Abstract
Goal
To describe and validate a non-contacting sensor that used reflected ultrasound to separately monitor respiratory, non-respiratory, and caretaker movements of infants.
Methods
An In-Phase and Quadrature (I&Q) detection scheme provided adequate bandwidth, in conjunction with post-detection filtering, to separate the 3 types of movement. The respiratory output was validated by comparing it to the electrical activity of the diaphragm (Edi) obtained from an infant ventilator in 11 infants. The non-respiratory movement output was compared to movement detected by miniature accelerometers attached to the wrists, ankles, and heads of 7 additional infants. Caretaker movement was compared to visual observations annotated in the recordings.
Results
The respiratory rate determined by the sensor was equivalent to that from the Edi signal. The sensor could detect the onset of inspiration significantly earlier than the Edi signal (23+/−69ms). Non-respiratory movement was identified with an agreement of 0.9 with the accelerometers. It potentially interfered with the respiratory output an average of 4.7+/− 4.5% and 14.9+/1 15% of the time in infants not requiring or on ventilatory support, respectively. Caretaker movements were identified with 98% sensitivity and specificity. The sensor outputs were independent of body coverings or position.
Conclusion
This single, non-contacting sensor can independently quantify these three types of movement.
Significance
It is feasible to use the sensor as trigger for synchronizing mechanical ventilators to spontaneous breathing, to quantify overall movement, to determine sleep state, to detect seizures, and to document the amount and effects of caretaker activity in infants.
Keywords: accelerometer, caretaker, electrical activity of the diaphragm, infant, in-phase and quadrature detection. movement, non-contacting sensor, respiratory monitor, ultrasound
I. Introduction
The most common methods for measuring respiratory activity involve contacting systems, such as impedance plethysmography or an attachment of a sensor of flow to the airway. Non-contacting methods are useful when no contact is desired or possible. These include the use of pressure mattresses [1], radar [2], infrared imaging of warm expired gas [3], ultrasound methods of detecting airflow at the face [4], or reflected ultrasound from the underside of a mattress [5]. Non-contacting sensors are especially useful for sleep apnea detection, and have been used in infants for synchronization of a mechanical ventilator with spontaneous breathing efforts even when a patient has an artificial airway or must wear nasal prongs with large leaks in the airway-infant interface [6]. In this latter application, the most important characteristic is the accurate and rapid detection of the onset of inspiration [7]. This is because infants with respiratory distress have respiratory rates of 60-120/minute and inspiratory times of approximately 300ms. The trigger for synchronizing the ventilator must assist early in inspiration to produce increased and more consistent tidal volumes [8].
All systems for monitoring respiratory activity, both contacting and non-contacting, are limited by artifacts of non-respiratory and caretaker movements. Extensive efforts in the development of these systems have been made to eliminate these artifacts. Non-respiratory and caretaker movements that produce the artifacts, however, provide useful clinical information. Overall movement is an indicator of well-being, as patients with increased levels of tumor necrosis factor-alpha have lethargy and reduced movement [9], is useful for determining the stage of sleep [10] and documenting patient comfort and agitation, and has potential for assessing the neurodevelopment of infants [11], [12]. Caretaker movement is important in assessing the physiological response to handling of infants, and to document the amount of care the infant is receiving.
The purpose of this paper is to describe and validate a single, non-contacting sensor that can reliably detect respiratory, non-respiratory, and caretaker movements as separate channels of information. Furthermore, we assessed the ability of the sensor to detect the onset of inspiration to demonstrate the feasibility of the use of the sensor respiratory movement output to synchronize a mechanical ventilator with the infant's spontaneous breathing effort.
II. Methods
A) Description of the Sensor, Circuitry, and Algorithm
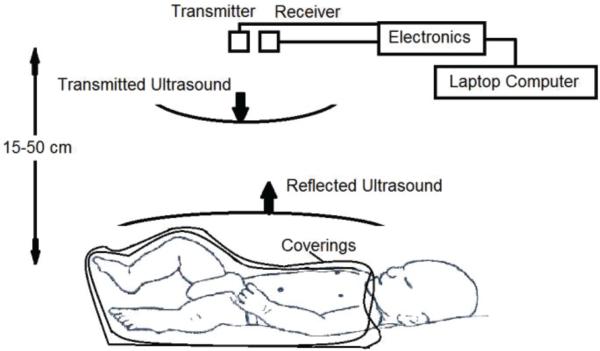
The basic system is shown in Figure 1. The sensor head consisted of a transmitter and a receiver placed 15-50 cm above the infant, approximately centered over the torso of the infant, mounted either on the ceiling of the isolette with silicone suction cups, or on a bracket attached to an open crib or radiant warmer bed. The sensor could be moved several centimeters toward the head or the toes without a change in function. The infant was nursed in the usual coverings or bundled in blankets. The sensor head was attached to an electronics unit by shielded cables, and data were acquired with a laptop computer.
Figure 1.
Diagram of the sensor and the infant.
The transmitter emitted a 40 kHz continuous ultrasound (half-angle 20 degrees,) that insonated the head and torso of the infant. The frequency of 40 kHz was chosen because of the excellent propagation of the ultrasound, the efficient reflection off the infant, and since the transmitter and receiver transducers are readily available. Even with the coverings, less than 1% of the ultrasound energy was absorbed, and this was approximately three orders of magnitude less than the safety standards for workers exposed to ultrasound [13]. This ultrasound was above the range of human hearing, and did not disturb the infant or the caretaker.
The receiver in the sensor head transduced the ultrasound that was reflected off the infant. Movement of the infant caused the reflected signal to have a slight shift in its phase with respect to the transmitted signal, due to the Doppler Effect. This phase shift was detected by the electronics, based on an in-phase and quadrature demodulation (I&Q) scheme that allowed the detection of the phase shift over several wavelengths in an unambiguous fashion. This detection scheme was not limited in bandwidth, so that an algorithm could be developed to process the signals and to give three separate outputs, 1) the respiratory waveform, 2) non-respiratory movement of the infant, and 3) movement of caretakers that were in the field of view of the insonated infant and the receiver.
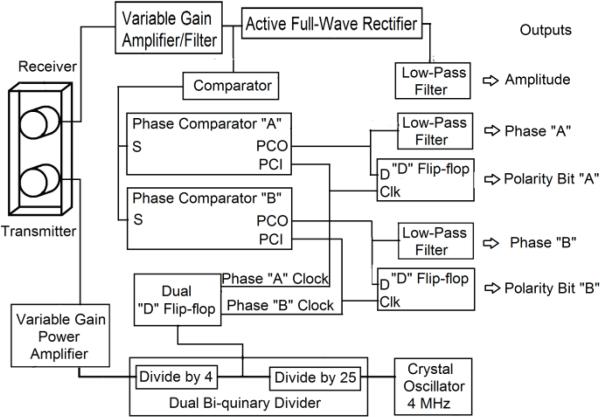
A functional block diagram of the system is shown in Fig. 2. All logic functions were implemented using standard TTL components. The transmitter was driven by a variable gain amplifier whose input was a 40 kHz square wave derived by a 100:1 division of a crystal-controlled oscillator operating at 4MHz. The 4 MHz signal was also divided by a bi-quinary divider to produce a 160 kHz square wave that was in-phase with the transmitter signal that was used for the reference signals for the phase detection. The 160 KHz signal was processed by the dual D-flip-flop to produce an in-phase Clock signal (Phase A Clock), and a quadrature phase signal which lagged the in-phase signal by 90 degrees (Phase B Clock) at 40 kHz, that were used for the I&Q detection system of the received reflected signal as shown in Fig. 3(a).
