Abstract
Backgrounds/Aims
To understand the changing demands for hepatic resection (HR), we collected data regarding HR performed in a tertiary centre over a period of 10 years.
Methods
We carried out extensive search of institutional databases to identify HR cases performed between January 2005 and December 2014. A study cohort of 9,016 patients were divided into 5 disease categories, namely hepatocellular carcinoma (HCC), intrahepatic cholangiocarcinoma (ICC), intrahepatic duct stone disease (IHDS), colorectal cancer liver metastasis (CRLM), and uncommon/rare diseases (URD).
Results
There were 5,661 (62.8%) HCC cases, followed by 1441 (16.0%) CRLM, 942 (10.5%) ICC, 638 (7.1%) IHDS and 334 (3.7%) URD. The number of annual HR cases gradually increased from 443 in 2005 to 1,260 in 2015. Annual HCC cases also gradually increased, but the annual proportion of HCC cases fluctuated narrowly between 58.3% and 70.2%. Annual CRLM cases increased rapidly, and their proportion increased progressively from 4.7% to 20.5%. Annual ICC cases increased slowly, and their annual proportion fluctuated between 7.2% and 15.6%. Annual IHDS cases decreased slowly, and their annual proportion decreased progressively from 17.2% to 3.4%, while annual URD cases fluctuated, with annual proportions varying between 2.3% and 5.6%.
Conclusions
Annual cases of HR increased over the last 10 years in a tertiary center probably due to a center-specific centralization effect. The number of CRLM cases increased rapidly; those of HCC and ICC increased gradually, and those of IHDS declined gradually. We believe that these results reflect real changes in the types of liver disease requiring HR.
Keywords: Hepatocellular carcinoma, Intrahepatic cholangiocarcinoma, Liver metastasis, Intrahepatic duct stone, Benign liver disease, Hepatic resection, Prevalence, Incidence
INTRODUCTION
Hepatic resection (HR) is indicated for a variety of hepatobiliary diseases and metastatic lesions, and so constitutes a major proportion of the workload in the field of general surgery. The analysis of cases should provide insight into the demands of the various diseases requiring HR.
In Korea, the proportions of common hepatobiliary diseases encountered in everyday surgical practice have changed during the last decade, probably due to more frequent early diagnosis as well as actual changes in the prevalence of certain diseases. However, direct analysis of the incidence and prevalence of common hepatobiliary diseases is very difficult, and such epidemiologic information is available only through government-controlled cancer registries.1,2,3
It could be useful to understand the changing demands for HR and recent trends in the types of liver diseases requiring HR. Therefore, we aimed to analyse cohort data regarding HR performed in a tertiary centre over a period of 10 years.
MATERIALS AND METHODS
By extensive search of institutional databases of HR cases dealt with between January 2005 and December 2014, we identified more than 10,000 adult patients who underwent HR, after excluding liver transplantation-associated surgery. At first, the cases were divided into two groups according to the role of HR. One group comprised cases of primary-purpose HR performed to directly remove liver lesions (e.g., hepatocellular carcinoma and intrahepatic cholangiocarcinoma), and the other group comprised cases of secondary-purpose HR performed along with other resectional procedures (e.g., bile duct cancer surgery or gallbladder cancer surgery including HR). In order to make the design of the present study as simple and comprehensible as possible, we focused only on primary-purpose HR. The study cohort was divided into 5 disease categories as follows: hepatocellular carcinoma (HCC), intrahepatic cholangiocarcinoma (ICC), intrahepatic duct stone disease (IHDS), colorectal cancer liver metastasis (CRLM), and uncommon or rare disease entities (URD) including hemangioma, liver cyst, abscess and focal nodular hyperplasia. Other rare disease entities were not taken into account in this study. Finally, the study cohort comprised 9,016 patients undergoing HR over the 10-year study period.
This retrospective cohort study was approved by the Institutional Review Board of our institution. Descriptive statistical analyses were performed using SPSS (version 20; IBM).
