Abstract
Background
Female sex workers (FSW) and people who inject drugs (PWID) are at high risk for HIV infection, with FSW-PWID at even greater risk. HIV-related research often focuses on the primary mode of transmission –sexual or parenteral transmission for FSW and PWID, respectively- with less known on how sex work and injection drug use (IDU) are collectively associated with the risk environment experienced by sex workers. We investigated this relationship among FSW in three Russian cities.
Methods
In 2011, FSWs (N=754) in Tomsk, Krasnoyarsk, and Kazan were recruited via respondent-driven sampling and completed a survey and rapid HIV screening. Multivariable models evaluated the role of injection history (classified as active: last 6 months, former: prior to last 6 months, and never) with a set of sexual and structural HIV risk outcomes.
Results
IDU was common: 11% actively injected drugs and 11% were former injectors. HIV infection was most prevalent among active injectors (AOR: 6.7; 95% CI:2.4–18.9) and former injectors (AOR:4.5; 95%CI:1.7–11.6), compared to non-injectors. Some 6–8% of non-injecting FSWs reported recent physical or sexual client violence and 23% police extortion. Compared to these non-injectors, active injecting was associated with unprotected anal sex (AOR: 2.8, 95%CI:1.2–6.4), client violence (AOR: 7.3, 95%CI:2.1–24.7), and police extortion (AOR: 3.0 95%CI:1.5–5.9%). Self-reported sexual and structural risk outcomes were also more prevalent among active compared to former injectors; however, few differences existed between former and non-injectors.
Conclusions
FSW experience sexual, structural, and HIV risk outcomes and these risks are amplified for actively injecting FSWs. FSW who stopped injecting drugs demonstrated risk profiles closer to those of sex workers who had no history of injection. HIV prevention programs and outreach can provide opportunities to include harm reduction interventions and linkage to treatment for FSW to move FSWs towards lower risk environments.
Keywords: HIV, Russian Federation, Female sex worker, Injection drug use, Violence, Prevention
Introduction
Female sex workers (FSWs) and people who inject drugs (PWID) are vulnerable populations for HIV acquisition and transmission, with a 13-fold increased odds of HIV infection for FSWs compared to the adult female population.(Baral et al., 2012) While HIV epidemics have declined globally, nine countries, including the Russian Federation, have witnessed increased HIV incidence within the last decade.(UNAIDS, 2012) The majority of these infections are concentrated among key populations, including FSW and PWID. While HIV epidemiology is distinct these two populations, they share both behavioral risk factors and sexual networks.(El-Bassel, Shaw, Dasgupta, & Strathdee, 2014; Mazhnaya et al., 2014; Platt et al., 2013; Platt et al., 2007) At the confluence of injection drug use (IDU) and heterosexual HIV risks, female sex workers who inject drugs (FSW-PWIDs) are a dually high-risk group exposed to both sexual and parenteral transmission pathways.(Strathdee et al., 2010; Ulibarri et al., 2011)
The broader risk environment shapes harms related to both substance use and sex work.(Maher et al., 2011; T Rhodes, 2002) This framework posits a reciprocal interaction of physical, social, economic, and policy-related factors that act at the micro and macro-levels to “impact the production or reduction of drug harms” or harms related to sex work.(T. Rhodes, 2009) The interplay of these environmental factors and their impact on HIV among FSW and PWID is increasingly evident.(Blanchard & Aral, 2010; Shannon, Strathdee, et al., 2014; Strathdee et al., 2010) For example, for PWID, criminalization and heavy policing of drug use may lead to hidden injecting practices and rushed safety precautions that increase opportunities for HIV transmission and acquisition.(Strathdee et al., 2010) Likewise, the use of condoms as evidence of sex work by law enforcement may reduce FSWs’ condom carriage and subsequent use with clients.(Wurth, Schleifer, McLemore, Todrys, & Amon, 2013) Harms within the risk environment may be most pronounced for FSW-PWIDs who work and live in the nexus of these risk environments and who may be more hidden in their sex work and drug use so as to avoid encounters with police.(Deering et al., 2013)
Sexual and structural risk harms are considered particularly high in the Russian Federation, where criminalization of illicit drug use and administrative penalties for engagement in sex work impart risk for police harassment and violence.(Arps & Golichenko, 2014; Elovich & Drucker, 2008; Odinokova, Rusakova, Urada, Silverman, & Raj, 2014) Here, sex work generally takes place in a variety of forms including a range from (but not limited to) individual street-based sex work to employment with an agency or totcka in which sex workers may work collectively on the street or in bars, hotels and other venues.(Aral, St Lawrence, Dyatlov, & Kozlov, 2005) Though working with agencies or totchkas carry their own risks related to the power dynamics of the organization, they offer some source of protection against violence from clients and police. Individual street-based sex workers may choose to work independently, but many FSW who engage in IDU are often expelled or prohibited from working with an agency or totchka and tend to take on individual street-based work.(Decker et al., 2014) These women, given the visibility of where they work and lack of protection, are often more vulnerable to violence perpetrated by clients, police, and strangers, and may also be targeted as a result of drug use.(Aral et al., 2005)
Much of the HIV-related research on FSWs in the Russian Federation draws from samples of PWIDs who also engage in sex work, with far less known about non-PWID FSWs and how their sexual and structural risks compare with FSW-PWIDs.(N. Abdala et al., 2008; Nadia Abdala et al., 2010; Platt et al., 2007; Platt et al., 2005; Platt et al., 2009) There is also a need to understand the risks among FSW-PWID who bring drug use to cessation. While ending IDU may reduce risks inherent in injecting drug use, these FSW may still experience the impact of the drug use risk environment and remain at risk of relapse and re-entry into this environment.(El-Bassel et al., 2014; Shannon, Goldenberg, Deering, & Strathdee, 2014) In this vein, there is a need to consider the respective risk environments of sex work and IDU and the dynamic movement between them in order to comprehensively inform HIV prevention in the region. In other settings, epidemiologic studies of HIV among FSW, however, typically include measures of lifetime or recent IDU and, justifiably, include IDU as a confounder in associations with HIV infection due to associated parenteral transmission. However, we hypothesize that sex work and IDU may synergistically increase risk. As such, the role of IDU in the risk environment may be much more complex for FSW than simply parenteral transmission risks. Reducing IDU among FSW in the Russian Federation may lead to important improvements in HIV risks for FSW. In 2011, we conducted a study of HIV epidemiology among FSW as part of an evaluation of the Globus HIV prevention program for FSW in three cities of the Russian Federation. These cities included Tomsk, Kazan, and Krasnoyarsk, where little HIV epidemiologic research has been conducted with FSW. With this analysis, we evaluate the role of injection status (non-injection, active, and former injecting) with sexual and structural HIV risk outcomes as well as engagement in HIV services among FSWs.
Methods
Following an extensive formative and qualitative phase, a cross-sectional quantitative survey was conducted among FSW from July through September 2011. Data collection was conducted within an evaluation of the Globus HIV prevention program for female sex workers. The Globus program constituted the most significant source of funding and prevention efforts for key populations in The Russian Federation and came from the Global Fund to Fight AIDS, Tuberculosis and Malaria. Further details are available elsewhere.(Decker et al., 2014)
All study activities were conducted in collaboration with a Russian non-governmental organization, and local partner organizations based at each site. Local research assistants, all of whom had experience in research and/or HIV prevention outreach for sex workers, participated in an intensive training that included study procedures and human subjects protections, and carried out all study activities in the Russian language.
