Abstract
Background
Common mental disorders (CMD) during pregnancy can have a clearly harmful influence on both mothers and children. Some studies have reported related factors for mental disorders, such as region-specific background. This study examined the prevalence of CMD and its related factors in mid-pregnancy in Japan.
Methods
Pregnant women between 12 and 24 weeks gestation and aged ≥20 years were consecutively recruited at a maternity hospital in Japan between May 2014 and September 2014. CMD were diagnosed using the Mini-International Neuropsychiatric Interview (MINI), self-rated depressive symptoms were assessed using the Edinburgh Postnatal Depression Scale, and interpersonal traumatic experience was measured using the Life Events Checklist.
Results
Among 297 eligible pregnant women, 177 participated in the study. Two participants (1.1 %) met the criteria for major depressive disorder. The most frequent diagnosis was agoraphobia (n = 7; 3.9 %). Eleven participants (6.2 %) met the criteria for one or more diagnoses, with 2 participants having two mental disorders and 3 having three mental disorders. Six participants developed CMD after gestation. Logistic regression analysis revealed history of psychiatric disorder, past interpersonal traumatic experience, and feeling pressure to have a child were associated with CMD.
Conclusion
These findings indicate a lower prevalence of CMD in mid-pregnancy in Japan than reported in most other countries. Besides the related factors reported previously, feeling pressure to have a child might increase risk for CMD among pregnant women in Japan. Asian cultural background might be related to the lower CMD prevalence and risk factors identified in this study.
Keywords: Pregnancy, Prevalence, Common mental disorders, Structured interview
Background
Depression during pregnancy has widespread negative effects on mothers and babies including increased risks for preterm birth, low birth weight, postpartum depression, self-harm or suicide, failure to seek prenatal care, difficulty performing usual activities, poor diet, and tobacco and alcohol use [1, 2]. The effects of common mental disorders (CMD), which usually include not only mood disorders but anxiety and substance abuse disorders, on both pregnant women and their babies have also drawn attention. For instance, posttraumatic stress disorder (PTSD) during pregnancy was recently shown to increase the risk for preterm birth [3]. Prevalence of antenatal depression varies between 5.2 and 17.8 % worldwide [4–9] and for anxiety disorder varies between 0.0 and 10.5 % [3, 5, 7–11].
Sociocultural as well as methodological differences might account for some of the variance. It has been suggested that Asian populations report symptoms less often partly due to stigma [12, 13] and that some of the risk factors for depression and CMD might be relatively uncommon in Asia [14]. As an example, postpartum depression was more prevalent among women in India and China who gave birth to a girl than those who gave birth to a boy [15, 16], but no such trend was found among women in Western countries [17]. According to some researchers, the source of the still deeply ingrained gender preference in favor of boys in Asia is that male children carry on the family name, the family business, and contribute financially to the family [16, 18].
For over 150 years, Japan has been greatly affected by Western culture, while at the same time has retained its cultural identity in many ways. It would be highly relevant, therefore, to examine from a sociocultural perspective the prevalence and risk factors for CMD during pregnancy in Japan. While the prevalence and risk factors for CMD among pregnant women expecting their first babies have been investigated in a study involving clinics affiliated with medical universities [5], the findings might not generalize to pregnant women with children. Moreover, fewer than 10 % of pregnant women give birth at university hospitals in Japan [19, 20], and women who do so might have different characteristics from the majority of women who give birth in non-university hospital clinics.
This study aimed first to clarify prevalence and related factors of CMD by conducting a standardized structured interview among pregnant women in a local hospital, and second to compare these findings with those in other countries.
Methods
Participants
Participants were consecutively recruited from Tuesday to Friday between May 2014 and September 2014 at Toda Chuo Women’s Hospital (TCWH), Saitama Prefecture, which is located in the greater Tokyo area. Recruitment was not carried out on Mondays due to schedule conflicts among the research team, however, pregnant women who visited TCWH on Mondays did not differ significantly in terms of age or Edinburgh Postnatal Depression Scale (EPDS) scores from those who attended on other days of the week. Eligibility criteria for all pregnant women were: (1) 12–24 weeks of gestation, (2) age ≥20 years, and (3) ability to read and write Japanese. Based on previous studies [21, 22], we estimated that 6 % of pregnant women would have EPDS scores of ≥9, with a positive predictive value of 50 %; thus, prevalence of depression would be 3 %. We also estimated that width of the 95 % confidence interval (CI) would be 3 % with a power of 0.6. Therefore, 173 participants would be needed for the study.