Figure 2.
Functional block diagram of the sensor hardware system.
Figure 3.
Reference and output signals of the electronics in the I&Q detection scheme.
The receiver was connected to a variable gain amplifier/filter that amplified the received 40 KHz signal several thousand-fold. This signal was presented to a comparator that converted the signal into logic levels “0” or “1.” The output of the comparator was connected simultaneously to the inputs of Phase A and Phase B Comparators. The clock inputs to Phase A and Phase B Comparators were the in-phase Phase A clock and the quadrature Phase B Clock, respectively.
The phase comparator outputs (PCO) of the Phase A Comparator and Phase B Comparators were each connected to a low-pass filter, which were resistor-capacitor networks with a time constant of 0.1 ms that provided a smoothed output of the phase of the received signal with respect to the transmitted signal. The phase comparator outputs were also connected to D-flip-flops that were clocked by the respective phase clock signals. These flip-flops detected the polarity of the phase of the received signal zero-crossing from the comparator outputs, and produced Polarity Bits A and B. These polarity bits were used to decode the two phases.
The waveforms of this process are shown in Fig. 3(b) to demonstrate the sensor outputs as a reflector is moved toward the sensor. Movement of the reflector through one wavelength (approximately 0.9cm) represents 360 degrees of phase shift for the reflected signal with respect to the transmitted signal. Thus, in Fig. 3(b), the X-axis represents the signal changes for a 360 phase shift, or the movement of the reflector toward the sensor through approximately 0.9cm. The waveforms of this process are shown in Fig. 3(b) to demonstrate the sensor outputs as a reflector is moved toward the sensor. Movement of the reflector through one wavelength (approximately 0.9cm) represents 360 degrees of phase shift for the reflected signal with respect to the transmitted signal. This translated into an output change of 10V, giving the sensor a potential sensitivity of several microns of movement.
Thus, in Fig. 3(b), the X-axis represents the signal changes for a 360-degree phase shift, or the movement of the reflector toward the sensor through approximately 0.9cm.
Polarity Bit A changes from 0 to 1 at the beginning of the movement, with Polarity Bit A set to logic level 1 until one-half wavelength of movement. With further movement toward the sensor, the Phase A signal decreases, with the Polarity Bit A changing from logic level 1 to 0 to indicate the object is moving toward the sensor with decreasing Phase A output. At the beginning of the movement, Phase B is decreasing, with the Polarity Bit B set to 0, until a quarter wavelength of movement (corresponding to 90 degrees phase difference) and then increases, with Polarity Bit B changing to 1, indicating movement toward the sensor. In both the Phase A and B signals, the range of the smoothed phase outputs is that of the power supply (0 to 5VDC).
The electronic circuit was devised to have two phase outputs and two polarity bit outputs so that the direction of movement could be unambiguously tracked across wavelengths by the I&Q detector. Phase A and Phase B comparators were the type I comparators of the CD4046 integrated circuit (Fairchild Semiconductors, Inc., San Jose, CA) that had a specification for linearity from 0.5 to 4.5 volts. These values were subsequently used in the decoding algorithm described below. The information from both phase outputs, corrected by the Polarity Bits, is identical, except that when either Phase output A or B are near the limit of their range, above 4.5V or below 0.5V, there was little change in the voltage output for the change in the phase angle, which led to a low signal to noise ratio. Therefore, to produce the respiratory output from these four signals, only the specified range of linear operation of the comparators was used so as to eliminate noise. Since the difference in the phase between the outputs is fixed at 90 degrees, one or the other is always in their usable range.
The flow chart of the algorithm used to create the respiratory waveform from these four inputs is shown in Fig. 4. The Phase A, Phase B, and Polarity Bits A and B are inputs to the algorithm. If Phase A is in the usable range (0.5 to 4.5v), it is used, otherwise Phase B is used. The Phase signal chosen is then differenced and used, or inverted if Polarity Bit A or Polarity Bit B is zero. The selected Phase, once corrected by the corresponding Polarity Bit, is accumulated to produce the respiratory output signal.
Figure 4.
Algorithm for determining the respiratory output signal by the use of the I&Q detection scheme. Respiratory movement was calculated from the appropriate phase signal that was chosen based on the amplitude in the linear range, which was differentiated and corrected by the polarity bit, and then accumulated. Movement was detected as the quotient of the power in the band pass filter (BPF) and the low pass filter (LPF) after smoothing.
Non-respiratory movement was detected directly from the Phase A output. As can be seen in Fig. 3(b), movement through a single wavelength of the ultrasound produces a full-scale excursion of the phase signals. These movements produced a high-frequency component to the phase output that was filtered and used as an indication of movement. In preliminary experiments, we have found that movement could be defined as a separate output from the sensor by computing the power in the Phase A signal in the range of 28-33Hz and normalizing it to the power of the Phase A signal in the range of DC-5Hz. Prior to taking the quotient, we smoothed the power function with a 200-point moving average window filter to reduce noise. The resulting ratio of power is a dimensionless number that is a continuous indication of movement that can resolve movements of approximately 200ms duration.
B. Validation Process
1) Signals for Comparison
Signals from the sensor and those for comparison in the validation were acquired with a commercially available data acquisition system (MP-150 hardware system with HLT-100 isolated input module (BioPac Inc., Goleta, CA)) that was controlled by a software system that provided real-time graphical display and stored data in files on a laptop computer (Acknowledge software, Version 4.3, BioPac Inc., Goleta, CA). All analog signals for comparison to the sensor were acquired from all channels simultaneously at a rate of 1000samples/s per channel, graphically displayed in real time, and stored in files on a laptop computer. During data acquisition, annotations were added to the recording to document patient status, changes in the experimental set-up, and episodes of caretaker movement. The acquired data was redisplayed graphically, and the above algorithms were performed within the Acknowledge software system using standard routines on the stored data.
a) Respiratory effort
We compared the sensor respiratory output, to the electrical activity of the diaphragm, or Edi, as determined by a commercially available mechanical ventilator (Servo-i, Maquet Corporation, Solna, Sweden) as an independent reference for respiratory effort. A plug-in module in the ventilator detected the electromyogram of the diaphragm from a feeding tube (5.5 Fr diameter) that had nine built-in microelectrodes that were flush with the surface and connected to the ventilator with thin cables in the feeding tube. Proprietary software in the ventilator combined differential EMG signals picked up by pairs of the microelectrodes to produce one signal that represented the Edi [14], [15]. A utility software package in the Servo- i was used to export data in real time through an RS-232 port, in conjunction with an external software package (Servo Tracker, Maquet Corporation, Solna, Sweden) that provided the Edi, airway pressure and flow as voltages for recording via a digital to analog converter (National Instruments, Model USB-6212 BNC) at a rate of 100 samples/s. We tested a step response in airway pressure as detected by an independent pressure transducer, and found a delay time of 10ms maximum in this system.
