Abstract
Objective
The intention of this manikin-based trial was to evaluate whether laypersons are able to operate an I-gel laryngeal mask (I-gel) modified for mouth-to-mask ventilation after receiving brief on-site instruction.
Setting
Entrance hall of a university hospital and the city campus of a public technical university, using a protected manikin scenario.
Methods
Laypersons were handed a labelled, mouthpiece-integrated I-gel laryngeal mask and a corresponding instruction chart and were asked to follow the printed instructions.
Outcome measures
The overall process was analysed and evaluated according to quality and duration.
Results
Data from 100 participants were analysed. Overall, 79% of participants were able to effectively ventilate the manikin, 90% placed the laryngeal mask with the correct turn and direction, 19% did not position the mask deep enough and 85% believed that their inhibition threshold for performing resuscitation was lowered. A significant reduction in reluctance before and after the trial was found (p<0.0001). A total of 35% of participants had concerns about applying first aid in an emergency. Former basic life support (BLS) training significantly reduced the time of insertion (19.6 s, 95% CI 17.8 to 21.5, p=0.0004) and increased overall success (p=0.0096).
Conclusions
Laypersons were able to manage mouth-to-mask ventilation in the manikin with a reasonable success rate after receiving brief chart-based on-site instructions using a labelled I-gel mask. Positioning the mask deep enough and identifying whether the manikin was successfully ventilated were the main problems observed. A significant reduction in reluctance towards initialising BLS by using a modified supraglottic airway device (SAD) may lead to better acceptance of bystander resuscitation in laypersons, supporting the introduction of SADs into BLS courses and the stocking of SADs in units with public automatic external defibrillators.
Keywords: MEDICAL EDUCATION & TRAINING, ACCIDENT & EMERGENCY MEDICINE, EDUCATION & TRAINING (see Medical Education & Training)
Strengths and limitations of this study.
This study aimed to qualitatively investigate the feasibility of using a modified I-gel as a reasonable alternative to mouth-to-mouth ventilation by laypersons and to determine participants' attitudes towards providing first aid in general and after becoming familiar with the device.
The use of an easily operated supraglottic airway device reduces laypersons' reluctance to initiate first aid and mouth-to-mask ventilation.
A limitation of our study is the simulated setting using a manikin, which could have affected the scenario and limited the transferability of the data to real life situations but provides safe qualitative information.
The lack of a conventional mouth-to-mouth ventilation group precludes a comparison to a control group.
Introduction
Bag-valve mask ventilation (BVMV) and bag-valve ventilation connected to a supraglottic airway device (SAD) with an inflatable cuff, for example, Laryngeal Mask Classic and Supreme, have been found to be too complex for laypersons to use.1 2 This study addresses the idea of placing and using a modified I-gel laryngeal mask (I-gel) (a gel-like thermoplastic elastomer with a non-inflatable cuff)—a SAD with mouth-to-mask ventilation—on a manikin by laypersons using a newly designed instruction chart.
Laypersons, especially in domestic settings, are often confronted with circulatory arrests before professional medical healthcare providers arrive.3 Moreover, the worldwide trend towards increasing urbanisation and rural depopulation is a challenge for first responders and ambulance services4 and may emphasise the role of laypersons' responsibilities for providing prompt help in emergencies.
The probability of long-term survival after cardiac arrest is very much dependent on immediate resuscitation by laypersons or first responders.5–7 According to the latest ERC guidelines, the ideal ratio between chest compressions and mouth-to-mouth ventilations is 30:2. Once the patient's trachea is intubated or the airway is secured with a SAD, it is recommended to continue chest compression at a rate of 100/min without interruption while ventilating the lungs ∼10 times/min. This combination enables a relevant higher median coronary perfusion pressure.8 It is well known that only performing chest compression resuscitation provides superior benefits compared with no cardiopulmonary resuscitation (CPR)9 and may be an option for lay responders with limited experience in mouth-to-mouth ventilation, acknowledging the consequences of no or incorrect ventilation. Nevertheless, managing the airway of patients in emergency situations, especially if professional help requires more than 5–10 min to arrive at the scene, is an essential step in first aid because it strongly impacts morbidity and mortality.10 However, in approximately two-third of all observed cardiac arrests, ‘first aiders’ do not attempt resuscitation as a result of doubts and fears concerning infectious secretions and making mistakes in mouth-to-mouth resuscitation.5 Therefore, an easily applied and hygienic alternative, such as a SAD, that can minimise people’s concerns towards first aid ventilation is desirable. However, BVMV and bag-valve ventilation devices connected to a SAD with an inflatable cuff have been shown to be too complex for laypersons to use.1 2 Several studies have demonstrated that, at least in the hands of trained medical staff, the use of SADs during CPR reduces the ‘no-flow-time’,11 increases the quantity of chest compressions12 and can ultimately improve outcomes.