Study population and sampling
Three of the ten regions in which the Globus program was implemented were selected for study, specifically Tomsk, Kazan, and Krasnoyarsk. Resource constraints allowed for the study of only three of the ten sites. Cities with consistent program implementation and a range of estimated PWID population prevalence and HIV prevalence among PWID were prioritized. These sites represent large urban centers in Siberia or Tatarstan Regions. Kazan, the capital of the Republic of Tatarstan, is located in European Russia and is the eighth largest city in the Russian Federation. Krasnoyarsk and Tomsk are both industrial centers in Siberia, with 500,000 to 1 million inhabitants respectively. Industry and institutes of higher education, coupled with access by rail and river, have made all three cities common areas of relocation for those from rural areas, including those who enter the sex industry. In these settings, sex work is predominantly sold on the street and/or at venues (bars, hotels, saunas, etc.). Sex work and loitering are subject to administrative penalties, with policing that is heterogeneous within and between sites. Eligible participants were female, aged 18 years or older, and actively engaged in sex work, defined as having sold sex for money, drugs, or other items of value within the last three months.
Recruitment and Consent
Respondent-driven sampling (RDS) was used to recruit FSW participants in the three regions. RDS is often used for reaching hard to reach populations, including FSW and PWID.(Malekinejad et al., 2008) This peer-based, chain recruitment method engaged seeds and enrolled participants as future recruiters. A total of 759 participants were enrolled, though five surveys were excluded from analysis based on missingness of key indicators, resulting in the inclusion of data from 754 surveys in the analysis.
All study activities took place in the local NGO partner office or clinic; with the exception of Kazan, where study activities were additionally conducted via a mobile unit due to the distance between the NGO office and streets and venues where sex work were more common.
Upon determination of eligibility, participants underwent informed consent process in the Russian language with trained staff members. Verbal consent was used in lieu of signed consent to protect participant confidentiality.
Study Instruments and Measures
Participants completed an anonymous sociobehavioral survey and rapid, salivary-based HIV screening assay. The self-administered computerized survey was developed in English, translated into Russian language and piloted with native speakers prior to implementation. Survey measures were refined based on the formative phase and feedback from local staff and experts. The survey collected data on participant demographics, substance use, sexual behavior, and HIV prevention use. The exposure or independent variable of interest, history of injection drug use, was classified as active injecting: self- reported injecting drug use within the last six months; formerly injecting: self-reported lifetime history of injecting drugs but no injection within the last six months; and, non-injecting: no self-report of ever injecting drugs in one’s lifetime. Other independent variables were informed based on our formative research, and defined as follows. Other substance use variables included any substance use (alcohol or legal drugs) when trading sex in the last 6 months. Sex work venues included street, hotel, train station, internet, salon, club, sauna, or other location. Street-based sex work was considered one of the most structurally vulnerable locations in which to sell sex, based on prior research and discussions with local partners.(Aral et al., 2003; Odinokova et al., 2014), thus venues were classified to a binary variable of street vs. non-street venues. Organization of sex work was measured as past or current work with ‘an agency, pimp or momka (madam), or for a tochka (collective organization that runs sex work) that takes a portion of your earnings in exchange for arranging clients or providing protection,’ as compared to those who only worked independently.
Outcome variables of interest included both sexual and structural HIV risk outcomes. Sexual risks included: unprotected vaginal sex with clients, estimated proportions of clients that request anal sex, and unprotected anal sex with clients. We distinguished vaginal from anal sex due to evidence of increased HIV acquisition during unprotected receptive anal intercourse.(Baggaley et al., 2013; Baggaley, White, & Boily, 2010) Structural HIV risk outcomes included police extortion for money, sex, or information; and physical and sexual violence or coercion by clients. Structural HIV risk outcomes were assessed via separate items, given that sex workers may have multiple experiences of violence and/or exploitation. Measures of engagement in HIV prevention included ever being tested for HIV infection and being involved in Globus outreach and/or the program clinic. The Globus prevention program was the source of HIV prevention for FSWs in these regions and thus uptake of Globus services serve as a proxy for general uptake of HIV prevention programs for FSW. Recall periods for all measures of sexual behaviors, substance use, and structural HIV risk outcomes were the last 6 months and lifetime (ever); for the purposes of this analysis we focus on recent behaviors and experiences (last 6 months).
All participants completed the OraQuick Rapid HIV-1/2 Antibody test (OraSure Technologies Inc., Bethlehem, Pa.) according to manufacturer’s instructions. HIV screening results were available to participants within 15 minutes. All evaluation staff members had previous experience conducting rapid HIV tests and completed refresher trainings prior to the study. National pre- and post-test HIV counseling protocols were followed: participants were provided with pre- and post-test counseling and encouraged to complete confirmatory testing. The government mandates that confirmatory testing must be completed at the government AIDS clinic; all complied, with the exception of four participants whose HIV status was previously confirmed. Our anonymous data collection prohibited acquisition of the AIDS clinic confirmatory test results for validation of the rapid HIV test results.
The parent study evaluation was approved by the Open Health Institute (Moscow, Russia), and approved as public health practice, by the Johns Hopkins Bloomberg School of Public Health Human Subjects Committee, a mechanism primarily used for collaborative evaluation and capacity building. The current secondary analyses were approved as exempt.
Analysis
We sought to evaluate associations of injecting status (non-injecting, formerly injecting, and active injecting) with sexual and structural HIV risk outcomes and engagement in HIV services.
Missing data were imputed with the most conservative value; this process was used for variables that were missing by less than 10%. Four participants (0.5%) failed to respond to the question of injecting drug use history and these were conservatively imputed as ‘no self-report of ever injecting drugs in one’s lifetime’.
Descriptive analyses were conducted to characterize the sample including demographics and sex work characteristics, HIV prevalence and key sexual, structural and HIV service engagement outcomes among the total sample and by active, former, and non-injection history. Chi-square tests were used to evaluate statistical significance based on p<0.05. Simple bivariate and multivariable logistic analyses were conducted to assess the association between injection status and sexual, structural, and HIV prevention outcomes. Each respective outcome of interest was handled as a dependent variable, because our goal was not to present a risk factor model but to understand how histories of injecting drug use influence different components of FSWs’ risk environments. Potential confounders, including age (continuous), work location, and duration of sex work (continuous) were included in the multivariable logistic analyses, regardless of estimated strength of their bivariate association with dependent variables. Other variables significantly associated with injection drug use histories (p<0.05) were also included in the model, including financial status, having a source of income, days per week selling sex, alcohol use during sex work, and legal drug use during sex work. Potential colinearity of variables in the logistic models was assessed by calculating the variance inflation factors, all of which calculated below 1.3.
Despite lack of consensus on the appropriate use and calculation of RDS estimators, many RDS studies use RDS-specific estimators to create weights based on individual self-reported network size for the calculation of population-based estimates.(McCreesh et al., 2012; Mills et al., 2014; Salganik, 2012; Schonlau & Liebau, 2012) Participants of this study faced challenges in estimating their individual network size, prohibiting the calculation of RDS estimators. All analyses were conducted in STATA 12 and adjusted for potential clustering of evaluation participants induced by site and RDS sampling using complex survey design procedures.(STATaCorp, 2011; Szwarcwald, de Souza Junior, Damacena, Junior, & Kendall, 2011) Significance levels of categorical variables (injection groups) were assessed using Wald’s test.
