAX8 does not inhibit the response of PC12 cells to NGF, suggesting that MAX8 may be biocompatible for in vivo neurotrophic growth factor delivery.
Figure 6. PC12 cells extend neuron-like processes while in direct contact with MAX8.
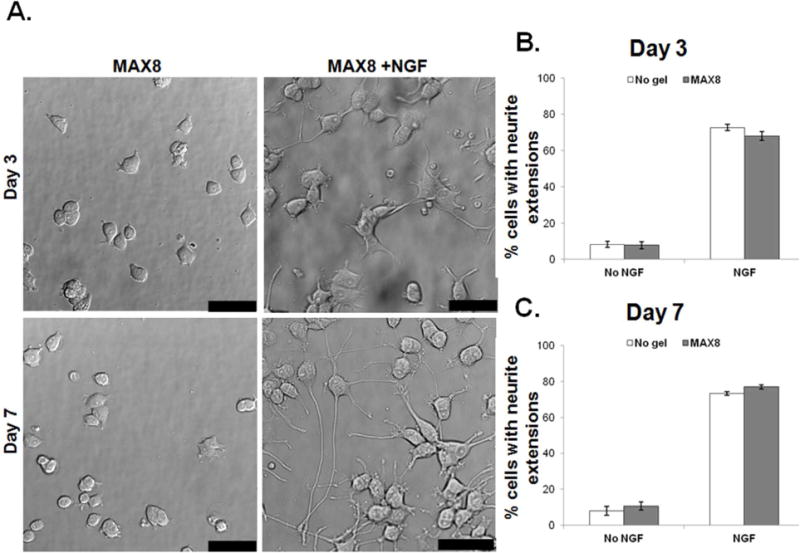
(A) NUNC chamber slides were coated with either 0.5 wt% MAX8 or 0.5 wt% MAX8 containing 1μg NGF. PC12 cells were allowed to adhere on top of the MAX8 gel and imaged at the given intervals. Shown are representative images; bar represents 25 μm. After 3 (B) or 7 (C) days images were analyzed for neurite-like extensions. Error bars represent the SEM for all experiments in this figure.
MAX8 containing encapsulated NGF results in biological activity PC12 neurite-like extension formation after 28 days in continuous culture
The maintenance of neurite-like extensions has been shown by others to depend upon the continued presence of NGF, as NGF-differentiated PC12 cells withdrawn from NGF lose their neurites within 2 days (data not shown;26). Typical long-term cell culture experimental protocols call for the addition of NGF every 2–3 days, roughly equivalent to the half-life of NGF (Figure 7C). Our data suggests that MAX8 allows for the slow, steady release of NGF. To test if the released NGF remains biologically active after an extended time of encapsulation, 0.5 wt% MAX8 containing either encapsulated 1 μg NGF or no encapsulated NGF was placed into a transwell, allowed to gelate, and left in 24-well dish containing media for either 14 or 21 days. The transwell containing MAX8 was then transferred to new wells containing serum-starved (16 hours) PC12 cells, and the cells were analyzed for possible neurite-like extensions for an additional week. During these experiments, 88 percent of PC12 cells continued to extend and maintain neurite-like extensions 21 days after the NGF was encapsulated within MAX8; 86 percent of PC12 cells extended neurite-like extensions after 28 days (Figures 7A, B). Next, we wanted to investigate how the amount of factor released from MAX8 compared to a single growth factor treatment injected directly into cell culture media. NGF or BDNF was either encapsulated within MAX8 or added directly to media and subjected to ELISA analyses to determine the amount of remaining NGF. The amount of NGF and BDNF present in the media remained remarkably constant for at least 21 days for samples containing growth factors encapsulated within MAX8 (Figure 7C). Conversely, the levels of NGF and BDNF were almost undetectable from background after 18 days when NGF or BDNF were added as a single bolus at the beginning of the experiment (Figure 7C). During these experiments, the half-life of unencapsulated NGF was approximately 3.5 days and the half-life of unencapsulated BDNF was approximately 3.4 days. These data confirm that MAX8 containing encapsulated NGF results in biological activity PC12 neurite-like extension formation after 28 days in continuous culture, and that NGF and BDNF are steadily released after encapsulation within 0.5 wt% MAX8.