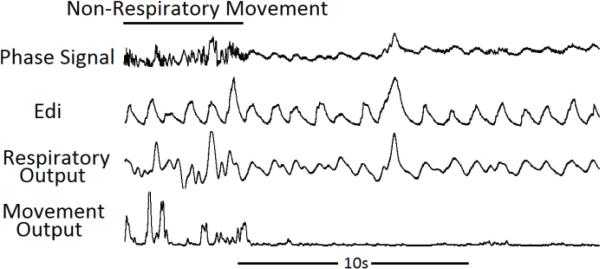
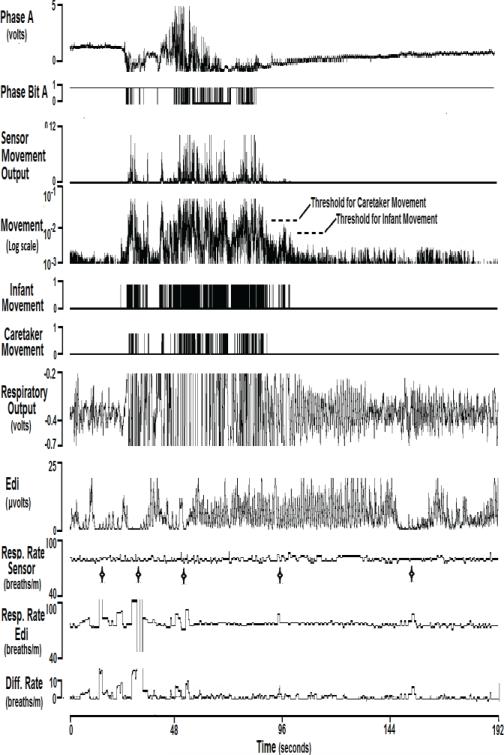
The phase signal of the sensor, Edi, and respiratory and movement output of the sensor are shown in Figure 5. The high frequency components in the sensor phase signals were associated with movement, and resulted in the excursions of the movement signals in the first 6 seconds of the record. This high frequency component represents the received signal passing through several wavelengths in a short period of time due to the speed of the movement of the head and limbs. The sensor movement output reflected the non-respiratory movements and was well correlated in time.
Figure 5.
Output of the phase signal of the sensor, Edi for comparison, and the sensor respiratory and movement output in a 900g infant. The high-frequency component in the first part of the recording of the SENSOR phase signal corresponded to non-respiratory movement of the infant that was not detected by the Edi signal. During movement, there was some distortion of the respiratory output of the sensor.
b) Non-respiratory movement
We compared the sensor movement output of the algorithm to non-respiratory movements as detected by an independent system of miniature accelerometers. Each accelerometer was a 3-axis MEM chip (Model MMA7340LT, sensitivity 440mv/g, Freescale Semiconductors, Tempe, AZ) that was encapsulated in an epoxy housing 6.7×3.3×10mm, and weighed less than 200mg, including the cable. The accelerometers were fixed to the wrists and ankles with Velcro straps, and head movement was detected with an accelerometer taped to a cap worn by the infant. The signals from the 3 axes of each accelerometer were AC- coupled (time-constant= 0.05sec) through a buffer amplifier with a 200Hz low-pass filter, and the absolute values for each axis were obtained through an active rectifier and summed so as to provide a single signal that reflected both acceleration of the device and changes in its orientation to the Earth's gravitation field. The summed signal from each of the five accelerometers attached to the four limbs and head were then summed, so that a single signal represented any non-respiratory movement in any of the accelerometers. The accelerometer system was calibrated to a full-scale of 2.2V for 1g, for the sum of the five accelerometers. The absolute zero-g voltage of the summed signal was tested by recording the output of the entire accelerometer system during a free-fall through 0.5m, during which time the system reached equilibrium at 0g. The smallest detectable movement from any accelerometer was approximately 50mg, corresponding to a signal of about 22 mv in the summed signal.
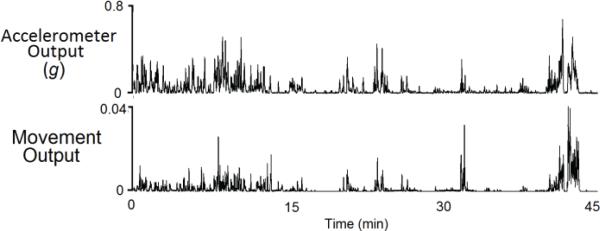
Fig. 6 shows a one-hour recording of the sensor movement output and the output of the accelerometer system in a 1750g infant. There was good visual correlation of the two signals.
Figure 6.
The accelerometer system output and the movement output of the sensor for comparison. The signals were well correlated in time.
c) Movement of the caretaker
It was appreciated early in the development of the sensor that movement of hands of a caretaker between the subject and the sensor produced large excursions of the non-respiratory movement output. This was due to the more rapid movement of the hands than the limbs of the infant, and a skipping wavelengths when a new target of the reflected signal was received. During the recordings, we made annotations in the Acknowledge system for periods of time when the caretaker was handling the infants, for comparison in subsequent analysis.
2) Patient Studies
The validation was performed in two clinical protocols. Both were approved by the UCSD Institutional Review Board, and infants were enrolled after written, informed parental consent was obtained. All infants were in stable clinical condition, and the clinical team in charge of their care approved of performing the studies. The description of the infants and the clinical conditions of the studies is shown in Table I.
TABLE I.
Infant Characteristics and Clinical Conditions.