Results
Among the 754 FSWs enrolled across three sites, 11% (n=81) were actively injecting drugs (within the last 6 mo.) and 11% (n=82) were former injectors (prior to the last 6mo.), totaling 163 (22%) with any history of injection use. Table 1 presents the sociodemographic characteristics of participants by injection status. Across injection status, there were significant differences in age; almost half of non-injectors were comprised of the youngest age group, while those with injecting histories had greater proportions in the older age categories (p=0.02). Similarly, duration in sex work was longer among those with histories of injection compared to non-injectors (p<0.001). A higher proportion of active injectors (79.0%) indicated their financial status was below minimum necessary to meet needs, compared to former (41.5%) and non-injectors (43.9%, p<0.001). Significantly fewer active injectors had another source of income (p=0.007). Greater proportions of active injectors worked on the street (92.6%) compared to former (64.6%) and non-injectors (63.5%, p=0.01).
Table 1.
Characteristics of female sex workers from three Russian cities, comparing injection drug use risk groups (N=754)
| Characteristic | Non-injecting (n=591) |
Formerly injecting (n= 82) |
Active injecting (n= 81) |
Total (n=754) |
p-value |
|---|---|---|---|---|---|
| Demographic characteristics | % (n) | % (n) | % (n) | % (n) | |
| City | 0.34 | ||||
| Kazan | 30.6 (181) | 46.3 (38) | 40.7 (33) | 33.4 (252) | |
| Kraznoyarsk | 35.4 (209) | 32.9 (27) | 18.5 (15) | 33.3 (251) | |
| Tomsk | 34.0 (201) | 20.7 (17) | 40.7 (33) | 33.3 (251) | |
| Originally from Russian Federation | 91.4 (540) | 95.1 (78) | 96.3 (78) | 92.3 (696) | 0.24 |
| Age (95% CI)* | 25.6 (24.6 – 26.5) | 27.9 (25.8 – 30.1) | 27.3 (25.4 – 29.1) | 26.0 (25.0 – 27.0) | 0.02 |
| 18–24 years | 48.6 (287) | 28.1 (23) | 33.3 (27) | 44.7 (337) | |
| 25–29 years | 31.3 (185) | 35.4 (29) | 29.6 (24) | 31.6 (238) | |
| 30 years and over | 20.1 (119) | 36.6 (30) | 37.0 (30) | 23.7 (179) | |
| Relationship status:* | 0.05 | ||||
| Never Married/Dating | 64.1 (379) | 47.6 (39) | 55.6 (45) | 61.4 (463) | |
| Married/Living together as married | 21.5 (127) | 31.7 (26) | 30.9 (25) | 23.6 (178) | |
| Divorced/Widowed | 14.4 (85) | 20.7 (17) | 13.6 (11) | 15.0 (113) | |
| Mean number of children: (95%CI) | 1.5 (1.47 – 1.60) | 1.9 (1.65 – 2.08) | 1.5 (1.29 – 1.71) | 1.6 (1.49 – 1.64) | |
| Current financial situation:* | <0.01 | ||||
| Has finances to meet all essential and nonessential needs | 19.0 (112) | 13.4 (11) | 3.7 (3) | 16.7 (126) | |
| Has finances to meet most needs | 43.0 (254) | 45.1 (37) | 17.3 (14) | 40.5 (305) | |
| Below the minimum necessary to live/Just able to meet basic needs | 38.1 (225) | 41.5 (34) | 79.0 (64) | 42.8 (323) | |
| Currently has another source of income* | 28.9 (171) | 24.4 (20) | 8.6 (7) | 26.3 (198) | 0.01 |
| Sex work characteristics (current) | |||||
| Working location as a sex worker* | <0.01 | ||||
| Street | 63.5 (375) | 64.6 (53) | 92.6 (75) | 66.7 (503) | |
| Non-street venue | 36.6 (216) | 35.4 (29) | 7.4 (6) | 33.3 (251) | |
| Duration of sex work involvement* | <0.001 | ||||
| < 1 year | 14.4 (85) | 1.2 (1) | 7.4 (6) | 12.2 (92) | |
| 1 to <2 years | 16.4 (97) | 9.8 (8) | 6.2 (5) | 14.6 (110) | |
| 2 to <3 years | 25.2 (149) | 23.2 (19) | 12.4 (10) | 23.6 (178) | |
| 3 to <4 years | 13.0 (77) | 13.4 (11) | 6.2 (5) | 12.3 (93) | |
| 4 or more years | 31.0 (183) | 52.4 (43) | 67.9 (55) | 37.3 (281) | |
| No of days selling sex per week:* | 0.02 | ||||
| 1 – 2 days | 8.4 (49) | 13.58 (11) | 3.7 (3) | 8.5 (63) | |
| 3 – 4 days | 43.9 (256) | 29.6 (24) | 27.2 (22) | 40.5 (302) | |
| 5 or more | 47.7 (278) | 56.8 (46) | 69.1 (56) | 51.0 (380) |
Significant at p<0.05;
marginally significant at p<0.10 in chi2 analysis of tabulations (adjusted for clustering);
Table 2 presents HIV prevalence sexual and structural HIV risk outcomes, and engagement in HIV prevention by injecting status. HIV prevalence, based on rapid HIV screening test, was significantly higher for active injectors (16.1%) and former injectors (8.5%), than non-injectors (1.5%, p<0.001). Higher proportions of active injectors (17.3%) reported unprotected anal sexual intercourse in the last six months, compared to former (4.9%) and non-injectors (4.4%; p=0.01). Police extortion in the last six months, including for money, sex, or information, was prevalent but varied across groups, with 23.7% of non-injectors, 35.4% of former injectors, and 55.6% of active injectors reporting any police extortion in the last six months (p=0.01). Likewise, client violence (last 6 months) –including, both physical and sexual- were varied across groups and was most common among active injectors. All groups estimated that approximately 31.7% of their male clients injected drugs. There was no difference in use of the Globus HIV prevention program by injection status, with approximately 35.3% of the sample utilizing outreach services and 39.8% utilizing both clinic and outreach services. New HIV diagnoses (instances in which the participant were first made aware of their positive HIV infection status during the study) were rare across all categories, though were more common among active injectors (4.3%), and former injectors (1.4%), compared to non-injectors (0.2%; p<0.01; data not shown).
Table 2.