Figure 1 shows the flowchart of recruitment. From May 2014 to September 2014, of 277 women approached out of 297 potentially eligible women, 20 were failed to contact, 12 had no ability of Japanese, and 4 (aged < 20 years) were excluded. Among 261 women, 177 (67.8 %) agreed to participate in the study.
Fig. 1.
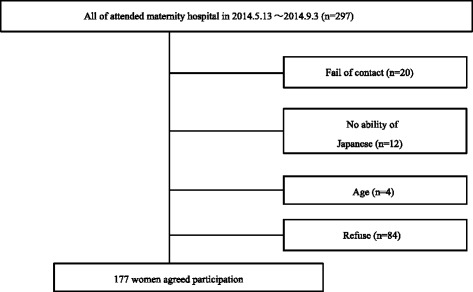
Flow chart of the study
Measures and procedures
This study was conducted with the approval of the Institutional Review Board of TCWH. All pregnant women who attended TCWH during the study period were asked to take the EPDS and received a brief explanation of the study. Eligible women were provided a complete description of the study during their next visit, at which time written informed consent was obtained. After the assessment, each participant received a gift voucher (2,000 JPY [17 USD]) for their participation.
A questionnaire inquired about participants’, gestational age, age, education level, work status, household income in one year, marriage status, smoking status (never, current, or past), number of family members, planned pregnancy (yes, no), pressures related to having a child (yes, no), past psychiatric history (yes, no), family psychiatric history (yes, no), and childbirth experience (primipara or unipara/multipara).
The Mini-International Neuropsychiatric Interview (MINI) [23] is a brief (15–30 min) structured interview widely used to evaluate the presence of Axis I psychiatric disorders, as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition [24]. Assessment in this study included the following psychiatric disorders: major depressive episodes, dysthymia, manic and hypomanic episodes, generalized anxiety disorder, panic disorders, agoraphobia, obsessive-compulsive disorder, posttraumatic stress disorder, bulimia and anorexia nervosa, and alcohol or other substance dependence, which were defined as CMD in the study. The MINI was conducted by three trained examiners, namely, a trained psychiatrist (DN), who trained two clinical psychologists (KU, MM) through lectures and role playing. To assess inter-rater reliability, the three raters (one conducting the interview and one observing) assessed a random sample of 10 cases. Ratings were reliable for all diagnoses without psychotic disorders, with kappa values of 1.0.
Self-report depressive symptoms were obtained using the EPDS, which is used most often for screening perinatal depression in international research. This self-report measure focuses on cognitive symptoms of depression, excluding somatic items that can generate false positives during pregnancy and postpartum [25]. The EPDS, which has been validated in Japan [22], comprises 10-items, scored 0–3 points per item for a potential scale score of 0–30.
The Life Events Checklist, which was developed alongside with the Clinician-Administered PTSD Scale, was used to assess interpersonal traumatic experience [26, 27]. Participants were asked if they had ever experienced an interpersonal traumatic event known to potentially cause PTSD in their lifetime, such as interpersonal violence, weapon assault, confinement, sexual violence, other harmful sexual experience, and physical abuse.
Statistical analysis
We calculated the prevalence (95 % CI) of CMD. To establish a model of factors related to CMD, we selected the following factors as basic background information: age, work status, and family psychiatric history. Work status was coded as 0 (part-time, not working, or student) or 1 (working full-time), and family psychiatric history as 0 (no history of psychiatric hospitalization (awareness of problem but no visit) or 1 (apparent mental symptoms).
Psychiatric history [7, 28], primipara [11], past interpersonal traumatic experiences [11, 28], work status and feeling pressure to have a child were selected because previous studies showed these variables were associated with CMD during pregnancy. Regarding work status, having regular jobs might be protective for depressive symptoms [29, 30].