Figure 7. Encapsulated NGF released from MAX8 is biologically active for up to 28 days.
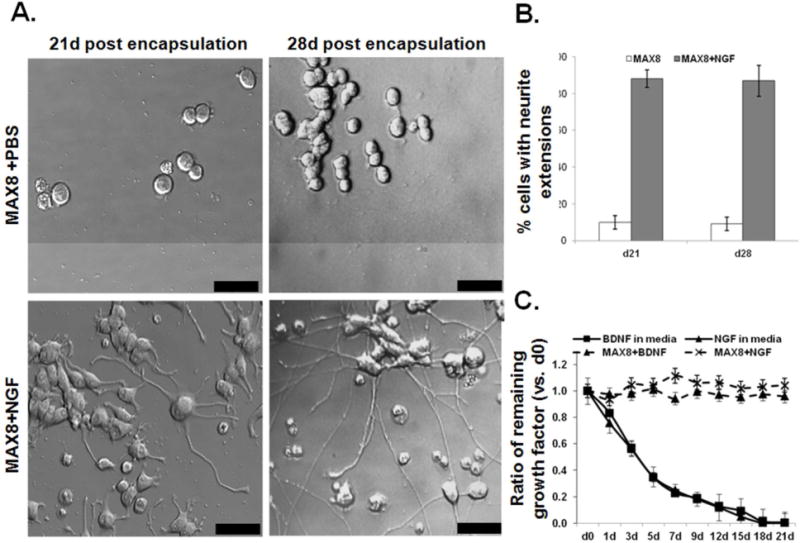
(A) NGF encapsulated within MAX8 was released for 14 or 21 days before the gels were moved to wells containing PC12 cells. 1 week later cells were imaged. Shown are representative images; bars represent 25 μm. (B). Images from three separate experiments were analyzed for PC12 cells with neurite-like extensions. (C) 1 μg of NGF or BDNF was encapsulated within 0.5 wt% MAX8 or 1 μg of NGF or BDNF was added directly to serum free media. Media was collected at various intervals and the amount of growth factor was determined by ELISA analyses. The ratio of growth factor (compared to d0) is shown. Error bars represent the SEM for all experiments in this figure.
Encapsulation within MAX8 does not disrupt growth factor signaling
Our data show PC12 cells extending neurite extensions in response to NGF encapsulated within 0.5 wt% MAX8 and strongly suggest that encapsulated NGF is able to release from the gel into the local milieu in a biologically active form. To verify this hypothesis, control 3T3 mouse embryonic fibroblast cells, which proliferate in response to biologically active NGF40, were cultured in the presence of NGF either in the media (Figure 8A) or encapsulated within MAX8 (Figure 8B). Confirming that NGF released from MAX8 elicits biological responses from an additional cell line, 3T3 cells showed a dose-response to NGF encapsulated within MAX8 and proliferated between 17 and 35 percent more than untreated cells, similar to 3T3 cells treated with unencapsulated NGF (Figures 8A, B). To verify that encapsulated NGF and BDNF resulted in activation of signaling pathways downstream of each growth factor receptor, either DI water, 1 μg NGF, or 1 μg BDNF was encapsulated within a 0.5 wt% MAX8 gel, allowed to gelate within a transwell, and moved to well containing media. After 24 hours, the media was harvested and moved to a new well containing serum-starved PC12 cells. After 1 hour, cells were lysed to isolate total protein. Encapsulated NGF resulted in increased levels of phosphorylated ERK in PC12 cells indicating, that the NGF signaling pathway was activated (Figure 8C). Together, these experiments show that encapsulated and released NGF and BDNF is biologically active.