HIV risk environment among female sex workers from three Russian cities, comparing injection drug use risk groups (N=754)
| Characteristic | Non-injecting (n=591) |
Formerly injecting (n= 82) |
Active injecting (n= 81) |
Total (n=754) |
p-value |
|---|---|---|---|---|---|
| % (n) | % (n) | % (n) | % (n) | ||
| HIV prevalence* | 1.5 (9) | 8.5 (7) | 16.1 (13) | 3.9 (29) | 0.001 |
| Sexual risk outcomes (last 6 months): | |||||
|
Avg. percentage of clients for oral sex Mean (95%CI) |
75.1 (66.0 – 84.2) | 90.1 (60.6 – 100) | 78.0 (69.0 – 87.0) | 78.0 (69.0 – 87.0) | |
|
Avg. percentage of clients for vaginal sex Mean (95%CI) |
80.9 (72.1 – 89.8) | 77.7 (48.8 – 100) | 78.2 (69.5 – 87.0) | 78.2 (69.5 – 87.0) | |
|
Avg. percentage of clients for anal sex Mean (95%CI) |
16.5 (8.4 – 24.7) | 9.6 (7.1 – 12.2) | 44.3 (0.1 – 88.8) | 18.8 (9.7 – 27.9) | |
| Condom use during vaginal sex** | 0.10 | ||||
| Always | 85.3 (504) | 91.5 (75) | 62.9 (51) | 83.6 (630) | |
| Any unprotected vaginal sex | 14.7 (87) | 8.5 (7) | 37.0 (30) | 16.5 (124) | |
| Condom use during anal sex | 0.01 | ||||
| Always or no anal sex | 95.6 (565) | 95.1 (78) | 82.7 (67) | 94.2 (710) | |
| Any unprotected anal sex | 4.4 (26) | 4.9 (4) | 17.3 (14) | 5.8 (44) | |
| Structural HIV risk outcomes: violence and coercion (last 6 months) | |||||
| Police extortion: Had to pay or compensate police to sell sex | |||||
| Yes, money* | 19.0 (112) | 31.7 (26) | 42.0 (34) | 22.8 (172) | 0.05 |
| Yes, sex* | 4.0 (23) | 6.1 (5) | 12.4 (10) | 5.0 (38) | 0.01 |
| Yes, information* | 2.7 (16) | 2.4 (2) | 9.9 (8) | 3.5 (26) | 0.03 |
| Any police extortion (at least one of the above)* | 23.7 (140) | 35.4 (29) | 55.6 (45) | 28.4 (214) | 0.01 |
| Physical violence by client* | 6.3 (37) | 6.1 (5) | 39.5 (32) | 9.8 (74) | 0.01 |
| Client coerced or physically forced to have vaginal sex* | 8.6 (51) | 9.7 (8) | 33.3 (27) | 11.4 (86) | 0.001 |
| Substance use (current): | |||||
| Substance use when trading sex: | |||||
| Alcohol | 68.0 (402) | 89.0 (73) | 59.3 (48) | 69.4 (523) | 0.03 |
| Legal drugs | 2.3 (14) | 8.5 (7) | 11.1 (9) | 4.0 (30) | 0.01 |
| More than one type of substance (including illegal drugs) | 5.1 (30) | 22.0 (18) | 51.9 (42) | 11.9 (90) | 0.01 |
|
Percentage of clients estimated to inject Mean (95%CI) |
31.2 (26.8 – 35.8) | 30.4 (24.5 – 36.2) | 36.4 (30.6 – 42.2) | 31.7 (28.0 – 35.4) | |
| Aware of transmission risk related to using a shared needle | 96.1 (568) | 93.9 (77) | 91.4 (74) | 95.4 (719) | 0.01 |
| Engagement in HIV services: | |||||
| Involved with GLOBUS via (last 12 months): | 0.36 | ||||
| None | 24.5 (145) | 14.6 (12) | 38.3 (31) | 24.9 (188) | |
| Outreach only | 33.8 (200) | 46.3 (38) | 34.6 (28) | 35.3 (266) | |
| GLOBUS program clinic + outreach | 41.6 (246) | 39.0 (32) | 27.2 (22) | 39.8 (300) | |
| Ever tested for HIV | 88.3 (515) | 97.6 (80) | 70.4 (57) | 87.4 (652) | 0.12 |
Significant at p<0.05;
marginally significant at p<0.10 in chi2 analysis of tabulations (adjusted for clustering);
Table 3 presents adjusted odds ratios for HIV status, sexual and structural HIV risk outcomes, and engagement in HIV services by injection status. This table presents a comparison of former and active injectors’ exposures to those of non-injectors (reference group) as well as comparison of active injectors to the reference of former injectors (fifth column). Adjusted odds of HIV infection was 4.5 times higher for former injectors and 6.7 times higher for active injectors, compared to non-injectors (p=0.01). Active injectors had greater odds of self-reported unprotected anal sex with clients, compared to non-injectors (AOR: 2.8; 95%CI: 1.2–6.4) and marginally higher than former injectors (AOR: 2.5; 95%CI: 0.8–7.6). Former injection status was associated with having at least 10% of clients request anal sex, relative to non-injectors (AOR: 2.1; 95%CI: 1.1–4.1). Contrary to this, there was no difference in unprotected vaginal sex among active or former injectors, compared to non-injectors, though the odds were four-fold higher among active injectors relative to former injectors (AOR: 4.3; 95%CI: 1.2–14.4). The odds of police extortion, including for money, sex, or any form of extortion were higher for active injectors when compared to both former and non-injectors. The odds of physical violence by clients were also higher for active injectors compared to both former (AOR: 7.7 95%CI: 2.2–27.1) and non-injectors (AOR:7.3; 95%CI: 2.1–24.7). Similar trends were observed with forced or coerced sex. With respect to engagement in HIV services, active injectors were less likely to use combinations of outreach and clinic for HIV prevention, than non-injectors (AOR: 0.3; 95%CI: 0.1–0.9), though use of outreach programs only were similar across groups.
Table 3.
Adjusted Odds Ratios of behavioral, structural and HIV outcomes among female sex workers from three Russian cities, comparing injection drug use risk groups (N=754)
| Characteristic: | Former compared to Non-injecting | Active compared to Non-injecting | Active compared to Former injecting |
|---|---|---|---|
| Adjusted OR (95%CI) (ref: non-injecting) | Adjusted OR (95%CI) (ref: non-injecting) | Adjusted OR (95%CI) (ref: former injecting) | |
| HIV prevalence | 4.5 (1.7 – 11.6)* | 6.7 (2.4 – 18.9)* | 1.5 (0.7 – 3.4) |
| Sexual risk outcomes (last 6 months): | |||
| Any unprotected vaginal sex | 0.7 (0.3 – 1.8) | 2.8 (0.6 – 13.4) | 4.3 (1.2 – 13.4)* |
| At least 10% of clients request anal sex | 2.1 (1.1 – 4.1)* | 1.6 (0.9–2.9)** | 0.8 (0.5 – 1.2) |
| Any unprotected anal sex | 1.1 (0.3 – 3.5) | 2.8 (1.2 – 6.4)* | 2.5 (0.8 – 7.6)** |
| Structural HIV risk outcomes: violence and coercion (last 6 months) | |||
| Police extortion: Had to pay or compensate police to sell sex | |||
| Yes, money | 1.4 (0.6 – 4.0) | 2.2 (1.1 – 4.7)* | 1.5 (0.6 – 3.6) |
| Yes, sex | 2.3 (0.8 – 6.4) | 3.2 (1.2–8.7)* | 1.4 (0.6 – 3.3) |
| Yes, information | 1.1 (0.3 – 4.5) | 3.0 (0.7 – 12.8) | 2.8 (0.3 – 26.6) |
| Any police extortion (reports at least one of the above) | 1.4 (0.6 – 3.3) | 3.0 (1.5 – 5.9)* | 2.2 (1.1 – 4.3)* |
| Physical violence by client* | 1.0 (0.3 – 2.8) | 7.3 (2.1–24.7)* | 7.7 (2.2 – 27.1)* |
| Client coerced or physically forced to have vaginal sex | 1.1 (0.6 – 2.2) | 3.3 (1.5 – 7.1)* | 2.9 (1.3 – 6.5)* |
| Engagement in HIV services: | |||
| Involved with GLOBUS via (last 12 months): | |||
| Outreach only | 1.5 (0.7 – 3.0) | 0.9 (0.3 – 2.6) | 0.6 (0.2 – 1.6) |
| GLOBUS program clinic + outreach | 0.7 (0.2 – 2.0) | 0.3 (0.1 – 0.9)* | 0.5 (0.1 – 2.1) |
| Ever tested for HIV | 2.5 (0.8 – 8.1) | 0.2 (0.0 – 1.0)** | 0.1 (0.0 – 0.2)* |
Significant at p<0.05;
Marginally significant at p<0.10; analysis adjusted for clustering by site and RDS sampling, adjusted for other confounders: age, financial status, income, days per week selling sex, duration of sex work, work location (street vs. non-street venue), alcohol use during sex work, legal drug use during sex work; Ref: reference category
Table 4 presents needle and syringe risks and use of harm reduction in the last six months among those who are currently injecting. Most of the women who were actively injecting reported injecting drugs prior to initiating sex work (70.4%). More than half reported both sharing used needles/syringes with others and using a shared needle or syringe. Approximately 48.2% reported currently using a needle exchange program.