| Infant # | Ethnic/Sex1 | Study Wt. (g) | Study age (days) | Record length (min) | Conditions2 |
|---|---|---|---|---|---|
| Infants in Protocol 1 | |||||
| 1 | H/M | 2070-2100 | 53,55 | 249 | Open crib, SU,SC |
| 2 | AA/F | 940 | 17 | 99 | Isolette, SB |
| 3 | AA/F | 1395-1740 | 32-44 | 558 | Isolette, SU,PB |
| 4 | H/F | 1380-1410 | 35-37 | 489 | Isolette, SU,SC,SB,PB,PC |
| 5 | C/M | 810-900 | 15-22 | 827 | Isolette, PC,PB |
| 6 | H/M | 1010-1050 | 39-42 | 532 | Isolette, SB |
| 7 | H/M | 1160-1230 | 47-51 | 336 | Isolette, PB,SC |
| 8 | C/M | 1430-1500 | 13-17 | 485 | Isolette, PB,SB |
| 9 | H/M | 1145-1185 | 25-28 | 907 | Isolette, PB,SB |
| 10 | C/M | 1120 | 48 | 281 | Isolette, PB,SB |
| 11 | A/M | 1270-1275 | 38 | 639 | Isolette, PB,SB |
| Total | 5402 | ||||
| Infants in Protocol 2 | |||||
| 12 | C/M | 1330, 1750 | 43 | 155 | Open crib, SC,SU,PC,PU |
| 13 | C/F | 1140 | 18 | 42 | Isolette SC,SU,PC,PU |
| 14 | H/M | 3250 | 13 | 104 | Open crib, SC,SU,PC,PU |
| 15 | C/M | 3008 | 26 | 66 | Open crib, SC,SU,PC,PU |
| 16 | C/M | 2220, 2680 | 58 | 107 | Open crib, SC,SU,PC,PU |
| 173 | H/M | 3388 | 21 | 41 | Open crib, SC,SU,PC,PU |
| 18 | H/F | 2200 | 85 | 105 | Isolette, SC,SU,PC,PU |
| Total | 620 | ||||
C=Caucasian, H=Hispanic, AA=African-American M=Male, F=Female
SC=Supine, covered, SU=Supine, uncovered, SB= Supine, bundled PC=Prone, covered, PU=Prone, uncovered, PB=Prone, bundled
Infant #17 with narcotic withdrawal
a) Protocol 1
This protocol was devised to validate and characterize the respiratory output of the sensor. For this protocol we studied eleven infants who were requiring non-invasive respiratory support with continuous positive airway pressure (CPAP) or synchronized intermittent mandatory ventilation (SIMV) applied by nasal prongs. These infants were chosen because they were on respiratory support provided by Servo-i ventilator that also provided the Edi signal for comparison to the respiratory output of the sensor. Infants were studied in the usual coverings, consisting of blankets and bundling, in both the supine and prone positions. We performed 29 recordings (1-3 studies in each infant) of 45 to 249 minutes duration for a total time of 5402 minutes. To compare the respiratory rates obtained from the sensor to that obtained from the Edi, segments of the files that did not contain caretaker movement were chosen for analysis. We determined the accuracy of detection of the onset of inspiration by the sensor compared to the Edi by choosing other 10- minute segments wherein there was little or no ventilatory support. To assess the overall amount of movement that could potentially interfere with the respiratory signal, the entire length of the original recordings was used.
b) Protocol 2
The second protocol was devised to validate the separation of non-respiratory and caretaker movement from the respiratory output of the sensor. We studied seven infants who were active and vigorous, and who were not requiring ventilatory support. We chose them to represent a large range of weights (1140-3388g) and normal physical activity while being nursed in isolettes or open cribs, in both supine and prone positions, and also when uncovered and covered with their usual blankets. We performed nine recordings of 41-108 minutes duration, for a total time of 620 minutes that was used for analysis.
3) Signal Processing
We processed the data using the standard functions of the Acknowledge software system after data acquisition. At each step in the process, we examined the data graphically to verify proper analysis of the signals.
a) Respiratory output
A detailed comparison of the respiratory output and the Edi was performed in two parts. The first was a comparison of the infants’ spontaneous respiratory rates, and the second was to compare the timing of the onset of inspiration defined by the sensor respiratory output and the Edi. For the second comparison, we selected one recording from each infant that contained little or no ventilatory support that could interfere with the spontaneous breathing.
The respiratory rate was calculated in the same way for the sensor respiratory output and the Edi. Segments of data, ranging from 26-57 minutes were selected for the analysis wherein there was no caretaker movement or artificial breaths given by the ventilator. The raw sensor signals were first smoothed with a 10-sample moving window average, since the Edi output used for comparison was updated at 100Hz by the Servo-i ventilator (see above), and then low-pass filtered (Blackman, cutoff frequency 2 Hz, −5.3 dBV at 3 Hz, −68 dBV at 4 Hz). The sensor signals were then differenced every 10 data points. A threshold detector was applied to the differenced signal to produce a binary representation of inspiration (1) and expiration (0). A threshold value of approximately 1.5% of the full-scale range of each signal was used, as it produced an accurate representation of the data on visual inspection of the waveforms and reduced short transitions due to noise. The respiratory rate was calculated for sequential 20-second intervals, based on the transition of inspiration to expiration. A 20-second interval was chosen because of the large variation in the respiratory rate, and because clinical monitoring systems use a similar interval for updating the respiratory rate.
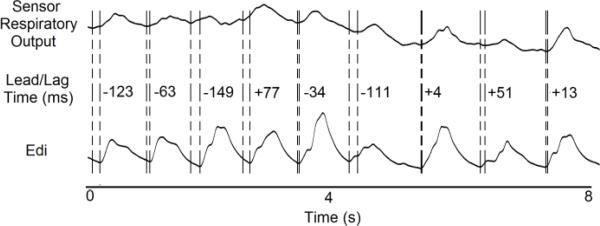
To compare the determination of the onset of inspiration, other segments of 10 minute duration were used that were free of caretaker movement, but that included ventilator-induced breaths with a rate of up to 8 per minute. These segments were displayed graphically for the respiratory output, Edi, and airway pressure, so that breaths produced by the ventilator or a disruption of the spontaneous breathing due to the ventilator were not included. A cursor was moved manually through the graphical display to visually define the inflection points of the sensor respiratory output and the Edi. The time differences between the points of inflection of the two signals were then measured. Automation of the process could not be done within the Acknowledge software. An example of an analyzed record is shown in Fig. 7, with the time differences added to the figure. By convention, negative times represented the sensor respiratory output leading the Edi, and positive times, lagging.
Figure 7.
Comparison of the sensor respiratory output and the Edi. Lead/lag times between the inflection points in the sensor respiratory output and the Edi that indicated the start of inspiration were determined and are shown numerically in ms.
b) Non-respiratory movement
We processed the data from infants in Protocol 2 for non-respiratory movement. The amplitude of the sensor movement signal, while temporally correlated to the accelerometer system as shown in Fig. 6, was not assumed to be linearly correlated. Signal processing of the sensor movement signal and that of the accelerometer system was performed to define a single threshold for each system that could be used as a positive indicator of movement in all recordings. Although accelerometers have been used in studies of infant movement, thresholds for “significant” movement in that system have not been reported. Therefore, a simple receiver-operator curve analysis was not employed, since the definition of true positive movement for the accelerometers was not available. The optimal threshold in each system was therefore determined so as to fulfill two requirements: 1) the lowest threshold so as to compare the smallest movements, and 2) the same proportion of positive and negative indications of movement in both systems in any recording.
We first determined the thresholds to fulfill the two requirements in each recording, and then calculated the proportion of positive movement and the percent agreement between the two systems in each recording. The averages of the thresholds in all the recordings were then used to recalculate the proportion of positive movement and the percent agreement in all the recordings to give an indicator of the overall performance for the validation.
The optimal thresholds for both systems were obtained by the following procedure. First, the data in each recording of the sensor and accelerometer system were scaled to normalize the data for the full-scale range in the recording. We produced a histogram of 1,000 bins of the normalized data and plotted the proportion of the data in each bin against the data value of the bin, as shown in Fig. 8(a).
Fig. 8.
Method to define equivalent thresholds for the sensor and the accelerometers.