Figure 8. Encapsulation within MAX8 does not disrupt growth factor signaling.
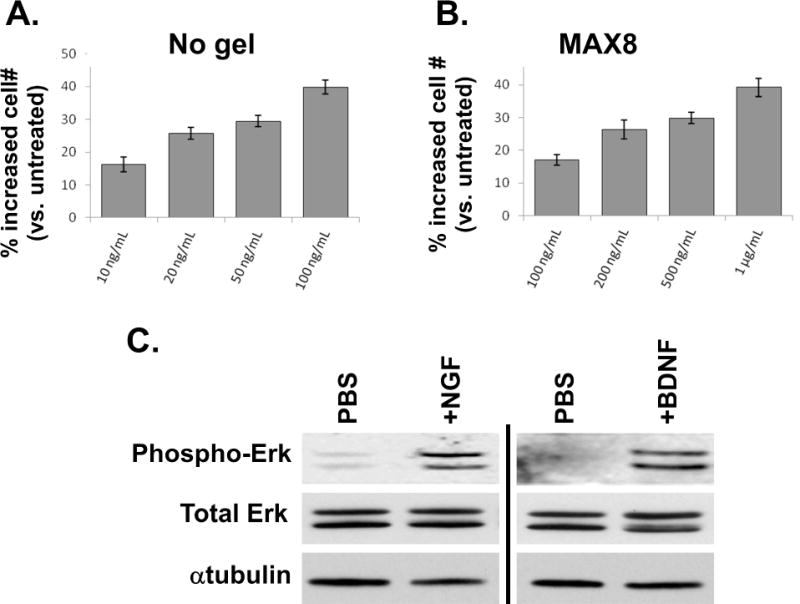
Serum-starved 3T3 cells were allowed to adhere in a 24-well dish for one hour before the addition of either deinoized water or 1μg NGF (A) or transwells containing 0.5 wt% MAX8 plus DI water or 1μg NGF (B). Cells were counted 24 hours later. (C) Media collected from transwells containing 0.5 wt% MAX8 plus DI water or 1 μg NGF were added to serum-starved PC12 cells. Cell lysates were harvested after 1 hour and used in Western analyses. Error bars represent the SEM for all experiments in this figure.
Conclusions
Hydrogels provide an effective means to deliver proteins and provide a stabilizing environment in which encapsulated proteins are protected from degradation, potentially resulting in improved therapeutic efficacy3–5, 32. The hydrogel network can be tailored to control the total amount and/or release rate of encapsulated macromolecules3, 5, 41. Additionally, adjusting hydrogel pore size allows for the slow diffusion and subsequent release of proteins encapsulated within the gel, while simultaneously providing temporal control of the release. The ability to fine-tune therapeutic delivery is especially important to applications wseeking to deliver neurotrophic growth factors, where duration and dosage are critical concerns. Interestingly, we saw PC12 cells form neurite-like extensions from low doses of released NGF (Figures 5, 6, and 7). This may be partially due to increased NGF protection while within the gel or that proximity to the gel made higher concentrations of growth factor unnecessary and is similar to decreased effective doses we have published when curcumin is encapsulated within MAX825. Future experiments will strive to better define the mechanism of this phenomenon.
The structure and properties of an encapsulated protein greatly influences its release from an injectable peptide hydrogel. Although similar in size, we found that encapsulation of BDNF within MAX8 resulted in an increased amount and rate of BDNF release compared to when NGF was encapsulated within MAX8 (Figure 1). This should not be surprising given that proteins and antibodies have distinct surface compositions that impart solubility and charge differences that influence their controlled release32, 42. Depending on a protein’s isoelectric point (pI) and the pH of the solution, a given protein will have a net positive (pI > pH), a neutral (pI = pH), or negative (pI < pH) charge displayed on its surface. The net charges of encapsulated macromolecules interact with the net charges within a hydrogel, resulting in either a repulsive force that hastens release if the net charges are similar or an attractive force that retards release if their charges are opposite32. Because MAX8 has a net positive charge at pH7.4, repulsive forces will aid in the release of proteins with a net positive charge like NGF (net charge of +5) and BDNF (net charge +10) from the hydrogel. Importantly, our data also suggests that the release profiles of encapsulated proteins can be further fine-tuned to form electrostatic interactions with the diffusing protein as a means to control their release43, 44.