Also, there seems to be the common wish in Asia to have a male child to carry on the family name. Feeling pressure to have a child is particularly relevant for pregnant women between 12 and 24 weeks of gestation who might not yet know the sex of the fetus. Additionally, marriage status [7], home crowding [9], number of children [7] and alcohol consumption [9] are reported to be factors related to mental disorder or current suicide risk. However, we excluded these factors from analysis because each included <10 participants in this study.
We performed bivariate and multivariable logistic regression analyses to identify independent significant factors associated with CMD during pregnancy, and reported odds ratios and 95 % CIs. All statistical analysis was performed using SPSS statistical software, version 22.0 for Windows (IBM Corporation, Armonk, NY). All tests were two-sided, and p-values ≤0.05 were considered statistically significant.
Results
Prevalence of CMD
The demographic characteristics are shown in Table 1. Table 2 shows CMD prevalence in the second trimester. Two participants (1.1 %) met the criteria for major depressive disorder. The most frequent diagnosis was agoraphobia (n = 7; 3.9 %). Also, 11 (6.2 %) participants met the criteria for one or more diagnoses: 2 had two mental disorders and 3 had three mental disorders. Six women of the 11 women developed CMD after gestation.
Table 1.
Demographic and characteristics of pregnant women who participated in the study
| Variables | Number | Percent | Mean | SD |
|---|---|---|---|---|
| Gestational age (week) | 177 | 17.26 | 1.707 | |
| Age | 177 | 31.15 | 4.378 | |
| Education | ||||
| Junior high school | 5 | 2.8 | ||
| High school | 37 | 20.9 | ||
| Junior or technical college | 67 | 37.9 | ||
| University or more | 68 | 38.4 | ||
| Work | ||||
| No job or part time | 116 | 65.5 | ||
| Full time job | 61 | 34.5 | ||
| Household income | ||||
| < 3million yen | 14 | 7.9 | ||
| 3million yen ~ 5million yen | 55 | 31.1 | ||
| 5million yen ~ 7million yen | 61 | 34.5 | ||
| ≧7million yen | 47 | 26.6 | ||
| Marriage status | ||||
| Marriage | 169 | 95.5 | ||
| Commuter marriage | 1 | 0.6 | ||
| Cohabitation | 1 | 0.6 | ||
| Remarriage | 1 | 0.6 | ||
| Going to get Married | 5 | 2.8 | ||
| Number of family members | ||||
| 1 person | 1 | 0.6 | ||
| 2 persons | 96 | 54.2 | ||
| 3 persons ≦ | 80 | 45.2 | ||
| Smoke | ||||
| Never smoke | 133 | 75.1 | ||
| Current smoke | 0 | 0 | ||
| past smoke | 44 | 24.9 | ||
| Birth experience | ||||
| Primipara | 97 | 54.8 | ||
| Unipara or Multipara | 80 | 45.2 | ||
| Planned pregnancy, yes | 117 | 66.1 | ||
| Pressure to give birth to child, yes | 28 | 15.8 | ||
| Past psychiatric history, yes | 20 | 11.3 | ||
| Past psychiatric history of family, yes | 15 | 8.5 | ||
| Interpersonal traumatic experience, yes | 16 | 9.0 | ||
| EPDS score | 177 | 2.82 | 3.052 |
Table 2.
Prevalence of psychiatric diagnosis at gestational age 12 weeks to 24 weeks in a local maternity hospital (Total = 177)
| Diagnosis | Number | % (95 % CI) |
|---|---|---|
| Mood disorders | ||
| Major depression | 2 | 1.1 (0.00–0.04) |
| Dysthymia | 0 | 0.0 (0.00–0.00) |
| Manic episode | 0 | 0.0 (0.00–0.00) |
| Anxiety disorders | ||
| Panic disorder | 2 | 1.1 (0.00–0.04) |
| Agoraphobia | 7 | 3.9 (0.02–0.08) |
| Social anxiety disorder | 2 | 1.1 (0.00–0.04) |
| Generalized anxiety disorder | 3 | 1.7 (0.01–0.05) |
| Obsessive-compulsive disorder | 1 | 0.6 (0.00–0.03) |
| PTSD (Post traumatic stress disorder) | 0 | 0.0 (0.00–0.00) |
| Substance use disorders | ||
| Alcohol dependence | 2 | 1.1 (0.00–0.04) |
| Alcohol abuse | 0 | 0.0 (0.00–0.00) |
| Drug dependence | 0 | 0.0 (0.00–0.00) |
| Drug abuse | 0 | 0.0 (0.00–0.00) |
| Eating disorders | ||
| Anorexia nervosa | 0 | 0.0 (0.00–0.00) |
| Bulimia nervosa | 0 | 0.0 (0.00–0.00) |
| At least one diagnosis | 11 | 6.2 (0.03–0.11) |
Related factors for CMD
Table 3 gives the results of bivariate and multivariate logistic regression analysis, with CMD as a dependent variable. In bivariate logistic regression analysis, CMD was significantly associated with younger age, past psychiatric history, family psychiatric history, planned pregnancy, and interpersonal traumatic experience In multivariate logistic regression analysis, CMD was significantly associated with psychiatric history, interpersonal traumatic experience, and feeling pressure to have a child.
