Abstract
IL-23 is a key driver of pathogenic Th17 cell responses. It has been suggested that the transcription factor T-bet is required to facilitate IL-23-driven pathogenic effector functions; however, the precise role of T-bet in intestinal T cell responses remains elusive. Here, we show that T-bet expression by T cells is not required for the induction of colitis or the differentiation of pathogenic Th17 cells but modifies qualitative features of the IL-23-driven colitogenic response by negatively regulating IL-23R expression. Consequently, absence of T-bet leads to unrestrained Th17 cell differentiation and activation characterized by high amounts of IL-17A and IL-22. The combined increase in IL-17A/IL-22 results in enhanced epithelial cell activation and inhibition of either IL-17A or IL-22 leads to disease amelioration. Our study identifies T-bet as a key modulator of IL-23-driven colitogenic responses in the intestine and has important implications for understanding of heterogeneity among inflammatory bowel disease patients.
 How transcription factor T-bet and Th17 cells contribute to colitis remains incompletely understood. Here the authors identify T-bet as a negative regulator of IL-23R pathway activation and show that T-bet deficient T cells drive colitogenic Th17 responses dependent on the cytokines IL-17A and IL-22.
How transcription factor T-bet and Th17 cells contribute to colitis remains incompletely understood. Here the authors identify T-bet as a negative regulator of IL-23R pathway activation and show that T-bet deficient T cells drive colitogenic Th17 responses dependent on the cytokines IL-17A and IL-22.
Th17 cells are enriched at mucosal sites, produce high amounts of IL-17A, IL-17F and IL-22, and have an essential role in mediating host protective immunity against a variety of extracellular pathogens1. However, on the dark side, Th17 cells have also been implicated in a variety of autoimmune and chronic inflammatory conditions, including inflammatory bowel disease (IBD)2. Despite intense interest, the cellular and molecular cues that drive Th17 cells into a pathogenic state in distinct tissue settings remain poorly defined.
The Th17 cell programme is driven by the transcription factor retinoid-related orphan receptor gamma-t (RORγt) (ref. 3), which is also required for the induction and maintenance of the receptor for IL-23 (refs 4, 5). The pro-inflammatory cytokine IL-23, composed of IL-23p19 and IL-12p40 (ref. 6), has been shown to be a key driver of pathology in various murine models of autoimmune and chronic inflammatory disease such as experimental autoimmune encephalomyelitis (EAE)7, collagen induced arthritis8 and intestinal inflammation9,10,11,12. Several lines of evidence, predominantly derived from EAE, suggest that IL-23 promotes the transition of Th17 cells to pathogenic effector cells9,10,11,12. Elegant fate mapping experiments of IL-17A-producing cells during EAE have shown that the majority of IL-17A+IFN-γ+ and IL-17A−IFN-γ+ effector cells arise from Th17 cell progeny13. This transition of Th17 cells into IFN-γ-producing ‘ex' Th17 cells required IL-23 and correlated with increased expression of T-bet. The T-box transcription factor T-bet drives the Th1 cell differentiation programme14 and directly transactivates the Ifng gene by binding to its promoter as well as multiple enhancer elements15. Indeed, epigenetic analyses have revealed that the loci for T-bet and IFN-γ are associated with permissive histone modifications in Th17 cells suggesting that Th17 cells are poised to express T-bet which could subsequently drive IFN-γ production16,17.
A similar picture is emerging in the intestine where IL-23 drives T-cell-mediated intestinal pathology which is thought to be dependent on expression of T-bet18 and RORγt (ref. 19) by T cells. In support of this we have recently shown that IL-23 signalling in T cells drives the emergence of IFN-γ producing Th17 cells in the intestine during chronic inflammation20. Collectively these studies suggest a model whereby RORγt drives differentiation of Th17 cells expressing high amounts of IL-23R, and subsequently, induction of T-bet downstream of IL-23 signalling generates IL-17A+IFN-γ+ T cells that are highly pathogenic. Indeed, acquisition of IFN-γ production by Th17 cells has been linked to their pathogenicity in several models of chronic disease13,21,22,23,24 and a population of T cells capable of producing both IL-17A and IFN-γ has also been described in intestinal biopsies of IBD patients25,26.
However, in the context of intestinal inflammation, it remains poorly defined whether the requirement for RORγt and T-bet reflects a contribution of Th17 and Th1 cells to disease progression or whether Th17 cells require T-bet co-expression to exert their pathogenic effector functions. Here, we use two distinct models of chronic intestinal inflammation and make the unexpected finding that T-bet is dispensable for IL-23-driven colitis. Rather the presence of T-bet serves to modify the colitogenic response restraining IL-17 and IL-22 driven pathology. These data identify T-bet as a key modulator of IL–23-driven colitogenic effector responses in the intestine and have important implications for understanding of heterogeneous immune pathogenic mechanisms in IBD patients.
Results
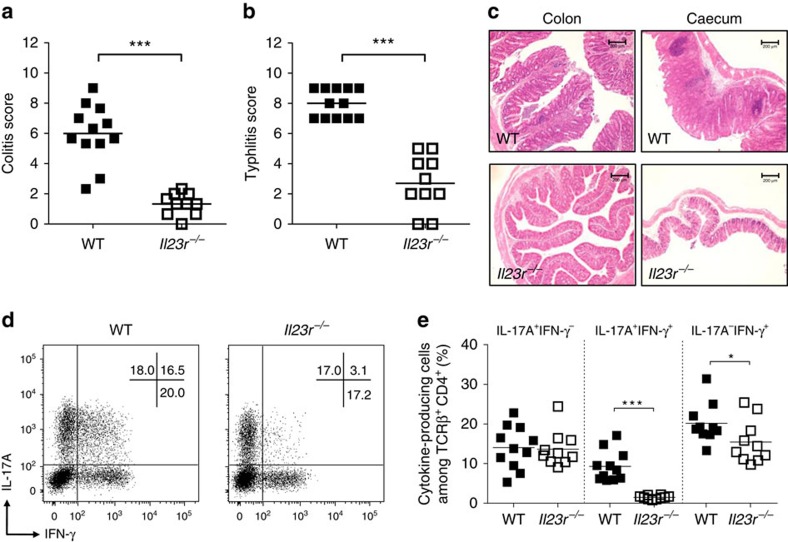
IL-23 promotes IL-17A+IFN-γ+ intestinal T cells
Using the T cell transfer model of colitis, which involves the transfer of naïve CD4+ T cells into lymphopenic Rag1−/− hosts27,28, we previously demonstrated that direct signalling of IL-23 into T cells promotes colitis and the emergence of IL-17A+IFN-γ+ T cells20. To assess the contribution of IL-23 signalling to the development of intestinal inflammation and differentiation of IL-17A+IFN-γ+ T cells in a lymphocyte replete setting, we induced colitis by oral infection with Helicobacter hepaticus (Hh) and concomitant administration of IL-10R blocking antibody (Hh+anti-IL-10R)9. This T-cell-dependent model of colitis is characterized by a mixed Th1/Th17 response and inflammation is blocked in Il12p40−/− mice (deficient in both IL-12 and IL-23) but not Il12p35−/− mice (deficient only in IL-12), inferring an essential role for IL-23 in disease pathogenesis. Consistent with this, we observed marked accumulation of IL-23R-expressing Th17 cells29 in the colon during the course of infection (Supplementary Fig. 1A,B). To assess the functional role of IL-23R signalling, we induced colitis in wild type (WT) or IL-23R-deficient (Il23r−/−) mice by infection with Hh+anti-IL-10R. As expected WT mice developed severe colitis and typhlocolitis characterized by cellular infiltration, broadening of crypts and epithelial hyperplasia (Fig. 1a–c). By contrast, Il23r−/− mice showed only mild signs of inflammation in the colon and caecum. Genetic ablation of IL-23R did not affect the differentiation of IL-17A+IFN-γ− T cells but led to a sixfold reduction in the frequency of IL-17A+IFN-γ+ T cells and a small decrease in IL-17A−IFN-γ+ T cells (Fig. 1d,e). Together, these data demonstrate that IL-23 is essential for the development of Hh-induced colitis and the emergence of IL-17A+IFN-γ+ T cells.
Figure 1. IL-23 signalling is required for bacteria-driven T-cell-dependent colitis and the emergence of IL-17A+IFN-γ+ T cells.
C57BL/6 WT and Il23r−/− mice were infected orally with Hh and received weekly i.p. injections of IL-10R blocking antibody. Mice were killed at 4 weeks post infection and assessed for intestinal inflammation. (a) Colitis scores. (b) Typhlitis sores. (c) Representative photomicrographs of colon and caecum (× 10 magnification; scale bars, 200 μM). (d) Representative flow cytometry plots of colonic lamina propria gated on viable CD4+ T cells. (e) Frequencies of IL-17A+ and/or IFN-γ+ CD4+ T cells present in the colon. Data represent pooled results from two independent experiments (n=12 for WT, n=10 for Il23r−/−). Bars are the mean and each symbol represents an individual mouse. *P<0.05, ***P<0.001 as calculated by Mann–Whitney U test.