RESULT
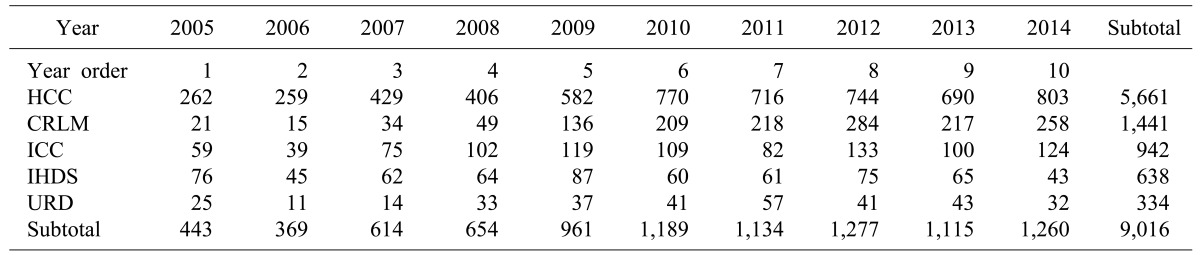
In the cohort of 9,016 HR cases, there were 5,661 (62.8%) HCC cases, followed by 1441 (16.0%) CRLM, 942 (10.5%) ICC, 638 (7.1%) IHDS, and 334 (3.7%) URD. A detailed profile of the annual incidences is given in Table 1. The total number of annual HR cases increased gradually from 443 in year 2005 to 1,260 in year 2015 (Fig. 1).
Table 1. Annual incidences of liver resection cases.
HCC, hepatocellular carcinoma; ICC, intrahepatic cholangiocarcinoma; IHDS, intrahepatic duct stone disease; CRLM, colorectal cancer liver metastasis; URD, uncommon or rare diseases
Fig. 1. Cumulative incidences of annual cases in the five disease categories. HCC, hepatocellular carcinoma; ICC, intrahepatic cholangiocarcinoma; IHDS, intrahepatic duct stone disease; CRLM, colorectal cancer liver metastasis; URD, uncommon or rare diseases.
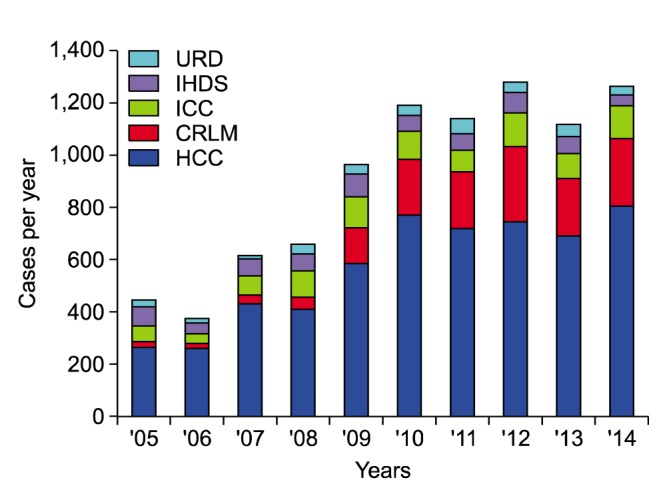
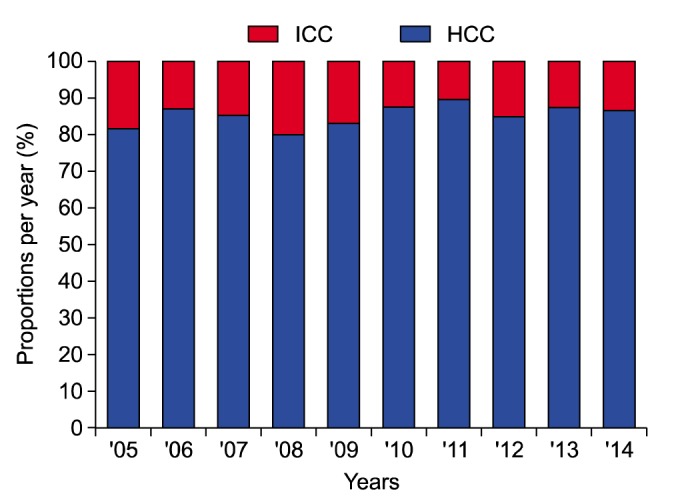
Annual HCC cases increased gradually from 262 in year 2005 to 803 in year 2014 (Fig. 2), but the annual proportion of HCC cases fluctuated narrowly between 58.3% and 70.2% (Fig. 3). Annual CRLM cases increased rapidly from 21 in year 2005 to 258 in year 2014 (Fig. 2), and the proportion of annual HR cases increased