Endotracheal intubation is still the gold standard for airway management. However, since intubation should only be applied by professional healthcare providers with sufficient technical training and experience, BVMV and SADs, for example, laryngeal masks (LMAs), are an acceptable alternative.8 Although LMAs might have a higher risk of aspiration during CPR than endotracheal intubation, only a few notable cases have been reported under these circumstances.8 Compared to the use of endotracheal tubes, SADs do not generally require an interruption of chest compression.12 Moreover, LMAs have advantages compared to the use of BVMV as they have been reported to be easier and more efficient in terms of their application1 and are less likely to cause regurgitation during CPR when used as a first line airway device.13 Among the SADs, the laryngeal mask has the highest proven success rates in individuals with limited clinical experience.1
The goal of this study was to investigate the ability of laypersons to operate a modified I-gel labelled with different coloured marks to aid in recognising proper mask placement in mouth-to-mask ventilation on the scene using a manikin, with instructions provided by a newly designed manual. In this trial, we used the I-gel because its features may make insertion by casual users easier.14 Among the different models of LMAs, the I-gel is the fastest to insert and is the most popular airway device,15 with acceptable seal formation and closing pressures.8
Information regarding the participants' evaluation of this method was gathered, in addition to the specific main reasons for individuals being reluctant to perform first aid in general.
Methods
In a manikin-based prospective feasibility trial, we investigated laypersons' abilities to provide mouth-to-mask ventilation using a modified I-gel laryngeal mask after receiving brief on-site instruction. The institutional review board (Rhine-Westphalia University of Technology Aachen, Germany, Medical Faculty, Ethical Review Committee; Chairman: Professor G. Schmalzing) waived the requirement for written informed consent as no impact on individual health was anticipated. This manuscript is presented in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology statement.
Recruitment of participants
Data were collected during March 2014 in the University Hospital of Aachen (Uniklink Rheinisch Westfälische Technische Hochschule (RWTH) Aachen) entrance hall and the city campus of RWTH Aachen, Germany.
Inclusion criteria were that the participants had no prior medical education (ie, physicians, nurses, medical students, paramedics and medical technologists), with the exception of having attended ‘first aid’ or basic life support (BLS) courses in the past. Exclusion criteria were any type of formal medical education.
We randomly selected and individually approached each subject. Prior to the experiment, participants were asked for personal data regarding age, sex, profession, first aid training (if they had received any, how long ago and how often), resuscitation experience, and whether personal convictions prevented them from performing first aid and mouth-to-mouth ventilation. Participants agreed with the anonymous scientific analysis of their personal data.