The scale on the X-axis shown on the figure was expanded to 0.3 for clarity (lowest 300 bins). The frequency distribution of the normalized proportion of data points was lower for the sensor than the accelerometer system, but there were similar proportions above 2% of the full-scale range. This indicates the extreme sensitivity of both systems with the sensor having greater sensitivity than the accelerometer system at the limit of movement detection.
We then determined the normalized values at which there was equal proportion of + indications of movement in the sensor and accelerometer system by accumulating the bins of the histogram of the normalized proportion of points in the Fig. 8a for both systems. The normalized proportions were then plotted against their respective normalized values, and overlaid on the same axes, as shown in Fig. 8(b). The intersections of the two plots indicates an equal proportion of + indications of movement in the two systems, designated by A, B, and C. Point A is the lowest threshold (highest sensitivity). The absolute value of both the sensor and the accelerometer corresponding to the normalized value at Point A represented the threshold values for each system to fulfill the two assumptions of the analysis. The overlay plot in Fig. 8(b) B has been expanded even further for the lowest 200 bins (lowest 20% of the recorded data) of the histogram.
In each recording, we used these thresholds to calculate the positive and negative indications of movement for the sensor and the accelerometer system. We constructed a 2×2 table of the + and – indications to calculate the percent agreement between the indications as follows:
We then made a series of determinations of the percent agreement while changing the thresholds of both the sensor and the accelerometer systems over a range of approximately 0.5% of the full scale value. This was the equivalent of 5 bins of the original histogram analysis. For each recording, we determined the optimal threshold for both the sensor and the accelerometer system that produced the highest percent agreement at the highest sensitivity.
To determine the overall thresholds in both systems, we then averaged the optimal thresholds of all the individual recordings of each system, and recalculated the positive indications of movement based on the average thresholds from all recordings in both systems. A similar 2×2 table was then constructed to calculate the overall percent agreement between the two systems over all the recordings for the validation.
Since the sensor had greater sensitivity than the accelerometer system, we tested the effect of using a lower threshold for the sensor, while keeping the threshold for the accelerometer system constant at its mean value across the recordings. This analysis was based on the use of the accelerometer system as the accepted standard for indications of movement, with the sensor output being the dependent variable. This analysis was meant to provide a noise floor for the sensor wherein the higher sensitivity would lead to more false positive indications of movement.
c) Movement of the caretaker
Periods of movements of the caretaker were noted from the annotated recordings. In preliminary recordings, we noted that caretaker movement produced large excursions in the movement output of the sensor, as high as 2 orders of magnitude greater than the largest infant non-respiratory movement. We chose to use a threshold for caretaker movement that was 5 times higher than the average threshold for non-respiratory movement (several S.D. greater than the mean value) for comparison to annotations made in the recordings in real-time.
4) Statistical Analysis
Validation of the outputs of the sensor was performed by comparison of the respiratory output, non-respiratory movements, and movements of the caretaker. Paired testing was performed to compare differences in values obtained from the sensor and the comparator signals within recordings, and for generalizability, two-tailed testing was performed to compare the average values for all recordings. Parametric testing was performed where data were normally distributed (t-tests), and non-parametric testing was performed (Wilcoxon's Signed Rank Test or Mann-Whitney Rank Sum Test) for non-normally distributed data.
a) Agreement of the respiratory output and the Edi
Protocol 1 data were used for this part of the validation. Differences in the respiratory rates from the sensor and the Edi signal in each recording, and mean respiratory rates derived from the sensor and the Edi for all the recordings from the group were compared.
We tabulated the lead/lag time of the onset of inspiration from the data obtained by the visual determination of the response times. The differences in the mean lead/lag times for the individual recordings and for those of the mean of all recordings were compared.
b) Agreement of the non-respiratory movement output of the sensor and the accelerometer system
Protocol 2 was used for this part of the validation. The optimal thresholds in individual recordings for the sensor and the accelerometer system that fulfilled the two requirements in that they 1) produced the maximal agreement for both positive and negative indications of movement and 2) these thresholds represented the highest sensitivity. The overall performance of the sensor non-respiratory movement output was validated by comparing the mean percent movement and agreement in the individual recordings with the mean percent movement and agreement that were recalculated in each recording using the group mean thresholds for each system.
The average percent movement detected at the mean overall threshold for the sensor was tabulated to estimate the amount of interference non-respiratory movement could have produced in the respiratory output in the infants in both protocols.
c) Agreement of the sensor and movement of the caretaker
The episodes of caretaker movement were compared to those identified by the annotations in the recordings. The true and false positive indications of the episodes were used to compute the sensitivity and specificity of the sensor to detect caretaker movement.
III. Results
A) Respiratory Output of the Sensor
The results of the validation based on the comparison of the respiratory rates are shown in Table II for the infants in Protocol 1. The respiratory rate was highly variable in both systems reflecting the irregular breathing of these premature infants. The mean difference between the respiratory rates was 1.2 breaths per minute, which was not significant in any individual recording (p=0.147, Wilcoxon Signed Rank Test). The group mean rates were also not significantly different between the sensor and the Edi (p=0.577, Student t-test).
TABLE II.
Respiratory Rate, Time Difference for Inspiration, and Percent of Non-Respiratory Movement for Infants in Protocol 1.
| Respiratory Rate | Lead/Lag to | Percent Movement | |||||
|---|---|---|---|---|---|---|---|
| Infant # | EDI Mean (SD) | Sensor Mean (SD) | Diff in RR Mean (SD) | Onset of # Breaths | Inspiration Mean (SD) | Recording Length (min) | % of Record |
| 1 | 70.5 (10.5) | 70.1 (6.6) | 7.7 (8.7) | 274 | −20 (67) | 249 | 13.9 |
| 2 | 68.2 (12.9) | 65.5 14.9) | 2.7 (20.9) | 877 | −26 (72) | 99 | 1 |
| 3 | 66 (12.3) | 70.9 (13.1) | −4.9 (9.3) | 471 | −2 (53) | 558 | 9.3 |
| 4 | 62.3 (14.9) | 63.5 (8.5) | −1.2 (13.4) | 512 | −16 (44) | 489 | 10.4 |
| 5 | 57.4 (12.3) | 59.8 (17.3) | −2.5 (17.4) | 518 | −23 (52) | 827 | 3.1 |
| 6 | 44.1 (24.5) | 48 (14.1) | −3.9 (23.4) | ---- | ---- | 532 | 4 |
| 7 | 56.310.1) | 54.9 (7.6) | 1.3 (9.7) | 513 | −28 (78) | 336 | 0.2 |
| 8 | 65 (8.6) | 66.3 (8.9) | 1.3 (10.2) | 418 | −26 (74) | 485 | 0.8 |
| 9 | 46.3 (16.1) | 46.4 (19.1) | 0.3 (10.8) | 365 | −13 (50) | 907 | 3.6 |
| 10 | 42.7 (10.6) | 56.8 (10.3) | −14.2 (12) | 280 | −30 (73) | 281 | 0.9 |
| 11 | 57.4 (18.4) | 58 (17.4) | 0.6 (111.9) | 751 | −42 (77) | 639 | 4.5 |
| Mean (SD) | 55.1(13.7) | 62.5(11) | −1.2 (13.4) | −23 (68) | 4.7 (4.5) | ||
| Total | 4979 | 5402 | |||||
The time differences for the onset of inspiration are shown in the Table. Data are missing for infant #6, since he required too much respiratory support to have an adequate amount of artifact-free data for the analysis. We were, however, able to calculate the percent movement for this infant. The sensor detected the onset of inspiration an average of 23ms before the Edi inflection. This lead-time was significant in all individual recordings (P<.001 by paired t-test) and for the mean of all recordings (P<.001 by Mann-Whitney Rank Sum Test).