Table 4.
Recent needle/syringe risks and harm reduction use among female sex workers who inject from three Russian cities (n=81)
| Characteristic (last 6 months) | Actively injecting (n= 81) |
|---|---|
| % (n) | |
| Timing of injecting drug use and sex work | |
| Initiated injecting drug use prior to sex work initiation | 70.4 (57) |
| Initiated injecting drug use and sex work at same time | 12.4 (10) |
| Initiated sex work use prior to injecting drug initiation | 17.3 (14) |
| Frequency sharing needles/syringes with others | |
| Never | 42.9 (34) |
| Sometimes or rarely | 54.3 (44) |
| Always or often | 3.7 (3) |
| Frequency using a shared needled/syringe | |
| Never | 0.00 (0) |
| Sometimes or rarely | 50.6 (41) |
| Always or often | 49.4 (40) |
| Frequency of using a new needle | |
| Never | 46.9 (38) |
| Sometimes | 50.6 (41) |
| At every injection | 2.5 (2) |
| Uses needle exchange program | 48.2 (39) |
Discussion
Overall, this study identifies variations in HIV risk profile based on injection status among FSWs from three cities in the Russian Federation. FSWs who reported no history of injection were exposed to some levels of violence, with 6–8% reporting recent physical or sexual client violence and 23% reporting recent police extortion. Relative to this group and controlling for other factors, active injectors had markedly higher HIV risk outcomes. These outcomes included increased risk for unprotected anal sex, police extortion, and physical and sexual violence perpetrated by clients. These findings suggest that risks among those who currently inject drugs extend beyond parenteral transmission, as injection drug use may exacerbate sexual and structural risks that are prevalent within the sex work environment. In this sample, active injection was reported by 11% of the FSW sample, but was marked by almost seven-fold greater odds of HIV infection, compared to those who had never injected. Compared to former injectors, active injectors also demonstrated increased sexual risks as well as client and police-perpetrated violence. Importantly, our findings also demonstrate that those FSWs who brought injecting practices to cessation had a risk profile that was closer to that of sex workers who reported never injecting drugs. Though former injectors had almost five times the odds of HIV infection, relative to non-injectors, the removal of the IDU risk environment appears to bring FSWs who had previously injected back to the level of risk that non-injectors face, in terms of sexual and structural risk outcomes.
The findings of increased recent unprotected vaginal and anal sex acts among active injectors and the potential for HIV acquisition related to anal sex should not be underestimated. Biologically, HIV transmission through anal intercourse is 16–18 times greater than penile-vaginal transmission.(Baggaley et al., 2013; Baggaley et al., 2010) In the context of sex work, condomless anal sex has also been associated with higher payment for service as well as forced sexual intercourse.(Schwandt, Morris, Ferguson, Ngugi, & Moses, 2006) In this sample, women who actively injected drugs reported lower levels of alternative income and street-based work and, likewise, increasing vulnerabilities to accepting riskier client sexual requests and experiencing client violence. These sexual and structural outcomes may be the result of making condom use decisions while under the influence of substances, or due to the need for increased income, barriers imposed by clients, lower capacity to select clients who are safer, and/or heavy policing activity, as it is in other settings.(Deering et al., 2013; Odinokova et al., 2014; Ulibarri et al., 2011) Even after controlling for other correlates of condom use, including income and financial status, as well as street-based sex work, active IDU remained highly associated with unprotected anal sex. As such, reducing IDU among FSW may provide secondary benefit by ultimately improving condom use during sex work.
Increased street-based sex work, police harassment, and client violence was more common among FSW-PWID than non-injectors or those who formerly injected. Ethnographies of FSW in the Russian Federation have described street-based FSW as the lowest rank of sex worker, often more vulnerable to police harassment and client violence.(Aral et al., 2003) Police harassment may lead to more hidden sex work practices and, in some cases, reduce condom use.(OSF, 2012) Prior research in Moscow has demonstrated the association of client violence and HIV outcomes.(Decker, Wirtz, Baral, et al., 2012) Longitudinal studies and meta-analyses of intimate partner violence demonstrate the temporal association of violence with HIV infection.(Jewkes, Dunkle, Nduna, & Shai, 2010; Li et al., 2014) These studies provide support to the potential transmission of HIV during client-perpetrated violence. Mathematical modeling of a similar HIV epidemic in Ukraine reciprocally demonstrated that reducing sexual violence against sex workers, including both anal and vaginal forced sex, can significantly reduce HIV incidence.(Decker et al., 2013) Mathematical models as well as prospective studies of community-based empowerment programs and safer work environments have also demonstrated reductions in violence and HIV incidence.(Beattie et al., 2010; Bekker et al., 2014; Jana, Basu, Rotheram-Borus, & Newman, 2004; Reza-Paul et al., 2008; Shannon, Strathdee, et al., 2014; Wirtz et al., 2014) Taken together, these studies suggest that reducing environmental risks of violence against FSW has important epidemic impacts. Bringing drug use to cessation among Russian FSWs may be one means to move women into environments where there are lower exposures to violence and reduced opportunities for HIV transmission or acquisition. In the Russian setting where access to effective drug treatment programs are limited, safer work places and community empowerment programs may provide alternative and acceptable means to reduce sexual and structural risks for those who are yet unable to bring drug use to cessation.
While this study demonstrated lower HIV risks among former and non-injectors, this does not imply that non-injecting sex workers are free of risks related to substance use. Former injectors still reported some levels of client violence and police extortion, suggesting that may violence continue even after cessation of IDU. High proportions of non- and former injectors reported using alcohol during sex work may impair sexual decision making, reduce use of protection methods, increase other risky sexual behaviors, and may be associated with increased HIV incidence.(Hutton et al., 2013; Vandepitte et al., 2013) Moreover, study participants, regardless of their injecting status, unanimously estimated that approximately 30% of their clients inject drugs. These clients may ultimately bridge the gap between drug use and sex work transmission networks, even for women who never or no longer inject. This is particularly relevant in the Russian context, where 44% of heterosexual PWIDs reported at least one sexual partner who was not injecting drugs and only one in four PWIDs reported consistent condom use with sexual partners.(N. Abdala et al., 2008; Eritsyan, Levina, White, Smolskaya, & Heimer, 2013)
The similarities in engagement of HIV prevention services among study participants and low proportion of undiagnosed infection suggest significant opportunities for HIV prevention for FSWs and FSW-PWIDs. FSW participants of the qualitative phase described periods of cessation followed by relapse through which they describe continuously utilizing Globus program resources, even during recidivism.(Decker, Wirtz, & Beyrer, 2012) This highlights the dynamic movement between the sex work and IDU environment (Figure 1) and the need to ensure access to HIV prevention and harm reduction across these stages. Reaching those women who engage in sex work and, including those who also inject drugs, is a necessity for HIV prevention programs in the Russian Federation. Harm reduction for FSW-PWID, such as needle exchange opportunities, can be efficiently included in HIV prevention programs for FSW.(WHO, UNAIDS, UNFPA, & NSWP, 2012) In the Russian Federation, provision of opiate substitution therapy (OST) is illegal; however, in other settings where there is significant overlap between sex work and IDU, linkage from sex work programs to OST may be particularly beneficial to addressing these risks.(Degenhardt et al., 2014) OST is one of the key harm reductions approaches recommended by the UNODC and WHO due to demonstrated improvements in reducing opiate dependency and, secondarily, reducing injecting behaviors and HIV infection, and improving adherence to ART treatment among those living with HIV.(MacArthur et al., 2012; Moatti et al., 2000; WHO, UNODC, & UNAIDS, 2012) In many settings, needle and syringe programs (NSPs) and referrals to OST programs have been effectively integrated within services for sex workers and key interventions for FSW have likewise been integrated within NSPs to address these overlapping risks.