Here, we present data examining the feasibility of using MAX8, a peptide-based beta-hairpin hydrogel, as a delivery vehicle for the clinically relevant neurotrophic growth factors NGF and BDNF. Encapsulation of NGF or BDNF resulted in a low, steady release of growth factors into cell culture media and we found that increased dosages of NGF or BDNF increased the amount and rate of growth factor release. NGF/BDNF release was inversely related to the concentration of MAX8, indicating that altering MAX8 concentration could be a way to fine-tune growth factor delivery. Encapsulation of NGF within MAX8 did not negatively impact gel formation, alter the ability of MAX8 to be shear-thin delivered by syringe and immediate recover into a solid hydrogel. PC12 cells developed neurite-like extensions in response to NGF released from MAX8, suggesting that NGF remains biologically active after encapsulation within MAX8. Direct physical contact of PC12 cells with NGF-containing hydrogel did not inhibit neurite formation. Long-term studies showed that NGF encapsulated within MAX8 remains biologically active for longer than 28 days, much longer than the 3.4 day half-life of NGF or 4.1 day half life of BDNF in aqueous solution (Figure 7C). MAX8 does not inhibit normal growth factor signaling, as released NGF resulted in fibroblast proliferation and encapsulated NGF/BDNF resulted in Erk phosphorylation in PC12 cells. Taken together, our data suggest that MAX8 can serve as an injectable time-release gel to deliver low levels of therapeutic proteins and growth factors at precise locations. Acting as a time-release gel, this new application for MAX8 allows for greater dosage control and sustained therapeutic delivery, potentially alleviating side effects and improving the efficacy of current growth factor therapies.
Acknowledgments
This work was supported in part by Award Number NIGMS-8P20GM103464-0 (SL and SAL) from the National Institute of General Medical Sciences of the National Institutes of Health, the American Cancer Society Grant Number RSG-09-021-01-CNE (SAL), and funds from the Nemours Foundation (SL and SAL). DJP and SS would like to thank funding from the UD-NIST Center for Neutron Scattering under cooperative agreement 70NANB12H239 from NIST, U.S. Department of Commerce. The statements, findings, conclusions and recommendations are those of the author(s) and do not necessarily reflect the view of NIST or the U.S. Department of Commerce.
Footnotes
Conflict of Interest Disclosure
The authors declare no competing financial interest.