IL-23 signals are dispensable for T-bet and RORγt expression
Evidence obtained from in vitro studies suggests that IL-23 drives the acquisition of IFN-γ production by Th17 cells in a T-bet-dependent manner21,30,31. In addition, IL-23 has been shown to enhance RORγt expression in naive CD4+ T cells transduced with IL-23R-expressing retrovirus4. Thus, IL-23 could drive the differentiation of IL-17A+IFN-γ+ T cells by virtue of its ability to induce and/or maintain expression of RORγt and T-bet. To address this, we generated mixed bone-marrow chimaeras by reconstituting irradiated Rag1−/− mice with WT (CD45.1+) and Il23r−/− (CD45.2+) bone marrow cells at 1:1 ratio. Following reconstitution of the haematopoietic system, we induced intestinal inflammation by infection with Hh+anti-IL-10R. This approach allowed us to investigate the phenotype of WT and Il23r−/− CD4+ T cells exposed to the same inflammatory environment. Indeed, intestinal pathology in mixed bone-marrow chimaeras was indistinguishable from that in WT mice (Supplementary Fig. 2A and Fig. 1a). Both WT and Il23r−/− CD4+ T cells were able to accumulate in the colon (Supplementary Fig. 2B) and we observed equivalent frequencies and total numbers of IL-17A+IFN-γ− and IL-17A−IFN-γ+ cells among WT and Il23r−/− T cells (Supplementary Fig. 2C,D). By contrast, differentiation of IL-17A+IFN-γ+ cells was significantly reduced in Il23r−/− CD4+ T cells indicating that IL-23 signalling directly into T cells in a cell autonomous way is required for the emergence of this effector cell type20.
Next, we assessed the expression of RORγt and T-bet protein by cytokine producing T cells of WT and Il23r−/− origin. As expected, IL-17A+IFN-γ− cells expressed high amounts of RORγt and IL-17A−IFN-γ+ cells expressed high amounts of T-bet, whereas co-expression of both RORγt and T-bet was exclusive to IL-17A+IFN-γ+ T cells (Supplementary Fig. 2E–G). Noticeably, there were no discernible differences in RORγt or T-bet protein amounts between IL-17A or IFN-γ single producers of WT and Il23r−/− origin (Supplementary Fig. 2G). In addition, the remaining IL-17A+IFN-γ+ cells detectable in T cells derived from Il23r−/− bone marrow expressed equivalent amounts of T-bet and RORγt compared with their WT counterparts (Supplementary Fig. 2G). These results demonstrate that cell-intrinsic IL-23 signals are required for the emergence of IL-17A+IFN-γ+ T cells but are dispensable for the maintenance of RORγt and T-bet expression in intestinal CD4+ T cells under inflammatory conditions.
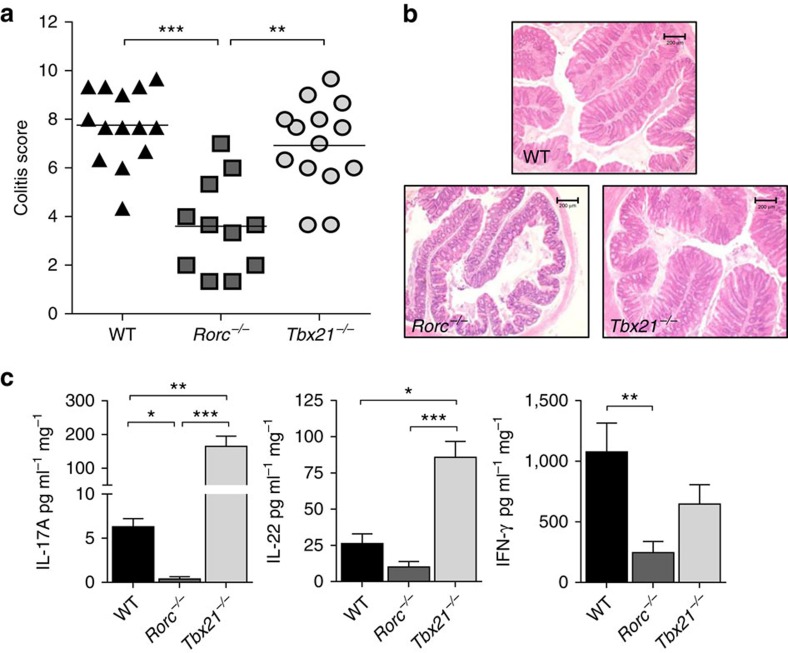
RORγt but not T-bet is required for T cell transfer colitis
To elucidate the impact of RORγt and T-bet expression on the colitogenic potential of T cells, we transferred Rag1−/− mice with CD4+ T cells from C57BL/6 WT, Tbx21−/− or Rorc−/− donors and assessed the development of colitis. T cell transfer colitis is a useful model to dissect the contribution of adaptive immune cells to the development of the disease as genes can be selectively ablated in the T cell donors hence avoiding confounding effects on other immune populations. In keeping with previous reports19 Rorc−/− T cells, which are deficient in both RORγ and RORγt, induced only mild colitis upon transfer into Rag1−/− recipients (Fig. 2a,b). Consistent with the attenuated histological features, we detected reduced amounts of pro-inflammatory cytokines IL-17A, IL-22 and IFN-γ in colon explant cultures of Rorc−/− T cell recipients (Fig. 2c). Strikingly, transfer of Tbx21−/− CD4+ T cells led to the development of a similar degree of intestinal inflammation as transfer of WT T cells (Fig. 2a,b). Despite equivalent pathology, analysis of cytokine secretion in colon explant cultures revealed a distinct inflammatory signature in recipients of Tbx21−/− T cells, characterized by significantly elevated amounts of the Th17 signature cytokines IL-17A and IL-22 (Fig. 2c). Surprisingly, transfer of Tbx21−/− T cells only marginally affected IFN-γ amounts, suggesting that T-bet-independent IFN-γ secretion by T cells, or IFN-γ expressing innate cells, contribute to IFN-γ production in this setting.
Figure 2. RORγt but not T-bet expression by CD4+ T cells is required for the development of T cell transfer colitis.
C57BL/6 Rag1−/− mice were injected i.p. with 4 × 105 CD4+CD25−CD45RBhi T cells from C57BL/6 WT, Rorc−/− or Tbx21−/− donors. Mice were killed when recipients of Tbx21−/− T cells developed clinical signs of disease (4–6 weeks) and assessed for intestinal inflammation. (a) Colitis scores. (b) Representative photomicrographs of proximal colon sections (× 10 magnification; scale bars, 200 μM). (c) Concentration of cytokines released from colon explants into the medium after overnight culture. Data represent pooled results from two independent experiments (n=14 for WT, n=11 for Rorc−/−, n=14 for Tbx21−/−). Bars are the mean and each symbol represents an individual mouse. Bars are the mean and error bars represent s.e.m. *P<0.05, **P<0.01, ***P<0.001 as calculated by Kruskal–Wallis one-way ANOVA with Dunn's post-test.
Further analysis showed that dysregulated Th2 or Foxp3+ regulatory T cell (Treg cells) responses are unlikely to account for the difference in colitogenic potential of T-bet and RORγt-deficient T cells. We did not detect any significant differences in the frequency of Foxp3+ Treg cells, IL-4 or IL-13 expressing cells between Rorc−/− and Tbx21−/− T cells (Supplementary Fig. 3A–C).
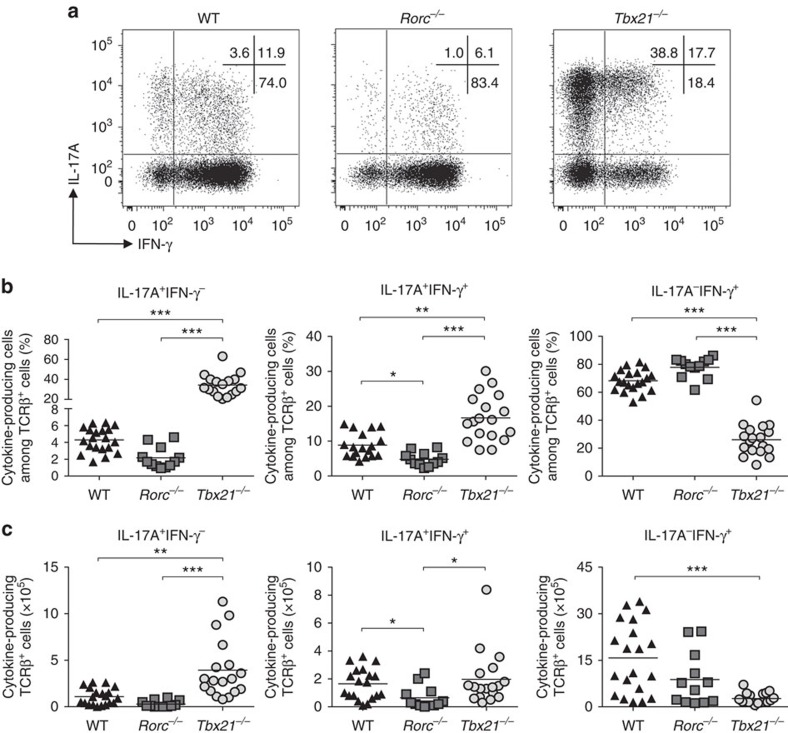
T-bet is dispensable for IL-17A+IFN-γ+ intestinal T cells
Next we addressed the impact of T-bet or RORγt-deficiency on intestinal CD4+ T cell differentiation. Consistent with their role in T helper cell development, deficiency in T-bet led to impaired differentiation of IFN-γ+ cells while the emergence of IL-17A+ cells was markedly reduced in RORγt-deficient T cells (Fig. 3a). The attenuated intestinal pathology observed in recipients of Rorc−/− T cells (Fig. 2a) correlated with a significantly decreased frequency and total number of IL-17A+IFN-γ+ T cells in the colon (Fig. 3b,c). By contrast, T-bet deficiency did not affect the differentiation and accumulation of IL-17A+IFN-γ+ T cells (Fig. 3a–c), indicating that T-bet is dispensable for the generation of this effector cell population. Together, these data reinforce the requirement for RORγt in the generation of intestinal Th17 cells and provide evidence that T-bet is dispensable for the differentiation of intestinal IL-17A+IFN-γ+ T cells.