progressively from 4.7% in year 2005 to 20.5% in 2014 (Fig. 3). Annual ICC cases increased slowly from 59 in year 2005 to 124 in year 2014 (Fig. 2), and their annual proportions fluctuated between 7.2% and 15.6% (Fig. 3). Annual IHDS cases decreased slowly, and their annual proportions decreased progressively from 17.2% to 3.4%. Annual URD cases fluctuated, with annual proportions varying between 2.3% and 5.6%. Considering only cases of HCC and ICC, the annual proportion of ICC cases also fluctuated between 10.3% and 20.1% (Fig. 4). Annual IHDS cases decreased slowly from 76 in year 2005 to 43 in year 2014 (Fig. 2). For IHDS, annual case numbers slowly decreased and their proportion of annual HR cases decreased progressively from 17.2% in 2005 to 3.4% in 2014 (Fig. 3). Annual URD cases fluctuated from 25 in year 2005 to 32 in year 2014 (Fig. 2), with annual proportions varying between 2.3% and 5.6%.
Fig. 2. Changes in the incidences of annual cases per disease category.
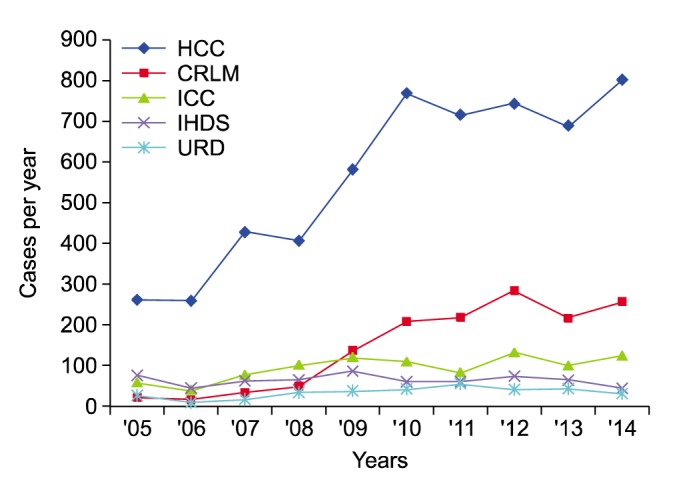
Fig. 3. Changes in the proportions of annual cases per disease category.
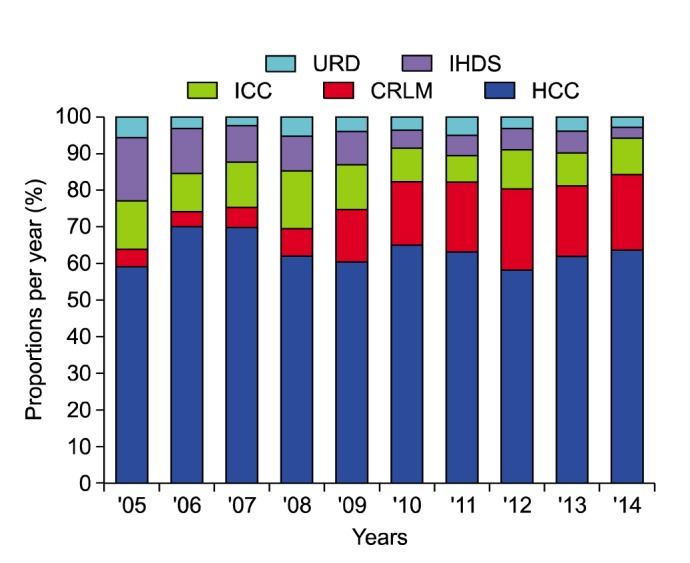
Fig. 4. Changes in the proportions of annual cases in the hepatocellular carcinoma (HCC) and intrahepatic cholangiocarcinoma (ICC) categories.