We calculated the percent movement in all 29 recordings in Protocol 1 using the mean threshold for the sensor derived from the group average in Protocol 2 to estimate the potential interference of non-respiratory movement of the infants with the respiratory output of the sensor. The percentage of the recording with potential interference is also shown in Table II. The average percent of non-respiratory movement, weighted for the recording times, was 4.7+/− 4.5% of the recordings. In 9 of the 11 infants, this potential interference was less than 10% of the recording time, with a maximum of 13.9% in Infant #1.
Infants in Protocol 1 were all studied in the clinical condition in which they were being nursed. We found no differences in the results between the supine and prone positions. Infants in Protocol 2 were studied both uncovered and covered with their usual blankets. We found no visual difference in the respiratory output signal when they were covered or uncovered, except that in several of the infants, the respiratory output signal was enhanced by the coverings. This may have been due to the larger reflective surface of the blankets being moved by respiratory movement than the smaller reflective surface of their body when they were uncovered.
B) Non-Respiratory Movement
Non-respiratory movement was characterized for the agreement between the sensor and accelerometer system for individual recordings, and then for agreement at a single threshold for all recordings. Furthermore, we assessed the amount of movement that would interfere with the respiratory output in infants in both protocols, and finally, we demonstrated the separation of non-respiratory movement of the infant and that of the caretaker.
1) Agreement of the sensor and the accelerometer system in individual recordings and overall performance
The sensitivity of changes in the threshold for the sensor while keeping the accelerometer threshold constant at the mean group value in the 9 recordings in Protocol 2 is shown in Fig. 9. The percent agreement increased with increasing threshold of the sensor in all recordings. The mean sensor threshold and mean percent agreement for all the recordings has been added as the cross bars. There was better agreement at a higher sensor threshold, wherein only the larger movements were correlated between the sensor and accelerometer system. This corroborates the selection of this threshold as the highest sensitivity and selectivity for the group data.
Figure 9.
Plot of the percentage agreement of the sensor and accelerometer system vs. the threshold value of the sensor as it was varied while keeping the accelerometer threshold constant at the group mean value. The percent agreement increased with increasing sensor threshold in the individual recordings. The poorest agreement was in Infant # 17 who was in narcotic withdrawal. The bars show the mean overall agreement and the mean sensor threshold. The overall mean agreement was 90% between the two systems.
The poorest agreement, 0.83, was seen in Infant #17, who had a significantly higher amount of movement than the other infants because of narcotic withdrawal. The poorer correlation was due to fine tremors that were detected by the accelerometer system but not the sensor. For the purpose of generalizing the application of the sensor to these types of infants, we included the lower threshold in the mean threshold and the percentage agreement calculations. The lower threshold and agreement can be seen in Infant #17, with increased agreement at a higher threshold. We chose to use the mean threshold for subsequent calculations in the second protocol as it was the most sensitive threshold and gave the most general estimate of the agreement for all infants.
Although there was a large variation in the optimal thresholds for both the sensor and the accelerometer system, the use of the group mean threshold values for the sensor and the accelerometer system produced similar results for the percentage agreement and the percentage movement in the recordings. The results of the analysis for the thresholds for movement are shown in Table III. In the individual recordings shown are the optimal thresholds for the accelerometer system and the sensor, the percent movement, and the percent agreement. Shown also are the percent movement and agreement from the recalculation based on the mean thresholds for both systems for all the recordings. The differences between the percent movement for the individual recordings and that recalculated for the individual recordings using the mean thresholds were not significantly different (p=0.902 by Mann-Whitney Rank Sum Test). The percent agreement averaged 0.93 in the individual recordings, and as expected, averaged less, 0.90, for recalculated data based on the mean thresholds. This difference, although small, was significant (p<.01 by t-test).
TABLE III.
Threshold and Movement Data for Individual Recordings and Mean Values for All Recordings in Protocol 2..
| Data for Individual Recordings | Data for Group | |||||
|---|---|---|---|---|---|---|
| Infant # | Threshold ACC (mv) | Threshold Sensor (×10−3) | %Movement at Optimal Threshold1 | Agreement | %Movement at Mean Threshold2 | Agreement |
| 12 | 213 | 5.7 | 6.9 | 0.97 | 5.6 | 0.92 |
| 13 | 124 | 3.74 | 6.2 | 0.925 | 3.9 | 0.88 |
| 14 | 289 | 5.35 | 18.1 | 0.96 | 18.6 | 0.89 |
| 15 | 290 | 5.68 | 5 | 0.97 | 7.2 | 0.94 |
| 16 | 195 | 4.52 | 11.5 | 0.93 | 11.7 | 0.92 |
| 173 | 180 | 1.41 | 44.5 | 0.83 | 47.5 | 0.79 |
| 18 | 234 | 3.11 | 8.9 | 0.94 | 9.9 | 0.93 |
| Mean | 218 | 4.22 | 14.44 | 0.93 | 14.91 | 0.90 |
| S.D. | 60 | 1.58 | 13.97 | 0.05 | 15.16 | 0.05 |
Optimal threshold for each recording was used.
Mean thresholds for all of the recordings were used and recalculated data are shown.
Infant with narcotic withdrawal. Note lower threshold and higher percent movement.
The percent movement in the infants in the second protocol is shown in Table III. The infants in this group were larger, were not on ventilatory support, and had more movement, averaging 14.9 +/− 15.1% of the recordings. The percent movement was less than 10% in 7 of the 9 recordings.
2) Agreement with caretaker movement
There were 187 episodes of caretaker movement identified by the annotations in the recordings. There were 184 true positive indications identified by the sensor, with 3 false positive indications, probably due to movement of the isolette. There were no false negative indications. The sensitivity and specificity of the sensor to identify episodes of caretaker movement was therefore 98%.
C) Overall system performance
Figure 10 shows a composite of the raw Phase A signal, the separate movement outputs and respiratory output of the sensor and the algorithms, the Edi signal for comparison, and the respiratory rates derived from the sensor and the Edi. The movement output has been plotted on a log scale to show the large dynamic range of the sensor, and the mean thresholds for the infant and caretaker movements have been added. The sensor separated isolated non-respiratory and caretaker movement using the thresholds. Caretaker movement could not be distinguished from caretaker movement + infant movement, as the two were related. In either, despite large excursions in the Phase A signal, and that passed through several wavelengths, the respiratory rate from the sensor was stable. There were 5 episodes in which there was a large difference between respiratory rates derived from the sensor and the Edi, marked by stars in the figure. These episodes were related to noise in the Edi signal that caused a malfunction of the respiratory rate determination by the Edi during periods of apnea. There discrepancies were seen in the fourth and fifth episodes, again during apnea which was not as pronounced.