Figure 3. T-bet expression by CD4+ T cells is not required for the emergence of IL-17A+IFN-γ+ T cells.
C57BL/6 Rag1−/− mice were injected i.p. with 4x105 CD4+CD25−CD45RBhi T cells from C57BL/6 WT, Rorc−/− or Tbx21−/− donors. Mice were killed when recipients of Tbx21−/−T cells developed clinical signs of disease (4–6 weeks). (a) Representative plots of IL-17A and IFN-γ expression in colonic CD4+ T cells. (b) Frequencies of IL-17A+ and/or IFN-γ+ cells among colonic CD4+ T cells. (c) Total numbers of IL-17A+ and/or IFN-γ+ CD4+ T cells present in the colon. Data represent pooled results from three independent experiments (n=20 for WT, n=18 for Tbx21−/−, n=12 for Rorc−/−). Bars are the mean and each symbol represents an individual mouse. *P<0.05, **P<0.01, ***P<0.001 as calculated by Kruskal–Wallis one-way ANOVA with Dunn's post-test.
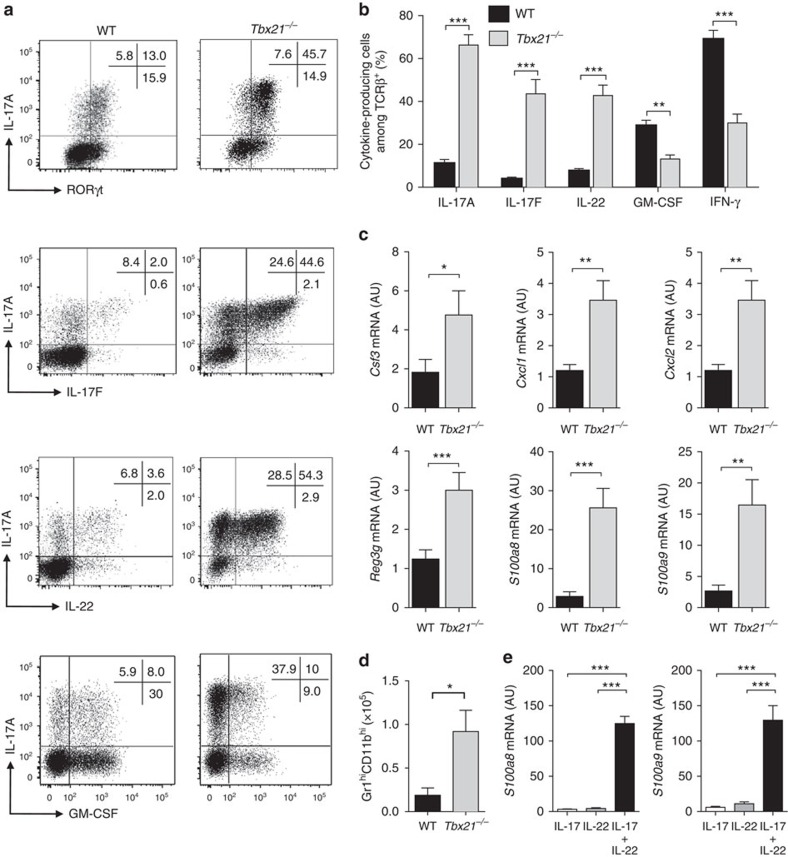
T-bet deficiency promotes an exacerbated Th17-type response
Our transfer of Tbx21−/− T cells revealed a striking increase in the frequency of IL-17A+IFN-γ− cells (Fig. 3) and we reasoned that T-bet-deficiency could impact on Th17 cell cytokine production. Therefore, we transferred WT or Tbx21−/− CD4+ T cells into Rag1−/− recipients and measured the expression of RORγt, IL-17A, IL-17F and IL-22 by CD4+ T cells isolated from the colon. In agreement with our earlier findings, Tbx21−/− T cells gave rise to significantly increased frequencies of RORγt-expressing T cells capable of producing IL-17A (Fig. 4a). Furthermore, T-bet deficiency also led to a dramatic expansion of IL-17F and IL-22-expressing cells, which constituted only a minor fraction in WT T cells (Fig. 4a,b). By contrast, the frequency of granulocyte-macrophage colony-stimulating factor (GM-CSF) and IFN-γ producing cells was significantly reduced in T-bet-deficient T cells as compared with WT T cells. When analysed in more detail we noted that the production of IL-17A, IL-17F and IL-22 increased specifically in T-bet-deficient IL-17A+IFN-γ+ T cells as compared with WT T cells whereas IFN-γ production decreased overall in the absence of T-bet as expected (Supplementary Fig. 4A). Similarly, GM-CSF production was also generally reduced in Tbx21−/− CD4+ T cells further suggesting a shift in the qualitative nature of the T cell response.
Figure 4. T-bet-deficient CD4+ T cells promote an exacerbated Th17-type inflammatory response.
C57BL/6 Rag1−/− mice were injected i.p. with 4x105 CD4+CD25−CD45RBhi T cells from C57BL/6 WT or Tbx21−/− donors. Mice were killed when recipients of Tbx21−/−T cells developed clinical signs of disease (4–6 weeks). (a) Representative plots of cytokines and transcription factors in WT or Tbx21−/− colonic CD4+ T cells. (b) Frequency of IL-17A+, IL-17F+, IL-22+, GM-CSF+ or IFN-γ+ colonic T cells in WT or Tbx21−/−. (c) quantitative reverse transcription PCR (qRT-PCR) analysis of mRNA levels of indicated genes in colon tissue homogenates. (d) Total number of neutrophils (CD11b+ Gr1high) in the colon. (e) Primary epithelial cells were isolated from the colon of steady state C57BL/6 Rag1−/− mice and stimulated with 10 ng ml−1 cytokines for 4 h after which cells were harvested and analysed by qRT-PCR for the indicated genes. Data in b–d represent pooled results from two independent experiments (n=14 for WT, n=11 for Tbx21−/−). Bars are the mean and error bars represent s.e.m. Data in e are pooled results from four independent experiments, bars are the mean and error bars represent s.e.m. *P<0.05, **P<0.01, ***P<0.001 as calculated by Mann–Whitney U test.
Next, we compared the expression of genes that are downstream of IL-17A, IL-17F and IL-22 signalling in colon homogenates of Rag1−/− recipients of WT or Tbx21−/− T cells. Transcript expression of Csf3, Cxcl1, Cxcl2, Reg3g, S100a8 and S100a9 were significantly increased in the colon of Rag1−/− recipients of Tbx21−/− T cells (Fig. 4c). Consistent with this, we also found increased numbers of neutrophils in the colonic lamina propria of these mice (Fig. 4d). To test possible interactions between IL-22 and IL-17A on expression of these genes we isolated epithelial cells from the colon of Rag1−/− mice and stimulated them with IL-17A, IL-22 or combination of both cytokines. We found a marked synergistic increase in the expression of the neutrophil chemoattractants S100a8 and S100a9 (ref. 32) messenger RNA (mRNA) following stimulation with IL-17A and IL-22 (Fig. 4e and Supplementary Fig. 4B). Together, our data demonstrate that colitis induced by Tbx21−/− T cells is characterized by an exacerbated Th17-type response and that synergistic activity of IL-22 and IL-17A on epithelial cells may result in enhanced neutrophil recruitment and development of intestinal inflammation with distinct hall marks.
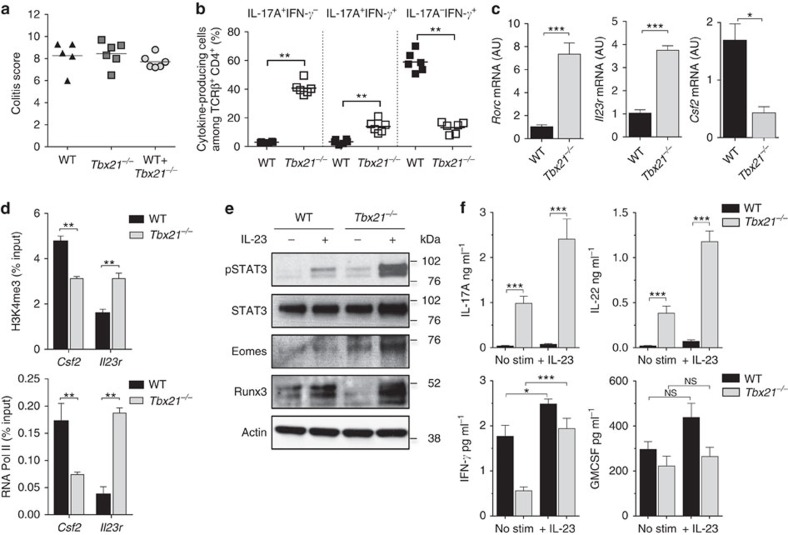
T-bet-deficient CD4+ T cells are hyper-responsive to IL-23
Next, we sought to compare gene-expression signatures and functional properties of pathogenic T cells generated from WT and Tbx21−/− T cells. To investigate this, we purified CD4+ T cells from the inflamed colon of Rag1−/− mice that had been transferred with an equal number of WT (CD45.1+) and Tbx21−/− (CD45.2+) T cells. Intestinal pathology of mice receiving WT and Tbx21−/− T cells was indistinguishable from that in mice transferred with WT or Tbx21−/− only T cells (Fig. 5a). Importantly, the increased differentiation of Tbx21−/− T cell progeny into IL-17A+IFN-γ+ T cells was preserved in the co-transfer (Fig. 5b and Supplementary Fig. 5A) further supporting the notion that T-bet is dispensable for acquisition of IFN-γ production by Th17 cells. Comparison of gene-expression signatures showed that T-bet-deficient T cells had significantly higher expression of Rorc, Il23r, Ccr6 and Il1r1 indicating a specific cell-intrinsic role for T-bet in the repression of Th17 signature genes (Fig. 5c and Supplementary Fig. 5B). In addition, Tbx21−/− T cells had upregulated expression of neutrophil chemoattractant Cxcl3 and decreased expression of the gene encoding GM-CSF (Csf2). Interestingly, we found similar amounts of mRNA for Il10 and Tgfb3 (Supplementary Fig. 5B) suggesting that these cytokines do not contribute to the observed differences in pathogenic effector function between WT and Tbx21−/− T cells.
