Abstract
Background:
Although we have seen tremendous advancement in microsurgery over the last 2 decades and free tissue transfer has become standard for head and neck reconstruction, surgeons still struggle to prevent postoperative complications. We examined the relationship between body mass index (BMI) and postoperative complications in patients undergoing rectus abdominis free flap transfer after anterolateral craniofacial resection.
Methods:
This was a retrospective review of reconstructive surgery using rectus abdominis musculocutaneous free flap in patients with locally advanced maxillary sinus carcinoma from 2003 to 2014 (n = 35, 27 men and 8 women; average age, 60.9 ± 7.8 years). All patients underwent craniofacial reconstruction after anterior and middle cranial fossa skull base resection and maxillectomy (class IV, subtype a) with palatal resection. Patients were categorized based on sex, BMI, and other parameters.
Results:
Recipient-site infection occurred in 11 patients (31.4%), cerebrospinal fluid leakage in 6 (17.1%), partial flap necrosis in 2 (5.7%), total flap necrosis in 1 (2.9%), and facial fistula in 4 (11.4%). Women showed partial flap necrosis significantly more frequently (P = 0.047), probably owing to poor vascular supply of the subcutaneous fat layer. Patients with low BMI (<20 kg/m2) showed recipient-site infection (P = 0.02) and facial fistula (P = 0.01) significantly more frequently owing to insufficient tissue volume and poor vascular supply.
Conclusion:
Postoperative recipient-site infection and facial fistula occurred mainly in low-BMI patients. Surgeons should take care to achieve sufficient donor tissue on low-BMI patients. Using a prosthetic obturator in low-BMI patients for craniofacial reconstruction can be a good alternative option to reduce postoperative complications due to insufficient donor tissue volume.
Craniofacial reconstruction has undergone significant advancement during the past 2 decades, after technical improvements in microsurgery that have increased the options available regarding the type of flap used, such as rectus abdominis, latissimus, radial forearm, fibular, and anterolateral thigh flaps, for closure of complex skull-base defects.1–6 Although the use of a free flap has become standard for head and neck reconstruction, surgeons are still challenged to achieve better surgical outcomes without complications. Wide en bloc resection and craniofacial reconstruction using a free flap is the mainstay of maxillary sinus carcinoma treatment.7 Maxillary sinus carcinoma often invades the surrounding tissue including the orbit, nasal cavity, hard palate, and cranial base.8 It is necessary to reconstruct the barrier between the cranial base and nasal and/or oral cavity to protect the central nervous system and to restore the facial contour aesthetically, which requires a large amount of soft tissue. Rectus abdominis musculocutaneous flap is preferred to reconstruct the oncologic resected defect because it has well-vascularized tissue and makes voluminous tissue transfer possible.9,10 And also, rectus abdominis musculocutaneous free flap does not require intraoperative position change, which can shorten the operative time to reduce postoperative complication rate. However, it is difficult to harvest enough tissue volume from the patient’s abdomen to fill up the oncologic resected region. This may account for the dead space on the recipient site causing postoperative complications. Here, we describe the relationship between postoperative complications and body mass index (BMI) in patients who underwent craniofacial reconstruction with a rectus abdominis musculocutaneous free flap after the anterolateral craniofacial tumor resection.