Figure 1.
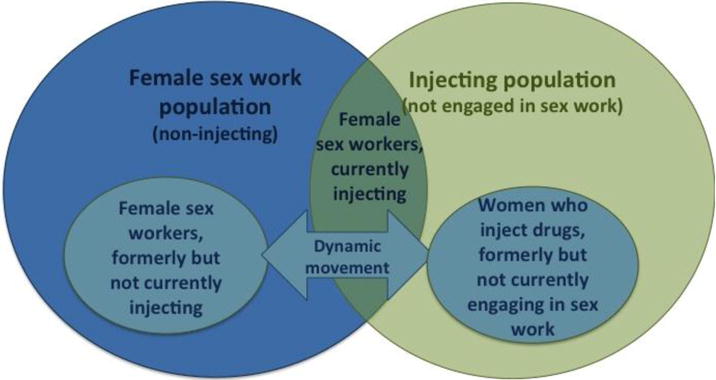
Dynamic movement between sex work and injecting drug use risk environments
Several limitations should be considered when reviewing these results. Relatively small numbers of FSWs with a history of injecting practices were enrolled in this study, limiting the precision of our estimates and should be interpreted with caution. The cross-sectional approach limits our ability to fully understand the temporal relationships among injection drug use and risk environment outcomes. The generalizability of these results to the wider FSW population in the study sites and wider Russian Federation is unknown; as with all behavioral studies, there may be selection bias induced by the voluntary nature of participation. The use of outreach workers for the initiation of seeds for RDS recruitment may have biased the sample towards inclusion of FSWs who have a history of engagement in HIV prevention programs. Markov chain theory, however, suggests that long RDS recruitment chains reduces the dependence on seeds and our estimates of engagement in HIV prevention programs and HIV testing are consistent with other studies of FSW, clients of FSW, and female PWID in the Russian Federation.(Heckathorn, 1997; King & Maman, 2013; Niccolai et al., 2012; Platt et al., 2009) Significant formative work was also conducted at the onset of this study to ensure that sampling reached across various street locations and venues. Unlike other studies conducted in the Russian Federation, which have predominantly recruited individual street-based sex workers, this study was able to recruit a range of sex workers, including those working individually on the street or through a range of venues, highlighting the heterogeneity of the sample. Limitations in obtaining self-reported network size data from participants prohibited the calculation of population-based RDS estimates, and estimates are thus reflective of the sample. Regions in which there was a range in prevalence of IDU among FSW were selected for inclusion. Thus, the results reported here, reflect the heterogeneity of risks among FSWs in these regions and may be less generalizable to regions of either extreme, e.g. where there is extremely high or low prevalence of HIV among PWIDs or where there is very low prevalence of injection behavior. Finally, we do not know how or why the former injectors cessated and this would be an important area to explore for future research.
The future of HIV prevention programs for key populations, such as the Globus program and other targeted prevention, are currently limited with the loss of the Global Fund and lack of support by the government.(Cohen, 2010) Vulnerable populations may become even more vulnerable in the near future due to politics and other environmental factors that prevent access to HIV prevention and treatment: drug use is criminalized, as is provision of opioid agonist therapy for treatment, and sex workers face structural risks, in addition to sexual risks. FSW in the Russian Federation face a range of sexual, structural, and HIV outcomes in the course of sex work. Our research demonstrates that actively injecting drugs appears to increase these outcomes, particularly those related to unprotected sex and violence. Moving FSW from injection drug use to non-use may be one step towards reducing outcomes that are seemingly inherent in the sex work risk environment. The few programs that remain need to be efficient and target the risk environment among FSW, including substance use, sexual risk, and experiences of violence and extortion. Targeted, non-stigmatizing programs for FSW may benefit by providing needle exchange services and following the example of the Globus program. These services may include comprehensive interventions to reduce sexual risks for HIV infection, addressing social risks and violence by providing resources for protection and social assistance, and discussing substance-using habits such as injection drug use and heavy alcohol intake.
Acknowledgments
This work was supported by the Global Fund through the Open Health Institute, the Johns Hopkins University Center for AIDS Research (1P30AI094189), and the National Institute on Drug Abuse (R03DA03569102). We thank the female sex workers who participated in this study, Svetlana Sadretdinova and her team at the Simona Clinic (Kazan, Russia), Marina Malisheva and Julia Burdina and their team at the Krasnyi Yar program (Krasnoyarsk, Russia), Nadezhda Ziryanova and Anna Petrova and their team at the Belaya Siren Project (Tomsk, Russia), Maria Ostrovskaya and Julia Kuznetzova for their coordination, and Shirin Kakayeva, Daesha Ramachandran, and Erin Pearson for qualitative analysis. We remember Marina Nikitina for her dedication to this work in Russia. We gratefully acknowledge the thoughtful feedback of two anonymous peer-reviewers.
Footnotes
Author Contributions:
ALW, MRD, CB, AP and VNM collaborated in the design and oversight of the study. MRD and ALW developed survey instruments; and ALW conducted statistical analysis in consultation with MRD, CB, AP and VNM. ALW wrote the initial drafts of this manuscript; MRD, CB, AP and VNM provided critical review. All authors had full access to the data, reviewed and edited the manuscript, and all take responsibility for its integrity as well as the accuracy of the analysis.
Conflicts of Interest:
The authors declare they have no conflicts of interest.