Figure 5. T-bet-deficient T cells are hyper-responsive to IL-23.
C57BL/6 Rag1−/− mice were injected i.p. with either WT or Tbx21−/− CD4+CD25-CD45RBhi T cells or a 1:1 mixtures of WT (CD45.1+) and Tbx21−/−(CD45.2+) CD4+CD25−CD45RBhi T cells. Mice were killed when recipients of Tbx21−/− T cells developed clinical signs of disease (∼5 weeks) and assessed for intestinal inflammation. (a) Colitis scores. (b) Frequencies of IL-17A+ and/or IFN-γ+ cells in the colon of mice receiving mix of WT and Tbx21−/− CD4+ T cells. (c) CD4+ T cells were purified by flow cytometry from the inflamed colon of mice receiving a mix of WT and Tbx21−/− CD4+ T cells and mRNA levels of indicated genes were analysed by quantitative reverse transcription PCR (qRT-PCR). (d) ChIP-qRT-PCR for the occupancy of H3K4me3 or RNA Pol II around the TSS of indicated genes in CD4+ T cells purified as described in c. (e) Immunoblot for pY705-STAT3, total STAT3, EOMES, Runx3 and Actin on whole cells lysates of CD4+ T cells purified as in c, left unstimulated or stimulated with IL-23 for 12 h. (f) Concentrations of indicated cytokines secreted into culture medium by CD4+ T cells purified and stimulated as described in e. Data in a–c and f represent results from one of two independent experiments (n=5 for WT, n=6 for Tbx21−/−, n=6 for WT+Tbx21−/−). Bars are the mean and each symbol represents an individual mouse. Bars are the mean and error bars represent s.e.m. Data in d are pooled results from two independent experiments, bars are the mean and error bars represent s.d. *P<0.05, **P<0.01, ***P<0.001 as calculated by Mann–Whitney U test.
We were intrigued by the fact that Il23r and Csf2 appeared to be differentially expressed in WT versus Tbx21−/− T cells and tested whether T-bet would be directly involved in regulating their transcription. We performed ChIP experiments in CD4+ T cells cultured in vitro under Th0 or Th1 conditions and analysed the recruitment of T-bet to the transcription start site (TSS) of Csf2 and to a specific region in intron 3 of Il23r where T-bet binding has been detected according to two independent T-bet ChIP-Seq experiments33,34. To correlate T-bet binding with gene activity we analysed in parallel the recruitment of RNA polymerase II (RNA Pol II) as well as the occurrence of the open-chromatin-associated histone mark H3K4me3 at the TSS of Csf2 and Il23r. T-bet was robustly recruited to Csf2 and Il23r in Th1 cells and despite elevated amounts of H3Kme3 at both genes only Csf2 showed enhanced transcriptional activity, as measured by the recruitment of RNA Pol II (Supplementary Fig. 5C). To further investigate the role of T-bet in the transcriptional regulation of Csf2 and Il23r we performed ChIP experiments on progeny of WT and Tbx21−/− CD4+ T cells sort-purified from T cell co-transfer experiments described above. In the absence of T-bet, the open-chromatin mark H3K4me3 was increased at the Il23r TSS as compared with WT cells and transcription of the Il23r genes was upregulated substantially in Tbx21−/− progeny (Fig. 5d). This was in contrast to the Csf2 gene where T-bet deficiency resulted in decreased occupancy of both H3K4me3 and RNA Poll II (Fig. 5d). These data provide a molecular basis for our functional studies and reveal opposing functions of T-bet leading to positive regulation of Csf2 but negative regulation of Il23r expression.
Given the increased amounts of Il23r expression, we reasoned that the exacerbated Th17 response induced by transfer of Tbx21−/− T cells could be the result of enhanced responsiveness to IL-23. Stimulation of colonic WT T cells with IL-23 resulted in phosphorylation of STAT3 and this was greatly enhanced in colonic Tbx21−/− T cells (Fig. 5e), suggesting that T-bet-deficient T cells are hyper-responsive to IL-23 due to higher expression of IL-23R. Analysis of cytokine production by sort-purified colonic T cells showed increased secretion of IL-17A and IL-22 in unstimulated and IL-23-activated Tbx21−/− compared with WT T cells (Fig. 5f). IL-23-stimulated IFN-γ production was also increased in Tbx21−/− T cells relative to unstimulated controls whereas IL-23 had no effect on GM-CSF production in WT or T-bet deficient T cells (Fig. 5f).
To investigate the potential mechanism responsible for T-bet-independent IFN-γ production, we measured induction of Eomesodermin (Eomes) and Runt-related transcription factor 3 (Runx3) downstream of IL-23 stimulation in sort-purified WT and Tbx21−/− colonic effector T cells. Eomes is a paralogue to T-bet with a known role in regulating IFN-γ production in both CD4+ and CD8+ T cells35,36,37. Eomes was detected in unstimulated Tbx21−/− T cells and its expression was further induced in response to IL-23 stimulation. In contrast, Eomes protein amounts were at the limit of detection in unstimulated and IL-23-stimulated WT T cells (Fig. 5e). In line with these results, we found that intracellular expression of Eomes was highly upregulated in colonic T-bet-deficient effector T cells as compared with their WT counterparts (Supplementary Fig. 6A). However, <10% of IL-17A+IFN-γ+ Tbx21−/− T cells expressed Eomes compared with ∼75% of IL-17A−IFN-γ+ T cells (Supplementary Fig. 6B) suggesting that this factor might drive IFN-γ expression specifically in the latter population. Runx3 has been shown to promote IFN-γ secretion directly either through binding to the Ifng promoter38 or indirectly through induction of Eomes39. Runx3 was induced in WT and T-bet-deficient T cells with greater fold induction observed in Tbx21−/− T cells (Fig. 5e). Thus, Eomes and Runx3 appear to be induced downstream of IL-23R signalling in Tbx21−/− CD4+ T cells and could potentially contribute to T-bet-independent IFN-γ production.
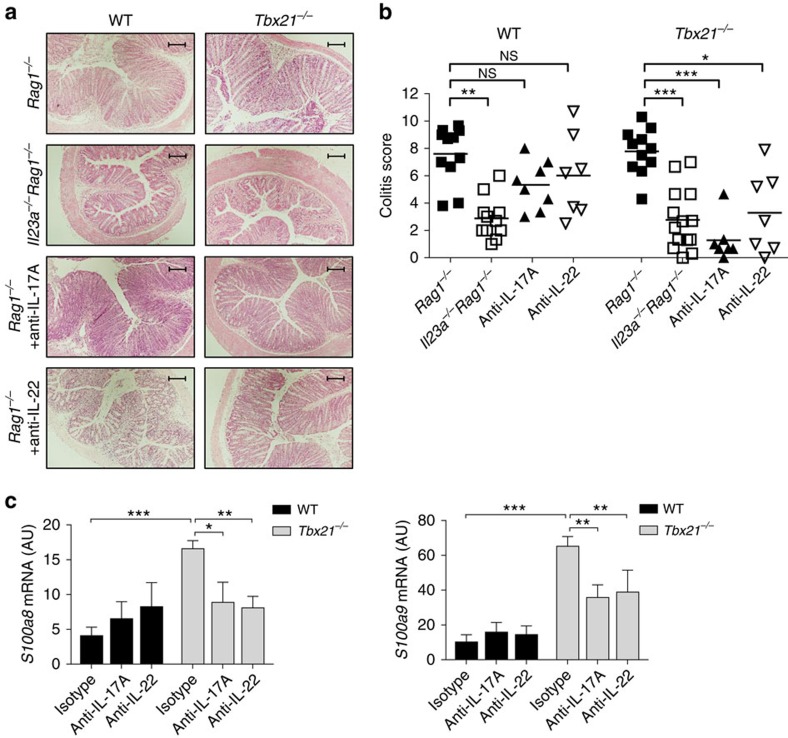
T-bet-deficient colitis depends on IL-23, IL-17A and IL-22
To investigate whether IL-23 has a functional role in the induction of colitis by T-bet-deficient T cells, Rag1−/− and Il23a−/−Rag−/− mice were transferred with WT or Tbx21−/− T cells. As expected, transfer of WT or Tbx21−/− T cells induced severe intestinal inflammation in Rag1−/− hosts. By contrast, colitis was significantly decreased when WT or Tbx21−/− T cells were transferred into IL-23 deficient Il23a−/−Rag1−/− recipients (Fig. 6a,b). To test which effector cytokines were required for colitis induced by T-bet-deficient T cells, we transferred cohorts of Rag1−/− recipients with WT or Tbx21−/− T cells and administered neutralizing antibodies to IL-17A or IL-22. Although neutralization of IL-17A or IL-22 did not significantly reduce inflammation in recipients of WT T cells, blockade of either cytokine abrogated intestinal pathology in Rag1−/− mice transferred with Tbx21−/− CD4+ T cells (Fig. 6a,b). To confirm that IL-17A/IL-22 produced by CD4+ T cells are indeed pathogenic factors in Tbx21−/− driven T cell transfer colitis, we stimulated intestinal epithelial cells with supernatant of IL-23-activated WT and Tbx21−/− T cells. Compared with WT supernatant, the supernatant of Tbx21−/− T cells induced a potent epithelial cell response (Fig. 6c). Similar to the in vivo blockade experiments, neutralization of IL-17A or IL-22 was only effective in Tbx21−/− T cells suggesting that augmented cytokine production may be a major driver in colitis induced by T-bet-deficient T cells. Taken together these results show that IL-23 promotes a distinct Th17-dependent pathogenic T cell response in the absence of T-bet.