Experimental setting
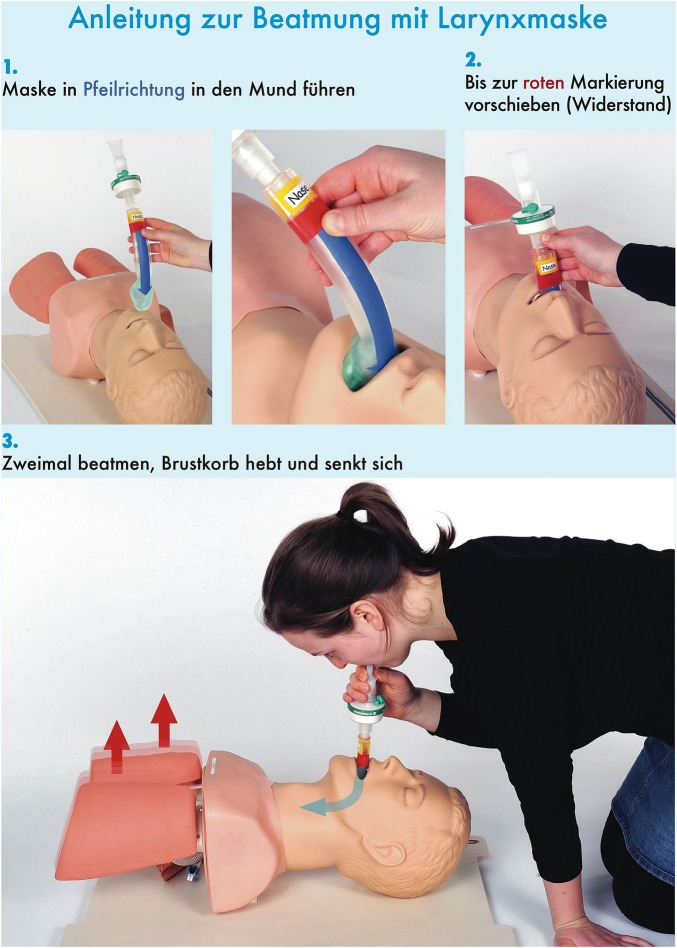
The I-gel is a gel-like transparent laryngeal mask that is made of a thermoplastic elastomer without an inflatable cuff.14 For this trial, it was labelled as follows: blue arrow for the direction, a red mark for the depth and a yellow mark with the label ‘nose’ on one side and ‘chin’ on the other side to indicate the orientation for insertion into the mouth of the manikin. To realise mouth-to-mask ventilation, a mouthpiece and hygienic filter were fixed to the ISO connector. The operation of the I-gel was displayed in four pictures on a separate instruction chart that was added to the package (figure 1).
Figure 1.
Instruction chart: ventilation with a laryngeal mask in three (1–3) steps. The colour of the lettering matches the colours of the labels on the laryngeal mask. The arrows on the mask and the chart illustrate the proper movement of the mask, the air and the lungs. (1) Lead the mask in the direction of the arrow into the mouth. (2) Push forward until the red mark is reached (resistance). (3) Ventilate twice until lifting and lowering of the chest is observed.
The experimental setting consisted of a manikin (Laerdal Airway Management Trainer Adult, Laerdal Medical GmbH Puchheim, Germany) on the floor with the non-transparent bagged ventilation package (instruction chart plus a previously labelled mouthpiece-equipped laryngeal mask (I-gel Laryngeal Mask, Intersurgical GmbH, Sankt Augustin, Germany)) nearby.
Participants were not instructed nor were they prepared prior to the experiment. They only knew about an experiment related to ‘first aid’ and that they should follow the directions given in the ‘aid package’ exactly. Thereafter, participants were handed a non-transparent package containing the modified I-gel and the ‘manual’. The trial started the moment the individuals were asked to open the package. During the experiment, participants were not given any verbal directions and nor were any of their questions answered.
The experimental site was an area that was protected and isolated from the view of an audience or other participants to avoid biases due to visual learning.
The primary (qualitative) outcome was the time from opening the bag until the second ventilation. Secondary qualitative and quantitative outcome parameters were the success of ventilation, the position of the mask and its direction, subjective judgements of success, the ease and comfort of the procedure as perceived by the participant and individuals' concerns about proceeding in case of an emergency. Moreover, we investigated the influence of former ‘first aid’ or BLS classes and age on individual performance.
Two questions followed each experiment:
Would you attempt to apply the mask using the instruction chart in an emergency?
Does the mask lower your inhibition threshold for performing ventilation?
Statistics
Statistical analysis was performed with GraphPad Prism V.6.0 for Mac (GraphPad Software, La Jolla, California, USA). A success rate of 90% was expected.2 16 The p<0.05 indicated statistical significance. To analyse the contingency, Fisher's exact test was used. An unpaired t test with equal SDs was also used. Moreover, an ordinary one-way ANOVA (analysis of variance) was employed. The data are presented as the means±SD if not otherwise mentioned.
Results
Data from 100 participants (67 men, 33 women) were analysed. On average, participants were 33.4±17.6 years old. The time elapsed since the last BLS course (n=92) was 8.2±8.1 years. Overall, individuals had completed 2.1±1.9 first aid courses. Two individuals (2%) had applied first aid skills in real life, and a total of 35% (n=35) had concerns about applying first aid in an emergency (table 1).