METHODS
Characteristics
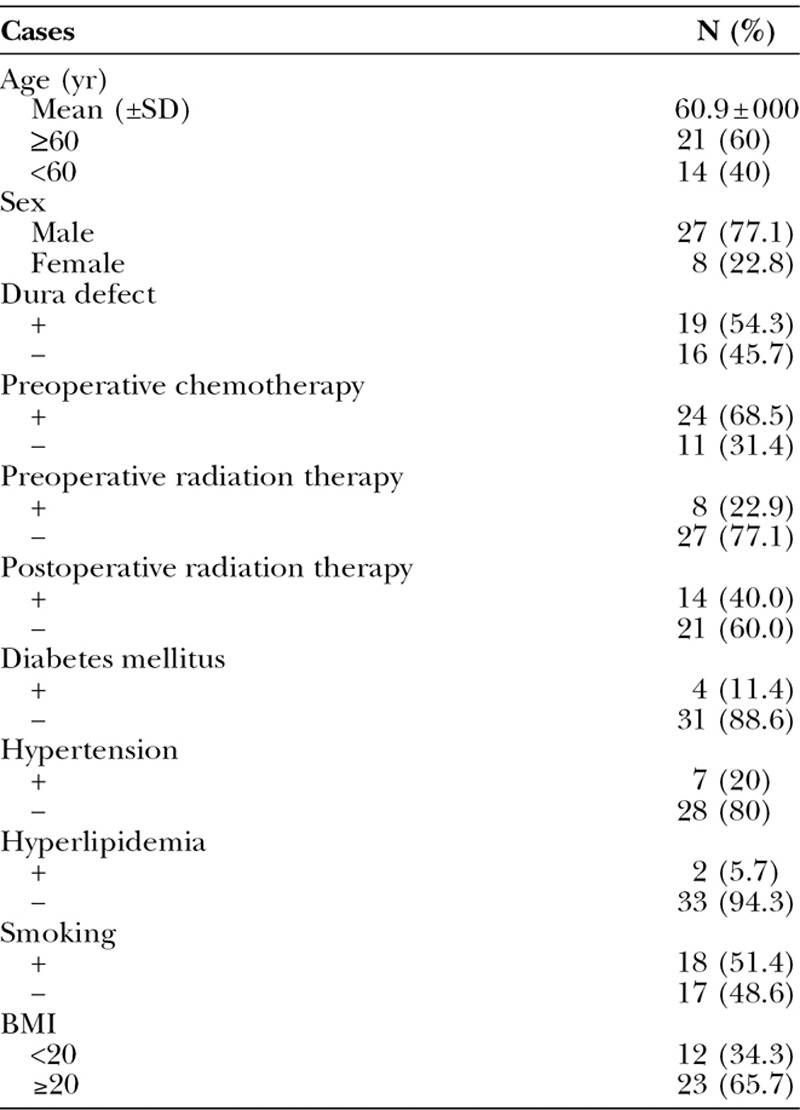
The study included 35 patients (27 men and 8 women; average age, 60.9 ± 7.8 years) with locally advanced maxillary sinus carcinoma with tumor size T3 and T4 who underwent anterolateral craniofacial resection and reconstruction using a free rectus abdominis musculocutaneous flap between 2003 and 2014. We used the International Union against Cancer seventh edition criteria for TNM stage classification. We retrospectively analyzed the relationship between the patient’s preoperative BMI and postoperative complications including recipient-site infection, cerebrospinal fluid leakage, partial flap necrosis, total flap necrosis, and facial fistula. Facial fistula mainly occurs around the medial canthus (Fig. 1). Additionally, we analyzed the relationship between the patient’s baseline status (age; sex; preoperative chemotherapy and/or radiation therapy; and presence of an intraoperative dura defect, diabetes mellitus, hypertension, and hyperlipidemia) and postoperative complications. All complications were estimated during the follow-up after the operations. Average follow-up was 38.6 months.
Fig. 1.

Facial fistula is one of the postoperative complications that can occur after anterolateral craniofacial resection using a free rectus abdominis musculocutaneous flap. This facial fistula occurred around medial canthus (arrow).
Regarding T classification, 24 patients were classified as T4a, 9 patients were T4b, and 2 patients were T3. Regarding N classification, 31 patients were classified as N0, 2 patients were N1, and 2 patients were N2. All patients were classified as M0. The historical diagnoses were as follows: squamous cell carcinoma in 29 patients, adenocarcinoma in 2 patients, adenoid cystic carcinoma in 1 patient, myoepithelial carcinoma in 1 patient, and undifferentiated carcinoma in 2 patients. Twenty-four patients received preoperative chemotherapy; 8 patients received preoperative radiotherapy with an average dose of 44 (range, 22–66) Gy, and 14 patients received postoperative radiotherapy with an average dose of 51 (range, 20–70) Gy. Four patients had diabetes mellitus; 7 patients had hypertension; 2 patients had hyperlipidemia, and 16 patients were smoking. Each patient’s body weight and height were estimated within 7 days before the operation. The average body weight was 60.9 ± 8.52 kg; average height was 163.7 ± 8.43 cm, and average BMI was 21.1 ± 2.51 kg/m2. We categorized patients with BMI <20 kg/m2 into the low-BMI group (n = 12) and others into a control group (n = 23; Table 1). To make it simple, we named BMI ≥20 as high-BMI group and BMI <20 as low-BMI group. Our grouping on BMI may different from the conservative definition of high and low BMI.
Table 1.