Table 3.
The result of logistic bivariate and multivariate regression analyses (n = 177)
| Variables | Bivariate | P | Multivariate | P |
|---|---|---|---|---|
| OR (95 % CI) | OR (95 % CI) | |||
| Age | 0.32 (0.04–2.54) | 0.28 | 0.80 (0.65–1.00) | 0.04 |
| Full time work, yes | 0.40 (0.08–1.93) | 0.26 | 0.12 (0.01–1.54) | 0.10 |
| Past psychiatric history, yes | 13.03 (3.53–48.14) | <0.01** | 6.80 (1.41–32.52) | 0.02* |
| Family past psychiatric history, yes | 4.81 (1.13–20.54) | 0.03* | 6.27 (0.94–41.80) | 0.06 |
| Birth experience, yes | 0.25 (0.05–1.20) | 0.08 | 0.44 (0.06–3.56) | 0.44 |
| Past interpersonal traumatic experiences, yes | 7.33 (1.88–28.62) | <0.01** | 10.91 (1.61–74.10) | 0.01* |
| Pressure to give birth to child, yes | 3.38 (0.92–12.44) | 0.07 | 11.56 (1.47–91.02) | 0.02* |
OR odds ratio, CI confidence interval
**p < 0.01、*p < 0.05
Discussion
Prevalence of major depressive disorder (MDD) and CMD was 1.1 and 6.2 %, respectively, which are much lower figures than seen in other countries [3, 6–11]. Such prevalence was comparable to the point prevalence in the general population in Japan [31]. It is well known that prevalence of CMD is in general lower in Asia than in other regions [32]. Aside from the stigma attached to having CMD, people in Asia seek treatment only when their symptoms cause significant impairment [12], which could reduce symptom reporting. Also, some researchers have suggested that the prevalence rate of PTSD might be related to the infant mortality rate, which is a sign of social circumstance and basic population health [33]. These cultural factors might explain the low prevalence of CMD we found among pregnant women in Japan. This low prevalence is also lower than that found for MDD (5.6 %) and CMD (12.1 %) among women in Japan expecting their first babies in clinics affiliated with medical universities [5]: some of the pregnant women who had visited university hospitals might have received fertility treatment or had complications, which also could account for the higher reported prevalence.
Feeling pressure to have a child was significantly associated with CMD, and might reflect traditional beliefs still present in Japan, where continuity of the family name is greatly valued. A previous study in Vietnam showed that strong gender preference increased the risk for CMD, although such women with CMD were likely to recover before late pregnancy [34]. On the other hand, dissatisfaction with a newborn baby’s sex was shown to be associated with postnatal depression among Japanese pregnant women who had their first baby [5]. Whether the impact of feeling pressure to have a child predicts depression in late pregnancy or after childbirth should be further elucidated.
There could be another cultural explanation why feeling pressure to have a child was associated with CMD. Many Asian cultures, including Japanese culture, emphasize connecting to, attending to, and fitting in with others [35]. Other people are critical for self-validation in these interdependent cultures, and people are motivated to find a way to fit in with relevant others, which sometimes engenders a sense of obligation [35]. The goals of relevant others are sometimes experienced as one’s personal goals, or meeting others’ goals might be a necessary requirement for satisfying one’s own goals [35]. Thus, some pregnant women might feel stressed when they compare themselves to other women who already have children or when faced with the high expectations of their husbands and in-laws that they produce a child without any complications.