References
- Abdala N, Krasnoselskikh TV, Durante J, Timofeeva MY, Verevochkin SV, Kozlov AP. Sexually transmitted infections, sexual risk behaviors and the risk of heterosexual spread of HIV among and beyond IDUs in St. Petersburg, Russia. European Addiction Research. 2008;14:19–25. doi: 10.1159/000110407. [DOI] [PubMed] [Google Scholar]
- Abdala N, White E, Toussova OV, Krasnoselskikh TV, Verevochkin S, Kozlov AP, Heimer R. Comparing sexual risks and patterns of alcohol and drug use between injection drug users (IDUs) and non-IDUs who report sexual partnerships with IDUs in St. Petersburg, Russia. BMC Public Health. 2010;10:676. doi: 10.1186/1471-2458-10-676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aral SO, St Lawrence JS, Dyatlov R, Kozlov A. Commercial sex work, drug use, and sexually transmitted infections in St. Petersburg, Russia. Soc Sci Med. 2005;60(10):2181–2190. doi: 10.1016/j.socscimed.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Aral SO, St Lawrence JS, Tikhonova L, Safarova E, Parker KA, Shakarishvili A, Ryan CA. The social organization of commercial sex work in Moscow, Russia. Sexually Transmitted Diseases. 2003;30(1):39–45. doi: 10.1097/00007435-200301000-00009. [DOI] [PubMed] [Google Scholar]
- Arps FS, Golichenko M. Sex workers, unite! (Litigating for sex workers’ freedom of association in Russia) Health Hum Rights. 2014;16(2):E24–34. [PubMed] [Google Scholar]
- Baggaley RF, Dimitrov D, Owen BN, Pickles M, Butler AR, Masse B, Boily MC. Heterosexual anal intercourse: a neglected risk factor for HIV? Am J Reprod Immunol. 2013;69(Suppl 1):95–105. doi: 10.1111/aji.12064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggaley RF, White RG, Boily MC. HIV transmission risk through anal intercourse: systematic review, meta-analysis and implications for HIV prevention. International Journal of Epidemiology. 2010;39(4):1048–1063. doi: 10.1093/ije/dyq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, Kerrigan D. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet Infectious Diseases. 2012 doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- Beattie TS, Bhattacharjee P, Ramesh BM, Gurnani V, Anthony J, Isac S, … Moses S. Violence against female sex workers in Karnataka state, south India: impact on health, and reductions in violence following an intervention program. BMC Public Health. 2010;10:476. doi: 10.1186/1471-2458-10-476. (Journal Article) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekker LG, Johnson L, Cowan F, Overs C, Besada D, Hillier S, Cates W., Jr Combination HIV prevention for female sex workers: what is the evidence? Lancet. 2014 doi: 10.1016/S0140-6736(14)60974-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard JF, Aral SO. Emergent properties and structural patterns in sexually transmitted infection and HIV research. Sexually Transmitted Infections. 2010;86(Suppl 3):iii4–iii9. doi: 10.1136/sti.2010.046037. [DOI] [PubMed] [Google Scholar]
- Cohen J. Praised Russian prevention program faces loss of funds. Science. 2010;329(5988):168. doi: 10.1126/science.329.5988.168. [DOI] [PubMed] [Google Scholar]
- Decker MR, Wirtz AL, Baral SD, Peryshkina A, Mogilnyi V, Weber RA, Beyrer C. Injection drug use, sexual risk, violence and STI/HIV among Moscow female sex workers. Sex Transm Infect. 2012 doi: 10.1136/sextrans-2011-050171. doi: sextrans-2011-050171 [pii] 10.1136/sextrans-2011-050171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Decker MR, Wirtz AL, Beyrer C. Evaluation Report: GLOBUS HIV Prevention Program for Commercial Sex Workers. Baltimore, MD: Center for Public Health and Human Rights, Johns Hopkins School of Public Health; 2012. [Google Scholar]
- Decker MR, Wirtz AL, Moguilnyi V, Peryshkina A, Ostrovskaya M, Nikita M, Beyrer C. Female Sex Workers in Three Cities in Russia: HIV Prevalence, Risk Factors and Experience with Targeted HIV Prevention. AIDS and Behavior. 2014;18(3):562–572. doi: 10.1007/s10461-013-0577-y. [DOI] [PubMed] [Google Scholar]
- Decker MR, Wirtz AL, Pretorius C, Sherman SG, Sweat MD, Baral SD, Kerrigan DL. Estimating the impact of reducing violence against female sex workers on HIV epidemics in Kenya and Ukraine: a policy modeling exercise. Am J Reprod Immunol. 2013;69(Suppl 1):122–132. doi: 10.1111/aji.12063. [DOI] [PubMed] [Google Scholar]
- Deering KN, Rusch M, Amram O, Chettiar J, Nguyen P, Feng CX, Shannon K. Piloting a ‘spatial isolation’ index: The built environment and sexual and drug use risks to sex workers. The International Journal on Drug Policy. 2013 doi: 10.1016/j.drugpo.2013.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Mathers BM, Wirtz AL, Wolfe D, Kamarulzaman A, Carrieri MP, Beyrer C. What has been achieved in HIV prevention, treatment and care for people who inject drugs, 2010–2012? A review of the six highest burden countries. The International Journal on Drug Policy. 2014;25(1):53–60. doi: 10.1016/j.drugpo.2013.08.004. [DOI] [PubMed] [Google Scholar]
- El-Bassel N, Shaw SA, Dasgupta A, Strathdee SA. Drug use as a driver of HIV risks: re-emerging and emerging issues. Current Opinion in HIV and AIDS. 2014;9(2):150–155. doi: 10.1097/COH.0000000000000035. 110.1097/COH.0000000000000035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elovich R, Drucker E. On drug treatment and social control: Russian narcology’s great leap backwards. Harm Reduct J. 2008;5:23. doi: 10.1186/1477-7517-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eritsyan KU, Levina OS, White E, Smolskaya TT, Heimer R. HIV prevalence and risk behavior among injection drug users and their sex partners in two Russian cities. AIDS Research and Human Retroviruses. 2013;29(4):687–690. doi: 10.1089/AID.2012.0161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Social Problems. 1997;44(2):174–199. doi: 10.1525/sp.1997.44.2.03x0221m. [DOI] [Google Scholar]
- Hutton H, McCaul M, Chander G, Jenckes M, Nollen C, Sharp V, Erbelding E. Alcohol Use, Anal Sex, and Other Risky Sexual Behaviors Among HIV-Infected Women and Men. AIDS and Behavior. 2013;17(5):1694–1704. doi: 10.1007/s10461-012-0191-4. [DOI] [PubMed] [Google Scholar]
- Jana S, Basu I, Rotheram-Borus MJ, Newman PA. The Sonagachi Project: a sustainable community intervention program. AIDS education and prevention: official publication of the International Society for AIDS Education. 2004;16(5):405–414. doi: 10.1521/aeap.16.5.405.48734. [DOI] [PubMed] [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. Lancet. 2010;376(9734):41–48. doi: 10.1016/s0140-6736(10)60548-x. [DOI] [PubMed] [Google Scholar]
- King EJ, Maman S. Structural barriers to receiving health care services for female sex workers in Russia. Qual Health Res. 2013;23(8):1079–1088. doi: 10.1177/1049732313494854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Marshall CM, Rees HC, Nunez A, Ezeanolue EE, Ehiri JE. Intimate partner violence and HIV infection among women: a systematic review and meta-analysis. Journal of the International AIDS Society. 2014;17:18845. doi: 10.7448/IAS.17.1.18845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacArthur GJ, Minozzi S, Martin N, Vickerman P, Deren S, Bruneau J, Hickman M. Opiate substitution treatment and HIV transmission in people who inject drugs: systematic review and meta-analysis. BMJ. 2012;345:e5945. doi: 10.1136/bmj.e5945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher L, Mooney-Somers J, Phlong P, Couture MC, Stein E, Evans J, Collaborative, t. Y. W. s. H. S. Selling sex in unsafe spaces: sex work risk environments in Phnom Penh, Cambodia. Harm Reduction Journal. 2011;8(1):30. doi: 10.1186/1477-7517-8-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malekinejad M, Johnston LG, Kendall C, Kerr LR, Rifkin MR, Rutherford GW. Using respondent-driven sampling methodology for HIV biological and behavioral surveillance in international settings: a systematic review. AIDS and behavior. 2008;12(4 Suppl):S105–130. doi: 10.1007/s10461-008-9421-1. [DOI] [PubMed] [Google Scholar]