Characteristics of Cases
Surgical Procedure
Head and neck surgeons performed neck dissections when lymphatic metastases were suspected. Tumor was resected using en bloc craniofacial resection with a Weber-Ferguson incision and an anterolateral craniofacial approach.7 Tensor fasciae latae was used for the dura defect when direct suturing was impossible. Plastic surgeons reconstructed the oncologic resected defect using a free rectus abdominis musculocutaneous flap. The part of the flap lateral to the umbilical was used to reconstruct the hard palate. One lobe was used to reconstruct the nasal cavity, and the other was used to reconstruct the facial skin. The rectus abdominis muscle was used to cover the cranial base defect. Subcutaneous tissue of the flap was used to fill the oncologic resected region. Flap pedicle was run through the parapharyngeal space, and microanastomosis was performed. Negative drainage was placed under cheek and head after completing the orientation of the free flap (Fig. 2).
Fig. 2.
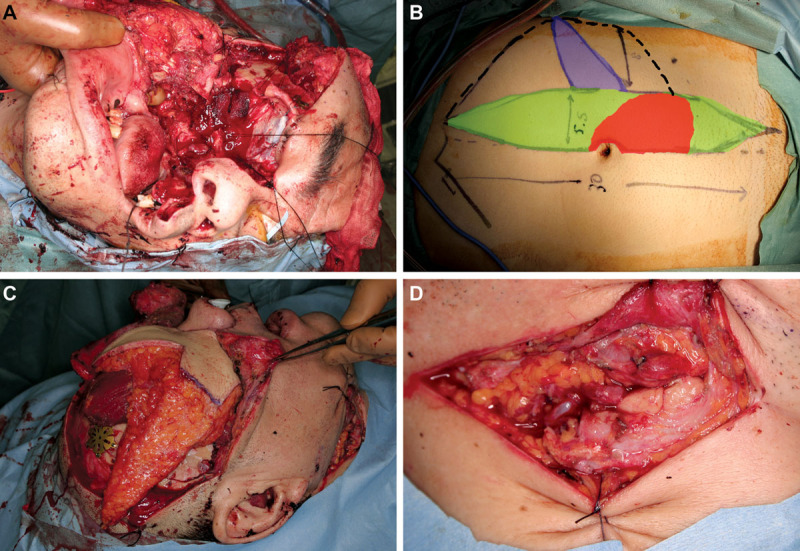
A, Representative intraoperative photograph after resection of the maxillary sinus carcinoma. The defect includes cranial base, hard palate, and maxillary bone. B, Rectus abdominis musculocutaneous flap design. The tissue around the umbilical area was used to reconstruct the hard palate (red). One part of the flap was used to reconstruct the nasal cavity (blue). The deepithelialized part of the flap (green) and surrounding subcutaneous tissue (dotted line) were used to fill the oncologic resected region. C, Representative intraoperative photograph after flap fixation to the defect. The muscle belly of the rectus abdominis was used to cover the cranial base. D, The flap pedicle was run through the parapharyngeal space, and microanastomosis was performed under the microscope.
Statistical Analysis
Descriptive statistics were calculated for each of the 2 groups. Fisher exact test or the χ2 test was used to evaluate the relationship between categorical variables and complications. Two-sided P values <0.05 were considered statistically significant for all statistical tests. Stat Flex version 6 (Artec Co. Ltd., Osaka, Japan) was used for all statistical analyses.
RESULTS
For all 35 patients, the average operation time was 15.0 ± 3.13 hours, and the average volume of intraoperative bleeding was 1731 ± 1188 mL. Among 19 patients with a dura defect, the defect was closed directly in 12 patients, a fascia graft of the temporal muscle was used in 4 patients, and the tensor fasciae latae was used in 3 patients.