Table 1.
Demographic data and previous first aid knowledge
| Features | |
| Age, years | 33.4±17.6 |
| Sex,(n) | |
| Male | 67 (67%) |
| Female | 33 (33%) |
| First aid education, n | |
| None | 8 (8%) |
| <5 years | 43 (43%) |
| >5 years | 49 (49%) |
| Applied first aid in real life, n | 2 (2%) |
n, number.
The data are presented as the means±SD or as numbers (and percentage).
The average time from turning over the instruction chart until the second ventilation was 31.9 s (31.9±15.4 s, 95% CI 28.9 to 35). Ninety-four per cent (n=94) of participants believed that their ventilation was successful. Seventy-nine per cent (n=79, 0.79±0.4, 95% CI 0.71 to 0.87) of participants were able to effectively ventilate the manikin. Ninety per cent of participants managed to place the laryngeal mask with the right turn and direction, which suggests a basic understanding of the first part of the instruction chart. Nineteen per cent of participants did not position the mask at the proper depth (table 2). Nonetheless, five of the individuals were able to successfully ventilate the manikin, despite placing the mask too deep (n=2) or not deep enough (n=3).
Table 2.
Main errors in the placement of the I-gel laryngeal mask
| Not deep enough | |
| Overall | 19% |
| Isolated | 14% |
| And wrong direction | 1% |
| And wrong turn | 5% |
| Too deep | 2% |
The data are presented as percentages.
In total, 92 individuals (92%) reported experience with former BLS training, and 8 participants (8%) had not experienced any formal first aid training. The insertion time and realisation of the second ventilation was significantly reduced by former BLS training (19.6 s, 95% CI 17.8 to 21.5, p=0.0004), and the time from turning over the instruction chart until the second ventilation was 30.3±1.4 and 50±8 s for those with and without prior BLS training, respectively (figure 2). We also found a significant correlation between BLS experience and success (p=0.0096) (table 3). Moreover, the number of BLS courses the participants had participated in significantly correlated with the success of ventilation (p=0.005). Furthermore, no significant difference in the success of ventilation initiation related to participants with previous first aid training within the past 5 years (n=43) compared to those with first aid training more than 5 years ago (n=49) could be detected (p=0.42). BLS training less than or more than 5 years ago did not influence the duration or success of the procedure (achieving a second ventilation) (p=0.58).
Figure 2.
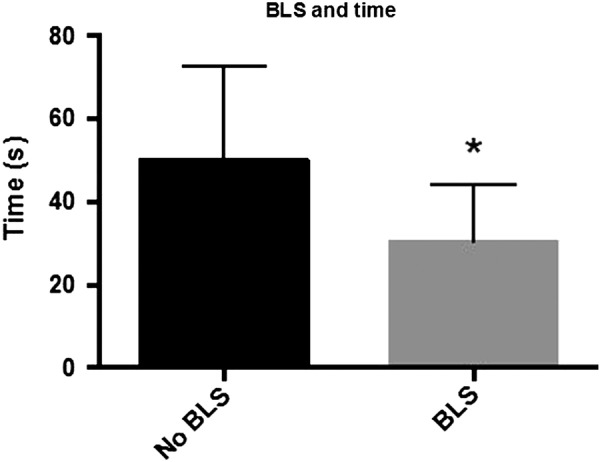
Previous basic life support (BLS) experience and insertion time. (BLS: n=92; No BLS: n=8). Time of insertion and realisation of the second ventilation was significantly reduced by previous BLS training (p=0.0004)*. The data are presented as the mean±SD.
Table 3.
Age, previous BLS experience and success of ventilation
| Success | No success | |
|---|---|---|
| Age<30 years | 55 | 11 |
| Age>30 years | 24 | 10 |
| BLS | 76* | 16 |
| No BLS | 3 | 5 |
BLS, basic life support.
*There was no significant difference between age (<30 years (n=66), >30 years (n=34)) and the success (p=0.1944 and p=0.1383) of ventilation. A significant difference in the rate of success between those with and without BLS experience (BLS: n=92; No BLS: n=8) was found (p=0.0096).
The data are the total numbers.
