Summary:
Ulnar neuropathy is caused by compression of the ulnar nerve in the upper extremity, frequently occurring at the level of the elbow or wrist. Rarely, ulnar nerve entrapment may be seen proximal to the elbow. This report details a case of ulnar neuropathy diagnosed and localized to the arcade of Struthers with electromyography (EMG) and ultrasound (US) imaging and confirmed at time of operative release. US imaging and EMG findings were used to preoperatively localize the level of compression in a patient presenting with left ulnar neuropathy. In this case, ulnar entrapment 8 cm proximal to the medial epicondyle was diagnosed. Surgical release was performed and verified the level of entrapment at the arcade of Struthers in the upper arm. Alleviation of symptoms was noted at 8-week follow-up; no complications occurred. US imaging can be used in complement with EMG studies to properly diagnose and localize the level of ulnar nerve entrapment. This facilitates full release of the nerve and may prevent the need for revision surgery.
Symptoms of ulnar neuropathy are paresthesias of the ring and small digits and weakness of ulnar innervated muscles of the hand.1 Common sites for ulnar nerve entrapment include the cubital tunnel and Guyon canal at the elbow and wrist, respectively; the arcade of Struthers is not a common site for compression.2,3 This thin aponeurotic band extends from the medial head of the triceps to the intermuscular septum, approximately 8 cm proximal to the medial epicondyle. In 70–80% of individuals, the ulnar nerve passes under the arcade.
Although electromyography (EMG) demonstrates abnormal nerve conduction, ultrasound (US) imaging can demonstrate swelling adjacent to compression sites.4 Herein, we describe a patient with ulnar neuropathy localized preoperatively to the arcade of Struthers by US imaging and EMG.
CASE REPORT
A 34-year-old white man presented with paresthesias in the left 4th and 5th digits beginning 3–4 months prior with no inciting trauma. He reported left forearm numbness but denied neck pain. He noted weakness in his left hand and dropping objects. Medical history was significant for hepatitis C, left shoulder dislocation, anxiety, and depression. He actively smoked and had prior intravenous drug use. Now disabled, he had worked as a bricklayer. Family history included type 2 diabetes.
On examination, atrophy was noted in the left abductor digiti minimi (ADM) and first dorsal interossei (FDI). He had 2/5 intrinsic strength with clawing of the ring and small finger. Sensation was absent in the ulnar distribution with 2-point discrimination >10 mm with positive Tinel sign at the elbow.
EMGs were performed 3–4 months after appearance of symptoms. Left ulnar sensory nerve action potentials were unobtainable in ring and small finger; the left dorsal ulnar cutaneous response was diminished. Left ulnar compound muscle action potentials (CMAPs) recording the ADM were normal with stimulation 4 cm below and 4 cm above the elbow. CMAPs on the left FDI showed low amplitude at each stimulation site. Conduction velocities on both the ADM and FDI were normal. Concentric needle EMG of the left arm revealed fibrillation potentials in the left FDI, left ADM, and the left flexor carpi ulnaris (FCU). No motor units were seen in the FDI and FCU; 1 single firing unit was seen in the ADM.
US imaging was utilized to evaluate the left ulnar nerve. The nerve was visualized with normal shape and contour below the FCU. When traced proximally, it went from a circumferential area of 4.98 mm2 to an enlargement of 8.07 mm2 at the sulcus. At 8 cm proximal to the left medial epicondyle, the left ulnar nerve had a maximal diameter of 14.89 mm2 with evidence of fascial thickening (Fig. 1). CMAPs were then performed proximal to 8 cm above the medial epicondyle. No CMAP was recorded in the left FDI or ADM. EMG and US imaging localized a left ulnar entrapment 8 cm proximal to the medial epicondyle.
Fig. 1.
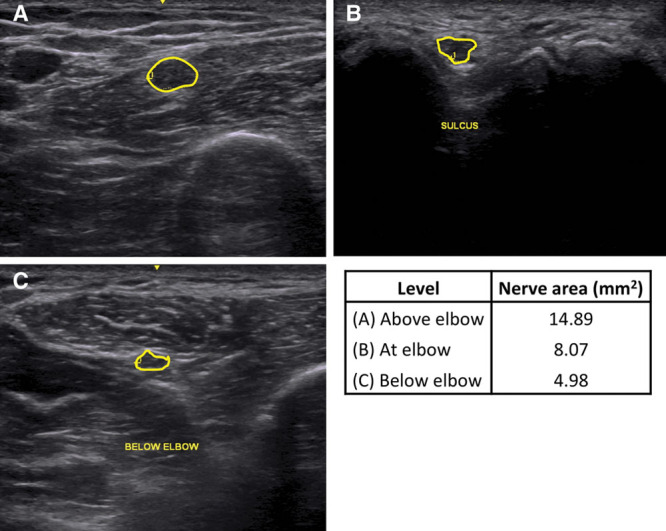
US evaluation of the ulnar nerve: (A) 8 cm proximal to the medial epicondyle, (B) at the elbow between the olecranon and the medial epicondyle, and (C) in the forearm between the 2 heads of the FCU. Yellow outlines denote the location of the nerve in each US image.