Figure 6. Colitis induced by T-bet-deficient T cells is dependent on IL-23, IL-17A and IL-22.
C57BL/6 Rag1−/− mice or Il23a−/−Rag1−/− were injected i.p. with 4 × 105 CD4+CD25-CD45RBhi T cells from C57BL/6 WT or Tbx21−/− donors. Rag1−/− recipients received weekly injections of blocking anti-IL-17A, anti-IL-22 or isotype control mAbs. Mice were killed when recipients of isotype control antibody developed clinical signs of disease (4–6 weeks). (a) Representative photomicrographs of proximal colon sections from the indicated experimental groups (× 10 magnification; scale bars, 200 μM). (b) Colitis score. (c) Primary epithelial cells were isolated from the colon of steady state C57BL/6 Rag1−/− mice and stimulated with supernatant of IL-23-stimulated WT or Tbx21−/− CD4+ T cells sort-purified from Rag1−/− recipients. Supernatants were added at 20% of total cell culture volume in combination with indicated blocking antibodies. Cells were harvested after 4 h and mRNA levels of indicated genes were analysed by quantitative reverse transcription PCR (qRT-PCR). Data in b represents pooled results from two independent experiments. Bars are the mean and each point represents an individual mouse. Data in c are pooled results from four independent experiments, bars are the mean and error bars represent s.e.m. *P<0.05, **P<0.01, ***P<0.001 as calculated by Kruskal–Wallis one-way ANOVA with Dunn's post-test.
Discussion
In the present study we show that bacteria-driven colitis is associated with the IL-23-dependent emergence of IFN-γ-producing Th17 cells co-expressing RORγt and T-bet. Strikingly, while RORγt is required for the differentiation of IFN-γ-producing Th17 cells and induction of colitis, T-bet is dispensable for the emergence of IL-17A+IFN-γ+ T cells and intestinal pathology. Our results show that instead of a mandatory role in the colitogenic response, the presence of T-bet modulates the qualitative nature of the IL-23-driven intestinal inflammatory response. In the presence of T-bet, IL-23-driven colitis is multifunctional in nature and not functionally dependent on either IL-17A or IL-22. By contrast, in the absence of T-bet a highly polarized colitogenic Th17 cell response ensues which is functionally dependent on both IL-17A and IL-22. T-bet-deficient T cells are hyper-responsive to IL-23 resulting in enhanced STAT3 activation and downstream cytokine secretion providing a mechanistic basis for the functional changes. These data newly identify T-bet as a key modulator of IL-23-driven colitogenic CD4+ T cell responses.
Contrary to our expectations T-bet expression by CD4 T cells was not required for their pathogenicity. In keeping with the negative effect of T-bet on Th17 differentiation40,41,42, we observed highly polarized Th17 responses in T-bet-deficient intestinal T cells. Early studies demonstrated that IFN-γ could suppress the differentiation of Th17 cells40 and thus the reduced IFN-γ production by Tbx21−/−T cells could facilitate Th17 cell generation. However, our co-transfer studies revealed unrestrained Th17 differentiation of Tbx21−/− T cells even in the presence of WT T cells, suggesting a cell autonomous role for T-bet-mediated suppression of the Th17 programme. Indeed, the role of T-bet as a transcriptional repressor of the Th17 cell fate has been described recently. For example, T-bet physically interacts with and sequesters Runx1, thereby preventing Runx1-mediated induction of RORγt and Th17 cell differentiation43. In addition, T-bet binds directly to and negatively regulates expression of many Th17-related genes15,34 and we identified IL23r to be repressed in a T-bet-dependent manner. In line with this we show here that T-bet-deficient intestinal T cells express higher amounts of Il23r as well as Rorc. This resulted in enhanced IL-23-mediated STAT3 activation and increased production of IL-17A and IL-22. It has also been suggested that T-bet activation downstream of IL-23R signalling is required for pathogenic IL-23-driven T cell responses43,44. However, we did not find a role for IL-23 in the induction and/or maintenance of T-bet expression and colitis induced by T-bet-deficient T cells was IL-23 dependent. Collectively, these findings demonstrate that T-bet deficiency leads to unrestrained expansion of colitogenic Th17 cells, which is likely mediated through enhanced activation of the IL-23R-STAT3 pathway.
The observation that T-bet-deficient T cells retain their colitogenic potential is in stark contrast to earlier studies. Neurath et al.18 convincingly showed that adoptive transfer of Tbx21−/− CD4+ T cells into severe combined immunodeficiency (SCID) recipients failed to induce colitis and this correlated with reduced IFN-γ and increased IL-4 production. Another study revealed that IL-4 plays a functional role in inhibiting the colitogenic potential of Tbx21−/− T cells, as recipients of Stat6−/−Tbx21−/− T cells developed severe colitis37. Importantly, the intestinal inflammation that developed in recipients of Stat6−/−Tbx21−/− T cells could be blocked by administration of IL-17A neutralizing antibody, suggesting that the potent inhibitory effect of IL-4/STAT6 signals on Th17 differentiation normally prevent colitis induced by Tbx21−/− T cells37. Various explanations could account for the discrepancy between our study and those earlier findings. First, in contrast to the published reports, we used naïve Tbx21−/− CD4+ T cells from C57BL/6 mice instead of BALB/c mice. An important difference between Tbx21−/− CD4+ T cells from these genetic backgrounds appears to be their differential susceptibility to suppression by IL-4/STAT6 signals. We found that transfer of Tbx21−/− T cells induced IL-17A-dependent colitis despite increased frequencies of IL-4-expressing cells in the intestine. This discrepancy may be due to higher amounts of IL-4 produced by activated CD4+ T cells from BALB/c versus C57BL/6 mice45, leading to the well-described Th2-bias of the BALB/c strain45. Second, differences in the composition of the intestinal microbiota between animal facilities can have a substantial effect on skewing CD4+ T cells responses. In particular, the Clostridium-related segmented filamentous bacteria (SFB) have been shown to drive the emergence of IL-17 and IL-22 producing CD4+ T cells in the intestine46. Importantly, the ability of naïve CD4+ T cells to induce colitis is dependent on the presence of intestinal bacteria, as germ-free mice do not develop pathology upon T cell transfer47. In line with this, we previously described that colonization of germ-free mice with intestinal microbiota containing SFB was necessary to restore the development of colitis47. Since our Rag1−/− colony is SFB+ and the presence of SFB was not reported in the previous studies, it is possible that differences in SFB colonization status contributed to the observed differences in pathogenicity of Tbx21−/− T cells.
It is important to note that T-bet-deficient T cells did not induce more severe colitis than WT T cells but rather promoted a distinct mucosal inflammatory response. Colitis induced by WT T cells is characterized by a multifunctional response with high amounts of IFN-γ and GM-CSF and a lower IL-17A and IL-22 response. Consistent with this, we have shown that blockade of GM-CSF abrogates T cell transfer colitis48 as well as bacteria-driven intestinal inflammation49 in T-bet sufficiency whereas blockade of IL-17A or IL-22 fails to do so. By contrast T-bet deficiency leads to production of high amounts of IL-17A and IL-22 in the colon and neutralization of either was sufficient to reduce intestinal pathology. Our in vitro experiments suggest that IL-17A and IL-22 synergise to promote intestinal epithelial cell responses, which may in part explain the efficacy of blocking IL-17A or IL-22 in colitis induced by T-bet-deficient T cells. A similar synergistic interplay has been described in the lung where IL-22 served a tissue protective function in homeostasis but induced airway inflammation in the presence of IL-17A (ref. 50). This highlights the complexity of the system in health and disease, and the need for a controlled production of both cytokines. We describe here only one mechanism of how IL-17A/IL-22 induce a context-specific epithelial cell response that potentially impacts on the order or composition of immune cell infiltration. Overall, these results provide a new perspective on T-bet, revealing its role in shaping the qualitative nature of the IL-23-driven colitogenic T cell response.