Focusing on the insertion time, a significant difference between participants aged >30 years (n=34, 41.1±3.4 s) compared with those aged <30 years (n=66, 27.2±1.2 s) was found (p=0.0001, 95% CI 8.03 to 19.7) (figure 3). There was no significant difference between the age groups (<30 years compared to >30 years) in relation to the success of the procedure (p=0.19 and p=0.14) (table 3). No sex-specific differences between the performances of male (n=67) and female (n=33) participants regarding insertion times (30.2±18 vs 35.3±2.9 s) (p=0.12) or success rates (p=0.80) were observed. Eighty-five per cent (n=85) of participants believed that their individual inhibition threshold for providing mouth-to-mouth ventilation during resuscitation was lowered using this modified laryngeal mask airway. A significant reduction in their reluctance to perform ventilation after the placement of the laryngeal mask was found relative to their feelings before the trial (p<0.0001) (figure 4).
Figure 3.
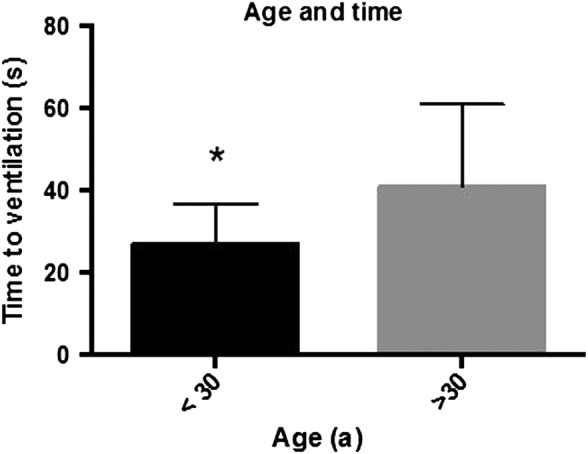
Age and time of insertion. Relating to the time of insertion, a significant difference between participants >30 years (n=34; 41.1±3.4 s) compared to those <30 years (n=66; 27.2±1.2 s) was found (p=0.0001*; 95% CI 8.03 to 19.7). The data are presented as the mean±SD.
Figure 4.
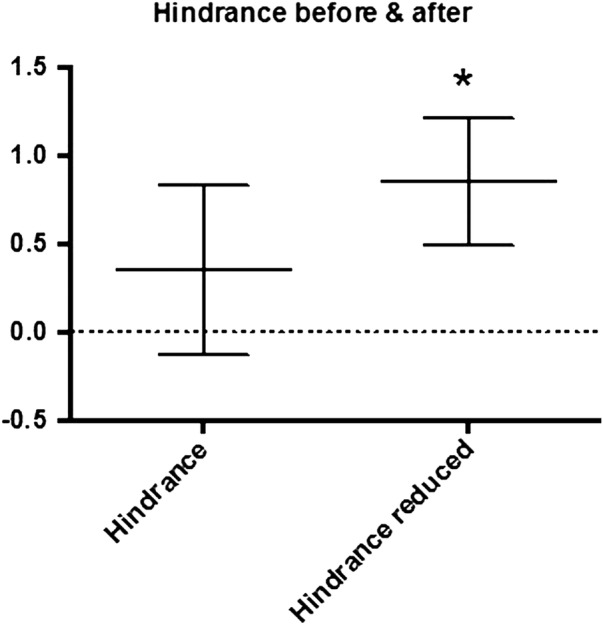
Hindrance before and after the experiment. A significant difference in participant hindrance before and after the placement of the laryngeal mask was observed (p<0.0001)*. The data are the mean±SD.
Discussion
In this pilot study, we showed that laypersons were able to successfully manage mouth-to-mask ventilation with a modified I-gel in a manikin using a simple instruction chart.