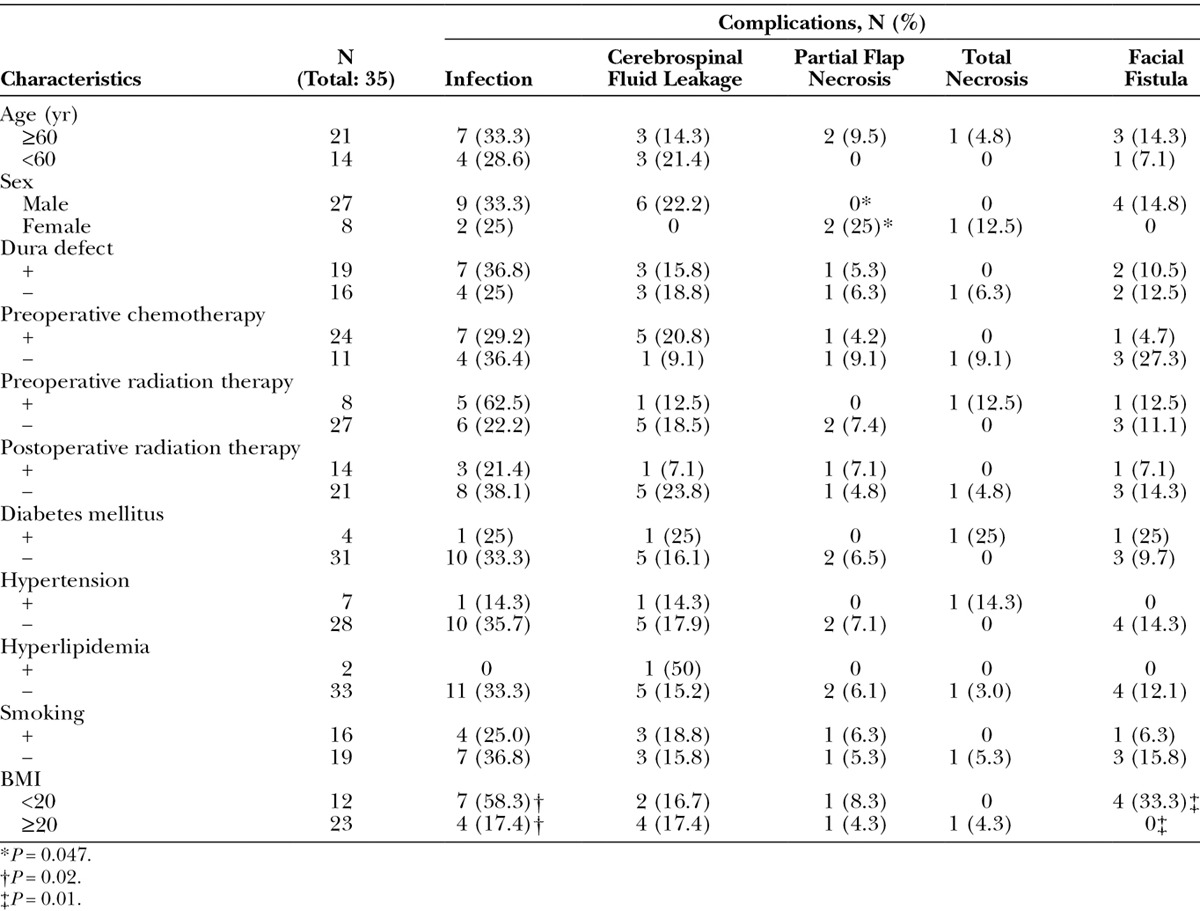
Postoperative complications occurred in 24 patients (68.6%): recipient-site infection in 11 (31.4%), cerebrospinal fluid leakage in 6 (17.1%), partial flap necrosis in 2 (5.7%), total flap necrosis in 1 (2.9%), and facial fistula in 4 (11.4%). Partial flap necrosis (P = 0.047) showed significant differences between male and female. And also, recipient-site infection (P = 0.02) and facial fistula (P = 0.01) showed statistically meaningful differences between low-BMI patients (BMI < 20 kg/m2) and high-BMI patients (BMI ≥ 20 kg/m2). However, no significant differences were found on other confounding factors such as age, preoperative chemotherapy, preoperative radiation therapy, postoperative radiation therapy, the presence of a dura defect, diabetes mellitus, hypertension, hyperlipidemia, and smoking (Table 2).
Table 2.
Complications in Each Characteristic
DISCUSSION
Malignant nasal cavity and paranasal sinus tumors account for only 3% of all head and neck cancer cases.11 Moreover, nasal cavity and paranasal sinus tumors often infiltrate into surrounding tissues before they are diagnosed because there are few symptoms of the tumor itself. It is necessary to resect the tumor with wide en bloc resection with a free margin including the orbit, nasal cavity, hard palate, facial skin, and skull base to completely cure the cancer.12 Saito et al13 described surgical procedures that achieve en bloc resection for malignant tumors of the skull base even when the tumor is impinging on the orbital apex, anterior and middle cranial fossa, and dura mater.