DISCUSSION
Over the last 10 years the annual number of adult patients undergoing HR for abovementioned 5-category diseases in our institution nearly tripled from 443 in year 2005 to 1,260 in year 2015. A progressive increase in the number of HCC patients greatly contributed to this increase. Considering that liver cancer incidence decreased slowly from 25.8 per 100,000 in 2005 to 21.1 persons per 100,000 in 2012, such a marked increase in HCC cases undergoing HR may point to a centralization effect of this specific tertiary centre.1,2,3 We also presume that another reason is an increased preference for HR as HCC treatment over non-surgical treatments because a majority of the HCC were diagnosed early through routine screening. In fact, approximately 80% of solitary HCCs undergoing HR in our institution were detected during regular health screening or routine follow-up.4 The patient concentration via the centralization effect enabled us to establish high-volume HCC databases, from which we could obtain single-centre data for 2558 patients undergoing resection of solitary HCC and 471 patients undergoing resection of large HCC ≥10 cm.4,5
HR is being performed more frequently for CRLM than before, and this also contributed to the noticeable increase in the number of annual HR cases. This rapid increase may also reflect the recent increase in colorectal cancer prevalence in the general population from 31.0 per 100,000 in year 2005 to 37.3 per 100,000 in year 2012.2 The proportion of CRLM HR cases rose to around 20% of all HR cases in 2014, indicating that HR is already an established treatment modality for CRLM combined with systemic chemotherapy,6,7,8 in Korea as in Western countries.
Annual cases of HR for ICC increased slowly, but their annual proportion fluctuated between 10.3% and 20.1% of the sum of ICC and HCC cases. Considering that ICC is rare compared with HCC,9,10,11 the high case number and proportion of ICC may reflect the centralization effect of this tertiary centre, where we were able to establish high-volume ICC databases and analyse the single-centre experiences of 659 patients undergoing resection for ICC.12 Although the actual incidence of ICC in the Korean general population is not available, it is generally accepted that its incidence is gradually increasing worldwide.9,10,11
Unlike CRLM, the annual number of cases of IHDS slowly decreased. Because of the progressive increase in annual HR volume, the proportion of IHDS rapidly and progressively decreased from 17.2% in year 2005 to 3.4% in year 2014. This definite decreasing trend may reflect the recent effective management and prevention of Clonorchis sinensis and other inflammatory diseases as well as a higher frequency of non-surgical treatment for hepatobiliary stone diseases.13
We arbitrarily included hemangioma, liver cyst, abscess and focal nodular hyperplasia as the URD group, the fifth category requiring HR. The actual prevalence of these diseases in the general population is not low, but only a small proportion of the patients have undergone HR because a majority of these diseases are not indicated for any surgical treatment.14,15,16
There are several limitations to this study. First, it was a retrospective, single-center study. Although the sample number was not small, HR case numbers and their proportions must have been greatly influenced by the center-specific centralization. Second, we could not reliably match the HR case numbers with the incidences of the corresponding diseases in the general population due to lack of nationwide registry data. Thus, high-volume multi-center studies should be carried out to reveal the real trends in hepatobiliary diseases requiring HR.
In summary, annual cases of HR increased in a tertiary center over the last 10 years probably due to a center-specific centralization effect. Among them, the total number of CRLM cases rapidly increased; those of HCC and ICC increased gradually, and that of IHDS declined gradually. We believe that these results may reflect the real changes in the types of liver diseases requiring HR and that they will be useful for predicting further changes in the near future.