Decompression was recommended based on clinical examination and EMG/US imaging. A 25-cm curvilinear incision was made posterior to the medial epicondyle (15 cm proximal, 10 cm distal). Deep to the brachial fascia laid the ulnar nerve, just superficial to medial intermuscular septum. Dissection was then carried proximally along the nerve, liberating it from beneath the brachial fascia. A point was noted 8 cm proximal to the medial epicondyle, in which the ulnar nerve pierced the intermuscular septum. Immediately adjacent to this point, the arcade of Struthers was seen constricting the nerve. This band was released, decompressing the nerve (Figs. 2 and 3). An indentation of the nerve and swelling adjacent to this point were present. The nerve was then traced proximally for a few more centimeters to ensure that there were no other sites of compression. The nerve was then decompressed distal to the arcade of Struthers, through the cubital tunnel, releasing Osborne ligament posterior to the medial epicondyle. Distally, the superficial and deep fascial systems of the 2 heads of the FCU muscle were then released, completing the nerve decompression. Further release did not reveal other areas of compression.
Fig. 2.
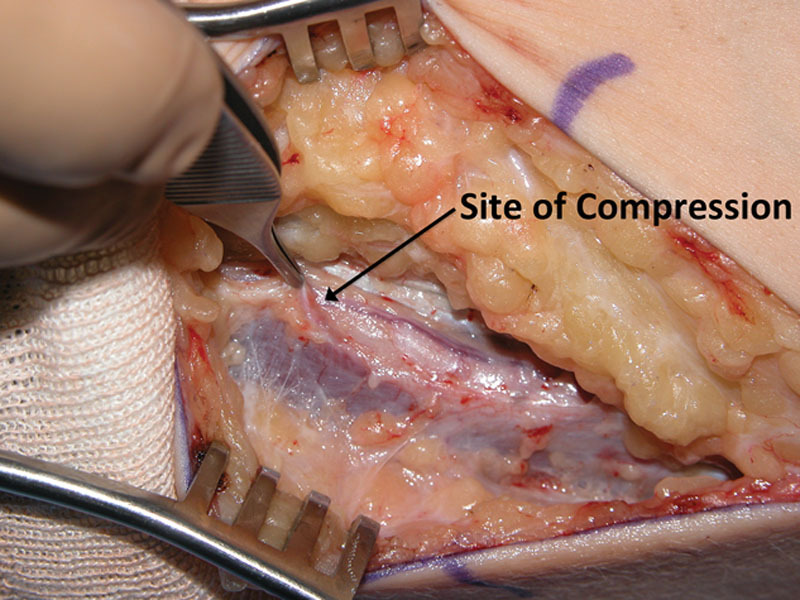
Intraoperative view of the ulnar nerve before release of the arcade of Struthers.
Fig. 3.
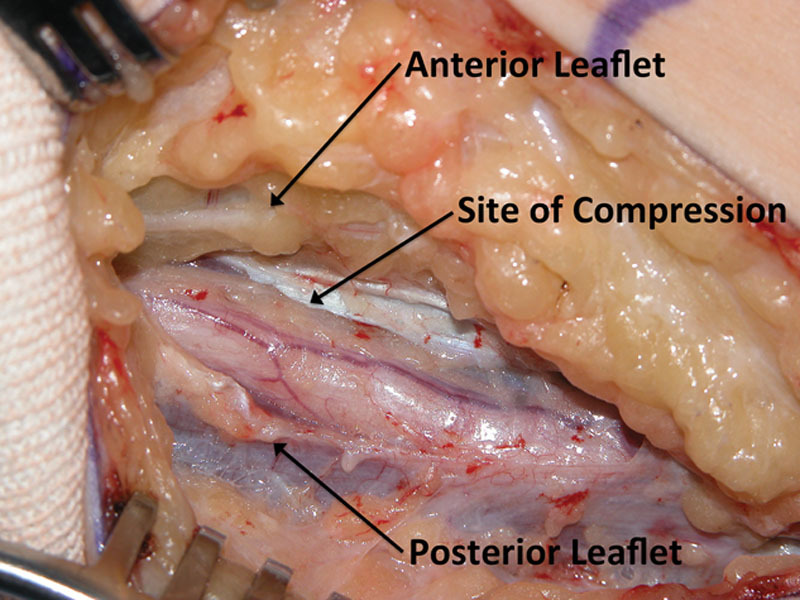
Intraoperative view of the ulnar nerve after release of the arcade of Struthers. Site of compression was seen 8 cm proximal to the medial epicondyle.