We also describe here the unexpected finding that a substantial proportion of T-bet-deficient intestinal T cells retain the ability to express IFN-γ. To investigate the potential mechanisms responsible for T-bet-independent IFN-γ production by intestinal CD4+ T cells we focused on two transcription factors, Runx3 and Eomes. Runx3 has been shown to promote IFN-γ expression directly through binding to the Ifng promoter38 and Eomes is known to compensate for IFN-γ production in T-bet-deficient Th1 cells37. We found IL-23-mediated induction of Runx3 protein in WT and Tbx21−/− T cells isolated from the intestine, thus identifying Runx3 downstream of IL-23R signalling. By contrast, we could only detect Eomes protein and its induction by IL-23 in T-bet-deficient but not WT T cells. Thus, Runx3 and Eomes are activated in response to IL-23 in T-bet-deficient cells and are likely to be drivers of T-bet-independent IFN-γ production. In support of this we found that the majority of T-bet-deficient IL-17A−IFN-γ+ T cells expressed Eomes. However, only a minor population of IL-17A+IFN-γ+ T cells stained positive for Eomes, suggesting the existence of alternative pathways for IFN-γ production by Th17 cells. Intriguingly, a recent study identified Runx3 and Runx1 as the transcriptional regulators critical for the differentiation of IFN-γ-producing Th17 cells51. The author's demonstrated that ectopic expression of Runx transcription factors was sufficient to induce IFN-γ production by Th17 cells even in the absence of T-bet. These findings, combined with our data on Runx3 activation downstream of IL-23R signalling strongly suggest that Runx3 rather than Eomes is driving IFN-γ expression by intestinal Th17 cells.
We have not formally addressed the role of IFN-γ in colitis driven by T-bet-deficient T cells. A recent report by Zimmermann et al.52 found that antibody-mediated blockade of IFN-γ ameliorates colitis induced by WT or T-bet-deficient T cells suggesting IFN-γ also contributes to the colitogneic response mediated by T-bet-deficient T cells as originally described for WT T cells53,54. By contrast with our results the Zimmerman study found that IL-17A blockade exacerbated colitis following transfer of Tbx21−/− T cells. The reason for the differential role of IL-17A in the two studies is not clear but it is notable that the Zimmerman study was performed in the presence of co-infection with SFB and Hh, and this strong inflammatory drive may alter the pathophysiological role of particular cytokines. Together the data indicate that T-bet deficiency in T cells does not impede their colitogenic activity but that the downstream effector cytokines of the response are context dependent.
In conclusion, our data further underline the essential role for IL-23 in intestinal inflammation and demonstrate that T-bet is an important modulator of the IL–23-driven effector T cell response. The colitogenic T cell response in a T-bet sufficient environment is multifunctional with a dominant GM-CSF and IFN-γ response. By contrast T-bet-deficient colitogenic responses are dominated by IL-17A and IL-22-mediated immune pathology. These results may have significant bearing on human IBD where it is now recognized that differential responsiveness to treatment may reflect considerable disease heterogeneity. As such, identification of suitable biomarkers such as immunological parameters, that allow stratification of patient groups, is becoming increasingly important55. Genome-wide association studies have identified polymorphisms in loci related to innate and adaptive immune arms that confer increased susceptibility to IBD. Among these are Th1 (STAT4, IFNG and STAT1) as well as Th17-related genes (RORC, IL23R and STAT3) (refs 56, 57). Thus, detailed profiling of the T cell response in IBD patients may help identify appropriate patient groups that are most likely to benefit from therapeutic blockade of certain effector cytokines. Finally, our studies highlight the importance of IL-23 in the intestinal inflammatory hierarchy and suggest that IL-23 could be an effective therapeutic target across a variety of patient groups.
Methods
Mice
Wild type C57BL/6, C57BL/6 Tbx21−/− (obtained from Jackson Laboratories) congenic B6.SJL-Cd45, C57BL/6 Rag1−/−, C57BL/6 Rorc−/− (obtained from Dan Littman) C57BL/6 Il23r−/−, C57BL/6.IL-23Rgfp/+ (obtained from Mohamed Oukka) and C57BL/6 Il23a−/−Rag1−/− (obtained from Dan Cua) mice were bred and maintained under specific pathogen-free conditions in accredited animal facilities at the University of Oxford. All procedures were conducted in accordance with the UK Scientific Procedures Act of 1986. All experimental protocols were approved by the UK Home Office and the Ethical Review Committee of the Oxford University Medical Sciences Division. Both female and male mice were used in experiments and animals were assigned randomly to experimental groups. Each cage contained animals of all the different experimental groups whenever possible.
Mice were negative for Helicobacter spp. and other known intestinal pathogens and were more than 6 weeks old when first used for T cell transfer or when used as recipients/donors in mixed bone-marrow chimera experiments.
T cell transfer colitis
For naïve T cell transfer colitis, 4 × 105 CD4+CD25−CD45RBhi T cells were injected i.p. into Rag1−/− or Il23a−/−Rag1−/− recipients. In co-transfer experiments, 2 × 105 CD4+CD25−CD45RBhi T cells from each source were mixed and injected i.p. into Rag1−/− hosts. Where indicated, mice were injected with anti-IL-17A (1 mg per mouse every 3 days, clone 17F3 BioXCell), anti-IL-22 (0.125 mg per mouse every 3 days, Genentech, clone 8E11) or isotype control for the duration of the experiment. Mice were killed at indicated time points or killed when weight loss approached 20% of the original body weight at the start of the experiment.
Induction of Hh/anti-IL-10R colitis
Mice were fed 1 × 108 cfu Hh by oral gavage with a 22G curved needle on days 0 and 1 of the experiment. In some experiments, mice also received 1 mg of an anti-IL-10R blocking antibody by i.p. injection once weekly starting at the day of Hh infection.
Generation of mixed bone-marrow chimeras
Bone marrow isolated from Il23r−/− mice was mixed at a 1:1 ratio with bone marrow taken from B6.SJL-Cd45 mice and injected intravenously into gamma-irradiated (5.5 Gy, 550Rad) C57BL/6 Rag1−/−recipients and chimaeras were used in experiments >8 weeks after injection.
Histological assessment of intestinal inflammation
Proximal, mid- and distal-colon samples were fixed in buffered 10% formalin solution. Paraffin-embedded sections were cut (5 mm) and stained with haematoxylin and eosin, and inflammation was scored in a blinded fashion using a previously described scoring system58. Briefly, each sample was graded semiquantitatively from 0 to 3 for the four following criteria: degree of epithelial hyperplasia and goblet cell depletion; leucocyte infiltration in the lamina propria; area of tissue affected; and the presence of markers of severe inflammation such as crypt abscesses, submucosal inflammation and ulcers. Scores for each criterion were added to give an overall inflammation score for each sample of 0–12. The total colonic score was calculated as the average of the individual scores from the sections of proximal-, mid- and distal-colon.
Isolation of leucocyte subpopulations and flow cytometry
Cell suspensions from spleen, mesenteric lymph nodes (MLN) and the lamina propria were prepared as described previously59 and first incubated with anti-CD16/CD32 (eBioscience) to prevent nonspecific binding. Single cell suspensions were stained with antibodies against CD4, CD11b, CD25, GR1, TCR-β, CD45.1, CD45.2, IL-4, IL-13, IL-17A, IL-22, IFN-γ, EOMES, RORγt, Foxp3, (all from eBioscience), CD45RB, IL-17F and T-bet (all from Biolegend). Intracellular staining was performed as follows: cells were restimulated for 4 h with 0.1 μg ml−1 phorbol 12-myristate 13-acetate (PMA) and 1 μg ml−1 ionomycin (both Sigma Aldrich) plus Brefeldin A (eBioscience), washed and incubated with anti-CD16/CD32. Cells were washed and stained for surface markers indicated above and fixed in eBioscience Fix/Perm buffer, followed by permeabilization in eBioscience permeabilization buffer for 1 h in the presence of antibodies. Cells were acquired with a BD LSR2 and analysis was performed with FlowJo (Tree Star) software
Colon explant cultures
Small pieces of colon (∼5 mm of mid-colon) were isolated, rinsed in PBS/BSA and weighed. Colon explants were cultured overnight in Roswell Park Memorial Institute medium (RPMI; Invitrogen) containing 10% FCS, 2 mM L-glutamine, 0.05 mM 2-mercaptoethanol and 100 U ml−1 each of penicillin and streptomycin (complete media) in 24-well tissue culture plates. Cytokine amounts in the supernatants were determined by Bender assay according to the manufacturers' protocol (eBioscience) and concentrations normalized to the weight of the explants.
T cell cultures
CD4+TCR-β+CD45.1+ (WT progeny) and CD4+TCR-β+CD45.1− (Tbx21−/− progeny) T cells were sort-purified from the colon of C57BL/6 Rag1−/− recipient mice. Cells were either lysed for quantitative PCR (qPCR) or plated at 2 × 105 cells per well in flat bottomed 96-well plates in RPMI (Invitrogen) containing 10% FCS, 2 mM l-glutamine, 0.05 mM 2-mercaptoethanol and 100 U ml−1 each of penicillin and streptomycin (complete media). IL-23 was added at 20 ng ml−1 (R&D) for 12 h after which cells were harvested and lysed for immunoblot analysed. Supernatants were collected and cytokine secretion quantified by Bender assay (eBioscience) as per the manufacturers' protocol.