- Mazhnaya A, Andreeva TI, Samuels S, DeHovitz J, Salyuk T, McNutt LA. The potential for bridging: HIV status awareness and risky sexual behaviour of injection drug users who have non-injecting permanent partners in Ukraine. Journal of the International AIDS Society. 2014;17:18825. doi: 10.7448/IAS.17.1.18825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moatti JP, Carrieri MP, Spire B, Gastaut JA, Cassuto JP, Moreau J. Adherence to HAART in French HIV-infected injecting drug users: the contribution of buprenorphine drug maintenance treatment. The Manif 2000 study group. AIDS. 2000;14(2):151–155. doi: 10.1097/00002030-200001280-00010. [DOI] [PubMed] [Google Scholar]
- Niccolai LM, Odinokova VA, Safiullina LZ, Bodanovskaya ZD, Heimer R, Levina OS, Rusakova MM. Clients of street-based female sex workers and potential bridging of HIV/STI in Russia: results of a pilot study. AIDS Care. 2012;24(5):665–672. doi: 10.1080/09540121.2011.630356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odinokova V, Rusakova M, Urada LA, Silverman JG, Raj A. Police sexual coercion and its association with risky sex work and substance use behaviors among female sex workers in St. Petersburg and Orenburg, Russia. The International Journal on Drug Policy. 2014;25(1):96–104. doi: 10.1016/j.drugpo.2013.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- OSF. Criminalizing Condoms. NY: Open Society Foundation; 2012. http://www.opensocietyfoundations.org/sites/default/files/criminalizing-condoms-20120717.pdf. [Google Scholar]
- Platt L, Jolley E, Rhodes T, Hope V, Latypov A, Reynolds L, Wilson D. Factors mediating HIV risk among female sex workers in Europe: a systematic review and ecological analysis. BMJ Open. 2013;3(7) doi: 10.1136/bmjopen-2013-002836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt L, Rhodes T, Judd A, Koshkina E, Maksimova S, Latishevskaya N, Parry JV. Effects of sex work on the prevalence of syphilis among injection drug users in 3 Russian cities. American Journal of Public Health. 2007;97:478–485. doi: 10.2105/AJPH.2005.069732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Platt L, Rhodes T, Lowndes CM, Madden P, Sarang A, Mikhailova L, Khutorskoy M. Impact of Gender and Sex Work on Sexual and Injecting Risk Behaviors and Their Association With HIV Positivity Among Injecting Drug Users in an HIV Epidemic in Togliatti City, Russian Federation. Sexually Transmitted Diseases. 2005;32:605–612. doi: 10.1097/01.olq.0000175391.13947.f7. [DOI] [PubMed] [Google Scholar]
- Platt L, Sutton AJ, Vickerman P, Koshkina E, Maximova S, Latishevskaya N, Rhodes T. Measuring risk of HIV and HCV among injecting drug users in the Russian Federation. European Journal of Public Health. 2009;19:428–433. doi: 10.1093/eurpub/ckp041. [DOI] [PubMed] [Google Scholar]
- Reza-Paul S, Beattie T, Syed HU, Venukumar KT, Venugopal MS, Fathima MP, Moses S. Declines in risk behaviour and sexually transmitted infection prevalence following a community-led HIV preventive intervention among female sex workers in Mysore, India. AIDS (London, England) 2008;22(Suppl 5):S91–100. doi: 10.1097/01.aids.0000343767.08197.18. Journal Article. [DOI] [PubMed] [Google Scholar]
- Rhodes T. The ‘risk environment’: a framework for understanding and reducing drug-related harm. International Journal of Drug Policy. 2002;13:85–94. [Google Scholar]
- Rhodes T. Risk environments and drug harms: A social science for harm reduction approach. International Journal of Drug Policy. 2009;20(3):193–201. doi: 10.1016/J.Drugpo.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Schwandt M, Morris C, Ferguson A, Ngugi E, Moses S. Anal and dry sex in commercial sex work, and relation to risk for sexually transmitted infections and HIV in Meru, Kenya. Sexually Transmitted Infections. 2006;82(5):392–396. doi: 10.1136/sti.2006.019794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon K, Goldenberg SM, Deering KN, Strathdee SA. HIV infection among female sex workers in concentrated and high prevalence epidemics: why a structural determinants framework is needed. Current Opinion in HIV and AIDS. 2014;9(2):174–182. doi: 10.1097/COH.0000000000000042. 110.1097/COH.0000000000000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shannon K, Strathdee SA, Goldenberg SM, Duff P, Mwangi P, Rusakova M, Boily MC. Global epidemiology of HIV among female sex workers: influence of structural determinants. The Lancet. 2014;(0) doi: 10.1016/S0140-6736(14)60931-4. doi: http://dx.doi.org/10.1016/S0140-6736(14)60931-4. [DOI] [PMC free article] [PubMed]
- STATaCorp. Survey Data Reference Manual. College Park: StataCorp; 2011. [Google Scholar]
- Strathdee SA, Hallett TB, Bobrova N, Rhodes T, Booth R, Abdool R, Hankins CA. HIV and risk environment for injecting drug users: the past, present, and future. The Lancet. 2010;376(9737):268–284. doi: 10.1016/S0140-6736(10)60743-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szwarcwald CL, de Souza PR, Junior, Damacena GN, Junior AB, Kendall C. Analysis of data collected by RDS among sex workers in 10 Brazilian cities, 2009: estimation of the prevalence of HIV, variance, and design effect. Journal of acquired immune deficiency syndromes. 2011;57(Suppl 3):S129–135. doi: 10.1097/QAI.0b013e31821e9a36. [DOI] [PubMed] [Google Scholar]
- Ulibarri MD, Strathdee SA, Ulloa EC, Lozada R, Fraga MA, Magis-RodrÃ‐guez C, Patterson TL. Injection drug use as a mediator between client-perpetrated abuse and HIV status among female sex workers in two mexico-US border cities. AIDS Behavior. 2011;12(1):179–185. doi: 10.1007/s10461-009-9595-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. UNAIDS Report on the Global AIDS Epidemic, 2012. Geneva: UNAIDS; 2012. [Google Scholar]
- Vandepitte J, Weiss HA, Bukenya J, Nakubulwa S, Mayanja Y, Matovu G, Grosskurth H. Alcohol Use, Mycoplasma genitalium, and Other STIs Associated With HIV Incidence Among Women at High Risk in Kampala, Uganda. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2013;62(1):119–126. doi: 10.1097/QAI.0b013e3182777167. 110.1097/QAI.1090b1013e3182777167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO, UNAIDS, UNFPA, & NSWP. Prevention and treatment of HIV and other sexually transmitted infections for sex workers in low- and middle-income countries: recommendations for a public health approach. Geneva: World Health Organization; 2012. [PubMed] [Google Scholar]
- WHO, UNODC & UNAIDS. WHO, UNODC, UNAIDS technical guide for countries to set targets for universal access to HIV prevention, treatment and care for injecting drug users – 2012 revision. Geneva: World Health Organization; 2012. [Google Scholar]
- Wirtz AL, Pretorius C, Beyrer C, Baral S, Decker MR, Sherman SG, Kerrigan D. Epidemic impacts of a community empowerment intervention for HIV prevention among female sex workers in generalized and concentrated epidemics. PLoS One. 2014;9(2):e88047. doi: 10.1371/journal.pone.0088047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurth MH, Schleifer R, McLemore M, Todrys KW, Amon J. Condoms as evidence of prostitution in the United States and the criminalization of sex work. 2013 doi: 10.7448/IAS.16.1.18626. [DOI] [PMC free article] [PubMed] [Google Scholar]