The incision was irrigated, and tourniquet was released; hemostasis was obtained using bipolar electrocautery. The incision was closed using 4-0 polysorb in a deep dermal fashion followed by 4-0 nylons for the skin. The wound was dressed with xeroform, 4 × 4, ABD pads, and a long arm splint was applied. The patient tolerated the procedure well and left the operative suite in stable condition; he had alleviation of symptoms at 8-week follow-up.
SUMMARY
Ochiai et al2 first reported ulnar entrapment neuropathy caused by the arcade of Struthers in 1992, and later reported 2 additional cases in 2000.3 In our case, the use of US imaging revealed an enlargement of the ulnar nerve 8 cm above the medial epicondyle. By localizing the suspected site of nerve entrapment, surgical decompression with complete release was facilitated.
Although the diagnosis of ulnar neuropathy relies on EMG, limitations include false-negative results and nonlocalizing findings.5 As US technology continues to advance, its diagnostic and therapeutic power increases. US imaging has many advantages—it is fast, painless, noninvasive, cost-effective, and dynamic. US imaging can localize compression sites, which is not possible via EMG.
US imaging is not without limitation as it relies on user technique and expertise. Few studies that have been published focus on ulnar neuropathy at the elbow and are limited by small sample size, lack of blinding, or lack of control groups.5 Beekman et al6 evaluated US image in ulnar neuropathy at the elbow, finding that symptomatic patients had a larger nerve diameter than controls (P < 0.0001). Nerve swelling is cascade of events occurring after compression including endoneurial edema, demyelination, inflammation, distal axonal degeneration, fibrosis, growth of new axons, remyelination, and thickening of the perineurium and endothelium.7
Although more studies need to be performed on the diagnostic value of US imaging for ulnar neuropathy, we have shown that it can be used in conjunction with EMG studies for localization. In ulnar entrapment above the elbow, which is less commonly found, US imaging localized the lesion, facilitating complete surgical release.
Footnotes
Disclosure: The authors have no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the authors.
REFERENCES
- 1.Bartels RH, Verbeek AL. Risk factors for ulnar nerve compression at the elbow: a case control study. Acta Neurochir (Wien) 2007;149:669–674; discussion 674. doi: 10.1007/s00701-007-1166-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ochiai N, Hayashi T, Ninomiya S. High ulnar nerve palsy caused by the arcade of Struthers. J Hand Surg Br. 1992;17:629–631. doi: 10.1016/0266-7681(92)90188-8. [DOI] [PubMed] [Google Scholar]
- 3.Ochiai N, Honmo J, Tsujino A, et al. Electrodiagnosis in entrapment neuropathy by the arcade of Struthers. Clin Orthop Relat Res. 2000;378:129–135. doi: 10.1097/00003086-200009000-00021. [DOI] [PubMed] [Google Scholar]
- 4.Scheidl E, Böhm J, Farbaky Z, et al. Ultrasonography of ulnar neuropathy at the elbow: axonal involvement leads to greater nerve swelling than demyelinating nerve lesion. Clin Neurophysiol. 2013;124:619–625. doi: 10.1016/j.clinph.2012.08.027. [DOI] [PubMed] [Google Scholar]
- 5.Beekman R, Van Der Plas JP, Uitdehaag BM, et al. Clinical, electrodiagnostic, and sonographic studies in ulnar neuropathy at the elbow. Muscle Nerve. 2004;30:202–208. doi: 10.1002/mus.20093. [DOI] [PubMed] [Google Scholar]
- 6.Beekman R, Schoemaker MC, Van Der Plas JP, et al. Diagnostic value of high-resolution sonography in ulnar neuropathy at the elbow. Neurology. 2004;62:767–773. doi: 10.1212/01.wnl.0000113733.62689.0d. [DOI] [PubMed] [Google Scholar]
- 7.Rempel D, Dahlin L, Lundborg G. Pathophysiology of nerve compression syndromes: response of peripheral nerves to loading. J Bone Joint Surg Am. 1999;81:1600–1610. doi: 10.2106/00004623-199911000-00013. [DOI] [PubMed] [Google Scholar]