Epithelial cell cultures
Primary epithelial cells were isolated from steady state colon of C57BL/6 Rag1−/− mice. Briefly, colons were cut open longitudinally, washed in cold PBS to remove colon content and cut into 1 cm pieces. Epithelial cells were liberated by a 10-min wash with RPMI containing 10% FCS and 5 mM EDTA in a shaking incubator. Supernatant was filtered, cells pelleted at 1,500 r.p.m. and plated at 2 × 105 cells per well in flat bottom 96-well plates in complete media. Recombinant IL-17 and IL-22 (Biolegend) were added for 4 h at the concentration indicated after which cells were harvested and lysed for qPCR.
In some experiments, CD4+TCR-β+CD45.1+ (WT progeny) and CD4+TCR-β+CD45.1− (Tbx21−/− progeny) T cells were sort-purified from the colon of C57BL/6 Rag1−/− recipient mice. Cells were stimulated with IL-23 (10 ng ml−1) for 12 h, the supernatant collected and added at 20% of total culture volume to epithelial cells in combination with blocking antibodies as indicated: anti-IL-17A (10 μg ml−1, clone 17F3 BioXCell), anti-IL-22 (10 μg ml−1, Genentech) or isotype control. Cells were stimulated for 4 h after which cells were harvested and lysed for qPCR.
qPCR
RNA was extracted according to the manufacturers' protocol (RNeasy, Qiagen) and cDNA synthesis was performed using Superscript III reverse transcription and Oligo dT primers (both from Invitrogen). qPCR reactions were performed using TaqMan Gene Expression Assays and normalized to hypoxanthine-guanine phosphoribosyltransferase (HPRT; all from Applied Biosystems). Samples were assayed in duplicate on a Bio-Rad CFX96 RT-qPCR or ABI Vii machine and differences were calculated using the 2ΔC(t) method.
Total protein extracts and immunoblot analysis
Total protein extracts were prepared by lysing cells in protein lysis buffer (20 mM Tris pH 8.0, 300 mM NaCl, 10% Glycerol, 1% NP-40) for 30 min on ice. After centrifugation at full speed to pellet debris, equal amounts of protein were resolved by SDS–polyacrylamide gel electrophoresis and analysed with anti-pY705-STAT3 (clone D3A7, Cat. Nr. 9145, 1/1,000 dilution, Cell Signaling), anti-STAT3 (clone 79D7, Cat. Nr. 4904, 1/1,000 dilution, Cell Signaling), anti-EOMES (clone 21Mags8, Cat. Nr. 14-4876-80, 1/500 dilution, eBiosciences), anti-Actin (clone AC-15, Cat. Nr. A5541, 1/1,0000 Sigma) or anti-Runx3 (1/1,000, gift from Yoram Groner). Images in Fig. 5e have been cropped for presentation. Full size images are presented in Supplementary Fig. 7A–E.
Chromatin immunoprecipitation
For in vitro ChIP assays, naïve CD4+CD25−CD44−CD62L+ T cells were sort-purified from spleens and lymphnodes of steady state C57BL/6 mice. Cells were plated at 3x105 cells per well in complete media in 48-well plates coated with anti-CD3 (5 μg ml−1). Antibodies and cytokines were added at the following concentrations: anti-CD28 (2 μg ml−1) and IL-2 (100 U ml−1, Peprotech) for Th0 or anti-CD28 (2 μg ml−1), IL-2 (100 U ml−1), IL-12 (10 ng ml−1, Peprotech) and anti-IL-4 (10 μg ml−1, Biolegend) for Th1. Cells were cultured for 36 h and stimulated with fresh IL-12 (10 ng ml−1) for the last 4 h. For ex vivo ChIP assays, CD4+TCR-β+CD45.1+ (WT progeny) and CD4+TCR-β+CD45.1− (Tbx21−/− progeny) T cells were sort-purified from the colon of C57BL/6 Rag1−/− recipient mice.
ChIP assays were performed as described60. Briefly, cells were washed once with PBS and fixed with 1% paraformaldehyde (Sigma) for 10 min at room temperature. 125 mM of Tris pH 7 was added to stop the reaction. Cells were pelleted, washed, lysed in sonication buffer (10 mM Tris-HCl pH 8.0, 100 mM NaCl, 1 mM EDTA, 0.5 mM EGTA, 0.1% Na-Deoxycholate, 0.5% Na-Lauroylsarcosine; all from Sigma) and sonicated using a Bioruptor Pico (Diagenode) to obtain a fragment size of around 500 base pairs. Lysates were centrifuged at full speed for 5 min at 4 °C and an aliquot (10%) was taken at this point as input control DNA. Remaining lysates were incubated with antibodies pre-bound to Protein G magnetic beads (Live Technologies) at 4 °C on a rotator overnight. The following antibodies were used, T-bet (Cat. Nr. sc-21003, 3 ug per IP, Santa Cruz), RNA Pol II (sc-899, 2 ug per IP, Santa Cruz) or H3K4me3 (Pab-003-050, 3 ug per IP, Diagenode). Beads were then placed on a magnet, washed five times with wash buffer (50 mM Hepes-KOH pH 7.6, 500 mM LiCl, 1 mM EDTA, 1% NP-40, 0.7% Na-deoxycholate; all from Sigma) and once with Tris-EDTA (TE) containing 50 mM NaCl. After the final wash, beads were resuspended in elution buffer (1 × TE containing 2% SDS) and reverse cross-linking performed at 65 °C in a shaking heat block overnight. Reverse cross-linking was similarly performed on input control DNA. The immunoprecipitated DNA fragments and input control DNA were purified using QIAquick PCR Purification Kit (Qiagen) as per the manufacturers' protocol and then analysed by quantitative reverse transcription PCR on a ABI Vii machine with SYBR Premix Ex Taq II master mix (Takara Bio) and the following primers: locus encoding Csf2 TSS, 5′-agagaaaggctaaggtcctgagga-3′ and 5′-ccaggaggttcagggcttcttt-3', locus encoding Il23r TSS, 5′-agggctctgctgacatttccat-3′ and 5′-acagctgcctctatgtatctcagga-3′, or locus encoding part of Il23r intron 3, 5′-gtcactgagcacctgtcccttc-3′ and 5′-aaacccctcaaccaacagcagg-3′.
Statistical analysis
Where appropriate the Mann–Whitney U test or Student's t-test was used. For comparison of more than two groups a Kruskal–Wallis one-way ANOVA followed by a Dunn's post hoc test or one-way ANOVA followed by a Bonferroni multiple comparison test was performed. All statistical analysis was calculated in Prism (Graphpad). Differences were considered to be statistically significant when P≤0.05.
Data availability
The data that support the findings of this study are available from the corresponding authors on request.
Additional information
How to cite this article: Krausgruber, T. et al. T-bet is a Key Modulator of IL-23-driven Pathogenic CD4+ T cell Responses in the Intestine. Nat. Commun. 7:11627 doi: 10.1038/ncomms11627 (2016).
Supplementary Material
Supplementary Figures 1-7
Acknowledgments
T.K., C.S., K.A., A.C., O.J.H., M.S. and F.P. are supported by the Wellcome Trust. F.P. is also supported by Fondation Louis Jeantet. We thank Dan Littman for providing the Rorc−/− strain and Yoram Groner for providing Runx3 antibody. We thank all members of the Oxford Translational Gastroenterology Unit, the Dunn School of Pathology and the Kennedy Institute of Rheumatology for assistance and support. We are grateful to Helen Ferry and Kate Alford for essential flow cytometry support and the staff of the University of Oxford for excellent animal care.
Footnotes
Author contributions T.K. and C.S. planned experiments and analysed the data. T.K., C.S. and F.P. wrote the paper. K.A., O.J.H., A.C., C.P., P.P.A. and M.S. performed particular experiments and were involved in data discussions. M.O. provided essential mouse strains.