After tumor resection, reconstructive surgeons need to pay attention to functional and aesthetic issues. The aims of craniofacial reconstructive surgery are protecting the central nervous system from life-threatening infection, restoring the facial contour, and reconstructing the palate for mastication and speech function. We selected the rectus abdominis musculocutaneous flap to harvest voluminous tissue because it contains wide cutaneous tissue, thick subcutaneous tissue, and a wide muscle belly sufficient to cover the defect. Craniofacial resection and reconstructive surgery generally entail a long operative time, considerable blood loss, transfusion, and use of a free flap, which are common risk factors of postoperative complications.14 In our cases, the average operation time was 15 hours, average blood loss was 1.731 mL, all patients received blood transfusion, and a free flap was used for reconstruction. Patients with nasal cavity and paranasal sinus carcinoma are at high risk for postoperative complications and require special attention from reconstructive surgeons to prevent such complications.
Obesity is one of the general risk factors for postoperative complications due to surgical difficulties, altered wound physiology, and impaired immune responses.14 Although high BMI places patients at increased risk for postoperative complications in general, the low-BMI patients showed significantly more complications after craniofacial reconstruction in this study. Four of 12 low-BMI (BMI < 20 kg/m2) patients had postoperative facial cutaneous fistula, but there were none in 23 high-BMI patients (BMI ≥ 20 kg/m2; P = 0.01). In addition, 7 of 12 low-BMI patients had postoperative inflammation at the recipient site but only 4 of 23 high-BMI patients had recipient-site inflammation (P = 0.047).
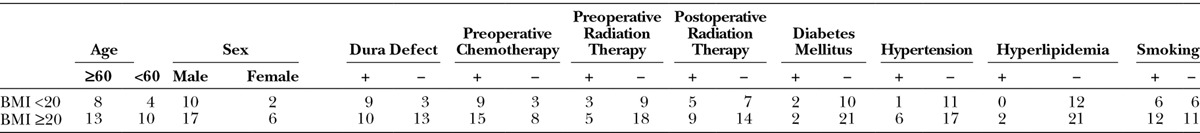
After stratification by BMI, considerable homogeneity was observed in the study population regarding age, medical comorbidities, preoperative chemotherapy and radiation therapy, intraoperative dura defects, postoperative radiation therapy, and smoking (Table 3). Although we did not measure the volume of flap tissue itself, we inferred that low-BMI patients had low tissue volume at the donor site.
Table 3.
Relationship between BMI and Other Confounding Factors
In our study, partial necrosis occurred in 2 female patients: 1 had a BMI of 22.73 kg/m2 and the other patient had a BMI of 19.83 kg/m2. Although these were statistically meaningful data in our study, we could not analyze further because of the small number of patients. A larger rigorous study may be required to find the relationship between sex and postoperative complications in craniofacial reconstruction.
For craniofacial reconstruction, we first reconstructed the skull base using muscle belly of the rectus abdominis musculocutaneous flap. Next, we proceeded to restore the facial contour by filling the oncologic resected region and reconstruct the palate for mastication and speech function. In low-BMI patients, it is difficult to harvest sufficient tissue volume to fill the tumor resected region without creating dead space that may cause inflammation at the recipient site postoperatively. Insufficient flap volume leads not only to infection but also to facial fistula. We supposed that the blood supply of the medial canthus is unstable when a Weber-Ferguson incision is used. Thus, it is necessary to lay well-vascularized soft tissue under the medial canthus skin.
For preventing facial fistula and recipient-site inflammation in low-BMI patients, using a prosthetic palatal obturator is recommended to save tissue volume for filling dead space in the oncologic resected region instead of using a free flap to reconstruct the hard palate. Although a prosthetic palatal obturator has some disadvantages, such as nasal leakage, cleaning, and constant prosthetic refinement, it also has advantages that lower postoperative complications, such as shortening the operative time and hospital stay and complete visualization of the maxillectomy cavity, which makes it easier to check for tumor recurrence. Furthermore, the use of a palatal obturator seemed to make no significant difference in health-related quality of life, according to a study by Rogers et al.14,15
CONCLUSIONS
For low-BMI patients undergoing craniofacial reconstruction, a preoperative imaging study is recommended to calculate the rectus abdominis musculocutaneous free flap tissue volume and estimate the volume of the oncologic defect. If harvesting enough tissue volume from the donor site is difficult, a prosthetic palatal obturator is recommended instead of performing the free flap reconstruction with insufficient tissue. According to our study, craniofacial reconstruction with insufficient tissue volume is a risk factor for postoperative complications in low-BMI patients, and the prosthetic obturator is a good alternative to free flap reconstruction for maxillectomy patients. Conserving tissue volume for filling the oncologic defect is not the only advantage of using a prosthetic obturator, as it will also shorten the operative time, which in itself lowers the postoperative complication rate.