Although unplanned pregnancy was not associated with CMD in this study, many previous studies have shown an association [7, 11, 28, 36], which might be due to Japan’s relatively high rate of elective abortions [37]. In the present study, we recruited only women with planned pregnancies; we did not recruit those with unplanned pregnancies who chose to terminate their pregnancy, which might have affected the results.
Past interpersonal traumatic experience was found to be significantly associated with CMD, which is consistent with the findings of previous studies [9, 28, 34]. Past interpersonal traumatic experience is past traumatic events in their lifetime, such as interpersonal violence, weapon assault, confinement, sexual violence, other harmful sexual experience, and physical abuse. Not surprisingly, past psychiatric history was associated with CMD. It is well known that the prevalence of CMD and suicidal behavior is higher in women who have been exposed to gender-based violence [38]. Therefore, clinicians should be alert to pregnant women’s past traumatic experience as well as past psychiatric history.
Younger age almost reached statistical significance. Findings of previous studies on age have been inconsistent, with older age shown to be associated with CMD in Vietnam [11, 34] but found to be protective for CMD in Japan [5] and the United States [39]. In Vietnam, women usually marry in their early 20's and have their first baby by age 25. Women over age 30 who are having a first or second baby might reflect difficulties establishing a partnership due to stigmatizing circumstances such as personal or family mental health problems, extreme poverty, or fertility problems [34]. However, in countries without these cultural circumstances, older age might not be a risk factor for CMD among pregnant women. In Japan, the trend is towards having children later in life [40], with no stigma against relatively older pregnant women. Also, being older is sometimes associated with economic stability or increased resilience to stressful events.
The strengths of this study are the use of reliable and standardized assessments and consecutive sampling. However, there are several limitations. First, approximately 30 % of pregnant women who refused to participate in the study had EPDS scores that were significantly higher than those of the participants, suggesting that they might be burdened further by participating. Therefore, prevalence might be underestimated in this study. Second, a relatively small number of women met the diagnostic criteria of various psychiatric disorders, although data from participants consecutively recruited in this study might provide valuable additional evidence to that of previous studies where participants were not recruited consecutively. Third, study duration was relatively short (i.e., May 2014 to September 2014), which introduces an additional factor of winter seasonal affective disorder, a recurrent subtype of depression [41]. This factor might also lead to underestimated prevalence. Fourth, we did not analyze important factors such as marital status [7] or home crowding [9]. Finally, our results were obtained from one hospital in the greater Tokyo area and thus the findings of this study might not generalize to other regions in Japan.
Conclusion
Our findings suggest that prevalence of CMD during mid-pregnancy in Japan is lower than that in most other countries. In addition to risk factors shown previously, feeling pressure to have a child might increase the risk for CMD, which might reflect certain aspects of Japanese culture.
Consent for publication
This study was conducted with the approval of the Institutional Review Board of Toda Chuo Women’s Hospital. All pregnant women who attended TCWH during the study period were asked to take the EPDS and received a brief explanation of the study. Eligible women were provided a complete description of the study during their next visit, at which time written informed consent was obtained. After the assessment, each participant received a gift voucher (2,000 JPY [17 USD]) for their participation.
Acknowledgements
We thank Mss. Natsuki Konno, Kasumi Araki, and Yuuri Matsumura for careful recruitment and research coordination. We also thank Prof. Keiichi Isaka, Dr. Hiroe Ito, and Dr. Hideto Shimada for their specialist obstetric advice, Dr. Hiroko Noguchi for training of the clinical research coordinators for this study, and Ms. Yumiko Kamoshida for her administrative assistance. None of the acknowledged individuals report any financial or other conflicts of interest relative to the subject of this work.
Funding
This study was supported by Grant-in-Aid for Young Scientists (A) from Japan Society for the Promotion of Science (primary investigator: Daisuke Nishi, MD, PhD), and Intramural Resaerch Grant for Neurological and Psychiatric Disorders of National Center of Neurology and Psychiatry Japan.