References
- 1.Awad BI, Carmody MA, Steinmetz MP. Potential Role of Growth Factors in the Management of Spinal Cord Injury. World Neurosurg. 2013 doi: 10.1016/j.wneu.2013.01.042. [DOI] [PubMed] [Google Scholar]
- 2.Macaya D, Spector M. Injectable hydrogel materials for spinal cord regeneration: a review. Biomed Mater. 2012;7(1):012001. doi: 10.1088/1748-6041/7/1/012001. [DOI] [PubMed] [Google Scholar]
- 3.Branco MC, Schneider JP. Self-assembling materials for therapeutic delivery. Acta Biomater. 2009;5(3):817–31. doi: 10.1016/j.actbio.2008.09.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kobsa S, Saltzman WM. Bioengineering approaches to controlled protein delivery. Pediatr Res. 2008;63(5):513–9. doi: 10.1203/PDR.0b013e318165f14d. [DOI] [PubMed] [Google Scholar]
- 5.Lin CC, Metters AT. Hydrogels in controlled release formulations: network design and mathematical modeling. Adv Drug Deliv Rev. 2006;58(12–13):1379–408. doi: 10.1016/j.addr.2006.09.004. [DOI] [PubMed] [Google Scholar]
- 6.Sonmez C, Nagy KJ, Schneider JP. Design of self-assembling peptide hydrogelators amenable to bacterial expression. Biomaterials. 2015;37:62–72. doi: 10.1016/j.biomaterials.2014.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Segers VF, Lee RT. Local delivery of proteins and the use of self-assembling peptides. Drug Discov Today. 2007;12(13–14):561–8. doi: 10.1016/j.drudis.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 8.Schneider JP, Pochan DJ, Ozbas B, Rajagopal K, Pakstis L, Kretsinger J. Responsive hydrogels from the intramolecular folding and self-assembly of a designed peptide. J Am Chem Soc. 2002;124(50):15030–7. doi: 10.1021/ja027993g. [DOI] [PubMed] [Google Scholar]
- 9.Pochan DJ, Schneider JP, Kretsinger J, Ozbas B, Rajagopal K, Haines L. Thermally reversible hydrogels via intramolecular folding and consequent self-assembly of a de novo designed peptide. J Am Chem Soc. 2003;125(39):11802–3. doi: 10.1021/ja0353154. [DOI] [PubMed] [Google Scholar]
- 10.Micklitsch CM, Medina SH, Yucel T, Nagy-Smith KJ, Pochan DJ, Schneider JP. Influence of Hydrophobic Face Amino Acids on the Hydrogelation of β-Hairpin Peptide Amphiphiles. Macromolecules. 2015;48(5):1281–1288. doi: 10.1021/ma5024796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rajagopal K, Ozbas B, Pochan DJ, Schneider JP. Probing the importance of lateral hydrophobic association in self-assembling peptide hydrogelators. Eur Biophys J. 2006;35(2):162–9. doi: 10.1007/s00249-005-0017-7. [DOI] [PubMed] [Google Scholar]
- 12.Rajagopal K, Lamm MS, Haines-Butterick LA, Pochan DJ, Schneider JP. Tuning the pH responsiveness of beta-hairpin peptide folding, self-assembly, and hydrogel material formation. Biomacromolecules. 2009;10(9):2619–25. doi: 10.1021/bm900544e. [DOI] [PubMed] [Google Scholar]
- 13.Ozbas B, Rajagopal K, Schneider JP, Pochan DJ. Semiflexible chain networks formed via self-assembly of beta-hairpin molecules. Phys Rev Lett. 2004;93(26 Pt 1):268106. doi: 10.1103/PhysRevLett.93.268106. [DOI] [PubMed] [Google Scholar]
- 14.Li Y, Rodrigues J, Tomas H. Injectable and biodegradable hydrogels: gelation, biodegradation and biomedical applications. Chem Soc Rev. 2012;41(6):2193–221. doi: 10.1039/c1cs15203c. [DOI] [PubMed] [Google Scholar]