In the case of cardiac arrest, survival often depends on early resuscitation by laypersons.5–7 According to the latest ERC guidelines, ventilation is part of basic cardiac life support (BCLS), ideally with a 30:2 ratio between chest compressions and ventilations.17
Unlike other projects and investigations, our study was not based on prior instruction or training. Moreover, we investigated the performance of laypersons without any professional medical background. A majority of prior studies included so-called laypersons such as paramedical personnel, nurses, firemen and medical students.18 For laypersons, SADs might be ‘an excellent or even superior’ alternative to ventilation,16 with less risk of aspiration.13 In addition, prior studies have proven the laryngeal mask in general to be a SAD with high success rates when used by individuals with limited clinical experience.19
In comparison, cuff inflation is one of the major pitfalls in the application of SADs.2 18 For this reason, we chose the I-gel, a second generation SAD (which incorporates a gastric drainage channel) with an oval corpus providing more rotational stability. Compared to various other SADs, the I-gel is one of the fastest to insert and easiest to handle, with high success rates20 and lower gastric inflation.21 In addition, there is no need for the operator to inflate a cuffed seal. In particular, cuff inflation using a syringe was found to be a major issue for laypersons operating SADs, resulting in uncertainty and prolonging the time needed to install artificial ventilation.2 18 22
A previous trial proved the process of connecting bag valve mask (BMVs) and SADs to be a source of error. Squeezing the BMV was a second major issue identified in this context; however, understanding the origin of faults and the difficulties of operating professional devices by laypersons and transferring this new information into action finally resulted in success.22 Owing to these previous complications, we decided to exclude the BMV in this study and chose a simple filter-protected mouthpiece placed at the ISO connection site of the I-gel to facilitate ventilation, which is similar to the BLS class favoured and mouth-to-mouth ventilation that is taught. Hence, none of our participants failed to initiate mouth-to-SAD ventilation.
For educational purposes, a variety of alternative instruction methods using different types of media to deliver instructions on how to apply BCLS, such as brief training sessions,16 recruitment of volunteers through mobile phone positioning systems,23 video clip demonstrations24 and scripted telephone instruction,25 have been shown to be successful. It was our aim to evaluate an alternative educational concept that enables laypersons to successfully handle professional airway equipment, for example, a modified laryngeal mask, for emergency ventilation. Compared to previous trials, applicants needed similar time periods (31.9±15.4 s) to successfully place the devices.18 26 Nevertheless, the time to insert a device in a manikin may vary significantly from that required to insert it in a patient.27
As in cases of cardiac arrests, the early initiation of CPR by a layperson contributes to a better chance of survival.5–7 This trial, in addition to the already published and realised concept of performing only chest compressions, may be a move towards an improved acceptance of performing first aid by laypersons as a result of less reluctance in response to the call for bystander CPR.
Similar to previous studies, we found a significant correlation between BLS experience, success and insertion time. This study shows that BLS-experienced individuals placed the mask faster and more successfully than those without BLS experience. Moreover, the number of BLS courses that participants had participated in was significantly correlated with the success of ventilation.28 A prior study has shown that participants with prior knowledge were significantly more likely to be confident enough to render first aid.3
Nevertheless, we acknowledge some limitations that should be discussed. The correct positioning of the mask was found to be the most crucial problem in transferring information from the instruction chart into action. Two potential explanations have been mentioned earlier, for example, the inability of even high fidelity simulation manikins ‘to recreate the feel and finer aspects of human airway anatomy’27 and that despite lubrication, the friction between two artificial materials may demand more power than anticipated by the individuals.2 An idea for enhancing the instructions in this context would be, in addition to better labelling2 of the I-gel, the use of extra bold type on the instruction chart and verbal instructions to support correct placement.18 Another challenge for the subjects regarding the ventilation of the manikin was to distinguish whether their ventilation was successful or not. Fifteen (n=15) individuals believed they had successfully ventilated the manikin, even though they had failed. In our manikin, the individuals could directly see the lungs, and it was obvious if they lifted up or not. In actual humans, it is even more difficult to determine if the lungs are ventilated as the upper part of the chest and body may also lift in the case of stomach ventilation. Moreover, whether this rate of misapprehension would be better in mouth-to-mouth ventilation remains unknown.
Ideas for steps that could follow this study include a reassessment after a comparison of mouth-to-mouth ventilation to the use of BVMV and the I-gel laryngeal mask and a comparison of different ways for teaching their application through videos, charts or just verbal instructions.
Hence, the next logical step would be to test the modified I-gel laryngeal mask on humans under anaesthesia and in real-life situations.