Footnotes
Competing interests
Dr. Usuda has no conflicts of interest to declare. Dr. Nishi has received research grants from the Japan Society for the Promotion of Science and National Center of Neurology and Psychiatry Japan, lecture fees from NTT DoCoMo, Inc., and Otsuka Pharmaceutical Co., Ltd. Ms. Makino has no conflicts of interest to declare. Dr. Tachimori has received research grants from the Ministry of Health, Labour, and Welfare of Japan, Intramural Research Grant for Neurological and Psychiatric Disorders of National Center of Neurology and Psychiatry. Dr. Matsuoka has received research grants from the Japan Science and Technology Agency, the National Center of Neurology and Psychiatry of Japan, and the Ministry of Health, Labour, and Welfare of Japan and has been a paid speaker for Ono Pharmaceutical Co., Ltd., Mochida Pharmaceutical Co., Ltd., Takeda Pharmaceutical Co., Ltd., Suntory Wellness Ltd., Otsuka Pharmaceutical Co., Ltd., and the DHA & EPA Association. Dr. Sano has no conflicts of interest to declare. Dr. Konishi has received research grants from the Japan Society for the Promotion of Science. Dr. Takeshima has received research grants from the Ministry of Health, Labour, and Welfare of Japan, Intramural Research Grant for Neurological and Psychiatric Disorders of National Center of Neurology and Psychiatry. Any funding source had no role in the design and conduct of the study; data collection; data management; analysis; interpretation of the data; review or approval of the manuscript; or decision to submit the manuscript for publication.
Authors’ contributions
KU and DN conceived and designed the study, DN obtained funding, KU, DN and MM collected the data, KU, DN and HT analyzed the data, all authors interpreted the data, KU and DN wrote the article in whole, all other authors revised the article critically. All authors read and approved the final manuscript.
References
- 1.Grote N, Bridge J, Gavin A, Melville J, Iyengar S, Katon W. A Meta-analysis of Depression During Pregnancy and the Risk of Preterm Birth, Low Birth Weight, and Intrauterine Growth Restriction. Arch Gen Psychiatry. 2010;67(10):1012–24. doi: 10.1001/archgenpsychiatry.2010.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stewart DE. Depression during Pregnancy. N Engl J Med. 2011;365:1605–11. doi: 10.1056/NEJMcp1102730. [DOI] [PubMed] [Google Scholar]
- 3.Yonkers KA, Smith MV, Forray A, Epperson CN, Costello D, Lin H, et al. Pregnant women with posttraumatic stress disorder and risk of preterm birth. JAMA Psychiatry. 2014;71(8):897–904. doi: 10.1001/jamapsychiatry.2014.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fisher J, Cabral de Mello M, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low- and lower-middle-income countries: a systematic review. Bull World Health Organ. 2012;90(2):139–49. doi: 10.2471/BLT.11.091850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kitamura T, Yoshida K, Okano T, Kinoshita K, Hayashi M, Toyoda N, et al. Multicentre prospective study of perinatal depression in Japan: incidence and correlates of antenatal and postnatal depression. Arch Womens Ment Health. 2006;9(3):121–30. doi: 10.1007/s00737-006-0122-3. [DOI] [PubMed] [Google Scholar]
- 6.Aras N, Oral E, Aydin N, Gulec M. Maternal age and number of children are risk factors for depressive disorders in non-perinatal women of reproductive age. Int J Psychiatry Clin Pract. 2013;17(4):298–306. doi: 10.3109/13651501.2013.821493. [DOI] [PubMed] [Google Scholar]
- 7.Fadzil A, Balakrishnan K, Razali R, Sidi H, Malapan T, Japaraj RP, et al. Risk factors for depression and anxiety among pregnant women in Hospital Tuanku Bainun, Ipoh, Malaysia. Asia-Pac Psychiatry. 2013;5(Suppl 1):7–13. doi: 10.1111/appy.12036. [DOI] [PubMed] [Google Scholar]