Fig. 10.
Composite of the sensor outputs, Edi, respiratory rates from the sensor and Edi in 1040 g infant. Even during times of both non-respiratory and caretaker movement, the respiratory rate derived from the sensor was stable. The episodes of major discrepancy between the rates (stars added to the figure) were due to the noise in the Edi signal during periods of apnea that caused the rate algorithm to malfunction.
IV Discussion
We have validated that this non-contacting sensor can give separate and reliable outputs for respiratory and non-respiratory movements of infants, and those of their caretakers. The use of reflected ultrasound for physiological monitoring has been described before. The sensor we describe had the advantage of the greater bandwidth necessary for the wider range of movements than respiratory movements alone. This was made possible by the in-phase and quadrature phase detection scheme prior to filtering. Previous reports of non-contacting ultrasound-based systems for detection of respiratory and non-respiratory movements made use of phase lock loop (PLL) detection that varied the frequency of the transmitter so as to maintain a fixed number of wavelengths of ultrasound between the sensor and subject [16], [17]. We decided not to use this scheme since the bandwidth and loop gain of the PLL also limits the operation of the system to pre-specified respiratory rates, and may require resetting or repositioning of the sensor to maintain the lock of the loop. Others used an I&Q detector but suggested the use of higher ultrasound frequencies (up to 600 kHz) to be able to capture a larger range of movement [18]. These higher frequencies are impractical for proper propagation and reflectance. Two other groups used a fixed transmitter frequency and phase demodulation by analog mixers, which necessitated filtering that limited the sensor to an expected movement range for respiration only [19], [20].
Instead, we used a fixed transmitter frequency and an in-phase and quadrature detection scheme that allows measurement of movement with a resolution of a very small fraction of a wavelength, and that can track the phase difference between the transmitted and received signals over several wavelengths. This eliminated the bandwidth limitations and allowed detection of the phase information containing very low frequencies associated with breathing (down to apnea), and the higher frequencies associated with non-respiratory and caretaker movement.
Although distortion with larger non-respiratory and caretaker movements distorted the respiratory output, this was found to be a small percentage of time of the records made under typical clinical circumstances, even in infants with a large range of weights and who were vigorous. Most non-respiratory movements were of very short duration, and did not interfere with the determination of respiratory rate. This suggests that the threshold for non-respiratory movement may have been set too low to be an indicator of “significant” movement for this application of the sensor.
We were surprised to see that the sensor performed equally well with the infants covered, uncovered, and bundled, and in either the supine or prone positions. We did not change the clinical conditions in which we found the infants, so that we could assess the overall performance of the sensor. Our analysis was not biased by the selection of the data files or data segments for any position or coverings. During the recordings, we also did not interfere with the routine nursing care the infant received; the episodes of care were clearly documented by the caretaker movement output of the sensor. The infants in Protocol 1 were more often bundled and were on ventilatory support, which could account for a lower amount of overall movement.
We have demonstrated that the sensor can reliably detect the onset of inspiration compared to the electrical activity of the diaphragm. The rapid response time, the small amount of interference from non-respiratory movement and its reliable identification by the sensor shows that it is feasible to use the sensor as a trigger to synchronize a mechanical ventilator with spontaneous breathing. The non-respiratory movement interfering with the operation of the sensor that we observed lasted only short periods of time with immediate recovery of the respiratory output of the sensor. These movements could be an inoperable condition for the trigger that would change the mode to non-synchronized ventilation, as is presently used. Since the sensor makes no contact with the patient and does not need to be attached to a leaky airway, the trigger could find great utility in non-invasive ventilation.
The validation of the detection of non-respiratory movement suggests many uses for the sensor, including a monitor of overall movement, detection of seizures, assessment of the effects of sedation and recovery from anesthesia in both humans and animals, sleep state determination, and the objective assessment of infants being treated for drug withdrawal. In many of these applications, the non-contacting nature of the sensor would be very helpful in developing a number of monitoring products. Adjustments in the threshold for different types of non-respiratory movement may be necessary, and could improve the agreement that we saw at the highest sensitivity in these infants.
The accurate detection of caretaker movement could be very useful in assessing the amount of care an infant is receiving, and the physiological effects of handling. In the practical clinical situation, the sensor does not need to function at times of caretaker movement, since alarms of physiological monitors are usually disabled during handling, and caretakers rely on their visual observation of respiration during handling. The sensor can provide objective documentation of caretaker activity that could be useful for work-flow studies and documenting the acuity of care.
Finally, the sensor is inexpensive to construct from readily available materials. Although the prototype used for these studies was implemented in TTL technology, newer technologies could be used to reduce the circuit size, lower power consumption, and add real-time computation of the respiratory, non-respiratory, and caretaker movements. With further development, the sensor should be applicable to older children and adults.
V. Conclusion
We have described and validated a single, non-contacting sensor for respiratory, non-respiratory, and caretaker movement in infants in an intensive care setting. The sensor could detect the onset of inspiration 23ms prior to a comparative measure of the electrical activity of the diaphragm, with adequate accuracy to be used as a trigger mechanism to synchronize a mechanical ventilator to the spontaneous breathing of the infant. The non-respiratory movement output had an agreement of 0.9 with an independent measure of movement by accelerometers. The detection of caretaker movement had a sensitivity and specificity of 0.98 compared to visual annotation of caretaker movements during our recordings. The separate outputs for the non-respiratory and caretaker movements may be useful for a number of other applications for the clinical assessment of infants and their care.
The sensor described was used in infants for this validation. With modifications in the design of the sensor head and post-detection filtering, it could be used in older children and adults. The sensor, as part of a synchronizer for adult and pediatric ventilators, could promote the present trend to use non-invasive ventilation as an alternative to invasive ventilation.
ACKNOWLEDGMENT
The authors thank the nursing and respiratory care staff of the Intensive Care Nursery at the University of California, San Diego Medical Center, for their assistance in this work. We especially acknowledge the assistance of Benjamin Castro, RRT, in setting up the Servo-i ventilator for the comparison signals.
This work was supported in part by National Heart, Lung, and Blood Institute under Grant 1R41 HL 102940.
Biography
 Gregory Heldt (M'14) received his undergraduate education in chemistry at Stanford University and his M.D. from the School of Medicine, University of California, San Diego in 1974. He completed his Pediatric residency at the University of California, San Francisco in 1977, and Fellowship in Neonatology and Pulmonology at the Cardiovascular Research Institute, San Francisco in 1980. He was on the faculty at UCSF until 1985, and has been at UCSD since. He became Professor of Pediatrics in 1994.
Gregory Heldt (M'14) received his undergraduate education in chemistry at Stanford University and his M.D. from the School of Medicine, University of California, San Diego in 1974. He completed his Pediatric residency at the University of California, San Francisco in 1977, and Fellowship in Neonatology and Pulmonology at the Cardiovascular Research Institute, San Francisco in 1980. He was on the faculty at UCSF until 1985, and has been at UCSD since. He became Professor of Pediatrics in 1994.