Conclusion
In this study, 79 (79%) of the participating laypersons were able to place the labelled I-gel laryngeal mask and to successfully initiate mouth-to-laryngeal mask ventilation in the manikin by following a newly designed instruction chart. When transferring the instructions into action, placing the mask deep enough and identifying whether the manikin was successfully ventilated emerged as the main barriers to the use of this device. Extra bold type on the instruction chart, verbal support18 and better labelling2 of the I-gel laryngeal mask may have improved the performance of the participants. The significant reduction in the reluctance of laypersons towards the implementation of BLS by placing the I-gel laryngeal mask may support a better acceptance of bystander resuscitation in laypersons. The results of this study support the introduction of SADs in BLS courses.
Footnotes
Contributors: GS, L-TB and AR conceived the study and drafted the manuscript. L-TB, NZ and CS performed the experiments and data acquisition. GS and L-TB analysed the data obtained together with AR. RR and MC supervised the statistical analysis and revised the manuscript. AR supervised the trial. All authors revised and approved the final version.
Funding: The trial was funded by departmental funding.
Competing interests: None declared.
Ethics approval: RWTH Aachen University Ethical Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: No additional data are available.
References
- 1.Alexander R, Hodgson P, Lomax D et al. A comparison of the laryngeal mask airway and Guedel airway, bag and facemask for manual ventilation following formal training. Anaesthesia 1993;48:231–4. doi:10.1111/j.1365-2044.1993.tb06909.x [DOI] [PubMed] [Google Scholar]
- 2.Schälte G, Stoppe C, Rossaint R et al. Does a 4 diagram manual enable laypersons to operate the Laryngeal Mask Supreme®? A pilot study in the manikin. Scand J Trauma Resusc Emerg Med 2012;20:21 doi:10.1186/1757-7241-20-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wiese CH, Wilke H, Bahr J et al. ‘Obligatory first aid courses’. Notfall+Rettungsmedizin 2008;11:482–6. doi:10.1007/s10049-008-1080-2 [Google Scholar]
- 4.‘International first aid and resuscitation guidelines 2011’ http://www.ifrc.org
- 5.Baubin M. Bystander resuscitation without mouth-to-mouth ventilation? Anaesthesist 2007;56:897–8. doi:10.1007/s00101-007-1245-2 [Google Scholar]
- 6.Hasselqvist-Ax I, Riva G, Herlitz J et al. Early cardiopulmonary resuscitation in out-of-hospital cardiac arrest. N Engl J Med 2015;372:2307–15. doi:10.1056/NEJMoa1405796 [DOI] [PubMed] [Google Scholar]
- 7.Herlitz J, Engdahl J, Svensson L et al. Factors associated with an increased chance of survival among patients suffering from an out-of-hospital cardiac arrest in a national perspective in Sweden. Am Heart J 2005;149:61–6. doi:10.1016/j.ahj.2004.07.014 [DOI] [PubMed] [Google Scholar]
- 8.Deakin CD, Nolan JP, Soar J et al. Erweiterte Reanimationsmaßnahmen für Erwachsene (‘‘dvanced life support”). Notfall+Rettungsmedizin 2010;13:559–620. doi:101007/s10049-010-1370-3 [Google Scholar]
- 9.Wenzel V, Lindner KH, Prengel AW. [Ventilation during cardiopulmonary resuscitation (CPR). A literature study and analysis of ventilation strategies]. Anaesthesist 1997;46:133–41. [DOI] [PubMed] [Google Scholar]
- 10.Piepho T, Thierbach A, Werner C. Supraglottic airway devices in emergency medicine. Notfall+Rettungsmedizin 2005;8:123–8. doi:1010.1007/s10049-004-0712-4 [Google Scholar]
- 11.Wiese CH, Semmel T, Müller JU et al. The use of the laryngeal tube disposable (LT-D) by paramedics during out-of-hospital resuscitation—an observational study concerning ERC guidelines 2005. Resuscitation 2009;80:194–8. doi:10.1016/j.resuscitation.2008.08.023 [DOI] [PubMed] [Google Scholar]