- 8.Su K-P, Chiu T-H, Huang C-L, Ho M, Lee C-C, Wu P-L, et al. Different cutoff points for different trimesters? The use of Edinburgh Postnatal Depression Scale and Beck Depression Inventory to screen for depression in pregnant Taiwanese women. Gen Hosp Psychiatry. 2007;29(5):436–41. doi: 10.1016/j.genhosppsych.2007.05.005. [DOI] [PubMed] [Google Scholar]
- 9.Farias DR, Pinto TDJP, Teofilo MMA, Vilela AAF, Vaz JDS, Nardi AE, et al. Prevalence of psychiatric disorders in the first trimester of pregnancy and factors associated with current suicide risk. Psychiatry Res. 2013;210(3):962–8. doi: 10.1016/j.psychres.2013.08.053. [DOI] [PubMed] [Google Scholar]
- 10.Giardinelli L, Innocenti A, Benni L, Stefanini MC, Lino G, Lunardi C, et al. Depression and anxiety in perinatal period: prevalence and risk factors in an Italian sample. Arch Womens Ment Health. 2012;15(1):21–30. doi: 10.1007/s00737-011-0249-8. [DOI] [PubMed] [Google Scholar]
- 11.Fisher J, Tran TD, Nguyen TT, Tran T. Common perinatal mental disorders and alcohol dependence in men in northern Viet Nam. J Affect Disord. 2012;140(1):97–101. doi: 10.1016/j.jad.2012.03.029. [DOI] [PubMed] [Google Scholar]
- 12.Simon GE, Goldberg DP, Von Korff M, Ustün TB. Understanding cross-national differences in depression prevalence. Psychol Med. 2002;32(4):585–94. doi: 10.1017/S0033291702005457. [DOI] [PubMed] [Google Scholar]
- 13.Shen Y-C, Zhang M-Y, Huang Y-Q, He Y-L, Liu Z-R, Cheng H, et al. Twelve-month prevalence, severity, and unmet need for treatment of mental disorders in metropolitan China. Psychol Med. 2006;36(2):257–67. doi: 10.1017/S0033291705006367. [DOI] [PubMed] [Google Scholar]
- 14.Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276(4):293–9. doi: 10.1001/jama.1996.03540040037030. [DOI] [PubMed] [Google Scholar]
- 15.Patel V, Rodrigues M, Desouza N. Gender, Poverty, and Postnatal Depression: A Study of Mothers in Goa, India. Am J Psychoanal. 2002;159(1):43–7. doi: 10.1176/appi.ajp.159.1.43. [DOI] [PubMed] [Google Scholar]
- 16.Xie R-h, He G, Liu A, Bradwejn J, Walker M, Wen SW. Fetal gender and postpartum depression in a cohort of Chinese women. Soc Sci Med. 2007;65(4):680–4. doi: 10.1016/j.socscimed.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Robertson E, Grace S, Wallington T, Stewart DE. Antenatal risk factors for postpartum depression: a synthesis of recent literature. Gen Hosp Psychiatry. 2004;26(4):289–95. doi: 10.1016/j.genhosppsych.2004.02.006. [DOI] [PubMed] [Google Scholar]
- 18.Klainin P, Arthur DG. Postpartum depression in Asian cultures: a literature review. Int J Nurs Stud. 2009;46(10):1355–73. doi: 10.1016/j.ijnurstu.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 19.Ministry of health Law. Overview of the System and the Basic Statistics, Changes in Number of Live Birth and Total Fertility Rate 2008. Available from: http://www.mhlw.go.jp/english/wp/wp-hw6/dl/01e.pdf (Accessed: 1st, March, 2016).
- 20.Ministry of Education, Culture, Sports, Science and Technology in Japan. Daigakubyouin no genjyou; 2009.
- 21.Otake Y, Nakajima S, Uno A, Kato S, Sasaki S, Yoshioka E, et al. Association between maternal antenatal depression and infant development: a hospital-based prospective cohort study. Environ Health Prev Med. 2014;19(1):30–45. doi: 10.1007/s12199-013-0353-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Okano T, Murata M, Masuji F, Tamaki R, Nomura J, Miyaoka H, et al. Validation and Reliability of Japanese Version of EPDS (Edinburgh Postnatal Depression Scale) Arch Psychiatr Diagn Clin Eval. 1996;7:525–33. [Google Scholar]
- 23.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(20):22–33. [PubMed] [Google Scholar]
- 24.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC; American Psychiatric Association; 1994.