- 15.Tavano L, Vivacqua M, Carito V, Muzzalupo R, Caroleo MC, Nicoletta F. Doxorubicin loaded magneto-niosomes for targeted drug delivery. Colloids Surf B Biointerfaces. 2013;102:803–7. doi: 10.1016/j.colsurfb.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 16.Collier JH, Segura T. Evolving the use of peptides as components of biomaterials. Biomaterials. 2011;32(18):4198–204. doi: 10.1016/j.biomaterials.2011.02.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L, Teller S, Clifton RJ, Jia X, Kiick KL. Tunable mechanical stability and deformation response of a resilin-based elastomer. Biomacromolecules. 2011;12(6):2302–10. doi: 10.1021/bm200373p. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agrawal CM, Ray RB. Biodegradable polymeric scaffolds for musculoskeletal tissue engineering. J Biomed Mater Res. 2001;55(2):141–50. doi: 10.1002/1097-4636(200105)55:2<141::aid-jbm1000>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 19.Hatefi A, Amsden B. Biodegradable injectable in situ forming drug delivery systems. J Control Release. 2002;80(1–3):9–28. doi: 10.1016/s0168-3659(02)00008-1. [DOI] [PubMed] [Google Scholar]
- 20.Farokhzad OC, Langer R. Impact of nanotechnology on drug delivery. ACS Nano. 2009;3(1):16–20. doi: 10.1021/nn900002m. [DOI] [PubMed] [Google Scholar]
- 21.Haines-Butterick L, Rajagopal K, Branco M, Salick D, Rughani R, Pilarz M, Lamm MS, Pochan DJ, Schneider JP. Controlling hydrogelation kinetics by peptide design for three-dimensional encapsulation and injectable delivery of cells. Proc Natl Acad Sci U S A. 2007;104(19):7791–6. doi: 10.1073/pnas.0701980104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pakstis LM, Ozbas B, Hales KD, Nowak AP, Deming TJ, Pochan D. Effect of chemistry and morphology on the biofunctionality of self-assembling diblock copolypeptide hydrogels. Biomacromolecules. 2004;5(2):312–8. doi: 10.1021/bm034249v. [DOI] [PubMed] [Google Scholar]
- 23.Yan C, Altunbas A, Yucel T, Nagarkar RP, Schneider JP, Pochan DJ. Injectable solid hydrogel: mechanism of shear-thinning and immediate recovery of injectable beta-hairpin peptide hydrogels. Soft Matter. 2010;6(20):5143–5156. doi: 10.1039/C0SM00642D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sathaye S, Mbi A, Sonmez C, Chen Y, Blair DL, Schneider JP, Pochan DJ. Rheology of peptide-and protein-based physical hydrogels: Are everyday measurements just scratching the surface? Wiley Interdiscip Rev Nanomed Nanobiotechnol. 2015;7(1):34–68. doi: 10.1002/wnan.1299. [DOI] [PubMed] [Google Scholar]
- 25.Altunbas A, Lee SJ, Rajasekaran SA, Schneider JP, Pochan DJ. Encapsulation of curcumin in self-assembling peptide hydrogels as injectable drug delivery vehicles. Biomaterials. 2011;32(25):5906–14. doi: 10.1016/j.biomaterials.2011.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Drubin DG, Feinstein SC, Shooter EM, Kirschner MW. Nerve growth factor-induced neurite outgrowth in PC12 cells involves the coordinate induction of microtubule assembly and assembly-promoting factors. J Cell Biol. 1985;101(5 Pt 1):1799–807. doi: 10.1083/jcb.101.5.1799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lindsey S, Jiang J, Woulfe D, Papoutsakis ET. Platelets from mice lacking the aryl hydrocarbon receptor exhibit defective collagen-dependent signaling. J Thromb Haemost. 2014;12(3):383–94. doi: 10.1111/jth.12490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lindsey S, Papoutsakis ET. The aryl hydrocarbon receptor (AHR) transcription factor regulates megakaryocytic polyploidization. Br J Haematol. 2011;152(4):469–84. doi: 10.1111/j.1365-2141.2010.08548.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lindsey S, Huang W, Wang H, Horvath E, Zhu C, Eklund EA. Activation of SHP2 protein-tyrosine phosphatase increases HoxA10-induced repression of the genes encoding gp91(PHOX) and p67(PHOX) J Biol Chem. 2007;282(4):2237–49. doi: 10.1074/jbc.M608642200. [DOI] [PubMed] [Google Scholar]