- 12.Gatward JJ, Thomas MJC, Nolan JP et al. Effect of chest compressions on the time taken to insert airway devices in a manikin. Br J Anaesth 2008;100:351–6. doi:10.1093/bja/aem364 [DOI] [PubMed] [Google Scholar]
- 13.Stone BJ, Chantler PJ, Baskett PJ. The incidence of regurgitation during cardiopulmonary resuscitation: a comparison between the bag valve mask and laryngeal mask airway. Resuscitation 1998;38:3–6. doi:10.1016/S0300-9572(98)00068-9 [DOI] [PubMed] [Google Scholar]
- 14.Intersurgical Userguide: i-gel single use supraglottic airway, Adult and paediatric sizes”, 2013. http://www.igel.com
- 15.Castle N, Owen R, Hann M et al. Assessment of the speed and ease of insertion of three supraglottic airway devices by paramedics: a manikin study. Emerg Med J 2010;27:860–3. doi:10.1136/emj.2009.084343 [DOI] [PubMed] [Google Scholar]
- 16.Schälte G, Stoppe C, Aktas M et al. Laypersons can successfully place supraglottic airways with 3 minutes of training. A comparison of four different devices in the manikin. Scand J Trauma Resusc Emerg Med 2011;19:60 doi:10.1186/1757-7241-19-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koster RW, Baubin MA, Bossaert LL et al. Basismaßnahmen zur Wiederbelebung Erwachsener und Verwendung automatisierter externer Defibrillatoren. Notfall+Rettungsmedizin 2010;13:523–42. doi:10.1007/s10049-010-1368-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurola J, Paakkonen H, Kettunen T et al. Feasibility of written instructions in airway management training of laryngeal tube. Scand J Trauma Resusc Emerg Med 2011;19:56 doi:10.1186/1757-7241-19-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Timmermann A, Cremer S, Heuer J et al. [Laryngeal mask LMA Supreme. Application by medical personnel inexperienced in airway management]. Anaesthesist 2008;57:970–5. doi:10.1007/s00101-008-1425-8 [DOI] [PubMed] [Google Scholar]
- 20.Jackson KM, Cook TM. Evaluation of four airway training manikins as patient simulators for the insertion of eight types of supraglottic airway devices. Anaesthesia 2007;62:388–93. doi:10.1111/j.1365-2044.2007.04983.x [DOI] [PubMed] [Google Scholar]
- 21.Fischer H, Hochbrugger E, Fast A et al. Performance of supraglottic airway devices and 12 month skill retention: a randomized controlled study with manikins. Resuscitation 2011;82:326–31. doi:10.1016/j.resuscitation.2010.11.014 [DOI] [PubMed] [Google Scholar]
- 22.Schälte G. Following on-site instructions for operating laryngeal mask supreme™ and laryngeal tube™ as an alternative to mouth-to-mouth ventilation in layperson CPR: a randomized trial in the manikin. J Anesthe Clinic Res 2012;3:1–7. doi:10.4172/2155-6148.1000265 [Google Scholar]
- 23.Ringh M, Rosenqvist M, Hollenberg J et al. Mobile-phone dispatch of laypersons for CPR in out-of-hospital cardiac arrest. N Engl J Med 2015;372:2316–25. doi:10.1056/NEJMoa1406038 [DOI] [PubMed] [Google Scholar]
- 24.Jokela J, Nurmi J, Genzwuerker HV et al. Laryngeal tube and intubating laryngeal mask insertion in a manikin by first-responder trainees after a short video-clip demonstration. Prehosp Disaster Med 2009;24:63–6. [DOI] [PubMed] [Google Scholar]
- 25.Beauchamp G, Phrampus P, Guyette FX. Simulated rescue airway use by laypersons with scripted telephonic instruction. Resuscitation 2009;80:925–9. doi:10.1016/j.resuscitation.2009.04.030 [DOI] [PubMed] [Google Scholar]
- 26.Howes BW, Wharton NM, Gibbison B et al. LMA SupremeTM insertion by novices in manikins and patients. Anaesthesia 2010;65:343–7. doi:10.1111/j.1365-2044.2010.06262.x [DOI] [PubMed] [Google Scholar]
- 27.Cook TM, Howes B, Wharton N. Evaluation of airway equipment: man or manikin? Anaesthesia 2011;66:529 doi:10.1111/j.1365-2044.2011.06726.x [DOI] [PubMed] [Google Scholar]
- 28.Wiese CH, Bartels U, Bahr J et al. Obligatory first aid courses. Notfall+Rettungsmedizin 2006;9:597–603. doi:10.1007/s10049-006-0852-9 [Google Scholar]