- 25.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry J Ment Sci. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 26.Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, et al. The development of a Clinician-Administered PTSD Scale. J Trauma Stress. 1995;8(1):75–90. doi: 10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- 27.Asukai N, Hirohata S, Kato H, Konishi T. Psychometric properties of the Japanese-language version of the Clinician-Administered PTSD Scale for DSM-IV (in Japanese) Jpn J Traumatic Stress. 2003;1:47–53. [Google Scholar]
- 28.Akçalı Aslan P, Aydın N, Yazıcı E, Aksoy AN, Kirkan TS, Daloglu GA. Prevalence of depressive disorders and related factors in women in the first trimester of their pregnancies in Erzurum, Turkey. Int J Soc Psychiatry. 2014;60(8):809–17. doi: 10.1177/0020764014524738. [DOI] [PubMed] [Google Scholar]
- 29.Shimada H, Nishi D, Usuda K, Matsoka Y, Ito H, Isaka K. Factors associated with depressive symptoms during mid-pregnacy at a Japanese university hospital. Jpn J Gen Hosp Psychiatry. 2016;28(1):29–34. [Google Scholar]
- 30.Yubune K, Goto K, Kume M. Evaruation of the process and structure stress: Characteristics during pregnancy. Japan Society of Women’s Health. 2008;7:67-78.
- 31.Tachimori H, Naganuma Y, Koyama T, Koyama A, N K. The report of key findings from the World Mental Health Japan Survery..The report of the Research on Psychiatric and Neurological Diseases and Mental Health (H16-KOKORO-013) from the Japan Ministry of Health, Labour and Welfare. 2007.
- 32.Demyttenaere K, Bruffaerts R, Posada-Villa J, Gasquet I, Kovess V, Lepine JP, et al. Prevalence, severity, and unmet need for treatment of mental disorders in the World Health Organization World Mental Health Surveys. JAMA. 2004;291(21):2581–90. doi: 10.1001/jama.291.21.2581. [DOI] [PubMed] [Google Scholar]
- 33.Matsuoka Y, Nishi D, Yonemoto N, Nakajima S, Kim Y. Towards an explanation of inconsistent rates of posttraumatic stress disorder across different countries: infant mortality rate as a marker of social circumstances and basic population health. Psychother Psychosom. 2010;79(1):56–7. doi: 10.1159/000259418. [DOI] [PubMed] [Google Scholar]
- 34.Fisher J, Tran T, Duc Tran T, Dwyer T, Nguyen T, Casey GJ, et al. Prevalence and risk factors for symptoms of common mental disorders in early and late pregnancy in Vietnamese women: a prospective population-based study. J Affect Disord. 2013;146(2):213–9. doi: 10.1016/j.jad.2012.09.007. [DOI] [PubMed] [Google Scholar]
- 35.Markus HR, Kitayama S. Culture and the Self: Implications for Cognition, Emotion, and Motivation. Psychol Rev. 1991;98:224–53. doi: 10.1037/0033-295X.98.2.224. [DOI] [Google Scholar]
- 36.Yanikkerem E, Ay S, Mutlu S, Goker A. Antenatal depression: prevalence and risk factors in a hospital based Turkish sample. J Pak Med Assoc. 2013;63(4):472–7. [PubMed] [Google Scholar]
- 37.Nations U. Demographic Yearbook. Sixty-third ed. New York: United Nations/Nations Unies; 2012. [Google Scholar]
- 38.Rees SSZ, Creamer M, Teesson M, Bryant R, McFarlane AC, et al. Onset of common mental disorders and suicidal behavior following women inverted question marks first exposure to gender based violence: a retrospective, population-based study. BMC Psychiatry. 2014;14(1):312. doi: 10.1186/s12888-014-0312-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Melville JL, Gavin A, Guo Y, Fan MY, Katon WJ. Depressive Disorders During Pregnancy: Prevalence and Risk Factors in a Large Urban Sample. NIH Public Access. 2011;116(5):1064–70. doi: 10.1097/AOG.0b013e3181f60b0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cabunet Office, Government of Japan. H25 Edition declining birthrate society measures white paper. 2013.
- 41.Levitan RD. The chronobiology and neurobiology of winter seasonal affective disorder. Dialogues Clin Neurosci. 2007;9(3):315–24. doi: 10.31887/DCNS.2007.9.3/rlevitan. [DOI] [PMC free article] [PubMed] [Google Scholar]