References
- 1.Jung KW, Won YJ, Kong HJ, Oh CM, Lee DH, Lee JS. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2011. Cancer Res Treat. 2014;46:109–123. doi: 10.4143/crt.2014.46.2.109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jung KW, Won YJ, Kong HJ, Oh CM, Cho H, Lee DH, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2012. Cancer Res Treat. 2015;47:127–141. doi: 10.4143/crt.2015.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jung KW, Won YJ, Oh CM, Kong HJ, Cho H, Lee DH, et al. Prediction of cancer incidence and mortality in Korea, 2015. Cancer Res Treat. 2015;47:142–148. doi: 10.4143/crt.2015.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, Ha TY, et al. The impact of tumor size on long-term survival outcomes after resection of solitary hepatocellular carcinoma: single-institution experience with 2558 patients. J Gastrointest Surg. 2015;19:1281–1290. doi: 10.1007/s11605-015-2849-5. [DOI] [PubMed] [Google Scholar]
- 5.Hwang S, Lee YJ, Kim KH, Ahn CS, Moon DB, Ha TY, et al. Long-term outcome after resection of huge hepatocellular carcinoma ≥ 10 cm: single-institution experience with 471 patients. World J Surg. 2015;39:2519–2528. doi: 10.1007/s00268-015-3129-y. [DOI] [PubMed] [Google Scholar]
- 6.Yoon YS, Kim CW, Lim SB, Yu CS, Kim SY, Kim TW, et al. Palliative surgery in patients with unresectable colorectal liver metastases: a propensity score matching analysis. J Surg Oncol. 2014;109:239–244. doi: 10.1002/jso.23480. [DOI] [PubMed] [Google Scholar]
- 7.Seo SI, Lim SB, Yoon YS, Kim CW, Yu CS, Kim TW, et al. Comparison of recurrence patterns between ≤5 years and >5 years after curative operations in colorectal cancer patients. J Surg Oncol. 2013;108:9–13. doi: 10.1002/jso.23349. [DOI] [PubMed] [Google Scholar]
- 8.Kim KH, Yoon YS, Yu CS, Kim TW, Kim HJ, Kim PN, et al. Comparative analysis of radiofrequency ablation and surgical resection for colorectal liver metastases. J Korean Surg Soc. 2011;81:25–34. doi: 10.4174/jkss.2011.81.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Njei B. Changing pattern of epidemiology in intrahepatic cholangiocarcinoma. Hepatology. 2014;60:1107–1108. doi: 10.1002/hep.26958. [DOI] [PubMed] [Google Scholar]
- 10.Lubezky N, Facciuto M, Harimoto N, Schwartz ME, Florman SS. Surgical treatment of intrahepatic cholangiocarcinoma in the USA. J Hepatobiliary Pancreat Sci. 2015;22:124–130. doi: 10.1002/jhbp.157. [DOI] [PubMed] [Google Scholar]
- 11.Yamamoto M, Ariizumi S. Surgical outcomes of intrahepatic cholangiocarcinoma. Surg Today. 2011;41:896–902. doi: 10.1007/s00595-011-4517-z. [DOI] [PubMed] [Google Scholar]
- 12.Hwang S, Lee YJ, Song GW, Park KM, Kim KH, Ahn CS, et al. Prognostic impact of tumor growth type on 7th AJCC staging system for intrahepatic cholangiocarcinoma: a single-center experience of 659 cases. J Gastrointest Surg. 2015;19:1291–1304. doi: 10.1007/s11605-015-2803-6. [DOI] [PubMed] [Google Scholar]
- 13.Cheon YK, Cho YD, Moon JH, Lee JS, Shim CS. Evaluation of long-term results and recurrent factors after operative and nonoperative treatment for hepatolithiasis. Surgery. 2009;146:843–853. doi: 10.1016/j.surg.2009.04.009. [DOI] [PubMed] [Google Scholar]
- 14.Hoffmann K, Unsinn M, Hinz U, Weiss KH, Waldburger N, Longerich T, et al. Outcome after a liver resection of benign lesions. HPB (Oxford) 2015;17:994–1000. doi: 10.1111/hpb.12496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ciria R, Cherqui D, Geller DA, Briceno J, Wakabayashi G. Comparative short-term benefits of laparoscopic liver resection: 9000 cases and climbing. Ann Surg. 2016;263:761–777. doi: 10.1097/SLA.0000000000001413. [DOI] [PubMed] [Google Scholar]
- 16.Hau HM, Atanasov G, Tautenhahn HM, Ascherl R, Wiltberger G, Schoenberg MB, et al. The value of liver resection for focal nodular hyperplasia: resection yes or no? Eur J Med Res. 2015;20:86. doi: 10.1186/s40001-015-0181-x. [DOI] [PMC free article] [PubMed] [Google Scholar]