PATIENT CONSENT
Patients provided written consent for the use of their images.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Califano J, Cordeiro PG, Disa JJ, et al. Anterior cranial base reconstruction using free tissue transfer: changing trends. Head Neck. 2003;25:89–96. doi: 10.1002/hed.10179. [DOI] [PubMed] [Google Scholar]
- 2.Chang DW, Langstein HN, Gupta A, et al. Reconstructive management of cranial base defects after tumor ablation. Plast Reconstr Surg. 2001;107:1346–1355; discussion 1356. doi: 10.1097/00006534-200105000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Chiu ES, Kraus D, Bui DT, et al. Anterior and middle cranial fossa skull base reconstruction using microvascular free tissue techniques: surgical complications and functional outcomes. Ann Plast Surg. 2008;60:514–520. doi: 10.1097/SAP.0b013e3181715707. [DOI] [PubMed] [Google Scholar]
- 4.Holom GH, Seland H, Strandenes E, et al. Head and neck reconstruction using microsurgery: a 9-year retrospective study. Eur Arch Otorhinolaryngol. 2013;270:2737–2743. doi: 10.1007/s00405-013-2390-7. [DOI] [PubMed] [Google Scholar]
- 5.Neligan PC. Head and neck reconstruction. Plast Reconstr Surg. 2013;131:260e–269e. doi: 10.1097/PRS.0b013e3182778938. [DOI] [PubMed] [Google Scholar]
- 6.Yamada A, Harii K, Ueda K, et al. Free rectus abdominis muscle reconstruction of the anterior skull base. Br J Plast Surg. 1992;45:302–306. doi: 10.1016/0007-1226(92)90057-5. [DOI] [PubMed] [Google Scholar]
- 7.Nishio N, Fujimoto Y, Fujii M, et al. Craniofacial resection for T4 maxillary sinus carcinoma: managing cases with involvement of the skull base. Otolaryngol Head Neck Surg. 2015;153:231–238. doi: 10.1177/0194599815586770. [DOI] [PubMed] [Google Scholar]
- 8.Banuchi V, Mallen J, Kraus D. Cancers of the nose, sinus, and skull base. Surg Oncol Clin N Am. 2015;24:563–577. doi: 10.1016/j.soc.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 9.Nishimoto S, Kakibuchi M, Hosokawa K, et al. Free rectus abdominis musculocutaneous flap for head and neck reconstruction. J Reconstr Microsurg. 1997;13:171–175. doi: 10.1055/s-2007-1006401. [DOI] [PubMed] [Google Scholar]
- 10.Cappiello J, Piazza C, Taglietti V, et al. Deep inferior epigastric artery perforated rectus abdominis free flap for head and neck reconstruction. Eur Arch Otorhinolaryngol. 2012;269:1219–1224. doi: 10.1007/s00405-011-1749-x. [DOI] [PubMed] [Google Scholar]
- 11.Silverberg E, Grant RN. Cancer statistics, 1970. CA Cancer J Clin. 1970;20:11–23. [PubMed] [Google Scholar]
- 12.Dulguerov P, Jacobsen MS, Allal AS, et al. Nasal and paranasal sinus carcinoma: are we making progress? A series of 220 patients and a systematic review. Cancer. 2001;92:3012–3029. doi: 10.1002/1097-0142(20011215)92:12<3012::aid-cncr10131>3.0.co;2-e. [DOI] [PubMed] [Google Scholar]
- 13.Saito K, Fukuta K, Takahashi M, et al. Management of the cavernous sinus in en bloc resections of malignant skull base tumors. Head Neck. 1999;21:734–742. doi: 10.1002/(sici)1097-0347(199912)21:8<734::aid-hed9>3.3.co;2-o. [DOI] [PubMed] [Google Scholar]
- 14.Sakai A, Okami K, Onuki J, et al. Statistical analysis of post-operative complications after head and neck surgery. Tokai J Exp Clin Med. 2008;33:105–109. [PubMed] [Google Scholar]
- 15.Rogers SN, Lowe D, McNally D, et al. Health-related quality of life after maxillectomy: a comparison between prosthetic obturation and free flap. J Oral Maxillofac Surg. 2003;61:174–181. doi: 10.1053/joms.2003.50044. [DOI] [PubMed] [Google Scholar]