References
- Weaver C. T., Elson C. O., Fouser L. A. & Kolls J. K. The Th17 pathway and inflammatory diseases of the intestines, lungs, and skin. Annu. Rev. Pathol. 8, 477–512 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shale M., Schiering C. & Powrie F. CD4(+) T-cell subsets in intestinal inflammation. Immunol. Rev. 252, 164–182 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov I. I. et al. The orphan nuclear receptor RORgammat directs the differentiation program of proinflammatory IL-17+ T helper cells. Cell 126, 1121–1133 (2006). [DOI] [PubMed] [Google Scholar]
- Zhou L. et al. IL-6 programs T(H)-17 cell differentiation by promoting sequential engagement of the IL-21 and IL-23 pathways. Nat. Immunol. 8, 967–974 (2007). [DOI] [PubMed] [Google Scholar]
- Huh J. R. et al. Digoxin and its derivatives suppress TH17 cell differentiation by antagonizing RORgammat activity. Nature 472, 486–490 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oppmann B. et al. Novel p19 protein engages IL-12p40 to form a cytokine, IL-23, with biological activities similar as well as distinct from IL-12. Immunity 13, 715–725 (2000). [DOI] [PubMed] [Google Scholar]
- Cua D. J. et al. Interleukin-23 rather than interleukin-12 is the critical cytokine for autoimmune inflammation of the brain. Nature 421, 744–748 (2003). [DOI] [PubMed] [Google Scholar]
- Murphy C. A. et al. Divergent pro- and antiinflammatory roles for IL-23 and IL-12 in joint autoimmune inflammation. J. Exp. Med. 198, 1951–1957 (2003). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kullberg M. C. et al. IL-23 plays a key role in Helicobacter hepaticus-induced T cell-dependent colitis. J. Exp. Med. 203, 2485–2494 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hue S. et al. Interleukin-23 drives innate and T cell-mediated intestinal inflammation. J. Exp. Med. 203, 2473–2483 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlig H. H. et al. Differential activity of IL-12 and IL-23 in mucosal and systemic innate immune pathology. Immunity 25, 309–318 (2006). [DOI] [PubMed] [Google Scholar]
- Yen D. et al. IL-23 is essential for T cell-mediated colitis and promotes inflammation via IL-17 and IL-6. J. Clin. Invest. 116, 1310–1316 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirota K. et al. Fate mapping of IL-17-producing T cells in inflammatory responses. Nat. Immunol. 12, 255–263 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szabo S. J. et al. A novel transcription factor, T-bet, directs Th1 lineage commitment. Cell 100, 655–669 (2000). [DOI] [PubMed] [Google Scholar]
- Zhu J. et al. The transcription factor T-bet is induced by multiple pathways and prevents an endogenous Th2 cell program during Th1 cell responses. Immunity 37, 660–673 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei G. et al. Global mapping of H3K4me3 and H3K27me3 reveals specificity and plasticity in lineage fate determination of differentiating CD4+ T cells. Immunity 30, 155–167 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukasa R. et al. Epigenetic instability of cytokine and transcription factor gene loci underlies plasticity of the T helper 17 cell lineage. Immunity 32, 616–627 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neurath M. F. et al. The transcription factor T-bet regulates mucosal T cell activation in experimental colitis and Crohn's disease. J. Exp. Med. 195, 1129–1143 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leppkes M. et al. RORgamma-expressing Th17 cells induce murine chronic intestinal inflammation via redundant effects of IL-17A and IL-17F. Gastroenterology 136, 257–267 (2009). [DOI] [PubMed] [Google Scholar]
- Ahern P. P. et al. Interleukin-23 drives intestinal inflammation through direct activity on T cells. Immunity 33, 279–288 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y. K. et al. Late developmental plasticity in the T helper 17 lineage. Immunity 30, 92–107 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nistala K. et al. Th17 plasticity in human autoimmune arthritis is driven by the inflammatory environment. Proc. Natl Acad. Sci. USA 107, 14751–14756 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bending D. et al. Highly purified Th17 cells from BDC2.5NOD mice convert into Th1-like cells in NOD/SCID recipient mice. J. Clin. Invest. 119, 565–572 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrison P. J. et al. Th17-cell plasticity in Helicobacter hepaticus-induced intestinal inflammation. Mucosal Immunol. 6, 1143–1156 (2013). [DOI] [PubMed] [Google Scholar]
- Annunziato F. et al. Phenotypic and functional features of human Th17 cells. J. Exp. Med. 204, 1849–1861 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosmi L. et al. Human interleukin 17-producing cells originate from a CD161+CD4+ T cell precursor. J. Exp. Med. 205, 1903–1916 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powrie F., Leach M. W., Mauze S., Caddle L. B. & Coffman R. L. Phenotypically distinct subsets of CD4+ T cells induce or protect from chronic intestinal inflammation in C. B-17 scid mice. Int. Immunol. 5, 1461–1471 (1993). [DOI] [PubMed] [Google Scholar]
- Read S., Malmstrom V. & Powrie F. Cytotoxic T lymphocyte-associated antigen 4 plays an essential role in the function of CD25(+)CD4(+) regulatory cells that control intestinal inflammation. J. Exp. Med. 192, 295–302 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awasthi A. et al. Cutting edge: IL-23 receptor gfp reporter mice reveal distinct populations of IL-17-producing cells. J. Immunol. 182, 5904–5908 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y. et al. T-bet is essential for encephalitogenicity of both Th1 and Th17 cells. J. Exp. Med. 206, 1549–1564 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghoreschi K. et al. Generation of pathogenic T(H)17 cells in the absence of TGF-beta signalling. Nature 467, 967–971 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryckman C., Vandal K., Rouleau P., Talbot M. & Tessier P. A. Proinflammatory activities of S100: proteins S100A8, S100A9, and S100A8/A9 induce neutrophil chemotaxis and adhesion. J. Immunol. 170, 3233–3242 (2003). [DOI] [PubMed] [Google Scholar]
- Nakayamada S. et al. Early Th1 cell differentiation is marked by a Tfh cell-like transition. Immunity 35, 919–931 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gokmen M. R. et al. Genome-wide regulatory analysis reveals that T-bet controls Th17 lineage differentiation through direct suppression of IRF4. J. Immunol. 191, 5925–5932 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearce E. L. et al. Control of effector CD8+ T cell function by the transcription factor Eomesodermin. Science 302, 1041–1043 (2003). [DOI] [PubMed] [Google Scholar]
- Suto A., Wurster A. L., Reiner S. L. & Grusby M. J. IL-21 inhibits IFN-gamma production in developing Th1 cells through the repression of Eomesodermin expression. J. Immunol. 177, 3721–3727 (2006). [DOI] [PubMed] [Google Scholar]
- Yang Y., Xu J., Niu Y., Bromberg J. S. & Ding Y. T-bet and eomesodermin play critical roles in directing T cell differentiation to Th1 versus Th17. J. Immunol. 181, 8700–8710 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djuretic I. M. et al. Transcription factors T-bet and Runx3 cooperate to activate Ifng and silence Il4 in T helper type 1 cells. Nat. Immunol. 8, 145–153 (2007). [DOI] [PubMed] [Google Scholar]
- Yagi R. et al. The transcription factor GATA3 actively represses RUNX3 protein-regulated production of interferon-gamma. Immunity 32, 507–517 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park H. et al. A distinct lineage of CD4 T cells regulates tissue inflammation by producing interleukin 17. Nat. Immunol. 6, 1133–1141 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rangachari M. et al. T-bet negatively regulates autoimmune myocarditis by suppressing local production of interleukin 17. J. Exp. Med. 203, 2009–2019 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan X. et al. A novel role of CD4 Th17 cells in mediating cardiac allograft rejection and vasculopathy. J. Exp. Med. 205, 3133–3144 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lazarevic V. et al. T-bet represses T(H)17 differentiation by preventing Runx1-mediated activation of the gene encoding RORgammat. Nat. Immunol. 12, 96–104 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y. et al. Induction and molecular signature of pathogenic TH17 cells. Nat. Immunol. 13, 991–999 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okamoto M. et al. Mina, an Il4 repressor, controls T helper type 2 bias. Nat. Immunol. 10, 872–879 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ivanov I. I. et al. Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell 139, 485–498 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stepankova R. et al. Segmented filamentous bacteria in a defined bacterial cocktail induce intestinal inflammation in SCID mice reconstituted with CD45RBhigh CD4+ T cells. Inflamm. Bowel Dis. 13, 1202–1211 (2007). [DOI] [PubMed] [Google Scholar]
- Griseri T., McKenzie B. S., Schiering C. & Powrie F. Dysregulated hematopoietic stem and progenitor cell activity promotes interleukin-23-driven chronic intestinal inflammation. Immunity 37, 1116–1129 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griseri T. et al. Granulocyte macrophage colony-stimulating factor-activated eosinophils promote interleukin-23 driven chronic colitis. Immunity 43, 187–199 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sonnenberg G. F. et al. Pathological versus protective functions of IL-22 in airway inflammation are regulated by IL-17A. J. Exp. Med. 207, 1293–1305 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y. et al. The transcription factors T-bet and Runx are required for the ontogeny of pathogenic interferon-gamma-producing T helper 17 cells. Immunity 40, 355–366 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann J. et al. T-bet expression by Th cells promotes type 1 inflammation but is dispensable for colitis. Mucosal Immunol. doi: 10.1038/mi.2016.5 (2016). [DOI] [PubMed] [Google Scholar]
- Powrie F., Correa-Oliveira R., Mauze S. & Coffman R. L. Regulatory interactions between CD45RBhigh and CD45RBlow CD4+ T cells are important for the balance between protective and pathogenic cell-mediated immunity. J. Exp. Med. 179, 589–600 (1994). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powrie F. et al. Inhibition of Th1 responses prevents inflammatory bowel disease in scid mice reconstituted with CD45RBhi CD4+ T cells. Immunity 1, 553–562 (1994). [DOI] [PubMed] [Google Scholar]
- Biancheri P., Powell N., Monteleone G., Lord G. & MacDonald T. T. The challenges of stratifying patients for trials in inflammatory bowel disease. Trends Immunol. 34, 564–571 (2013). [DOI] [PubMed] [Google Scholar]
- Duerr R. H. et al. A genome-wide association study identifies IL23R as an inflammatory bowel disease gene. Science 314, 1461–1463 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jostins L. et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature 491, 119–124 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Izcue A. et al. Interleukin-23 restrains regulatory T cell activity to drive T cell-dependent colitis. Immunity 28, 559–570 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhlig H. H. et al. Characterization of Foxp3+CD4+CD25+ and IL-10-secreting CD4+CD25+ T cells during cure of colitis. J Immunol. 177, 5852–5860 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krausgruber T. et al. IRF5 promotes inflammatory macrophage polarization and TH1-TH17 responses. Nat. Immunol. 12, 231–238 (2011). [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figures 1-7
Data Availability Statement
The data that support the findings of this study are available from the corresponding authors on request.