His research interests are the development of new technologies for mechanical ventilation of infants, specifically high-frequency ventilation and patient-triggered ventilation, pulmonary function testing, and development of artificial pulmonary surfactant therapies for respiratory distress. He has collaborated with the Hewlett-Packard Corp. in the development of infant monitor systems, the Infrasonics Corp., San Diego, in the development of the Star-Calc pulmonary function system and the Star-Sync ventilator trigger for the Infant Star ventilator, and the Discovery Laboratories Corp., in the development and FDA approval of Surfaxin, an artificial surfactant. He is actively involved in the research training of the Fellows in Neonatology at UCSD.
Dr. Heldt is a senior member of the Pediatric Academic Society and an active member of the Institutional Review Board at UCSD.
 Raymond Ward was raised in Monterrey, California. He received his B.S. in Physiology and Neuroscience from the University of California at San Diego in 2002.
Raymond Ward was raised in Monterrey, California. He received his B.S. in Physiology and Neuroscience from the University of California at San Diego in 2002.
From 2002 to 2004 he was the Surgical Laboratory Manager at Ichor Medical Systems and assisted in the creation and testing of an electroporation drug delivery device. Since 2004, he has worked in the division of Neonatology at the University of California San Diego Medical Center as the Chief Respiratory Therapeutics Coordinator where he is responsible for the creation and operation of a cGMP lung compliance assay. He aided Discovery Laboratories in the development and FDA approval of Surfaxin, an artificial surfactant. He also aids in the training of fellows in mechanical ventilation of infants and associated pulmonary technologies. In 2008, founded BioData Innovation Systems, a California Corporation. He led BioData in obtaining a successfully funded Phase I STTR grant funded by the National Heart, Lung and Blood Institute, and progressed the company's lead product, the sensor described in this paper. BioData submitted a patent application with the USPTO for the sensor in June 2015. Raymond and BioData also work on research and development of assays for lung pulmonary functions.
Footnotes
G. Heldt has no financial interests in BioData Innovation Systems, Inc., that has applied for the patent on the technology described in this paper.
Contributor Information
Gregory P. Heldt, University of California, San Diego, 200 W. Arbor Dr., San Diego, CA 92103 USA (gheldt@ucsd.edu)..
Raymond J. Ward, III, BioData Innovation Systems, Carlsbad, CA. 92009 (rward@biodatainnovation.com)
REFERENCES
- 1.Mukai K. A remote monitor of bed patient cardiac vibration, respiration, and movement. Proc of the 31st Annu. Int. Conf. of the IEEE EMBS (EMBC2009) 2009:5191–5194. doi: 10.1109/IEMBS.2009.5333716. [DOI] [PubMed] [Google Scholar]
- 2.Hu W. Noncontact accurate measurement of cardiopulmonary activity using a compact quadrature Doppler radar sensor. IEEE Trans. Biomed. Eng. 2014 Mar;61(3) doi: 10.1109/TBME.2013.2288319. [DOI] [PubMed] [Google Scholar]
- 3.Goldman LJ. Nasal airflow and thoracoabdominal motion in children using infrared thermographic video processing. Ped. Pulmonol. 2012;47:476–486. doi: 10.1002/ppul.21570. [DOI] [PubMed] [Google Scholar]
- 4.Arlotto P. An ultrasonic contactless sensor for breathing monitoring. Sensors (Basel) 2014 Aug;1420(8):15371–15386. doi: 10.3390/s140815371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yamana Y. A sensor for monitoring pulse rate, respiration rhythm, and body movement in bed. Conf Proc IEEE Eng Med Biol Soc. 2011:5323–5326. doi: 10.1109/IEMBS.2011.6091317. doi: 10.1109/IEMBS.2011.6091317. [DOI] [PubMed] [Google Scholar]
- 6.Bernstein G. Airway leak size in neonates and autocycling of three flow-triggered ventilators. Crit Care Med. 1995;23(10):1739–1744. doi: 10.1097/00003246-199510000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Bernstein G. Response time and reliability of three neonatal patient triggered ventilators. Am Rev Resp Dis. 1993;148(1):358–364. doi: 10.1164/ajrccm/148.2.358. [DOI] [PubMed] [Google Scholar]
- 8.Bernstein G, et al. Increased and more consistent tidal volumes during synchronized intermittent mandatory ventilation in newborn infants. Am J Respir Crit Care Med. 1994 Nov;150(5):1444–1448. doi: 10.1164/ajrccm.150.5.7952573. [DOI] [PubMed] [Google Scholar]
- 9.Spriggs DR. Recombinant human tumor necrosis factor administered as a 24-hour intravenous infusion: a phase I and pharmacologic study. J Natl Cancer Institute. 1988 Sep 7;80(3):1039–44. doi: 10.1093/jnci/80.13.1039. [DOI] [PubMed] [Google Scholar]
- 10.Terrill PI. Application of recurrence quantification analysis to automatically estimate infant sleep states using a single channel of respiratory data. Med Biol Eng Comput. 2012 Aug;50(8):851–865. doi: 10.1007/s11517-012-0918-4. [DOI] [PubMed] [Google Scholar]
- 11.Adde L. Early prediction of cerebral palsy by computer-based video analysis of general movements: a feasibility study. Dev Med Child Neurol. 2010;52(8):773–778. doi: 10.1111/j.1469-8749.2010.03629.x. [DOI] [PubMed] [Google Scholar]
- 12.Heinze F. Movement analysis by accelerometry of newborns and infants for the early detection of movement disorders due to infantile cerebral palsy. Med Biol Eng Comput. 2010;48(8):765–772. doi: 10.1007/s11517-010-0624-z. [DOI] [PubMed] [Google Scholar]
- 13.TLVs and BEIs Threshold Limit Values for Chemical Substances and Physical Agents. American Conference of Governmental Industrial Hygienists; Cincinnati, OH. 1998. [Google Scholar]
- 14.Emeriaud G. Diaphragm electrical activity during expiration in mechanically ventilated infants. Pediatric Research. 2006;59(5):705–710. doi: 10.1203/01.pdr.0000214986.82862.57. [DOI] [PubMed] [Google Scholar]
- 15.Beck J. Characterization of neural breathing pattern in spontaneous breathing infants. Pediatric Research. 2011;70(6):606–613. doi: 10.1203/PDR.0b013e318232100e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karsh H. Motion monitor. 1978 Oct;24 U.S. Patent 4,122,427. [Google Scholar]
- 17.Northrup RB. Ultrasonic respiration/convulsion monitoring apparatus and method for its use. 1980 Apr;15 U.S. Patent 4,197,856. [Google Scholar]
- 18.Barany LP. Ultrasonic non-contact motion monitoring system. 1993 Jun;22 U.S. Patent 5,220,922. [Google Scholar]
- 19.Geiger PD, Hudgins LH. Stand-off non-invasive acoustic baby monitor. 2000 Nov;21 U.S. Patent 6,150,941. [Google Scholar]
- 20.Seabron Z. Ultrasonic monitor. 2001 Jun;19 U.S. Patent 6,248,068. [Google Scholar]