- 30.Lee SJ, Lindsey S, Graves B, Yoo S, Olson JM, Langhans SA. Sonic hedgehog-induced histone deacetylase activation is required for cerebellar granule precursor hyperplasia in medulloblastoma. PLoS One. 2013;8(8):e71455. doi: 10.1371/journal.pone.0071455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Branco MC, Pochan DJ, Wagner NJ, Schneider JP. Macromolecular diffusion and release from self-assembled beta-hairpin peptide hydrogels. Biomaterials. 2009;30(7):1339–47. doi: 10.1016/j.biomaterials.2008.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Branco MC, Pochan DJ, Wagner NJ, Schneider JP. The effect of protein structure on their controlled release from an injectable peptide hydrogel. Biomaterials. 2010;31(36):9527–34. doi: 10.1016/j.biomaterials.2010.08.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Altunbas A, Pochan DJ. Peptide-based and polypeptide-based hydrogels for drug delivery and tissue engineering. Top Curr Chem. 2012;310:135–67. doi: 10.1007/128_2011_206. [DOI] [PubMed] [Google Scholar]
- 34.Boyce VS, Mendell LM. Neurotrophins and spinal circuit function. Front Neural Circuits. 2014;8:59. doi: 10.3389/fncir.2014.00059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yucel T, Micklitsch CM, Schneider JP, Pochan DJ. Direct Observation of Early-Time Hydrogelation in beta-Hairpin Peptide Self-Assembly. Macromolecules. 2008;41(15):5763–5772. doi: 10.1021/ma702840q. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Greene LA, Tischler AS. Establishment of a noradrenergic clonal line of rat adrenal pheochromocytoma cells which respond to nerve growth factor. Proc Natl Acad Sci U S A. 1976;73(7):2424–8. doi: 10.1073/pnas.73.7.2424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Connolly JL, Greene LA, Viscarello RR, Riley WD. Rapid, sequential changes in surface morphology of PC12 pheochromocytoma cells in response to nerve growth factor. J Cell Biol. 1979;82(3):820–7. doi: 10.1083/jcb.82.3.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Jiang J, Papoutsakis ET. Stem-cell niche based comparative analysis of chemical and nano-mechanical material properties impacting ex vivo expansion and differentiation of hematopoietic and mesenchymal stem cells. Adv Healthc Mater. 2013;2(1):25–42. doi: 10.1002/adhm.201200169. [DOI] [PubMed] [Google Scholar]
- 39.Migliorini E, Ban J, Grenci G, Andolfi L, Pozzato A, Tormen M, Torre V, Lazzarino M. Nanomechanics controls neuronal precursors adhesion and differentiation. Biotechnol Bioeng. 2013;110(8):2301–10. doi: 10.1002/bit.24880. [DOI] [PubMed] [Google Scholar]
- 40.Oger J, Arnason BG, Pantazis N, Lehrich J, Young M. Synthesis of nerve growth factor by L and 3T3 cells in culture. Proc Natl Acad Sci U S A. 1974;71(4):1554–8. doi: 10.1073/pnas.71.4.1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Annabi N, Tamayol A, Uquillas JA, Akbari M, Bertassoni LE, Cha C, Camci-Unal G, Dokmeci MR, Peppas NA, Khademhosseini A. 25th anniversary article: Rational design and applications of hydrogels in regenerative medicine. Adv Mater. 2014;26(1):85–123. doi: 10.1002/adma.201303233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Lee M, Chen TT, Iruela-Arispe ML, Wu BM, Dunn JC. Modulation of protein delivery from modular polymer scaffolds. Biomaterials. 2007;28(10):1862–70. doi: 10.1016/j.biomaterials.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 43.Gelain F, Unsworth LD, Zhang S. Slow and sustained release of active cytokines from self-assembling peptide scaffolds. J Control Release. 2010;145(3):231–9. doi: 10.1016/j.jconrel.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 44.Koutsopoulos S, Unsworth LD, Nagai Y, Zhang S. Controlled release of functional proteins through designer self-assembling peptide nanofiber hydrogel scaffold. Proc Natl Acad Sci U S A. 2009;106(12):4623–8. doi: 10.1073/pnas.0807506106. [DOI] [PMC free article] [PubMed] [Google Scholar]


